Management of cirrhosis Dr Nowlan Selvapatt Consultant Hepatologist






- Slides: 33
Management of cirrhosis Dr Nowlan Selvapatt Consultant Hepatologist Imperial College Healthcare NHS Trust
Overview 1. Understanding the scale of the problem 2. Brief overview of referral pathways 3. Diagnostics in Primary Care 4. Complications of cirrhosis 5. Considerations for Primary Care Management
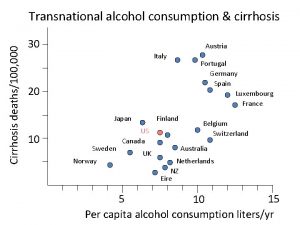
Understanding the scale of the problem
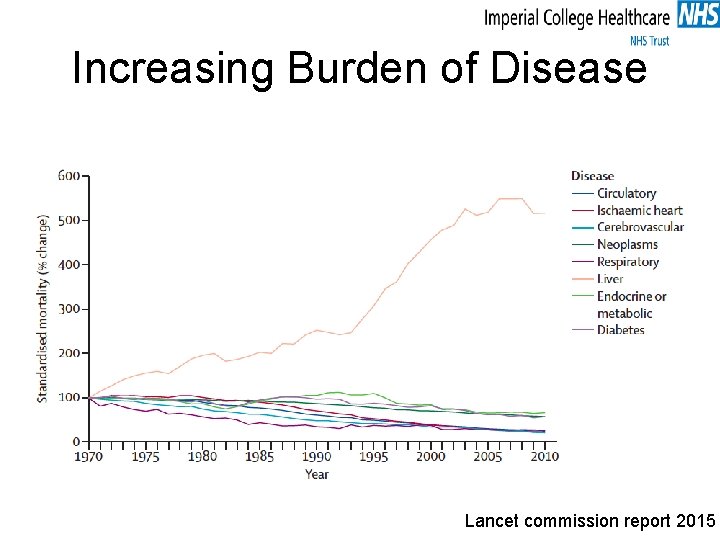
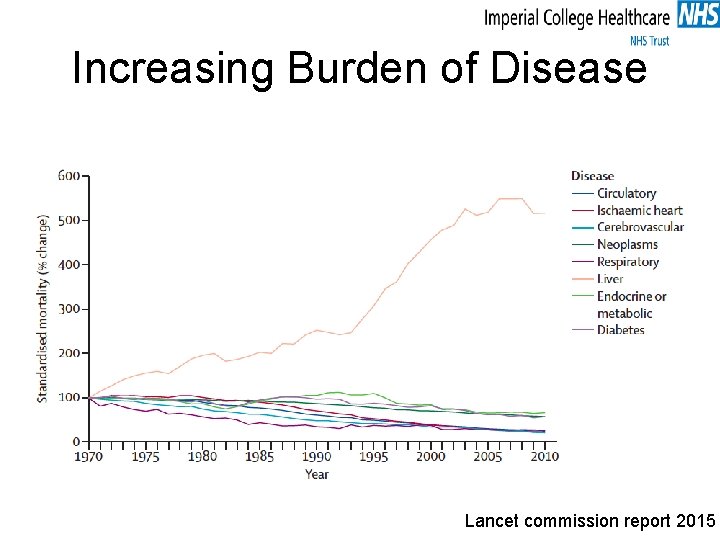
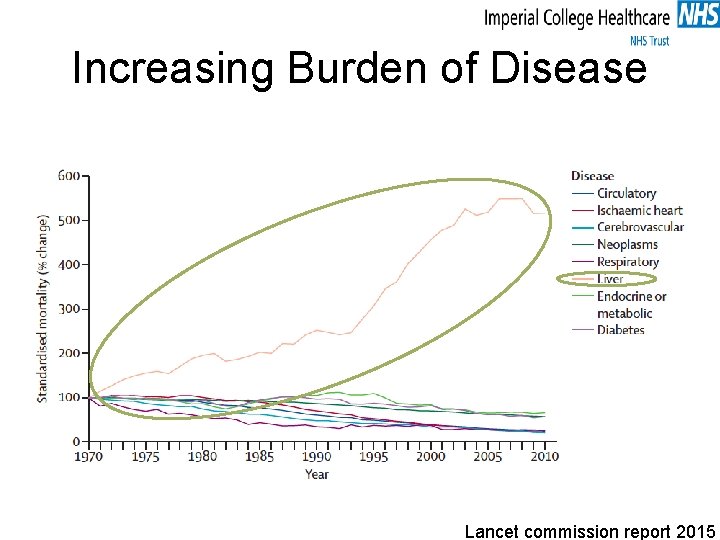
Increasing Burden of Disease Lancet commission report 2015
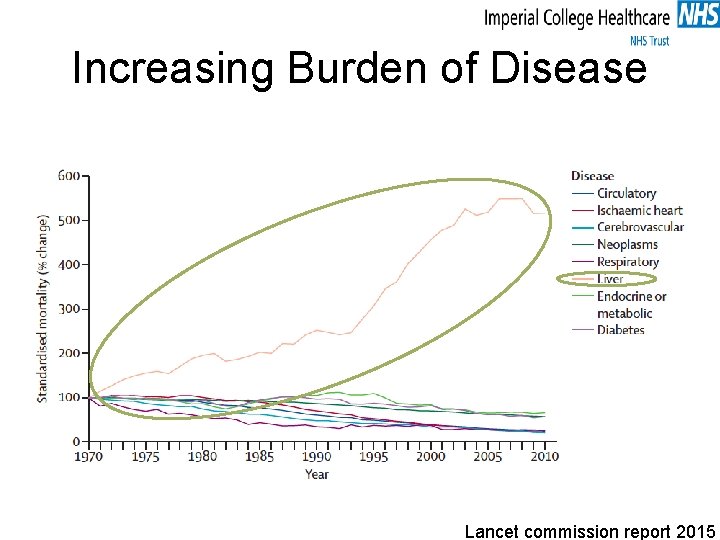
Increasing Burden of Disease Lancet commission report 2015
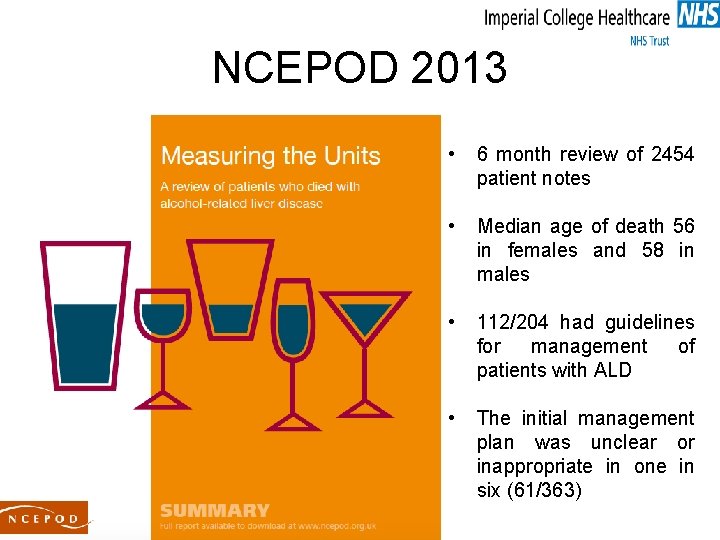
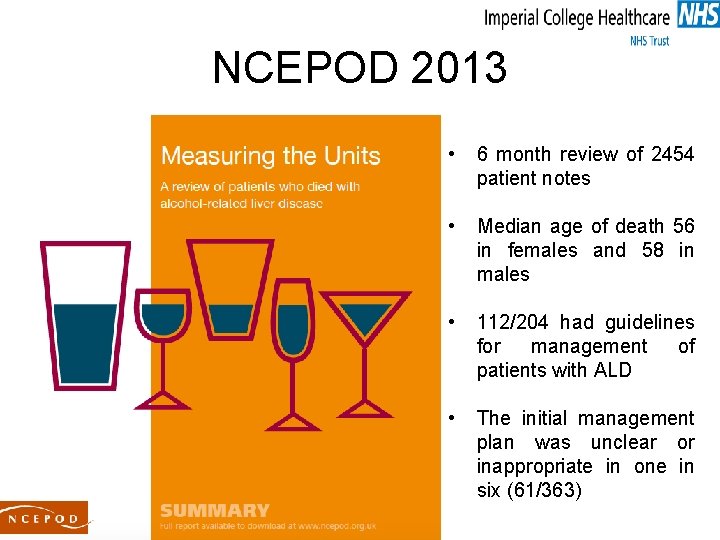
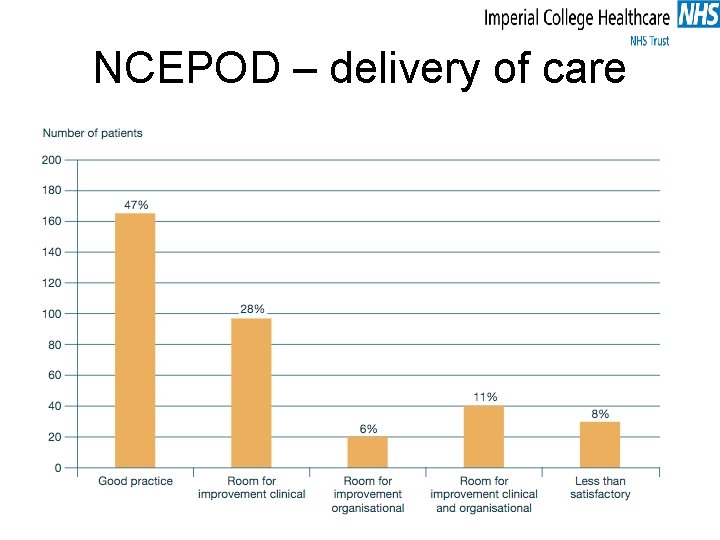
NCEPOD 2013 • 6 month review of 2454 patient notes • Median age of death 56 in females and 58 in males • 112/204 had guidelines for management of patients with ALD • The initial management plan was unclear or inappropriate in one in six (61/363)
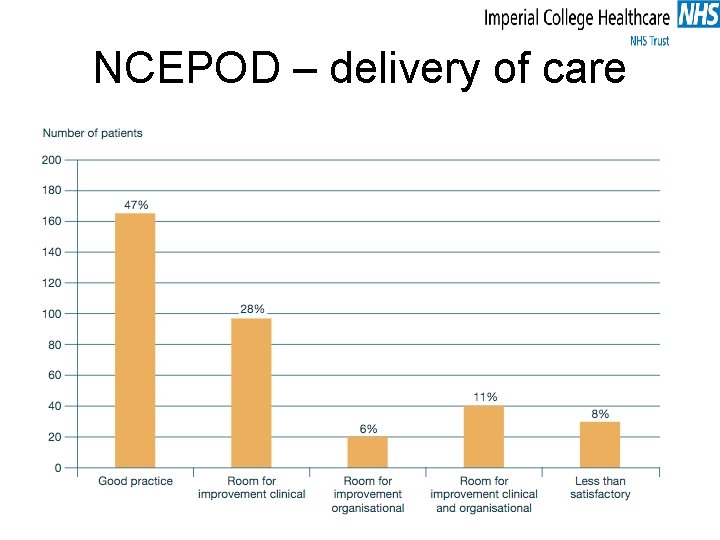
NCEPOD – delivery of care
Referral Pathways


Urgency of referrals Incidental radiological finding with compensated disease VS Decompensated cirrhosis or acute deterioation

Why bother referring?
Diagnostics in primary care
The role of the liver

Understanding components of LFTs AST/ALT Albumin Prothrombin time (bilirubin) Alkaline Phosphatase (GGT) (bilirubin) Platelets
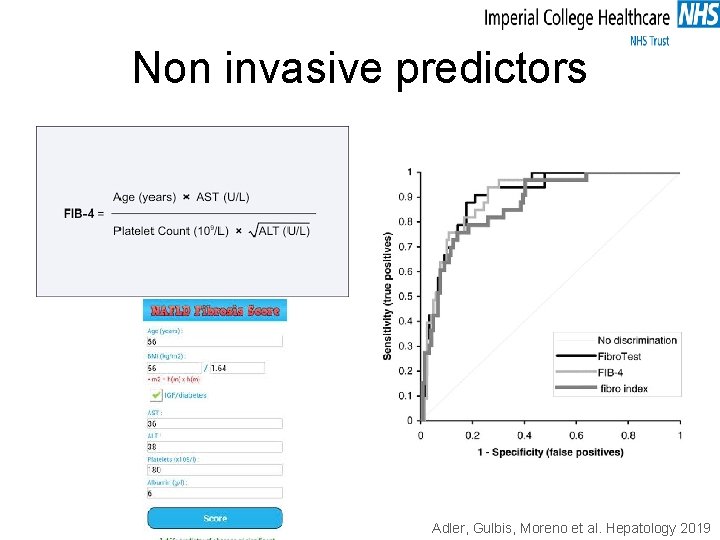
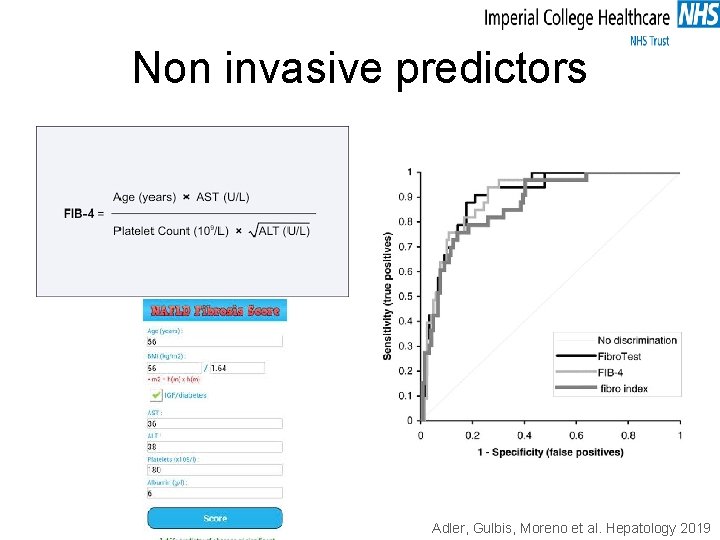
Non invasive predictors Adler, Gulbis, Moreno et al. Hepatology 2019
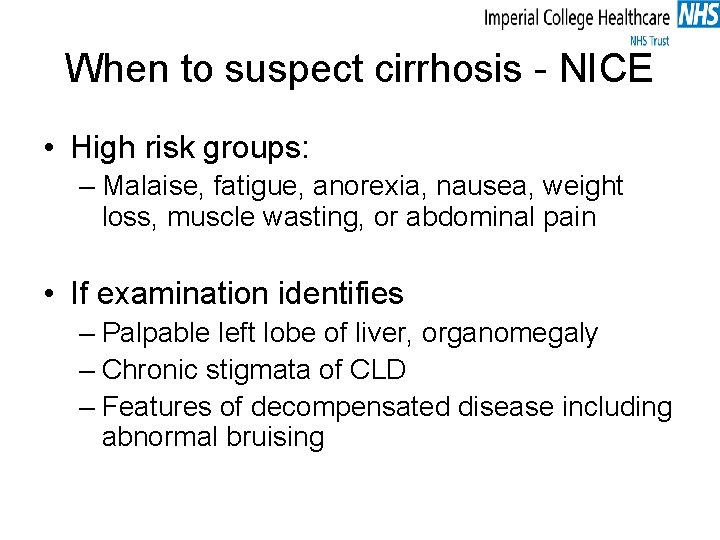
When to suspect cirrhosis - NICE • High risk groups: – Malaise, fatigue, anorexia, nausea, weight loss, muscle wasting, or abdominal pain • If examination identifies – Palpable left lobe of liver, organomegaly – Chronic stigmata of CLD – Features of decompensated disease including abnormal bruising
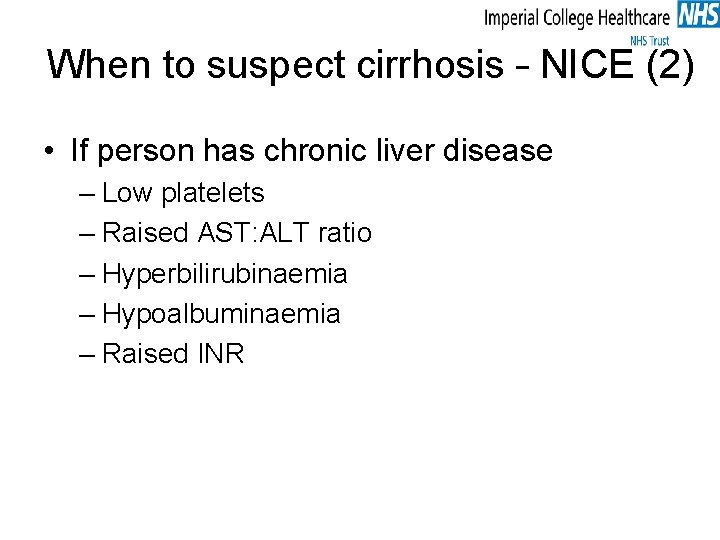
When to suspect cirrhosis – NICE (2) • If person has chronic liver disease – Low platelets – Raised AST: ALT ratio – Hyperbilirubinaemia – Hypoalbuminaemia – Raised INR
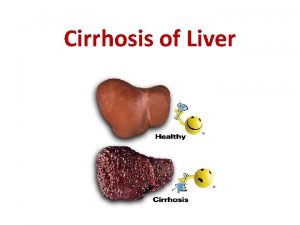
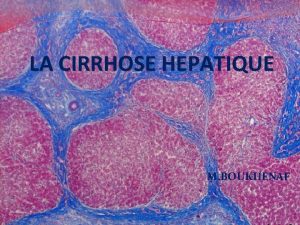
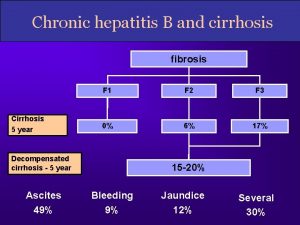
Complications of cirrhosis
Complications of cirrhosis • • • Varices Ascites Encephalopathy Sepsis Sarcopenia/Nutrition/Frailty Extra hepatic organ dysfunction (kidney, heart, adrenal…. )

Sepsis in cirrhosis Bacterial infections in cirrhosis: • leading cause morbidity/mortality in cirrhosis (x 4 MR) Frequency Ø hospitalised cirrhotic patients - 32 -34% Ø hospitalised cirrhotic patients with GI bleeding - 45% Ø vs. hospitalised patients overall 5 -7% • 30 -50% infections remain “culture negative” in cirrhosis Ø SIRS in cirrhosis is atypical *Bajaj et al; Hepatology ’ 12 ‘ 14; Verbake et al; Crit Care ‘ 11; Moreau et al, Gastro ‘ 13
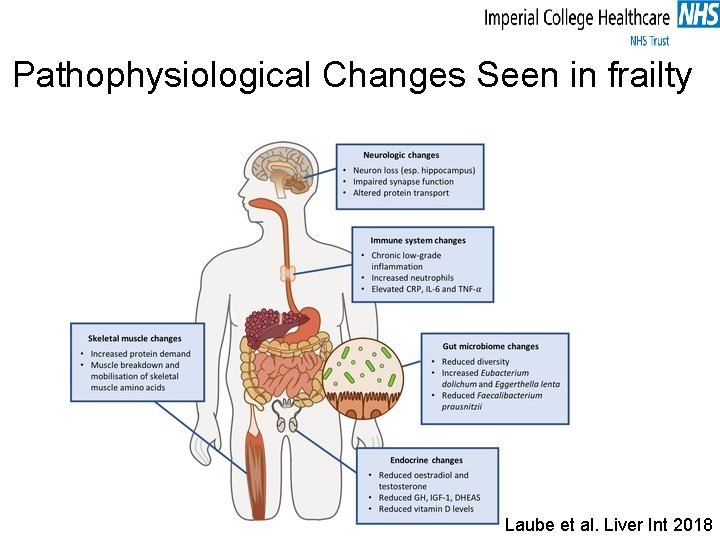
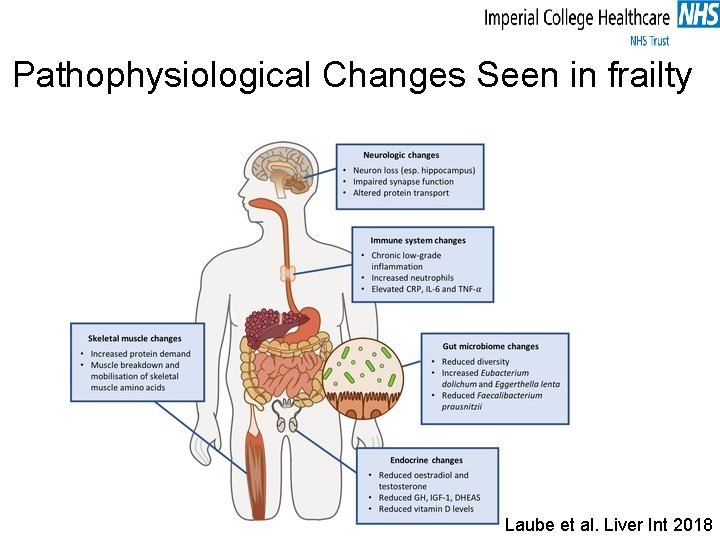
Pathophysiological Changes Seen in frailty Laube et al. Liver Int 2018
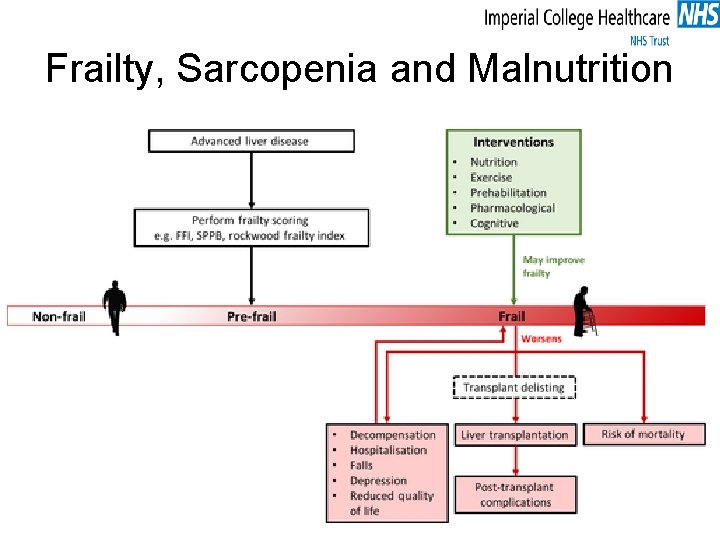
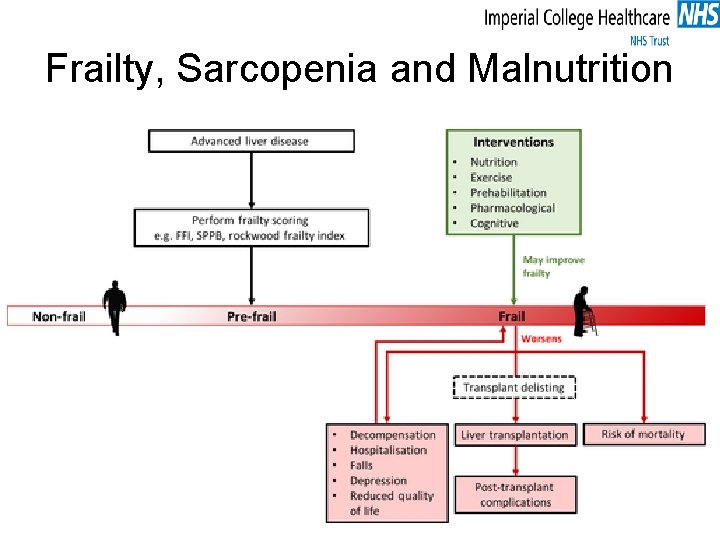
Frailty, Sarcopenia and Malnutrition
MDT Approach to frailty Management approaches to frailty Exercise 1. Aerobic exercise 2. Resistance training 3. Prehabilitation program prior to surgery or liver transplantation Nutrition 1. Adequate caloric intake to meet daily requirements 2. Protein supplementation 3. Late night snacks
MDT Approach to frailty (2) Pharmacological • Consider testosterone supplementation in patients with low serum testosterone levels Cognitive • Cognitive training programs including memory, attention and problem‐solving tasks
Primary Care Management
Managing cirrhosis in Primary Care • Education • Healthy eating and Diet • Alcohol consumption and smoking • Driving • Using Medication Safely • Referral to specialty hepatology services
Education https: //www. britishlivertrust. org. uk/wp-content/uploads/44952 Cirrhosis-DL-booklet-Web-compressed. pdf
Diet https: //www. britishlivertrust. org. uk/wp-content/uploads/44951 -DLD-BLT-A 5 -Booklet-webcompressed. pdf
Prescribing

Take home • Identifying cirrhosis can be difficult, diagnosis is often delayed. • Almost half of people with cirrhosis experience no symptoms of liver disease • Liver function tests may be normal or only mildly abnormal • Some people may present with the less specific features of liver disease, for example, fatigue, itch, or loss of appetite
Take Home (2) • Management of cirrhosis is multisystem – refer to specialist hepatology services early • Primary care has an important role within the MDT • Think: – Education – Nutrition – Medications – DVLA
 Dr nowlan selvapatt
Dr nowlan selvapatt Claire nowlan
Claire nowlan Claire nowlan
Claire nowlan The glass roses analysis
The glass roses analysis Claire nowlan
Claire nowlan Nursing management of cirrhosis of liver
Nursing management of cirrhosis of liver Knowledge management consultant
Knowledge management consultant Dr ian smith injury management consultant
Dr ian smith injury management consultant Green world management consultant & training institute
Green world management consultant & training institute Ovtopodump
Ovtopodump Assertivel
Assertivel Hyperestrinism in cirrhosis
Hyperestrinism in cirrhosis Pathophysiology of cirrhosis of liver
Pathophysiology of cirrhosis of liver Hepatic coma diet
Hepatic coma diet Stage 1 cirrhosis
Stage 1 cirrhosis Complication of liver cirrhosis
Complication of liver cirrhosis Complication of liver cirrhosis
Complication of liver cirrhosis What causes liver cirrhosis
What causes liver cirrhosis What is cirrhosis
What is cirrhosis Symptoms liver cirrhosis
Symptoms liver cirrhosis Micronodular cirrhosis vs macronodular
Micronodular cirrhosis vs macronodular Hepatocirhosis
Hepatocirhosis Hyperestrinism cirrhosis
Hyperestrinism cirrhosis Cirrhosis pes statement
Cirrhosis pes statement Gastrointestinalis
Gastrointestinalis Mitochondrial swelling
Mitochondrial swelling Pes statement for liver cirrhosis
Pes statement for liver cirrhosis Cirrhosis care near woodland
Cirrhosis care near woodland What is biliary cirrhosis
What is biliary cirrhosis Can ct scan miss cirrhosis
Can ct scan miss cirrhosis Cirrhosis
Cirrhosis Cirrhosis
Cirrhosis Easl 2018 decompensated cirrhosis
Easl 2018 decompensated cirrhosis Jojy mathew
Jojy mathew