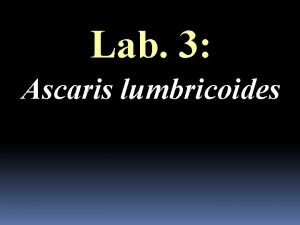
Nematodes of medical Importance I AFEKE UHAS ASCARIS


- Slides: 66
Nematodes of medical Importance I. AFEKE UHAS
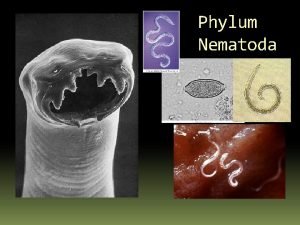
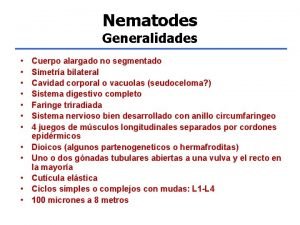
ASCARIS LUMBRICOIDES (ROUNDWORM) • Phylum: Metazoa • Sub-phylum: Nematoda • Infective agent: Ascaris lumbricoides
INTRODUCTION • Has a worldwide distribution and about 26% of the world’s population is infected. • Infection is common in both tropical/temperate regions where hygiene and sanitation standards are low. • Adults worms are normally found in the lumen of the small intestine • Infections is common in children
• In most areas there is a marked seasonal transmission cycle • Eggs can develop in sea water • Eggs do not embryonate below 18 o. C but can remain viable at 23 o. C for at least 40 days. • Clayey soils favour transmission better since they can retain moisture. • Eggs can remain viable in suitable soil for 7 days.
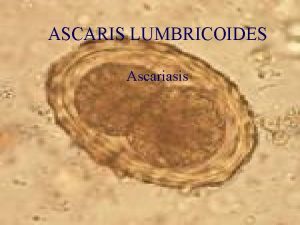
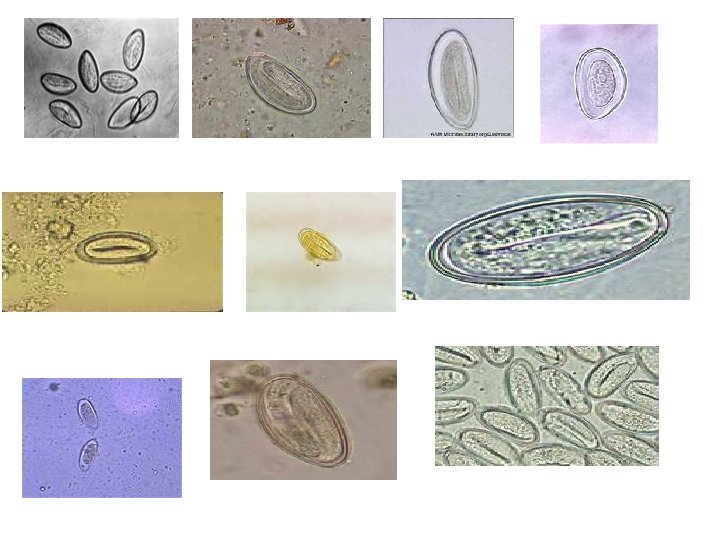
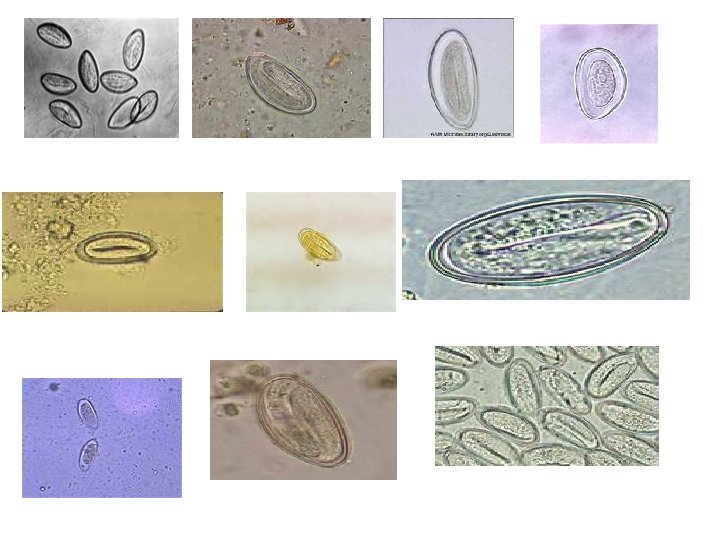
MORPHOLOGY • They are large and short tapering at both ends • Females are larger than males • Average daily output of eggs is between 200, 000 -250, 000 per female. • The posterior end of the male is curved and bears two spicules • Eggs when fertile are broad and ovoid, and have thick shells with coarse mammilated outer albuminous coat • About 15% of eggs are unfertilized and these have thin shells, are usually longer and narrow • Unfertilized eggs have irregular outer covering.

• Unfertilized Ovum Fertilized Ovum
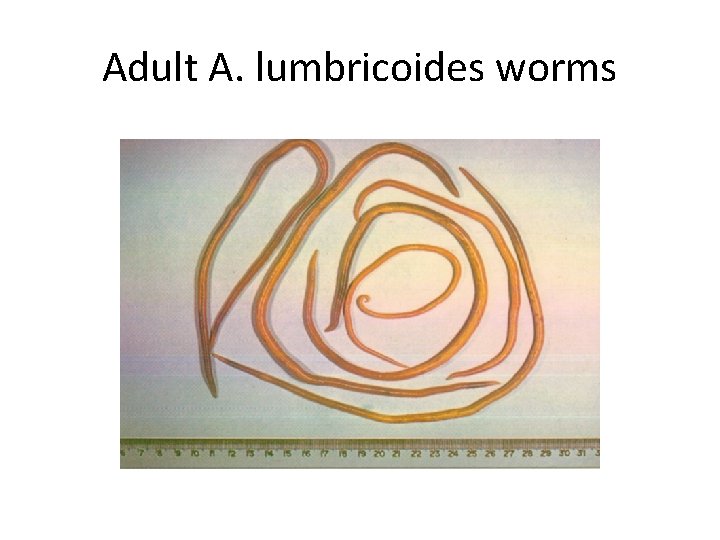
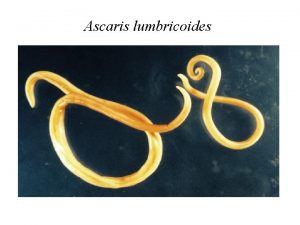
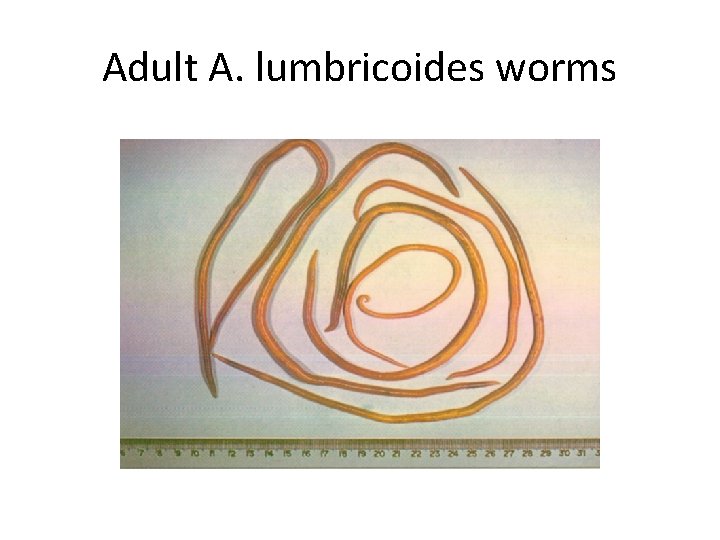
Adult A. lumbricoides worms
LIFE CYCLE • Fertilized ova passed in faeces take 10 -15 days to mature in moist soil or water • The second stage larvae is the infective stage • When a viable egg containing the infective stage larvae is ingested, it hatches in the duodenum • Larvae penetrate the mucosa and are carried in the lymphatics or veins through the liver to the heart and to the lungs in 3 days. • In the lungs they penetrate the alveoli, ascend the trachea and pass down the ileum, and mature as adults in 65 days • Adults can live for 1 -2 years.
CLINICAL MANIFESTATIONS • Majority of infections remain asymptomatic • However the presence of a few worms can be potentially dangerous • Clinical symptoms include • pneumonitis with cough/dyspnoea/substernal pain/fever/blood stained sputum which may contain larvae • These symptoms are known as Loffler’s syndrome • • Usually x-ray findings often show dense pulmonary infiltrations resembling acute T. B. • • There is moderate eosinophilia
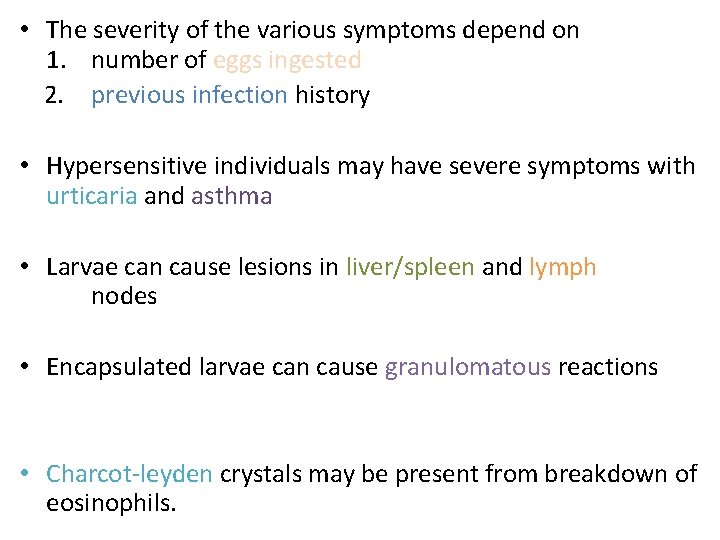
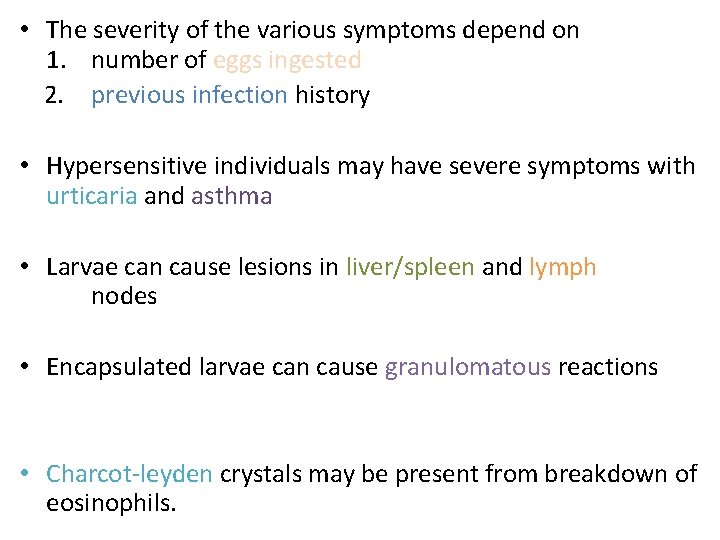
• The severity of the various symptoms depend on 1. number of eggs ingested 2. previous infection history • Hypersensitive individuals may have severe symptoms with urticaria and asthma • Larvae can cause lesions in liver/spleen and lymph nodes • Encapsulated larvae can cause granulomatous reactions • Charcot-leyden crystals may be present from breakdown of eosinophils.
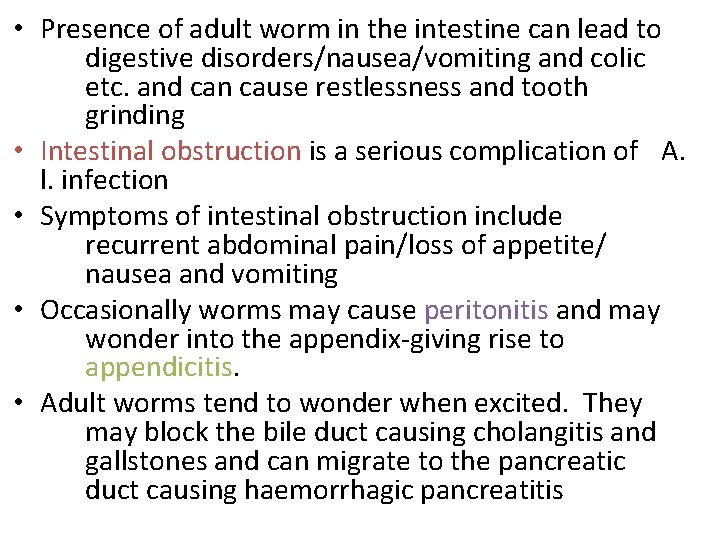
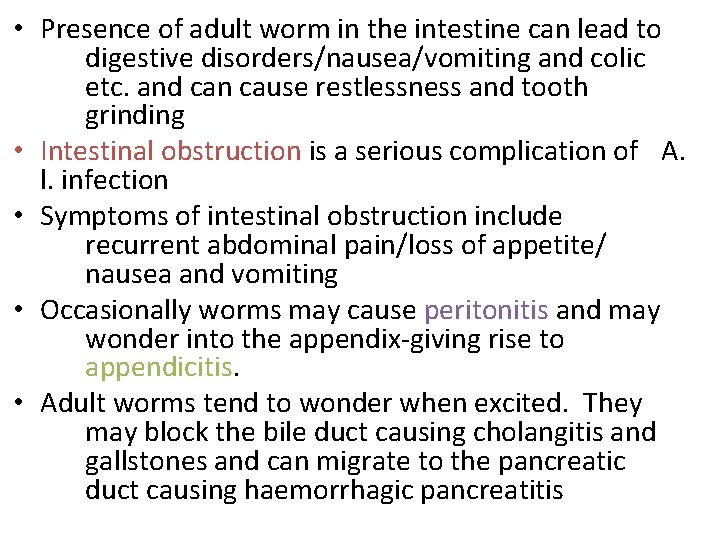
• Presence of adult worm in the intestine can lead to digestive disorders/nausea/vomiting and colic etc. and can cause restlessness and tooth grinding • Intestinal obstruction is a serious complication of A. l. infection • Symptoms of intestinal obstruction include recurrent abdominal pain/loss of appetite/ nausea and vomiting • Occasionally worms may cause peritonitis and may wonder into the appendix-giving rise to appendicitis. • Adult worms tend to wonder when excited. They may block the bile duct causing cholangitis and gallstones and can migrate to the pancreatic duct causing haemorrhagic pancreatitis
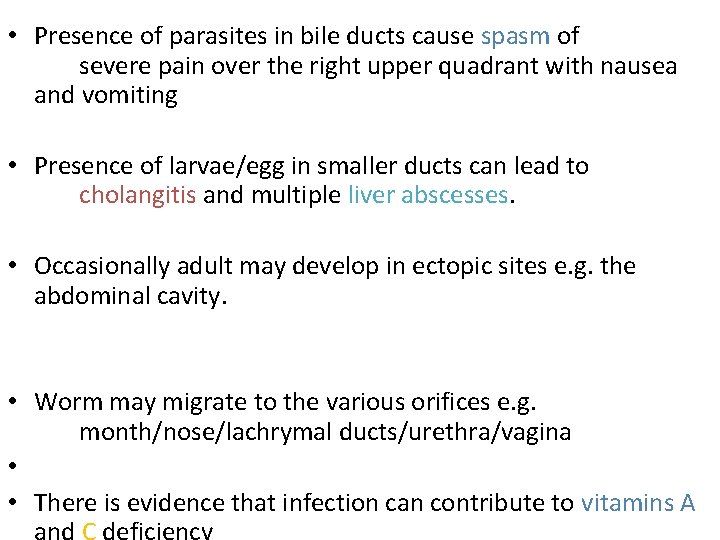
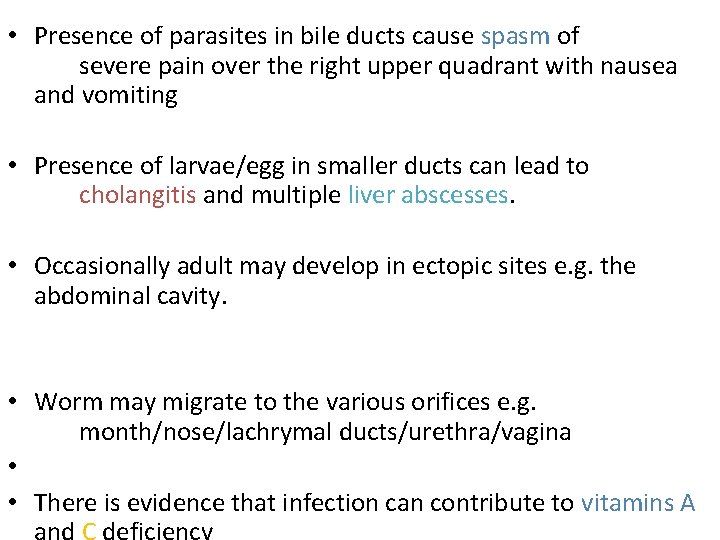
• Presence of parasites in bile ducts cause spasm of severe pain over the right upper quadrant with nausea and vomiting • Presence of larvae/egg in smaller ducts can lead to cholangitis and multiple liver abscesses. • Occasionally adult may develop in ectopic sites e. g. the abdominal cavity. • Worm may migrate to the various orifices e. g. month/nose/lachrymal ducts/urethra/vagina • • There is evidence that infection can contribute to vitamins A
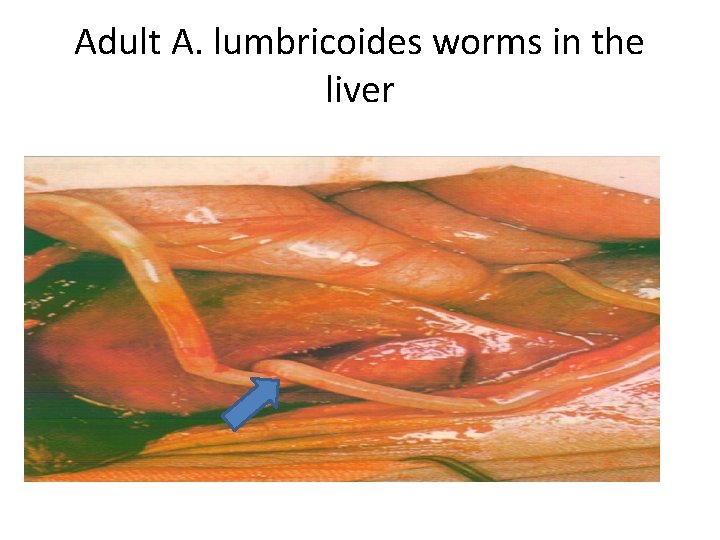
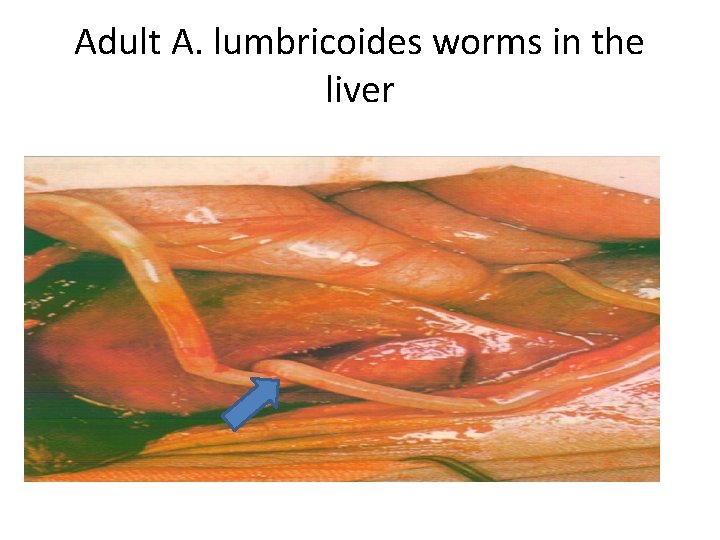
Adult A. lumbricoides worms in the liver
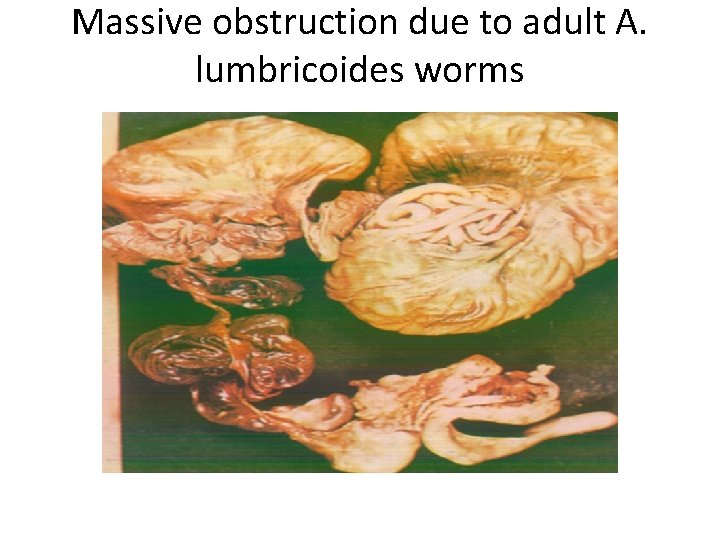
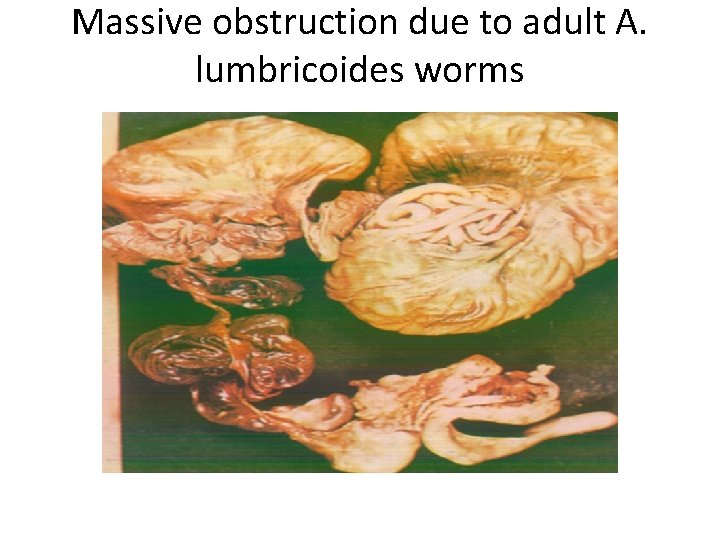
Massive obstruction due to adult A. lumbricoides worms
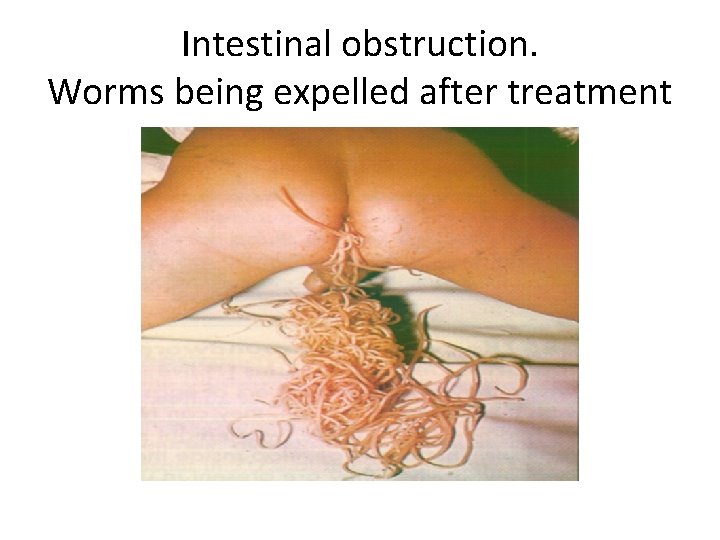
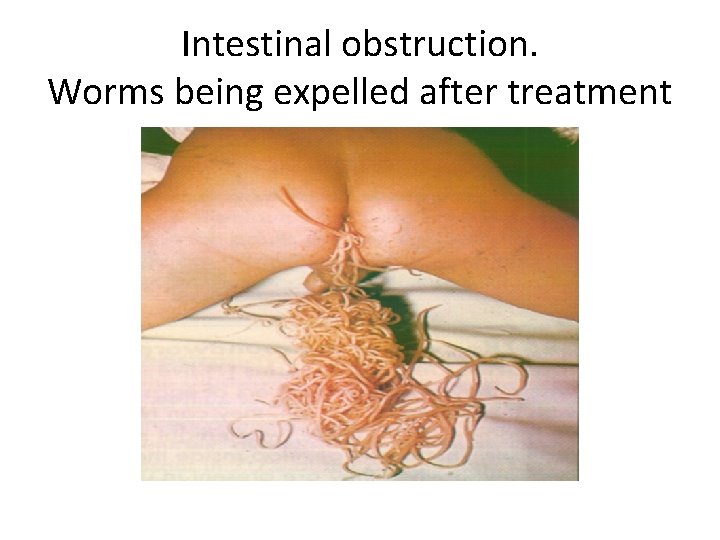
Intestinal obstruction. Worms being expelled after treatment
DIAGNOSIS • Eggs could be identified in stool preps using concentration methods/Kato thick smear techniques TREATMENT • Albendazole • Mebendazole • Ketraz etc.
ENTEROBIUS VERMICULARIS (PIN/THREAD WORM)
• Phylum: Metazoa • Sub-phylum: Nematoda • Infective agent: Enterobius vermicularis
INTRODUCTION • Suspected to be the most common helminthic infection • Has a worldwide distribution • Adults are found in the lumen of the caecum and appendix • May also be present in ascending colon and ileum
• Anterior end of worm is usually attached to the mucosa. • Infection is often asymptomatic • Infection often is common among the poor/children and is low among adults except mothers whose children are infected • Infections are shared in closed families
MORPHOLOGY • The organisms are small cylindrical nematodes • Are pointed at both ends • Females are larger than males and measures 8 - 13 x 0. 3 – 0. 5 mm • Females have long pointed tails • Male measures 2 – 5 x 0. 2 mm with curved posterior end • Males often die after copulation and appear in faeces.
TRANSMISSION • Direct transfer of infective eggs through contaminated hands from anus to month. • Indirectly through clothing/bedding/food or other articles contaminated with eggs. • Dust borne infection is possible in heavily contaminated institutions/households. • Eggs become infective within hours after deposition at the anus • Eggs can survive for about 2 weeks outside the host • Often during scratching eggs lodge in finger nails and are unknowingly carried to the mouth.
LIFE CYCLE • Gravid female migrates out of the anus at night and lays eggs (sticky and numerous) on perianal skin. • Female usually dies after oviposition possibly as a result of bursting • Gravid female can lay between 4, 000 – 17, 000 eggs in a lifetime. • Eggs have semi-transparent (thin) shell made up of an outer albuminous layer/two chitinous layers and an inner lipoidal membrane
• Eggs are laid usually partially embryonated containing infective 1 st stage (rhabditiform) larvae. • Outer layer (albuminous) is sticky and can cause itching in a sensitive person as does the activities of the female adults. • Eggs can be carried in dust and can be inhaled and swallowed • Eggs when swallowed release the 1 st stage larva in the duodenum
• Larva lodge in the crypts of ileum and moult twice • Young adults then move down the colon and attach to mucosa and mature in 15 -43 days. • Reinfection can occur if larvae are hatched on the perianal skin and migrate back into the anus. • Adult worm can live for 53 days. • Reinfection is more common in adults than in children and is responsible for recurrent mild infections every 40 -50 days.
CLINICAL MANIFESTATION • Usually asymptomatic • In children there could be loss of appetite and irritability • The most common symptom is perianal itching (prutitis/pruritus ani) which can lead to reduced sleep. • In females the vulva is involved and in girls E. vermicularis is the commonest cause of pruritis vulvae.
• Other symptoms include: vulvovaginitis salpingitis pelvic/liver granulomata • Appendicitis have been reported in some patients, though rare • Eosinophilia is common in 4 – 12% of infected individuals • Scratching may lead to secondary infections of the anal region
PATHOGENESIS • Ulcerative/haemorrhagic lesions of the small/large intestines have been reported but may be coincidental • Adult worms can cause necrotic changes by blocking the lumen of the appendix • In about 20% of young girls gravid female worms migrate into the vagina/uterus and can evoke an endometritis • Peritoneal granulomas containing eggs are frequently found in women
DIAGNOSIS • Ova could be found in faeces but are rare • Ova are better looked for in the perianal region using a swab (Graham swab). • Ova can be obtained by the cellophane method (Scotch tape) • Adult worms can be found on the surfaces of stools in heavy infections • Adults can sometimes be found around the anus or in the vulva in the evening
TREATMENT • Drugs of choice Albendazole Mebendazole • Other drugs Antepar Combantrin Ketax
STRONGYLOIDES – STERCORALIS
• Phylum: Metazoa • Sub-phylum: Nematoda • Infective agent: Strongyloides stercoralis
INTRODUCTION • Widely distributed but common in the tropics • Commonly co-exists with hookworm infection • Infection rate is about 25% in the tropics • • Larvae are unable to withstand temps below 8 o. C or above 40 o. C
• Strongyloides infections are less common than hookworm infections although S. s. females are more prolific that those of hookworms • • Reasons for rare Strongyloides infection are • a. Rabditiform larvae (1 st stage) are less resistant than hookworm eggs • b. Filariform larvae have a much shorter longevity • Transmission is entirely man to man although chimpanzees and dogs have been found to be naturally infected
MORPHOLOGY • Females are small, transparent, and filiform • Oesophagus occupies the anterior third of the body • Eggs are thin shelled/transparent/ovoid • Eggs are partially embryonated and usually hatch in tissues • Males are rare so females possibly produce eggs by parthenogenesis. • S. s can undergo one or many life cycles in the soil and remain free-living.
• Life cycle is direct LIFE CYCLE • Eggs are laid in the mucosa/submucosa of the small intestine • Eggs develop and hatch as rhabditiform larvae which escape into the intestinal lumen and are passed out in faeces • Larvae can be differentiated form those of hookworms by the presence of smaller buccal capsule • Larvae feed in soil and moult twice to become filariform (infective stage)
• The infective filariform larvae differ from those of hookworms by • a. the lack of sheath • b. the triradiate tip of the tail • c. the length of the pharynx • On contact with man, the larvae penetrate the skin to reach the small cutaneous blood vessels then they migrate to the liver, the heart and the lungs • After moulting twice, larvae penetrate the aleveoli / pass through the bronchi and trachea down the oesophagus to reach the stomach and the small intestine. • Once in the intestine the female burrows into the mucosal tissues, matures and lays eggs.
• Autoinfection could be brought about by rhabditiform larvae in faeces deposited on the perianal skin. • They develop into filariform larvae, which then penetrate through the skin. • In severely ill people/or people with chronic infections, rhabdition larvae passing down the gut may develop into filariform without reaching the exterior. • These filariform larvae penetrate the intestinal mucosa without coming out • In cases where patients’ resistance is low, all larval stages may be found in many of the visceral organs and rhabditiform/filariform larvae may even appear in sputum
CLINICAL MANIFESTATIONS • Most infected people are asymptomatic • There may be abdominal discomfort/intermittent gastric pain / diarrhoea / generalized urticaria • In serious clinical disease, presentations include, enteritis/malabsorption syndrome and electrolyte imbalance •
PATHOGENESIS Can be divided into 3 1. Penetration of skin by filariform larvae- causes no ground itch Where autoinfection is occurring there may be perianal and perineal ulceration. 2. Migrating larvae cause pneumonitis similar to Loffler’s syndrome in Ascariasis 3. Activities of adult females living/laying their eggs in the depths of the crypts of the ileum lead to inflammatory reactions
• In severe autoinfections, the submucosa becomes oedematous due to the presence of parasites • The mucosal layer becomes flattened and atrophic • Granulomatous lymphangitis may also result from the presence of the larva in lymphatics which coupled with inflammations and fibrosis causes a marked congestion and loss of elasticity of the gut • There could be severe haemorrhage/ulcerative enterocolitis with massive invasion of the whole bowel by larvae • Death may occur as a result of septicemia
• Disseminated strongyloidiasis occurs when the body’s cell-mediated immune responses are deficient. • In patients with malignant lymphoma larvae may be found in most organs of the body. • Fatalities may occur when larvae appear in the brain in cases where immunosuppressive drugs are used
DIAGNOSIS • Stool examination for rhabditiform larvae • Baermann filtration • No serological techniques yet TREATMENT • Albendazole / Mebendazole / Ivermectin

HOOKWORM INFECTIONS
• Phylum: Metazoa • Sub-phylum: Nematoda • Infective agents: Ancylostoma duodenale Necator americanus
INTRODUCTION • Hookworm infections are found in most tropical and subtropical areas • These are intestinal nematodes belonging to the Geohelminth group • The two most common human hookworms are Ancylostoma duodenale and Necator americanus • These are often present in huge numbers attached to the small intestine from where they suck blood and protein causing hookworm anaemia, stunted growth, general laziness and mental distress.
• The diagnostic stage of these two species (eggs) is essentially identical for both • Necator americanus – is common in far East, South Asia, South America, Tropical Africa etc • Ancylostoma duodenale – is found in Middle East, China, Japan etc. • Both species however can be found in multiple infections in Africa, Asia, South America etc.
MORPHOLOGY ANCYLOSTOMA DUODENALE • Small cylindrical, white, grey or reddish brown • They have 2 pairs of teeth for attachment to the small intestines (intestinal mucosa) • Male has a copulatory bursa at the rear end • Females are slightly larger than the males • Adult worm can live for 6 years or more • Female can produce 25, 000 – 35, 000 eggs each day and about 18 -54 million eggs during its life time. • Eggs are elliptical with a transparent shell – when freshly laid contains 2 or 4 segments (ie. blastomeres)
• NECATOR AMERICANUS Is shorter and more slender than Ancylostoma duodenale • The eggs of the females are slightly larger than that of A. duodenale • Female lays 6, 000 – 20, 000 eggs daily and life duration is on the average of 5 years.
LIFE CYCLE • On coming into contact with the human skin infective larvae (filariform larvae) penetrate the skin usually between the toes and joints and undergo migration. • They then enter the circulatory system and are carried to the heart and then to the lungs in 3 days. • In the lungs they penetrate the alveoli form where they ascend the bronchi and trachea to the oesophagus. • They are then swallowed and they reach the intestine in 24 hours (7 th day of infection)
• During migration the larvae moult and become sexually differentiated • They attached to the walls of the small intestines and sucks blood from their host. • The worms keep migrating (particularly A. duodenale) to new sites to suck more blood leaving the old and abandoned sites bleeding. • The adults live for 5 -6 years but could live up to 14 years
DIFFERENCES IN THE LIFE CYCLE • A. duodenale can infect by ingestion as well as through skin penetration • N. americanus infect only through skin penetration • During migration, larvae of N. americanus grow and develop in the lungs while those of A. duodenale do not
MODES OF INFECTION • Penetration through the skin (filariform larvae) • Orally through ingestion of larvae in contaminated food (A. d) • Contact with soiled clothes (faeces stained clothes) • Eating of uncooked meat containing larvae of A. duodenale, which have migrated into muscles of the animal where they survive for 26 – 34 days. • Through human milk – migrating filariform larvae of A. duodenale arrested in their development and migrated into the mammary glands where they are excreted in the milk and infect children.
• Transmission in children may be as a result of a. Laying of infants on contaminated soil b. Infected diapers c. Transplacental infection (rare)
PATHOLOGY • Ancylostoma duodenale – causes pathology at 3 stages of its infection. • A) Vesiculation (blister formation) and pustulation (elevation of skin containing purulent exudates filled with neutrophils) at site of entry (ground itch) • B) Asthma and bronchitis (inflammatory rxn) during migration through the lungs • C) Established intestinal infections – usually seen in endemic areas.
CLINICAL MANIFESTATIONS • Larval penetration may lead to severe prutitis, erythematous popular rash called the ground itch – usually at site of entry. • Migrating larvae may cause pulmonary symptoms like pneumonitis, dry cough, asthmatic wheezing, fever accompanied by high degree of eosinophilia. • There is also necrosis of intestinal tissues • There could also be blood loss due to direct ingestion of blood (injection of anticoagulants)
• In acute infections there is usually fatigues, lassitude, nausea, digestive disturbances, vomiting, abdominal pain, diarrhoea with black or red stools • In chronic especially in indigenous people, the main symptom is iron deficiency anaemia associated with gastric and intestinal dyspepsia (indigestion) • There is also oedema of the face and feet/ankles or generalized oedema there could be exhaustion breathlessness, palpitations • In children, the symptoms include, diarrhoea, vomiting, pallor and massive haemorrhage
HOOKWORM ANAEMIA • Hookworms are suspected to cause chronic blood loss and depletion of iron stores • This is due to the fact that they are habitual blood suckers and need serum for development • This type of anemia is related to worm load or burden • Blood loss is estimated at 0. 03 mls/day/ N. americanus 0. 15 ml/day/A. duodenale • Hookworm anemia is a common cause of heart failure in the tropics
HYPO PROTEINAEMIA: (LOW SERUM PROTEIN CONCENTRATION) • This presentation is as a result of enteropathy, (diseases of the intestine) blood loss and the limited capacity for albumin synthesis. • HOOKWORM ENTEROPATHY Hookworm are believed to cause malabsorption
DIAGNOSIS • Definitive diagnosis of infection depends on demonstration of eggs in stool • a. Direct smear or wet preparation. • b. Concentration techniques (light infections) a. Formol ether technique b. Na. Cl floatation technique c. Kato smear • Rhabditiform larvae may be found in stale stools and may be mistaken for Strongyloides in which larvae only and not eggs are found in stools. • Serological diagnosis is not practical since there are so many cross-reactions with other helminthes.
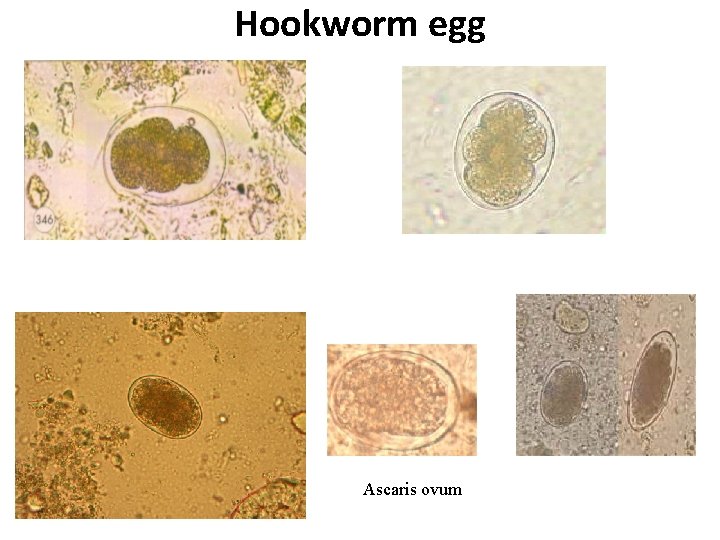
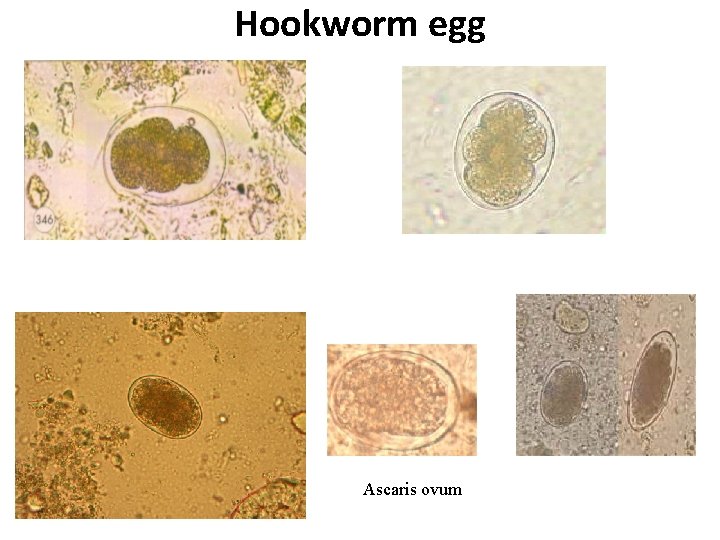
Hookworm egg Ascaris ovum
TREATMENT • Is targeted at 2 things a. Elimination of the parasite b. Treatment of anemia if present
ELIMINATION OF PARASITE (ADULT) • a. Albendazole: Effective against both A. duodenale and N. americanus (80% reduction in of egg count in a single dose of 400 mg. • b. Mebendazole: Effective against both A. duodenale and N. americanus • c. Levamisole • d. Combantrin (pyrantel pamoate) • e. Akopar (Bephenium hydroxynaph thoate) TREATMENT OF ANAEMIA • Oral administration of iron either in the form of ferrous sulphate or gluconate
PREVENTION • Sanitary disposal of faeces • Good health Education programme • Wearing of foot wear/soil sterilization • Avoid the use untreated faecal water for fertilizing gardens and farms etc. (Agricultural/cultural practices) • Avoid defaecation into the soil etc.
 Nematodes
Nematodes Nematoda fun fact
Nematoda fun fact Roundworm phylum name
Roundworm phylum name Nematoda
Nematoda Pseudocoelomate diagram
Pseudocoelomate diagram Morphology of nematodes
Morphology of nematodes Aceolomates
Aceolomates Characteristics of nematodes
Characteristics of nematodes Excretory system of nematodes
Excretory system of nematodes Mortar and pestle appearance
Mortar and pestle appearance Nematodes
Nematodes Renette cells in nematodes
Renette cells in nematodes Foliar nematodes treatment
Foliar nematodes treatment Are nematodes hermaphroditic
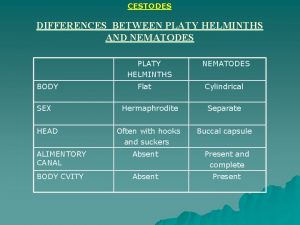
Are nematodes hermaphroditic Platy helminths
Platy helminths Anatomy of nematodes
Anatomy of nematodes Nematoides sistema digestorio
Nematoides sistema digestorio Ascaris
Ascaris Aschelminthes habitat
Aschelminthes habitat Ascaris lumbricoides
Ascaris lumbricoides Ascaris lumbricoides infective stage
Ascaris lumbricoides infective stage Phylum of ascaris lumbricoides
Phylum of ascaris lumbricoides Ascaris
Ascaris Pseudocoeloma
Pseudocoeloma Living organisms differ in
Living organisms differ in Ascaris lumbricoides คือ
Ascaris lumbricoides คือ Ascaris lumbricoides female cross section
Ascaris lumbricoides female cross section Taenia saginata huevo
Taenia saginata huevo Parasite ascaris
Parasite ascaris Strongyloides stercoralis
Strongyloides stercoralis Ascaridase
Ascaridase Ascaris
Ascaris Copulatory bursa
Copulatory bursa Masaryk university medical faculty
Masaryk university medical faculty Corticated and decorticated ascaris ova
Corticated and decorticated ascaris ova Graham scotch tape method
Graham scotch tape method Cordones necator
Cordones necator Ascaris
Ascaris Rotifera
Rotifera Ascaris lumbricoides symptoms
Ascaris lumbricoides symptoms Nematodeo
Nematodeo Ancylostoma
Ancylostoma Parasitic arthropods
Parasitic arthropods Taenia
Taenia Infoveterinar
Infoveterinar Filo nematelmintos
Filo nematelmintos Ascaris lumbricoides morphology
Ascaris lumbricoides morphology Ascaris lumbricoides taxonomy
Ascaris lumbricoides taxonomy Importance of medical law
Importance of medical law Tracer card in medical records
Tracer card in medical records Parasites of medical importance
Parasites of medical importance Torrance memorial transitional care unit
Torrance memorial transitional care unit Doctors license number
Doctors license number Cartersville medical center medical records
Cartersville medical center medical records Gbmc medical records
Gbmc medical records Hepburn osteometric board
Hepburn osteometric board Importance of amino acids
Importance of amino acids Difference between rm and crm
Difference between rm and crm Agricultural economics
Agricultural economics Types of natural vegetation in india
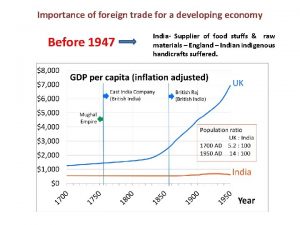
Types of natural vegetation in india Importance of foreign trade
Importance of foreign trade Ksbe blackboard
Ksbe blackboard What language is it
What language is it 10 importance of agriculture
10 importance of agriculture Importance of faculty in higher education
Importance of faculty in higher education Importance of data independence in database environment
Importance of data independence in database environment 100 dollar
100 dollar