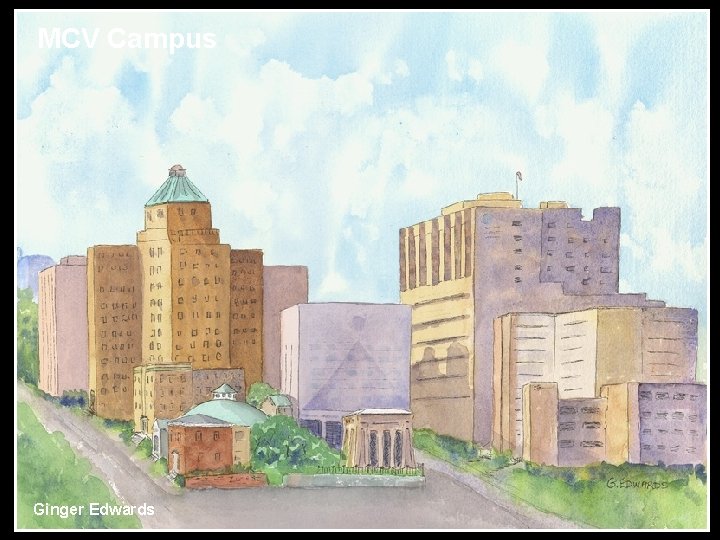
MCV Campus Ginger Edwards DISCLOSURES George W Vetrovec









- Slides: 55
MCV Campus Ginger Edwards
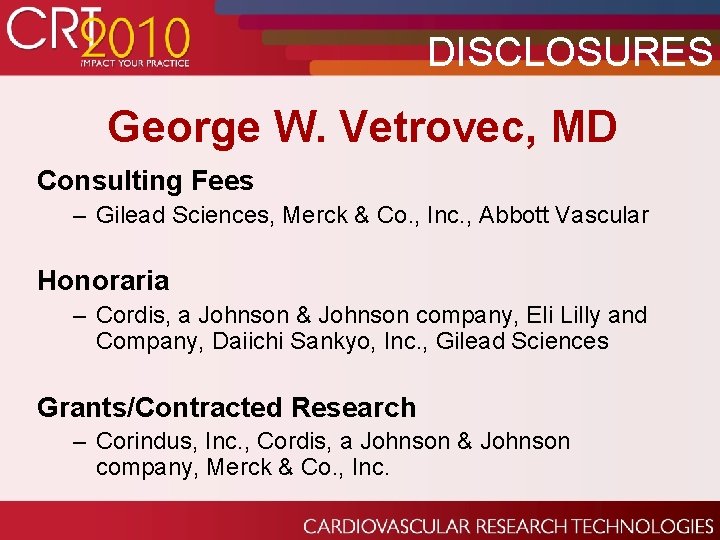
DISCLOSURES George W. Vetrovec, MD Consulting Fees – Gilead Sciences, Merck & Co. , Inc. , Abbott Vascular Honoraria – Cordis, a Johnson & Johnson company, Eli Lilly and Company, Daiichi Sankyo, Inc. , Gilead Sciences Grants/Contracted Research – Corindus, Inc. , Cordis, a Johnson & Johnson company, Merck & Co. , Inc.
Percutaneous Coronary Intervention: Basic Techniques George W. Vetrovec, MD. VCU Pauley Heart Center MCV Campus Virginia Commonwealth University
PCI Basics • • • Radiation Safety Angiography Contrast Volume Anatomic risk assessment of procedure Pharmacology Equipment use Stent Deployment Follow-up Angiography Compliance

Radiation Safety • In PCI flouro accounts for more radiation than Cine • Never fluoro when not viewing • Multiple views • Shielding • One Step Rule
Coronary Angiography
Contrast Volume Limit!
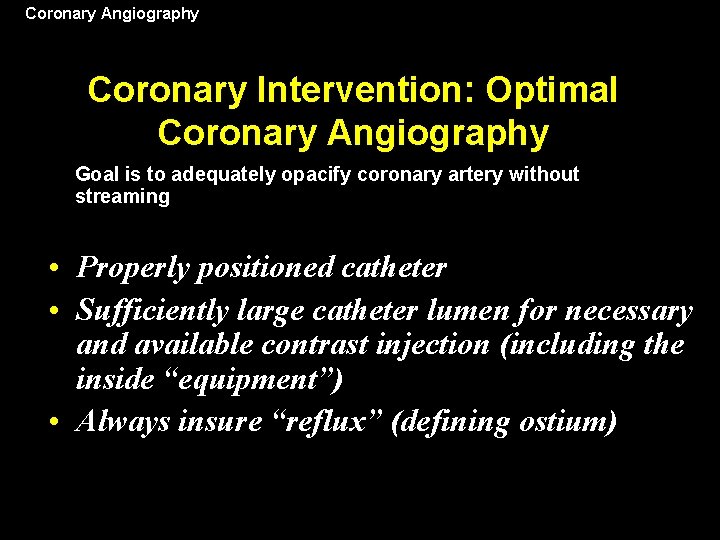
Coronary Angiography Coronary Intervention: Optimal Coronary Angiography Goal is to adequately opacify coronary artery without streaming • Properly positioned catheter • Sufficiently large catheter lumen for necessary and available contrast injection (including the inside “equipment”) • Always insure “reflux” (defining ostium)
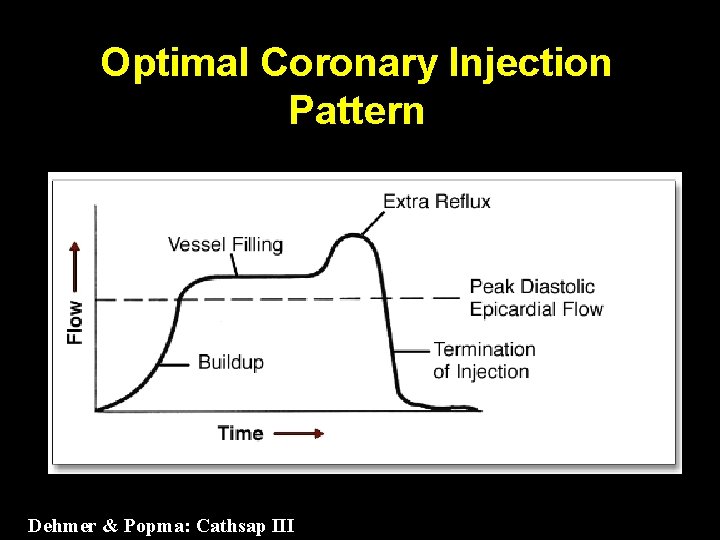
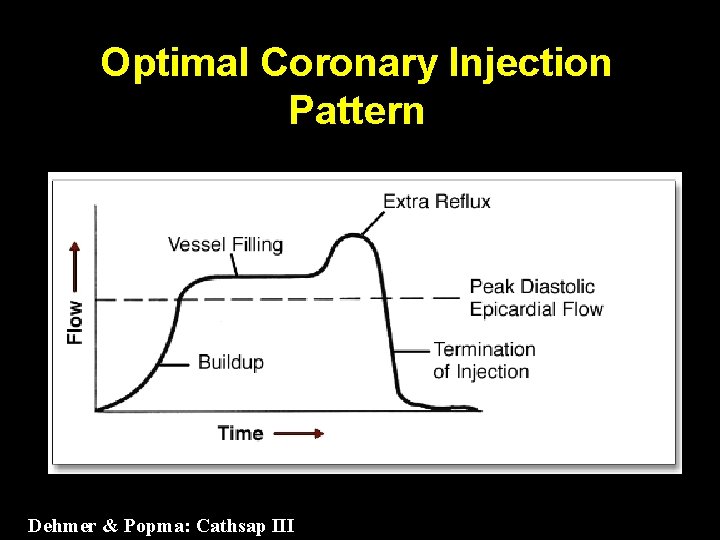
Optimal Coronary Injection Pattern Dehmer & Popma: Cathsap III
Coronary Angiography for PCI • Get a Clear View of vessel and lesion anatomy including side branches. • Better yet, get two high quality orthogonal views. • If the wire is not going properly in your “best view” look in a second view.
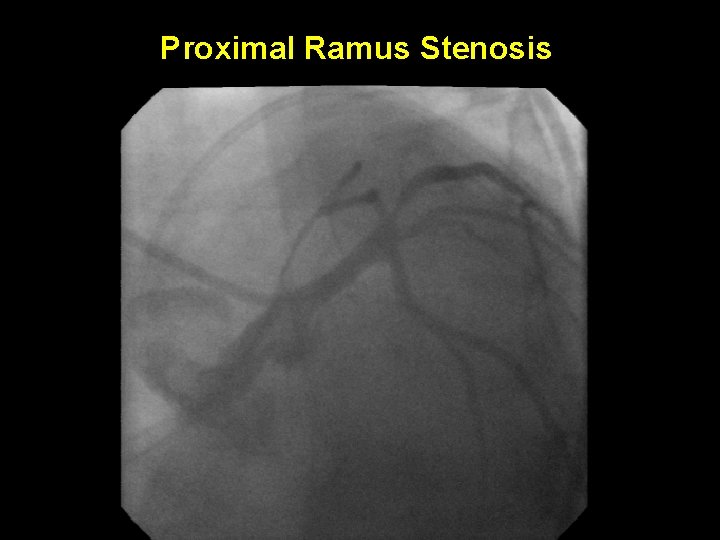
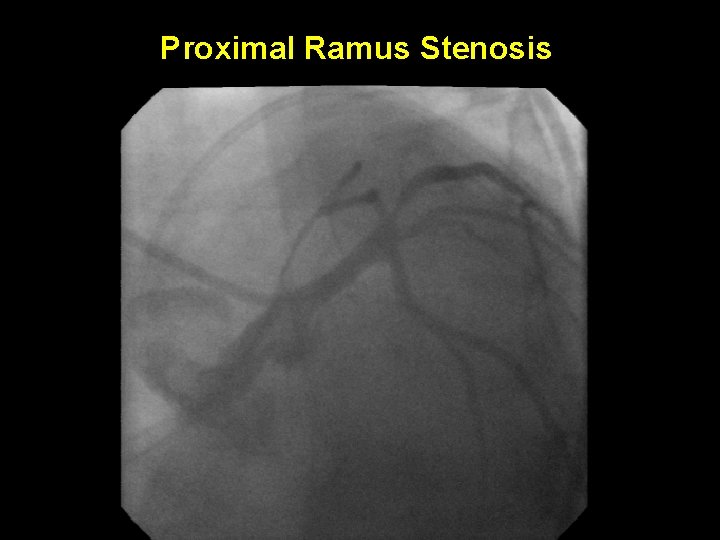
Proximal Ramus Stenosis
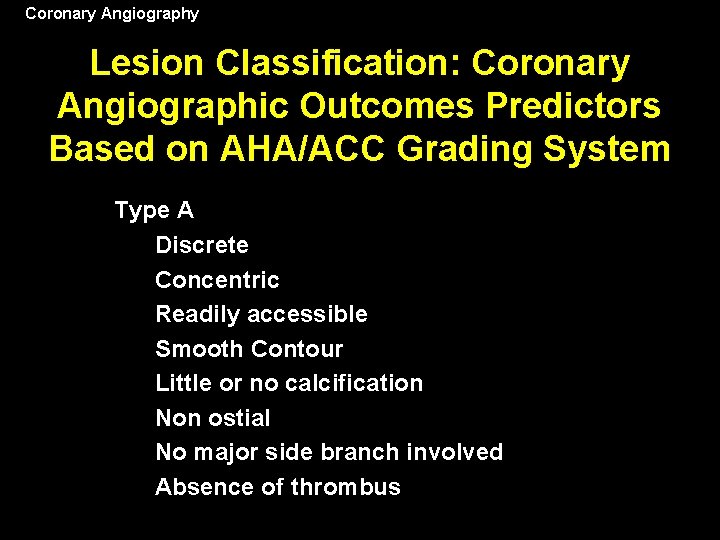
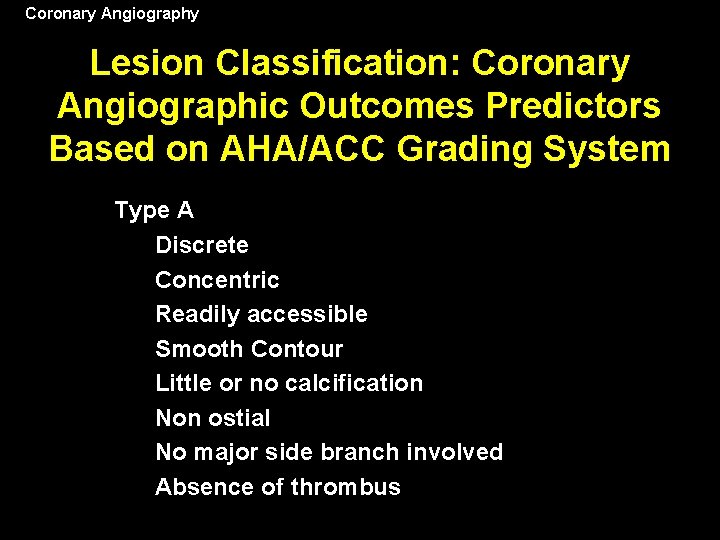
Coronary Angiography Lesion Classification: Coronary Angiographic Outcomes Predictors Based on AHA/ACC Grading System Type A Discrete Concentric Readily accessible Smooth Contour Little or no calcification Non ostial No major side branch involved Absence of thrombus
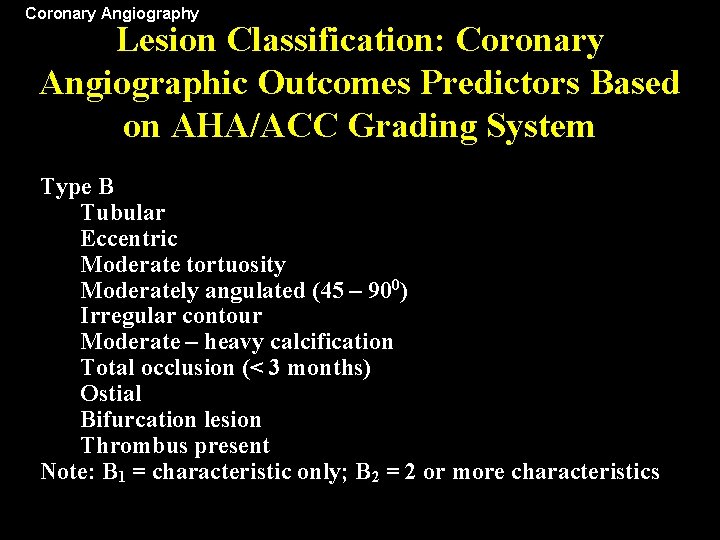
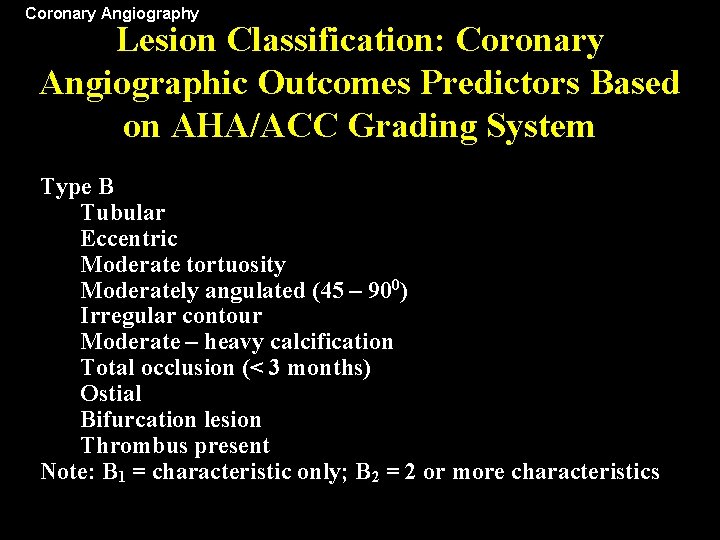
Coronary Angiography Lesion Classification: Coronary Angiographic Outcomes Predictors Based on AHA/ACC Grading System Type B Tubular Eccentric Moderate tortuosity Moderately angulated (45 – 900) Irregular contour Moderate – heavy calcification Total occlusion (< 3 months) Ostial Bifurcation lesion Thrombus present Note: B 1 = characteristic only; B 2 = 2 or more characteristics
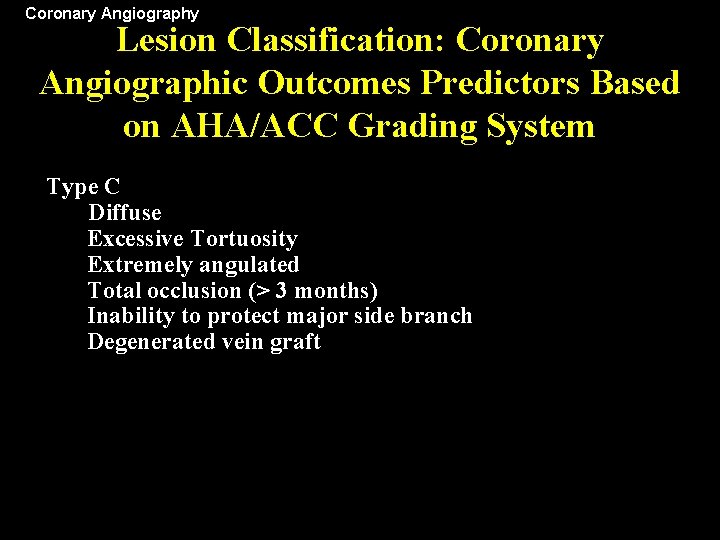
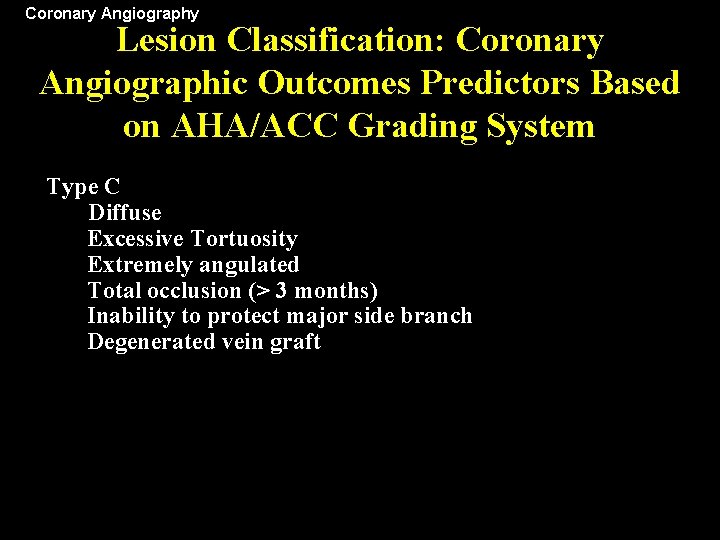
Coronary Angiography Lesion Classification: Coronary Angiographic Outcomes Predictors Based on AHA/ACC Grading System Type C Diffuse Excessive Tortuosity Extremely angulated Total occlusion (> 3 months) Inability to protect major side branch Degenerated vein graft
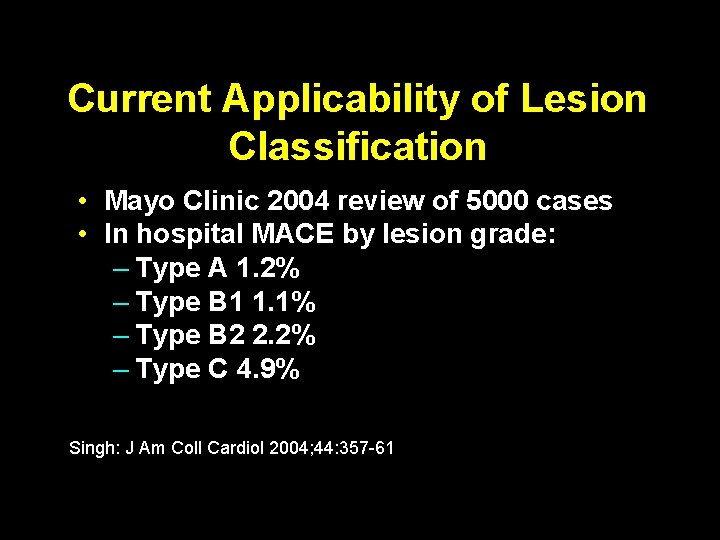
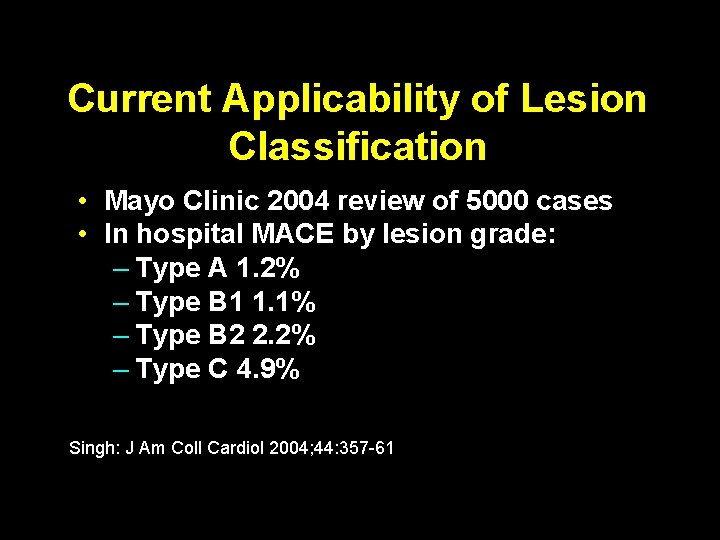
Current Applicability of Lesion Classification • Mayo Clinic 2004 review of 5000 cases • In hospital MACE by lesion grade: – Type A 1. 2% – Type B 1 1. 1% – Type B 2 2. 2% – Type C 4. 9% Singh: J Am Coll Cardiol 2004; 44: 357 -61
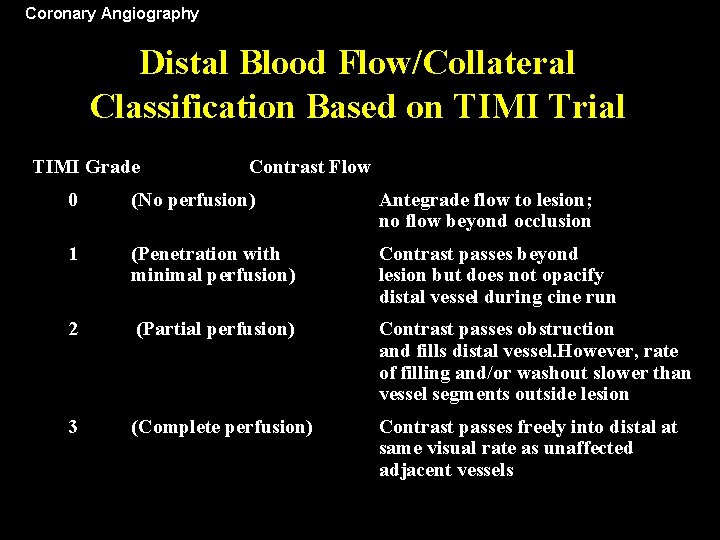
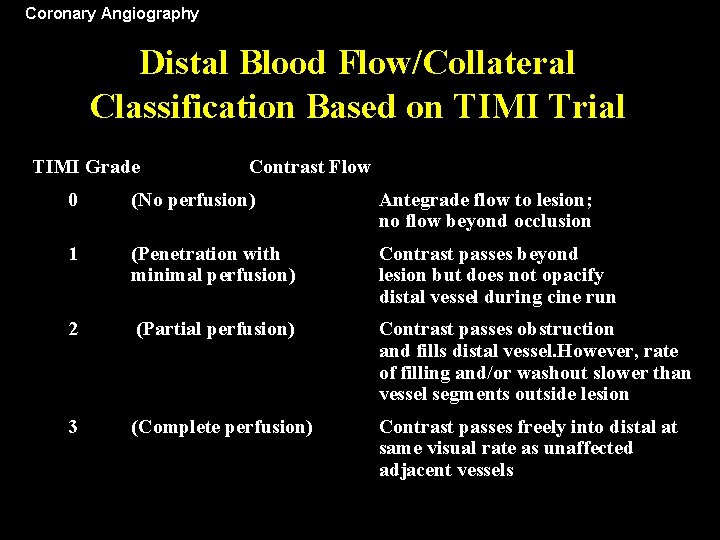
Coronary Angiography Distal Blood Flow/Collateral Classification Based on TIMI Trial TIMI Grade Contrast Flow 0 (No perfusion) Antegrade flow to lesion; no flow beyond occlusion 1 (Penetration with minimal perfusion) Contrast passes beyond lesion but does not opacify distal vessel during cine run 2 (Partial perfusion) Contrast passes obstruction and fills distal vessel. However, rate of filling and/or washout slower than vessel segments outside lesion 3 (Complete perfusion) Contrast passes freely into distal at same visual rate as unaffected adjacent vessels
Adjunctive Pharmacology
“Necessary” Pharmacology • • • Aspirin Clopidogrel/Prasugrel Anti-ischemic Therapy CHF Management if needed STATINS
General Patient Management • Pharmacology helps stabilize patient • Procedure electively only after patient clinically and hemodynamically stable!
Basic Equipment Use
Role of Guide Catheters • • Inject Contrast. Deliver Coronary Devices. Support Delivery of Devices/wires. Measure Arterial Pressure
Guide Catheters • Shapes – Never the same as diagnostics • Sizes – 6 fr. To 9 fr. The larger the shaft the greater the support. (Manufacturers have been unable to make Guides with internal diameters larger than the outer diameter!) • Types – Judkins, Amplatz, Multi-purpose, Xb • Side holes – Useful for RCA, Caution on Left Coronary (Limit coronary flow and injection)
Guide Catheters • Shapes – Never the same as diagnostics • Sizes – 6 fr. To 9 fr. The larger the shaft the greater the support. (Manufacturers have been unable to make Guides with internal diameters larger than the outer diameter!) • Types – Judkins, Amplatz, Multi-purpose, Xb • Side holes – Useful for RCA, Caution on Left Coronary (Limit coronary flow and injection)
Selection of Guide Catheters • Inside diameter determines the ability to inject contrast once equipment in place. – Solutions: Upsize or completely remove balloon from catheter for final pictures. Use monorail balloon catheters. • 7 fr. or 8 fr. Improves visibility and flexibility using simultaneous or kissing balloons or stents in branch disease. (Monorails reduce size Guide Catheter size required)
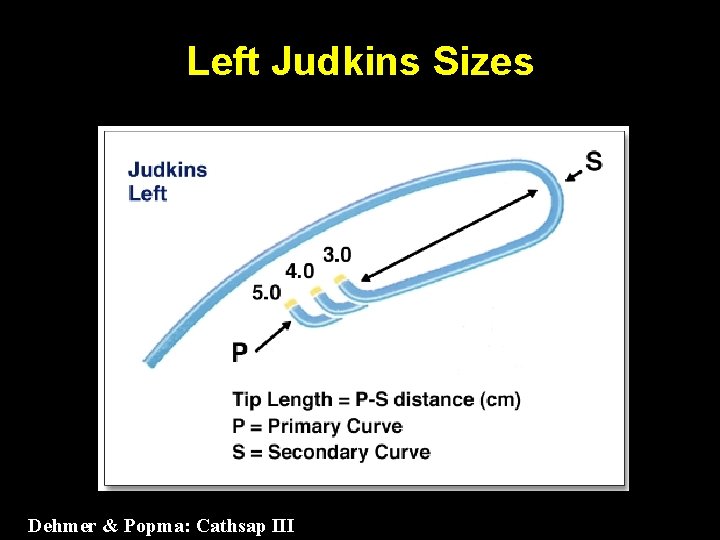
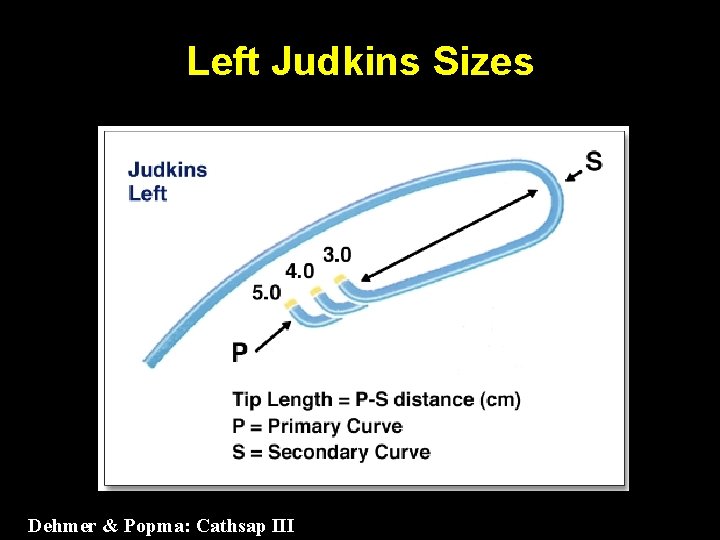
Left Judkins Sizes Dehmer & Popma: Cathsap III
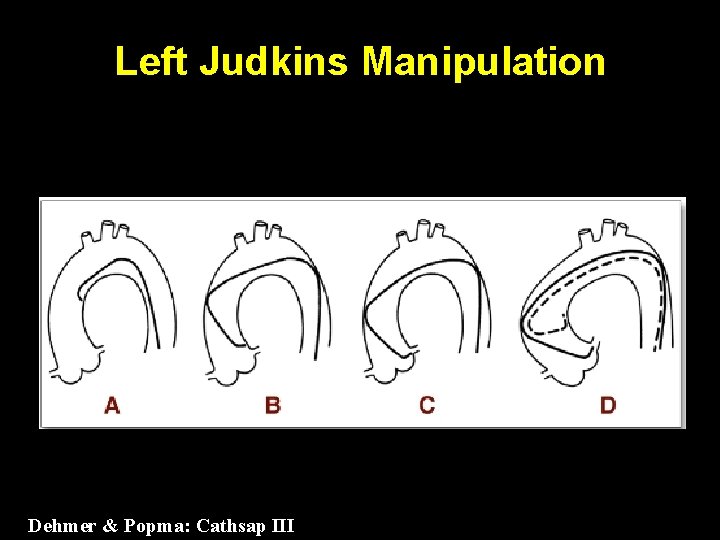
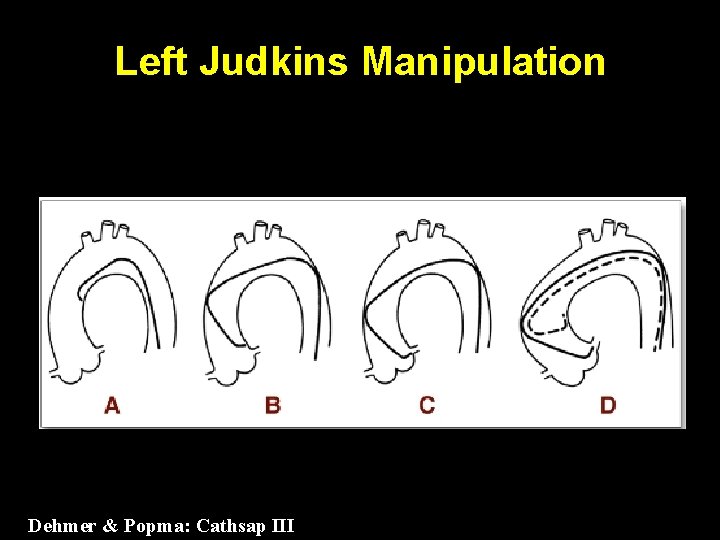
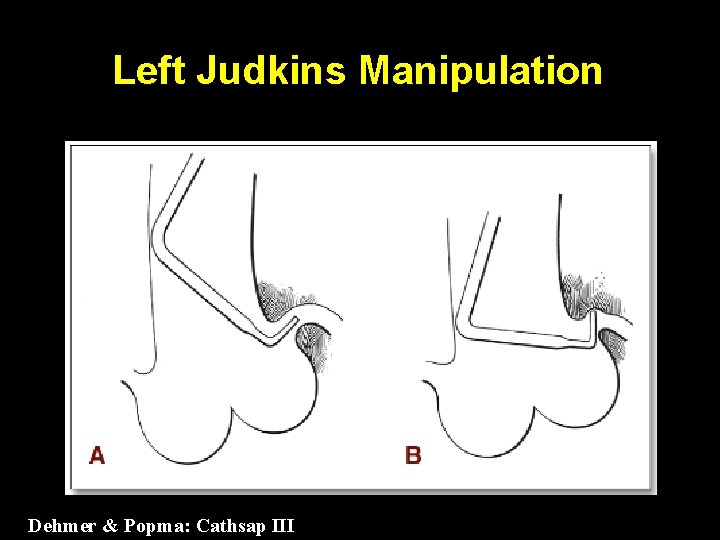
Left Judkins Manipulation Dehmer & Popma: Cathsap III
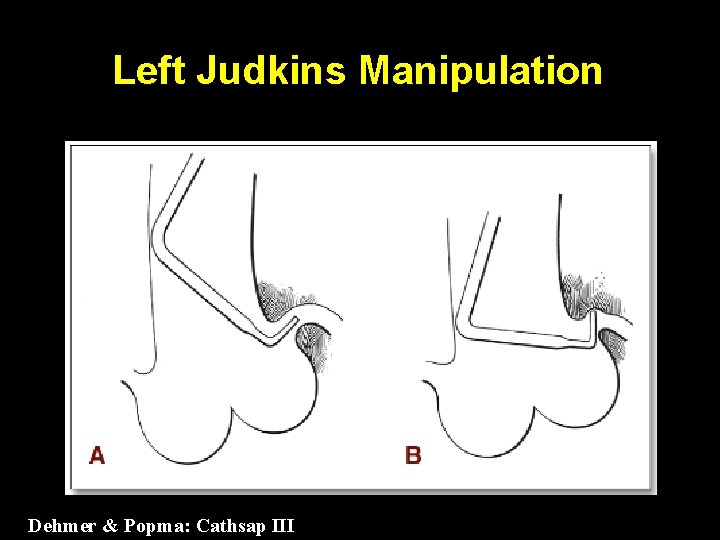
Left Judkins Manipulation Dehmer & Popma: Cathsap III
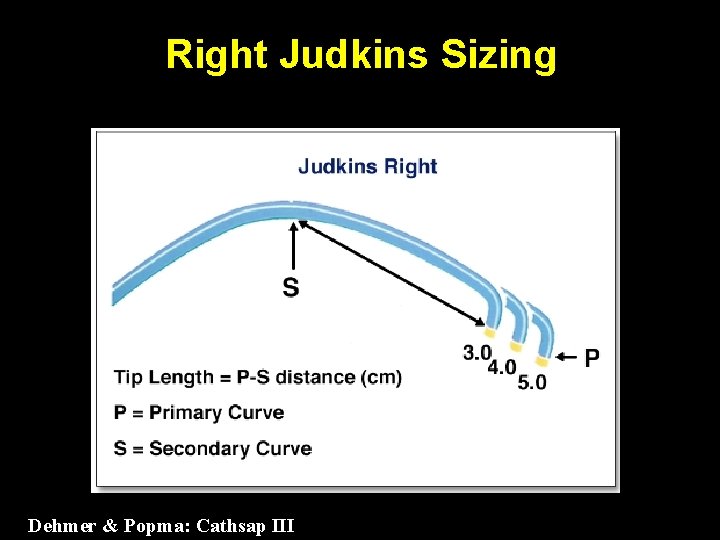
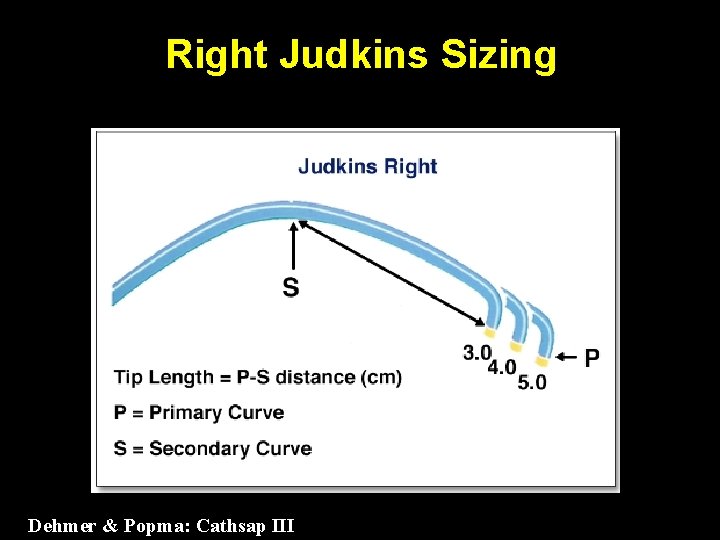
Right Judkins Sizing Dehmer & Popma: Cathsap III
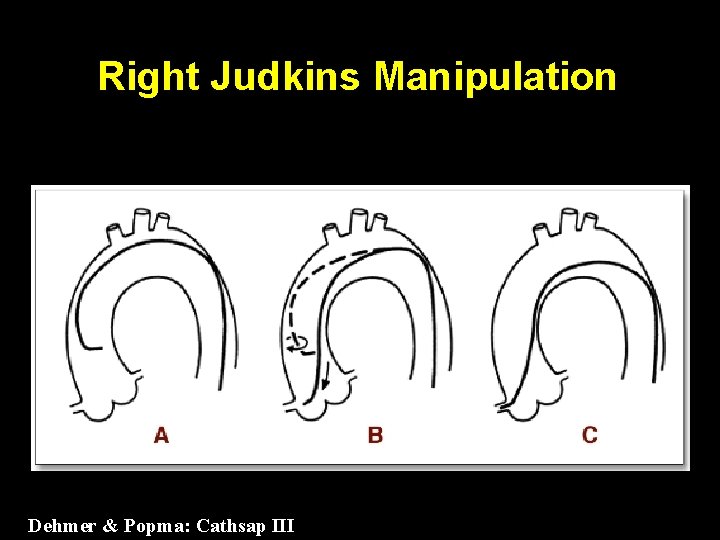
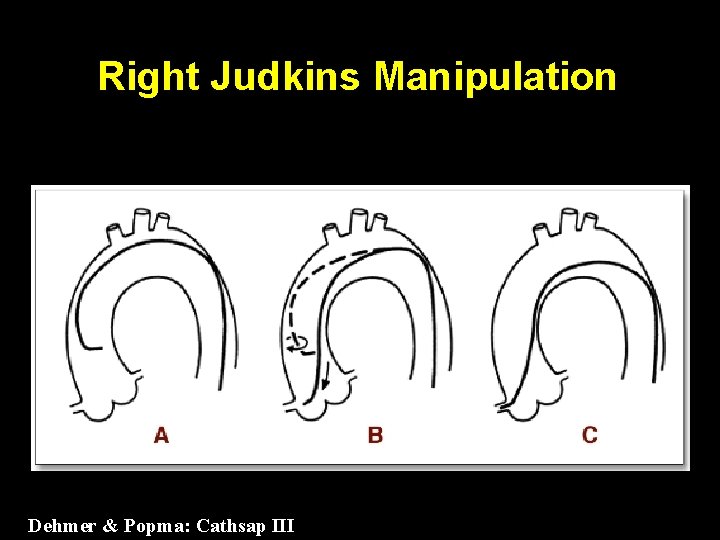
Right Judkins Manipulation Dehmer & Popma: Cathsap III

Right Judkins Manipulation Dehmer & Popma: Cathsap III
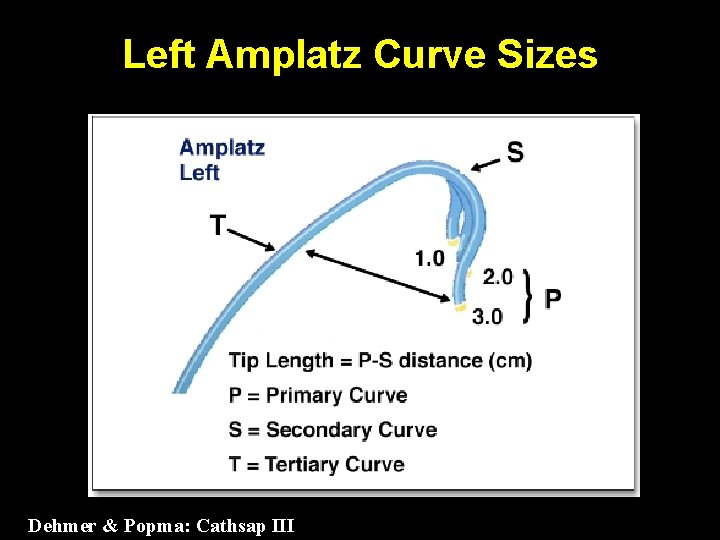
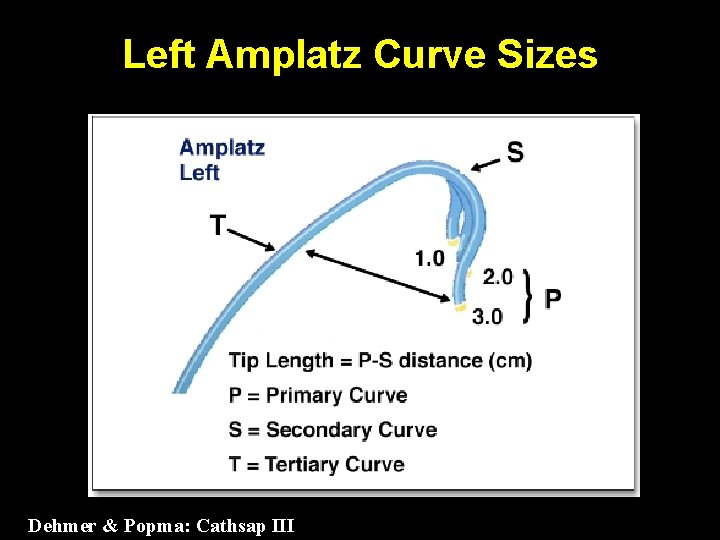
Left Amplatz Curve Sizes Dehmer & Popma: Cathsap III
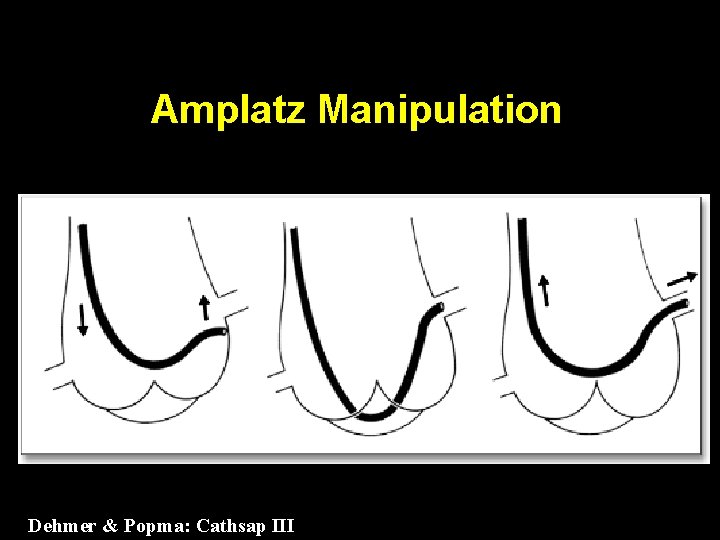
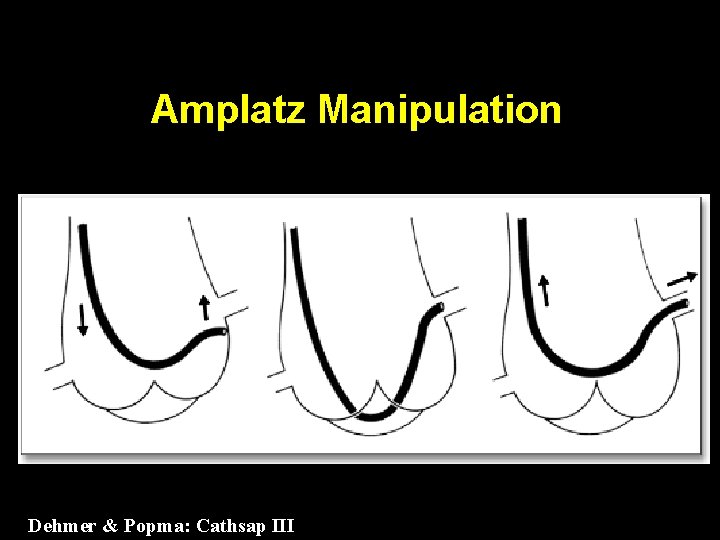
Amplatz Manipulation Dehmer & Popma: Cathsap III

Catheter Pressure Measurement Dehmer & Popma: Cathsap III
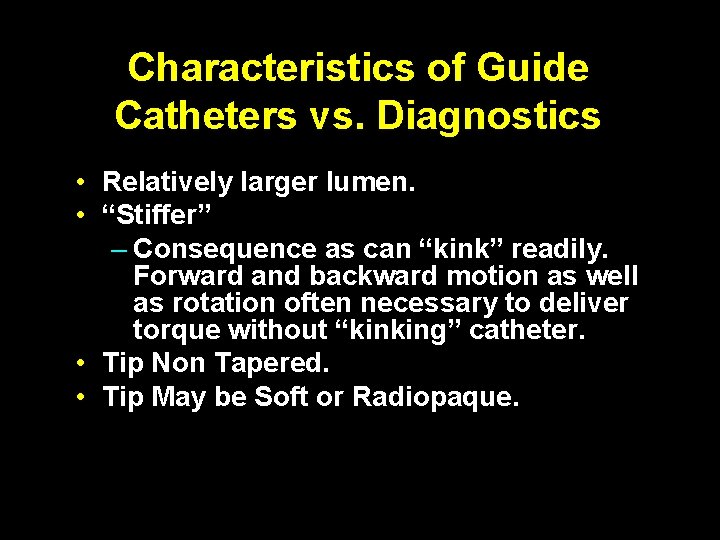
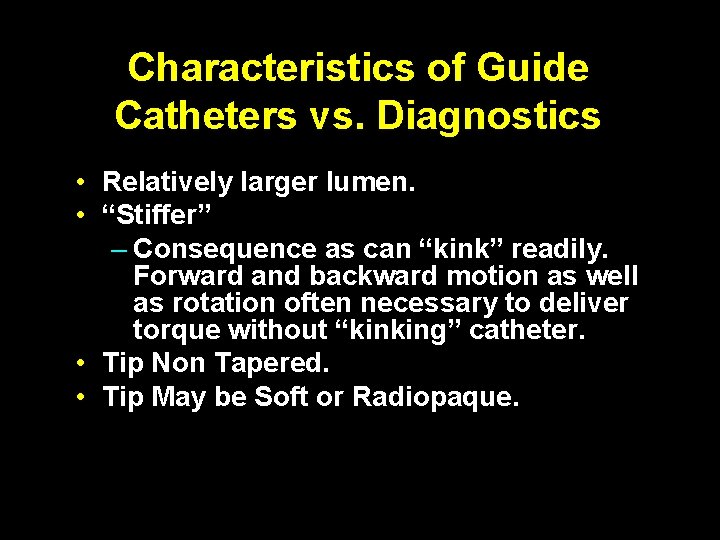
Characteristics of Guide Catheters vs. Diagnostics • Relatively larger lumen. • “Stiffer” – Consequence as can “kink” readily. Forward and backward motion as well as rotation often necessary to deliver torque without “kinking” catheter. • Tip Non Tapered. • Tip May be Soft or Radiopaque.
Guiding Catheters • • • Judkins Amplatz Voda XB Multipurpose Williams Kimny El Gamal Arani Radial Shapes
Guide Catheters • Support: • Left Coronary: – Amplatz, XB, L Judkins – Smaller curve allows one to “Amplatzise” left. • Right Coronary: – Amplatz
Guide Catheters • Removing Amplatz Guide from Left Coronary (to avoid Deep-Throating) • Advance and turn counter clockwise to have fall out into ventricle. • Removing from Right Coronary • Turn counter clockwise and withraw.
Guideswire • Tip characteristics: – Shapes – All shapeable, but some retain shape better. The stiffer the tip the greater push to cross a lesion but the greater the risk of perforation. – Stiffness - Floppy, Intermediate, etc. • Shaft Characteristics: – Support – regular, extra support, etc. The greater the support the easier deliverability except in tortuous vessels where stiffness may create friction in the vessel.

Guide Wires • Shaping: • Usual – 30 – 60 degree Hockey Stick configuration. • Circumflex Marginal – “S” bend. • LAD (High Takeoff) Left Judkins configuration.
Guide wires Pearls: – Teflon coated wires increase risk of perforation while they may improve cross ability. Therefore always change out as soon as across lesion to avoid perforation. – High support guide wires may not traverse extreme tortuosity – so may need to cross with low support wire and then exchange. – Wires with graded shaft stiffness transition improves wire passage through tortuosity. – Rotating wire as advanced with balloon/stent backup will improve guide wire steerability and advancement.
Stent Deployment
Stent Deployment • Correct size. • Correct Position. • Complete apposition Before Placing DES be sure no impending surgery
Drug Eluting Stent: Significance of Apposition



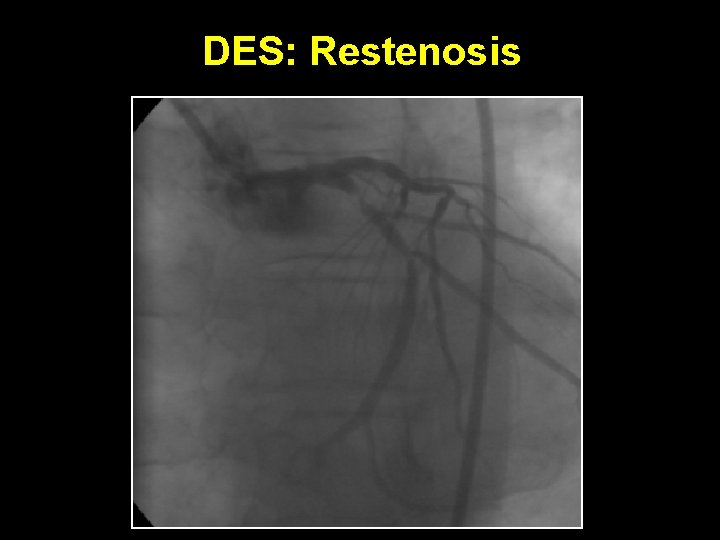
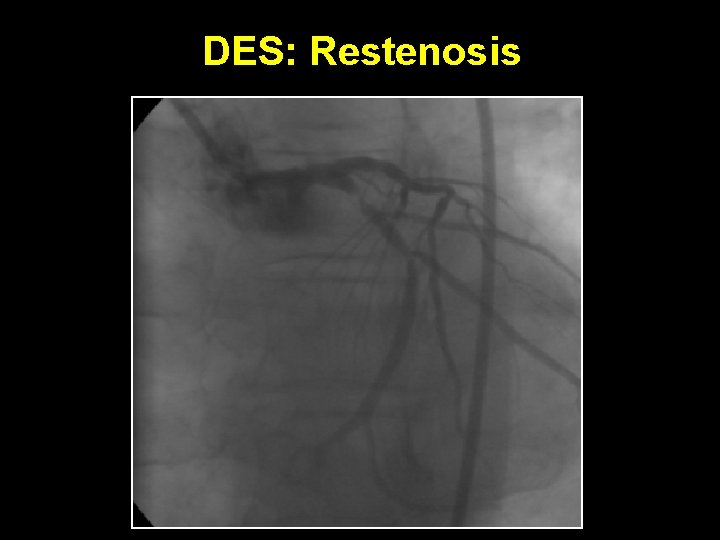
DES: Restenosis
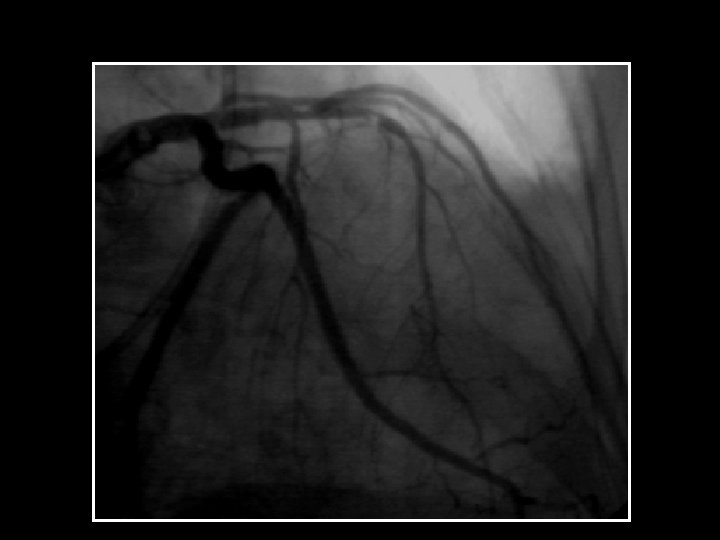
Post Procedure Angiography
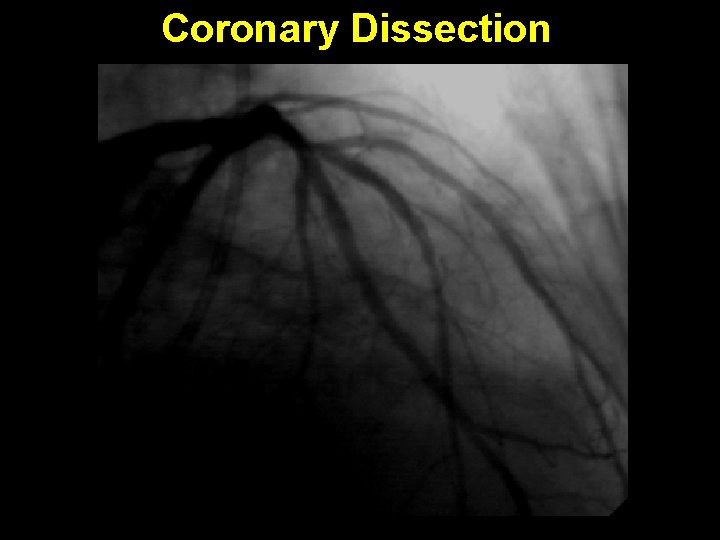
Coronary Dissection
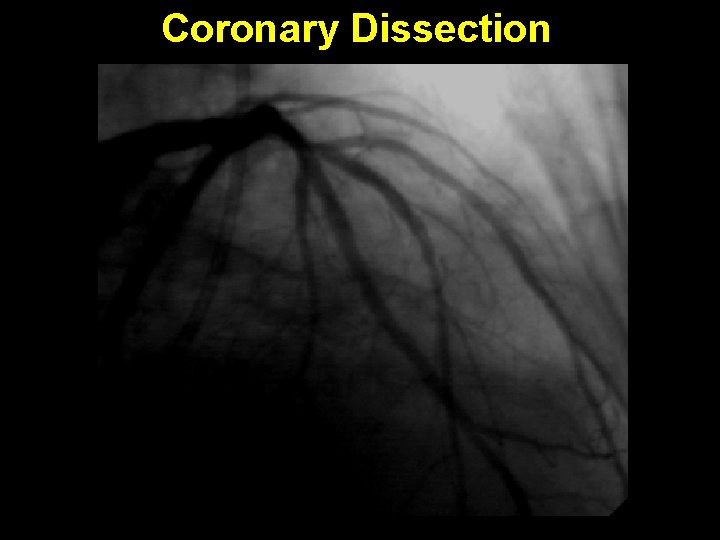
Coronary Dissection

Think first: Use force Last
Compliance • Stent Selection • Follow up
Percutaneous Interventional Techniques: The Basics Conclusions: Careful planning and appropriate use of angiography, pharmacology, basic equipment and procedures techniques can significantly reduce time, radiation and contrast volume while optimizing outcome and maximizing patient safety.

 Voluntary disclosures meaning
Voluntary disclosures meaning Disclosure slides
Disclosure slides Website disclosures under companies act 2013
Website disclosures under companies act 2013 No disclosures slide
No disclosures slide Becomes weakness
Becomes weakness Laboratory findings of megaloblastic anemia
Laboratory findings of megaloblastic anemia Qualitative reduction
Qualitative reduction Seuil d'indifférence calcul
Seuil d'indifférence calcul Mixed(mono+eos+baso)
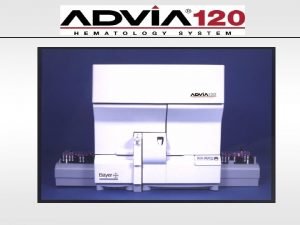
Mixed(mono+eos+baso) Menghitung mcv mch mchc
Menghitung mcv mch mchc Hretic
Hretic Packed cell volume
Packed cell volume Normochromic
Normochromic Bmp includes
Bmp includes Pemeriksaan darah perifer lengkap
Pemeriksaan darah perifer lengkap Rumus mch
Rumus mch Menghitung mcv mch mchc
Menghitung mcv mch mchc Blood cells
Blood cells Colorazione sopravitale
Colorazione sopravitale Fantastic mr fox ginger apple snaps
Fantastic mr fox ginger apple snaps Ginger and the heart
Ginger and the heart Ginger zhang
Ginger zhang Dr ginger hansen
Dr ginger hansen Michael t. stephenson
Michael t. stephenson Ginger for the heart story
Ginger for the heart story Ginger holmes
Ginger holmes Ginger rogers measurements
Ginger rogers measurements Canada dry ginger ale
Canada dry ginger ale George mason graduate housing
George mason graduate housing George washington and thomas jefferson venn diagram
George washington and thomas jefferson venn diagram King george vs george washington
King george vs george washington Brett edwards bath
Brett edwards bath Jd edwards summit
Jd edwards summit Jd edwards summit
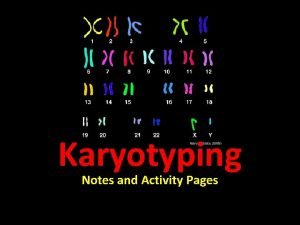
Jd edwards summit Karyotype
Karyotype Dr carla edwards
Dr carla edwards Latonya dilligard edwards
Latonya dilligard edwards 14 kriteria edwards
14 kriteria edwards John edwards vet
John edwards vet Premio deming categorias
Premio deming categorias Stephen a. edwards
Stephen a. edwards Eleanor edwards
Eleanor edwards Trans pecos weathering
Trans pecos weathering Nathan edwards georgetown
Nathan edwards georgetown Jd edwards
Jd edwards Dr stephen edwards
Dr stephen edwards Jonathan edwards apush definition
Jonathan edwards apush definition Dr w edwards deming 14 points
Dr w edwards deming 14 points Great plains texas landforms
Great plains texas landforms Trisomy 13
Trisomy 13 What is deming theory?
What is deming theory? Perbaikan edwards
Perbaikan edwards Cromosoma 13 sindrome
Cromosoma 13 sindrome Deposition
Deposition According to jonathan edwards sermon what is a constant
According to jonathan edwards sermon what is a constant Becky edwards aclu
Becky edwards aclu