Neurology Dr Chris Derry Consultant Neurologist Department of



- Slides: 32
Neurology Dr Chris Derry Consultant Neurologist Department of Clinical Neurosciences WGH, Edinburgh
Outline • What is neurology? • What is a neurologist? • Elements of neurological diagnosis – History – Examination • Demonstration • Signs/ videos – Laboratory tests – Final diagnosis
What is Neurology? • The medical specialty concerned with the diagnosis, investigation and management of disorders of the nervous system. • Clinical neurosciences vs basic neurosciences • Nervous system – Central Nervous System (CNS) – Peripheral Nervous System (PNS) – Autonomic nervous system (ANS)
What does a neurologist do? • Diagnostics of nervous system disease – Traditional role • Management of acute neurological conditions – Status epilepticus, encephalitis, acute stroke etc • Management of chronic neurological diseases – Epilepsy, parkinsons disease, multiple sclerosis • Research
Other nervous system specialists… • Neurosurgeon – Surgical treatment of neurological disease. Open and stereotactic procedures • Neuroradiologist – Neuroimaging. Interventional neuroradiology • Neurophysiologist – EEG, NCV/EMG, evoked potentials • Neuropathologist – Biopsy analysis, autopsy • Psychiatrist – Mental illness
Why are patients referred to a Neurologist? • GP – Neurological symptoms worrying patient/ doctor – headache/ numbness/ weakness • Other specialists – Neurological complications of other diseases – Confusing clinical pictures – Many tests not definitive – Some invasive/expensive
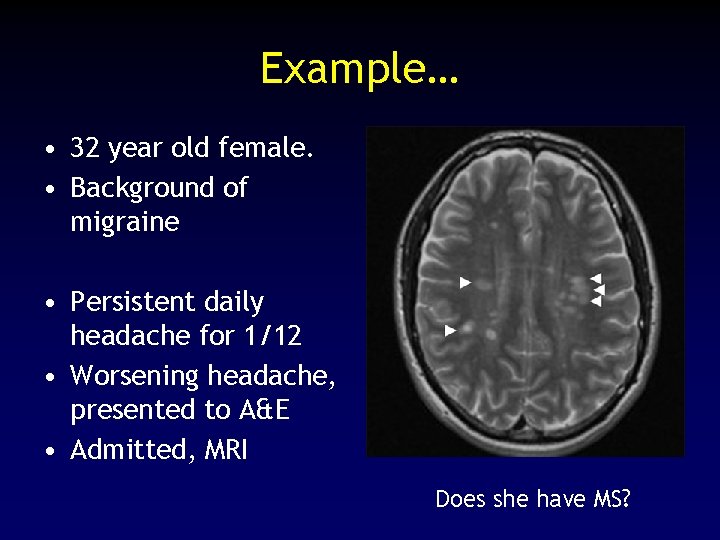
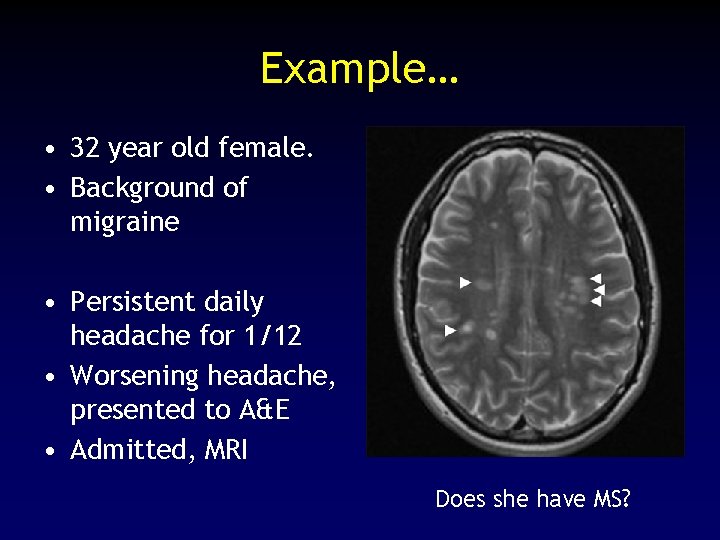
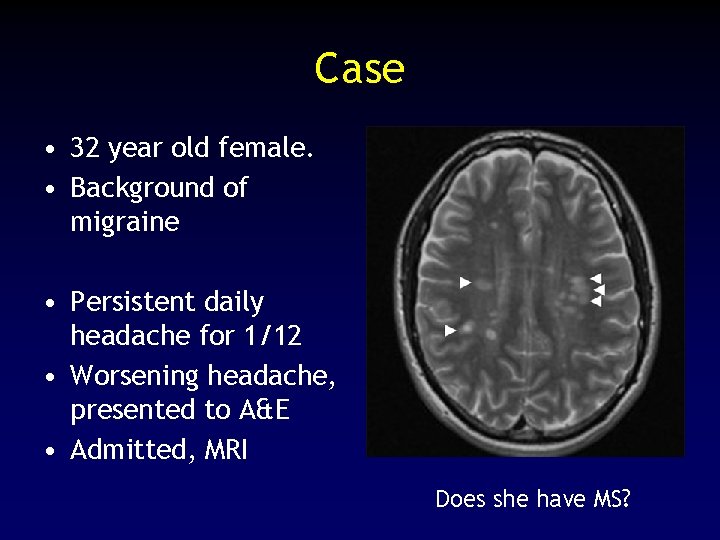
Example… • 32 year old female. • Background of migraine • Persistent daily headache for 1/12 • Worsening headache, presented to A&E • Admitted, MRI Does she have MS?
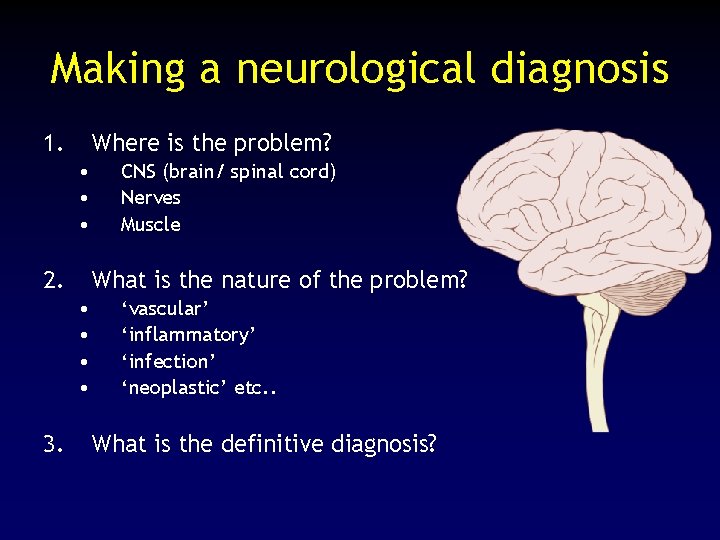
Making a neurological diagnosis 1. Where is the problem? • • • 2. What is the nature of the problem? • • 3. CNS (brain/ spinal cord) Nerves Muscle ‘vascular’ ‘inflammatory’ ‘infection’ ‘neoplastic’ etc. . What is the definitive diagnosis?
How are those stages reached? 1. History • • 80% of diagnostic information Particularly useful for localisation and mechanism 2. Examination • Can confirm localisation 3. Investigations • Can help with pathological/ definitive diagnosis
The neurological history • Presenting complaint – Headache, blackouts, dizziness, weakness, sensory symptoms, memory difficulties etc etc – Evolution of symptoms – Acute, subacute, chronic – Episodic, persistent – Systematic review – Additional neurological symptoms. ? Focal, multifocal or systemic disorder
The neurological history • Previous medical history – Earlier neurological symptoms, including symptoms seemingly unconnected • Family history – Many neurological disorders have a genetic basis • Social history – Consequences for job, family, driving, hobbies, sport, recreation – Smoking, alcohol – Drug history

Neurological examination • After the history, you usually have a fair idea of: – Where the lesion is – Type of lesion – And you may also know the final diagnosis… • Examination serves several purposes – Confirm localisation/ hypothesis testing • e. g Spinal cord vs peripheral nerve – – Screening for unsuspected abnormalities Closely observe patient behaviours Reassure patient Think!
Neurological examination • Cognition (Addenbrooke’s Cognitive Examination) • Cranial nerves • Limbs – – – Inspection (wasting etc) Tone Power Co-ordination Reflexes Sensation • Romberg’s/ Unterberger’s/ Hallpike’s • Gait
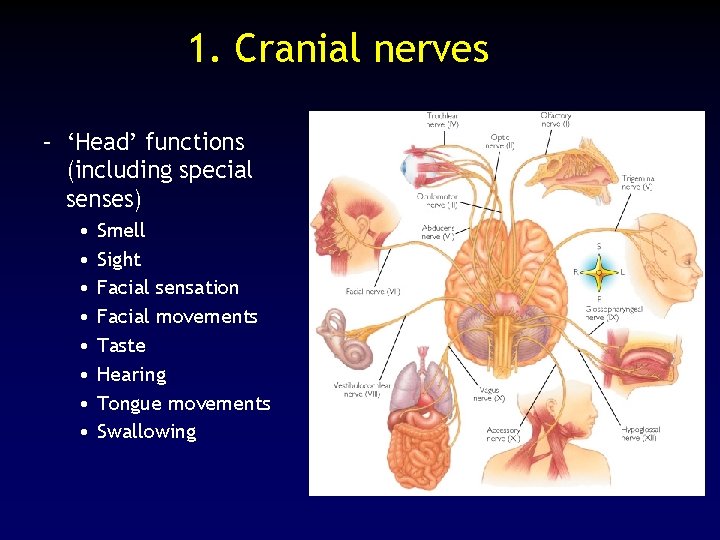
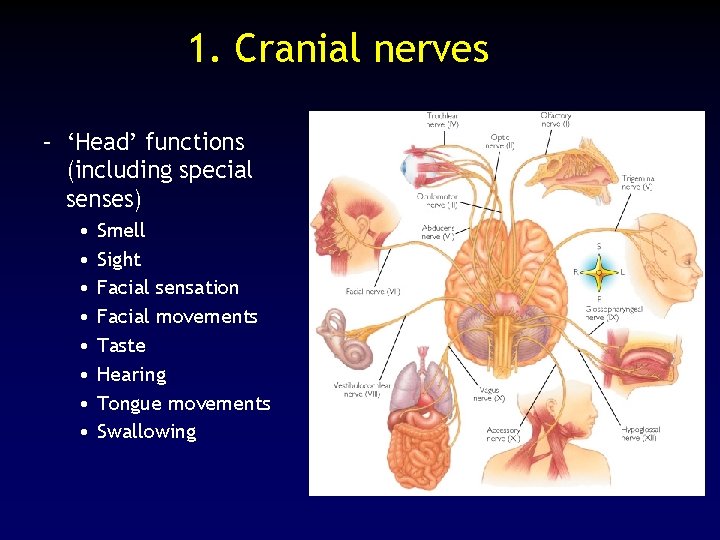
1. Cranial nerves – ‘Head’ functions (including special senses) • • Smell Sight Facial sensation Facial movements Taste Hearing Tongue movements Swallowing
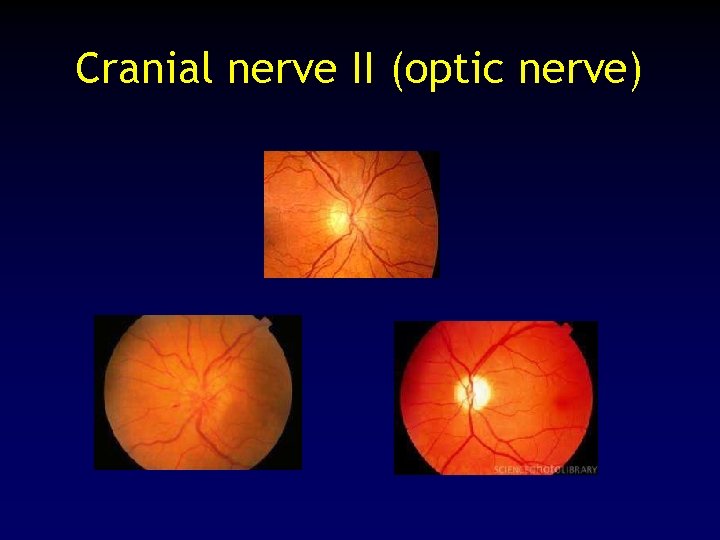
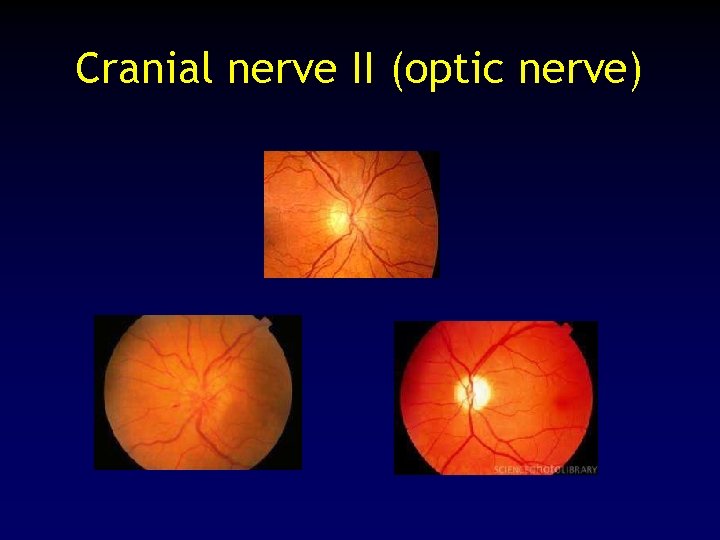
Cranial nerve II (optic nerve)
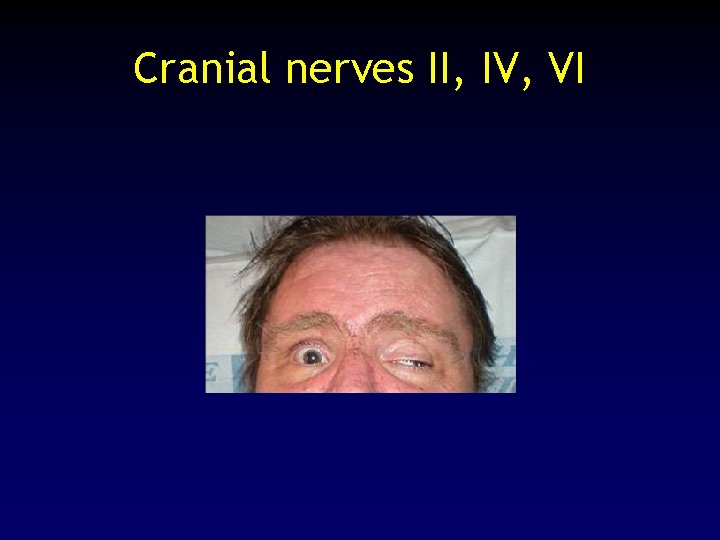
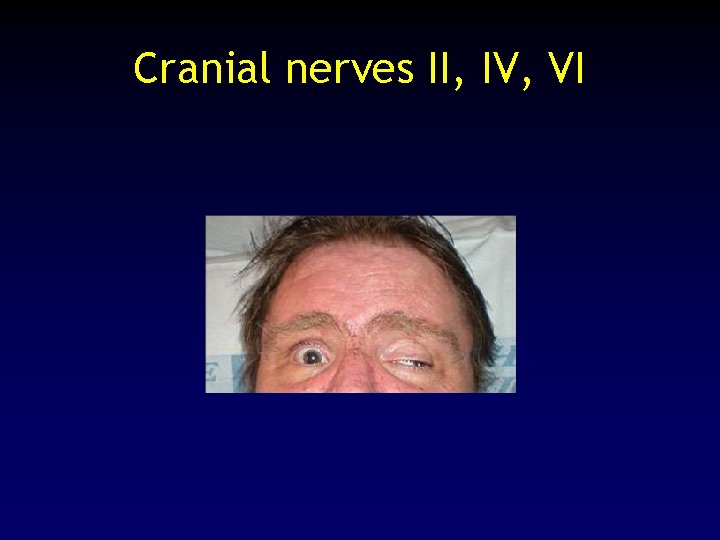
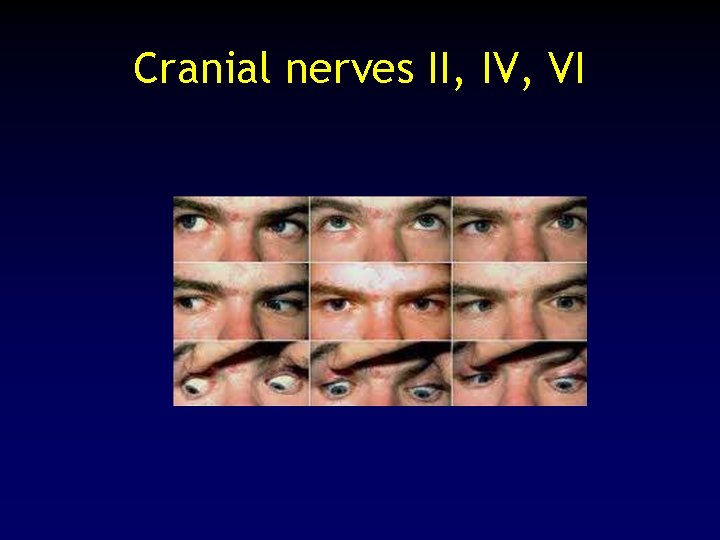
Cranial nerves II, IV, VI
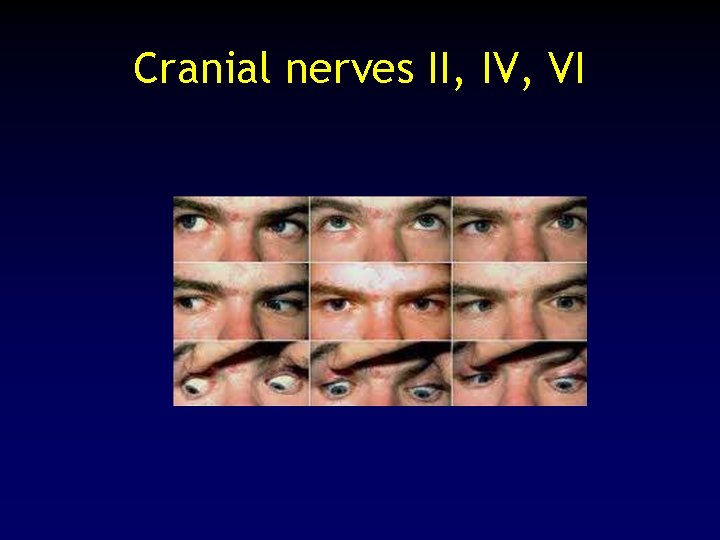
Cranial nerves II, IV, VI
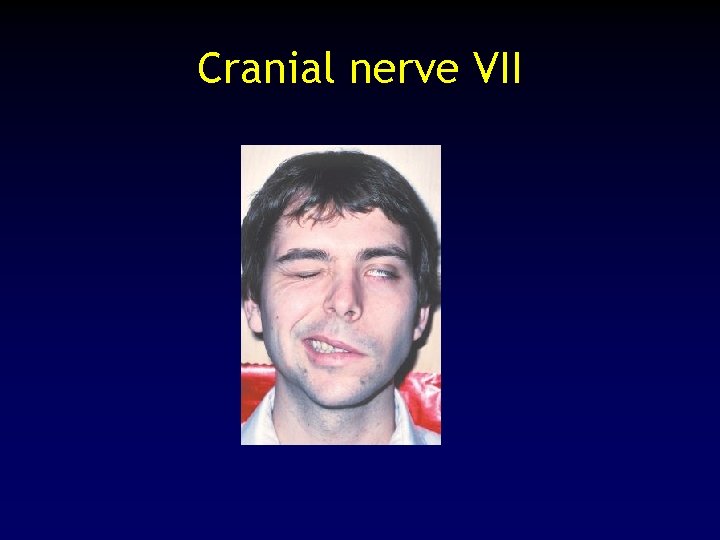
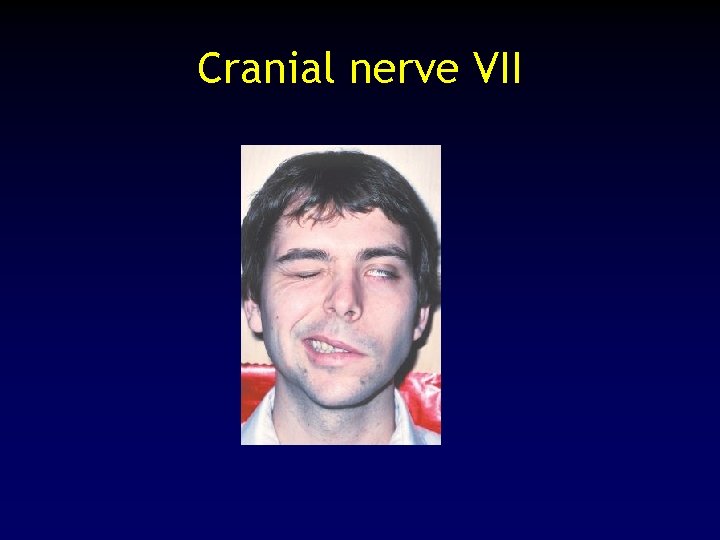
Cranial nerve VII
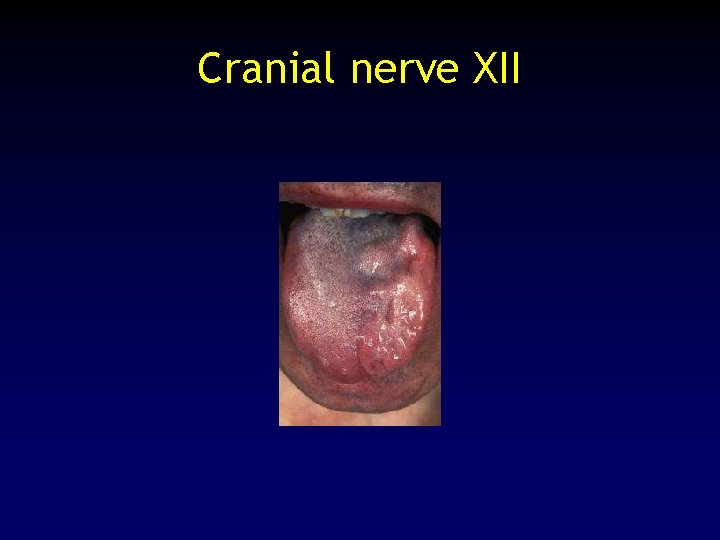
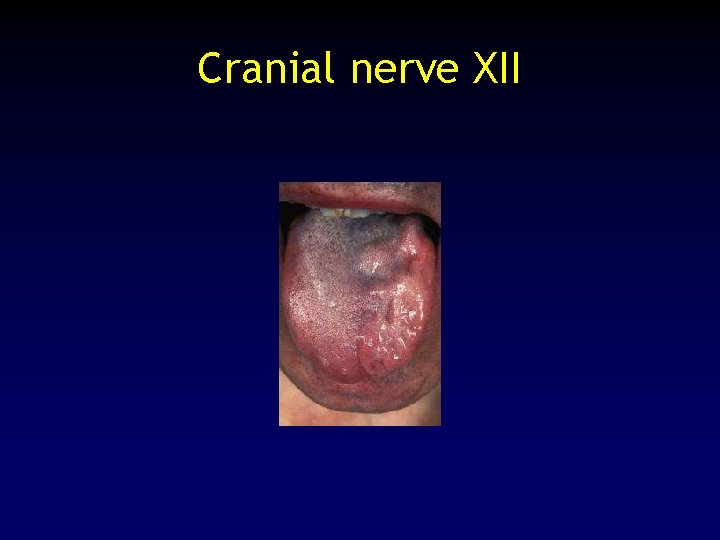
Cranial nerve XII
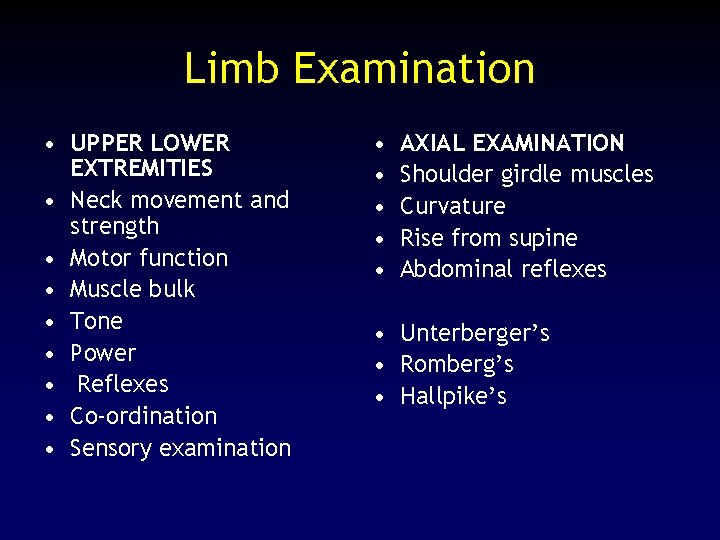
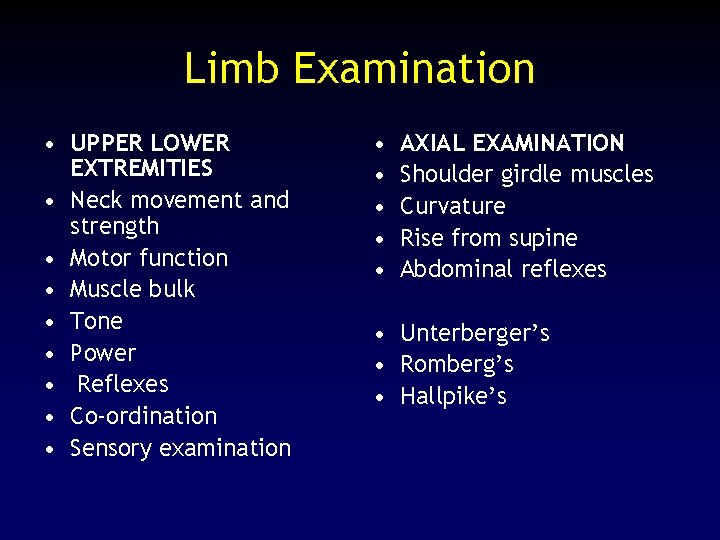
Limb Examination • UPPER LOWER EXTREMITIES • Neck movement and strength • Motor function • Muscle bulk • Tone • Power • Reflexes • Co-ordination • Sensory examination • • • AXIAL EXAMINATION Shoulder girdle muscles Curvature Rise from supine Abdominal reflexes • Unterberger’s • Romberg’s • Hallpike’s

Some “Spot” diagnoses • Parkinson’s Disease • Huntingdon’s Chorea
Investigations
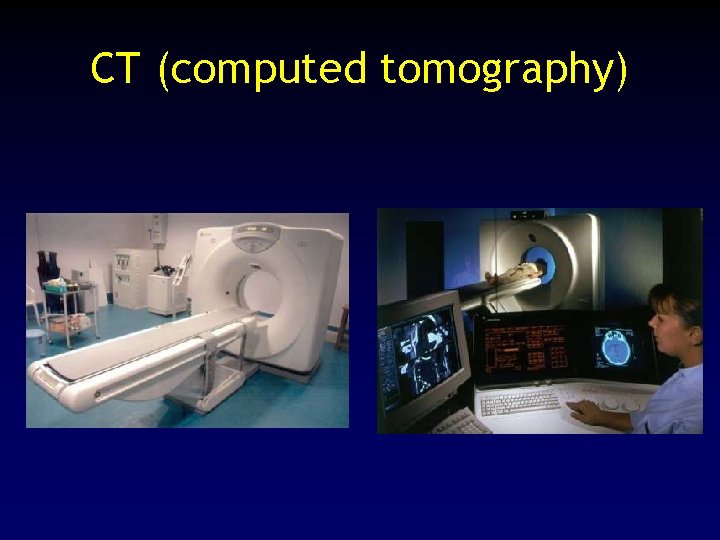
CT (computed tomography)
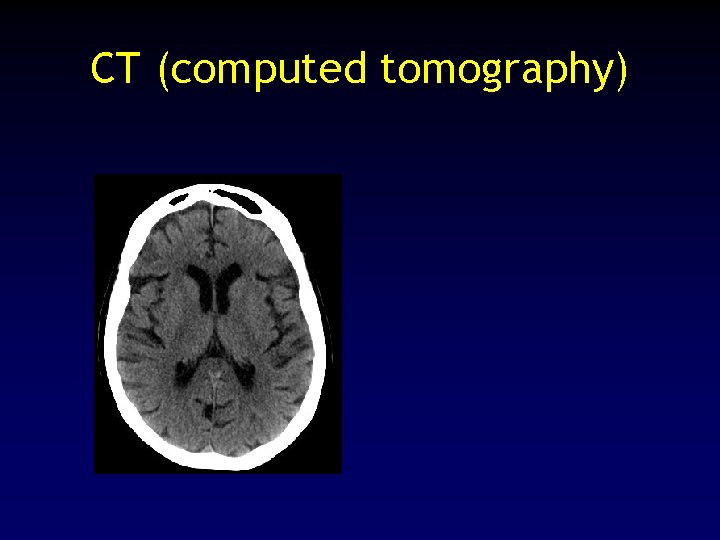
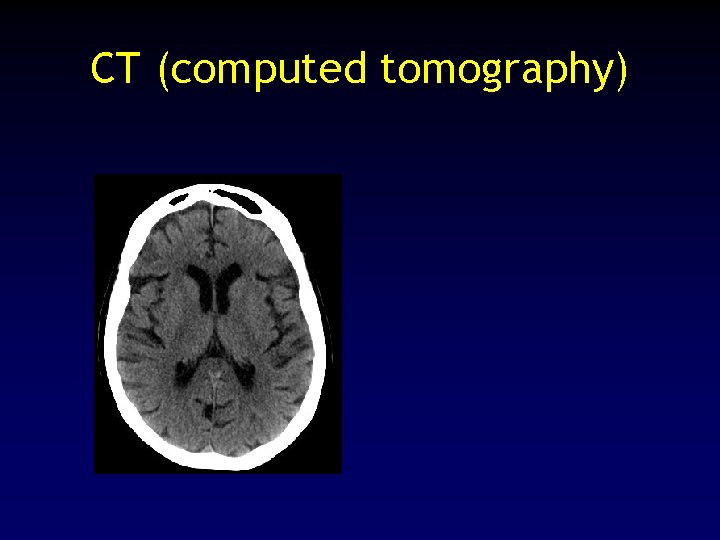
CT (computed tomography)
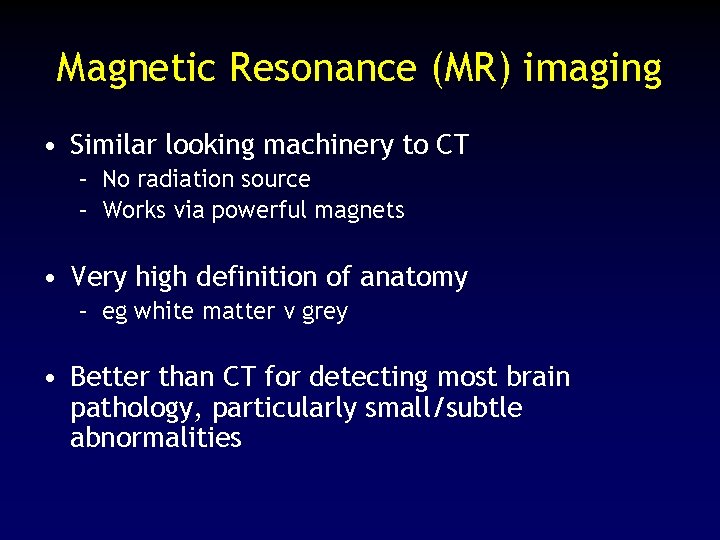
Magnetic Resonance (MR) imaging • Similar looking machinery to CT – No radiation source – Works via powerful magnets • Very high definition of anatomy – eg white matter v grey • Better than CT for detecting most brain pathology, particularly small/subtle abnormalities
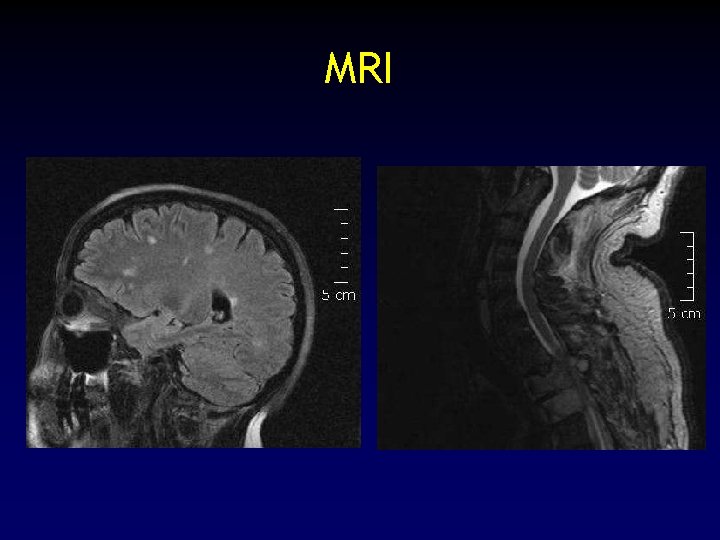
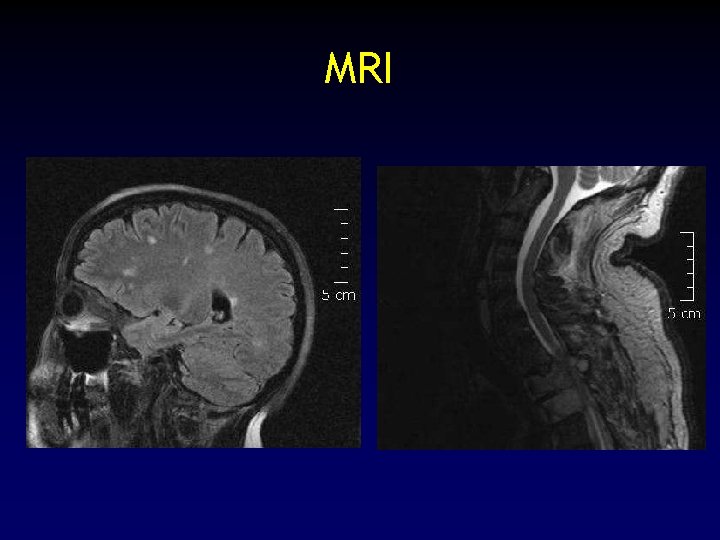
MRI
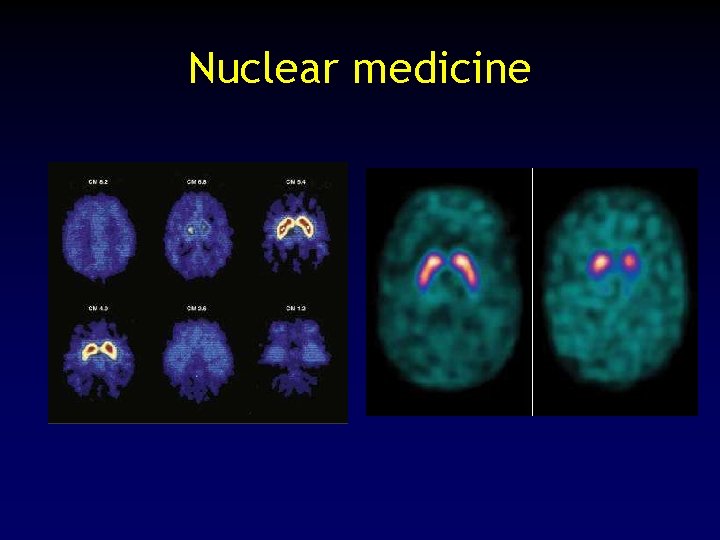
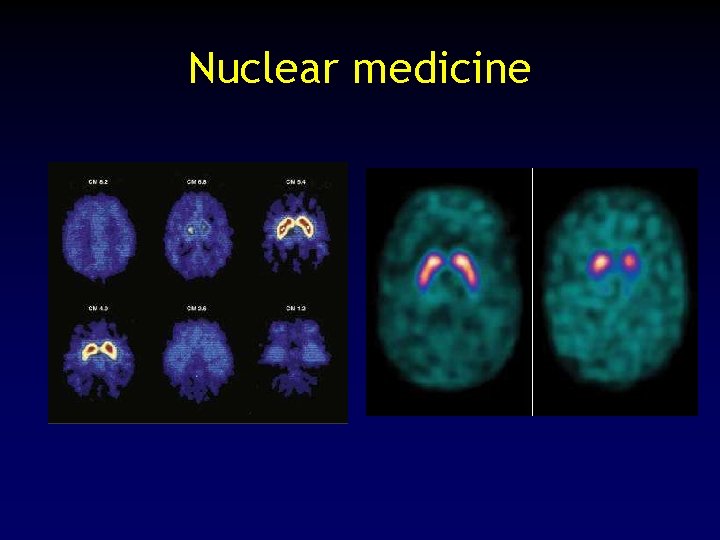
Nuclear medicine
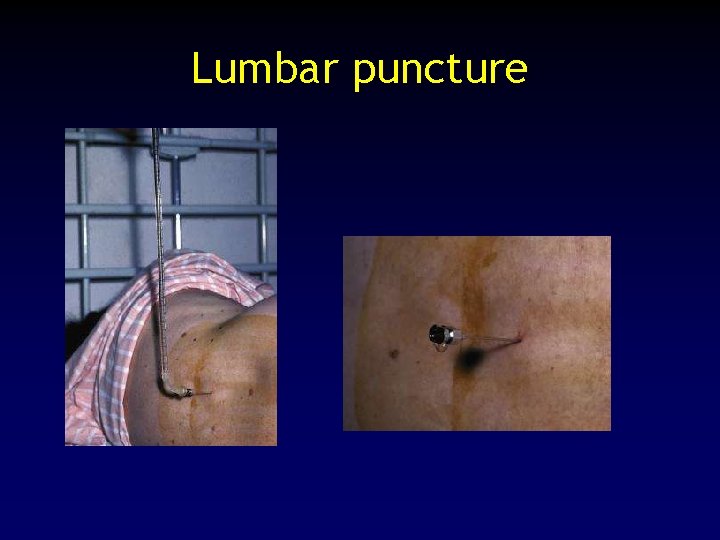
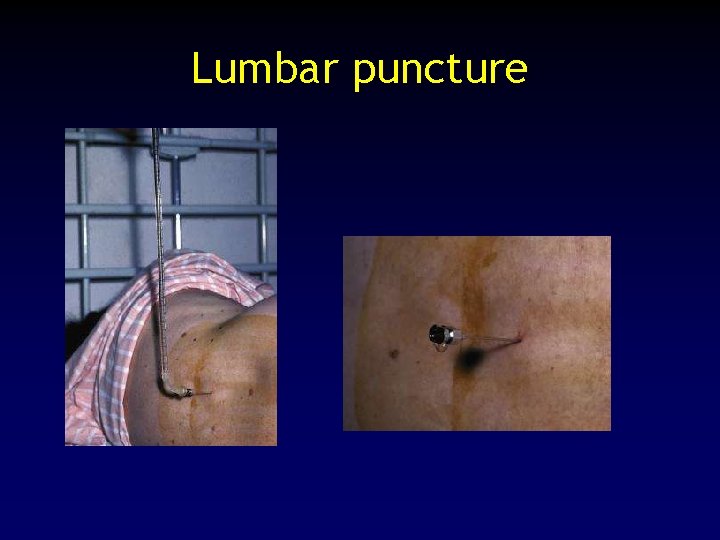
Lumbar puncture
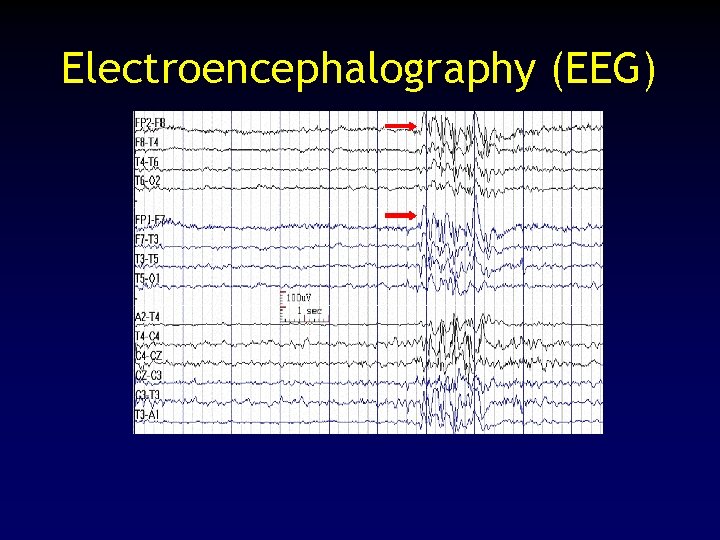
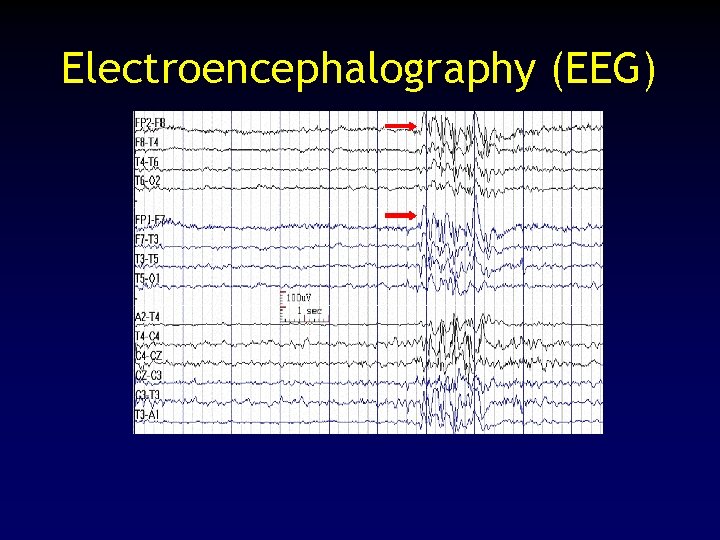
Electroencephalography (EEG)
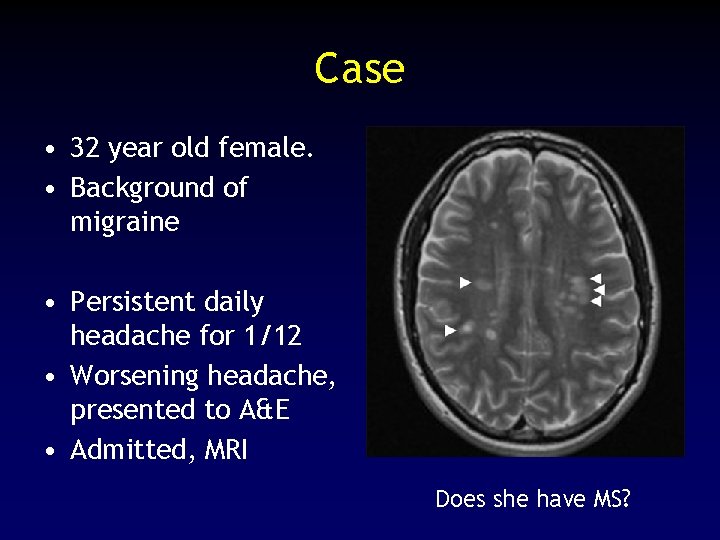
Case • 32 year old female. • Background of migraine • Persistent daily headache for 1/12 • Worsening headache, presented to A&E • Admitted, MRI Does she have MS?
Assessment • Full history – Remote neurological episodes (even minor) – Family history • Examination findings suggestive of previous neurological events • Consider investigations – repeating MRI – lumbar puncture • Uncertainty may persist…

 Belmont house school derry
Belmont house school derry Hsc pensions
Hsc pensions Department of neurology
Department of neurology Dr pearson neurologist
Dr pearson neurologist Richard perry neurologist
Richard perry neurologist Dr richard perry neurologist
Dr richard perry neurologist Gastrointernist
Gastrointernist Raeburn forbes
Raeburn forbes Kelly clarkson neurologist
Kelly clarkson neurologist Dr fok neurologist
Dr fok neurologist Dr nin bajaj
Dr nin bajaj Dr michelle lee jones neurologist
Dr michelle lee jones neurologist Dr aminian neurologist
Dr aminian neurologist Ernie butler neurologist
Ernie butler neurologist Deepak madhavan
Deepak madhavan Adrian pace neurologist
Adrian pace neurologist Alina webber
Alina webber Dr bennetto neurologist
Dr bennetto neurologist Dr paul cooper neurologist
Dr paul cooper neurologist Levenogestral
Levenogestral Merkel disc receptor
Merkel disc receptor Nlff neurology
Nlff neurology Alemutuzumab
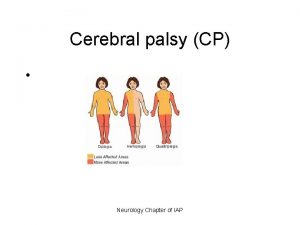
Alemutuzumab Cerebral palsy iap
Cerebral palsy iap Oregon neurology associates
Oregon neurology associates Internal medicine shelf percentile
Internal medicine shelf percentile Rachel ditrapani md
Rachel ditrapani md Walton centre for neurology
Walton centre for neurology Uf neurology residency
Uf neurology residency Umass memorial pharmacy
Umass memorial pharmacy Mary bridge neurology
Mary bridge neurology Neurology near loomis
Neurology near loomis Nlff neurology
Nlff neurology