MINERALS AND TRACE ELEMENTS Jana Novotn 1 Major
- Slides: 32
MINERALS AND TRACE ELEMENTS Jana Novotná
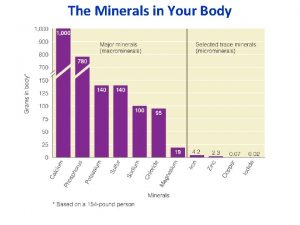
1. Major components of body molecules C, H, O, N, S (obtained through intake of water fat, carbohydrates, proteins) 2. Nutritionally important minerals Ca, P, Mg, Na K, Cl (<100 mg/day) 3. Trace elements Cr, Co, Cu, I, F, Fe, Mn, Mo, Se, Zn 4. Additional elements (non-essential for humans) Ni, Sn, V, B, Li
Transport and storage require specific binding to carrier proteins Transferrin – Fe, Cr, Mn, Zn Albumin – Cu, Zn Amino acids – Cu, (Fe) Trancobaltamin - Co Globulins - Mn
Normal routes of excretion of trace elements Bile – Cu, Mn, Cr, Zn, Urine – Co, Cr, Mo, Zn Pancreatic juice – Zn Sweat – Zn Mucosal cell sloughing – Fe, Zn
Sodium • Na+ is the major cation of extracellular fluid. • Plasma concentration - 135 -145 mmol/L • ICT concentration - 3 -10 mmol/L. • Maintaining of total body fluid homeostasis and water balance. • Decrease in blood pressure and decreases in sodium concentration result in the production of renin → aldosteron production → decreases the excretion of sodium in the urine
Sodium • Hypernatremia is associated with water depletion (dehydratation). • Low serum Na+ - hyponatremia, is associated with excess of intravascular (and perhaps extravascular) water. • Maintaining electric potential in animal tissues • Na+ are important in neuron (brain and nerve) function – action potential • Na+ are important in maintaining and influencing osmotic balance between cells and the interstitial fluid • Distribution is mediated by the Na+/K+-ATPase pump
Potassium • K+ is the principal cation of the intracellular fluid. • Plasma concentration - 3, 5 - 5, 2 mmol/L. • ICF concentration - 110 -160 mmol/L. • Key role of K+ in skeletal and smooth muscle contraction • The main dietary source is the cellular material we consume as foodstuffs.
Potassium • The concentration of K+ in plasma is influenced by the p. H of the blood (physiological p. H 7, 4 ± 0, 04). • Alkalosis (p. H > 7. 44) causes hypokalemia → transient shifting of K+ into cells, presumably by stimulation of the Na-K-ATPase. • Acidosis (p. H < 7, 36) causes hyperkalemia → transient shifting of K+ from cells at the expense of H+ • Hyperkalemia produces characteristic electrocardiographic changes (life-threatening effect of K+ excess on the heart).
Calcium • Total content of calcium in the body is more than 1200 mg. • 99% of total content is deposit in bones and teeth, • 1% in blood and body fluids • Intracellular calcium: - cytosol - mitochondria - other microsomes - regulated by "pumps" The serum level of calcium is closely regulated with a normal total calcium of 2 -2. 75 mmol/L (9 -10. 5 mg/d. L) and a normal ionized calcium of 1. 1 -1. 4 mmol/L (4. 5 -5. 6 mg/d. L).
Calcium metabolism Multiple biological functions of calcium Cell signaling Neural transmission Muscle function Blood coagulation Enzymatic co-factor Membrane and cytoskeletal functions Secretion Biomineralization
Calcium metabolism • Absorption – duodenum and proximal jejunum. • Active transport across cells. • Calcium-binding proteins (calbindins) are synthesized in response to the action of 1, 25 dihydroxycholecalciferol (vitamin D 3). • Parathyroid hormone – also increased intestinal absorption of Ca.
Calcium metabolism Absorption is inhibited by: oxalates (salts of oxalic acid), phytates (salts of phytic acid - found in grain, soyabeans), phosphates (formation of insoluble salts), sodium, caffein
Recommended daily amount: Children to age 11 – 1200 mg/day From age 11 to 24 – 800 mg/day From age 24 – 500 mg/day In woman after menopase – 1500 mg/day (osteoporosis prevention). Deficiency - hypocalcemia tetany, increased neuromuscular excitability, neurological disoders. Result of vit. D deficiency, hypoparathyroidism, renal insuficiency. Symptoms are: rickets (children), osteomatacia (adults) Toxicity – hypercalcemia (normally does not to occur) Hyperparathyroidism, vitamin D intoxication, cancer.
Phosphorus metabolism Major role in structure and function of all living cells and as a free ion Integral part of: nucleic acids nucleotides phospholipides phosphoproteins Enzymes that attach phosphates in ester or acid anhydride linkages Other enzymes (phosphatases, pyrophosphatases) Blood phosphate: H 2 PO 4 - and HPO 42 - Concentration measured as phosphorus: 2. 5 - 4. 5 mg/100 ml Skeletal hydroxyapatite - Ca(PO 4)2 or Ca(OH)2
Phosphorus metabolism Absorption in the jejunum. Phosphate absorption is regulate by 1, 25 dihydroxycholecalciferol and parathyroid hormone. PTH mediates mobilization and deposition of calcium and phosphate from bone. Deficiency Rickets in children, osteomalacia in adults. Abnormalities in erythrocytes, leucocytes, platelets, liver. Depletion of phosphate occurs as a result of diminished absorption from intestine or excessive wasting through kidney. Hyperphosphatemia is associated with renal diseases.
Magnesium • Nearly 99% of the total body magnesium is located in bone or the intracellular space. • Second plentiful cation of the extracellular fluids. • Mg is a cofactor of all enzymes involved in phosphate transfer 2+ reactions utilizing ATP and other nucleotide triphosphates as substrate. Required for the structural integrity of numerous intracellular proteins and nucleic acids. A substrate or cofactor for important enzymes such as adenosine triphosphatase, guanosine triphosphatase, phospholipase C, adenylate cyclase, and guanylate cyclase. A required cofactor for the activity of over 300 other enzymes. A regulator of ion channels; an important intracellular signaling molecule. A modulator of oxidative phosphorylation. • • • Mg 2+ is chelated between the beta and gamma phosphates, diminishes the dense anionic character of ATP
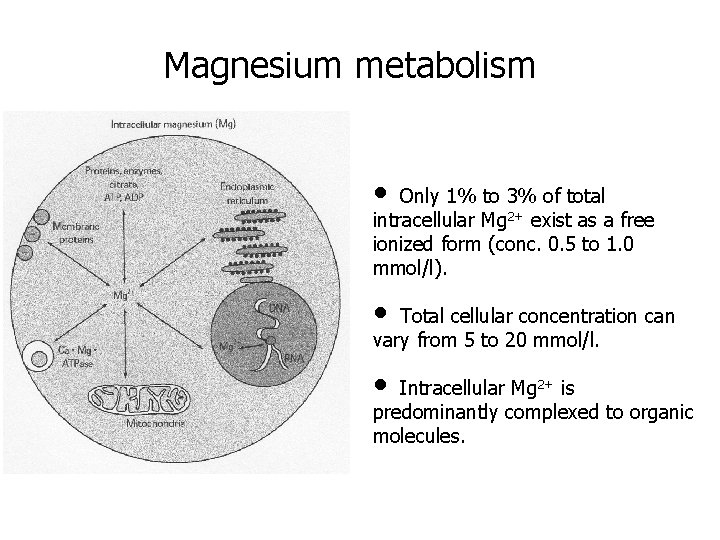
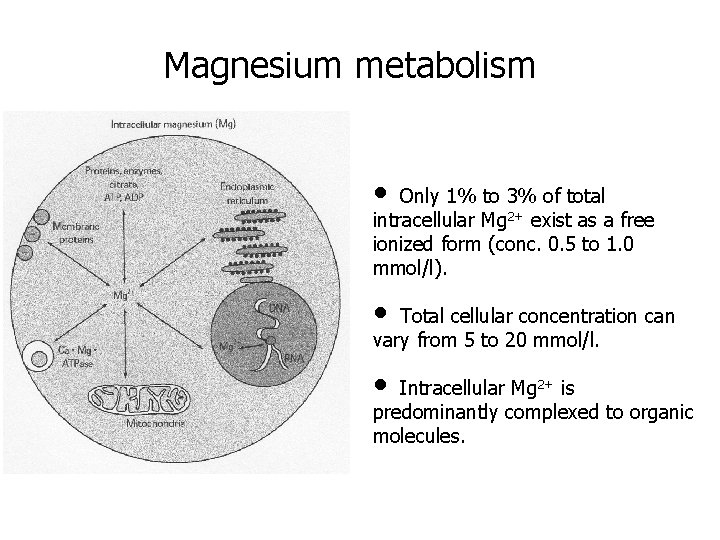
Magnesium metabolism • Only 1% to 3% of total intracellular Mg 2+ exist as a free ionized form (conc. 0. 5 to 1. 0 mmol/l). • Total cellular concentration can vary from 5 to 20 mmol/l. • Intracellular Mg 2+ is predominantly complexed to organic molecules.
Magnesium metabolism Effect on central nervous system: • Certain effects of Mg 2+ are similar to Ca 2+. • Increased concentration of Mg 2+ cause depression of CNS • Decreased concentration of Mg 2+ cause irritability of CNS Effect on neuromuscular system: • Direct depressant effect on skeletal muscles – excess of Mg 2+ cause decrease in acetylcholine release by motor nerve impulse. • The action of increased Mg 2+ on neuromuscular function are antagonized by Ca 2+. • Abnormaly low concentration of Mg 2+ in extracellular fluid result in increased acetylcholine release and increased muscle excitability (tetany). Excess of Mg 2+ cause vasodilatation.
Magnesium metabolism Hypomagnesemia cause: • changes in skeletal and cardiac muscle • changes in neuromuscular function, • hyperirritability, psychotic behaviour • tetany Hypermagnesemia cause: • muscle weakness • hypotension • ECG changes • sedation and confusion Hypermagnesemia is usual due to renal insuficiency.
Copper • Cu is an essential nutrient. • Rapid growth increases Cu demands in infancy. • The adult body contains approximately 100 mg of copper – the highest concentrations are in liver, kidney, and hearth. • The absorption in gastrointestinal tract requires a specific mechanism - metal binding protein metallothionein (Cu 2+ ions are highly insoluble). • Ceruloplasmin (CP) is a glycoprotein, copper-dependent ferroxidase (95% of the total copper in human plasma), oxidizes Fe 2+ to Fe 3+ in gastrointestinal iron absorption mechanism.
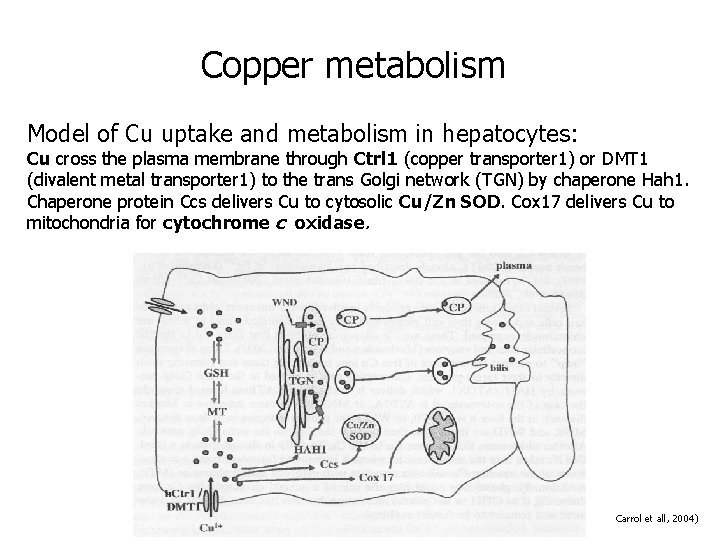
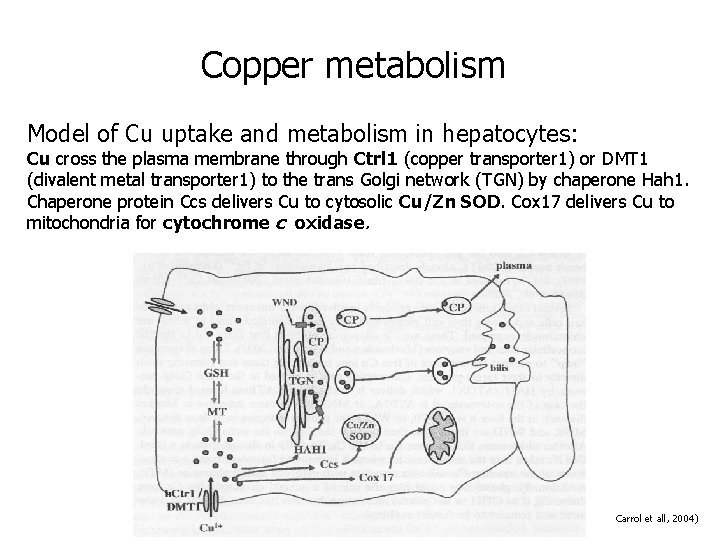
Copper metabolism Model of Cu uptake and metabolism in hepatocytes: Cu cross the plasma membrane through Ctrl 1 (copper transporter 1) or DMT 1 (divalent metal transporter 1) to the trans Golgi network (TGN) by chaperone Hah 1. Chaperone protein Ccs delivers Cu to cytosolic Cu/Zn SOD. Cox 17 delivers Cu to mitochondria for cytochrome c oxidase. Carrol et all, 2004)
Copper metabolism • Cu is an essential cofactor in a number of critical enzymes in metabolism: superoxide dismutase (Cu/Zn-SOD) cytochrome c oxidase (COX) tyrosinase monoamino oxidase lysyloxidase • Cu metabolism is altered in inflammation, infection, an cancer. • In infection, Cu is essential for production of Ile-2 by activated lymphocytes. • In cancer, plasma CP is positively correlated with disease stage.
Iron Major function of Fe – oxygen transport by hemoglobin. Fe 2+ and Fe 3+ are highly insoluble – special transporter systems are required. Food Fe is predominantly in Fe 3+, tightly bound to organic molecules. Apoferritin assimilates up to 4 300 Fe molecules to form Fe storage protein – ferritin. In the retikuloendothelial system ferritin provides an available storage form for iron. Apotransferrin (apo. Tf) – protein, that can bind 2 atoms of Fe to form transferrin, Fe carrier in plasma.
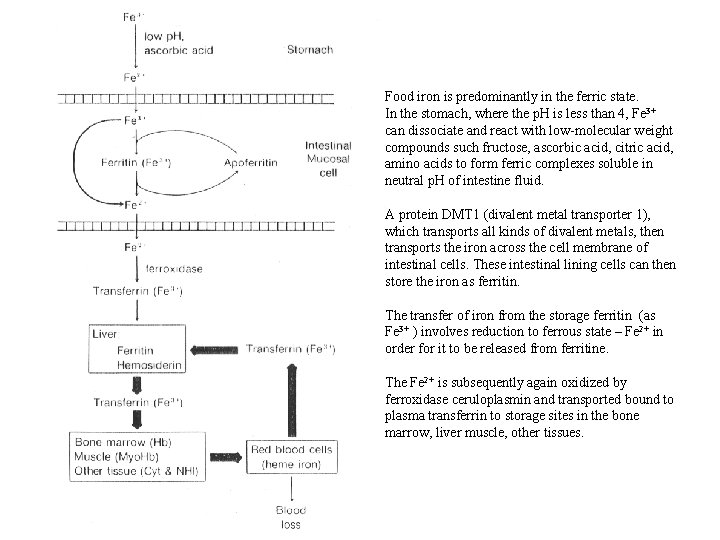
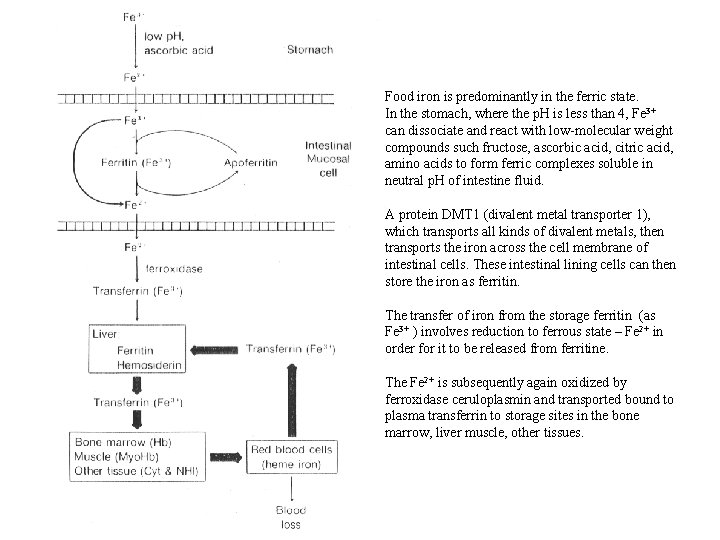
Food iron is predominantly in the ferric state. In the stomach, where the p. H is less than 4, Fe 3+ can dissociate and react with low-molecular weight compounds such fructose, ascorbic acid, citric acid, amino acids to form ferric complexes soluble in neutral p. H of intestine fluid. A protein DMT 1 (divalent metal transporter 1), which transports all kinds of divalent metals, then transports the iron across the cell membrane of intestinal cells. These intestinal lining cells can then store the iron as ferritin. The transfer of iron from the storage ferritin (as Fe 3+ ) involves reduction to ferrous state – Fe 2+ in order for it to be released from ferritine. The Fe 2+ is subsequently again oxidized by ferroxidase ceruloplasmin and transported bound to plasma transferrin to storage sites in the bone marrow, liver muscle, other tissues.
Molybdenum Metal required for the function of the metalloenzymes: xantine oxydase aldehyde oxidase sulfite oxidase Some evidence that Mo can interfere with Co metabolism by the diminishing the efficiency of copper utilization. (the foot content of Mo is highly dependent upon the soil type in which the foodstuff are grown).
Selenium • an integral component of glutathion peroxidase (intracellular antioxidant), • a scavenger of peroxides, • an essential element for immune function (selenoproteins). • Selenoproteins catalyse oxido-reduction reactions, protective function from oxidative stress (macrophage- or neutrophil-generated free-radical species, UV in sunlight. The foot content of Se is highly dependent upon the soil type in which the foodstuff are grown.
Manganese • High concentration of Mn 2+ is present in mitochondria • Functions as a necessary factor for activation of glycosyltransferases (enzymes responsible for the synthesis of oligosaccharides, glycoproteins, proteoglycans. • Required for superoxid dismutase activity, for activity of metalloenzymes: hydrolases kinases decarboxylases transferases. Deficiency of Mn extensively reduce glycoprotein and proteoglycan formation.
Zinc Component of zinc metalloenzymes : carbonic anhydrase lactate dehydrogenase glutamate dehydrogenase alkaline phosphatase thimidine kinase matrix metalloproteinases Gustin – protein in saliva – major role in taste.
Zinc Deficiency of Zn has serious consequence : • failure metabolism of nucleic acids (cell division, growth and differentiation) • multisystem disfunction as growth retardation, hypogonadism, ophtalmologic, gastrointestinal, neuropsychiatric symptoms. Zink deficiency in children are marked by poor growth and impairment of sexual development.
Chromium Regulation of glucose metabolism as a component of glucose tolerance factor (GTF). GTF increases effect of insulin (by facilitating its binding to cell receptor site). Chromium regulates plasma lipoprotein concentration. Reduces serum cholesterol and serum triglycerides. Iodine is incorporated into thyroid hormones. Iodine is absorbed in the form of inorganic iodine. Thyreoperoxidase oxidizes inorganic iodine and oxidized I is transported to phenyl group of tyrosin of thyroglobulin.
Fluorine Inorganic matrix of bone and teeth. Deficiency – osteoporosis and teeth caries. Boron Influences of metabolism and use of Ca, Cu, Mn, N, glucose, triglycerides. Control of membranes function and their stabilization. Negative influence on many metabolic processes – inhibition of some key enzymes (inhibition of energetic metabolism), immune system (respiratory burst).
Vanadium Control of sodium pump, inhibition of ATPase Tin Interaction with riboflavin Lithium Control of sodium pump, interference with the lipid metabolism Silicon Structural role in connective tissue, in metabolism of osteogenic cells Nickel Component of enzyme urease
 Jana novotn
Jana novotn Supfate
Supfate Novotn
Novotn Glucogenic amino acid
Glucogenic amino acid Jana novotn
Jana novotn Novotn
Novotn Minor elements
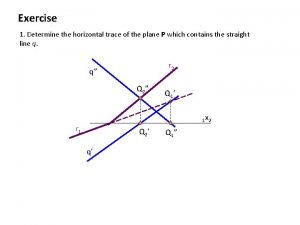
Minor elements Horizontal trace
Horizontal trace Documentary collection vs documentary credit
Documentary collection vs documentary credit Our skin
Our skin Novotn
Novotn Trace elements in seawater
Trace elements in seawater Minerals vs rocks
Minerals vs rocks Why do humans cannot survive without minerals?
Why do humans cannot survive without minerals? Elements are moved between minerals during metamorphism by:
Elements are moved between minerals during metamorphism by: Enzim
Enzim Minerals are inorganic elements that the body
Minerals are inorganic elements that the body What are vitamins functions
What are vitamins functions National outdoor award requirements
National outdoor award requirements Transnet track and trace
Transnet track and trace Listen and read. which sister
Listen and read. which sister Dscsa track and trace
Dscsa track and trace Trace and say
Trace and say Trainable ocr
Trainable ocr Hyundai vgm without login
Hyundai vgm without login Grain track and trace solutions
Grain track and trace solutions Mip track and trace
Mip track and trace Types of rocks song
Types of rocks song Granite and basalt difference
Granite and basalt difference Chapter 8 vitamins and minerals
Chapter 8 vitamins and minerals Difference between rocks and minerals
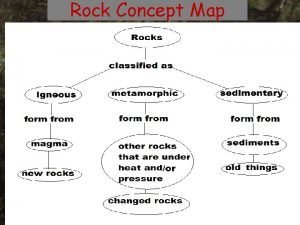
Difference between rocks and minerals Concept map of rock formation
Concept map of rock formation Suzanna socked me sunday poem
Suzanna socked me sunday poem