MUCOPOLYSACCHARIDOSISMPS Dr NZIOKI CM CONSULTANT ENDOCRINOLOGIST MACHAKOS LEVEL






- Slides: 21
MUCOPOLYSACCHARIDOSIS-MPS Dr. NZIOKI CM CONSULTANT ENDOCRINOLOGIST MACHAKOS LEVEL 5 HOSPITAL
Outline • • • Introduction Mode of inheritance Classification Clinical presentation Diagnosis Management of MPS
INTRODUCTION • Mucopolysaccharidosis (MPS) are hereditary progressive disorders caused by defective catabolism of sulfated components of connective tissue- glycosaminoglycans (GAG’s) • The major GAGs are: v dermatan sulfate (DS) v heparan sulfate(HS) v keratan sulfate(KS) v. Chondroitin -4 - sulfate v. Hyaluronan
Introduction conti’ • Enzymes associated with GAG catabolism are lysosomal hydrolases • Patients with MPS have less than 1%residual enzyme activity • GAGs accumulate in lysosomes – this results in cellular dysfunction and clinical abnormality

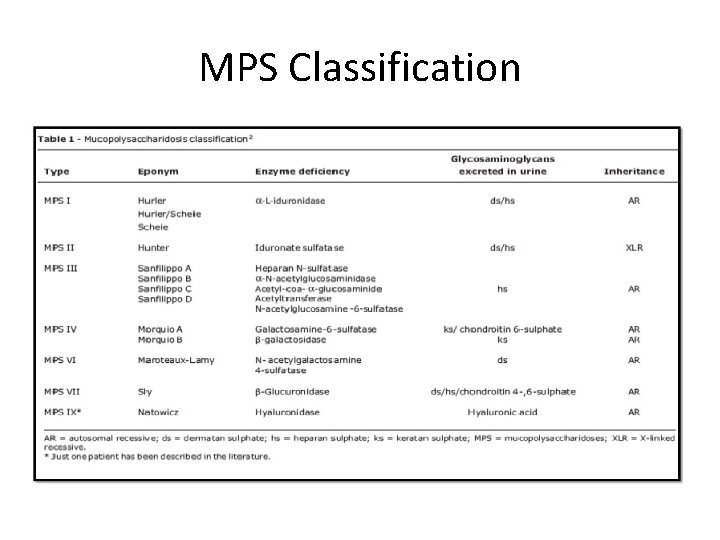
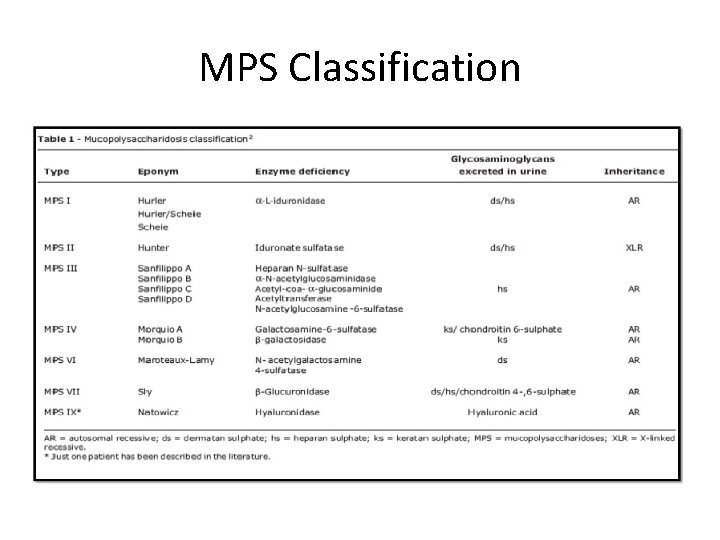
MPS Classification
MPS Classification • Four broad categories based on dominant clinical features o Soft tissue storage and skeletal disease with or without brain disease (MPS I, II, VII) o Soft tissue and skeletal disease(MPS VI) o Primary skeletal disorders (MPS IVA , IVB) o Primary central nervous system disorders ( MPS III A-D)
Clinical presentation • Many physical disorders • Varying degree of severity depending on MPS type • Features may not be apparent at birth but progress as storage of GAGs increase
Common presentations • CNS disease – mental retardation , developmental delay , severe behavioral problems , hydrocephalus • CVS disease- Valvular dysfunction • Pulmonary disease- airway obstruction, sleep apnoea • Opthalmologic – corneal clouding • Hearing impairment – deafness • Musculoskeletal disease- short stature, joint stiffness • Others – coarse facial features , hepatosplenomegally , hernia
Hurler , Hurler-Scheie, Scheie syndrome(MPS I) • • Autosomal recessive mode of inheritance Due to lysosomal α-L- Idoronidase deficiency Newborns are normal at birth Clinical features start manifesting by age 1 year
Clinical features • • • Developmental delay Coarse thick facial features Low nasal bridge Prominent dark eye brows Progressive joint stiffness Severe mental retardation




Diagnosis • High index of suspicion- a child with coarse facial features, bone disease, developmental delay, short stature, hepatosplenomegally , corneal clouding • GAG urinary concentration • Lysosomal Enzyme assay – definitive diagnosis from cultured fibroblasts, leukocytes • Prenatal diagnosis in selected family clustersamniocytes and chorionic villus culture

Management of MPS • Goal- to reduce severity of symptoms and improve quality of life • Multidisciplinary team care v. Neurologist v. Pediatrician v. Cardiologist v. Ophthalmologist v. Audiologist v. Orthopedic surgeon v. Physical and occupational therapist
Management • Supportive care especially physical therapy is critical • Main treatment modalities are v. Haematopoietic stem cell (peripheral blood leukocytes) transplant (HSCT) for MPS I and II. Has high risk of morbidity and mortality from cardiac and pulmonary complications. Reduces clinical progression of some features in some children v. Enzyme replacement therapy (ERT)- MPS I, II, VI • Treatment results in improvement of somatic disease
Thank you Asanteni
Reference • Joseph Muenzer. Overview of the mucopolysaccharidosis, , Rheumatology, Vol 50, 2011 • Thomas J et al. Diagnosis of mucopolysaccharidosis, Rheumatology , Vol. 50, 2011 • Lone Clark. Mucopolysaccharidosis type 1. Gene reviews 2016
 Hyperpigmentation in cushing syndrome
Hyperpigmentation in cushing syndrome 1562007 color
1562007 color Endocrinologist in parbhani
Endocrinologist in parbhani Dr maeve durkan cork
Dr maeve durkan cork Dr swade endocrinologist
Dr swade endocrinologist Dimitrios thomas endocrinologist
Dimitrios thomas endocrinologist Oha drugs
Oha drugs Dr. alireza amirbaigloo, md, endocrinologist
Dr. alireza amirbaigloo, md, endocrinologist Dr. alireza amirbaigloo, md, endocrinologist
Dr. alireza amirbaigloo, md, endocrinologist Endocrinologist lifestyle
Endocrinologist lifestyle Endocrinologist newcastle
Endocrinologist newcastle Dr ponder endocrinologist
Dr ponder endocrinologist Epicor sls
Epicor sls Scan based trading data
Scan based trading data Chinchilla business consultant
Chinchilla business consultant What is a consultant radiographer
What is a consultant radiographer Wireless communication consultant
Wireless communication consultant Judith james educational consultant
Judith james educational consultant Consultant contract 2003
Consultant contract 2003 Microsoft flow consultant
Microsoft flow consultant Partner technical consultant
Partner technical consultant Internet consultant job description
Internet consultant job description