Nodal Drainage Patterns in the Head and Neck

- Slides: 46
Nodal Drainage Patterns in the Head and Neck: Recognizing Them and Why Not to Miss Them! Heba Albasha 1, Dave Reyes 1, Janelle Wang 1, Joseph Probst 1, 2, Audrey Erman 1, 3, Rihan Khan 1, 2 University of Arizona College of Medicine 1 Banner – University Medical Center Departments of Radiology 1, Otolaryngology 3 Tucson, AZ ASNR 2016 e. Ed. E#: e. Ed. E-112 Control #: 2380
None of the authors have any relevant disclosures
Educational Goals 1. To familiarize the reader with nodal metastatic drainage patterns using a multitude of MRI cases of head and neck primary cancers with typical nodal metastatic patterns. 2. Review of patterns of cervical nodal metastatic spread of tumor on both 1. 5 T and 3. 0 T MRI. Conventional and advanced imaging will be included. 3. Anatomical nodal level review utilizing both MRI anatomy and supporting schematic drawings.
Outline • Clinical significance of nodal metastases • Lymph node level diagram • Head and neck cancer drainage pathways • Cases!
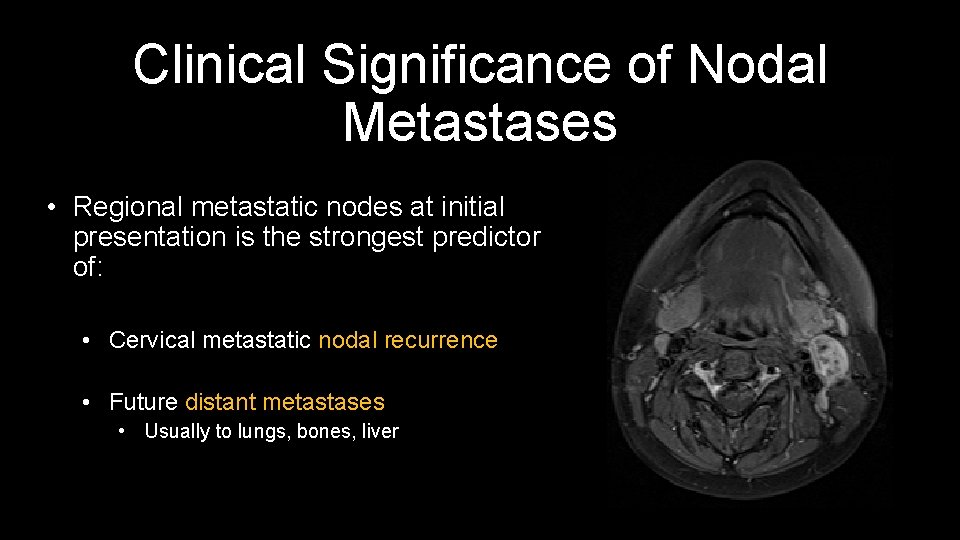
Clinical Significance of Nodal Metastases • Regional metastatic nodes at initial presentation is the strongest predictor of: • Cervical metastatic nodal recurrence • Future distant metastases • Usually to lungs, bones, liver
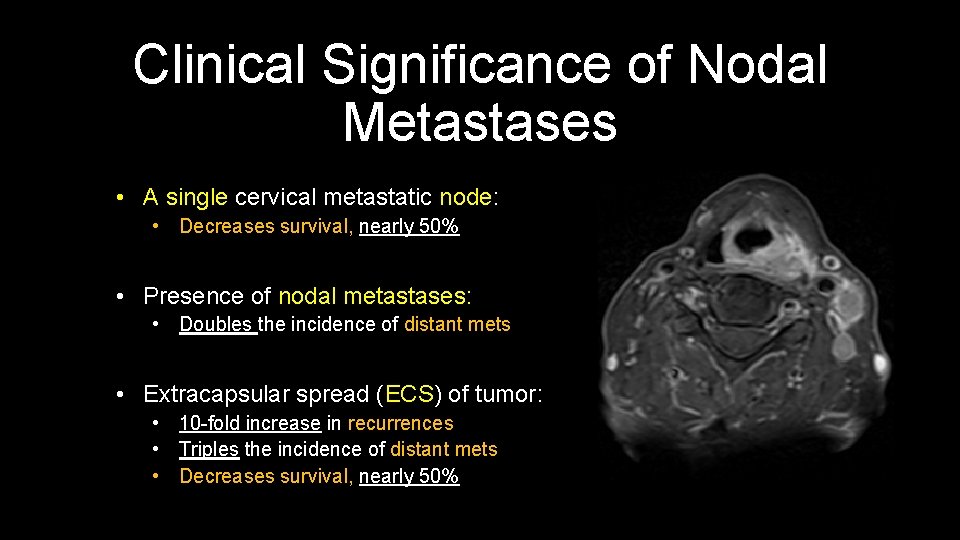
Clinical Significance of Nodal Metastases • A single cervical metastatic node: • Decreases survival, nearly 50% • Presence of nodal metastases: • Doubles the incidence of distant mets • Extracapsular spread (ECS) of tumor: • 10 -fold increase in recurrences • Triples the incidence of distant mets • Decreases survival, nearly 50%

Clinical Significance of Nodal Metastases • 15% of node negative necks develop metastatic disease (considering all upper aerodigestive tract sites) • Independent predictors of occult metastases: • • • Tumor site T stage Tumor thickness Histologic grade Vascular embolization Perineural infiltration
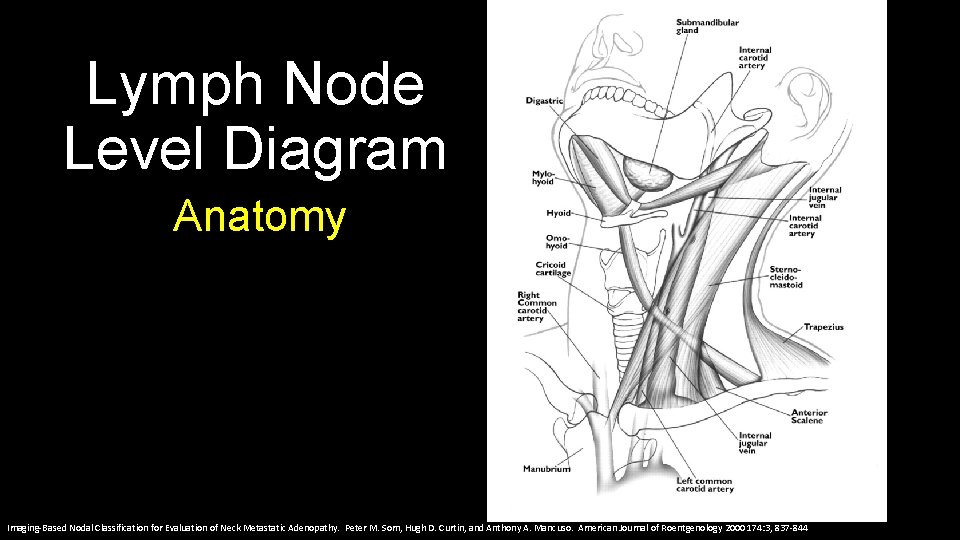
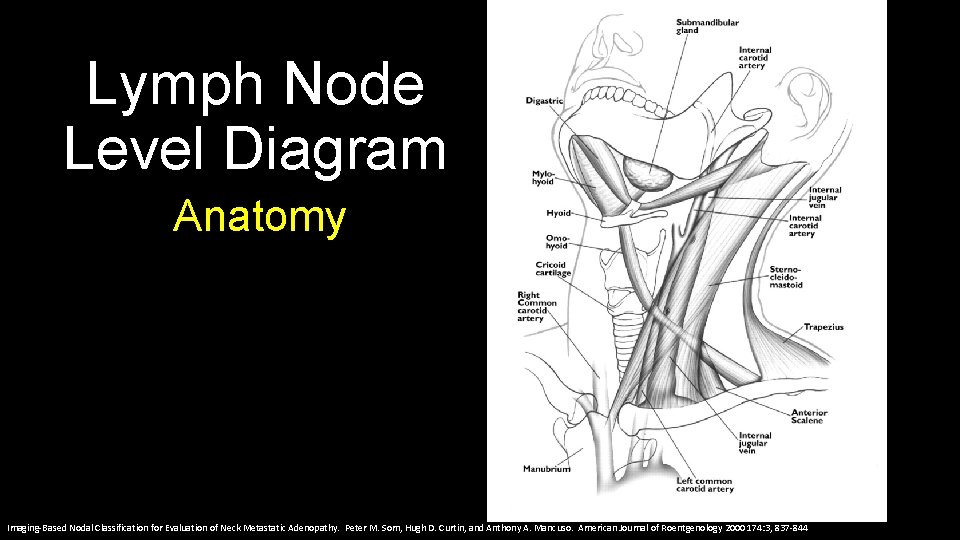
Lymph Node Level Diagram Anatomy Imaging-Based Nodal Classification for Evaluation of Neck Metastatic Adenopathy. Peter M. Som, Hugh D. Curtin, and Anthony A. Mancuso. American Journal of Roentgenology 2000 174: 3, 837 -844
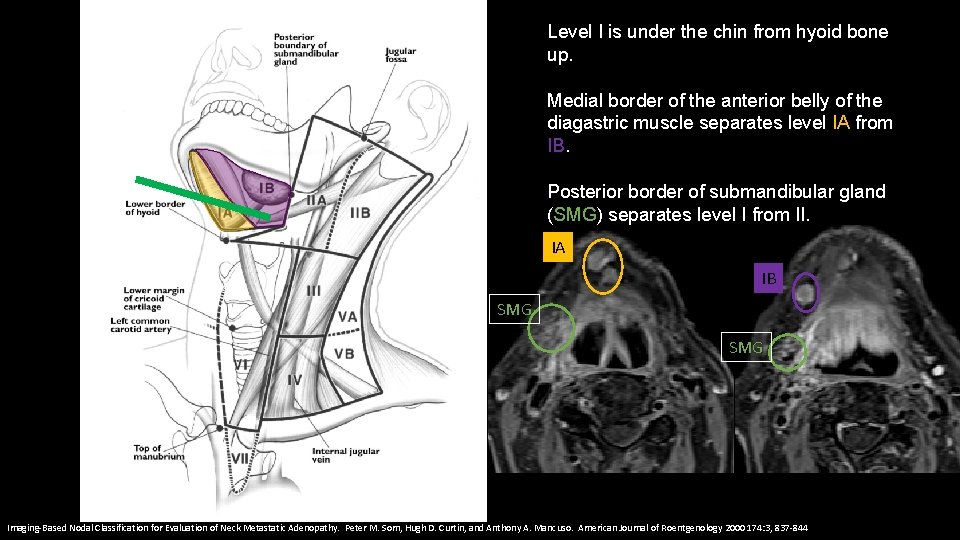
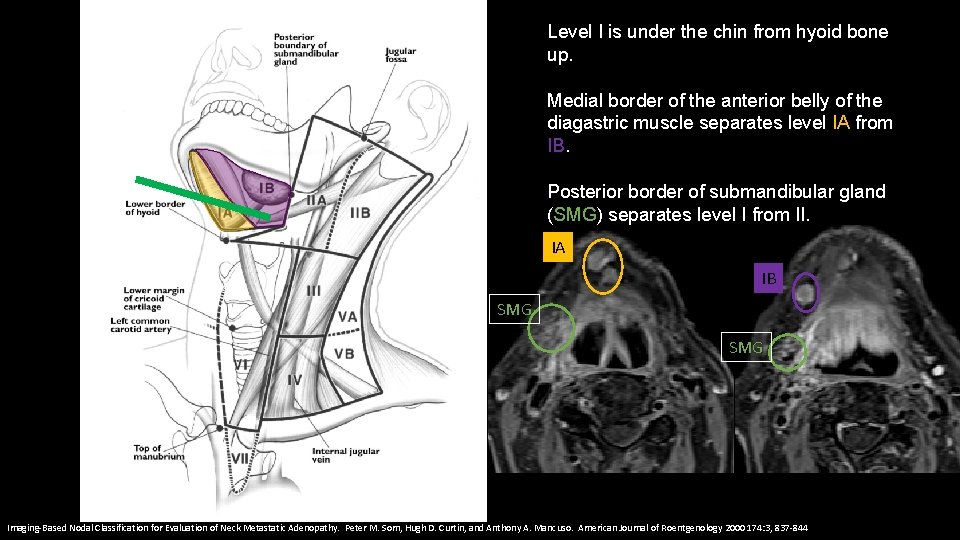
Level I is under the chin from hyoid bone up. Medial border of the anterior belly of the diagastric muscle separates level IA from IB. Posterior border of submandibular gland (SMG) separates level I from II. IA IB SMG Imaging-Based Nodal Classification for Evaluation of Neck Metastatic Adenopathy. Peter M. Som, Hugh D. Curtin, and Anthony A. Mancuso. American Journal of Roentgenology 2000 174: 3, 837 -844
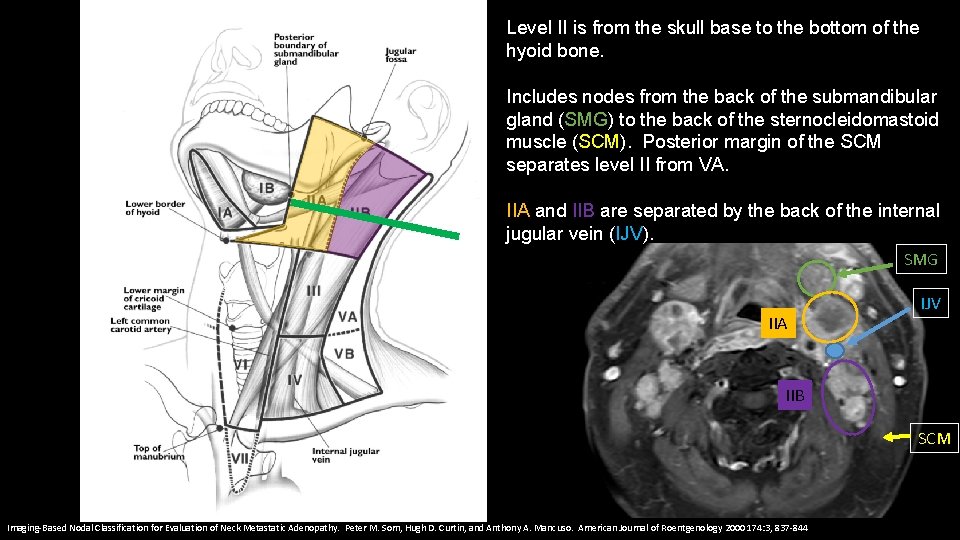
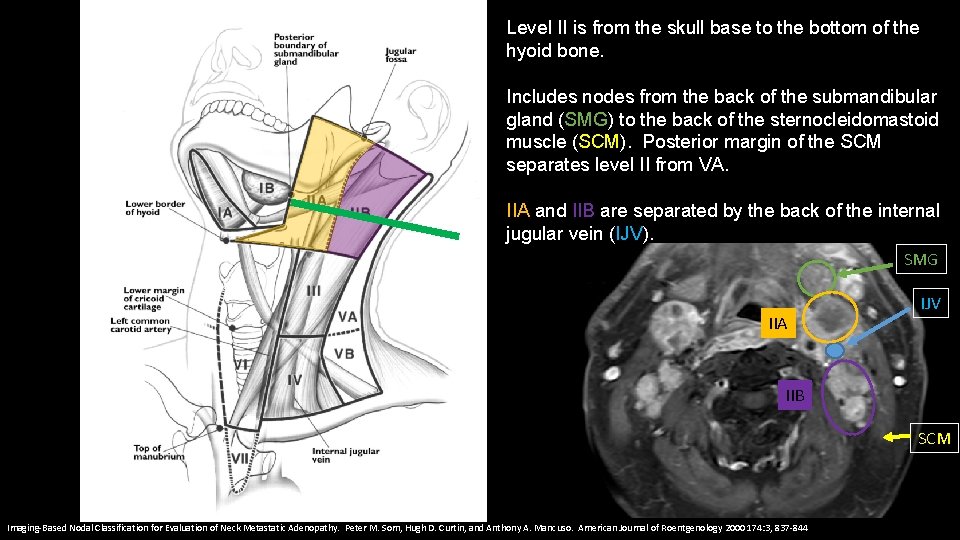
Level II is from the skull base to the bottom of the hyoid bone. Includes nodes from the back of the submandibular gland (SMG) to the back of the sternocleidomastoid muscle (SCM). Posterior margin of the SCM separates level II from VA. IIA and IIB are separated by the back of the internal jugular vein (IJV). SMG IIA IJV IIB SCM Imaging-Based Nodal Classification for Evaluation of Neck Metastatic Adenopathy. Peter M. Som, Hugh D. Curtin, and Anthony A. Mancuso. American Journal of Roentgenology 2000 174: 3, 837 -844
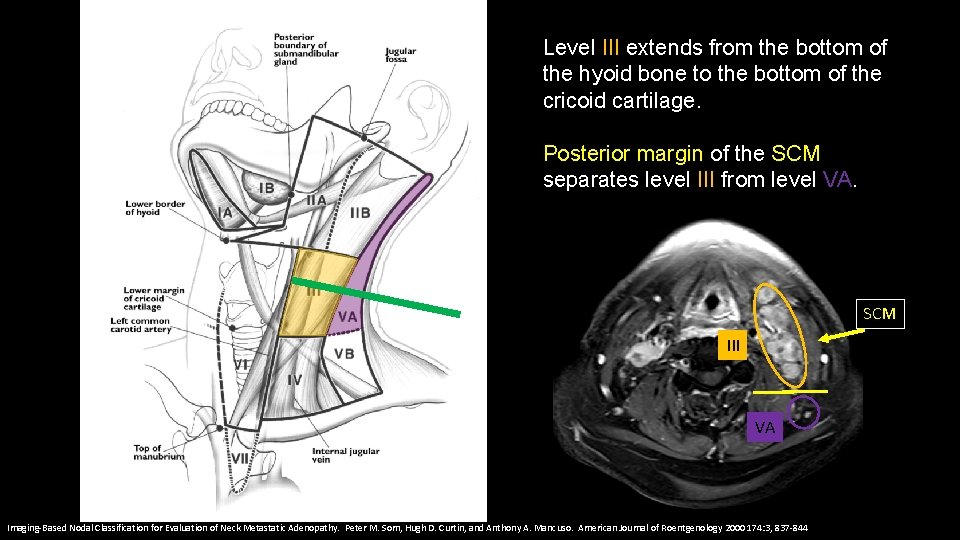
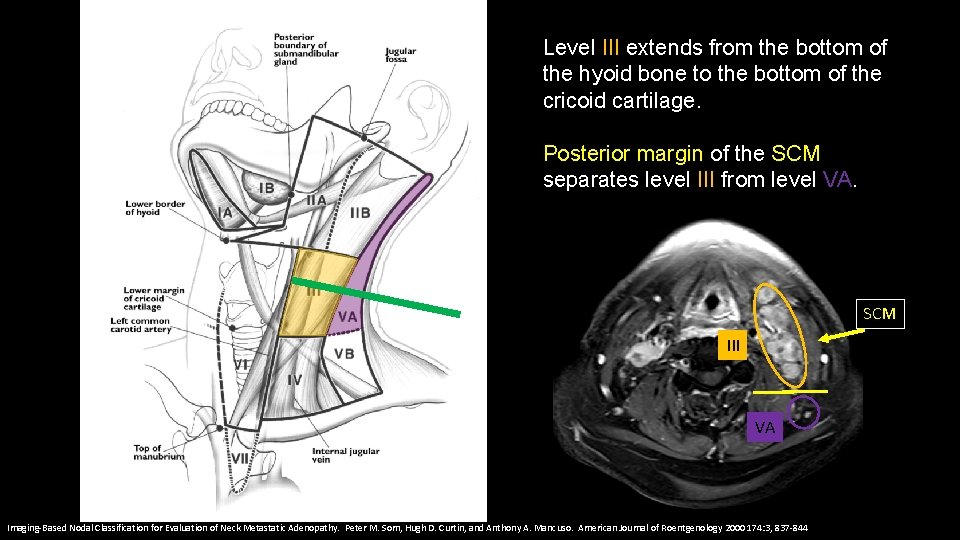
Level III extends from the bottom of the hyoid bone to the bottom of the cricoid cartilage. Posterior margin of the SCM separates level III from level VA. SCM III VA Imaging-Based Nodal Classification for Evaluation of Neck Metastatic Adenopathy. Peter M. Som, Hugh D. Curtin, and Anthony A. Mancuso. American Journal of Roentgenology 2000 174: 3, 837 -844
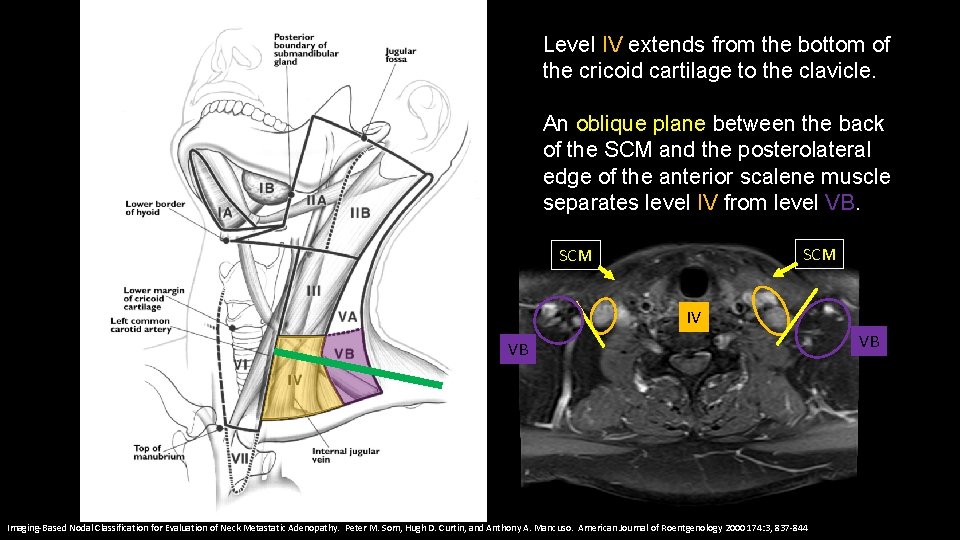
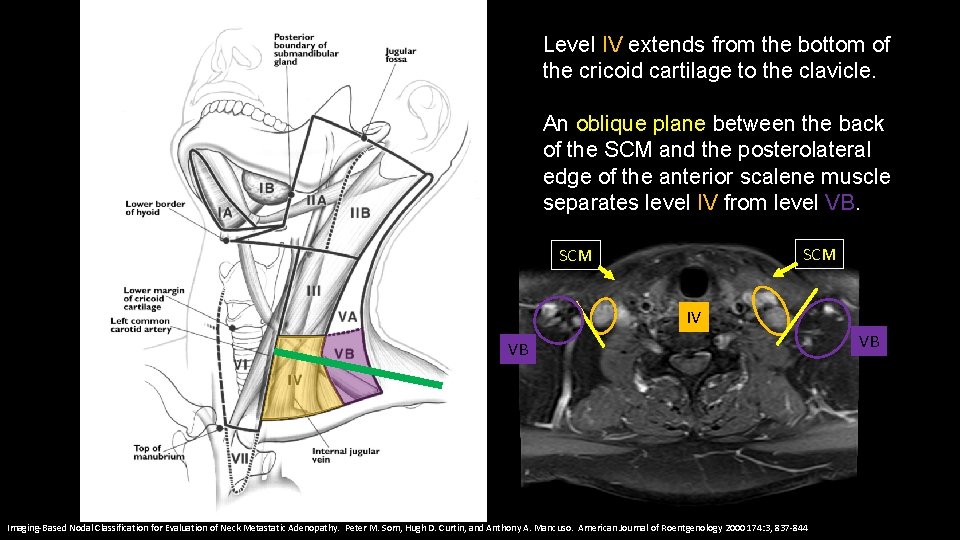
Level IV extends from the bottom of the cricoid cartilage to the clavicle. An oblique plane between the back of the SCM and the posterolateral edge of the anterior scalene muscle separates level IV from level VB. SCM IV VB Imaging-Based Nodal Classification for Evaluation of Neck Metastatic Adenopathy. Peter M. Som, Hugh D. Curtin, and Anthony A. Mancuso. American Journal of Roentgenology 2000 174: 3, 837 -844 VB
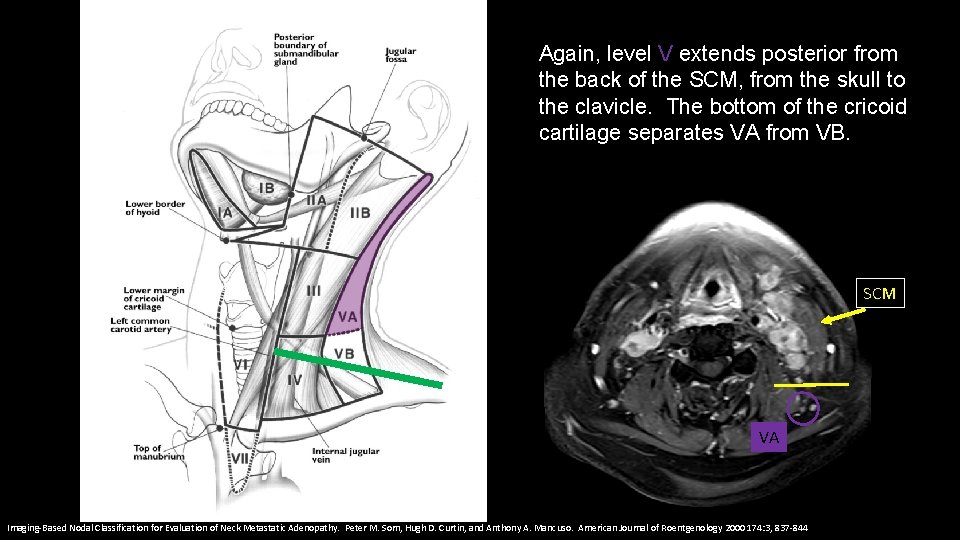
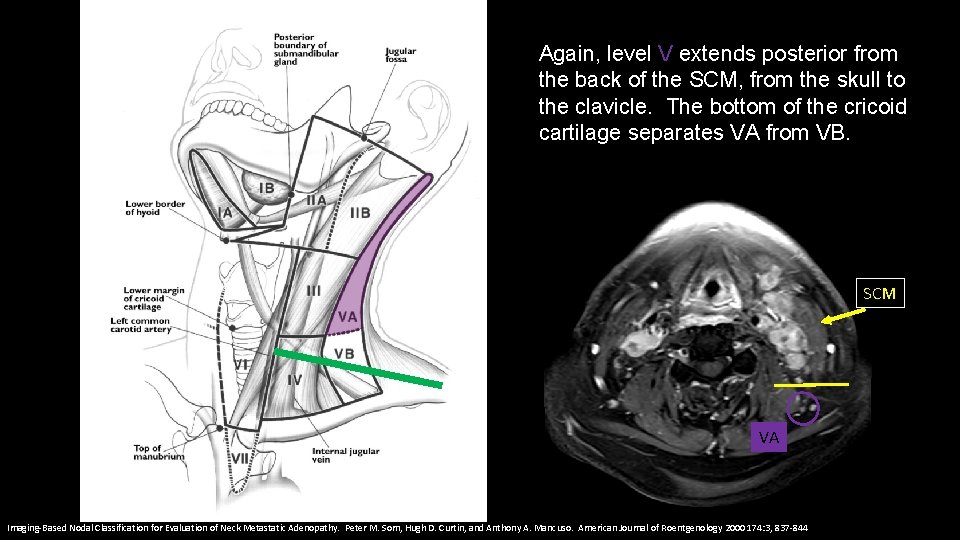
Again, level V extends posterior from the back of the SCM, from the skull to the clavicle. The bottom of the cricoid cartilage separates VA from VB. SCM VA Imaging-Based Nodal Classification for Evaluation of Neck Metastatic Adenopathy. Peter M. Som, Hugh D. Curtin, and Anthony A. Mancuso. American Journal of Roentgenology 2000 174: 3, 837 -844
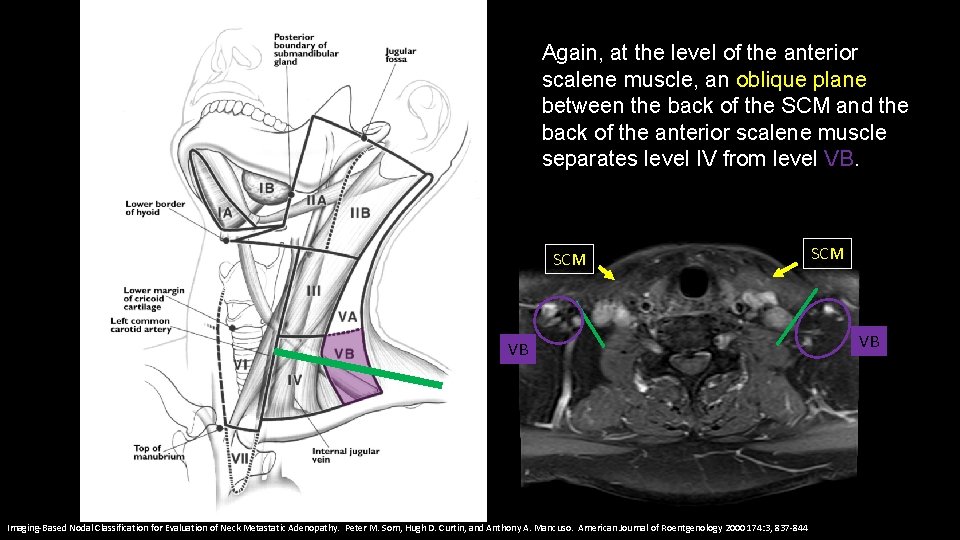
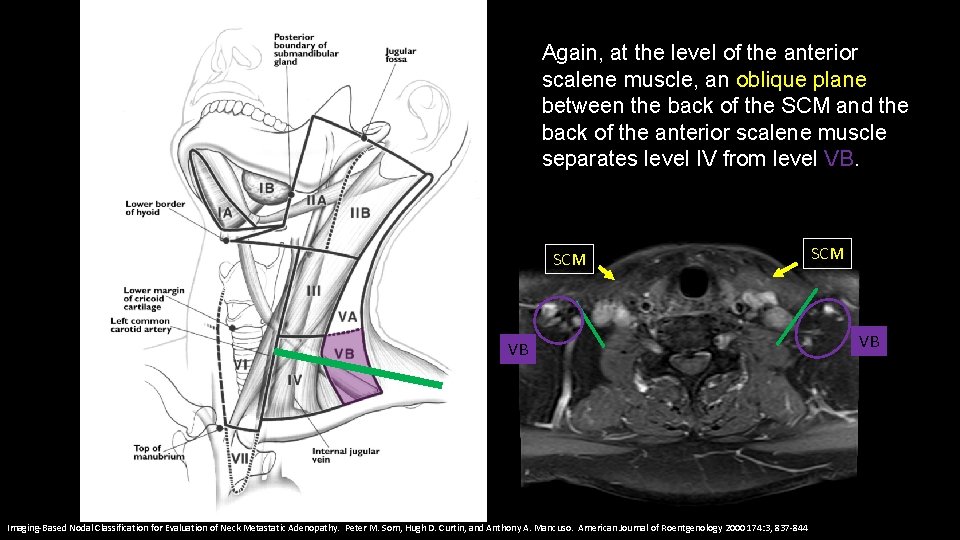
Again, at the level of the anterior scalene muscle, an oblique plane between the back of the SCM and the back of the anterior scalene muscle separates level IV from level VB. SCM VB Imaging-Based Nodal Classification for Evaluation of Neck Metastatic Adenopathy. Peter M. Som, Hugh D. Curtin, and Anthony A. Mancuso. American Journal of Roentgenology 2000 174: 3, 837 -844 SCM VB
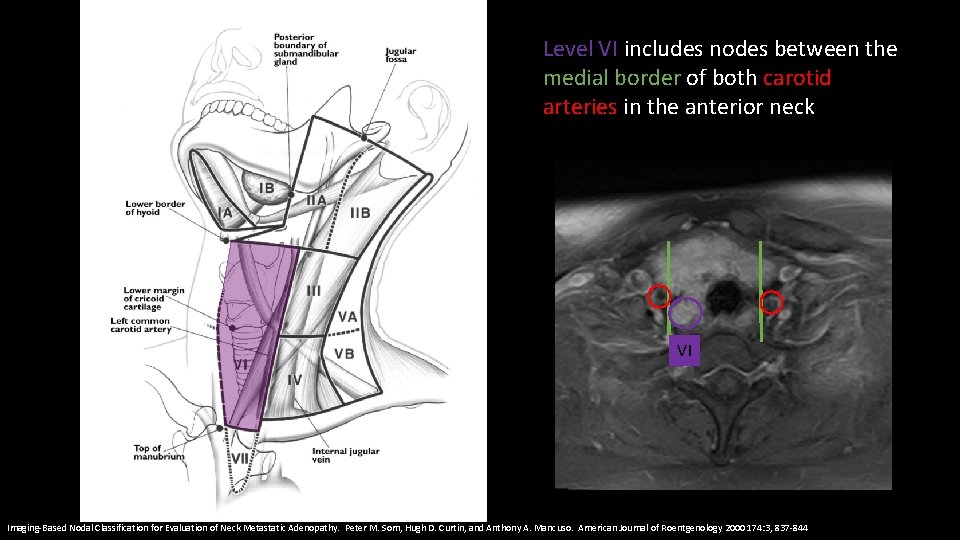
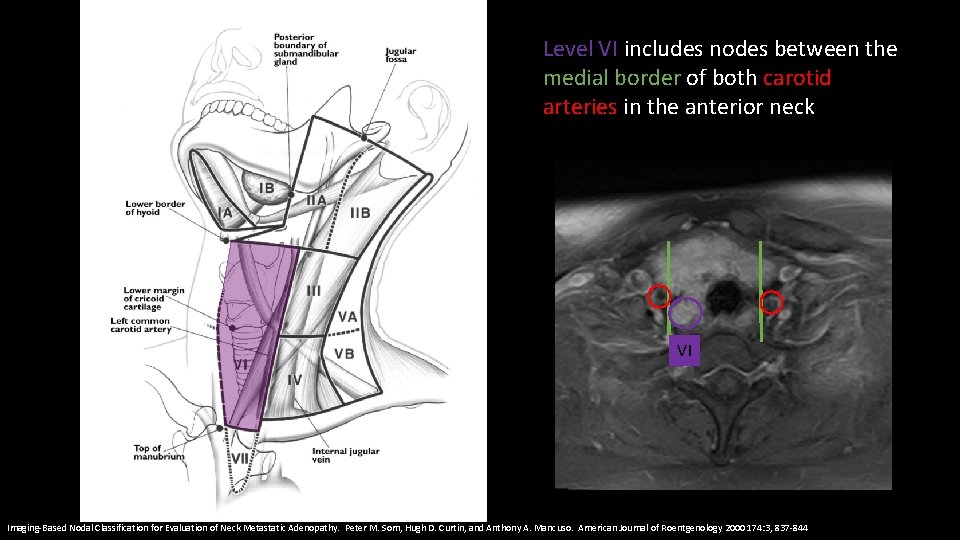
Level VI includes nodes between the medial border of both carotid arteries in the anterior neck VI Imaging-Based Nodal Classification for Evaluation of Neck Metastatic Adenopathy. Peter M. Som, Hugh D. Curtin, and Anthony A. Mancuso. American Journal of Roentgenology 2000 174: 3, 837 -844
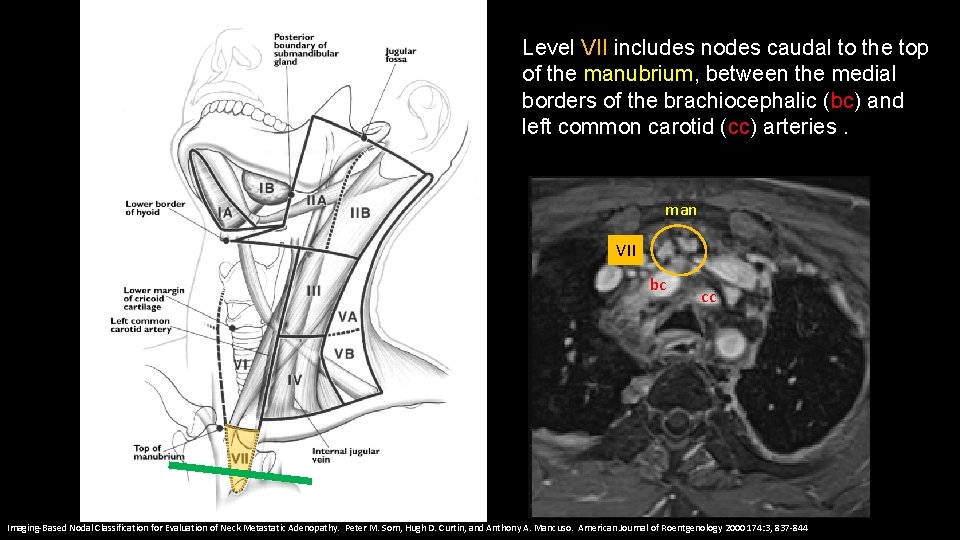
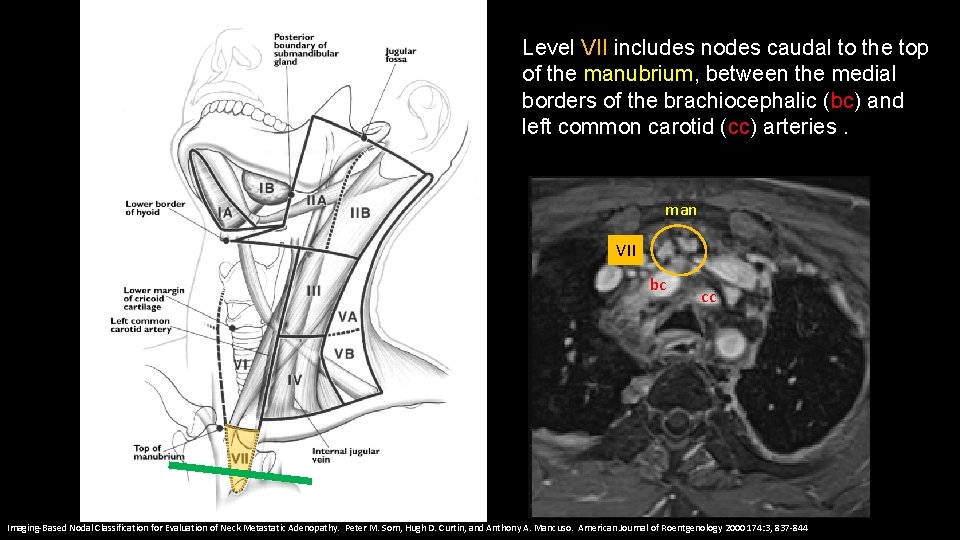
Level VII includes nodes caudal to the top of the manubrium, between the medial borders of the brachiocephalic (bc) and left common carotid (cc) arteries. man VII bc cc Imaging-Based Nodal Classification for Evaluation of Neck Metastatic Adenopathy. Peter M. Som, Hugh D. Curtin, and Anthony A. Mancuso. American Journal of Roentgenology 2000 174: 3, 837 -844
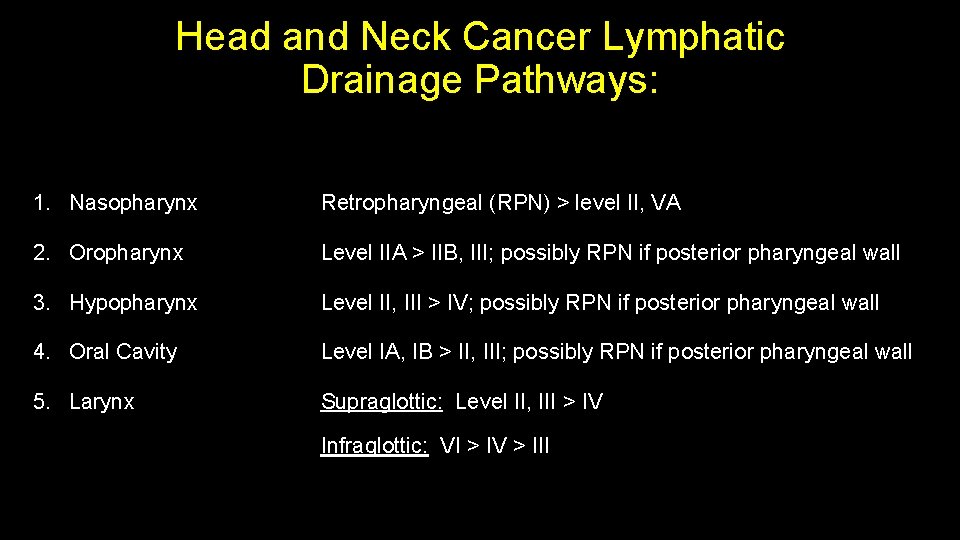
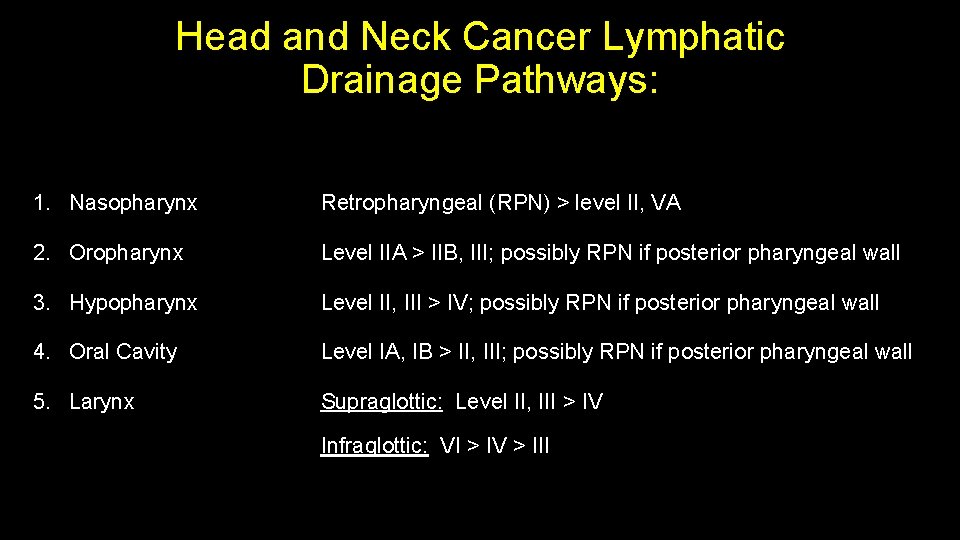
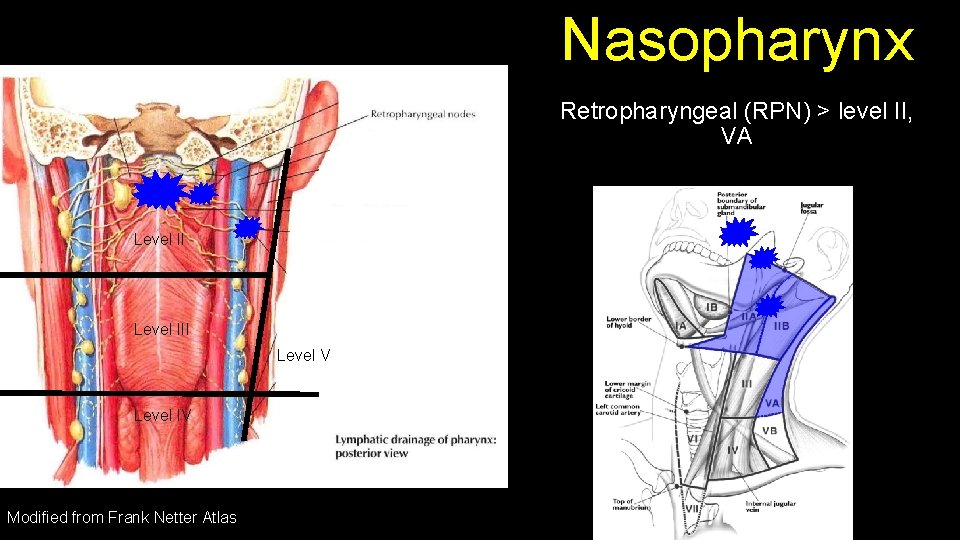
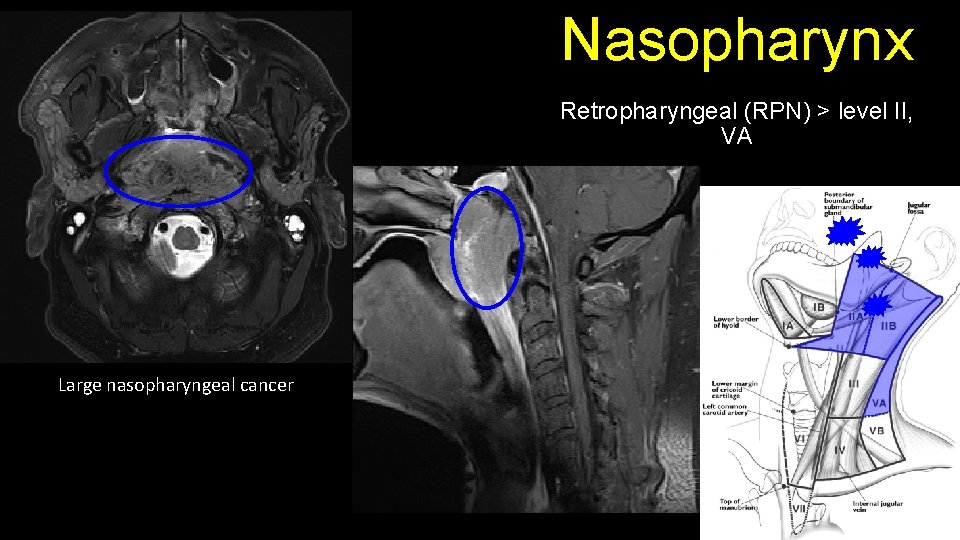
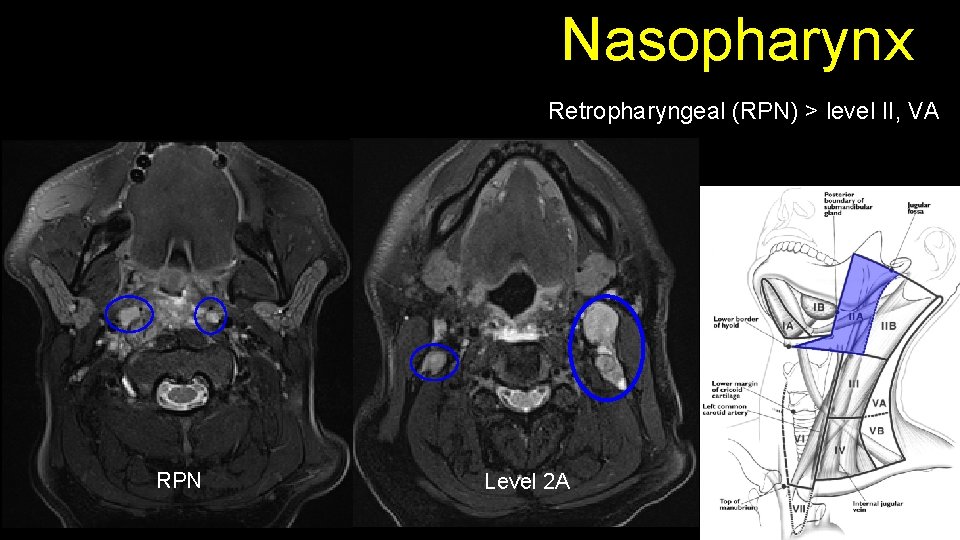
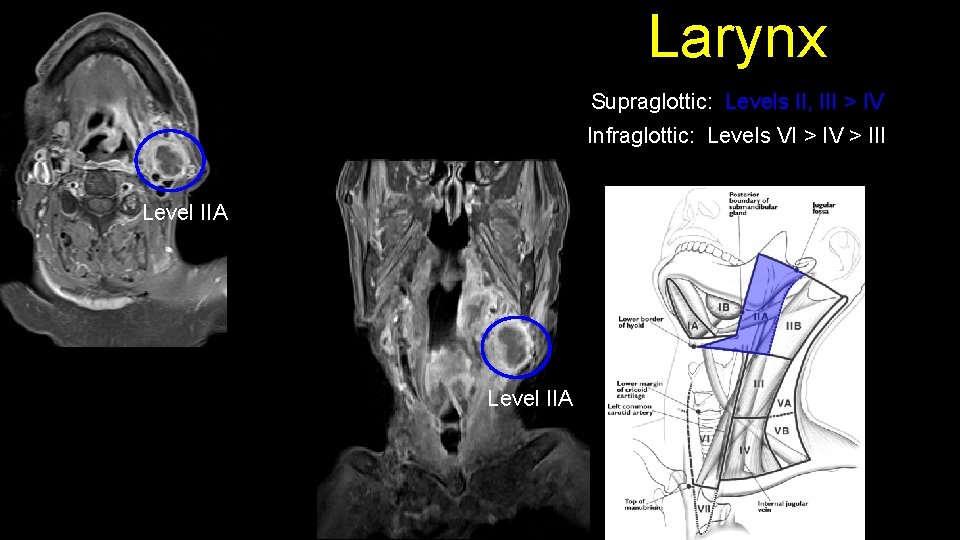
Head and Neck Cancer Lymphatic Drainage Pathways: 1. Nasopharynx Retropharyngeal (RPN) > level II, VA 2. Oropharynx Level IIA > IIB, III; possibly RPN if posterior pharyngeal wall 3. Hypopharynx Level II, III > IV; possibly RPN if posterior pharyngeal wall 4. Oral Cavity Level IA, IB > II, III; possibly RPN if posterior pharyngeal wall 5. Larynx Supraglottic: Level II, III > IV Infraglottic: VI > IV > III
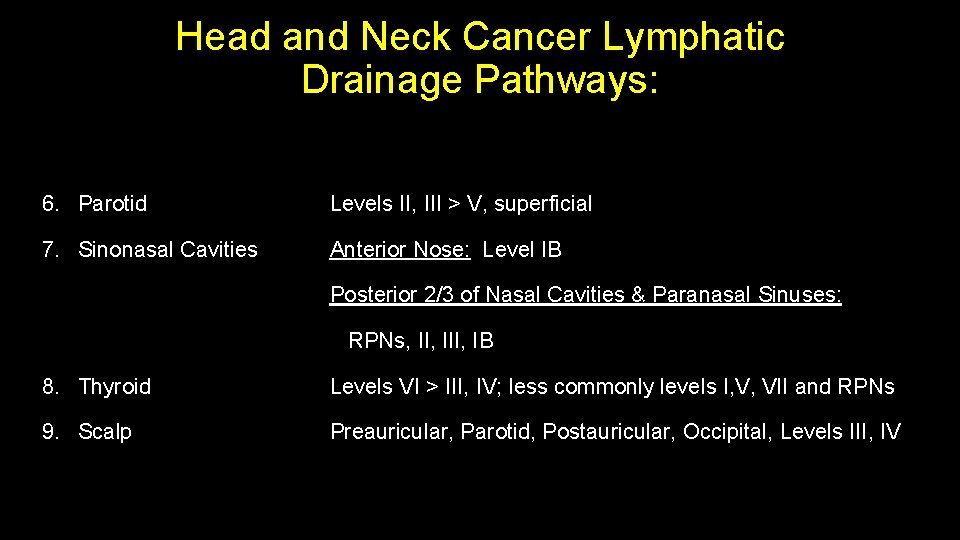
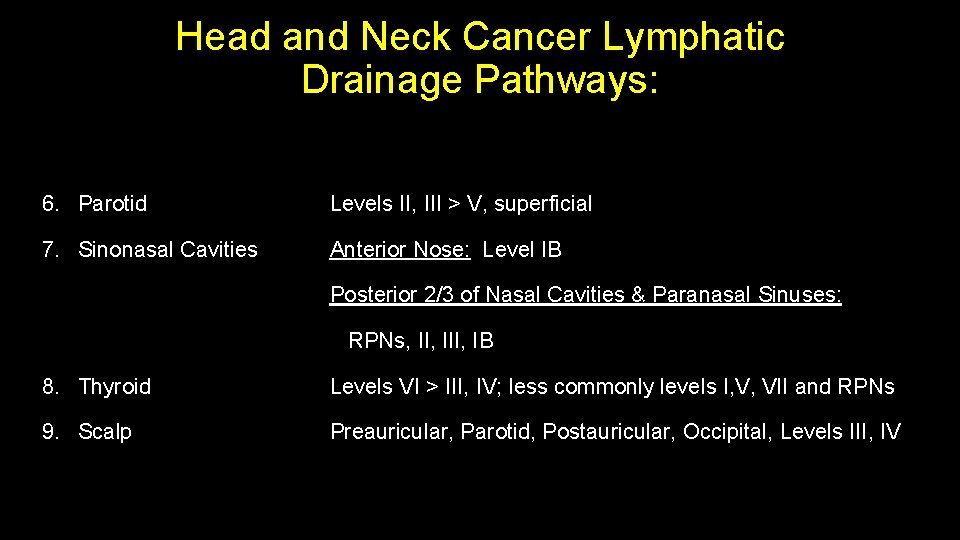
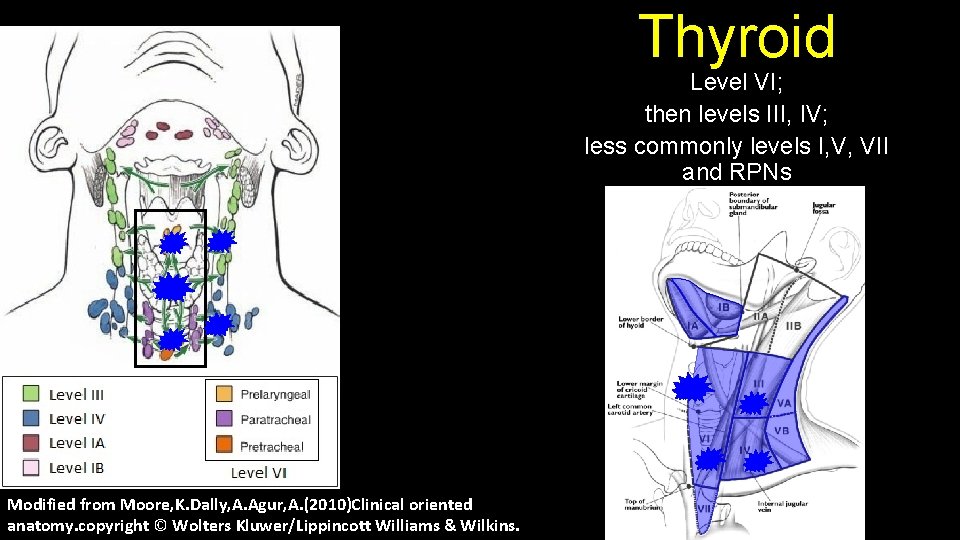
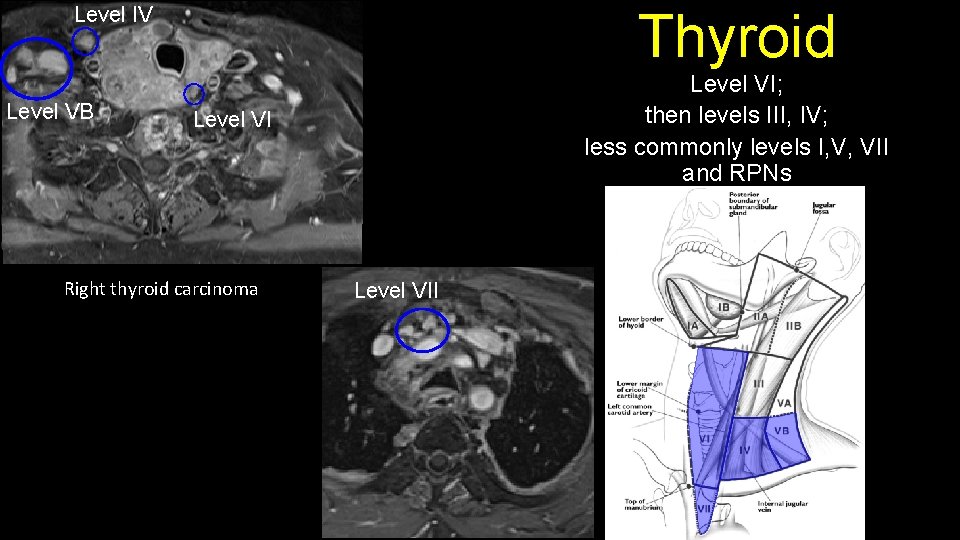
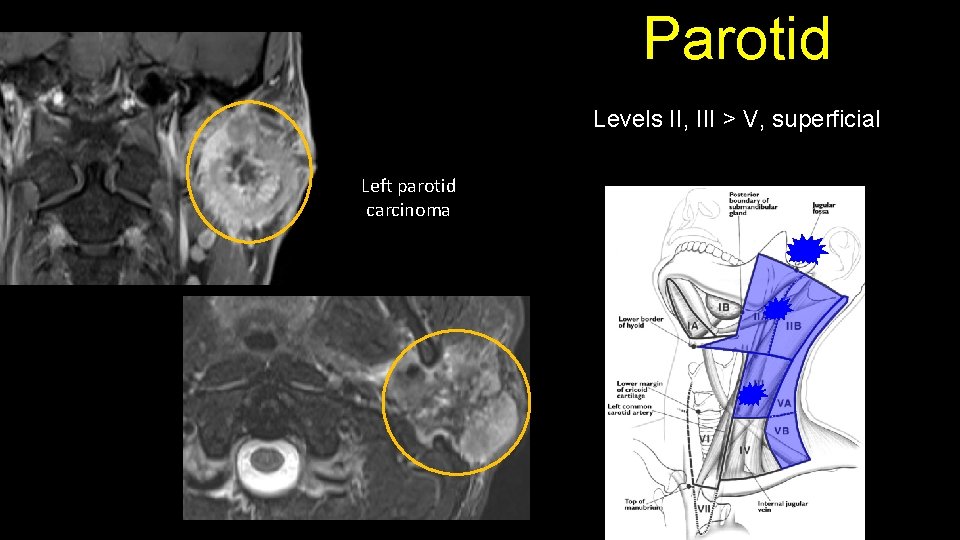
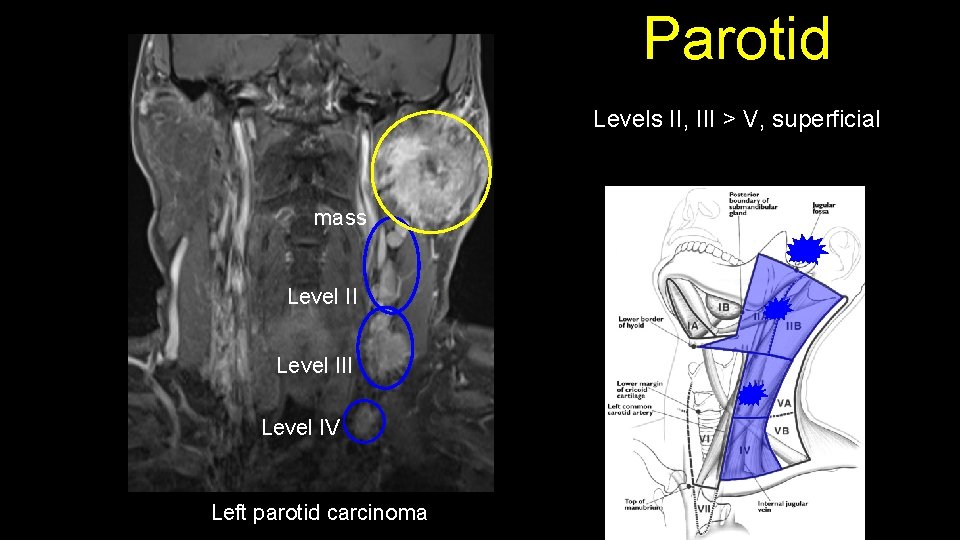
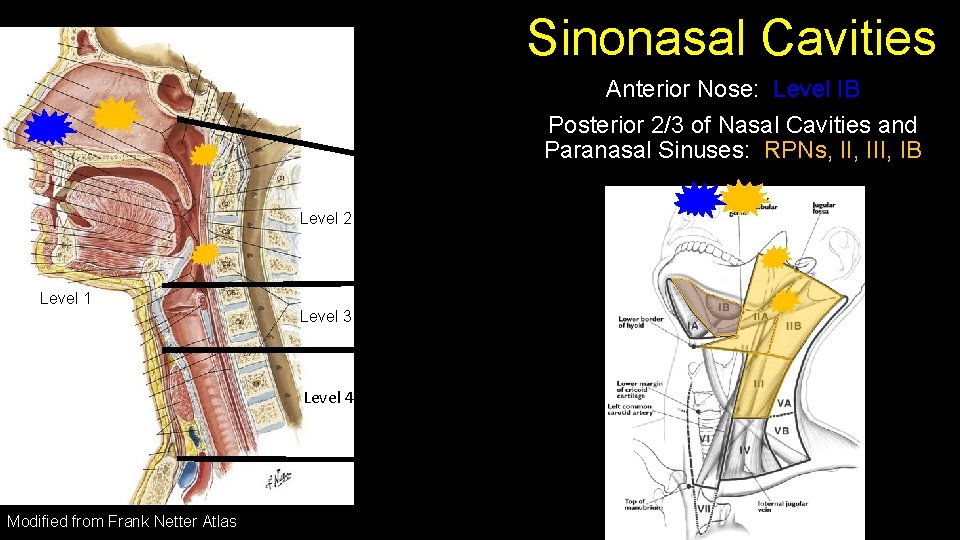
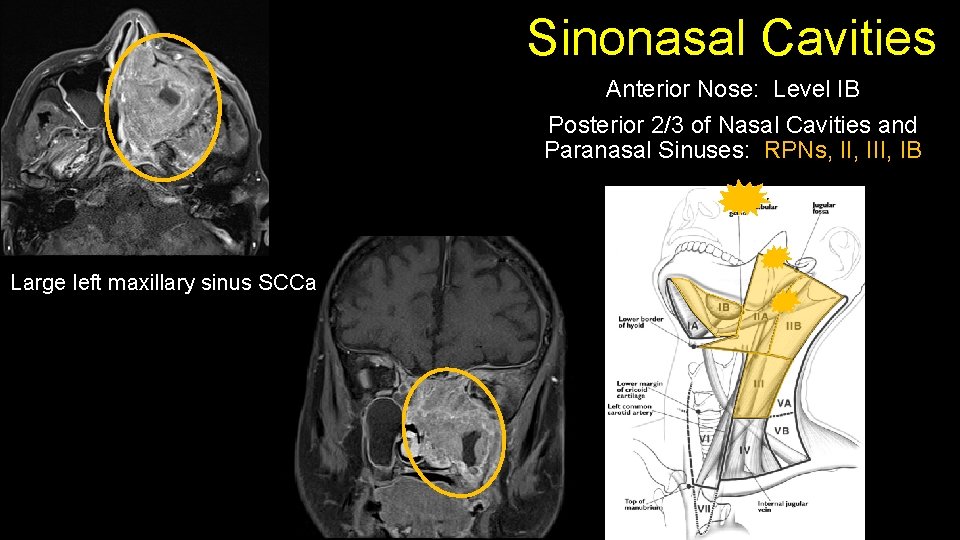
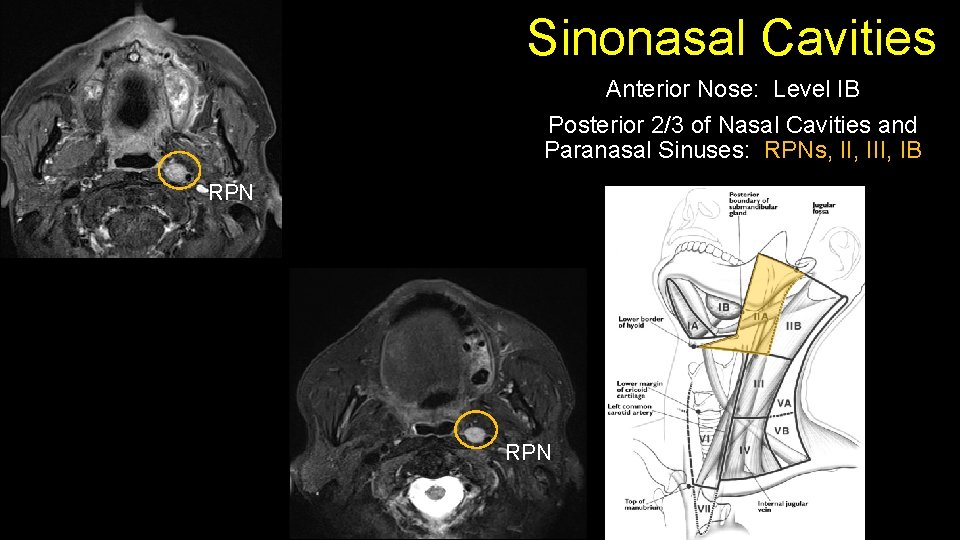
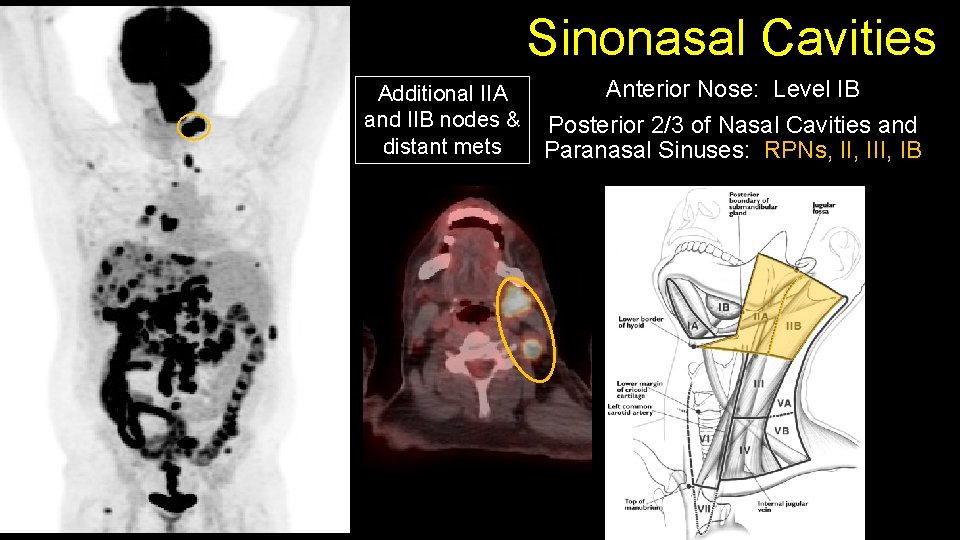
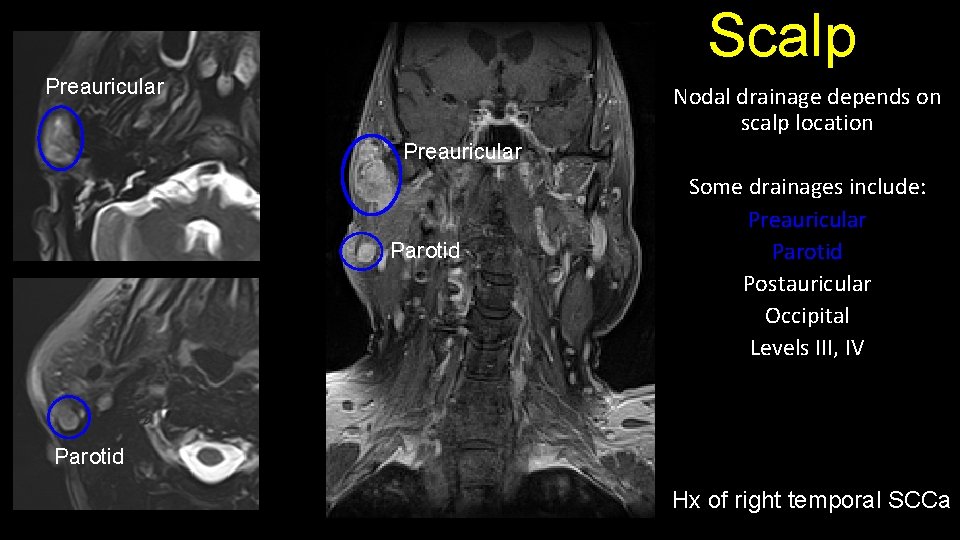
Head and Neck Cancer Lymphatic Drainage Pathways: 6. Parotid Levels II, III > V, superficial 7. Sinonasal Cavities Anterior Nose: Level IB Posterior 2/3 of Nasal Cavities & Paranasal Sinuses: RPNs, III, IB 8. Thyroid Levels VI > III, IV; less commonly levels I, V, VII and RPNs 9. Scalp Preauricular, Parotid, Postauricular, Occipital, Levels III, IV
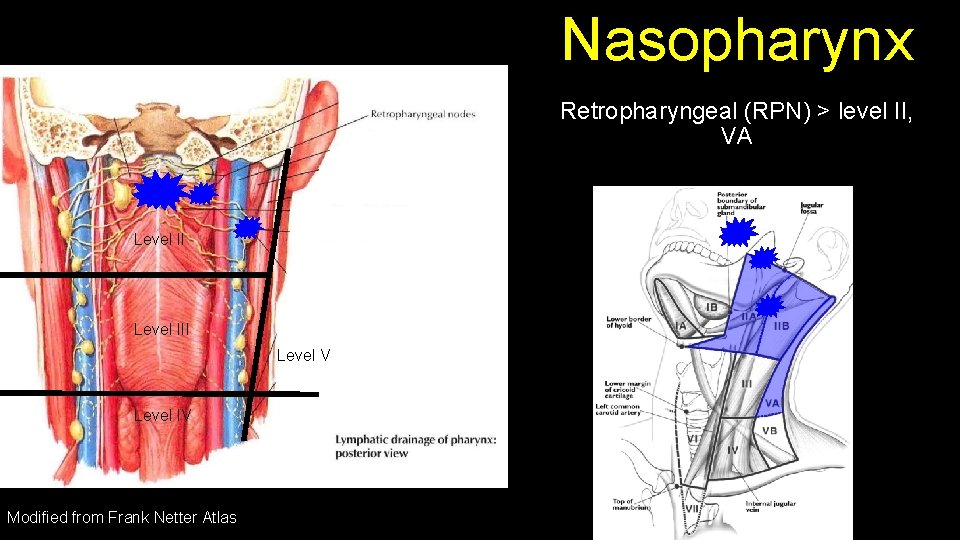
Nasopharynx Retropharyngeal (RPN) > level II, VA Level III Level V Level IV Modified from Frank Netter Atlas
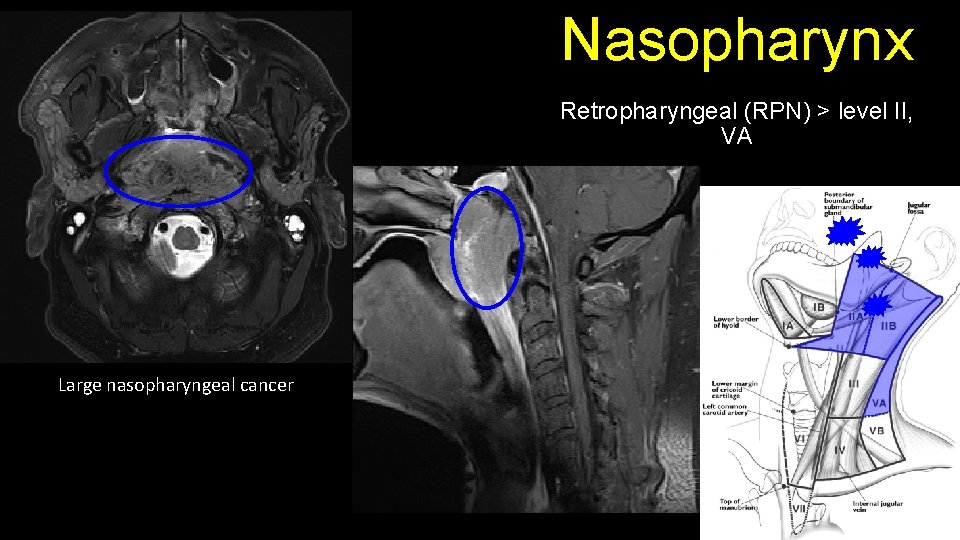
Nasopharynx Retropharyngeal (RPN) > level II, VA Large nasopharyngeal cancer
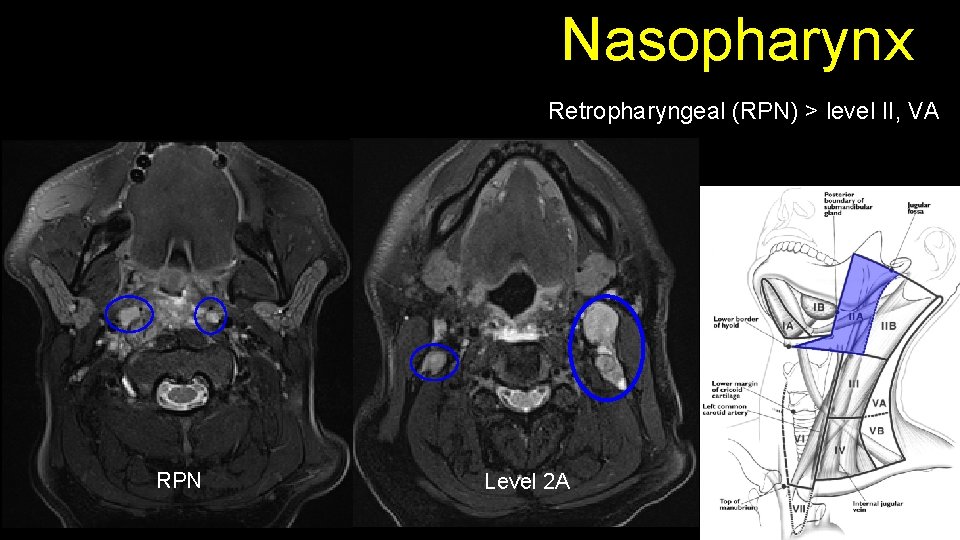
Nasopharynx Retropharyngeal (RPN) > level II, VA RPN Level 2 A
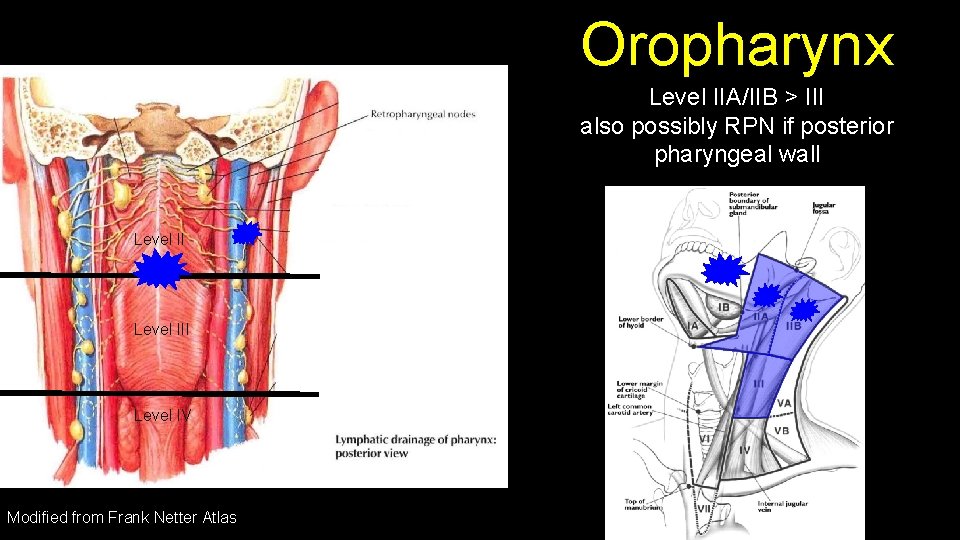
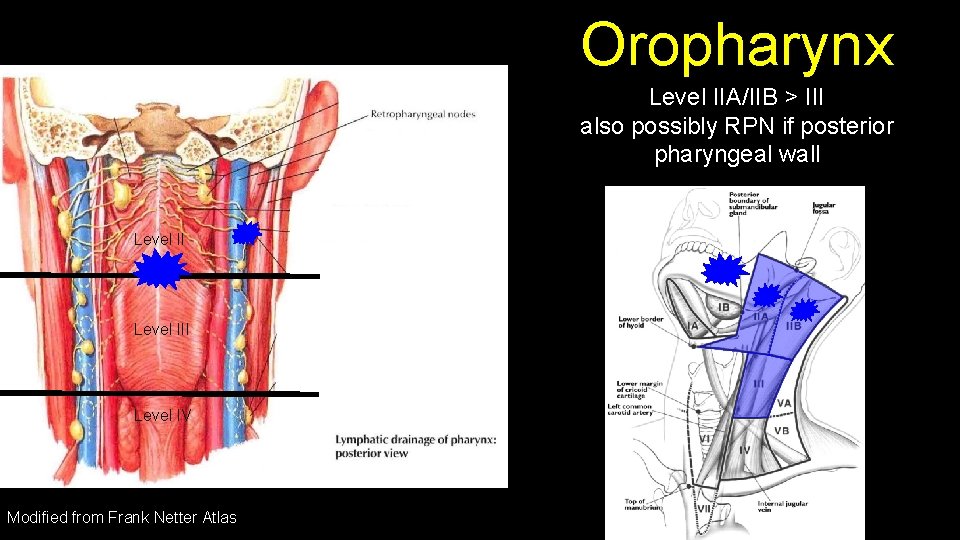
Oropharynx Level IIA/IIB > III also possibly RPN if posterior pharyngeal wall Level III Level IV Modified from Frank Netter Atlas
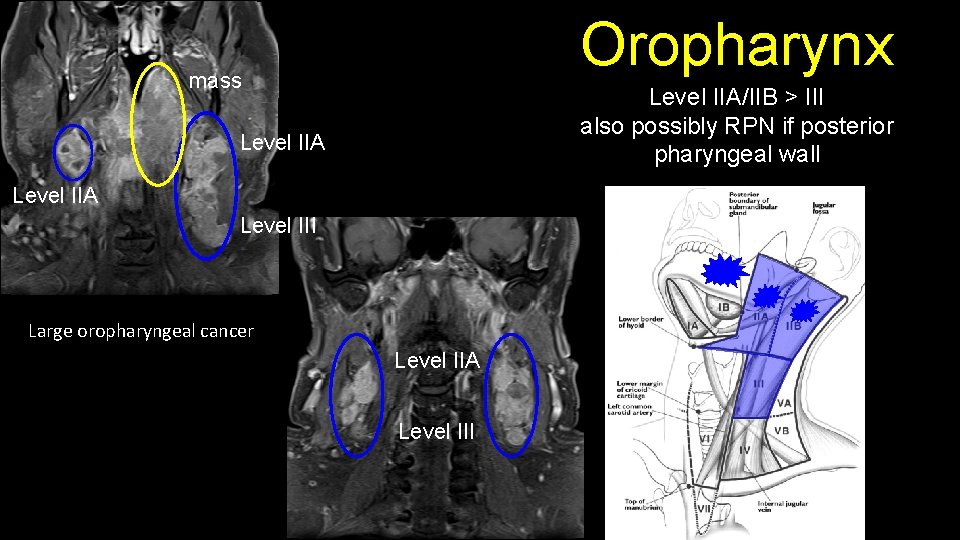
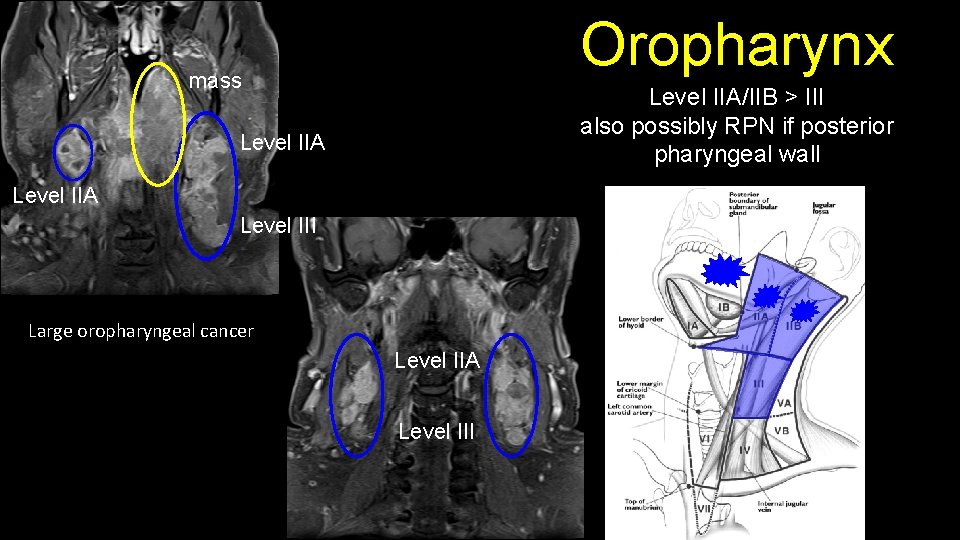
Oropharynx mass Level IIA/IIB > III also possibly RPN if posterior pharyngeal wall Level IIA Level III Large oropharyngeal cancer Level IIA Level III
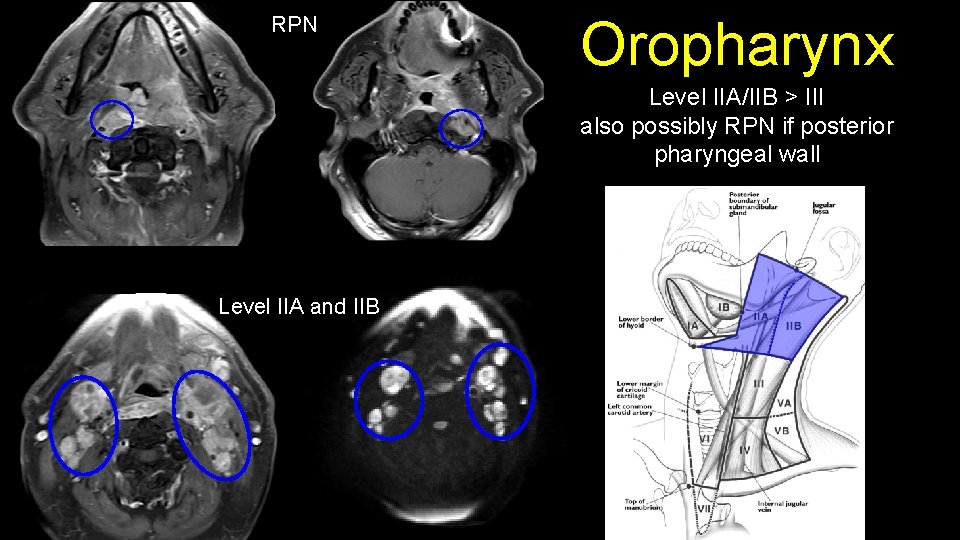
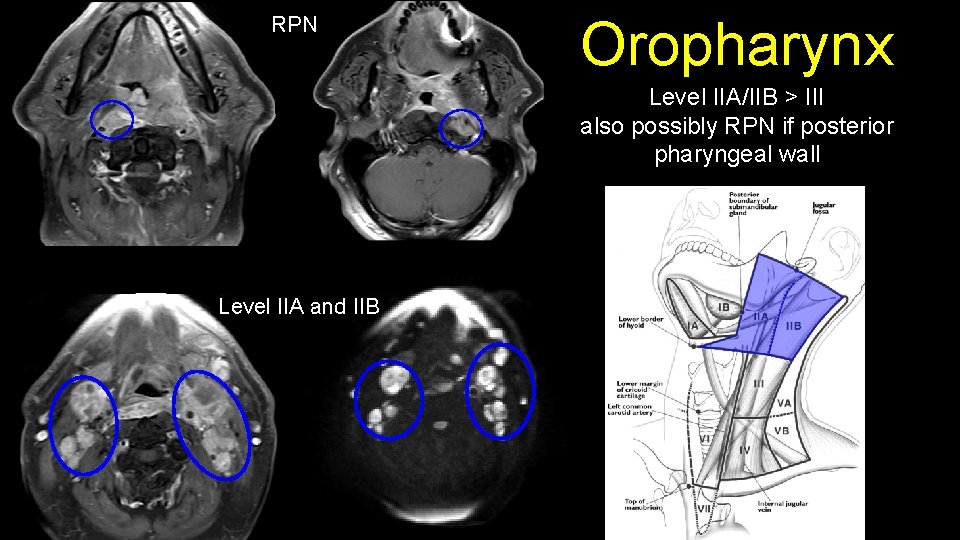
RPN Oropharynx Level IIA/IIB > III also possibly RPN if posterior pharyngeal wall Level IIA and IIB
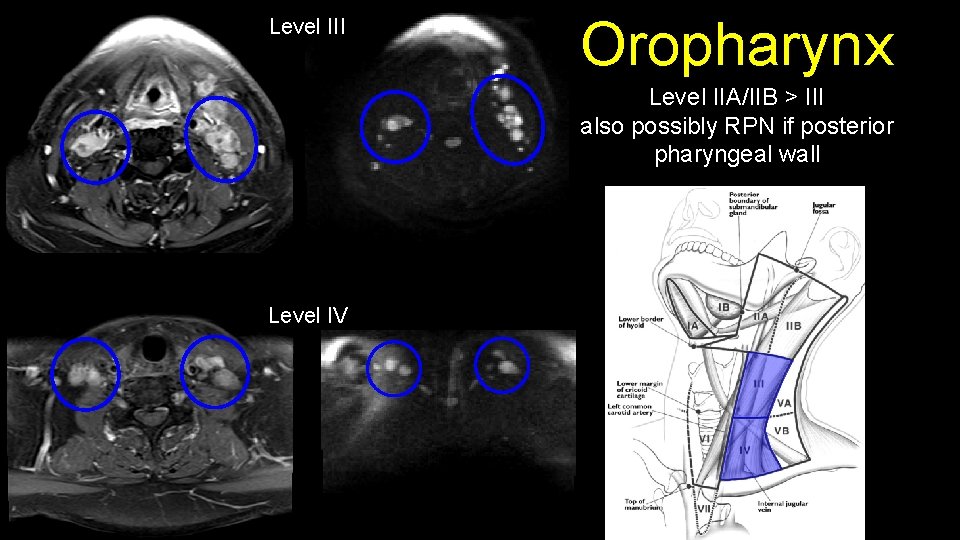
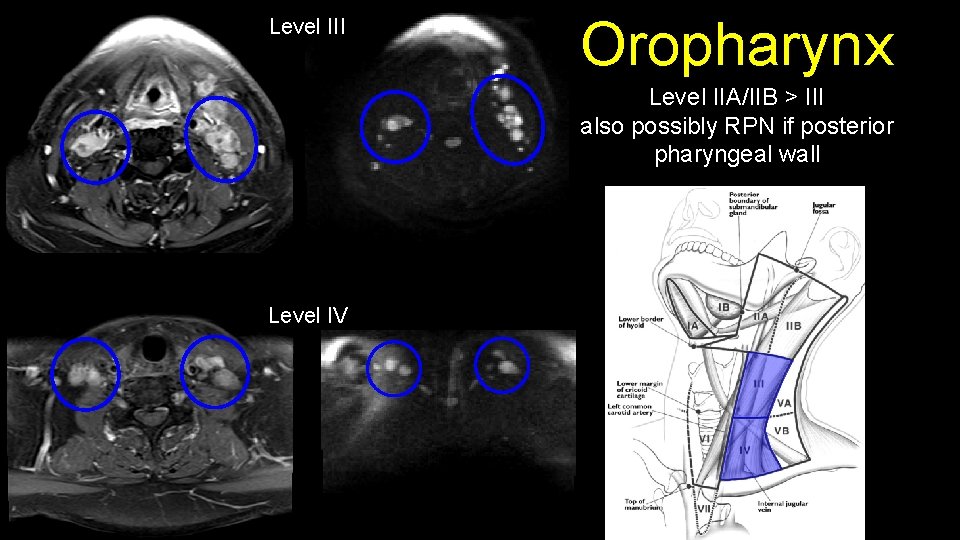
Level III Oropharynx Level IIA/IIB > III also possibly RPN if posterior pharyngeal wall Level IV
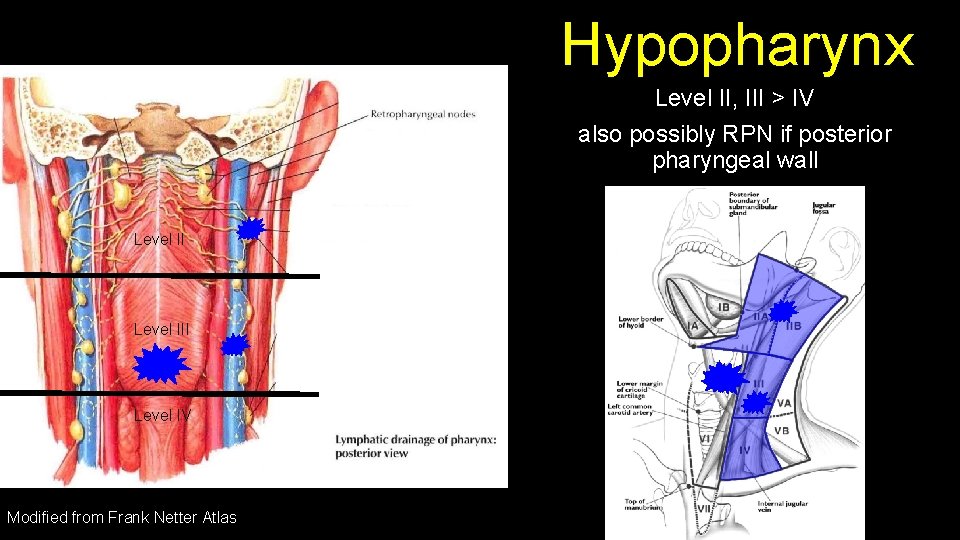
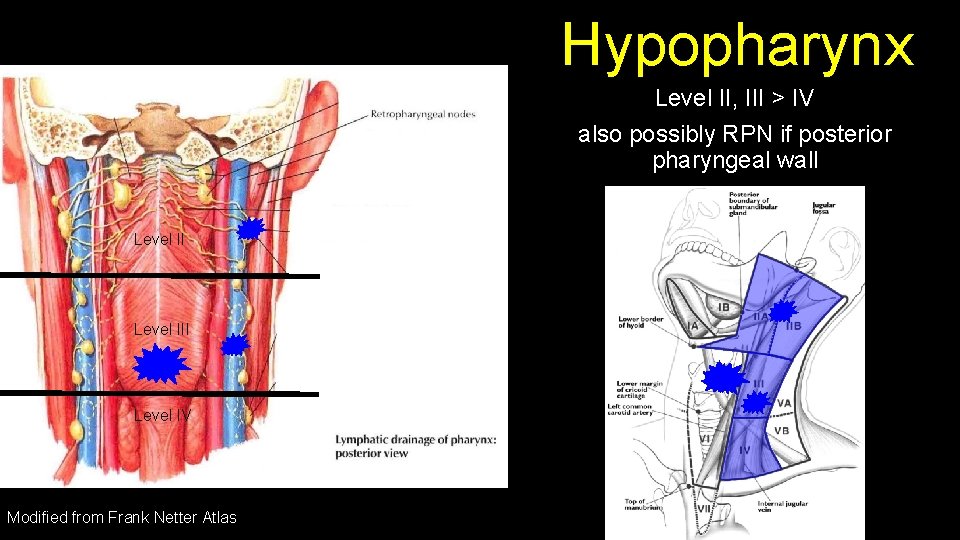
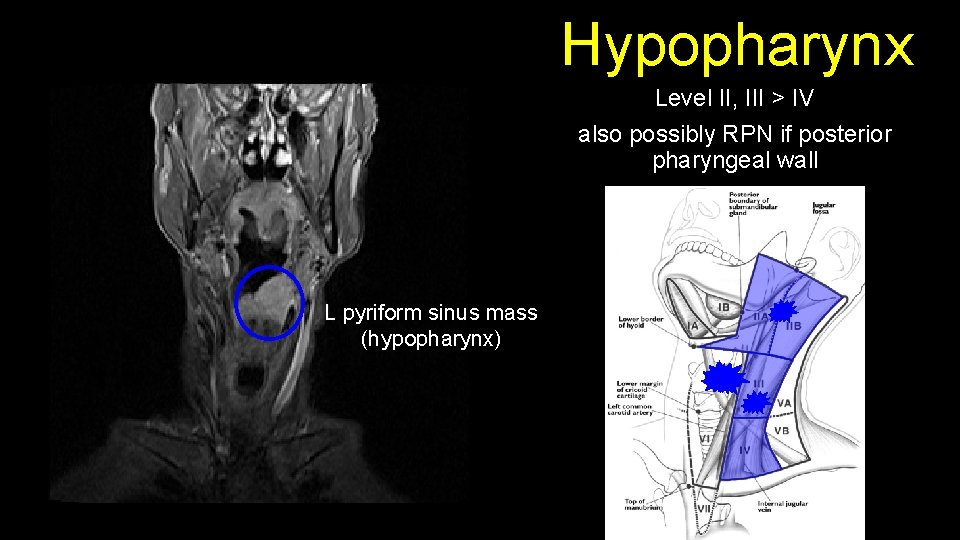
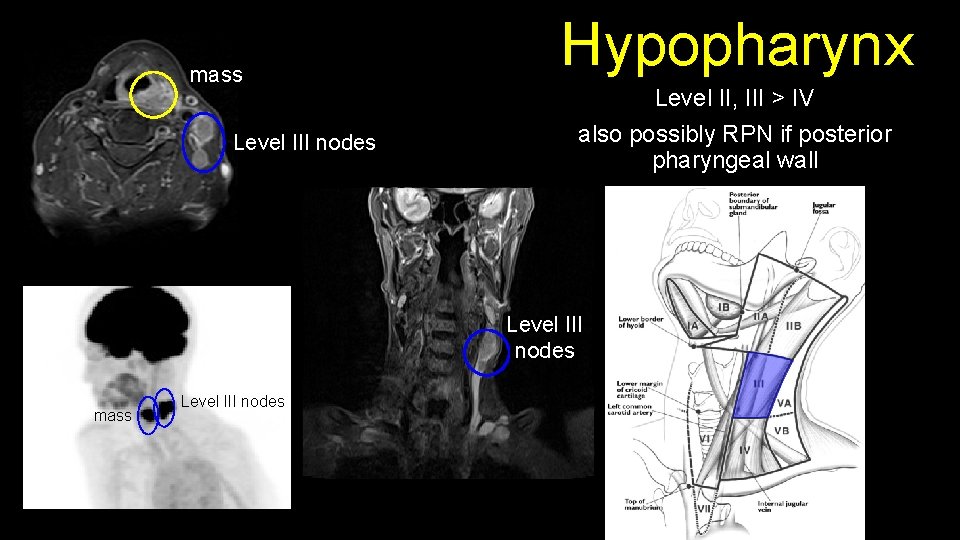
Hypopharynx Level II, III > IV also possibly RPN if posterior pharyngeal wall Level III Level IV Modified from Frank Netter Atlas
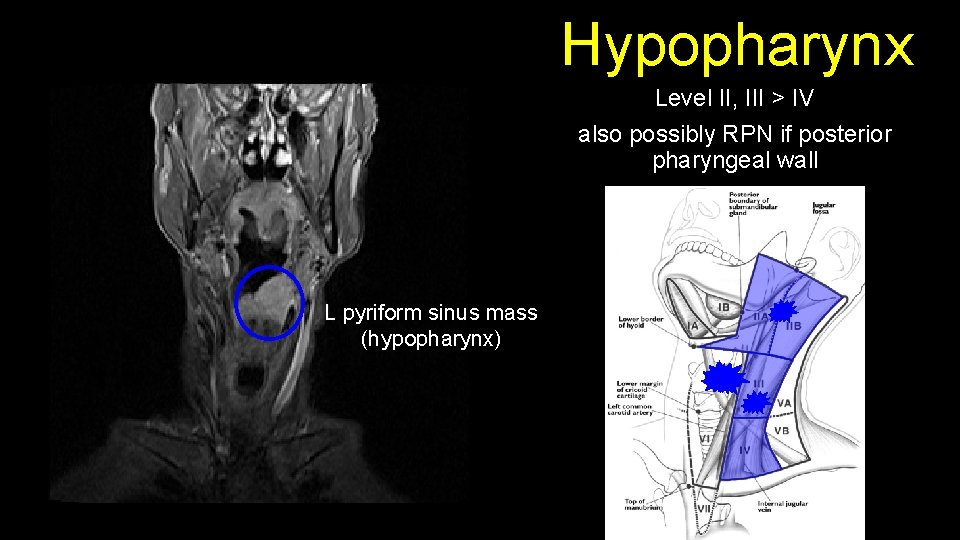
Hypopharynx Level II, III > IV also possibly RPN if posterior pharyngeal wall L pyriform sinus mass (hypopharynx)
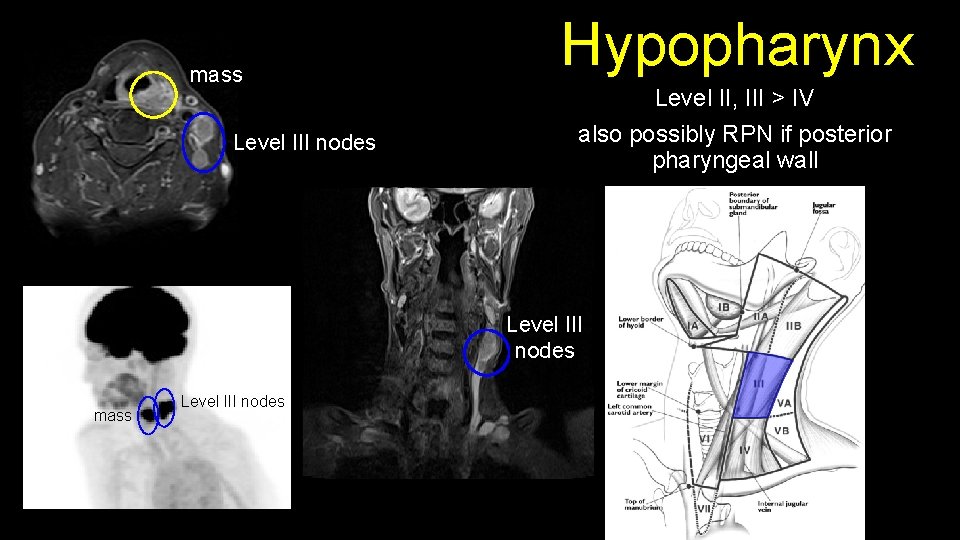
mass Level III nodes Hypopharynx Level II, III > IV also possibly RPN if posterior pharyngeal wall Level III nodes mass Level III nodes
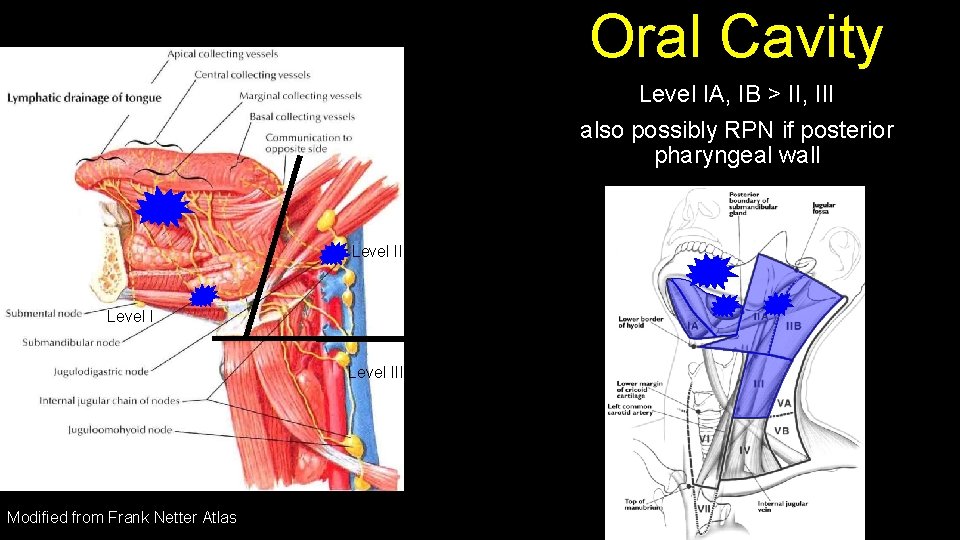
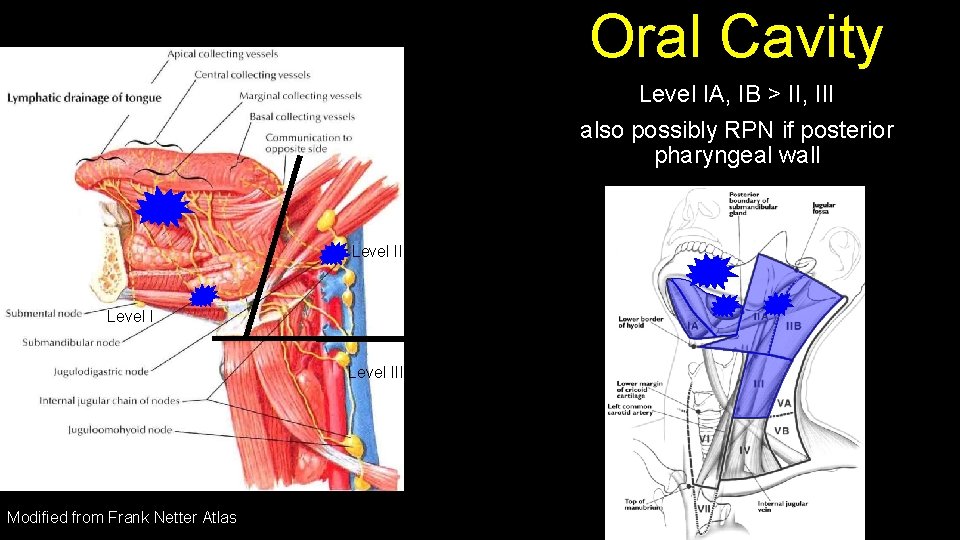
Oral Cavity Level IA, IB > II, III also possibly RPN if posterior pharyngeal wall Level III Modified from Frank Netter Atlas
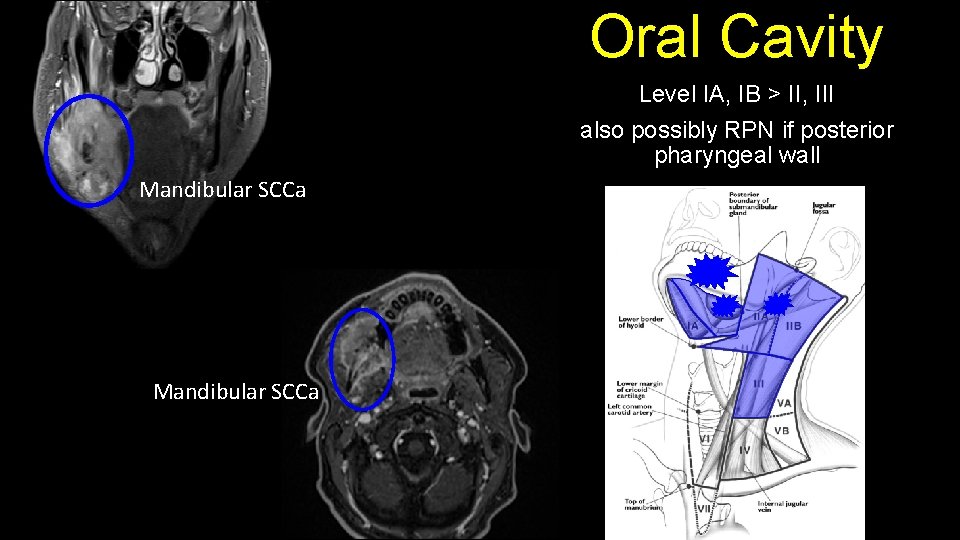
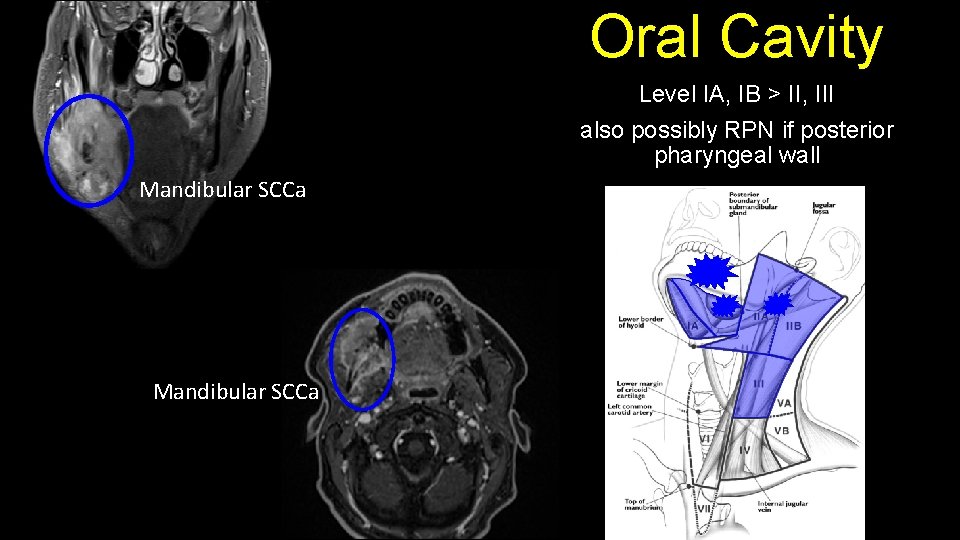
Oral Cavity Level IA, IB > II, III also possibly RPN if posterior pharyngeal wall Mandibular SCCa
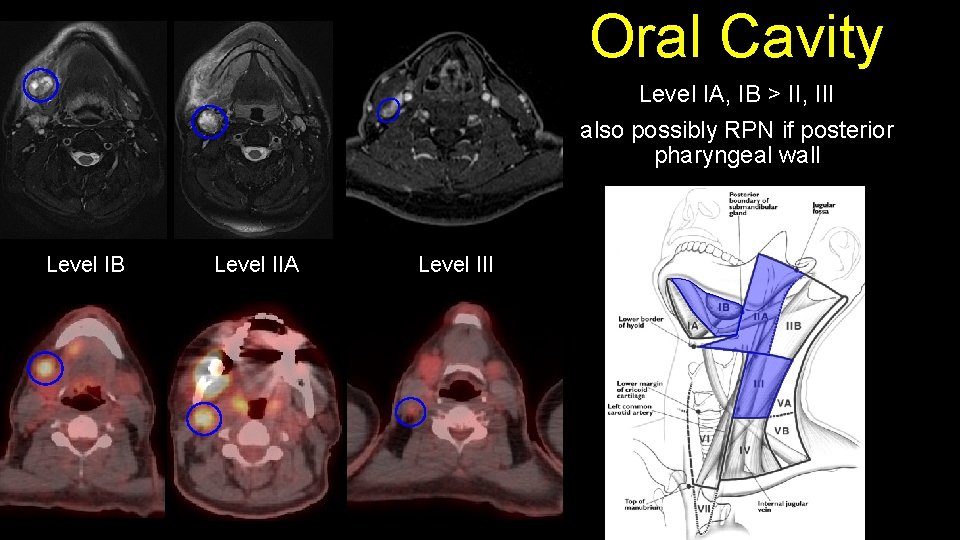
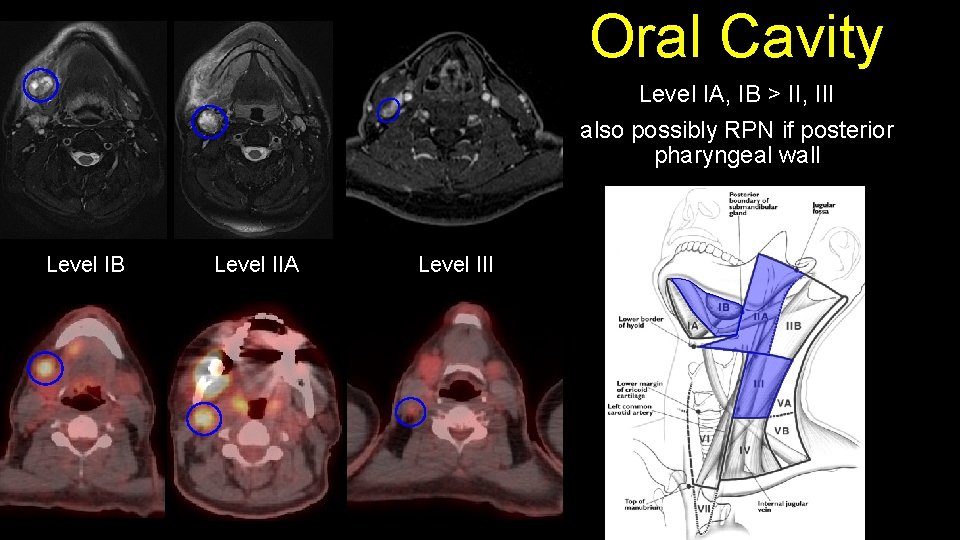
Oral Cavity Level IA, IB > II, III also possibly RPN if posterior pharyngeal wall Level IB Level IIA Level III
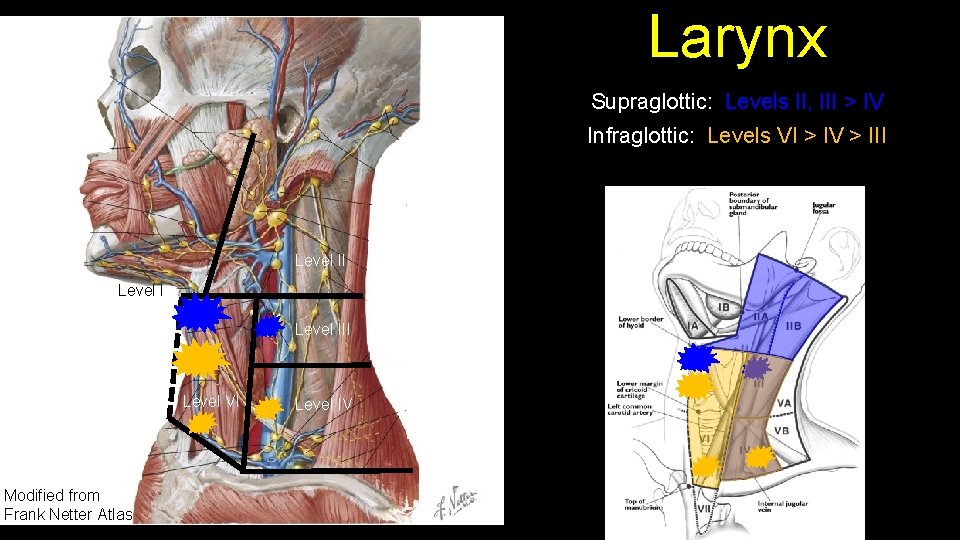
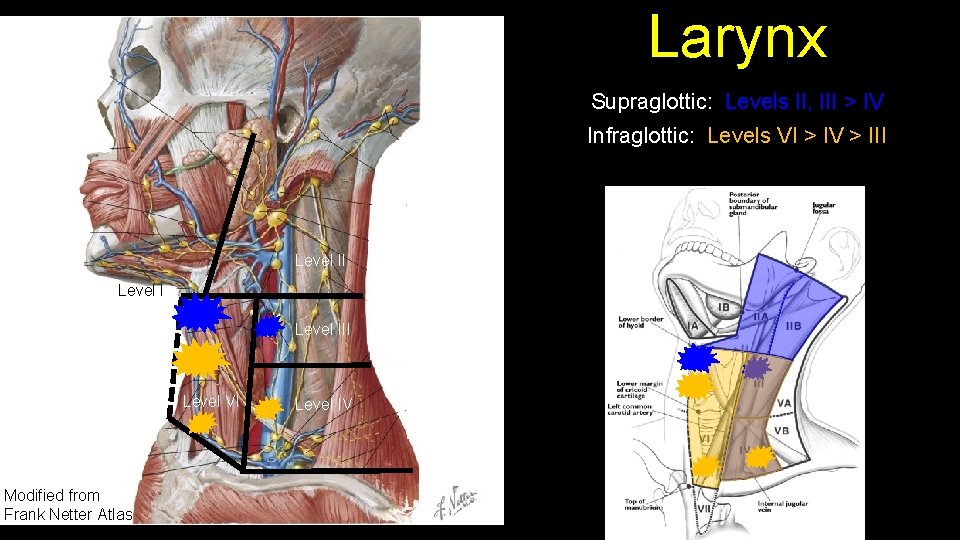
Larynx Supraglottic: Levels II, III > IV Infraglottic: Levels VI > IV > III Level III Level VI Modified from Frank Netter Atlas Level IV
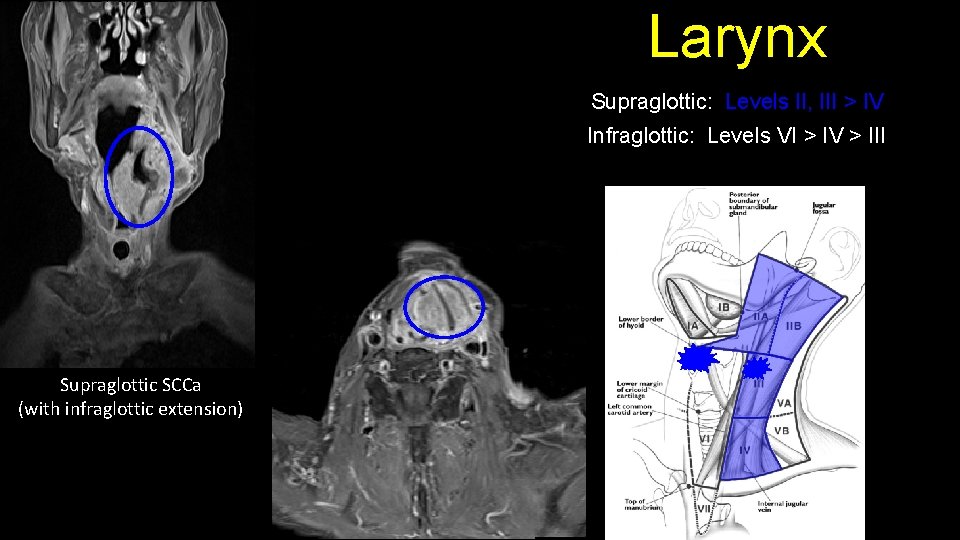
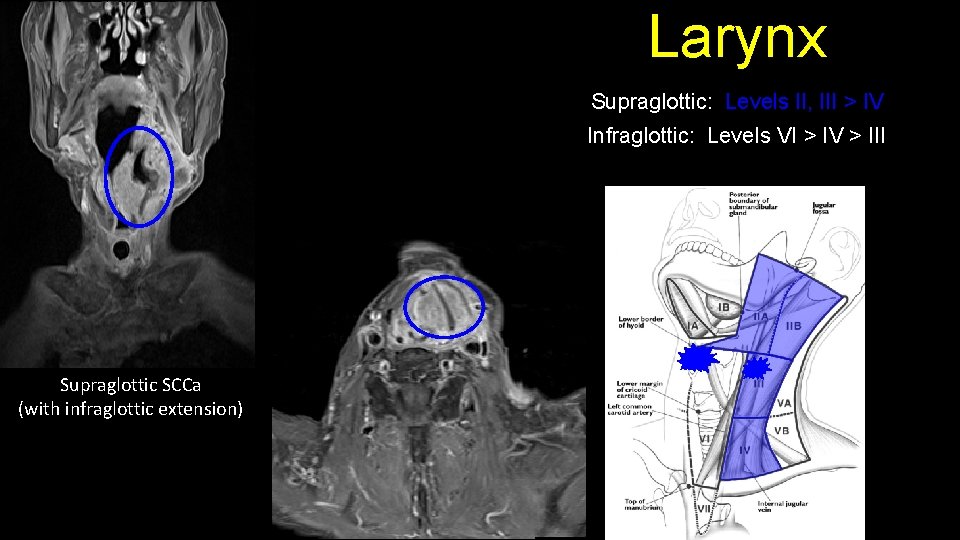
Larynx Supraglottic: Levels II, III > IV Infraglottic: Levels VI > IV > III Supraglottic SCCa (with infraglottic extension)
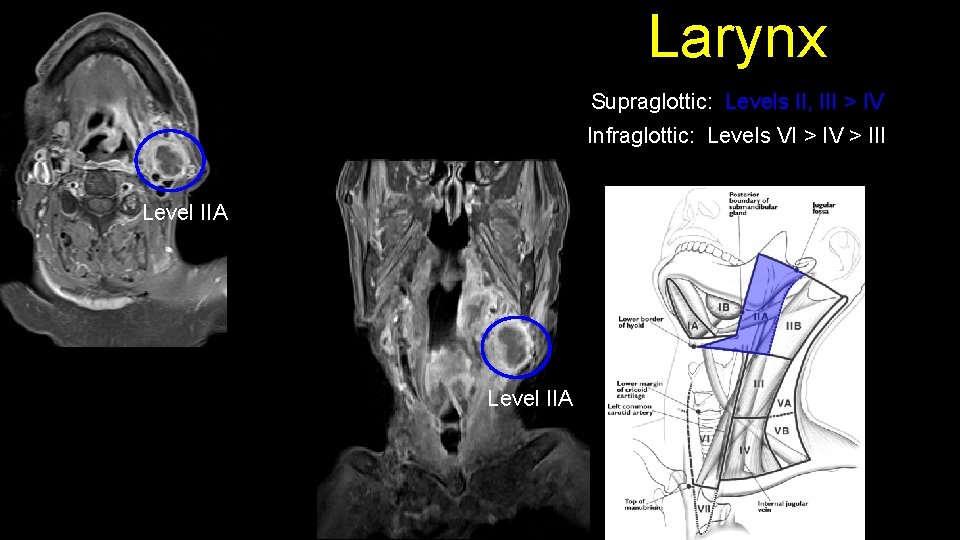
Larynx Supraglottic: Levels II, III > IV Infraglottic: Levels VI > IV > III Level IIA
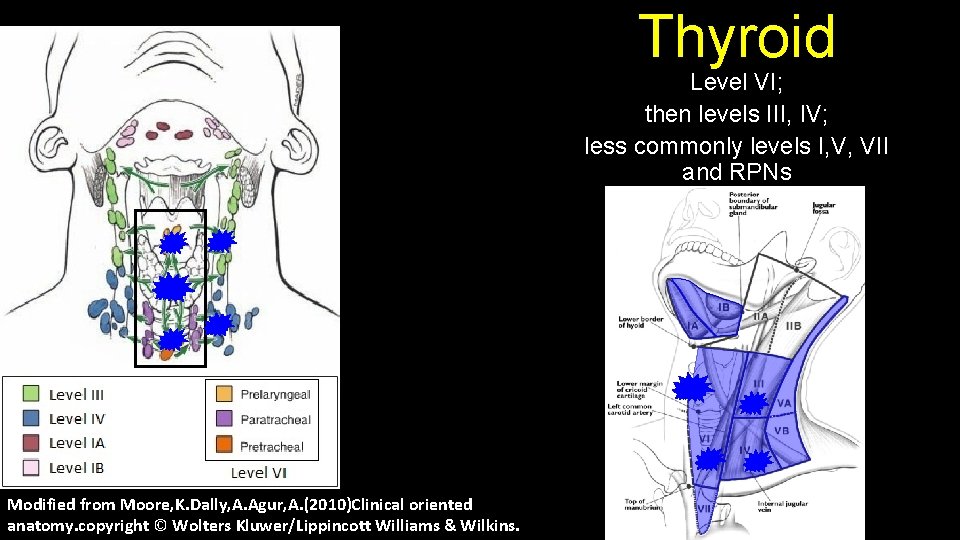
Thyroid Level VI; then levels III, IV; less commonly levels I, V, VII and RPNs Modified from Moore, K. Dally, A. Agur, A. (2010)Clinical oriented anatomy. copyright © Wolters Kluwer/Lippincott Williams & Wilkins.
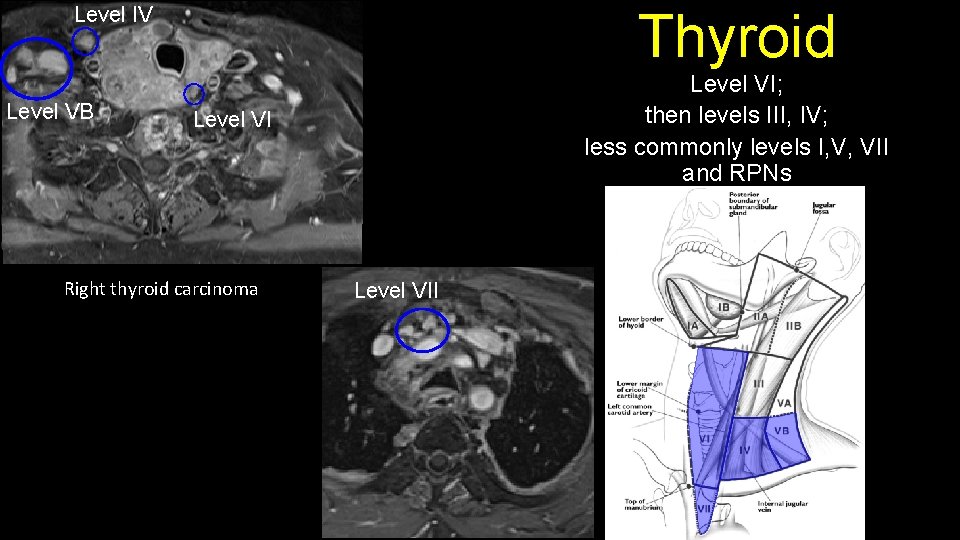
Level IV Level VB Thyroid Level VI; then levels III, IV; less commonly levels I, V, VII and RPNs Level VI Right thyroid carcinoma Level VII
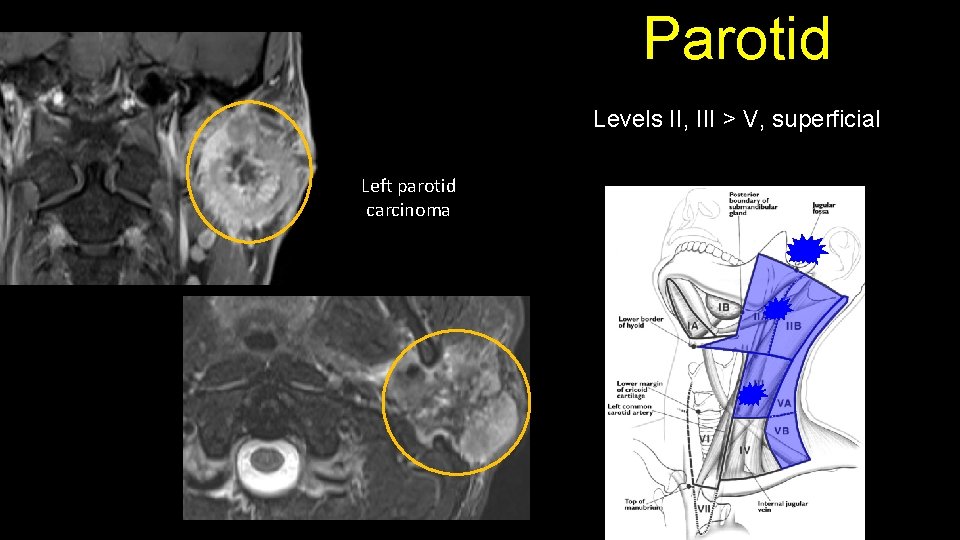
Parotid Levels II, III > V, superficial Left parotid carcinoma
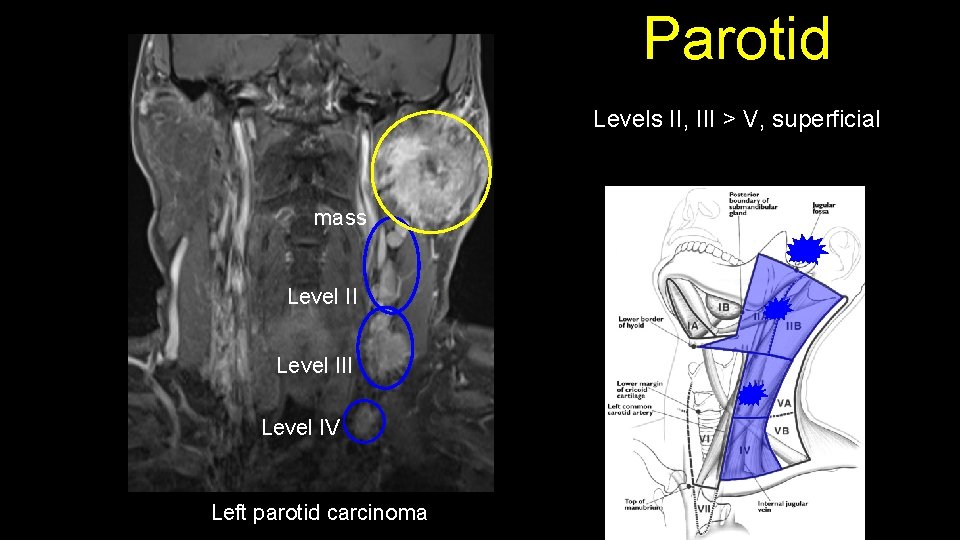
Parotid Levels II, III > V, superficial mass Level III Level IV Left parotid carcinoma
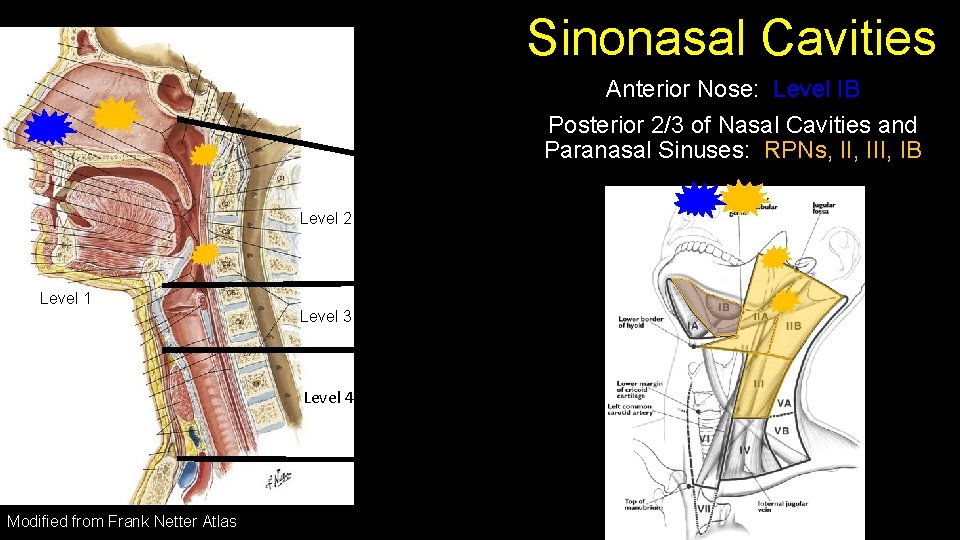
Sinonasal Cavities Anterior Nose: Level IB Posterior 2/3 of Nasal Cavities and Paranasal Sinuses: RPNs, III, IB Level 2 Level 1 Level 3 Level 4 Modified from Frank Netter Atlas
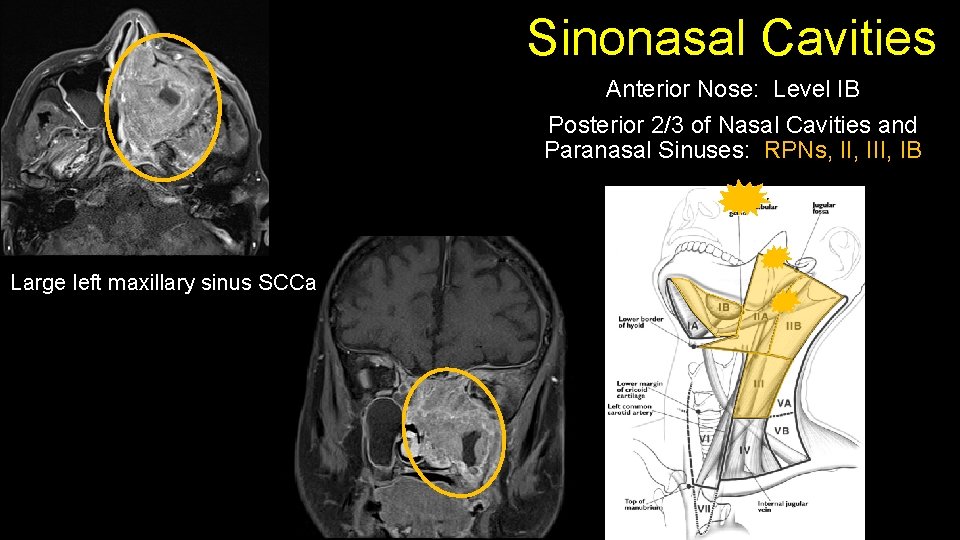
Sinonasal Cavities Anterior Nose: Level IB Posterior 2/3 of Nasal Cavities and Paranasal Sinuses: RPNs, III, IB Large left maxillary sinus SCCa
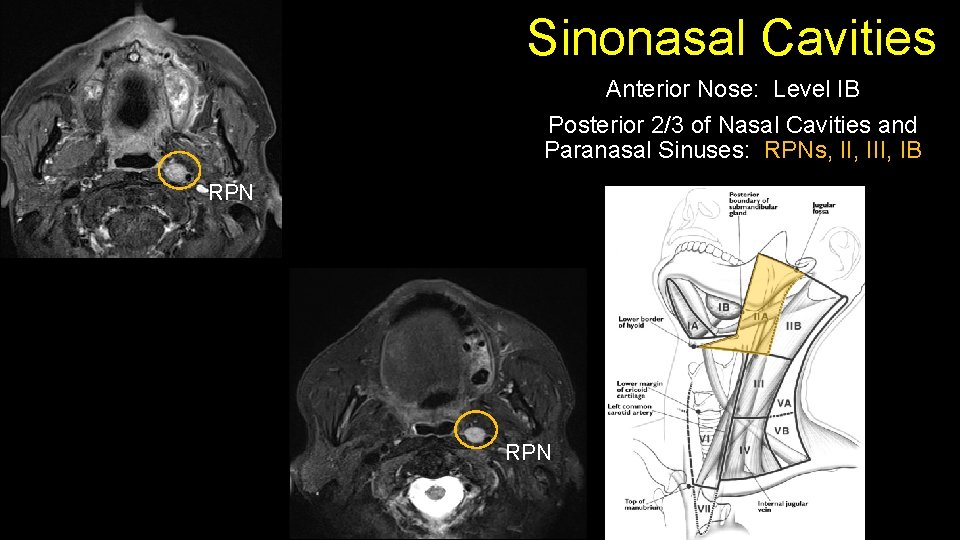
Sinonasal Cavities Anterior Nose: Level IB Posterior 2/3 of Nasal Cavities and Paranasal Sinuses: RPNs, III, IB RPN
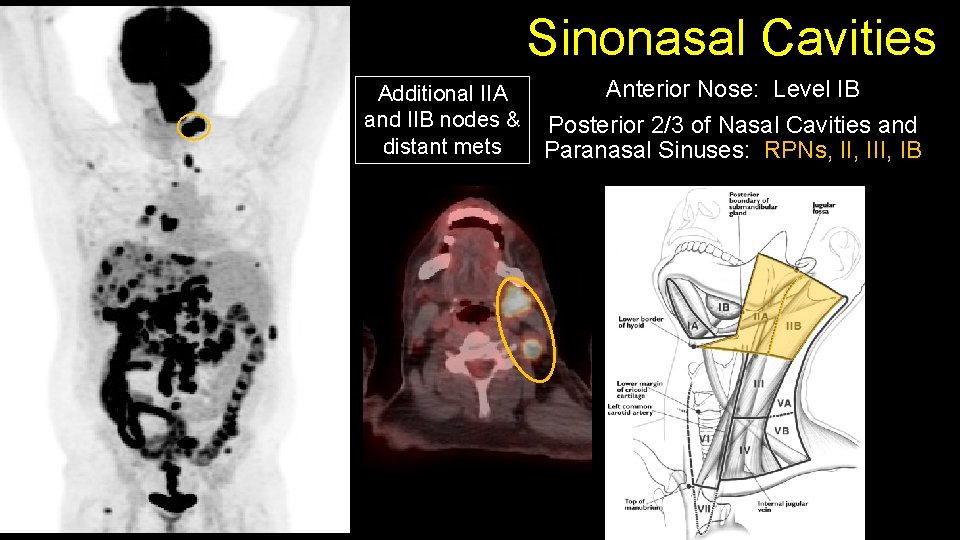
Sinonasal Cavities Additional IIA and IIB nodes & distant mets Anterior Nose: Level IB Posterior 2/3 of Nasal Cavities and Paranasal Sinuses: RPNs, III, IB
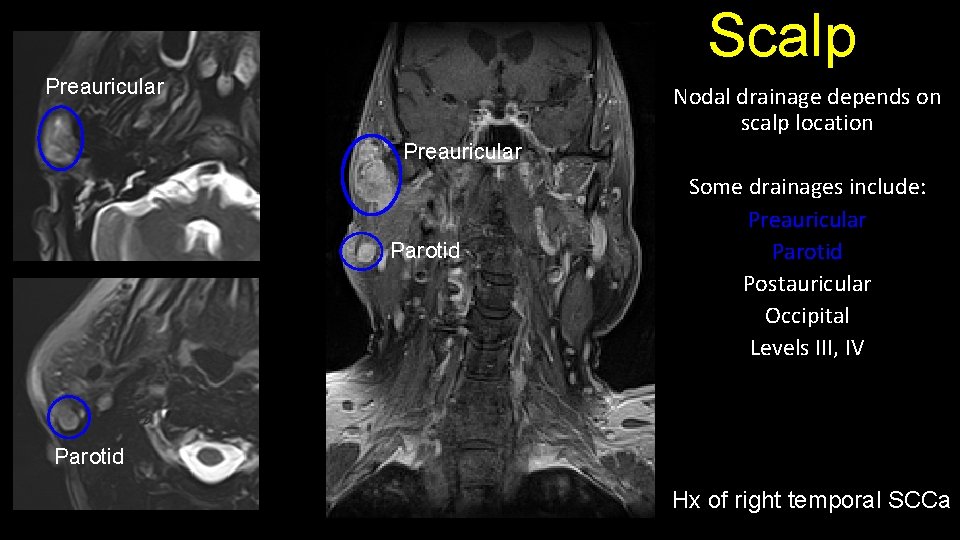
Scalp Preauricular Nodal drainage depends on scalp location Preauricular Parotid Some drainages include: Preauricular Parotid Postauricular Occipital Levels III, IV Parotid Hx of right temporal SCCa
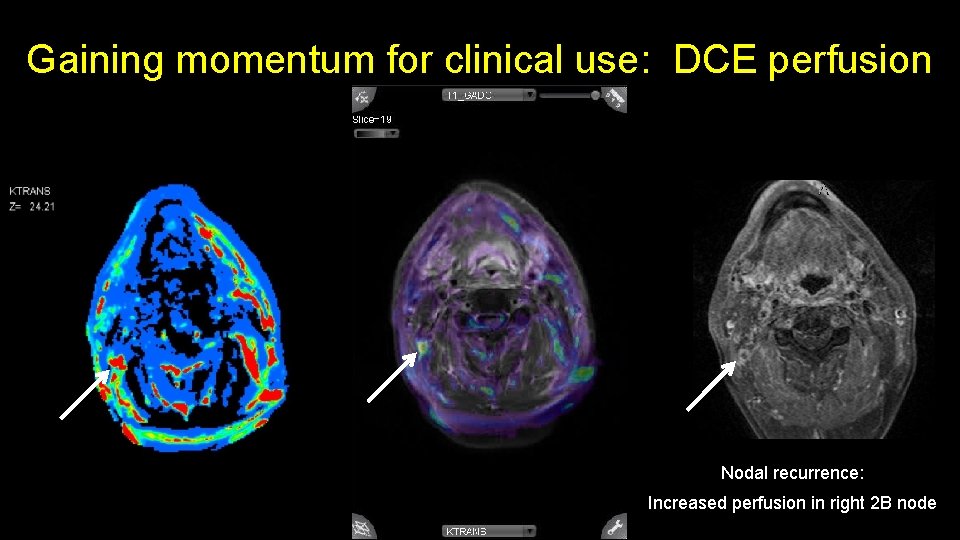
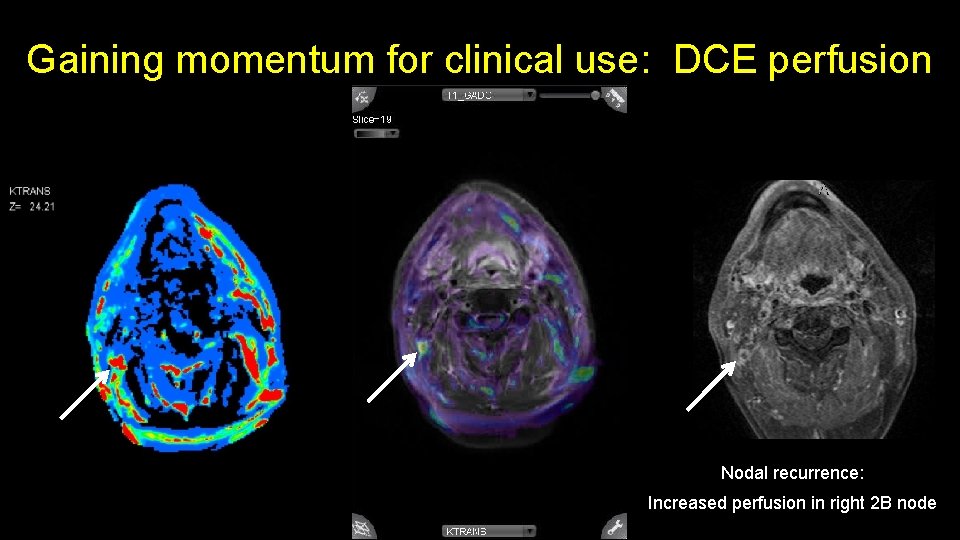
Gaining momentum for clinical use: DCE perfusion Nodal recurrence: Increased perfusion in right 2 B node
Conclusions After the reader has reviewed the presentation, they will be able to recognize the anatomical drainage patterns for cancers throughout the head and neck and be able to predict such patterns of spread utilizing both conventional and advanced MRI.
References 1. AJCCS. American joint committee on cancer staging manual. 7 ed. New York, NY: Springer, 2010. Corr. 7 th printing 2015 2. Mukherji SK, Armao D, Joshi VM. Cervical nodal metastases in squamous cell carcinoma of the head and neck: what to expect. Head Neck. 2001; 23(11): 995 -1005. 3. Head and Neck Imaging. Som PM and Curtin HD. Elsevier Health Sciences. 5 th edition. 2011. 4. Imaging-Based Nodal Classification for Evaluation of Neck Metastatic Adenopathy. Peter M. Som, Hugh D. Curtin, and Anthony A. Mancuso American Journal of Roentgenology 2000 174: 3, 837 -844