Mechanical Ventilation Karin Halvorson MD IMEMPulmCC Tulane Assistant
- Slides: 24
Mechanical Ventilation Karin Halvorson, MD IM/EM/Pulm/CC Tulane Assistant Professor
MODES n AC Minimum number of supported breaths n Target Volume or Pressure n n SIMV n Minimum number of supported breaths (synchronized to pt’s breathing) PSV n CPAP/Bi. PAP n T-piece n
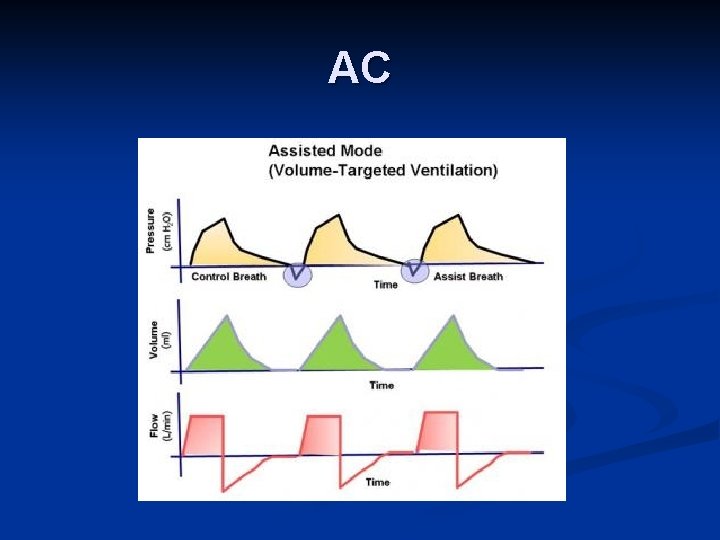
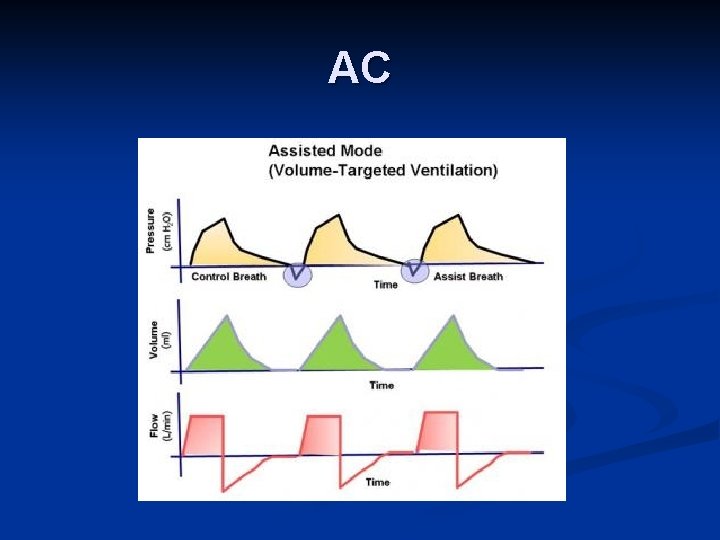
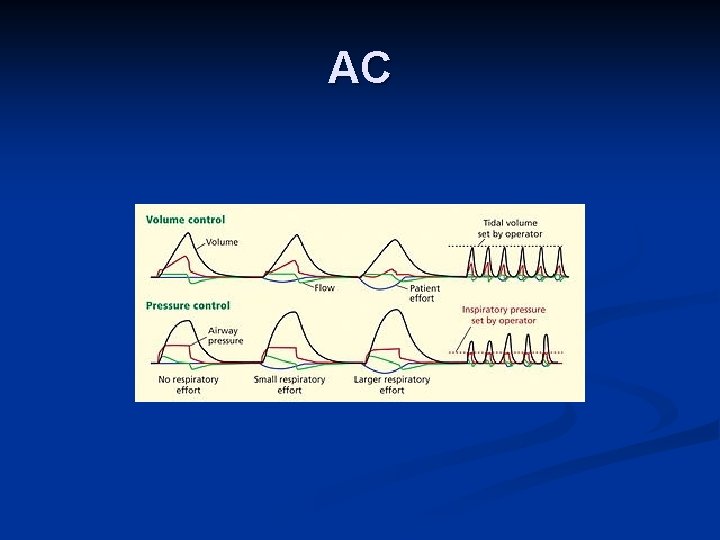
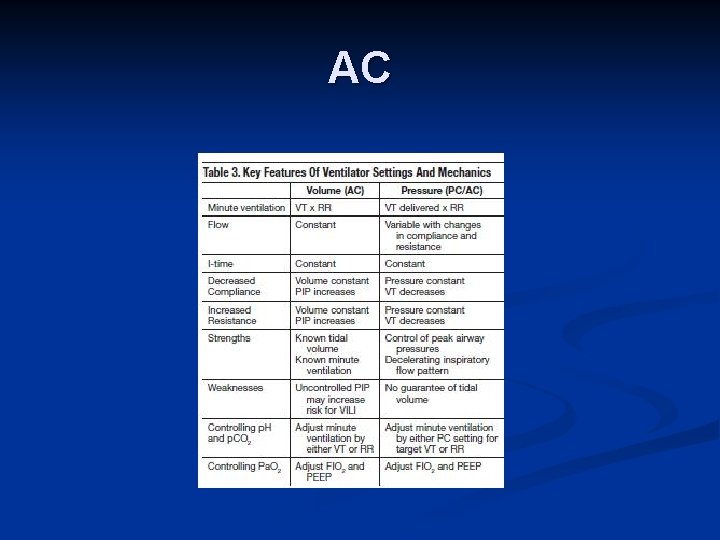
AC
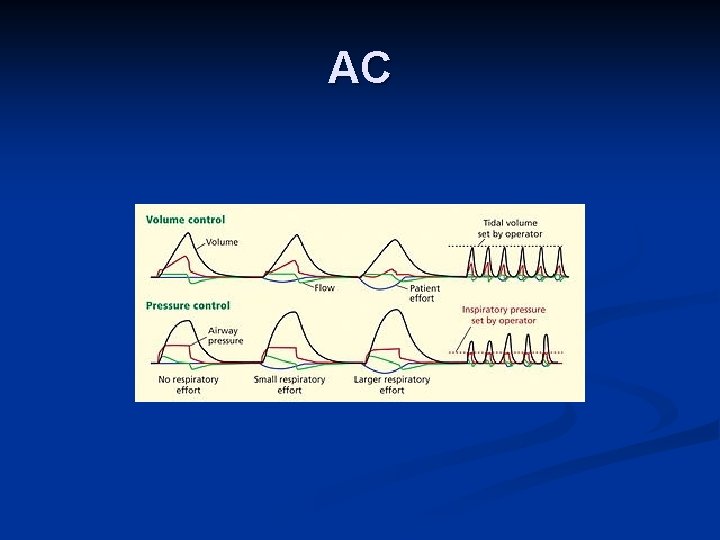
AC
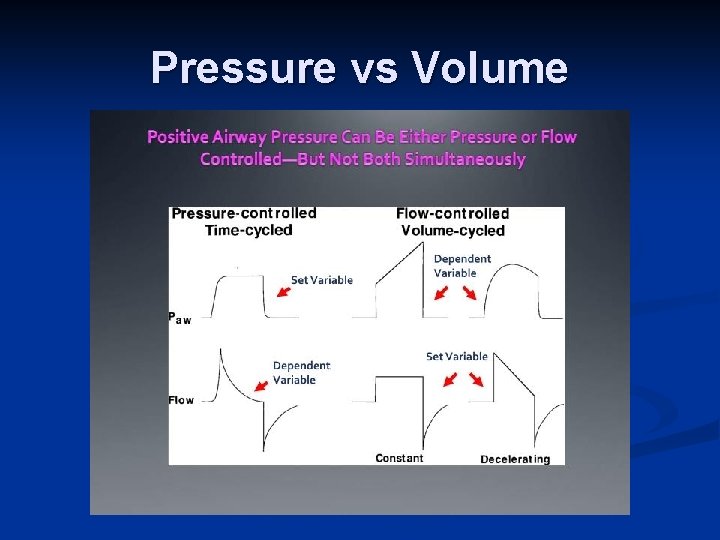
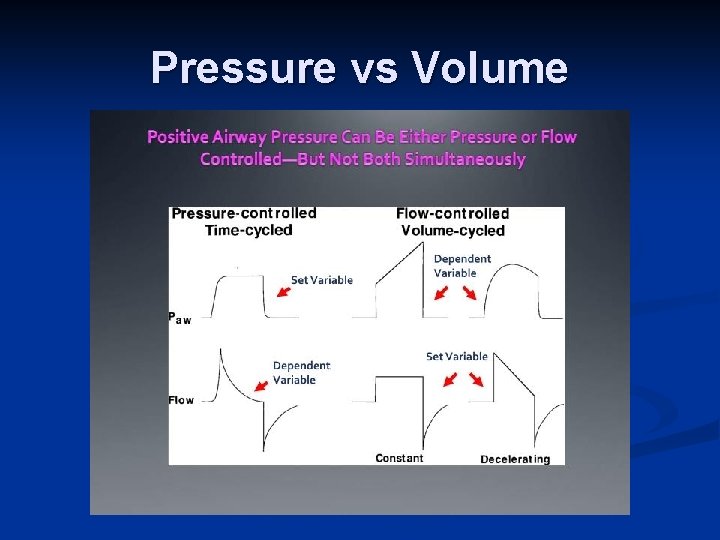
Pressure vs Volume
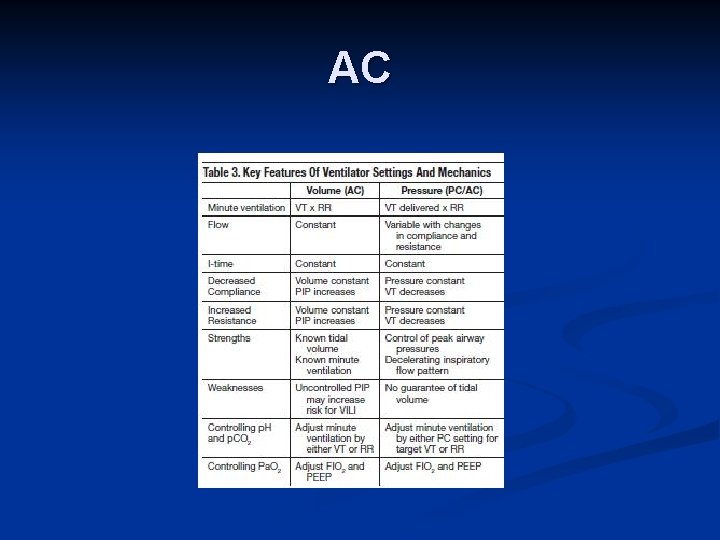
AC
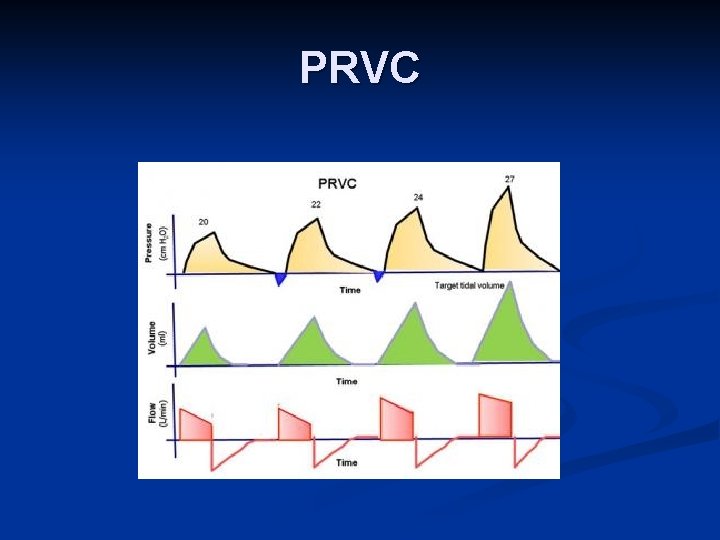
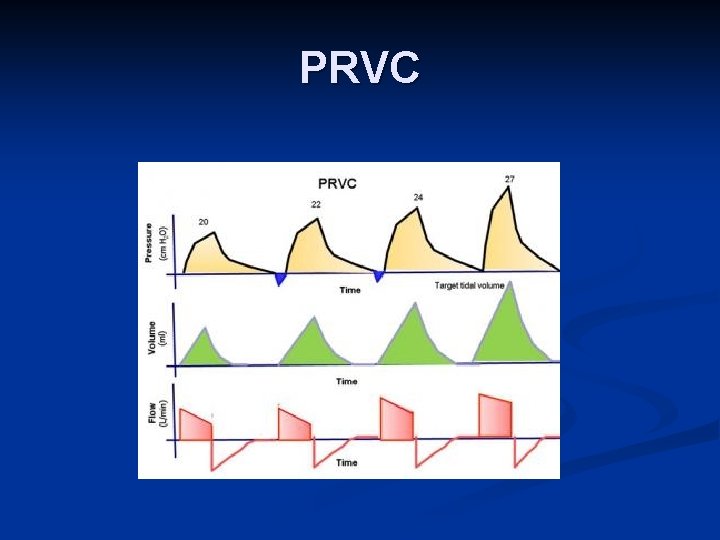
PRVC
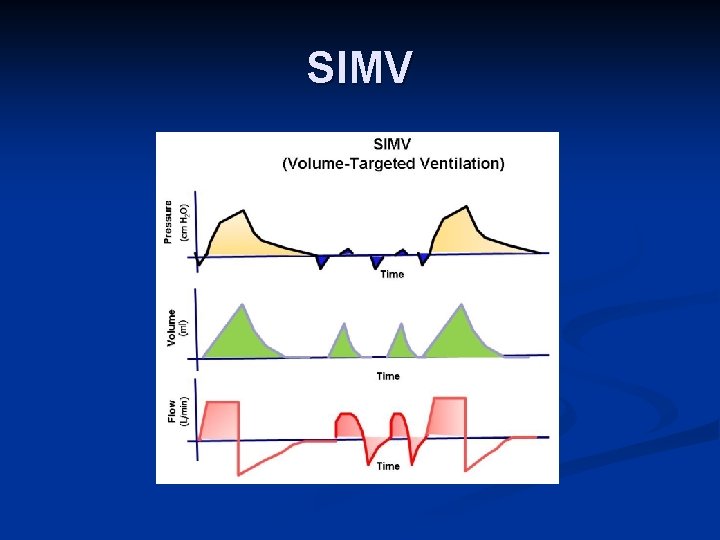
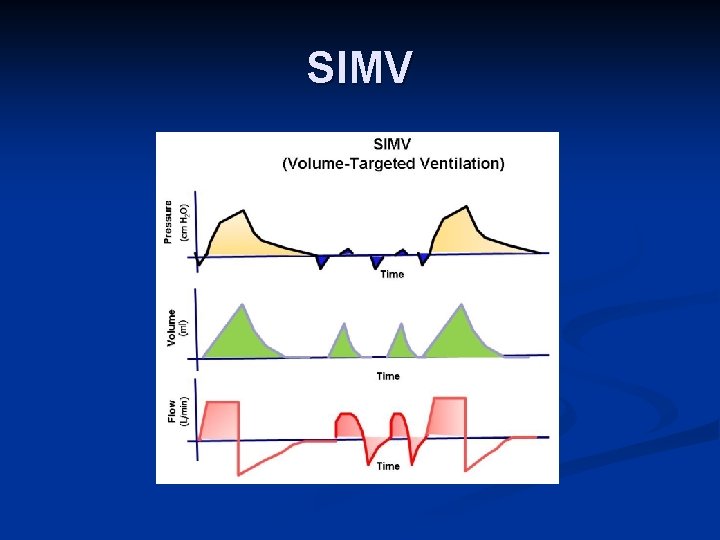
SIMV
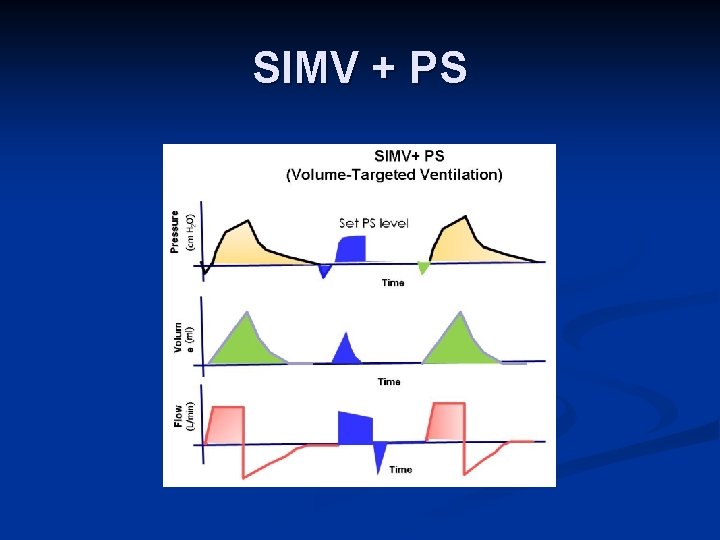
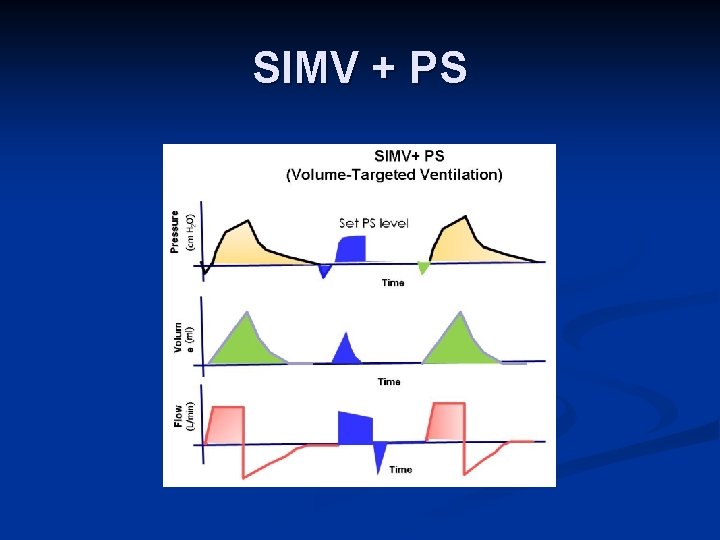
SIMV + PS
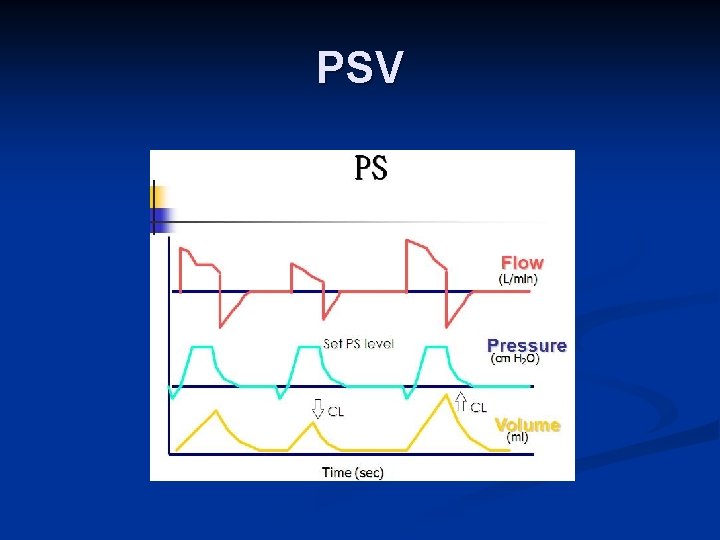
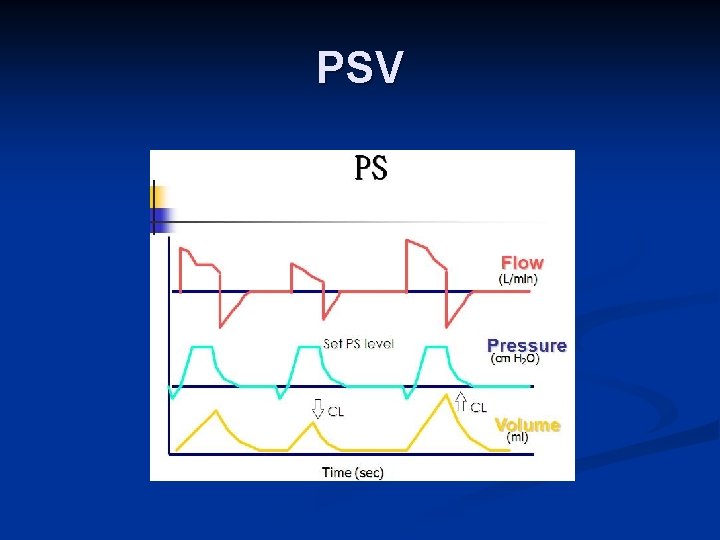
PSV
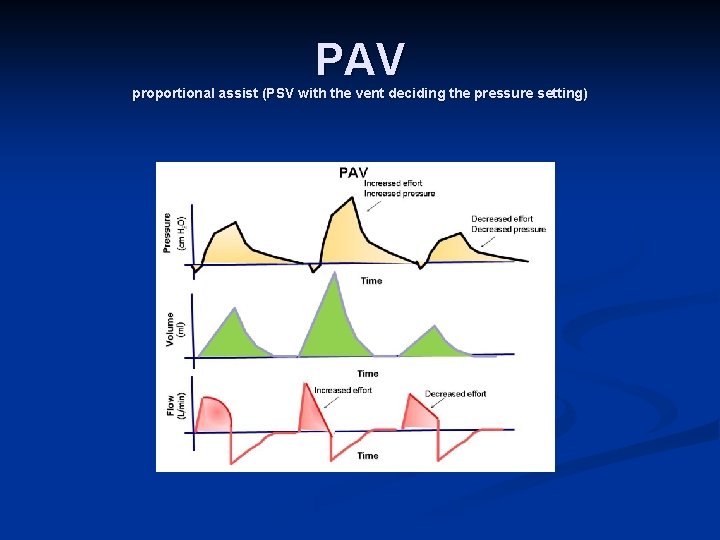
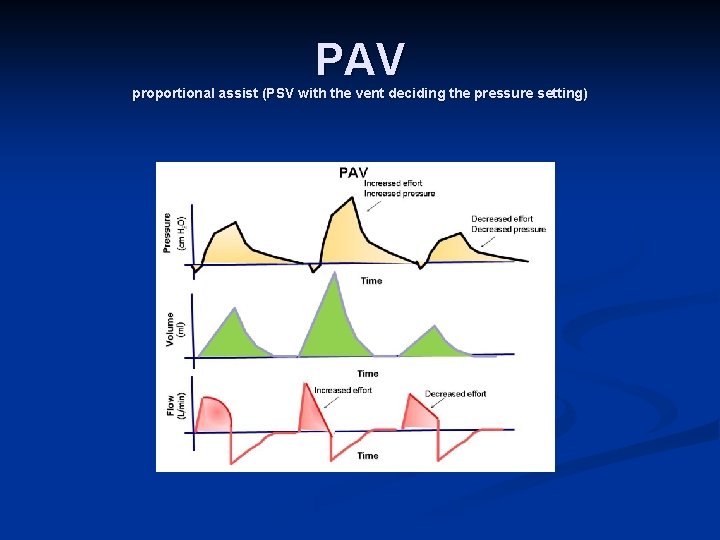
PAV proportional assist (PSV with the vent deciding the pressure setting)
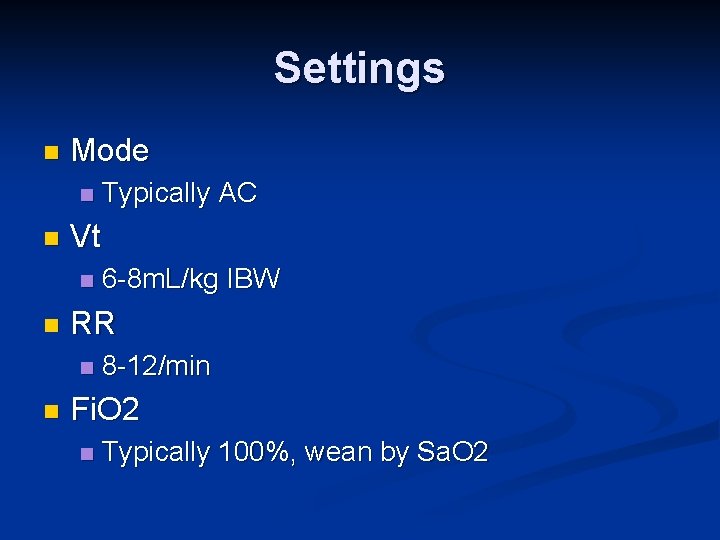
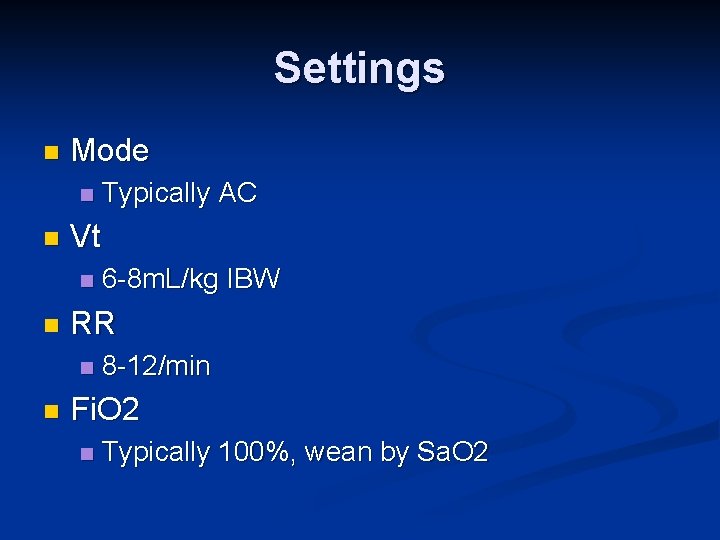
Settings n Mode n n Vt n n 6 -8 m. L/kg IBW RR n n Typically AC 8 -12/min Fi. O 2 n Typically 100%, wean by Sa. O 2
Modifiers n Oxygenation Fi. O 2 n PEEP n n Ventilation Mode n Vt n RR n
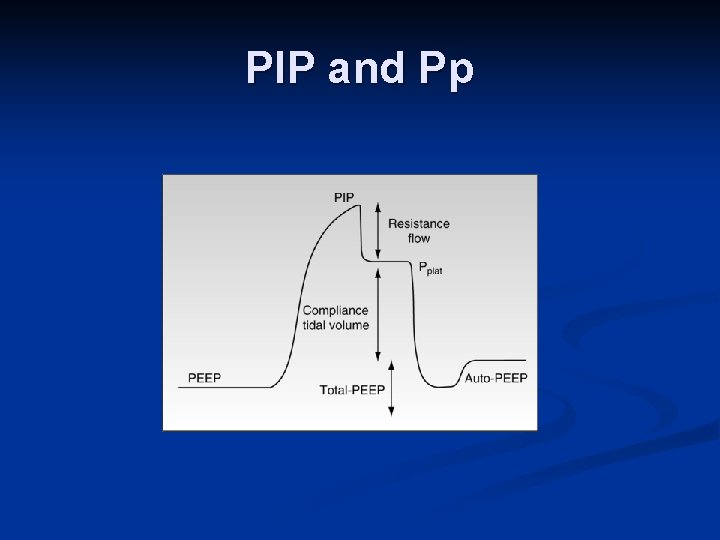
Peak & Plateau n Peak inspiratory pressure (PIP) n n Determined by airway resistance and lung compliance Plateau pressure (Pp) Determined by lung compliance n Goal <30 n
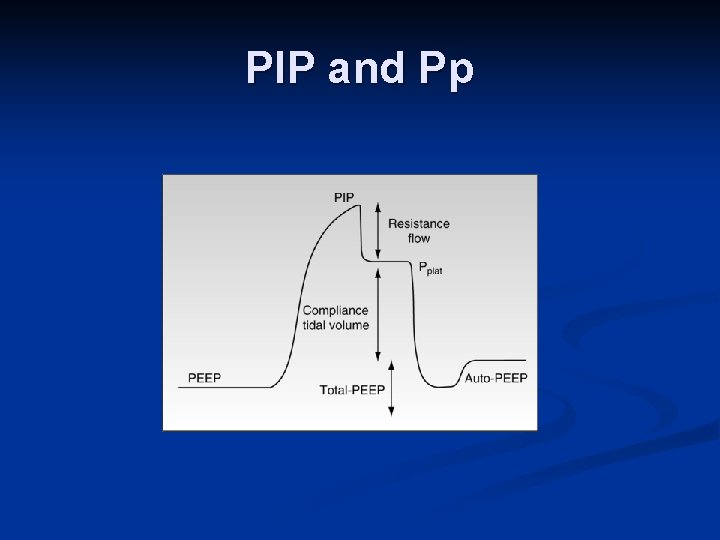
PIP and Pp
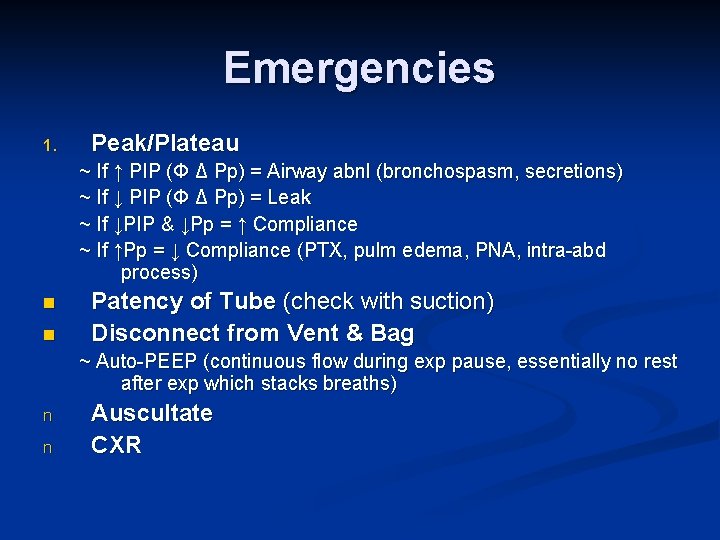
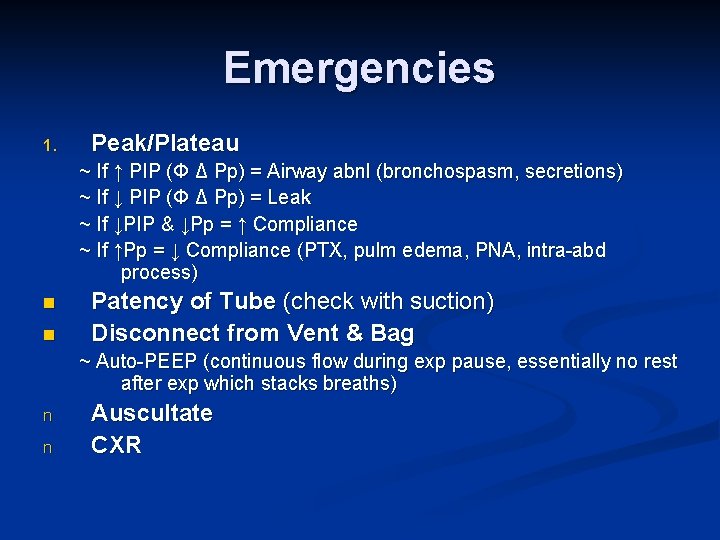
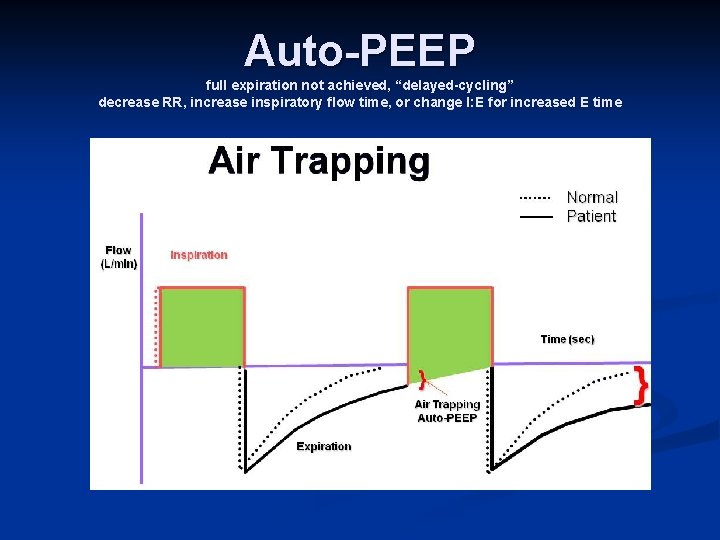
Emergencies 1. Peak/Plateau ~ If ↑ PIP (Φ Δ Pp) = Airway abnl (bronchospasm, secretions) ~ If ↓ PIP (Φ Δ Pp) = Leak ~ If ↓PIP & ↓Pp = ↑ Compliance ~ If ↑Pp = ↓ Compliance (PTX, pulm edema, PNA, intra-abd process) n n Patency of Tube (check with suction) Disconnect from Vent & Bag ~ Auto-PEEP (continuous flow during exp pause, essentially no rest after exp which stacks breaths) n n Auscultate CXR
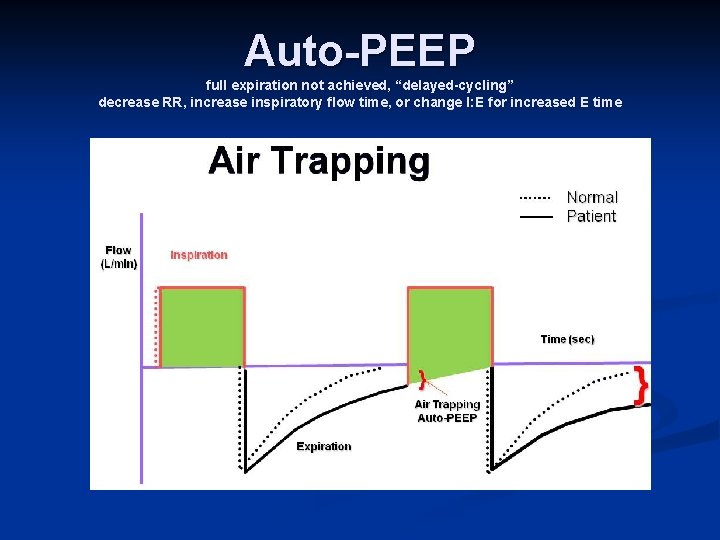
Auto-PEEP full expiration not achieved, “delayed-cycling” decrease RR, increase inspiratory flow time, or change I: E for increased E time
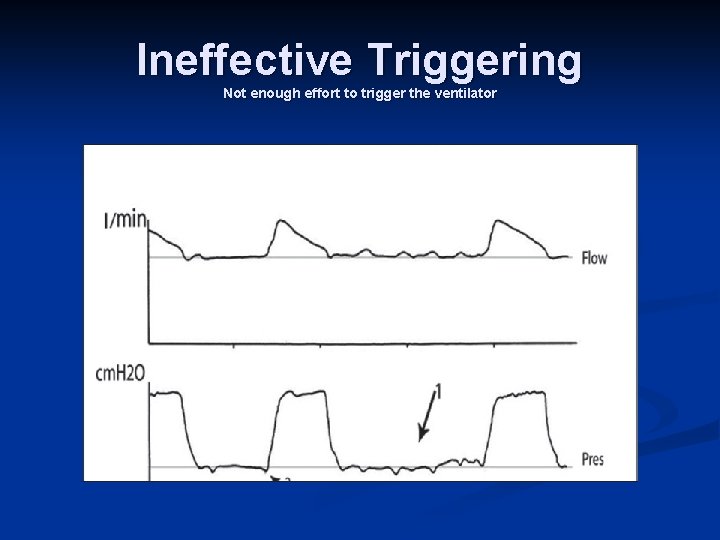
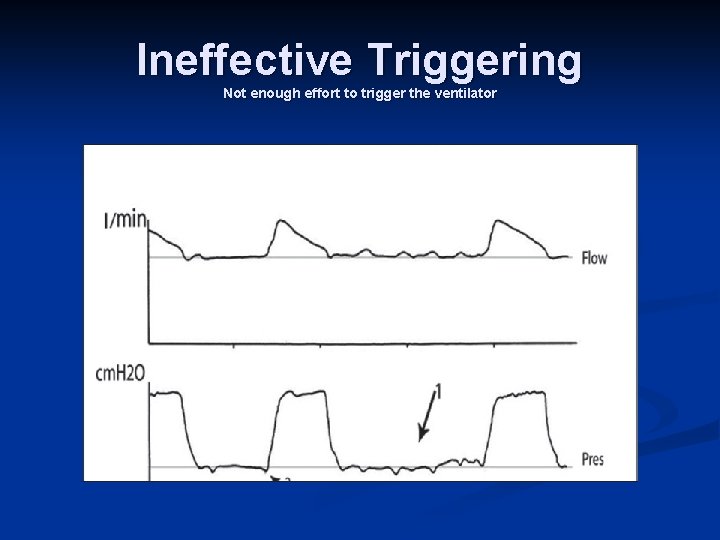
Ineffective Triggering Not enough effort to trigger the ventilator
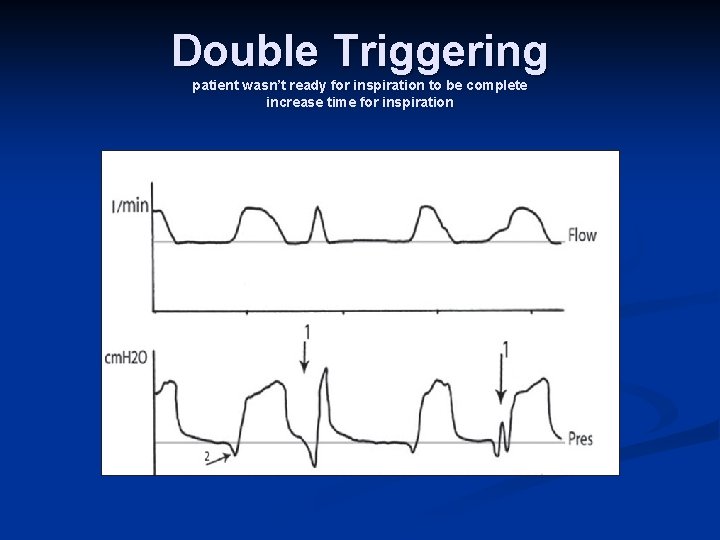
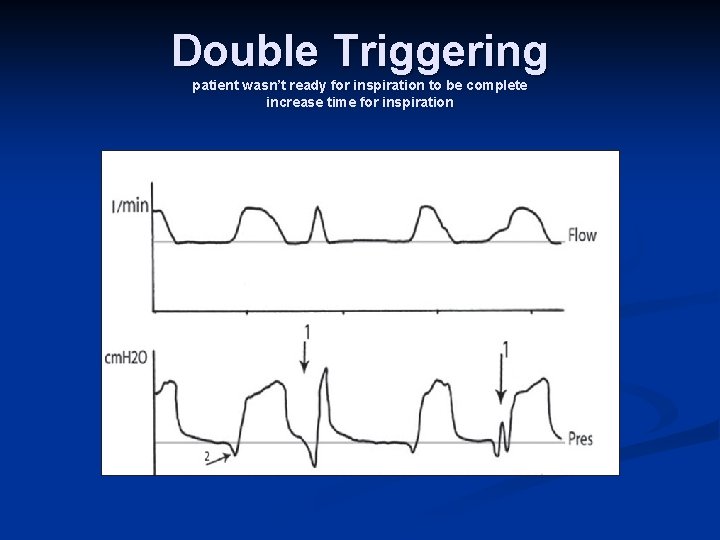
Double Triggering patient wasn’t ready for inspiration to be complete increase time for inspiration
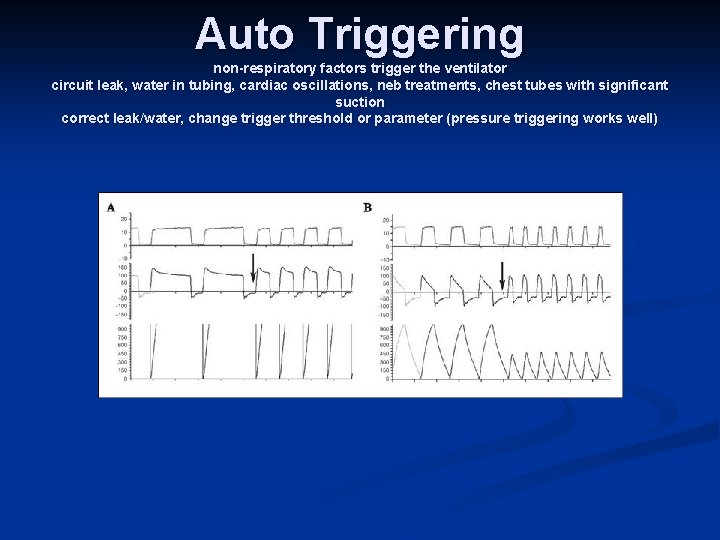
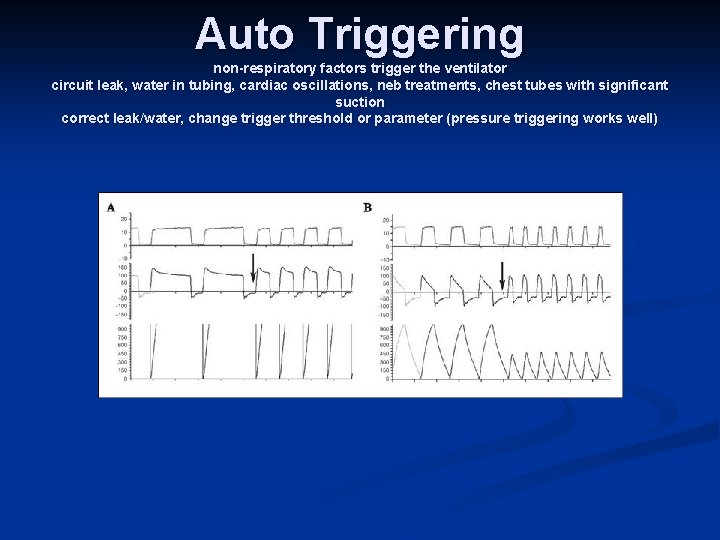
Auto Triggering non-respiratory factors trigger the ventilator circuit leak, water in tubing, cardiac oscillations, neb treatments, chest tubes with significant suction correct leak/water, change trigger threshold or parameter (pressure triggering works well)
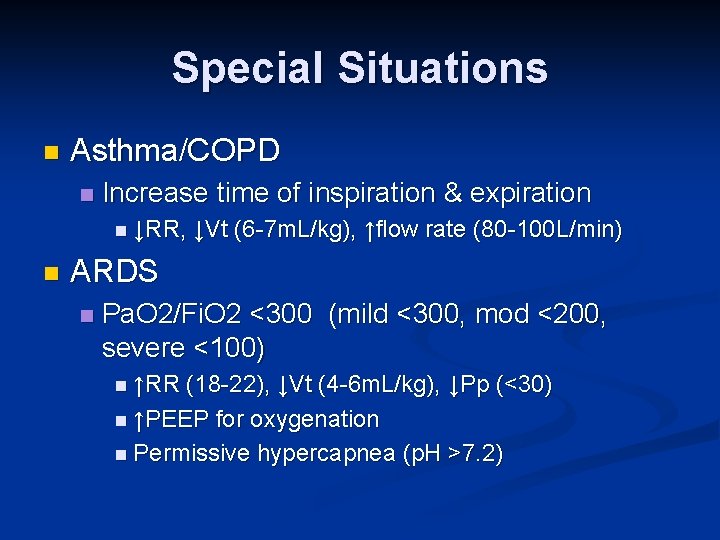
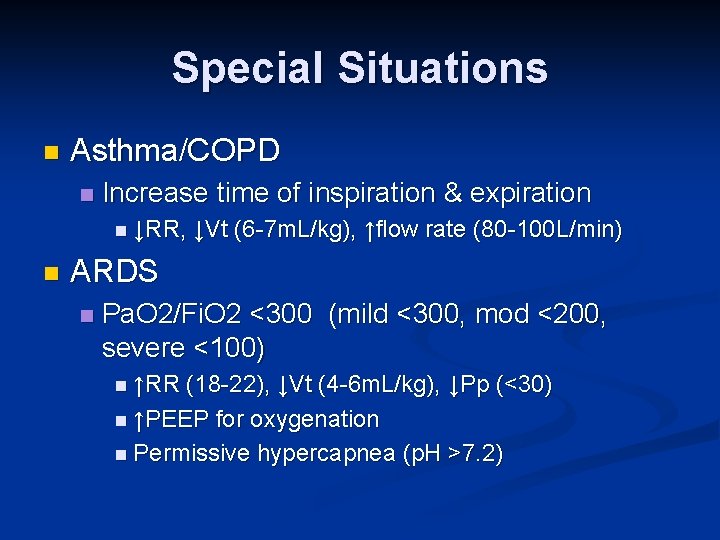
Special Situations n Asthma/COPD n Increase time of inspiration & expiration n ↓RR, n ↓Vt (6 -7 m. L/kg), ↑flow rate (80 -100 L/min) ARDS n Pa. O 2/Fi. O 2 <300 (mild <300, mod <200, severe <100) n ↑RR (18 -22), ↓Vt (4 -6 m. L/kg), ↓Pp (<30) n ↑PEEP for oxygenation n Permissive hypercapnea (p. H >7. 2)
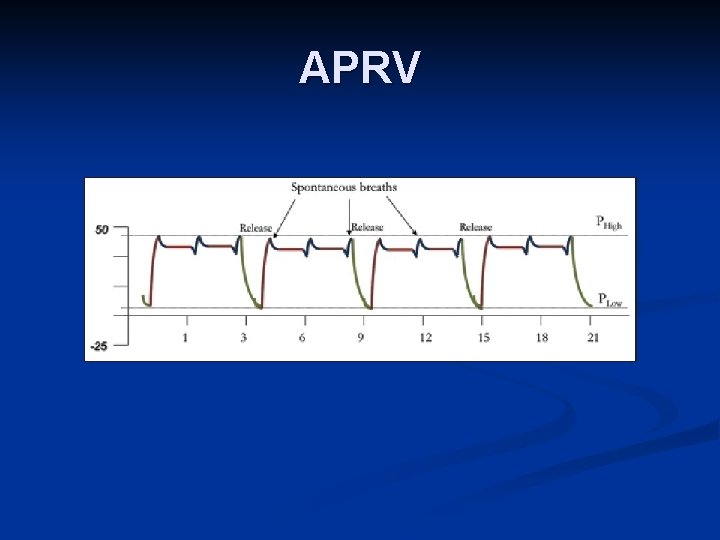
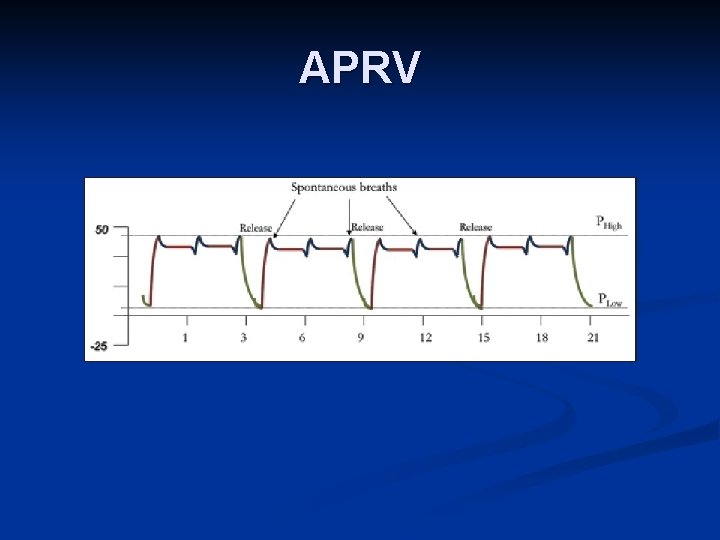
APRV
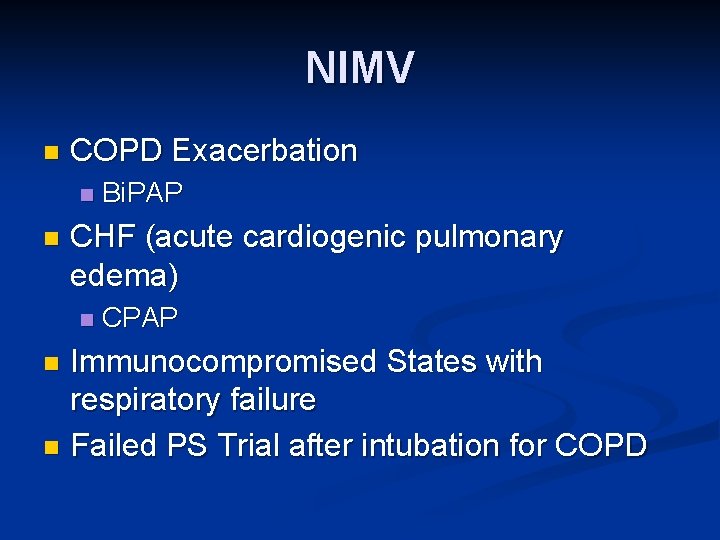
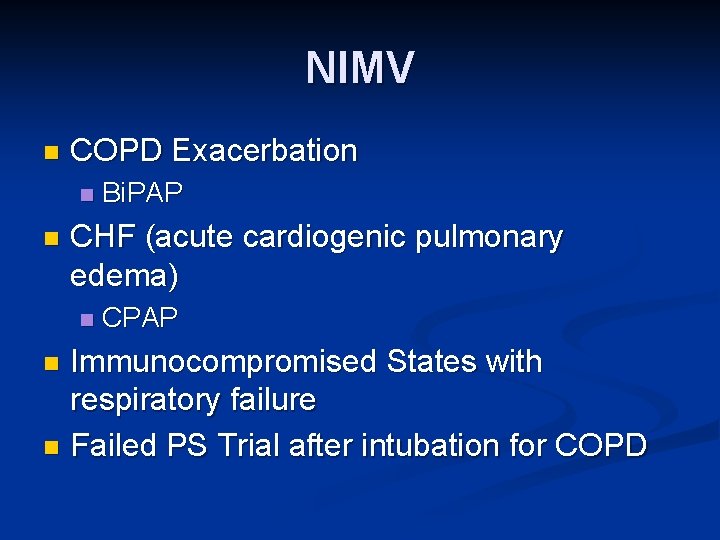
NIMV n COPD Exacerbation n n Bi. PAP CHF (acute cardiogenic pulmonary edema) n CPAP Immunocompromised States with respiratory failure n Failed PS Trial after intubation for COPD n
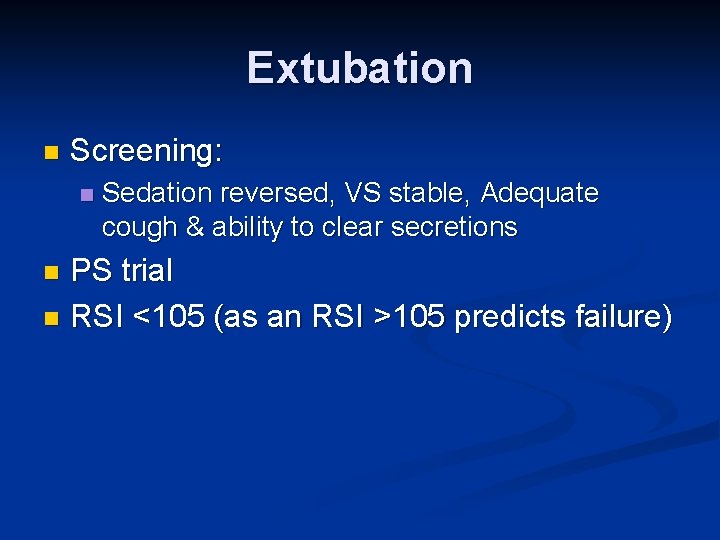
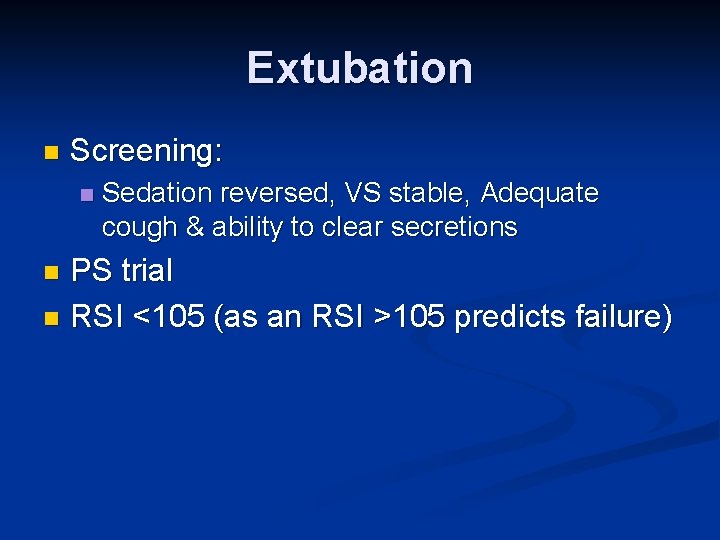
Extubation n Screening: n Sedation reversed, VS stable, Adequate cough & ability to clear secretions PS trial n RSI <105 (as an RSI >105 predicts failure) n