MEDICAL GRANDROUNDS SUWENDI M D Medicine Resident January








- Slides: 77
MEDICAL GRANDROUNDS SUWENDI, M. D. Medicine Resident January 11, 2007 Ledesma Hall Makati Medical Center
OBJECTIVES To present a case of infection in an immunocompromised host To be able to do a thorough evaluation of an immunocompromised patient with persistent cough To discuss the pathogenesis, clinical manifestations, diagnosis and management of an immunocompromised patient with Aspergillosis
GENERAL DATA Z. C. 47 y/o, female single Filipino business woman
CHIEF COMPLAINT Pancytopenia
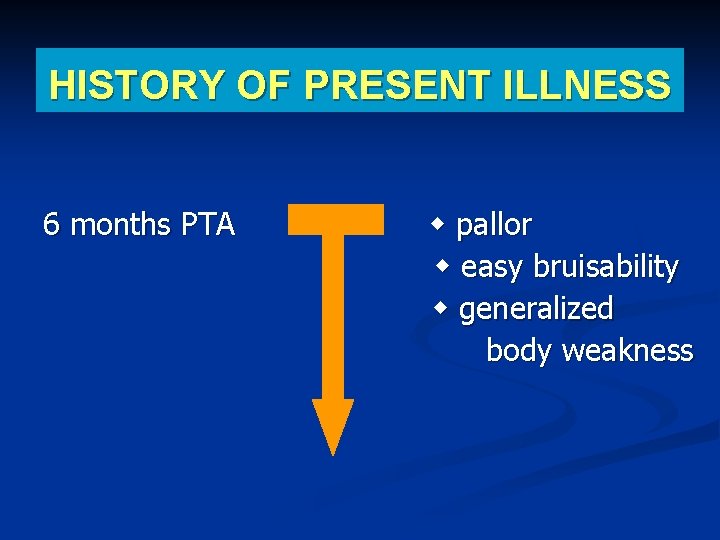
HISTORY OF PRESENT ILLNESS 6 months PTA pallor easy bruisability generalized body weakness
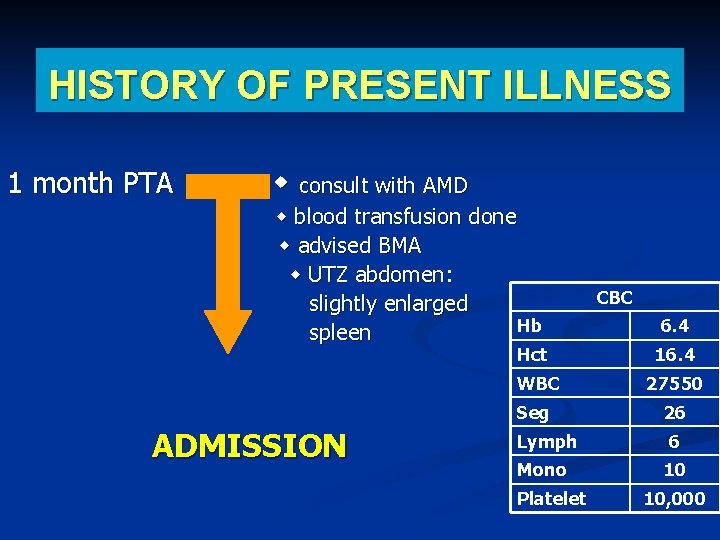
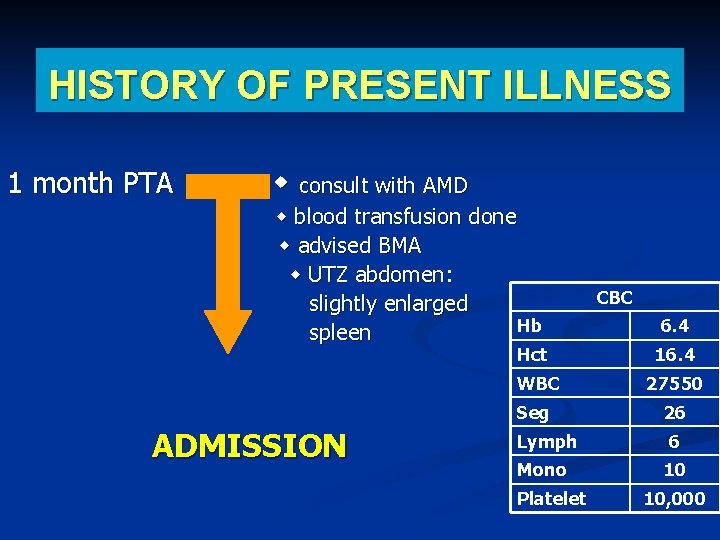
HISTORY OF PRESENT ILLNESS 1 month PTA consult with AMD blood transfusion done advised BMA UTZ abdomen: slightly enlarged Hb spleen Hct ADMISSION CBC 6. 4 16. 4 WBC 27550 Seg 26 Lymph Mono Platelet 6 10 10, 000
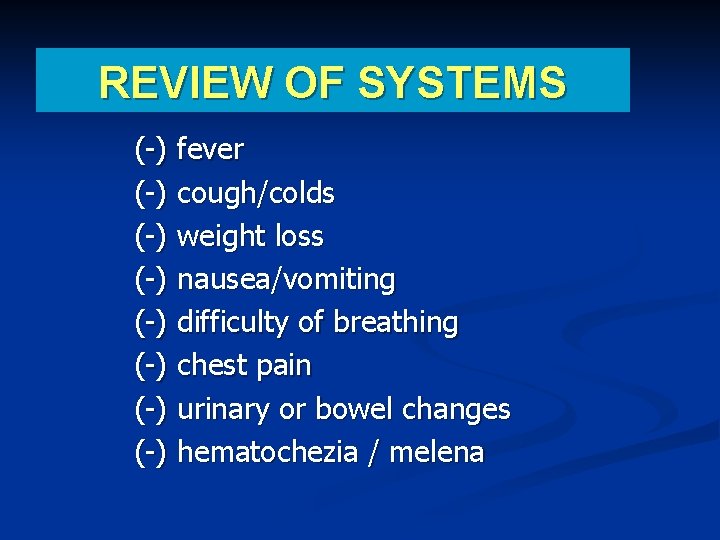
REVIEW OF SYSTEMS (-) fever (-) cough/colds (-) weight loss (-) nausea/vomiting (-) difficulty of breathing (-) chest pain (-) urinary or bowel changes (-) hematochezia / melena
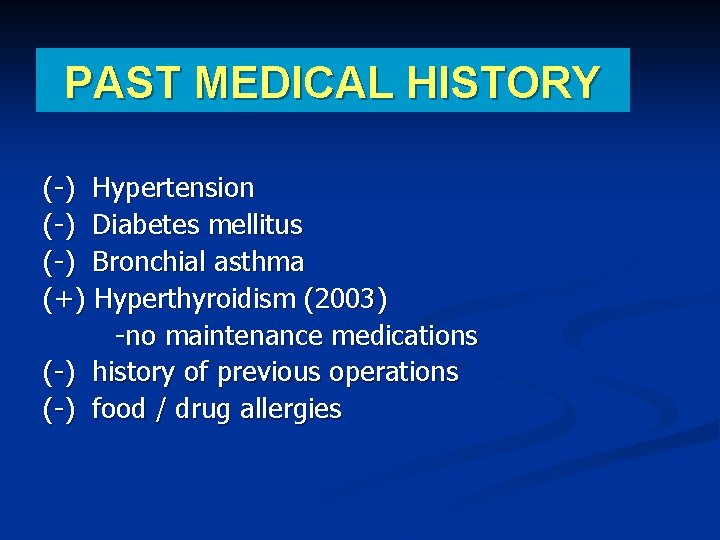
PAST MEDICAL HISTORY (-) Hypertension (-) Diabetes mellitus (-) Bronchial asthma (+) Hyperthyroidism (2003) -no maintenance medications (-) history of previous operations (-) food / drug allergies
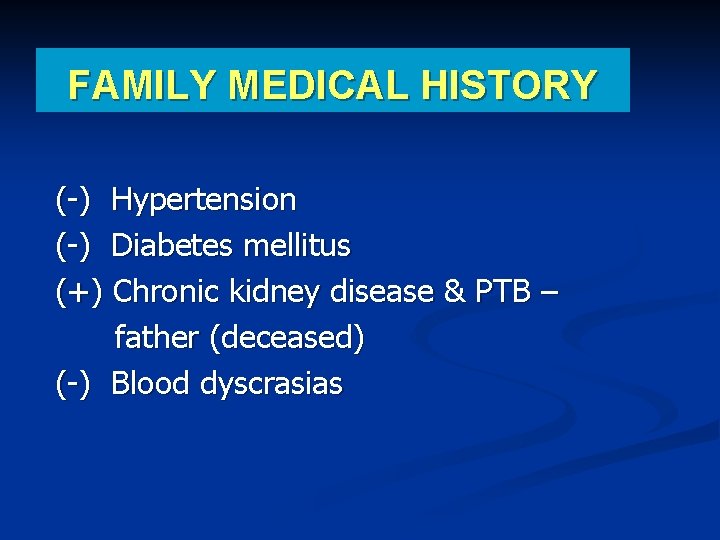
FAMILY MEDICAL HISTORY (-) Hypertension (-) Diabetes mellitus (+) Chronic kidney disease & PTB – father (deceased) (-) Blood dyscrasias
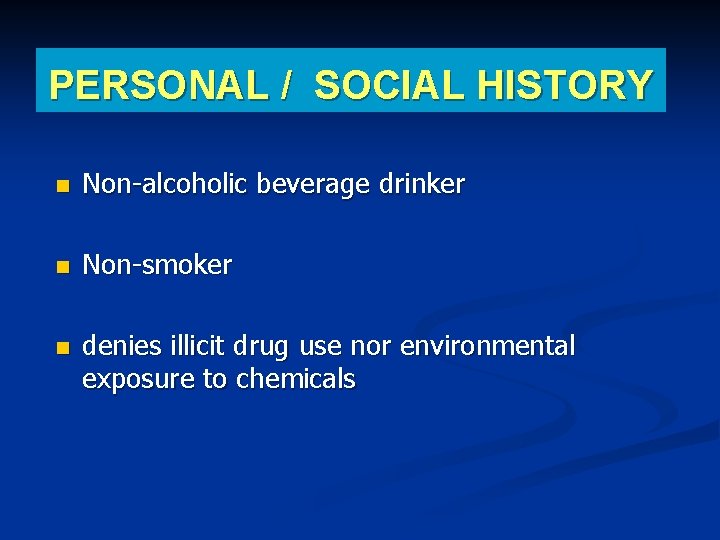
PERSONAL / SOCIAL HISTORY Non-alcoholic beverage drinker Non-smoker denies illicit drug use nor environmental exposure to chemicals
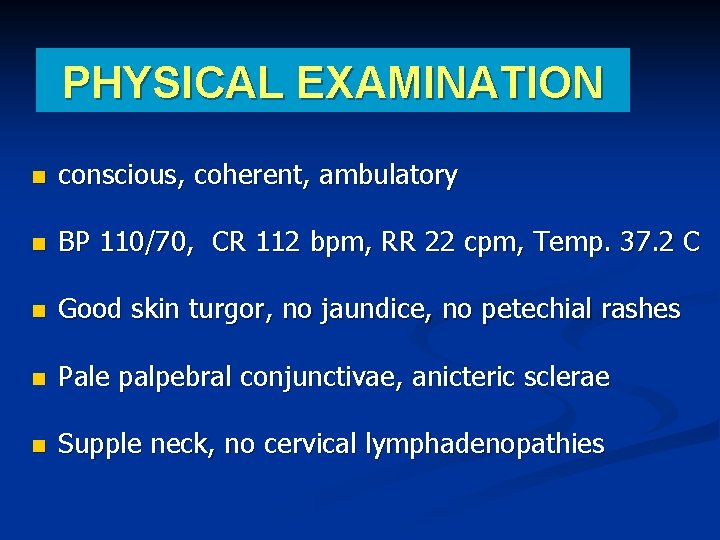
PHYSICAL EXAMINATION conscious, coherent, ambulatory BP 110/70, CR 112 bpm, RR 22 cpm, Temp. 37. 2 C Good skin turgor, no jaundice, no petechial rashes Pale palpebral conjunctivae, anicteric sclerae Supple neck, no cervical lymphadenopathies
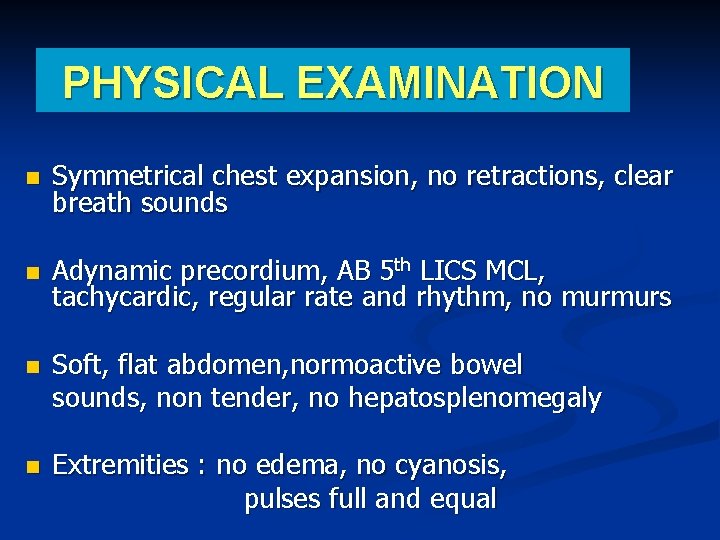
PHYSICAL EXAMINATION Symmetrical chest expansion, no retractions, clear breath sounds Adynamic precordium, AB 5 th LICS MCL, tachycardic, regular rate and rhythm, no murmurs Soft, flat abdomen, normoactive bowel sounds, non tender, no hepatosplenomegaly Extremities : no edema, no cyanosis, pulses full and equal
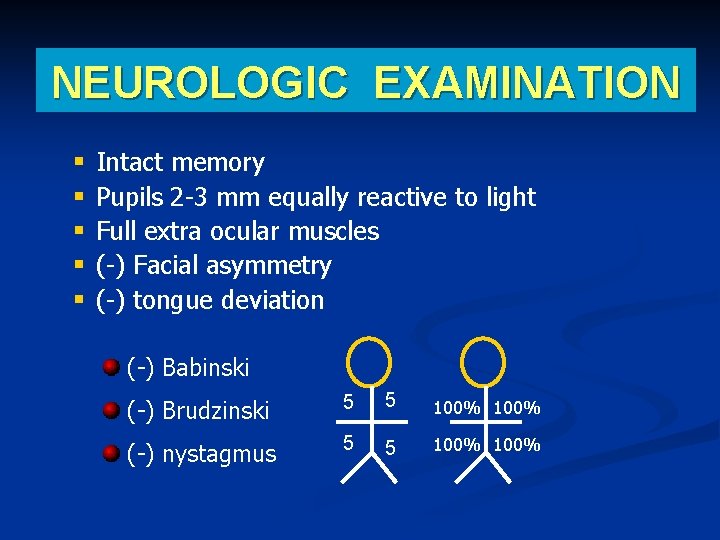
NEUROLOGIC EXAMINATION § § § Intact memory Pupils 2 -3 mm equally reactive to light Full extra ocular muscles (-) Facial asymmetry (-) tongue deviation (-) Babinski (-) Brudzinski 5 5 100% (-) nystagmus 5 5 100%
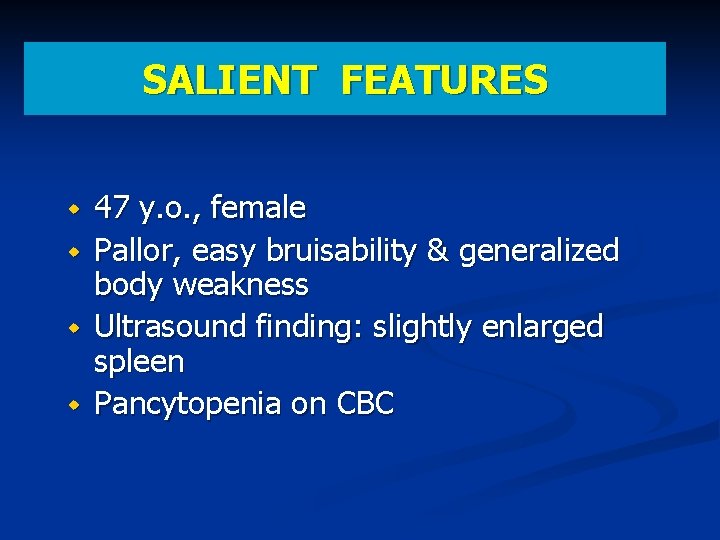
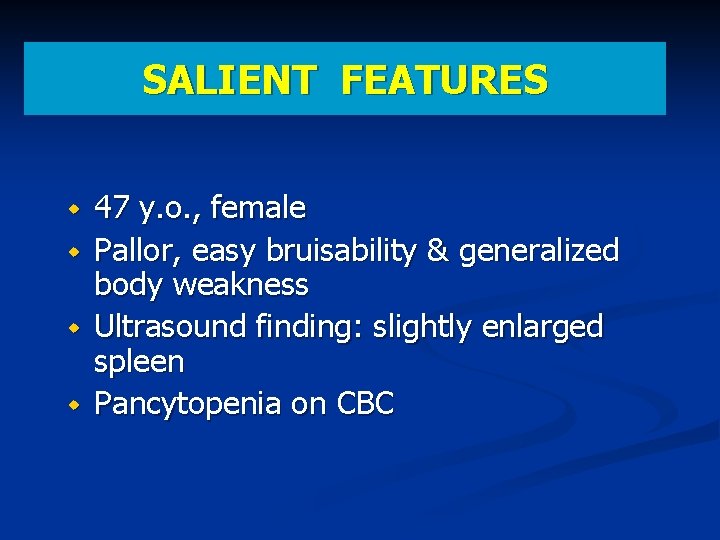
SALIENT FEATURES 47 y. o. , female Pallor, easy bruisability & generalized body weakness Ultrasound finding: slightly enlarged spleen Pancytopenia on CBC
ADMITTING IMPRESSION Pancytopenia R/o blood dyscrasia
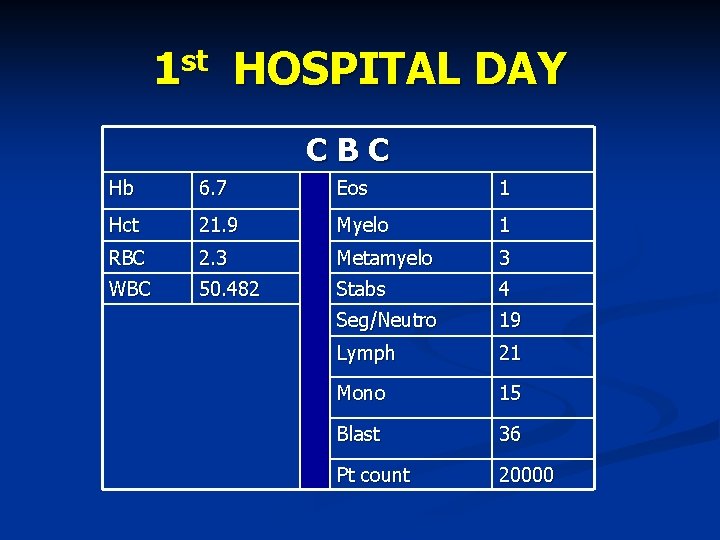
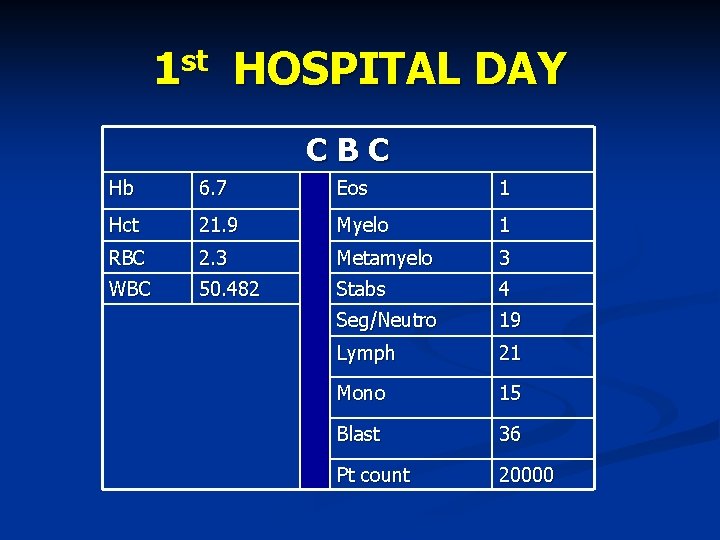
1 st HOSPITAL DAY CBC Hb 6. 7 Eos 1 Hct 21. 9 Myelo 1 RBC 2. 3 Metamyelo 3 WBC 50. 482 Stabs 4 Seg/Neutro 19 Lymph 21 Mono 15 Blast 36 Pt count 20000
1 st HOSPITAL DAY Tranfused 2 unit of PRBC & 4 units of platelet concentrate
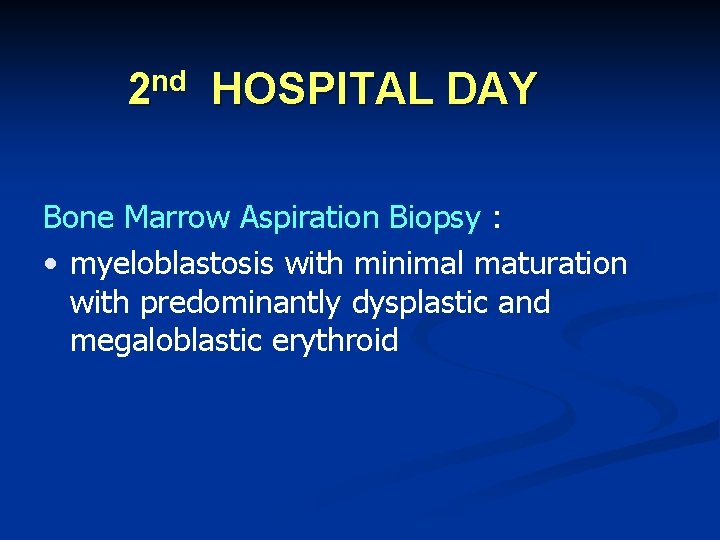
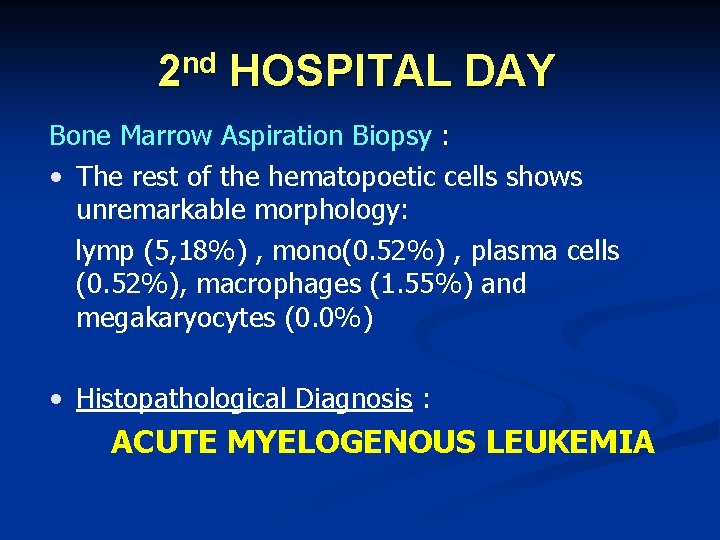
nd 2 HOSPITAL DAY Bone Marrow Aspiration Biopsy : • myeloblastosis with minimal maturation with predominantly dysplastic and megaloblastic erythroid
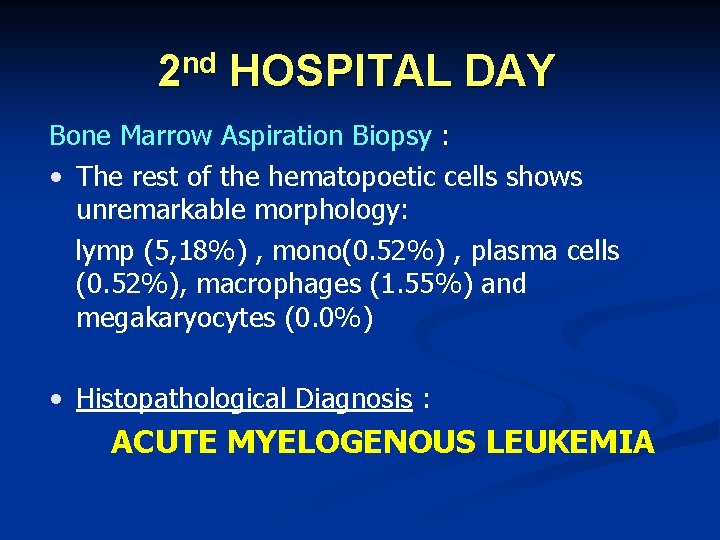
2 nd HOSPITAL DAY Bone Marrow Aspiration Biopsy : • The rest of the hematopoetic cells shows unremarkable morphology: lymp (5, 18%) , mono(0. 52%) , plasma cells (0. 52%), macrophages (1. 55%) and megakaryocytes (0. 0%) • Histopathological Diagnosis : ACUTE MYELOGENOUS LEUKEMIA
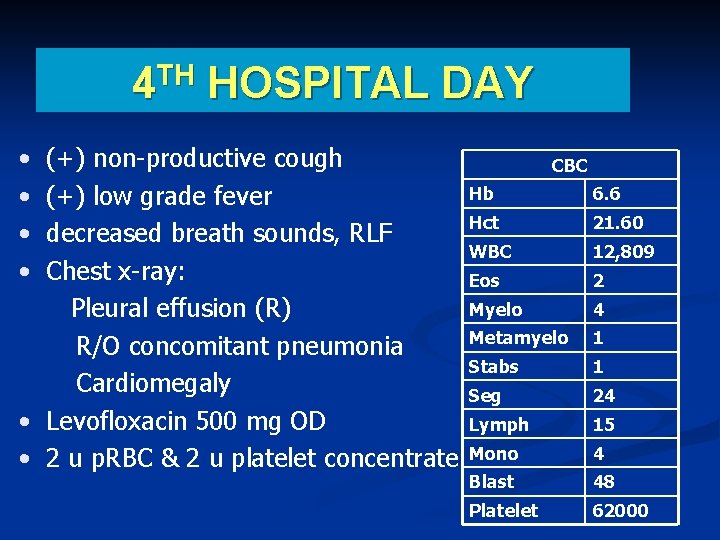
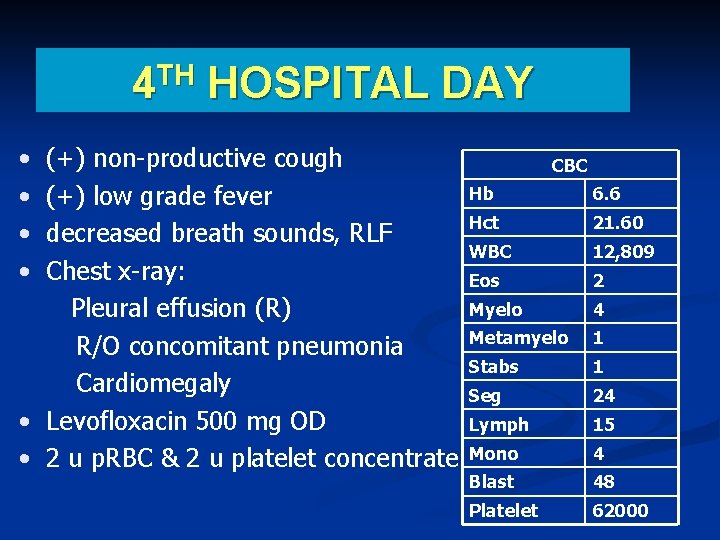
4 TH HOSPITAL DAY • • (+) non-productive cough (+) low grade fever decreased breath sounds, RLF Chest x-ray: Pleural effusion (R) R/O concomitant pneumonia Cardiomegaly • Levofloxacin 500 mg OD • 2 u p. RBC & 2 u platelet concentrate CBC Hb 6. 6 Hct 21. 60 WBC 12, 809 Eos 2 Myelo 4 Metamyelo 1 Stabs 1 Seg 24 Lymph 15 Mono 4 Blast 48 Platelet 62000
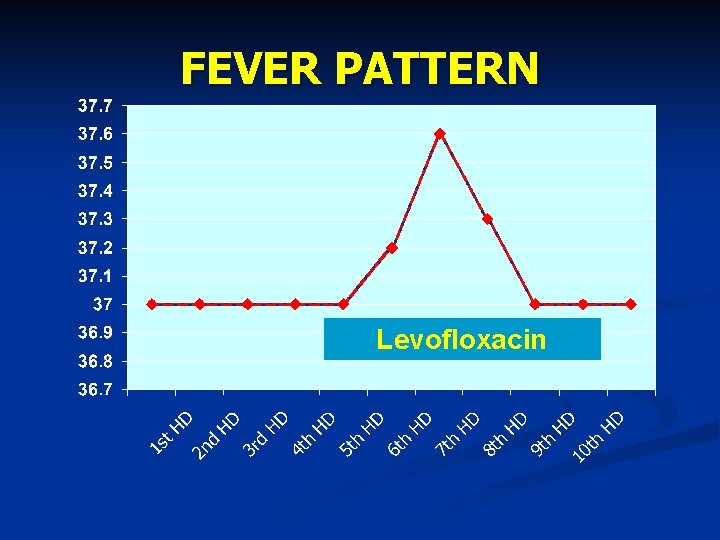
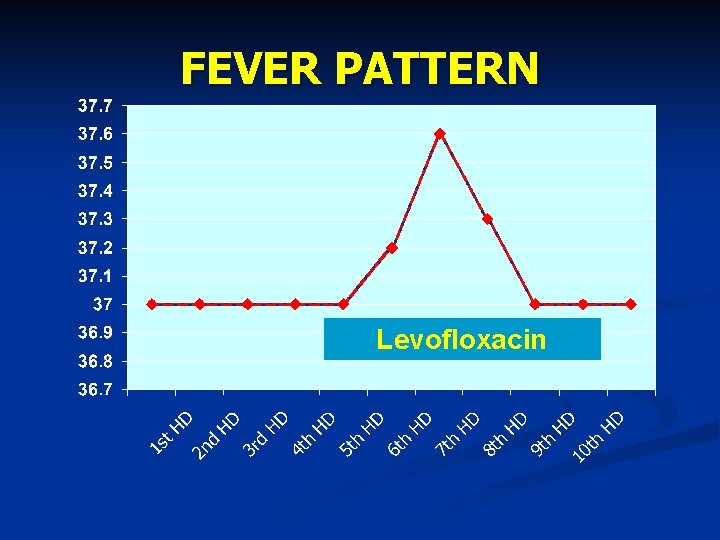
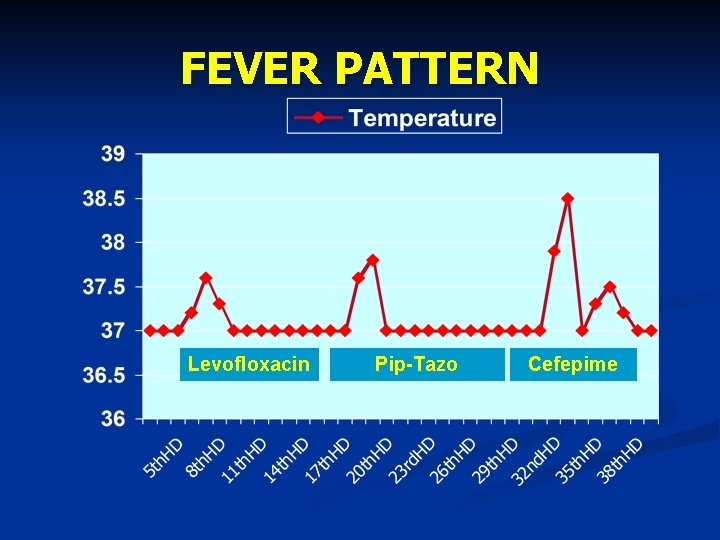
FEVER PATTERN Levofloxacin
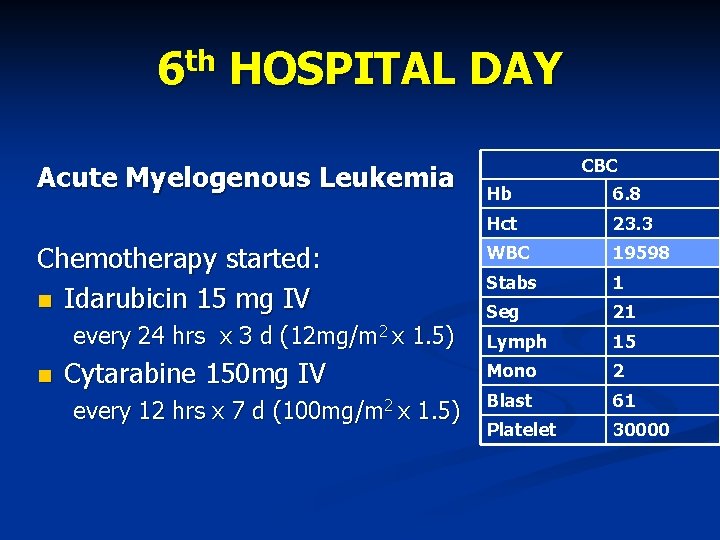
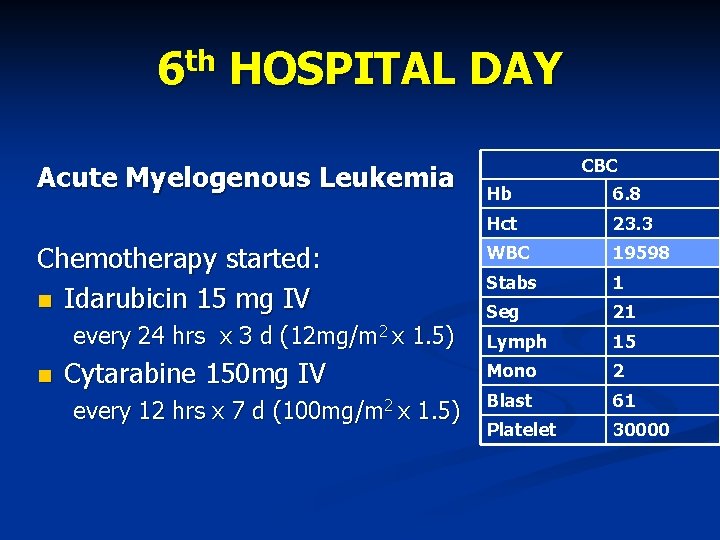
6 th HOSPITAL DAY Acute Myelogenous Leukemia Chemotherapy started: Idarubicin 15 mg IV every 24 hrs x 3 d (12 mg/m 2 x 1. 5) Cytarabine 150 mg IV every 12 hrs x 7 d (100 mg/m 2 x 1. 5) CBC Hb 6. 8 Hct 23. 3 WBC 19598 Stabs 1 Seg 21 Lymph 15 Mono 2 Blast 61 Platelet 30000
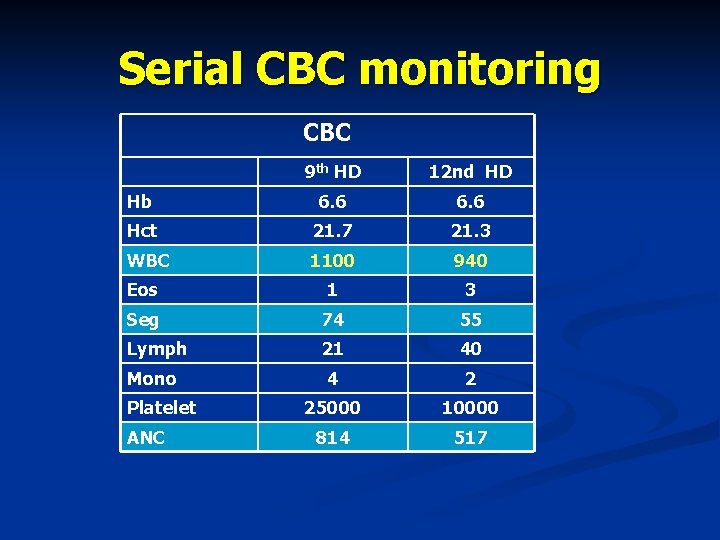
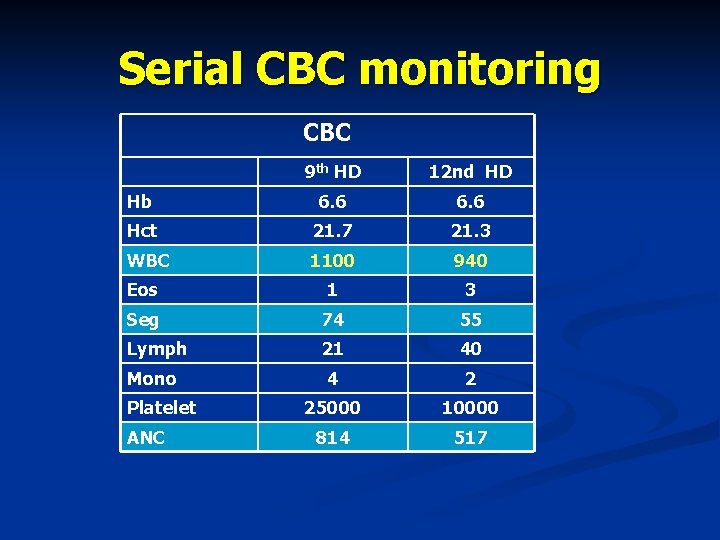
Serial CBC monitoring CBC 9 th HD 12 nd HD Hb 6. 6 Hct 21. 7 21. 3 WBC 1100 940 Eos 1 3 Seg 74 55 Lymph 21 40 4 2 25000 10000 814 517 Mono Platelet ANC
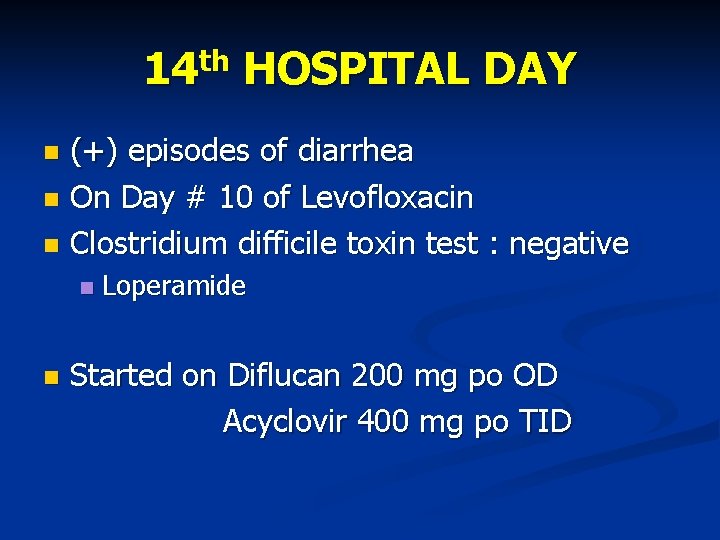
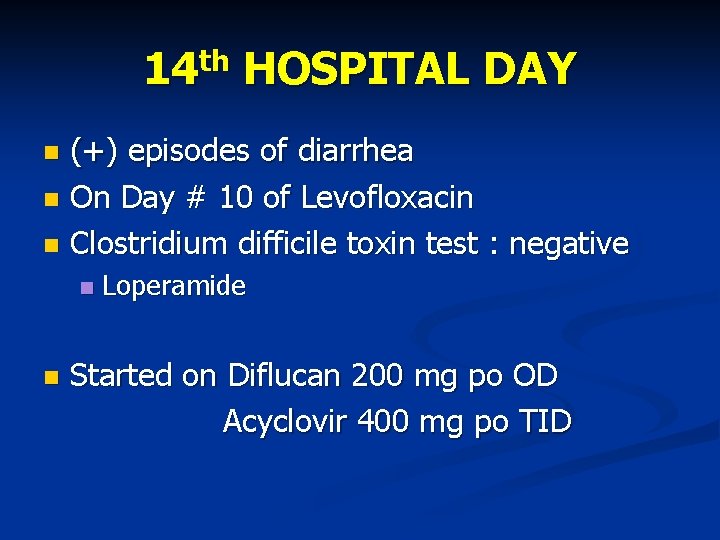
14 th HOSPITAL DAY (+) episodes of diarrhea On Day # 10 of Levofloxacin Clostridium difficile toxin test : negative Loperamide Started on Diflucan 200 mg po OD Acyclovir 400 mg po TID
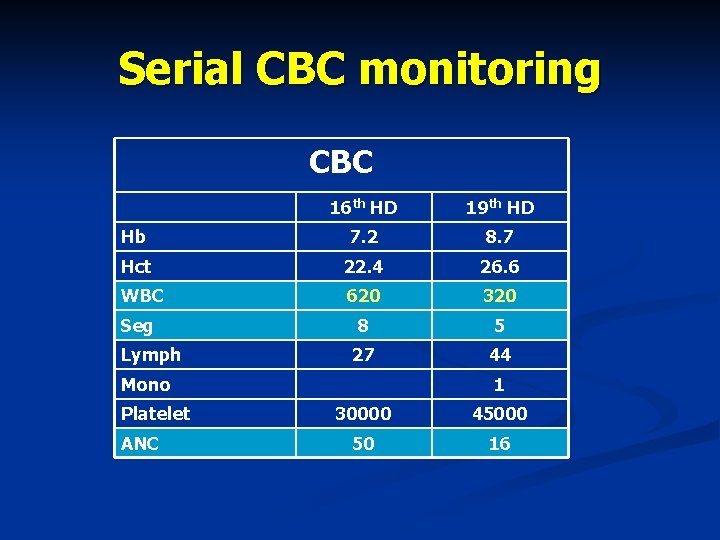
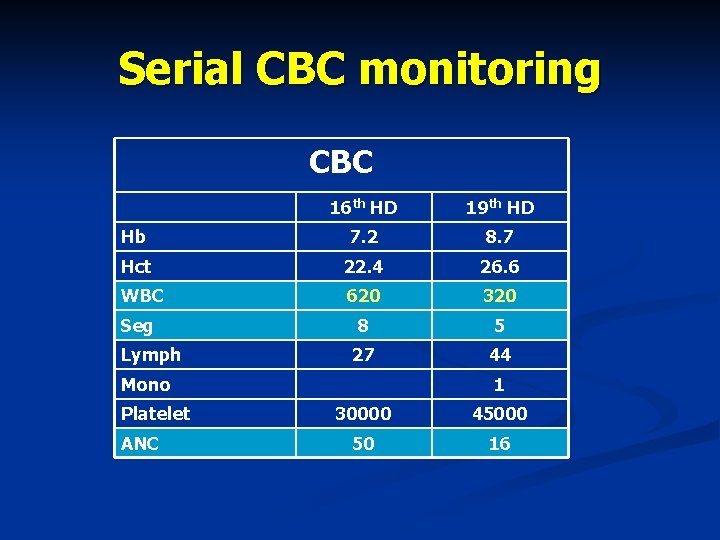
Serial CBC monitoring CBC 16 th HD 19 th HD Hb 7. 2 8. 7 Hct 22. 4 26. 6 WBC 620 320 Seg 8 5 27 44 Lymph Mono Platelet ANC 1 30000 45000 50 16
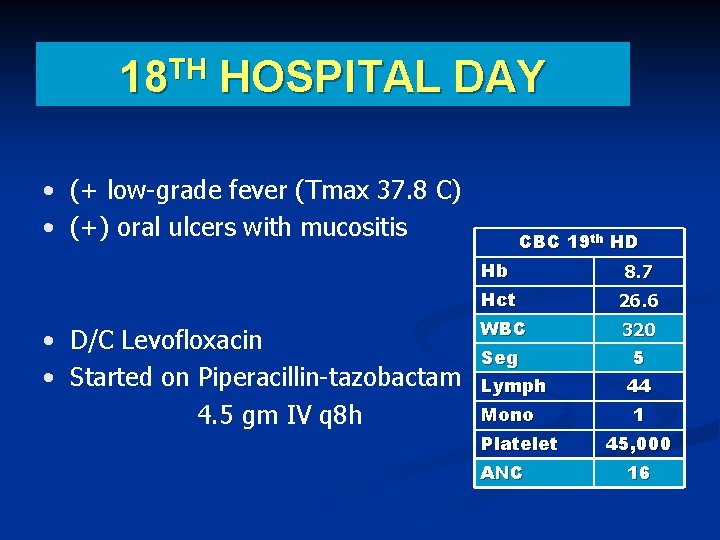
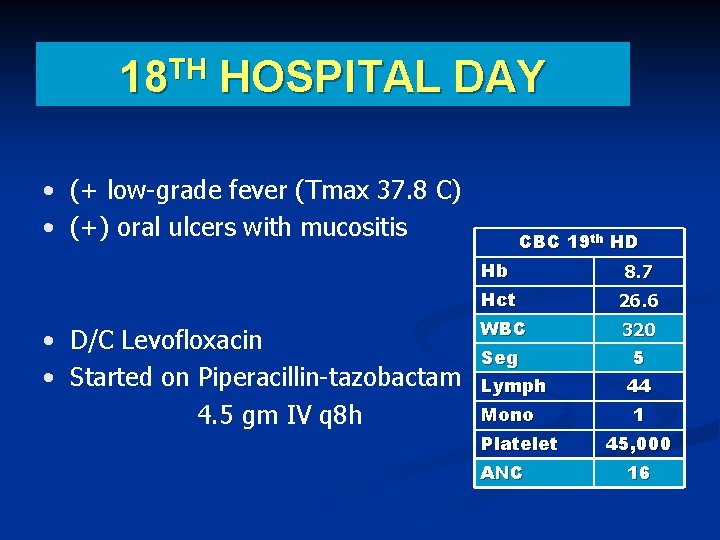
TH 18 HOSPITAL DAY • (+ low-grade fever (Tmax 37. 8 C) • (+) oral ulcers with mucositis • D/C Levofloxacin • Started on Piperacillin-tazobactam 4. 5 gm IV q 8 h CBC 19 th HD Hb 8. 7 Hct 26. 6 WBC Seg 320 5 Lymph 44 Mono Platelet ANC 1 45, 000 16
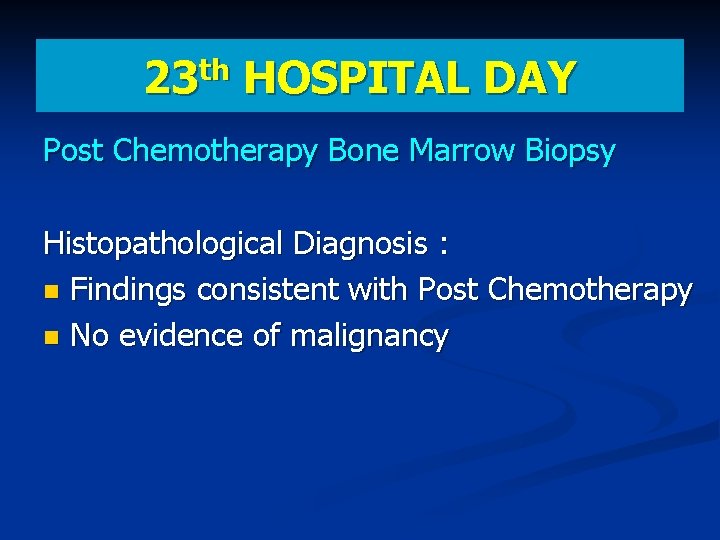
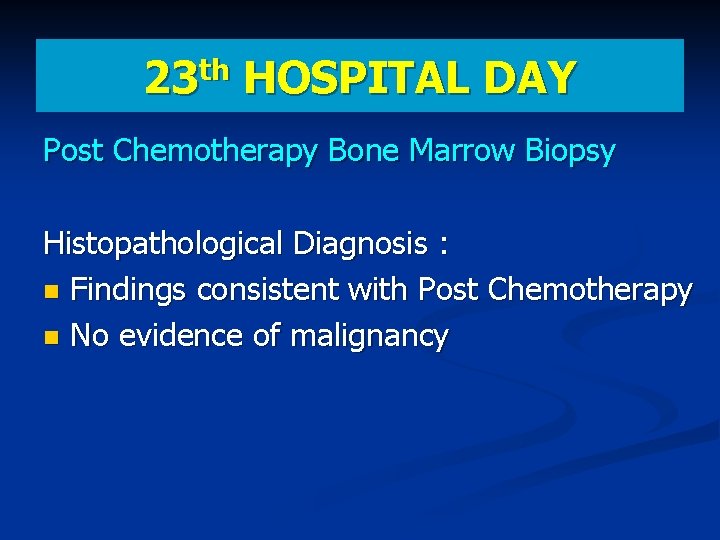
th 23 HOSPITAL DAY Post Chemotherapy Bone Marrow Biopsy Histopathological Diagnosis : Findings consistent with Post Chemotherapy No evidence of malignancy
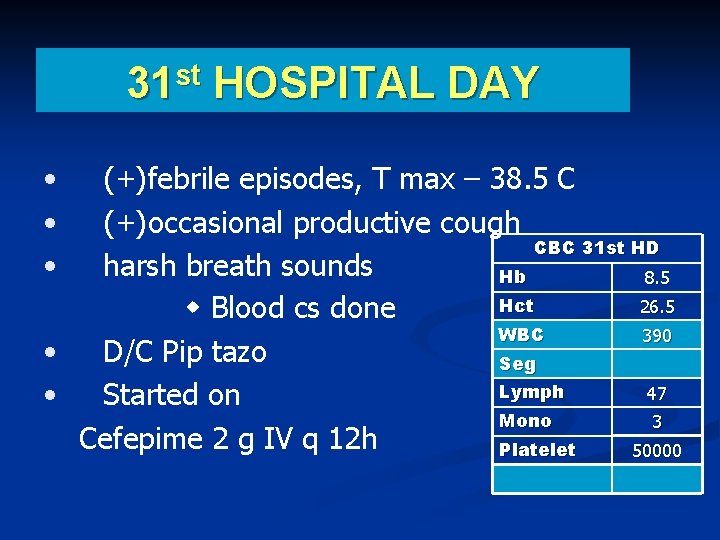
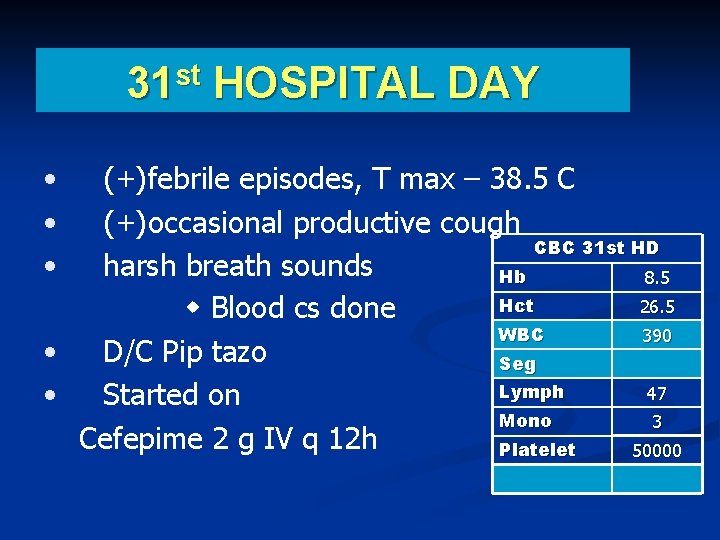
31 st HOSPITAL DAY • • • (+)febrile episodes, T max – 38. 5 C (+)occasional productive cough CBC 31 st HD harsh breath sounds Hb 8. 5 Hct 26. 5 Blood cs done WBC 390 • D/C Pip tazo Seg Lymph 47 • Started on Mono 3 Cefepime 2 g IV q 12 h Platelet 50000
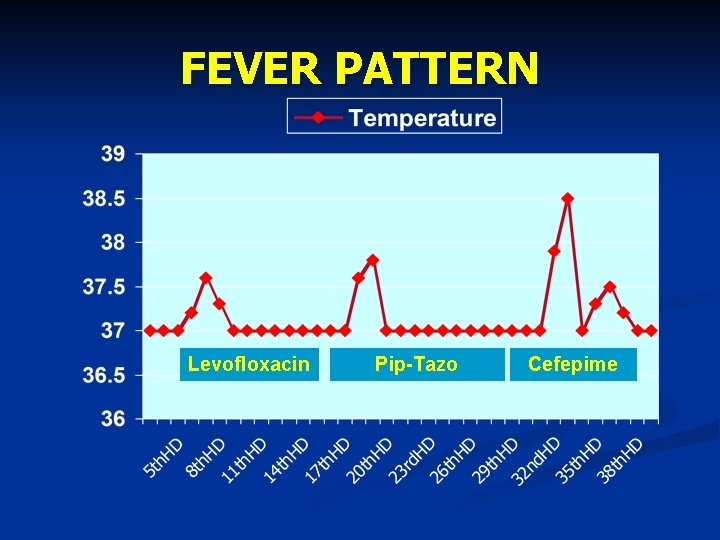
FEVER PATTERN Levofloxacin Pip-Tazo Cefepime
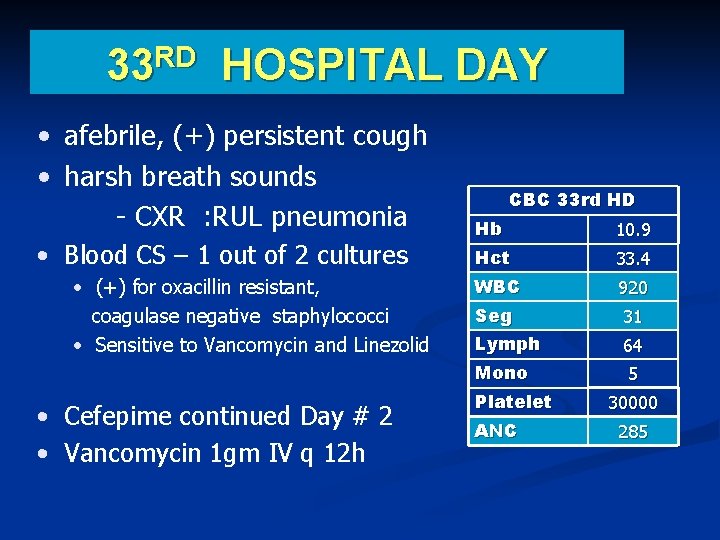
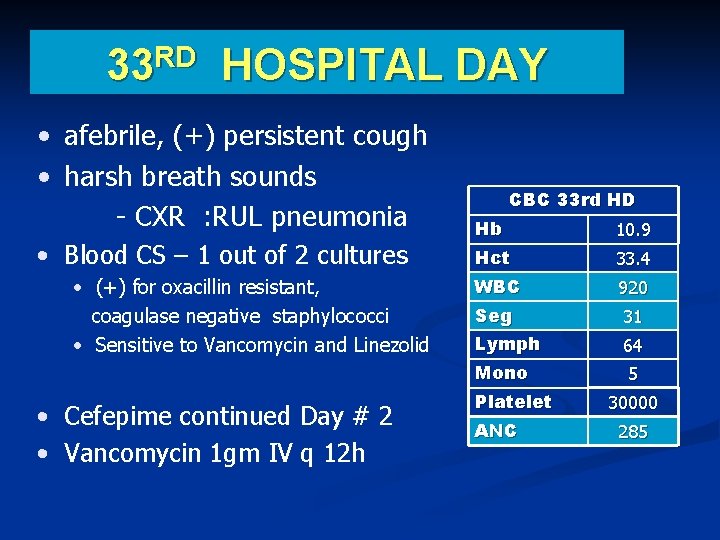
RD 33 HOSPITAL DAY • afebrile, (+) persistent cough • harsh breath sounds - CXR : RUL pneumonia • Blood CS – 1 out of 2 cultures • (+) for oxacillin resistant, coagulase negative staphylococci • Sensitive to Vancomycin and Linezolid • Cefepime continued Day # 2 • Vancomycin 1 gm IV q 12 h CBC 33 rd HD Hb 10. 9 Hct 33. 4 WBC 920 Seg 31 Lymph 64 Mono 5 Platelet ANC 30000 285
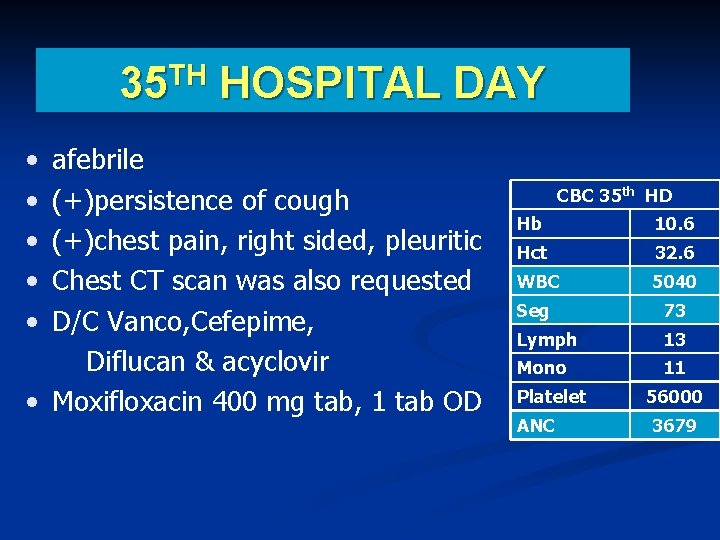
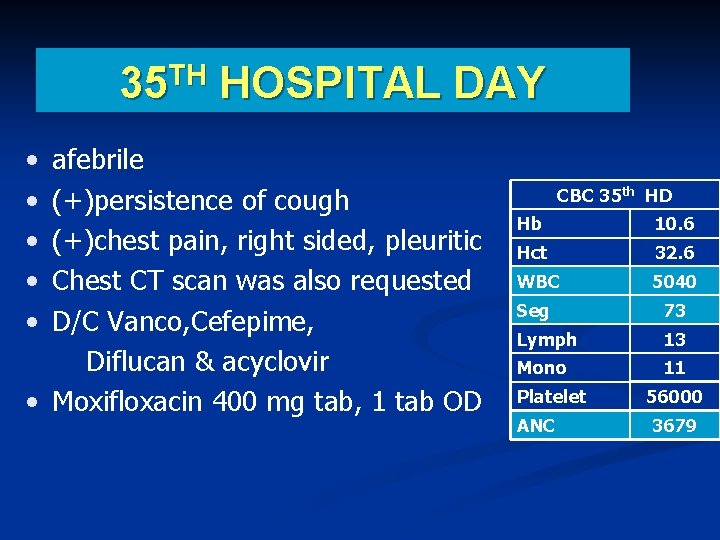
35 TH HOSPITAL DAY • • • afebrile (+)persistence of cough (+)chest pain, right sided, pleuritic Chest CT scan was also requested D/C Vanco, Cefepime, Diflucan & acyclovir • Moxifloxacin 400 mg tab, 1 tab OD CBC 35 th HD Hb 10. 6 Hct 32. 6 WBC 5040 Seg 73 Lymph 13 Mono 11 Platelet ANC 56000 3679
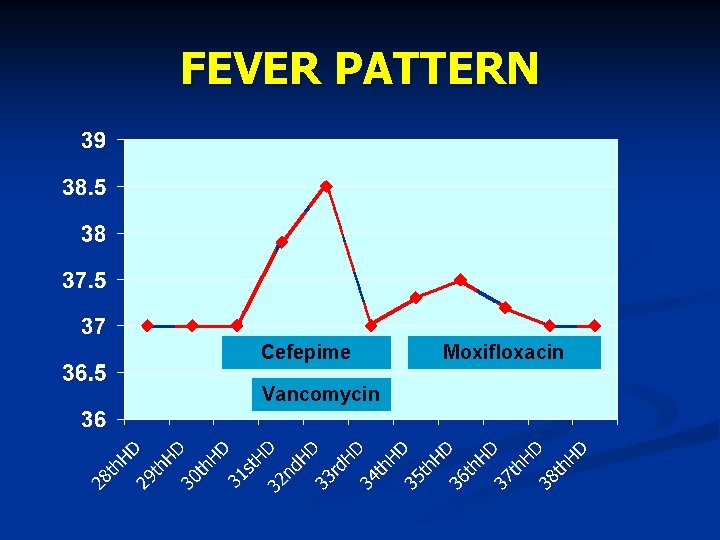
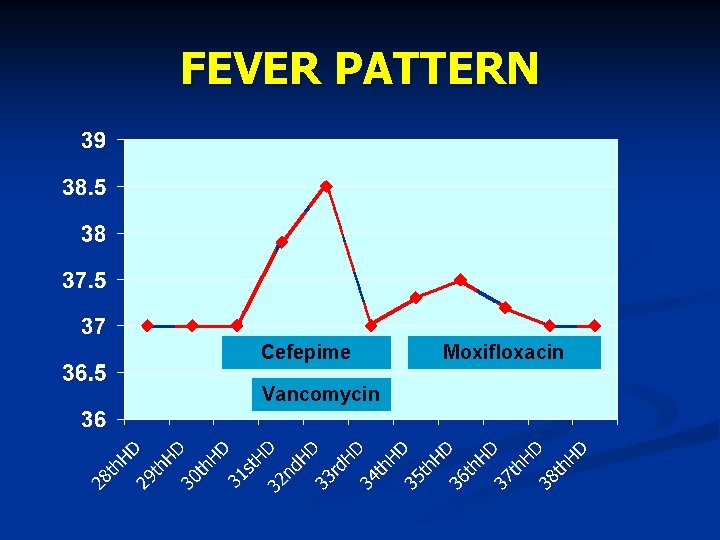
FEVER PATTERN Cefepime Vancomycin Moxifloxacin
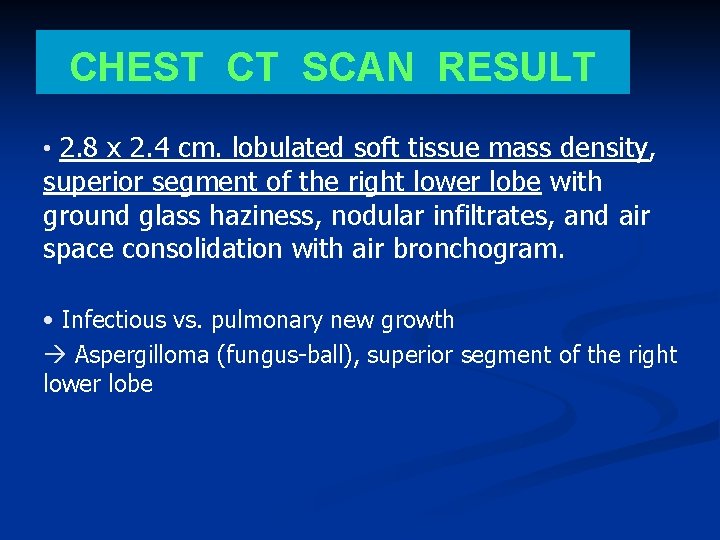
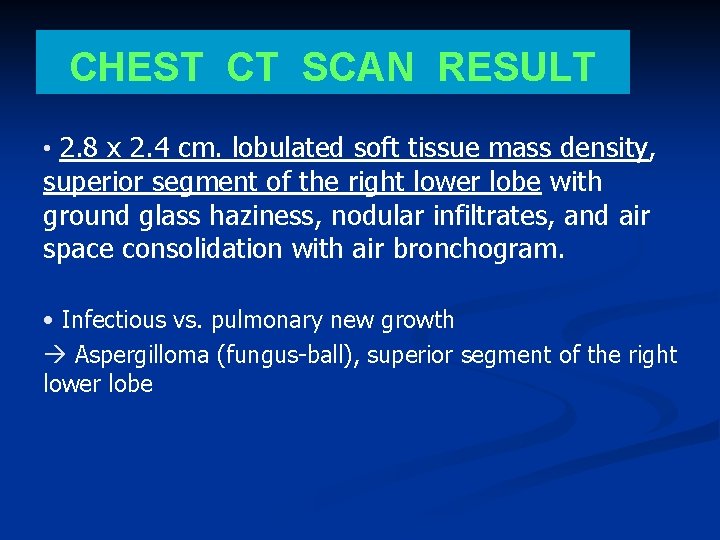
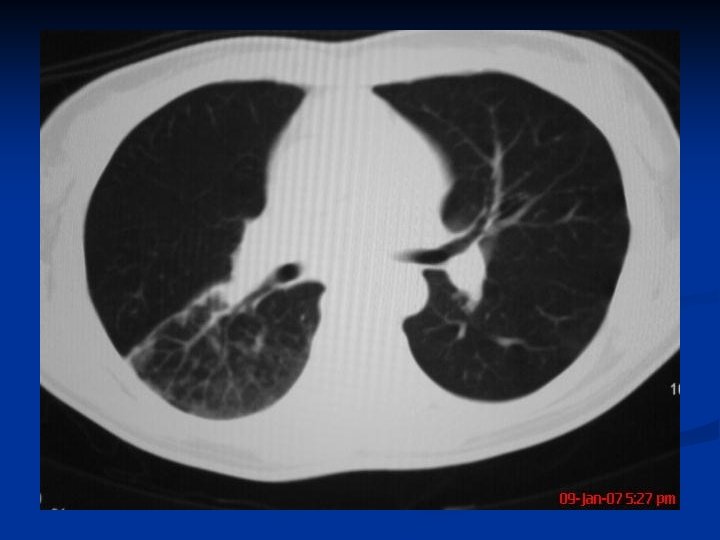
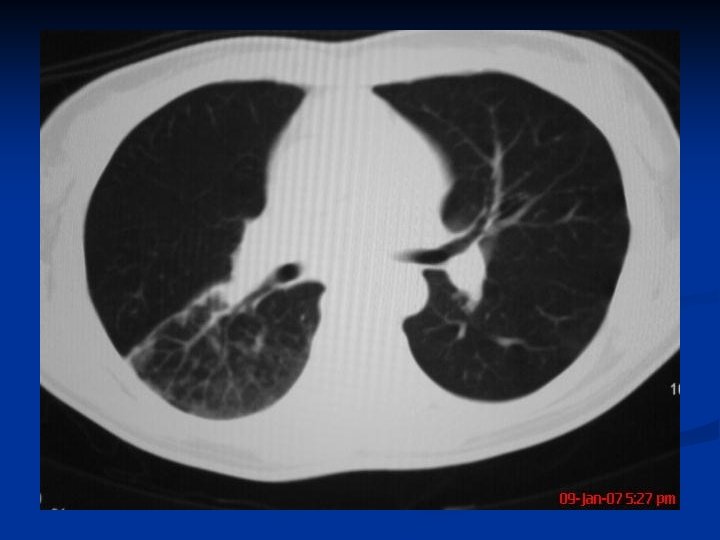
CHEST CT SCAN RESULT • 2. 8 x 2. 4 cm. lobulated soft tissue mass density, superior segment of the right lower lobe with ground glass haziness, nodular infiltrates, and air space consolidation with air bronchogram. • Infectious vs. pulmonary new growth à Aspergilloma (fungus-ball), superior segment of the right lower lobe



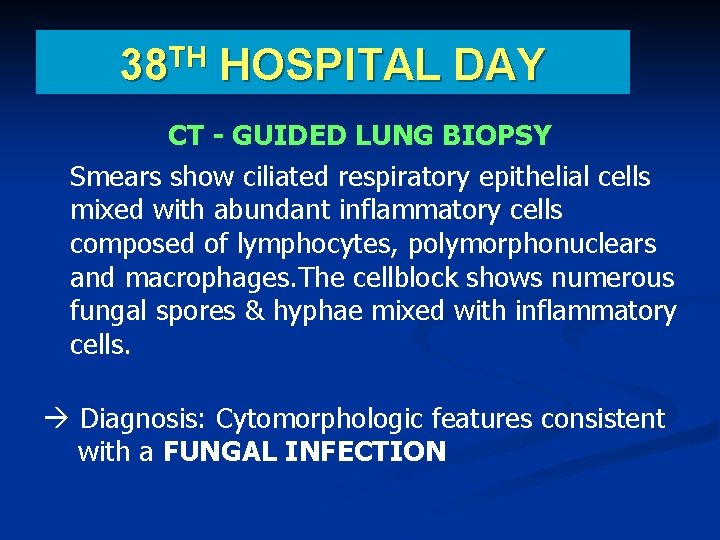
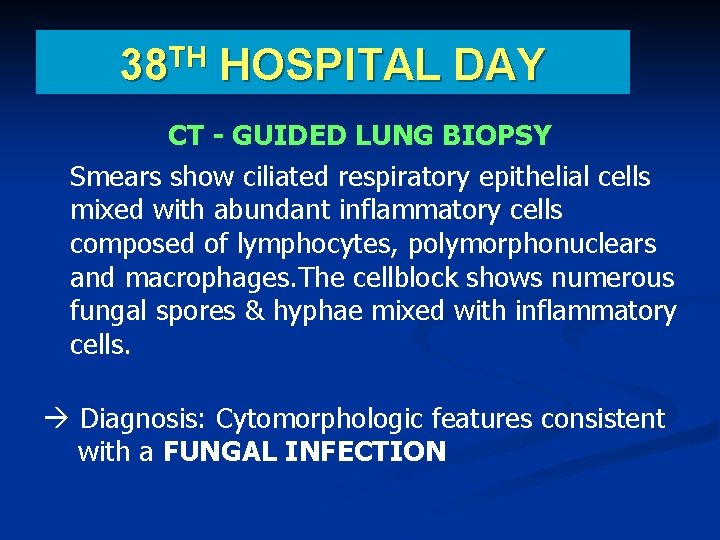
TH 38 HOSPITAL DAY CT - GUIDED LUNG BIOPSY Smears show ciliated respiratory epithelial cells mixed with abundant inflammatory cells composed of lymphocytes, polymorphonuclears and macrophages. The cellblock shows numerous fungal spores & hyphae mixed with inflammatory cells. à Diagnosis: Cytomorphologic features consistent with a FUNGAL INFECTION
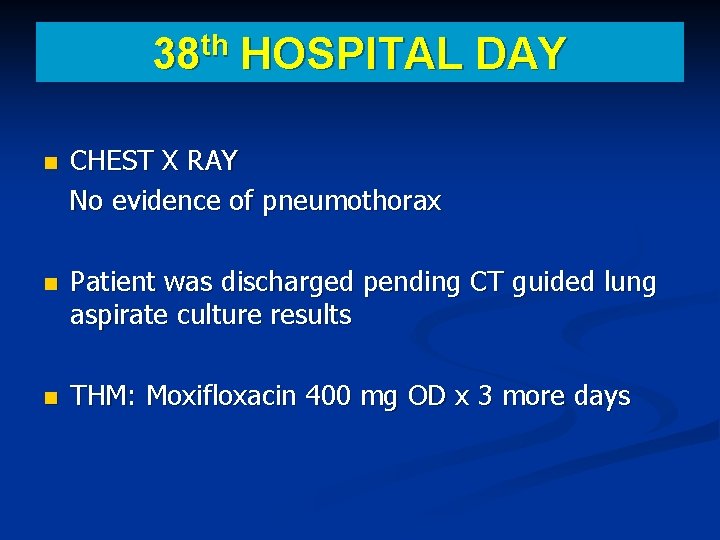
th 38 HOSPITAL DAY CHEST X RAY No evidence of pneumothorax Patient was discharged pending CT guided lung aspirate culture results THM: Moxifloxacin 400 mg OD x 3 more days
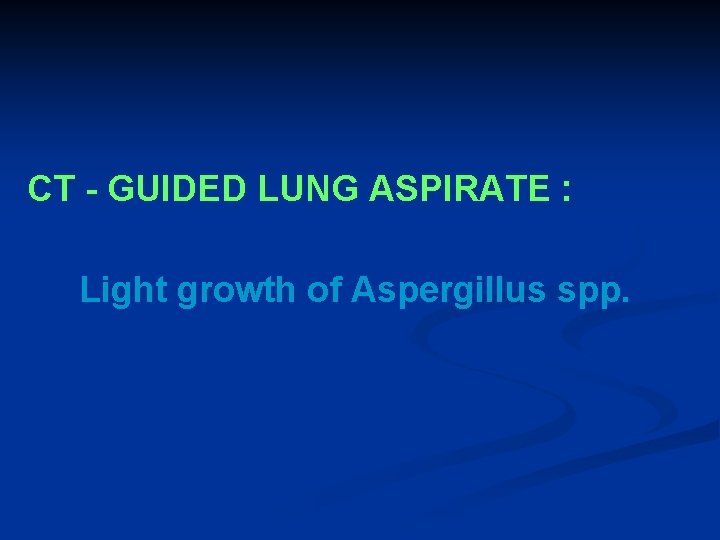
CT - GUIDED LUNG ASPIRATE : Light growth of Aspergillus spp.
FOLLOW UP TREATMENT Patient was started on Voriconazole 200 mg BID
FOLLOW UP CT SCAN


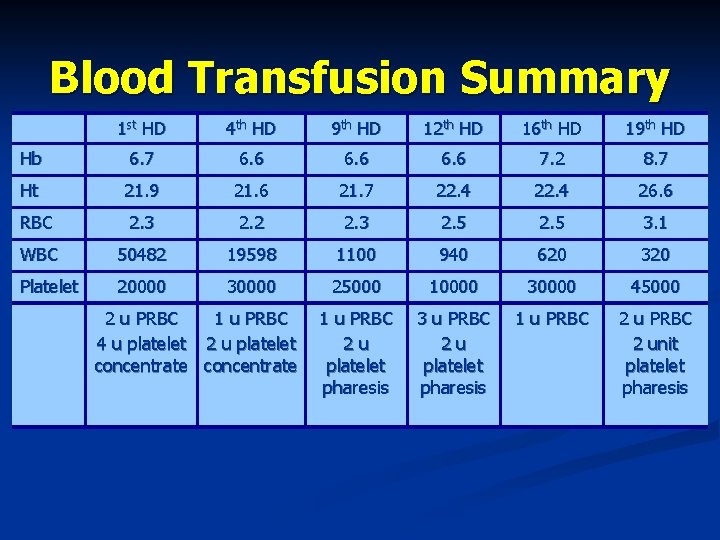
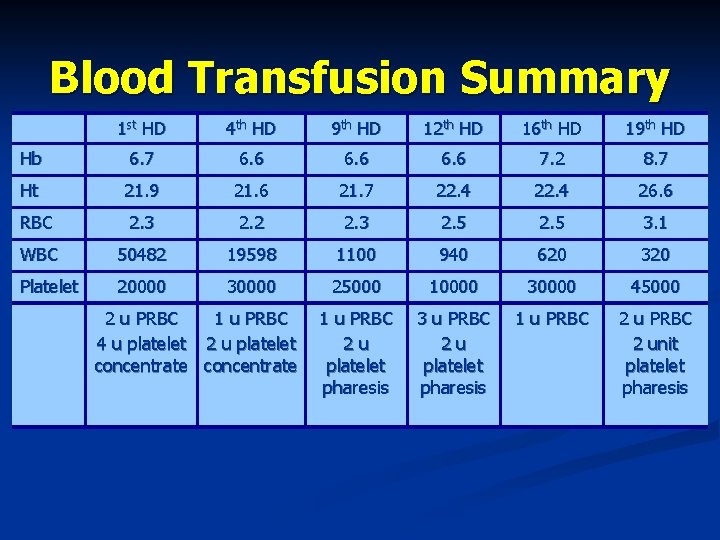
Blood Transfusion Summary 1 st HD 4 th HD 9 th HD 12 th HD 16 th HD 19 th HD Hb 6. 7 6. 6 7. 2 8. 7 Ht 21. 9 21. 6 21. 7 22. 4 26. 6 RBC 2. 3 2. 2 2. 3 2. 5 3. 1 WBC 50482 19598 1100 940 620 320 Platelet 20000 30000 25000 10000 30000 45000 1 u PRBC 2 u platelet pharesis 3 u PRBC 2 u platelet pharesis 1 u PRBC 2 unit platelet pharesis 2 u PRBC 1 u PRBC 4 u platelet 2 u platelet concentrate
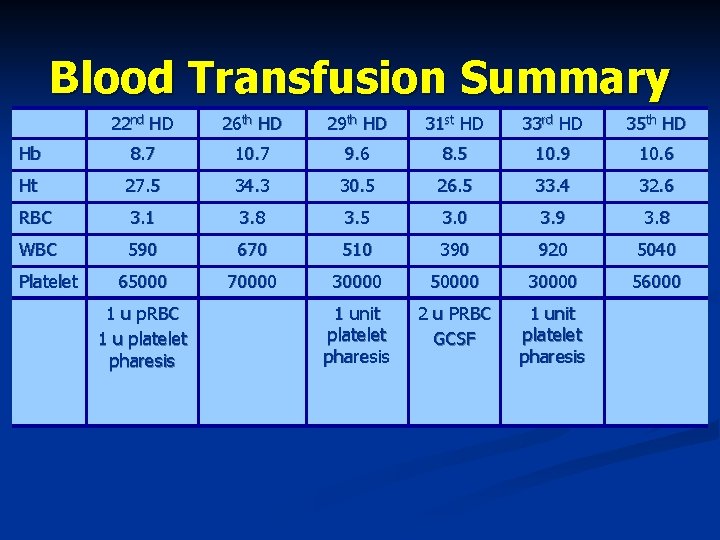
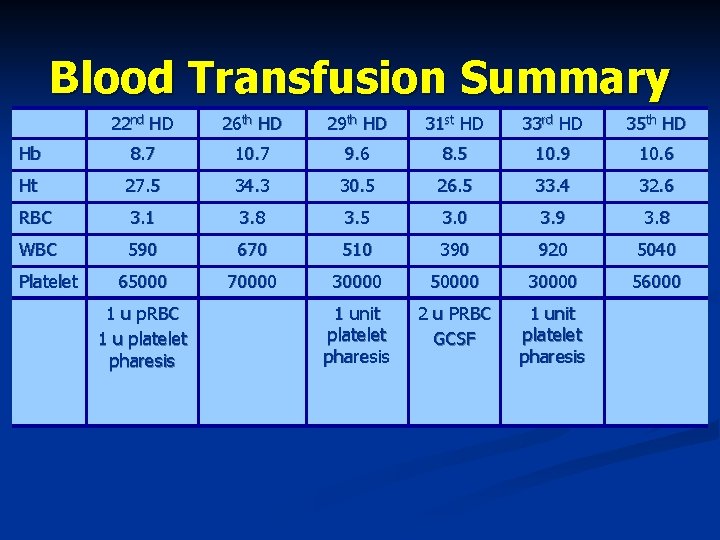
Blood Transfusion Summary 22 nd HD 26 th HD 29 th HD 31 st HD 33 rd HD 35 th HD Hb 8. 7 10. 7 9. 6 8. 5 10. 9 10. 6 Ht 27. 5 34. 3 30. 5 26. 5 33. 4 32. 6 RBC 3. 1 3. 8 3. 5 3. 0 3. 9 3. 8 WBC 590 670 510 390 920 5040 65000 70000 30000 56000 1 unit platelet pharesis 2 u PRBC GCSF 1 unit platelet pharesis Platelet 1 u p. RBC 1 u platelet pharesis

DISCUSSION
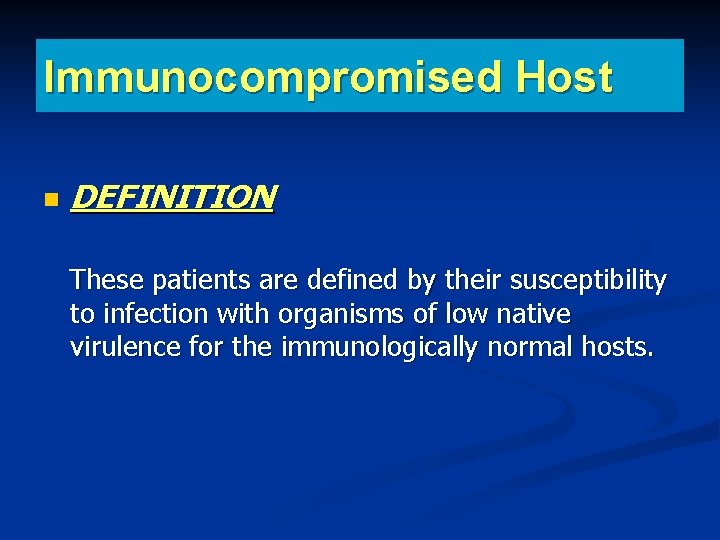
Immunocompromised Host DEFINITION These patients are defined by their susceptibility to infection with organisms of low native virulence for the immunologically normal hosts.
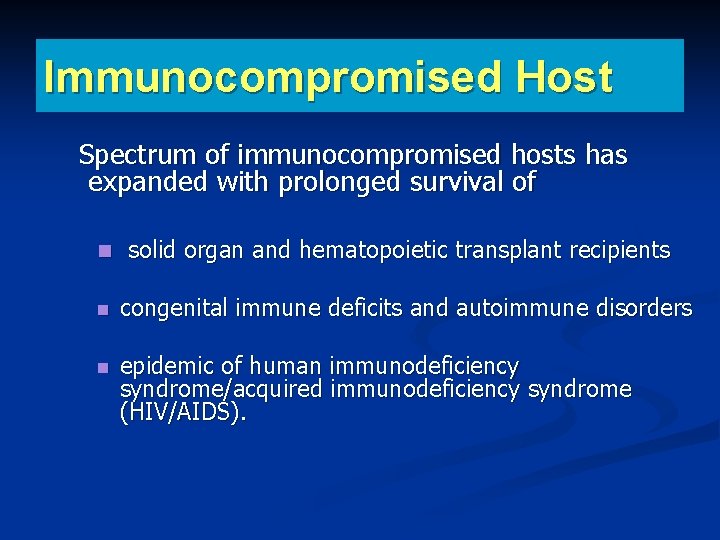
Immunocompromised Host Spectrum of immunocompromised hosts has expanded with prolonged survival of solid organ and hematopoietic transplant recipients congenital immune deficits and autoimmune disorders epidemic of human immunodeficiency syndrome/acquired immunodeficiency syndrome (HIV/AIDS).
Immunocompromised Host RISK FACTOR: Immunosuppressive therapies create a diverse set of immune deficits that create the substrate for opportunistic infections.
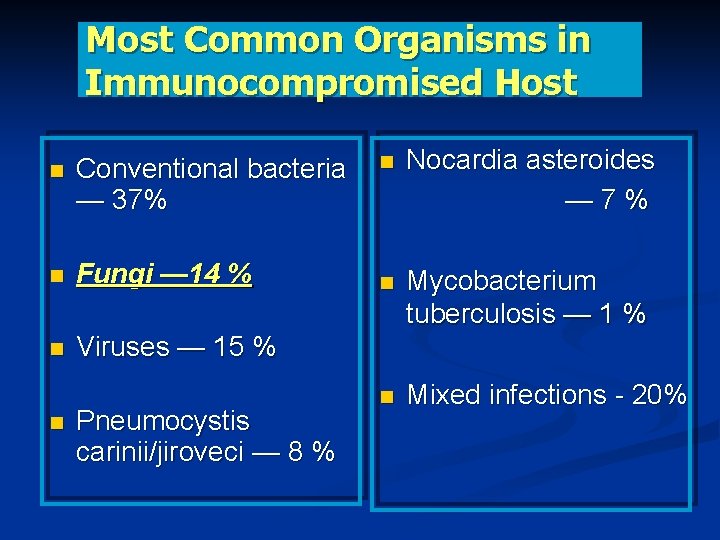
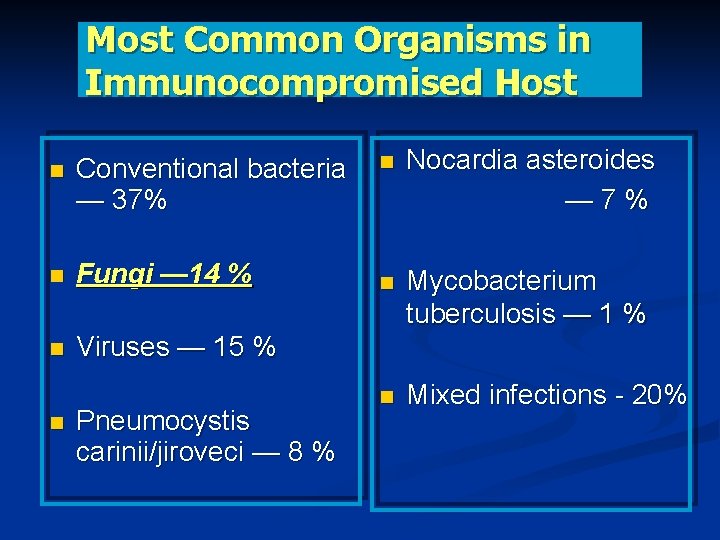
Most Common Organisms in Immunocompromised Host Conventional bacteria — 37% Fungi — 14 % Viruses — 15 % Pneumocystis carinii/jiroveci — 8 % Nocardia asteroides — 7% Mycobacterium tuberculosis — 1 % Mixed infections - 20%
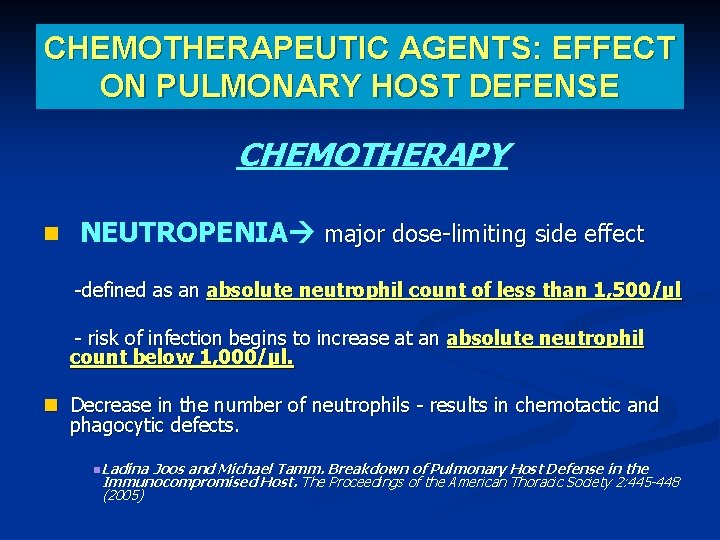
CHEMOTHERAPEUTIC AGENTS: EFFECT ON PULMONARY HOST DEFENSE CHEMOTHERAPY NEUTROPENIA major dose-limiting side effect -defined as an absolute neutrophil count of less than 1, 500/µl - risk of infection begins to increase at an absolute neutrophil count below 1, 000/µl. Decrease in the number of neutrophils - results in chemotactic and phagocytic defects. Ladina Joos and Michael Tamm. Breakdown of Pulmonary Host Defense in the Immunocompromised Host. The Proceedings of the American Thoracic Society 2: 445 -448 (2005)
CHEMOTHERAPEUTIC AGENTS: EFFECT ON PULMONARY HOST DEFENSE Pulmonary infiltrates emerge in 15 to 25% of patients with profound neutropenia after chemotherapy.
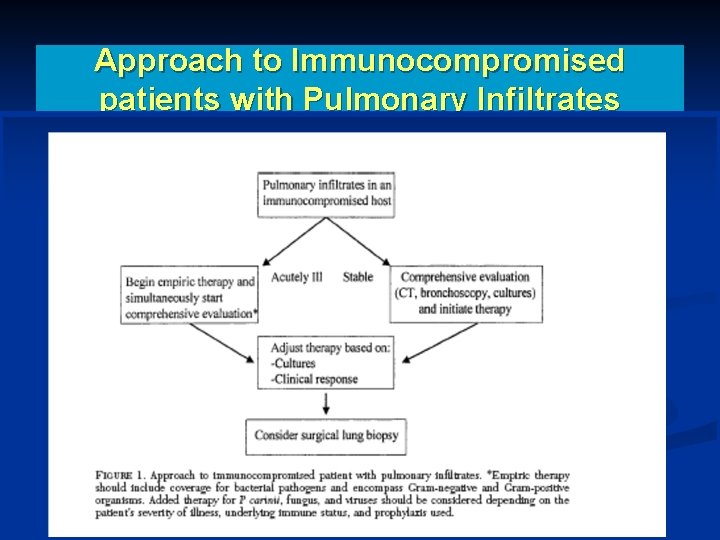
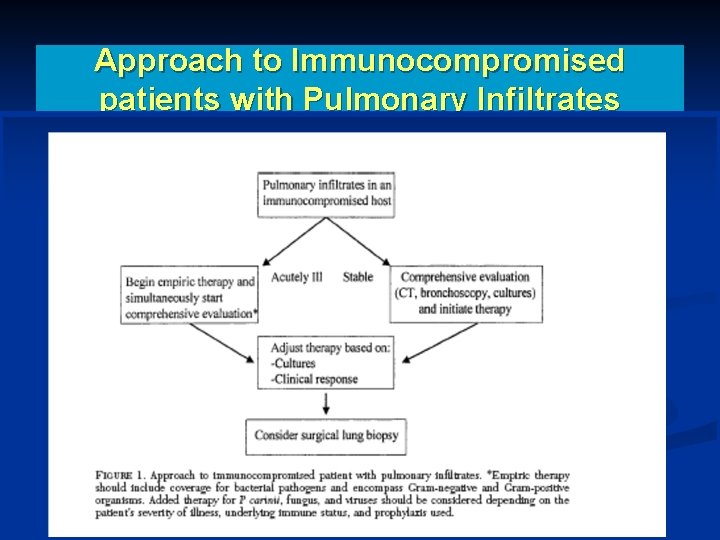
Approach to Immunocompromised patients with Pulmonary Infiltrates
Pulmonary Fungal Infections a major problem in neutropenic patients usually angioinvasive pulmonary aspergillosis develop in patients with hematologic malignancies after high-dose chemotherapy The risk of developing invasive pulmonary aspergillosis is directly related to the duration of the neutropenic phase. Ladina Joos and Michael Tamm. Breakdown of Pulmonary Host Defense in the Immunocompromised Host. The Proceedings of the American Thoracic Society 2: 445448 (2005)
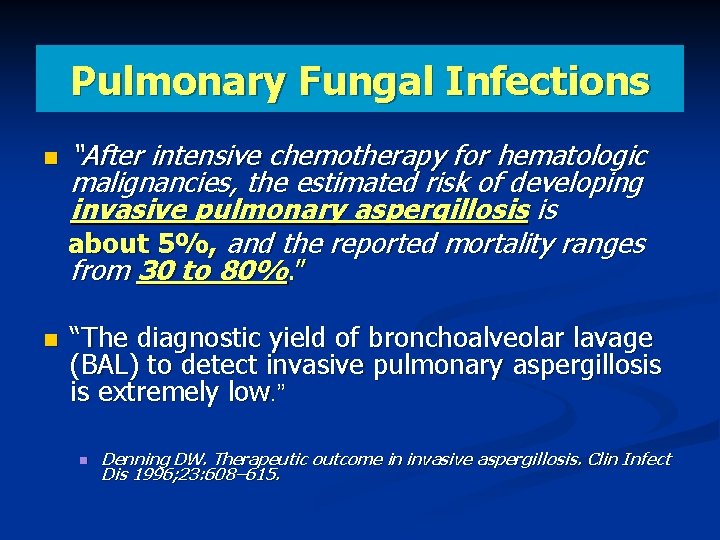
Pulmonary Fungal Infections “After intensive chemotherapy for hematologic malignancies, the estimated risk of developing invasive pulmonary aspergillosis is about 5%, and the reported mortality ranges from 30 to 80%. ” “The diagnostic yield of bronchoalveolar lavage (BAL) to detect invasive pulmonary aspergillosis is extremely low. ” Denning DW. Therapeutic outcome in invasive aspergillosis. Clin Infect Dis 1996; 23: 608– 615.
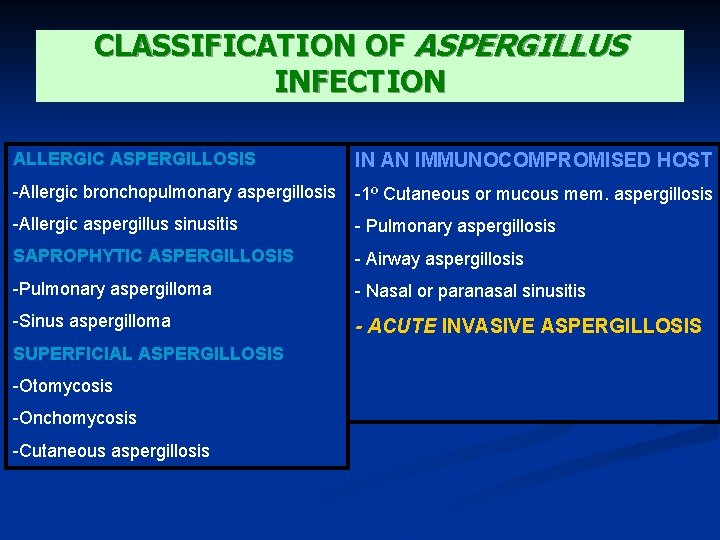
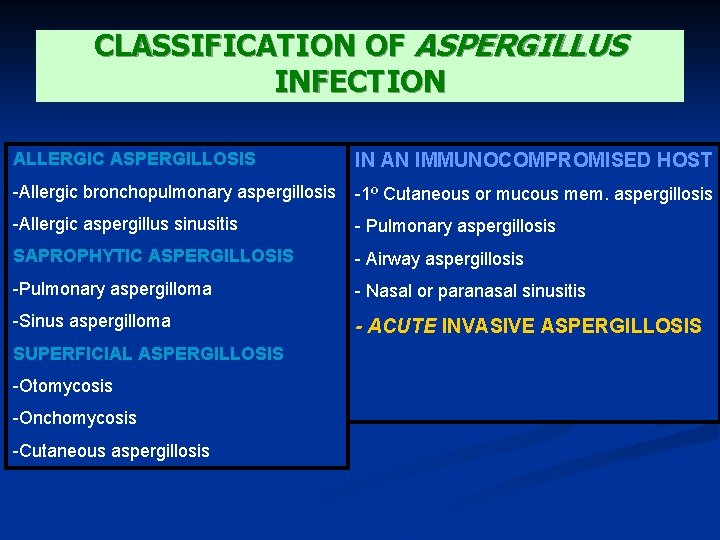
CLASSIFICATION OF ASPERGILLUS INFECTION ALLERGIC ASPERGILLOSIS IN AN IMMUNOCOMPROMISED HOST -Allergic bronchopulmonary aspergillosis -1º Cutaneous or mucous mem. aspergillosis -Allergic aspergillus sinusitis - Pulmonary aspergillosis SAPROPHYTIC ASPERGILLOSIS - Airway aspergillosis -Pulmonary aspergilloma - Nasal or paranasal sinusitis -Sinus aspergilloma - ACUTE INVASIVE ASPERGILLOSIS SUPERFICIAL ASPERGILLOSIS -Otomycosis -Onchomycosis -Cutaneous aspergillosis
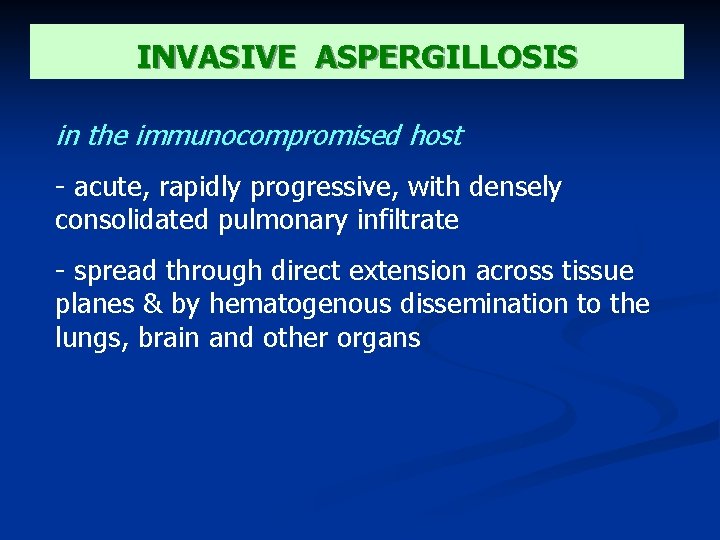
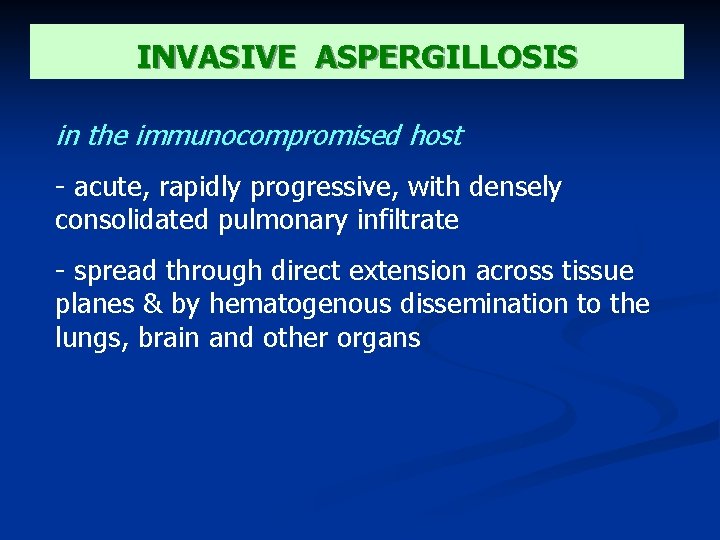
INVASIVE ASPERGILLOSIS in the immunocompromised host - acute, rapidly progressive, with densely consolidated pulmonary infiltrate - spread through direct extension across tissue planes & by hematogenous dissemination to the lungs, brain and other organs
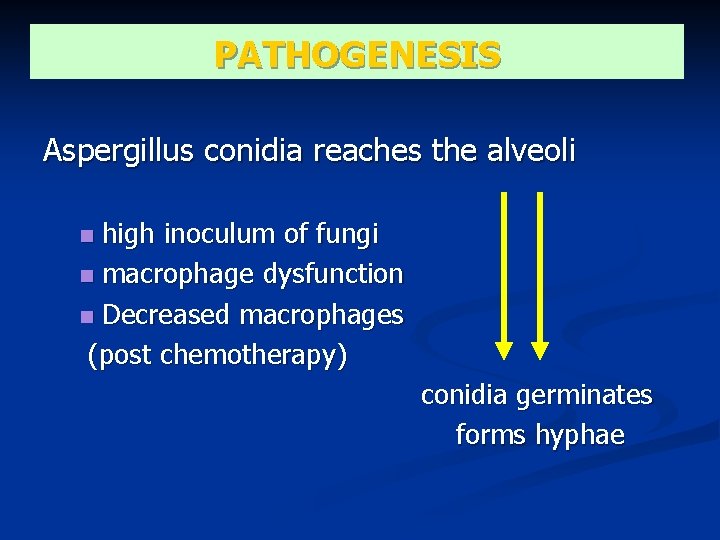
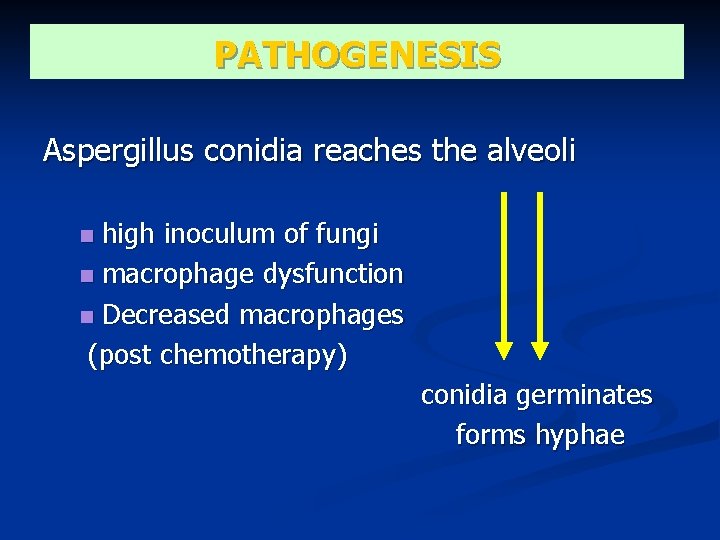
PATHOGENESIS Aspergillus conidia reaches the alveoli high inoculum of fungi macrophage dysfunction Decreased macrophages (post chemotherapy) conidia germinates forms hyphae
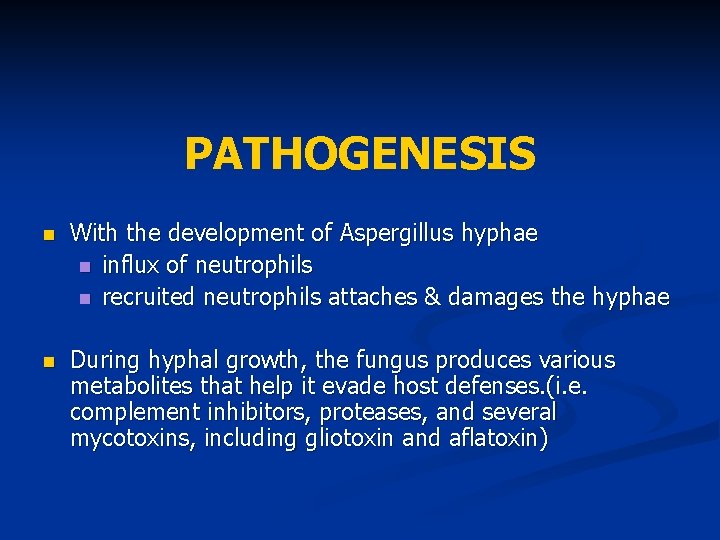
PATHOGENESIS With the development of Aspergillus hyphae influx of neutrophils recruited neutrophils attaches & damages the hyphae During hyphal growth, the fungus produces various metabolites that help it evade host defenses. (i. e. complement inhibitors, proteases, and several mycotoxins, including gliotoxin and aflatoxin)
PATHOLOGY - progression of the infection across tissue planes vascular invasion subsequent infarction tissue necrosis
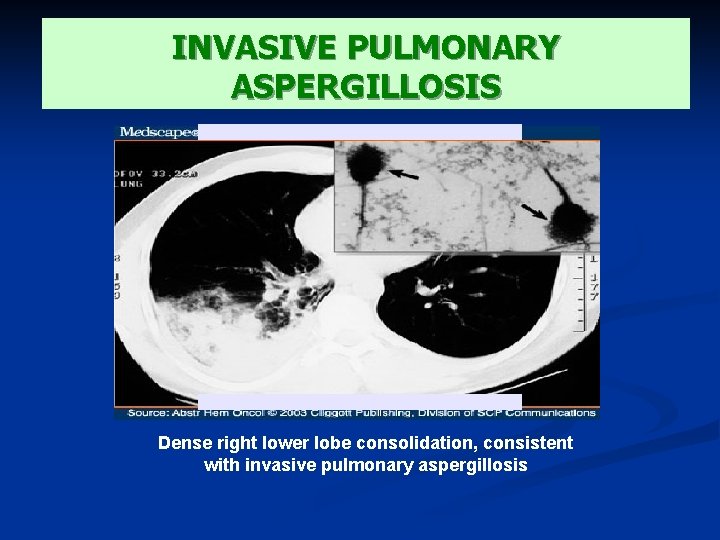
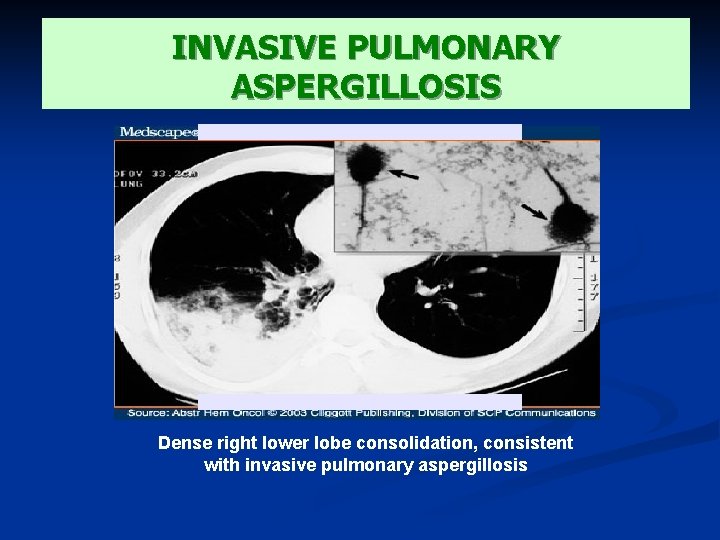
INVASIVE PULMONARY ASPERGILLOSIS Dense right lower lobe consolidation, consistent with invasive pulmonary aspergillosis
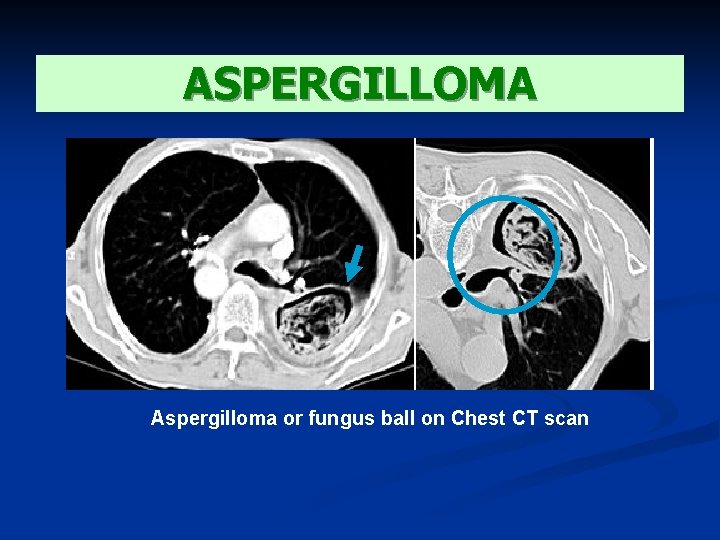
ASPERGILLOMA Vast majority of fungus balls in the lungs are due to aspergillus, with rare cases caused by Pseudoallescheria boydii or Mucorales Clinical manifestations: • asymptomatic • some may present with persistent productive cough, hemoptysis, wheezing, weight loss and finger clubbing.
ASPERGILLOMA • Complications: mild or massive hemoptysis, spread of infection to the pleura and contiguous vertebral bodies, dissemination to distant body sites (rare) • Approx. 10% resolve spontaneously • Tx : -Intracavitary Amphotericin B by transthoracic inj -Oral itraconazole -Surgical resection -Embolization
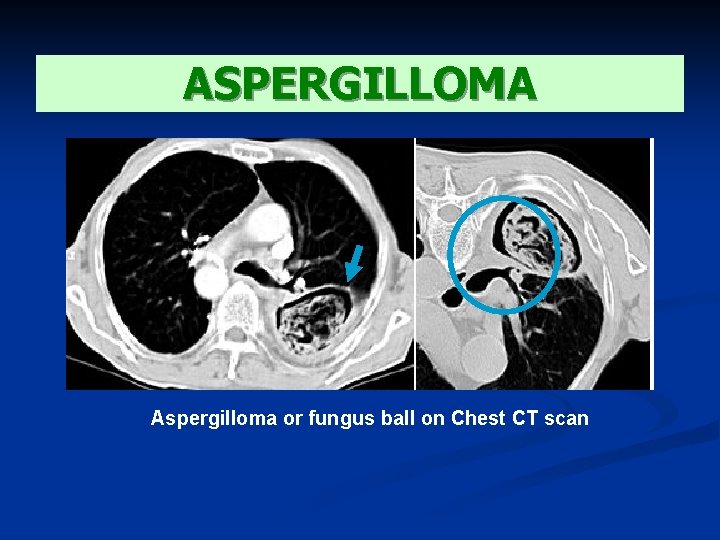
ASPERGILLOMA Aspergilloma or fungus ball on Chest CT scan
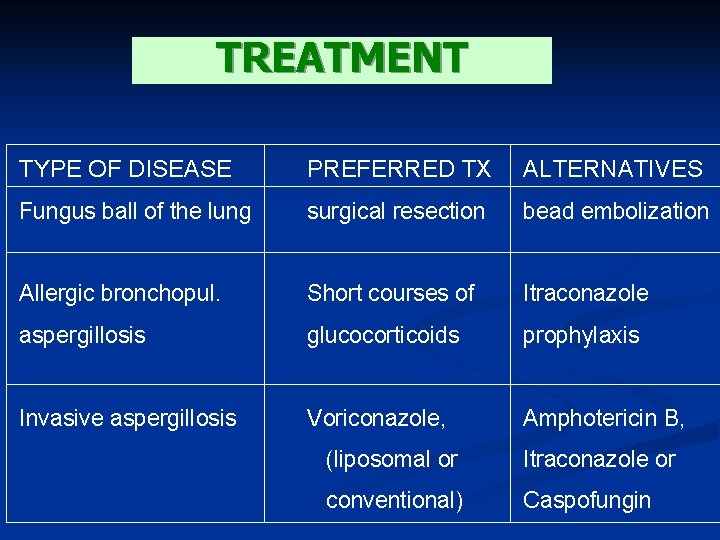
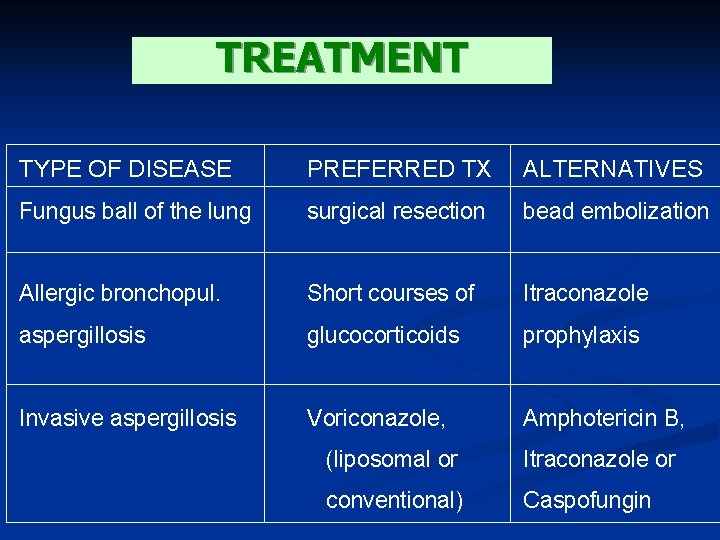
TREATMENT TYPE OF DISEASE PREFERRED TX ALTERNATIVES Fungus ball of the lung surgical resection bead embolization Allergic bronchopul. Short courses of Itraconazole aspergillosis glucocorticoids prophylaxis Invasive aspergillosis Voriconazole, Amphotericin B, (liposomal or Itraconazole or conventional) Caspofungin
TREATMENT 3 classes of antifungal agents are available for the treatment of Aspergillosis : 1. Polyenes (eg : Amphotericin B) 2. Azoles (eg : Itraconazole, Voriconazole) 3. Echinocandins (eg : Caspofungin)
TREATMENT AMPHOTERICIN B Treatment is limited by poor toleration & nephrotoxicity Dose : 1 – 1, 5 mg / kg per day Lipid formulation is currently available which can be administered with larger doses but showed fewer toxic effects

TREATMENT CASPOFUNGIN Is approved for the treatment of invasive aspergillosis in pts who cannot tolerate or who are refractory to standard therapy Dose : IV : loading dose 70 mg/day, followed by 50 mg/day
TREATMENT ITRACONAZOLE Is considered a 2 nd line agent for the tx of aspergillosis and is rarely used in immunocompromised pts with invasive disease Dose : 400 mg per day po Require acid environment for absorption, poor bioavailability and important drug interaction
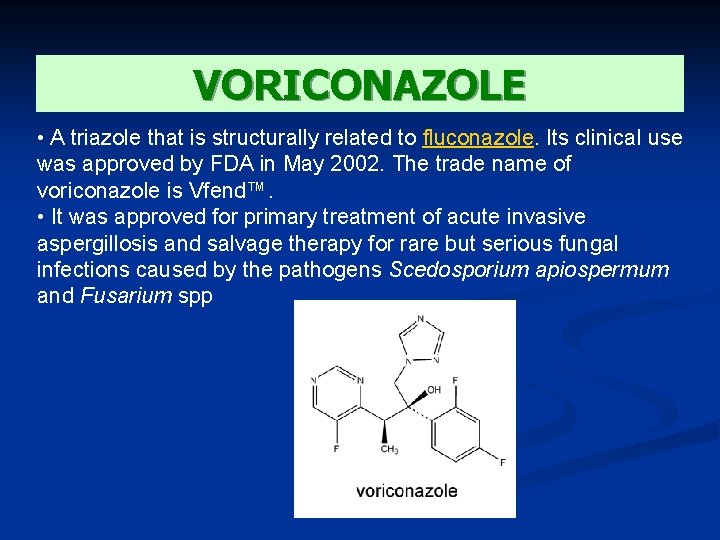
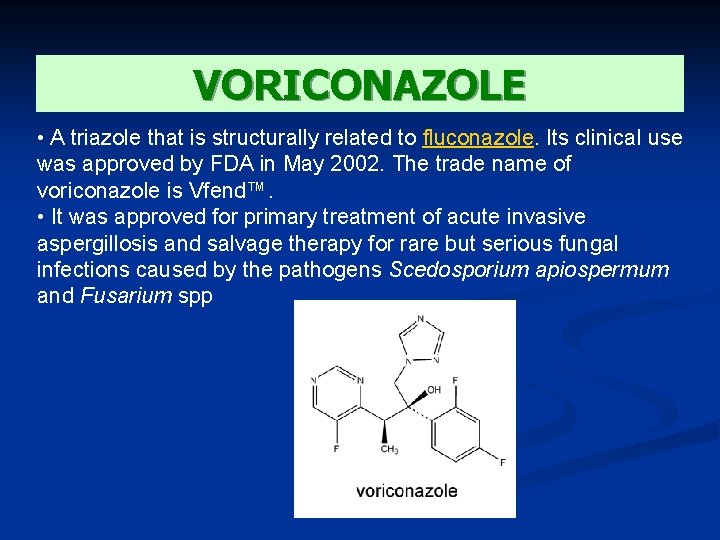
VORICONAZOLE • A triazole that is structurally related to fluconazole. Its clinical use was approved by FDA in May 2002. The trade name of voriconazole is Vfend™. • It was approved for primary treatment of acute invasive aspergillosis and salvage therapy for rare but serious fungal infections caused by the pathogens Scedosporium apiospermum and Fusarium spp
VORICONAZOLE - works principally by inhibition of cytochrome P 450 14 ademethylase (P 45014 DM). - favorable in vitro activity against a variety of fungi. These include, Candida spp. , Aspergillus spp. , Cryptococcus neoformans, Blastomyces dermatitidis, Coccidioides immitis, Histoplasma capsulatum, Fusarium spp. , and Penicillium marneffei. - a fungistatic agent against Candida spp. and Cryptococcus neoformans. It may be fungicidal against Aspergillus spp.
VORICONAZOLE - active Doses following both oral and intravenous administrations Oral: 200 mg twice daily IV: 3 to 6 mg/kg every 12 h doses SIDE EFFECTS: transient visual disturbances, skin rash and elevated hepatic enzyme levels
TREATMENT POSACONAZOLE is a broad spectrum triazole that is currently in development. Its activity is similar to Voriconazole against Aspergillus sp, but there is little published to date on its efficacy
CLINICAL STUDIES Voriconazole vs. Amphotericin B: Acute invasive aspergillosis National Institute of Allergy and Infectious Diseases Mycoses Study Group June 2001 - 277 patients treated for 12 weeks with Voriconazole and Amphotericin B - majority of study patients had underlying hematologic malignancies, including bone marrow transplantation; patients with solid organ transplantation, solid tumors, and AIDS. CONCLUSION: A satisfactory global response at 12 weeks was seen in 53% of voriconazole treated patients compared to 32% of amphotericin B treated patients. A benefit of voriconazole compared to amphotericin B on patient survival at Day 84 was seen with a 71% survival rate on voriconazole compared to 58% on amphotericin B.
CLINICAL STUDIES Fluconazole and Voriconazole Multidisk Testing of Candida Species for Disk Test Calibration and MIC Estimation Göran Kronvall* and Inga Karlsson Department of Microbiology and Tumor Biology, Sweden January 2001 Fluconazole and voriconazole MICs were determined for 114 clinical Candida isolates, including isolates of Candida albicans, Candida glabrata, Candida krusei, Candida lusitaniae, Candida parapsilosis, and Candida tropicalis. All strains were susceptible to voriconazole, and most strains were also susceptible to fluconazole, with the exception of C. glabrata and C. krusei, the latter being fully fluconazole resistant. Single-strain regression analysis (SRA) was applied to 54 strains. CONCLUSION: Voriconazole might be a first-choice azole in treating Candida infections.

THANK YOU!
 Meritus definition
Meritus definition Employment of non-resident aliens in the philippines
Employment of non-resident aliens in the philippines Transamerica estate planning foreign nationals
Transamerica estate planning foreign nationals Chapter 2 foundations of resident care
Chapter 2 foundations of resident care Acgme resident survey questions
Acgme resident survey questions Magic mask
Magic mask Chapter 10 positioning transfers and ambulation
Chapter 10 positioning transfers and ambulation What is tax id
What is tax id Resident and family engagement
Resident and family engagement Attending vs resident
Attending vs resident Orientation and resident rights quiz
Orientation and resident rights quiz Resident set management
Resident set management Ota resident lectures
Ota resident lectures Partially resident textures
Partially resident textures Resident assessment instrument definition
Resident assessment instrument definition Divine intervention resident
Divine intervention resident Resident and family engagement
Resident and family engagement Misappropriation of resident property
Misappropriation of resident property Resident customer service
Resident customer service Resident retention
Resident retention Acgme resident survey
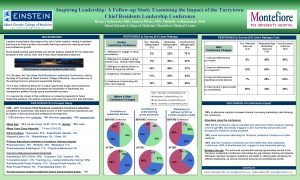
Acgme resident survey Tarrytown chief resident conference
Tarrytown chief resident conference Resident lifecycle
Resident lifecycle Yelena bogdan md
Yelena bogdan md A helpful way for an na to respond to hallucinations is to
A helpful way for an na to respond to hallucinations is to Define resident flora
Define resident flora Placement policy in os
Placement policy in os Greater baltimore medical center medical records
Greater baltimore medical center medical records Cartersville medical center medical records
Cartersville medical center medical records Difference between medical report and medical certificate
Difference between medical report and medical certificate Ptal california medical board
Ptal california medical board Torrance memorial hospital medical records
Torrance memorial hospital medical records 25 january scotland
25 january scotland Nysedregents chemistry
Nysedregents chemistry January 20
January 20 January 10th 1776
January 10th 1776 January comes before february
January comes before february His birth date was on 25 january 1759
His birth date was on 25 january 1759 Character traits of respect
Character traits of respect In which year was mozart born
In which year was mozart born January 29 2015
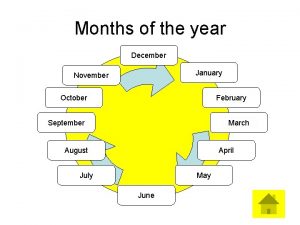
January 29 2015 January february march april
January february march april Arvod cannot find work as a mall santa in january.
Arvod cannot find work as a mall santa in january. December november october
December november october Elephant syllables
Elephant syllables January 24, 1848
January 24, 1848 9 months before january 26 2009
9 months before january 26 2009 January 2012 chemistry regents answers
January 2012 chemistry regents answers January 2012
January 2012 He was born in salzburg austria on january 27 1756
He was born in salzburg austria on january 27 1756 Spatial january
Spatial january An asset was purchased for $120 000 on january 1
An asset was purchased for $120 000 on january 1 April 2006 calendar
April 2006 calendar January february spelling
January february spelling Sunday, tuesday, january, saturday
Sunday, tuesday, january, saturday January february march
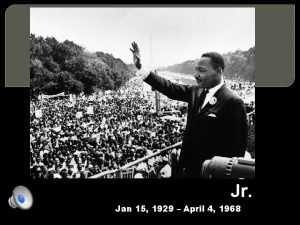
January february march January 15 1929
January 15 1929 January 31 2006
January 31 2006 Tinseltow
Tinseltow January 19, 1809
January 19, 1809 Meridel lesueur, new masses, january 1932
Meridel lesueur, new masses, january 1932 Life of a plant poem by risa jordan
Life of a plant poem by risa jordan Zodiac for january 20
Zodiac for january 20 Which famous musician is born in salzburg austria
Which famous musician is born in salzburg austria How old are you peter weatherall
How old are you peter weatherall Meridel lesueur new masses january 1932
Meridel lesueur new masses january 1932 What is the theme for the month of january
What is the theme for the month of january January 27, 1756
January 27, 1756 January 15, 1929
January 15, 1929 January 25 2018 chemistry regents answers
January 25 2018 chemistry regents answers March april june july august
March april june july august Manage end user devices
Manage end user devices January 19, 1809
January 19, 1809 Polytechnic hardware store
Polytechnic hardware store Ib history ia grade boundaries
Ib history ia grade boundaries Newton biography
Newton biography January 13 2006 calendar
January 13 2006 calendar January 15 1929
January 15 1929