Headache Clare Galton Consultant Neurologist 14115 The patient
- Slides: 35
Headache Clare Galton Consultant Neurologist 14/1/15
“The patient with a headache often finds himself a medical orphan. He is fortunate indeed if his headache is transient, for otherwise he may find himself on an excursion to the ophthalmologist, otolaryngologist, neurologist, dentist, psychiatrist, chiropractor, and the latest health spa. He is x rayed, fitted with glasses, analysed, massaged, relieved of his turbinates and teeth, and too often emerges with his headache intact” RC Packard 1979
Headaches • Primary care consultations – 6. 4 /100 women – 2. 5/100 men • Neurology OPD 30% • Life time prevalence of headache >90%
Headache • • Can I classify this headache? Do I need to investigate? What does the patient want? Is treatment appropriate? And if so what is the most sensible approach?
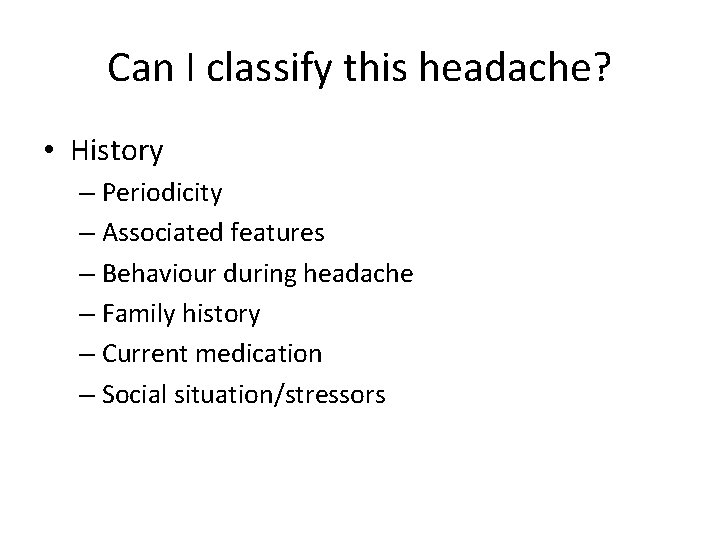
Can I classify this headache? • History – Periodicity – Associated features – Behaviour during headache – Family history – Current medication – Social situation/stressors
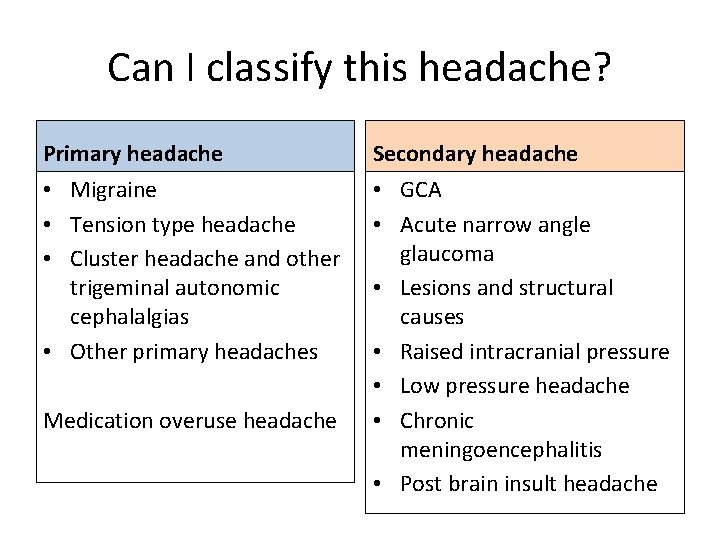
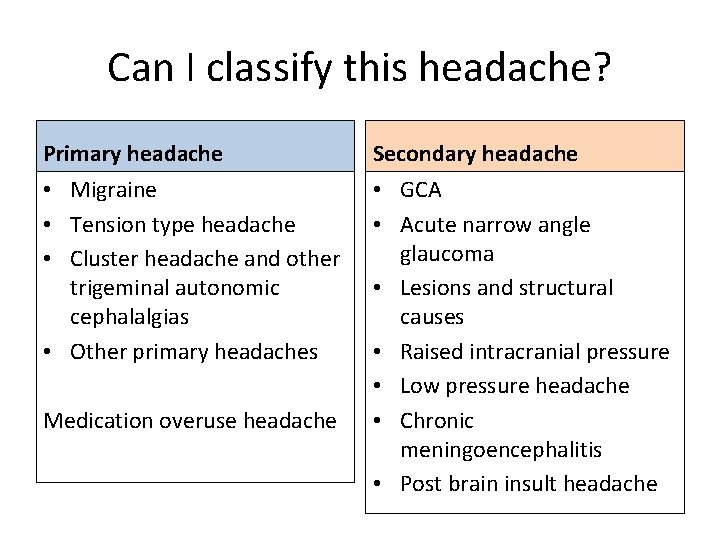
Can I classify this headache? Primary headache • Migraine • Tension type headache • Cluster headache and other trigeminal autonomic cephalalgias • Other primary headaches Medication overuse headache Secondary headache • GCA • Acute narrow angle glaucoma • Lesions and structural causes • Raised intracranial pressure • Low pressure headache • Chronic meningoencephalitis • Post brain insult headache
Primary headache syndromes • Migraine (with or without aura) • Tension type • Cluster and other trigeminal autonomic cephalalgias • Other primary headaches
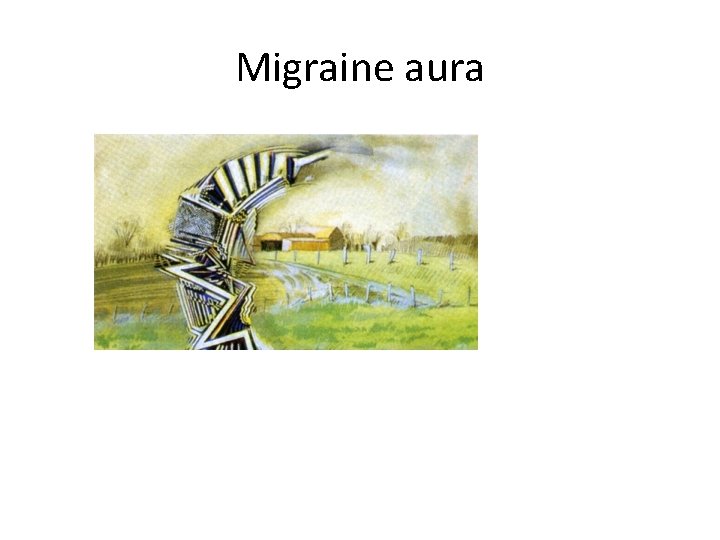
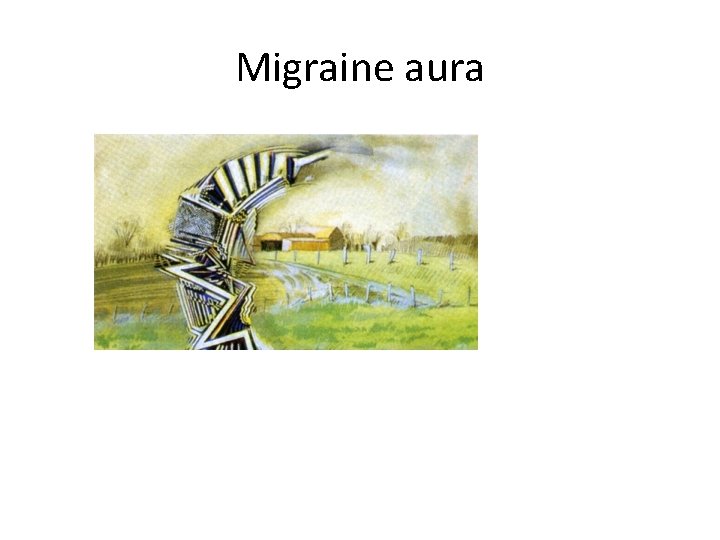
Migraine aura
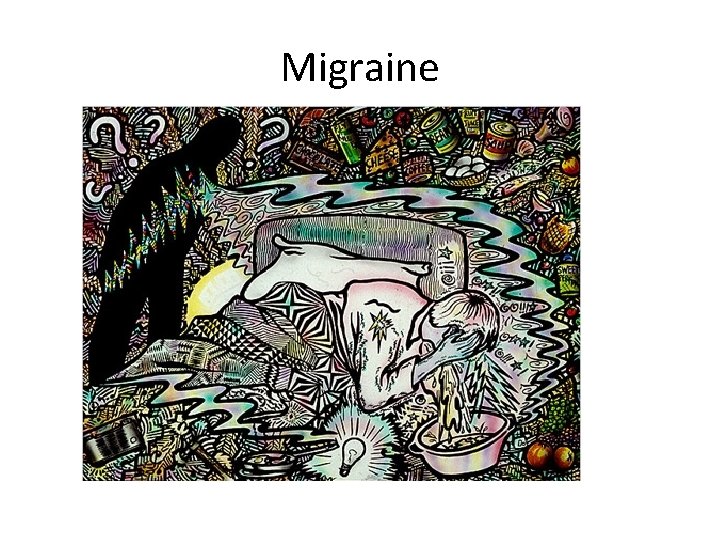
Migraine
Migraine characteristics • • Attacks of headache lasting 4 to 72 hours Nausea and/or vomiting Intolerance of light Intolerance of noise Recurrent attacks Visual or neurological aura lasting 6 – 60 mins Consistent trigger
Tension type headache
Tension type headache • • • Featureless headache Bilateral Tightening quality Mild to moderate severity Absence of features of migraine
Cluster headache
Cluster headache • • Severe unilateral pain Rapid onset Autonomic features on same side 15 mins to 3 hours duration 1 -8 attacks a day Restless during an attack Striking circadian rhythm
Other primary headache syndromes Hemicrania continua Primary stabbing headache Primary cough headache Primary exertional headache Primary headache associated with sexual activity • Primary thunderclap headache • Hypnic headache • • •
Secondary headache • Need to consider – Raised intracranial pressure – Low pressure headache – Chronic meningoencephalitis – Post brain insult headache – Giant cell arteritis – Glaucoma – Cerviogenic – Disorders of eyes/ears/nose/sinuses/teeth – Depression – Vascular disorders
Secondary headache • Need to consider – Raised intracranial pressure – Low pressure headache – Chronic meningoencephalitis – Post brain insult headache – Giant cell arteritis – Glaucoma – Cerviogenic – Disorders of eyes/ears/nose/sinuses/teeth – Depression – Vascular disorders
Headache concerning features • • New onset headache after age 50 Genuinely increasing frequency and severity Waking patient from sleep Unresponsive to treatment Always on same side Following head trauma Precipitated by exertion New headache in patients: – On anticoagulants – With HIV or cancer
General Examination • Blood pressure • Neck examination – Posture – Range of movement – Muscle tone – Muscle tenderness • Temporal pulses
Neurological Examination • Fundoscopy • Cranial nerves • Tone, power, reflexes and coordination in all four limbs • Plantars • Gait including heel toe walking
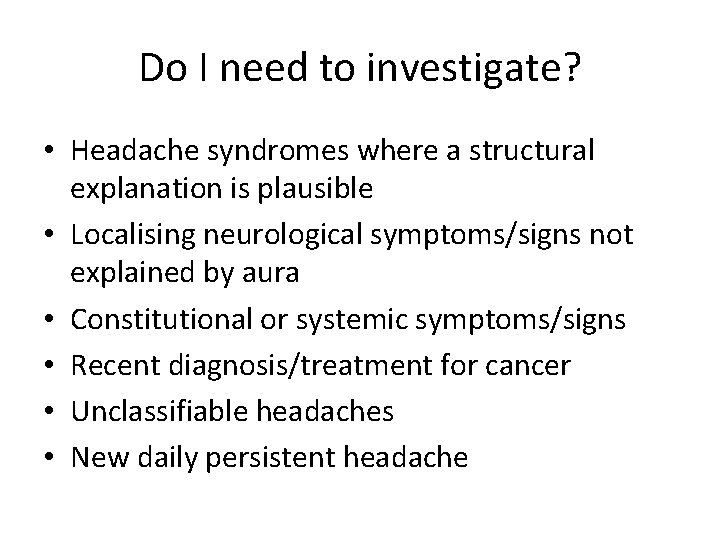
Do I need to investigate? • Headache syndromes where a structural explanation is plausible • Localising neurological symptoms/signs not explained by aura • Constitutional or systemic symptoms/signs • Recent diagnosis/treatment for cancer • Unclassifiable headaches • New daily persistent headache
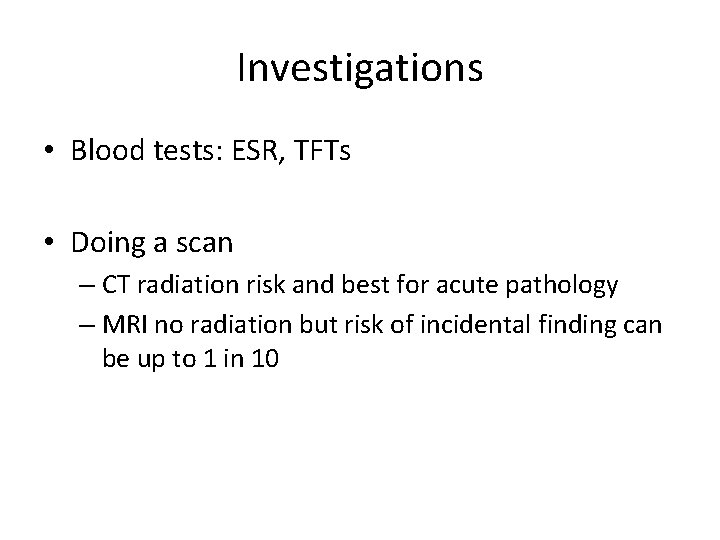
Investigations • Blood tests: ESR, TFTs • Doing a scan – CT radiation risk and best for acute pathology – MRI no radiation but risk of incidental finding can be up to 1 in 10
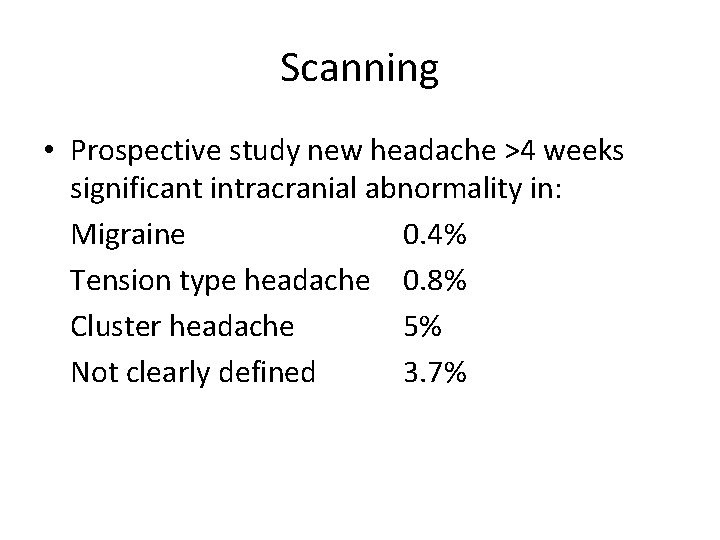
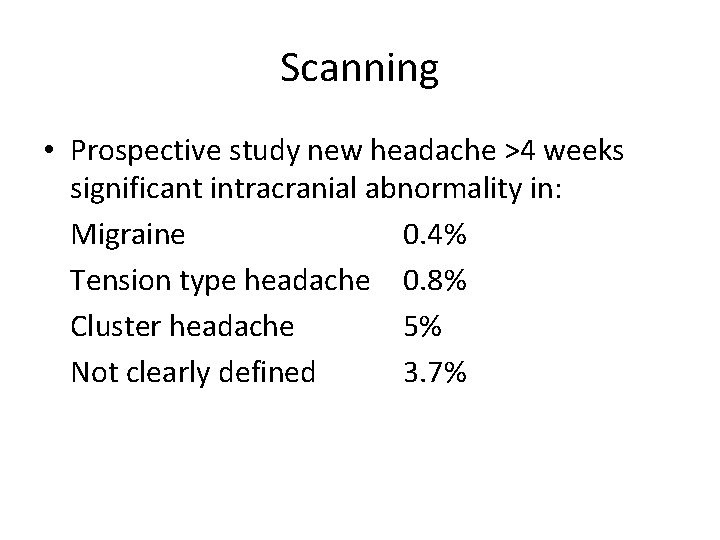
Scanning • Prospective study new headache >4 weeks significant intracranial abnormality in: Migraine 0. 4% Tension type headache 0. 8% Cluster headache 5% Not clearly defined 3. 7%
What does the patient want? • Explanation • Reassurance • Treatment
Is treatment appropriate? • Headache diary • Avoid opiates
Medication overuse headache • Most common culprits opiates-(codeine) and triptans • Any acute symptomatic treatment can cause it • Patients often under report what they are taking • Need to stop all medication for 7 -10 days • Then consider preventative treatment
Management of tension type headache • Lifestyle issues – work-home-leisure balance – exercise – sleep • Physical measures – relaxation – massage – self-help • Drugs – limited simple analgesics – Amitriptyline – SSRIs
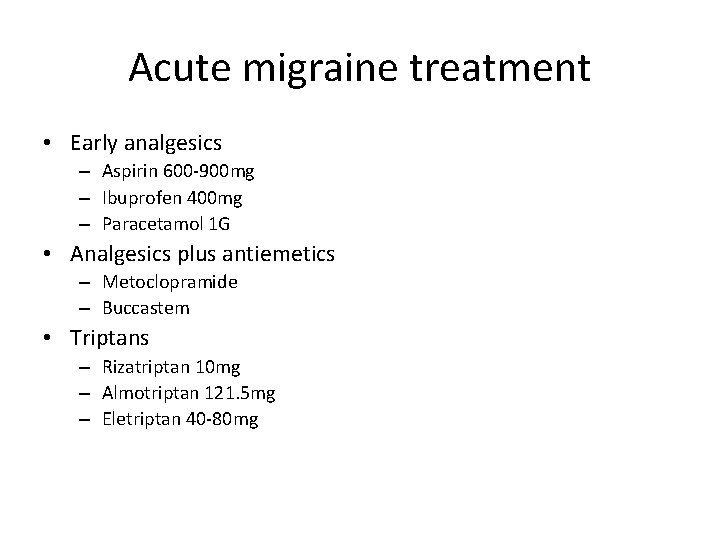
Acute migraine treatment • Early analgesics – Aspirin 600 -900 mg – Ibuprofen 400 mg – Paracetamol 1 G • Analgesics plus antiemetics – Metoclopramide – Buccastem • Triptans – Rizatriptan 10 mg – Almotriptan 121. 5 mg – Eletriptan 40 -80 mg
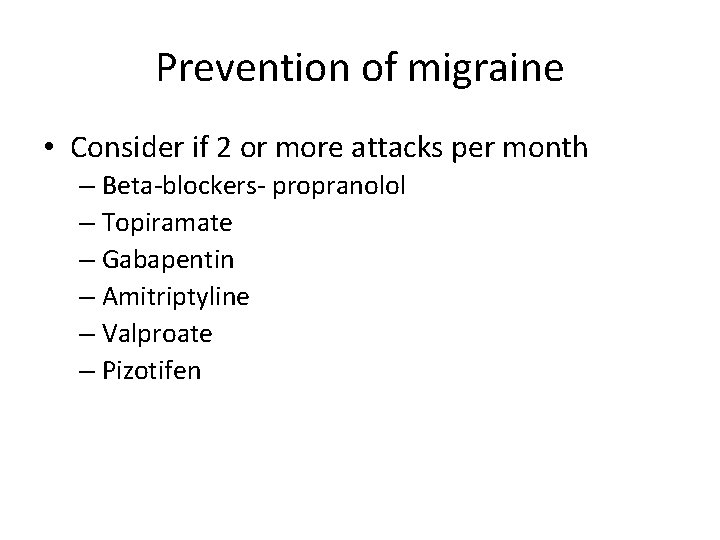
Prevention of migraine • Consider if 2 or more attacks per month – Beta-blockers- propranolol – Topiramate – Gabapentin – Amitriptyline – Valproate – Pizotifen
Cluster headache • Acute- oxygen or triptan (subcut or nasal) • Prophylaxis -Verapampil
Review • Classification of headaches – Primary headaches – Secondary headache disorders • Investigations and scanning • Patient expectations • A sensible approach to treatment
Indications for referral? 1. Where specialist diagnosis is required 2. Clincal features suggest significant or serious neurological disease 3. Failure to respond to appropriate adequate treatment 4. Patient at high risk of serious disease 5. Reassurance
Further reading • SIGN www. sign. ac. uk diagnosis and management of headache in adults: a clinical guideline • NICE guideline CG 150 Headaches: diagnosis and management of headaches in young people and adults