Supportive care in advanced cirrhosis Making the case








- Slides: 31
Supportive care in advanced cirrhosis — Making the case for collaboration Dr Hazel Woodland Clinical Research Fellow in Hepatology
What to cover? ■ Liver disease in the UK ■ What is advanced chronic liver disease ■ Prognosis ■ Barriers to palliative care ■ Challenges of providing palliative care
“Drink is, at its dark, pickled heart, a sepia pessimist. It draws curtains, pulls up the counterpane. It smothers and softens and smoothes. The bliss of drinking is that it softens and smooths. The bliss of drink is that it's a small death. The difference between you and us, you civilian amateur hobbyist drinkers and us professional, committed indentured alcoholics is that you drink for the lightness, we drink for the darkness. You want to feel good, we want to stop feeling so bad. All addictions become not about nirvana but maintenance. Not reaching for the stars but fixing the roof. ” AA Gill 2016, Pour Me
“Sometimes, drunk, I ruminate on the state of my liver, and think of all the cirrhotics I have watched turn yellow and die. They either bleed out, raving, coughing up and drowning in blood from ruptured oesophageal veins, or, in coma, they slip away, slip blissfully away down the yellowbrick ammonia-scented road to oblivion. ” Dr Samuel Shem 1978, The House of God
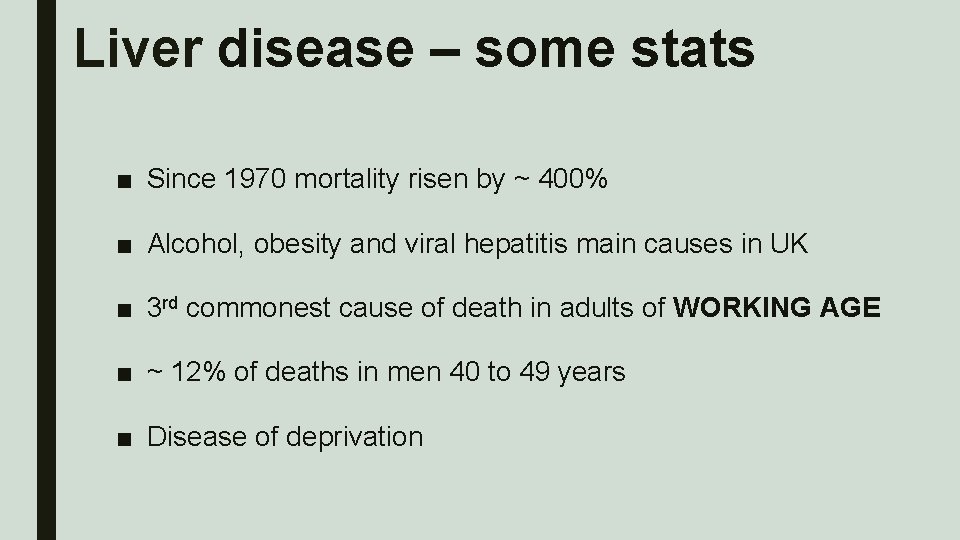
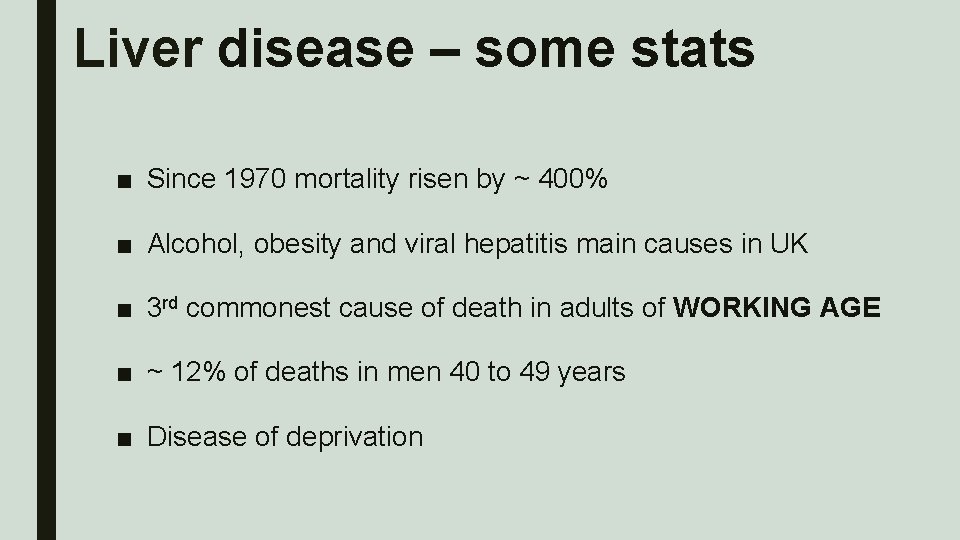
Liver disease – some stats ■ Since 1970 mortality risen by ~ 400% ■ Alcohol, obesity and viral hepatitis main causes in UK ■ 3 rd commonest cause of death in adults of WORKING AGE ■ ~ 12% of deaths in men 40 to 49 years ■ Disease of deprivation
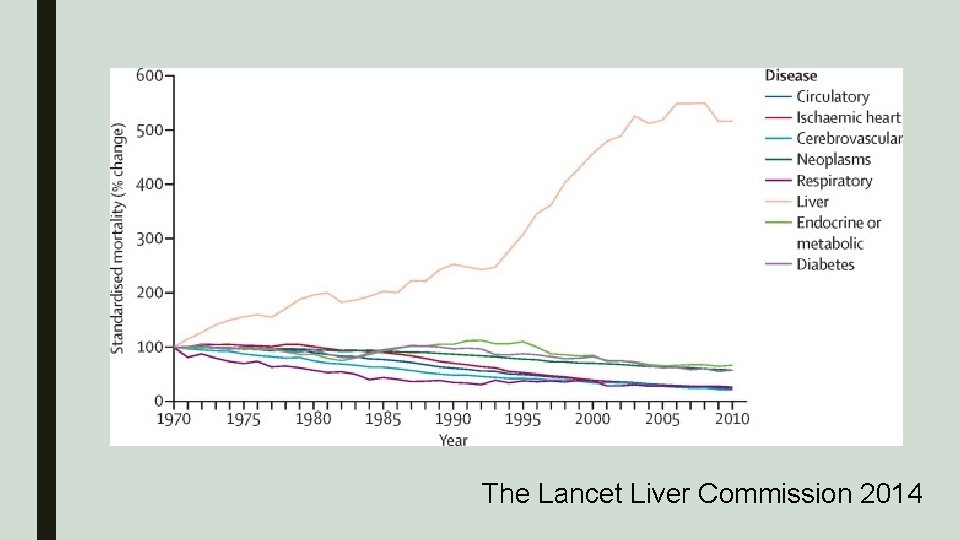
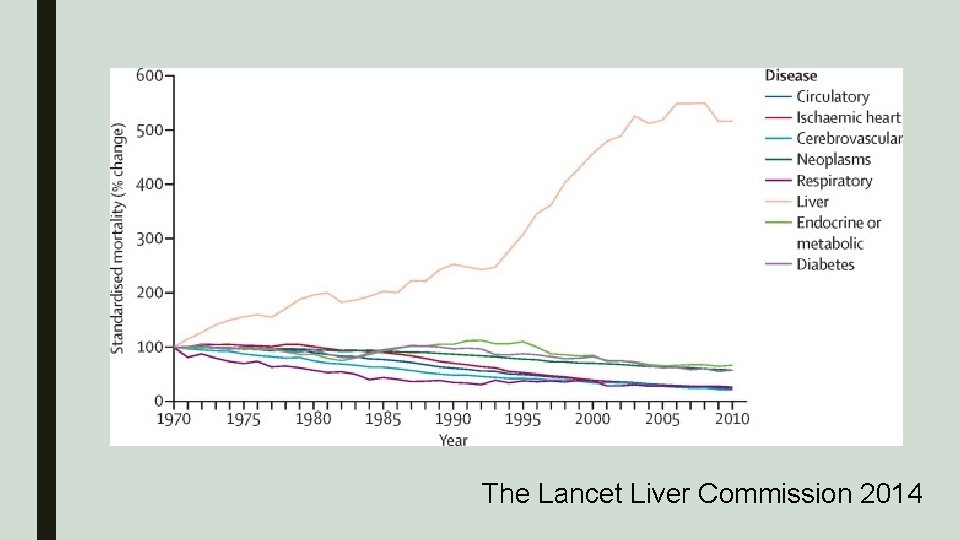
The Lancet Liver Commission 2014
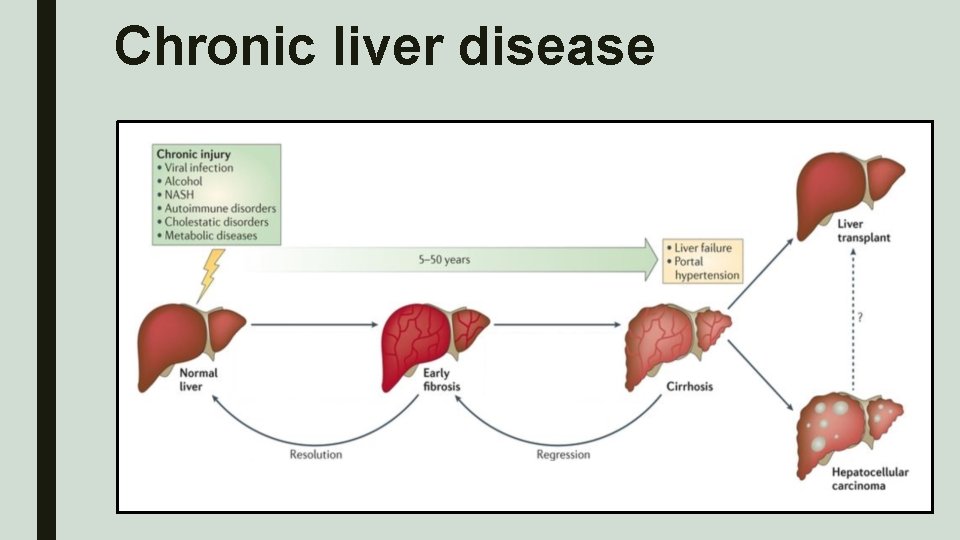
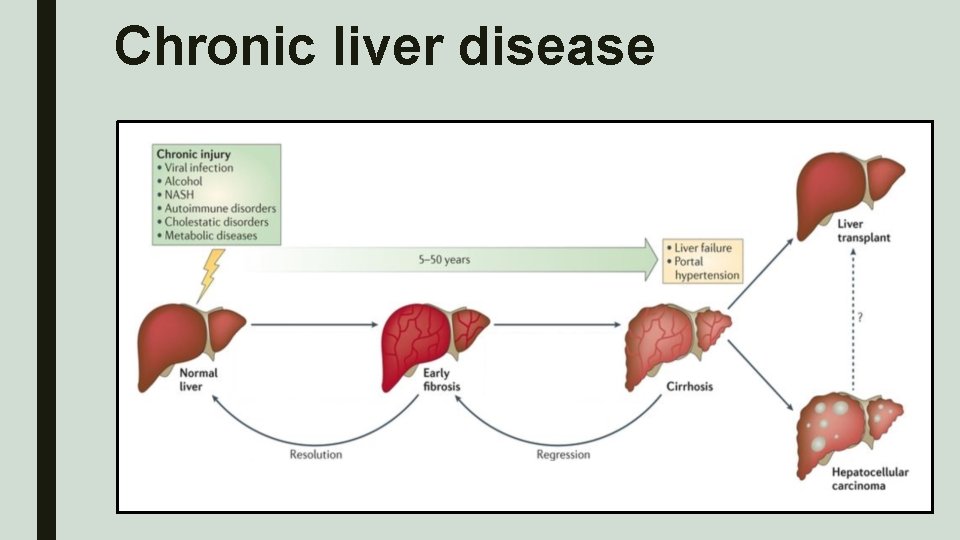
Chronic liver disease

What does CLD look like?
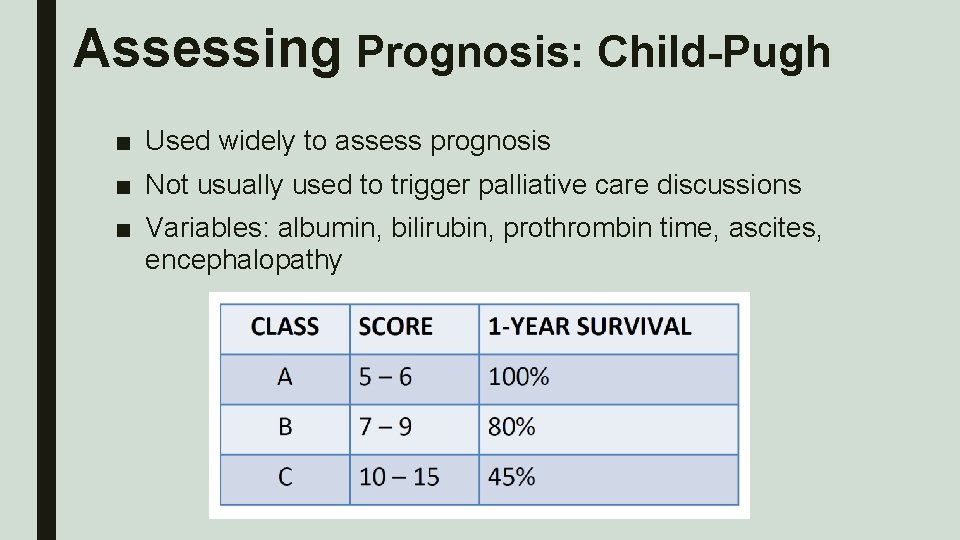
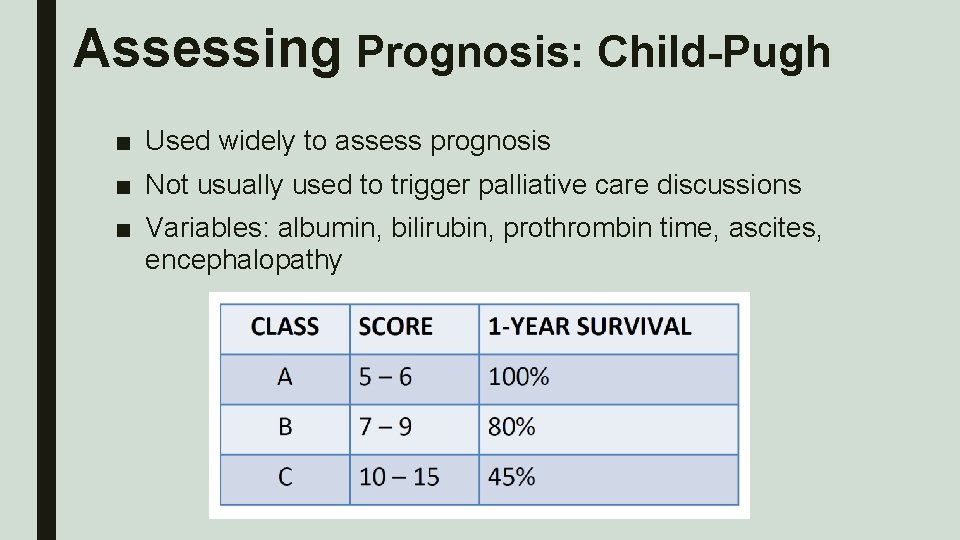
Assessing Prognosis: Child-Pugh ■ Used widely to assess prognosis ■ Not usually used to trigger palliative care discussions ■ Variables: albumin, bilirubin, prothrombin time, ascites, encephalopathy
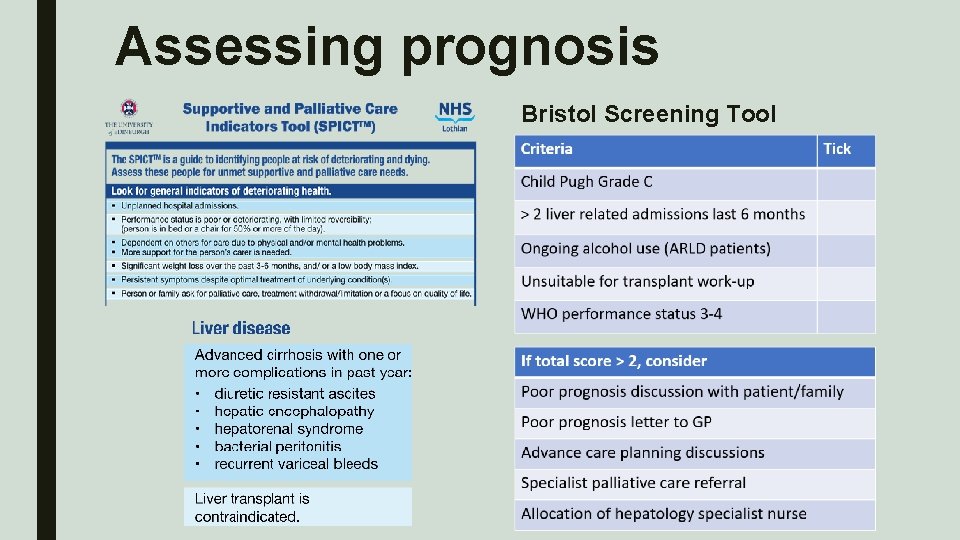
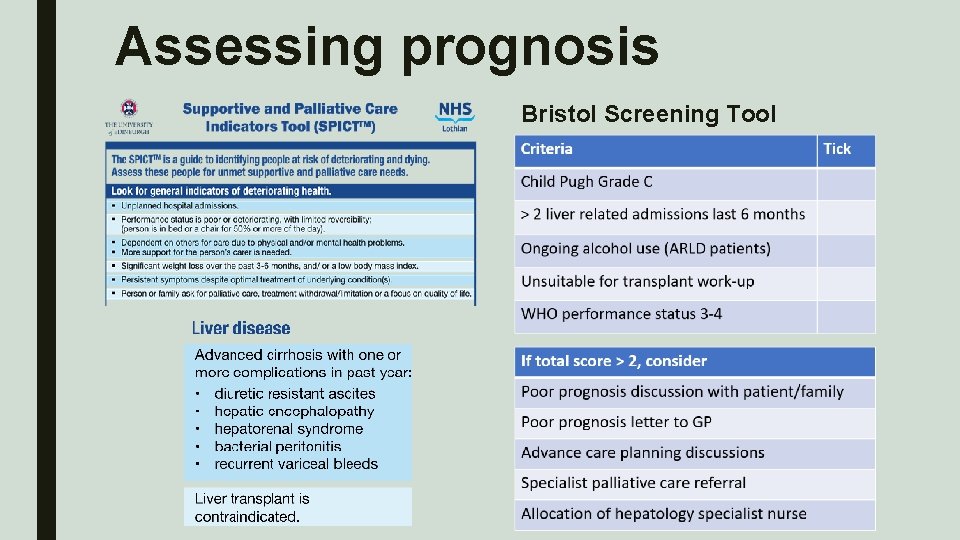
Assessing prognosis Bristol Screening Tool
Barriers to Palliative Care Patient Disease Physician
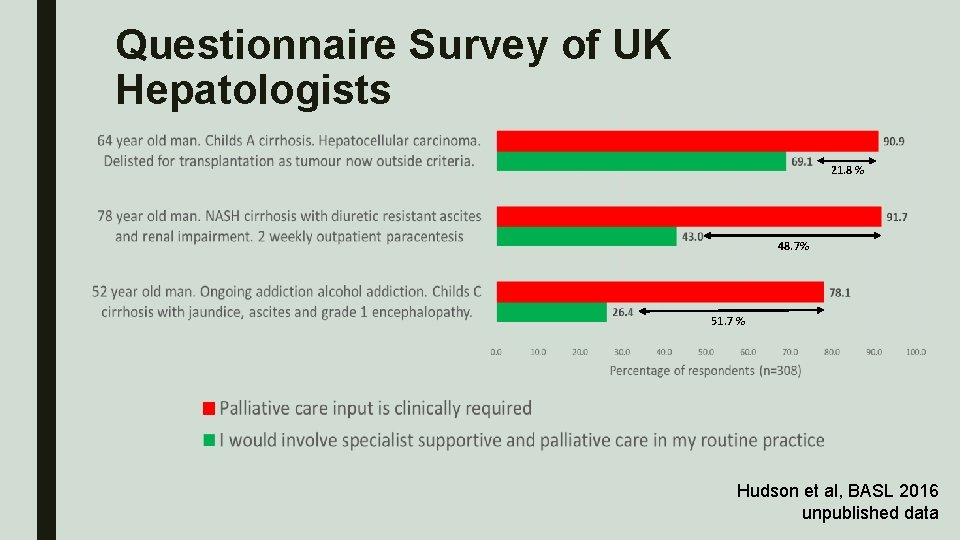
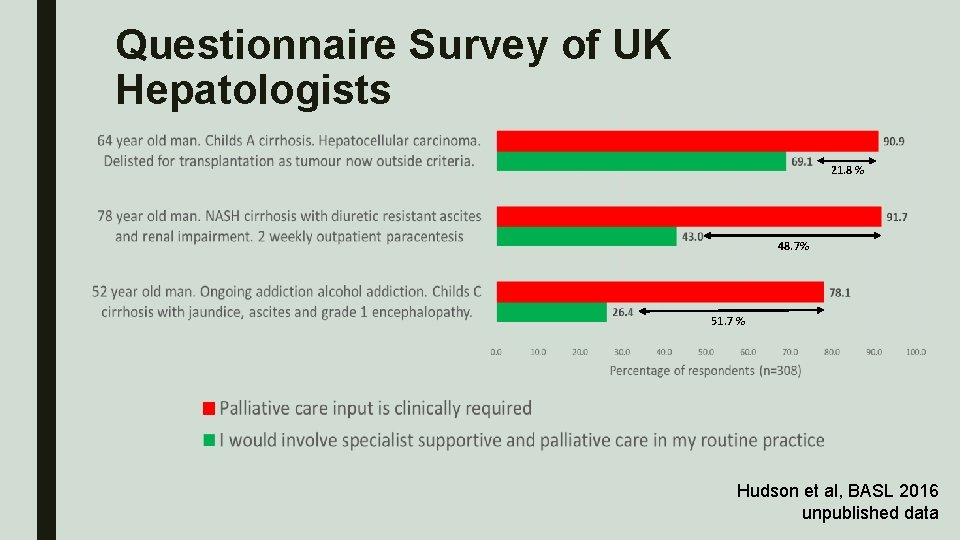
Questionnaire Survey of UK Hepatologists 21. 8 % 48. 7% 51. 7 % Hudson et al, BASL 2016 unpublished data
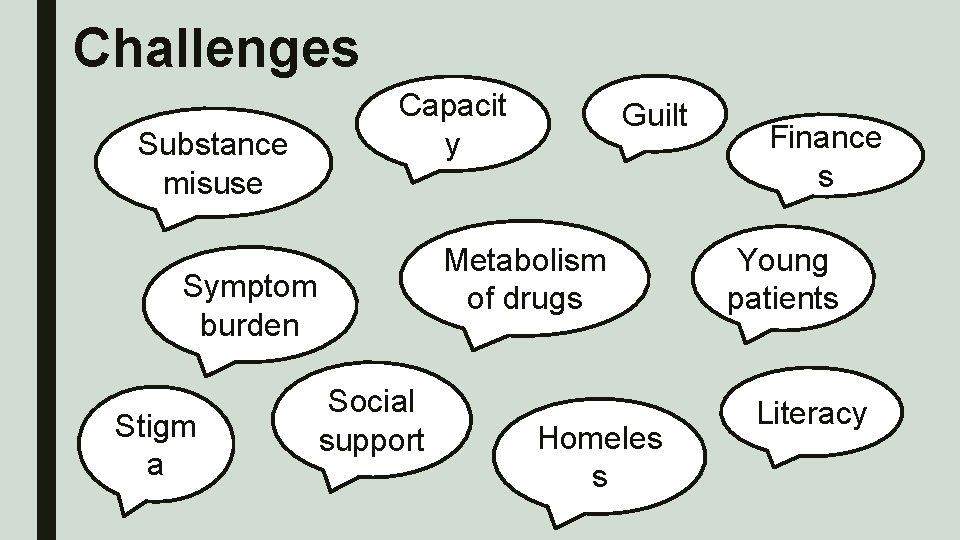
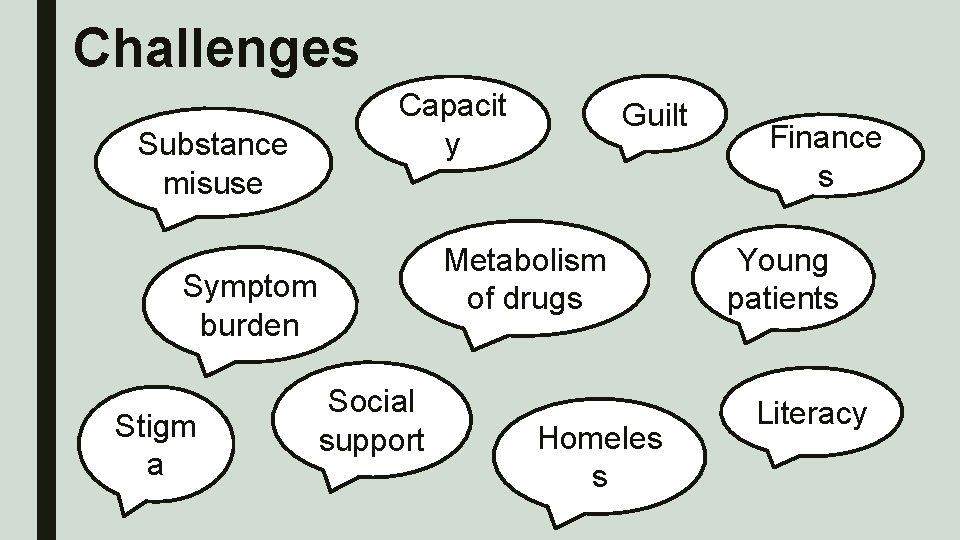
Challenges Capacit y Substance misuse Symptom burden Stigm a Social support Guilt Metabolism of drugs Homeles s Finance s Young patients Literacy
What to do about it?
Outline ■ Gauging unmet need – local experience ■ Integrating earlier palliative care – feasibility study

Local Experience


The Final 24 Hours A&E PC: chest/abdominal Medical pain Referred to Consultant surgeons (diabetes) post -take “Very Medical unwell – refer to registrar medical HDU” CT: no perforation. B B Care taken over 02 04 chest xray 06 08 10 CT scan 12 14 16 18 Medical SHO Clerk-in “frail and unwell” Surgical CT 2 ? perforation CT abdomen requested 20 ITU consultant “multiple organ failure. Physically frail. Prognosis poor. All active HDU measures should be pursued, however ITU admission not in pt’s interest. ” B chest xray 2 2 00 central line MHDU registrar “Drowsy. Unable to answer questions. Fatigued. ” Plan: ITU r/v, nasal high flow O 2, central line, arterial line 02 04 Discussion with family. DNACPR form signed MHDU consultant: “continues to deteriorate. Ask family to attend urgently” B 06 08 B 10 12 Medical registrar: “Monitored asystolic arrest. Patient dead” B chest xray 14 16 18 20 22 00 02 arterial B line Medical registrar: Gastroenterology consultant “main issue is sepsis. Possible UGIB. OGD currently hazardous” “complex tachycardia on monitoring. I suspect that this means the point of terminal decline, amiodarone seems futile but won’t harm the patient. D/W family: likely dying Plan: amiodarone/keep comfortable”

MULTI-SITE FEASIBILITY STUDY INTEGRATING PALLIATIVE CARE INTO THE MANAGEMENT OF PATIENTS WITH END STAGE LIVER DISEASE
Aims of study ■ To assess feasibility of incorporating early supportive care into ongoing active management of patients with advanced CLD ■ To assess impact of early involvement of palliative care specialists on patients’ symptoms, mood and quality of life ■ To assess acceptability of early supportive care input to patients and their carers ■ To create an opportunity for knowledge and skill sharing between specialists in hepatology and palliative care
Inclusion criteria ■ Diagnosis of cirrhosis (any aetiology) with refractory ascites or ■ More than one admission to hospital with episodes of decompensated liver disease (variceal bleed, jaundice, ascites, reversible encephalopathy) in the preceding year and ■ Able to provide fully informed written consent to participate in research
Exclusion criteria ■ Lack of capacity, inability or refusal to provide informed written consent to participate in research ■ Diagnosis of hepatocellular carcinoma or any other malignancy ■ Hepatic encephalopathy of grade 2 or above (West. Haven criteria)
Intervention ■ 1 hr joint consultation with Hepatologist/Gastroenterologist and a Palliative Medicine Consultant ■ Consultation in a private room ■ Patient asked to complete: – Hospital Anxiety and Depression Scale (HADS) – Integrated Palliative care Outcome Score (IPOS) ■ Carer asked to fill out Carer Experience Questionnaire ■ Consultation template ■ Patients offered written information on advance care planning at time of consultation, if appropriate
Recruitment ■ Patients identified by hepatology/gastroenterology team caring for them (inpatient or outpatient) ■ Information leaflet given ■ Encouraged to invite carer ■ Inpatients: verbal consent sought after 2 days ■ Outpatients: verbal consent is obtained for telephone contact after 1 week
Follow-up ■ Post consultation letter with support details ■ Letter summarising consultation will be sent to GP/usual gastroenterologists ■ Ongoing palliative care input arranged if needed ■ Follow up HADS and IPOS after 2 -4 months ■ Carers again asked to fill out the carer experience questionnaire
Progress ■ Recruitment ■ Reflections from joint consultations ■ Recognition of mutual benefit
Summary ■ Optimal end stage liver disease management: – Recognition of deterioration and triggered by gastro/hepatologists – …who open up conversations – Involving patients and carers – With parallel planning – And transmitting important information to key people – Uncertainty make this difficult… – …but shouldn’t be a reason not to do it – There is value to specialist palliative care expertise in some situations

Discussion Points ■ Whose role is it anyway? ■ The MDT attender – is this unsustainable? Or invaluable?

References (1) ■ NCEPOD. “Measuring the Units”-a review of patients who died with alcoholic related liver disease. National Confidential Enquiry into Patient Outcome and Death (UK); 2013: 1– 25 ■ ISD SMR 01, 11 June 2007 ■ • • • Hudson BE, Ameneshoa K, Gopfert A, et al Integration of palliative and supportive care in the management of advanced liver disease: development and evaluation of a prognostic screening tool Patel, A. A. , Walling, A. M. , May, F. P. et al. Palliative care and healthcare utilization for patients with end stage and supportive care intervention Frontline Gastroenterology 2017; 8: 45 -52 liver disease at end of life. Clin Gastroenterol Hepatol 2017; 15: 1612 -1619 ■ The costs of alcohol use and misuse in Scotland, Scottish Government 2008 Leon, D. A. , Mc. Cambridge, J. Liver cirrhosis mortality rates in Britain from 1950 to 2002: an analysis of routine data. Lancet 2006; 367: 52 -56 Measuring the Units: A Review of Patients who Died with Alcohol Related Liver Disease. NCEPOD 2013 https: //www. ncepod. org. uk/2013 report 1/downloads/Measuring. The. Units_Full. Report. pdf last accessed 11/11/2018 National Survey of Bereaved People (VOICES) England, 2015: https: //www. ons. gov. uk/peoplepopulationandcommunity/healthandsocialcare/healthcaresystem/bulletins/nationals urveyofbereavedpeoplevoices/england 2015 last accessed 10/11/2018 British Association for the Study of the Liver and British Society of Gastroenterology. A time to act: improving liver health and outcomes in liver disease. The National Plan for Liver Services UK, 2009

References (2) ■ Kimbell, B. , Murray, S. , Byrne, H. , Baird, A. , Hayes, P. , Mac. Gilchrist, A. , Finucane, A. , Brookes. Young, P. , O'Carroll, R. , Weir, C. , Kendall, M. & Boyd, K. 8 Mar 2018 In : Palliative Medicine. p. 1 -11 Palliative care for people with advanced liver disease: a feasibility trial of a supportive care liver nurse specialist ■ Kimbell, B, Boyd, K, Kendall, M, Iredale, J & Murray, SA 2015, Managing uncertainty in advanced liver disease: a qualitative, multiperspective, serial interview study BMJ Open, vol. 5, no. 11, e 009241. DOI: 10. 1136/bmjopen-2015 -009241 ■ Kimbell, B, Kendall, M, Boyd, K & Murray, S 2015, 'Supportive and palliative care in advanced liver disease: patients' needs and priorities' Journal of Hepatology, vol. 62, no. Suppl_2. ■ New Light on Adult Literacy and Numeracy in Scotland. Scottish Government, 2008 ■ Protosek J, Curry M, Buss M. Integration of Palliative Care in End-Stage Liver Disease and Liver Transplantation. J Pall Med 2014: 17(11) 1271 -1277 ■ Low J, Vickerstaff V, Davis S et al. Palliative care for cirrhosis: a UK survey of health professionals’ perceptions, current practice and future needs