Cirrhosis Dr Gerrard Uy Cirrhosis a histopathologically defined






- Slides: 35
Cirrhosis Dr. Gerrard Uy
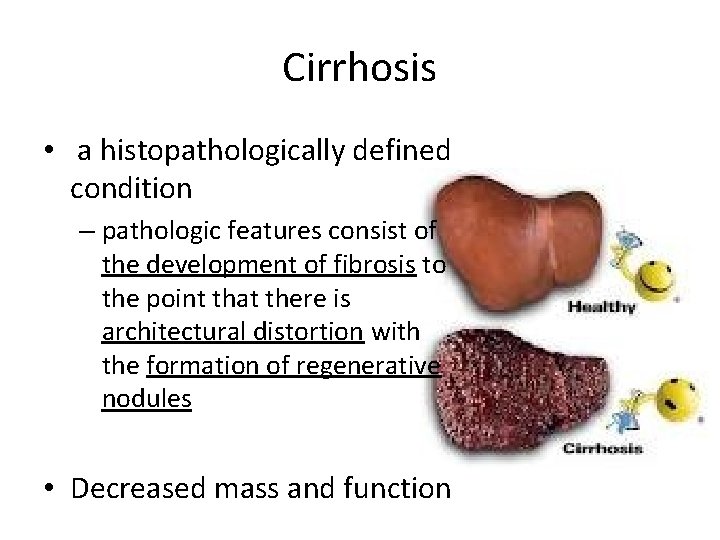
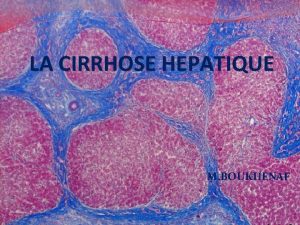
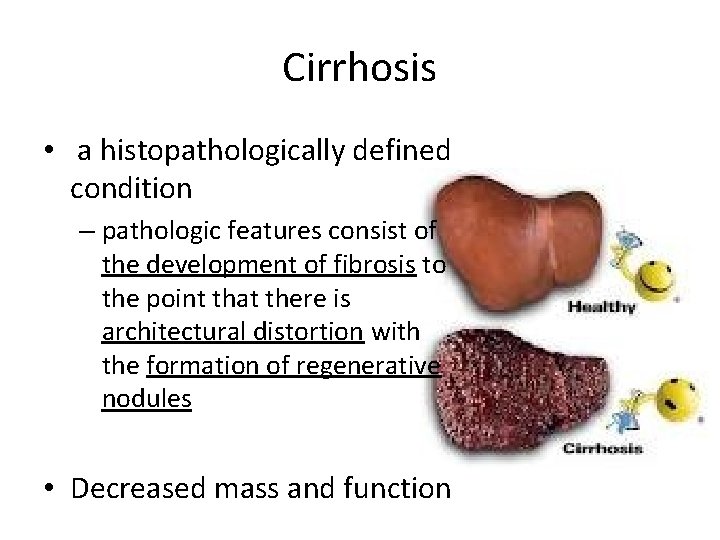
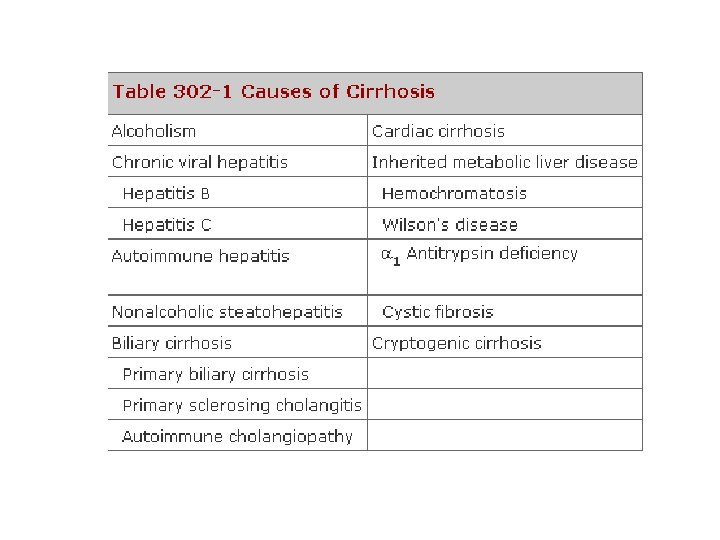
Cirrhosis • a histopathologically defined condition – pathologic features consist of the development of fibrosis to the point that there is architectural distortion with the formation of regenerative nodules • Decreased mass and function
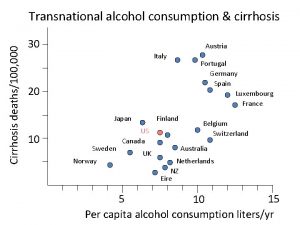
Alcoholic Cirrhosis • Excessive alcohol use can lead to development of: • alcoholic fatty liver • alcoholic hepatitis • alcoholic cirrhosis • Chronic alcohol use can produce fibrosis in the absence of accompanying inflammation
Alcoholic Cirrhosis • Pathogenesis: – Alcohol is the most commonly used drug in US – Ethanol is mainly absorbed by the small intestine – Three enzyme systems account for metabolism of alcohol in the liver – majority of ethanol oxidation occurs via ADH to form acetaldehyde – acetaldehyde-mediated hepatocyte damage – Hepatocyte loss occurs, and with increased collagen production and deposition – liver contracts and shrinks in size

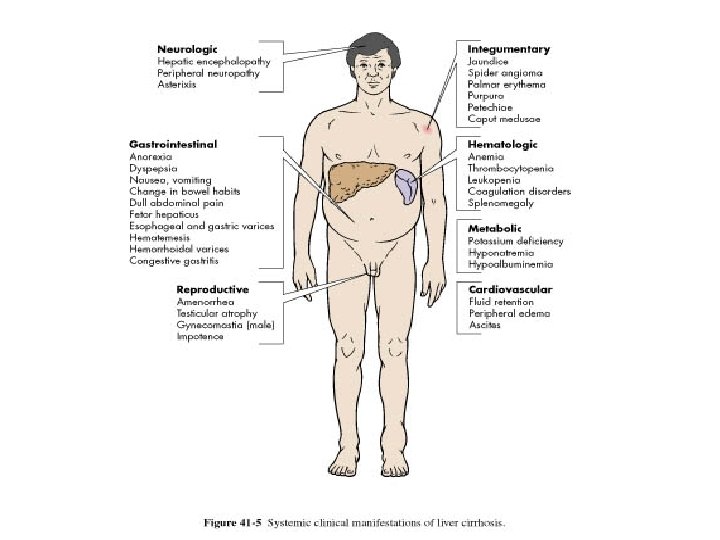
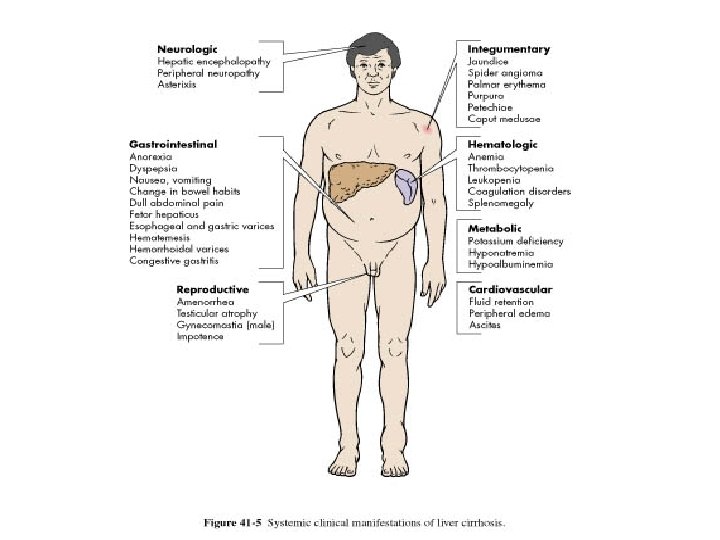
Alcoholic Cirrhosis • Clinical Features: – requires an accurate history regarding both amount and duration of alcohol consumption – nonspecific symptoms such as vague right upper quadrant pain, fever, nausea and vomiting, diarrhea, anorexia, and malaise – more specific complications of chronic liver disease, including ascites, edema, or upper gastrointestinal (GI) hemorrhage – jaundice or encephalopathy

Alcoholic Cirrhosis • Physical Exam: – Hepatomegaly, splenomegaly – scleral icterus, palmar erythema, spider angiomas, parotid gland enlargement, digital clubbing, muscle wasting, or the development of edema and ascites – Men: decreased body hair and gynecomastia – Women: menstrual irregularities
Alcoholic Cirrhosis • Lab tests: – may be completely normal – early cirrhosis – advanced liver disease: • • Anemia Serum total bilirubin can be normal or elevated Prothrombin times are often prolonged aminotransferases (ALT, AST) are typically elevated

Alcoholic Cirrhosis • Diagnosis: – HISTORY AND PE – Liver biopsy can be helpful to confirm a diagnosis but witheld until abstinence has been maintained for at least 6 months

Alcoholic Cirrhosis • Treatment: – ABSTINENCE - cornerstone of therapy – good nutrition and long-term medical supervision – Glucocorticoids – if no infection – Acetaminophen use is often discouraged
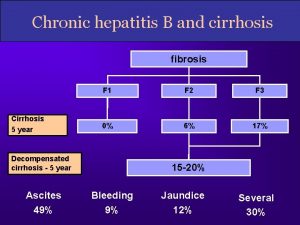
Cirrhosis due to Hep B and Hep C • hepatitis C virus (HCV) – approximately 80% develop chronic hepatitis C – and of those, about 20– 30% will develop cirrhosis over 20– 30 years – liver is small and shrunken with characteristic features of a mixed micro- and macronodular cirrhosis – inflammatory infiltrate is found in portal areas
Cirrhosis due to Hep B and Hep C • hepatitis B – about 5% develop chronic hepatitis B – and about 20% of those patients will go on to develop cirrhosis – ENDEMIC in southeast asia • up to 15% of the population may be infected having acquired the infection vertically at the time of birth
Cirrhosis due to Hep B and Hep C • CLINICAL FEATURES – can present with the usual symptoms and signs of chronic liver disease – Fatigue, malaise, vague right upper quadrant pain, and laboratory abnormalities – including quantitative HCV RNA testing and analysis for HCV genotype – hepatitis B serologies to include HBs. Ag, anti-HBs, HBe. Ag (hepatitis B e antigen), anti-HBe, and quantitative HBV DNA levels
Cirrhosis due to Hep B and Hep C • TREATMENT – Management of complications – beneficial effects of antiviral therapy – chr Hep B – Treatment of patients with cirrhosis due to hepatitis C is a little more difficult because the side effects of pegylated interferon and ribavirin – if it is successful, the benefit is great and disease progression is reduced
Biliary Cirrhosis • Depends on the anatomic site of involvement: – Intrahepatic obstruction – Extrahepatic obstruction • Common causes: – Primary biliary cirrhosis – Autoimmune cholangitis – Primary sclerosing cholangitis – Idiopathic adulthood ductopenia
Primary Biliary Cirrhosis • • • 100 -200 individuals per million Strong female preponderance Median age of around 50 years Cause is unknown Characterized by portal inflammation and necrosis of cholangiocytes
Primary Biliary Cirrhosis • Pathology – 4 distinct stages of the disease – Earliest lesion is chronic nonsuppurative destructive cholangitis • Clinical Features – fatigue out of proportion for the severity of the liver disease and age of the patient – Pruritus is seen in 50% of patients
Primary Biliary Cirrhosis • Physical Examination – Jaundice – Complications of chronic liver disease – Features that are unique to PBC • Hyperpigmentation • Xanthelasma • Xanthomata
Primary Biliary Cirrhosis • Laboratory Findings – Elevated GGT and ALP – Mildy elevated SGPT and SGOT – Hyperbilirubinemia – Thrombocytopenia – Anemia – leukopenia
Primary Biliary Cirrhosis • Diagnosis – Considered in middle aged women with chronic cholestatic liver enzyme abnormalities – Liver biopsy is most important

Primary Biliary Cirrhosis • Treatment – Ursodeoxycholic acid (UDCA) have been shown to improve both biochemical and histologic features – 13 -15 mg/kg/day – Frequent naps should be encouraged – Antihistamines for pruritus – Liver transplantation is the treatment of choice
Cardiac Cirrhosis • Definition – long-standing right-sided congestive heart failure may develop chronic liver injury and cardiac cirrhosis
Cardiac Cirrhosis • Pathogenesis: – elevated venous pressure transmitted via the inferior vena cava and hepatic veins to the sinusoids of the liver – become dilated and engorged with blood – liver becomes enlarged and swollen, and with long -term passive congestion and relative ischemia due to poor circulation – become necrotic, leading to pericentral fibrosis
Cardiac Cirrhosis • Diagnosis – diagnosis is usually made in someone with clearcut cardiac disease who has an elevated ALP and an enlarged liver
Other Types of Cirrhosis • Hemochromatosis – Inherited disorder of iron metabolism that results in progressive increase in hepatic iron deposition leading to cirrhosis and hepatocellular carcinoma • Wilson’s Disease – Inherited disorder of copper homeostasis leading to increase deposition of copper in the liver
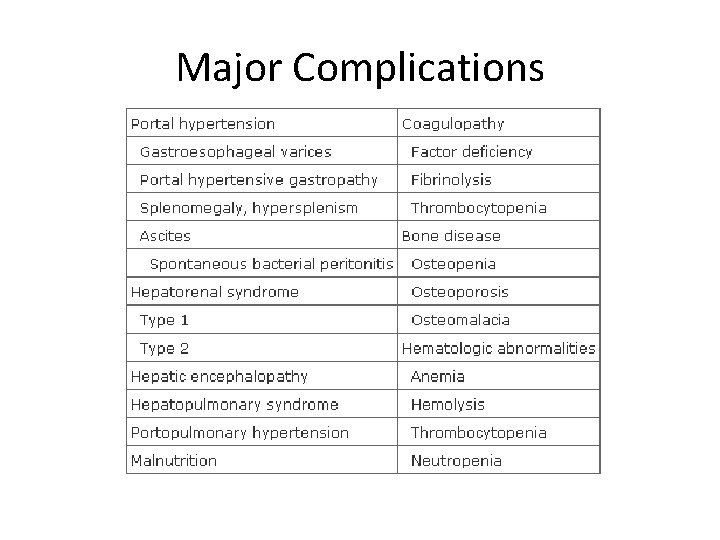
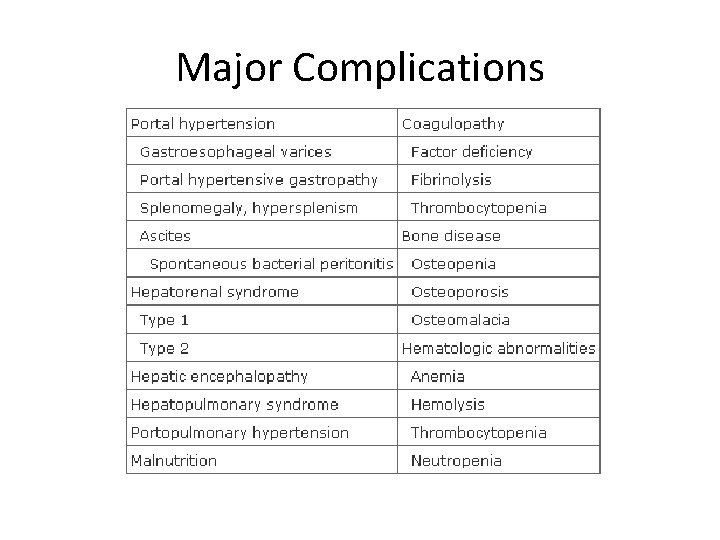
Major Complications
Portal Hypertension • Defined as elevation of the hepatic venous pressure gradient to >5 mmhg • Pathogenesis – Increased intrahepatic resistance to the passage of blood flow through the liver – Increased splanchnic blood flow secondary to vasodilation
Portal Hypertension • Responsible for 2 major complications of cirrhosis – Variceal hemorrhage – ascites • Subcategorized into prehepatic, intrahepatic, and posthepatic • 3 primary complications – Gastroesophageal varices – Ascites – hypersplenism

Spontaneous Bacterial Peritonitis • SBP is a common and severe complication of ascites • Can occur in up to 30% of individuals with severe cirrhosis and ascites • Bacterial translocation is the presumed mechanism for the development of SBP
Spontaneous Bacterial Peritonitis • Most common organisms: – E. coli – Streptococcus viridans – Staphylococcus aureus – Enterococcus sp. • Diagnosis of SBP is made when the fluid sample has an absolute neutrophil count > 250/mm 3 • Cefotaxime is the most commonly used antibiotic
Hepatorenal syndrome • A form of functional renal failure without renal pathology • Occurs in about 10% of patients with advanced cirrhosis • Diagnosis is made in the presence of a large amount of ascites in patients who have a progressive increase in creatinine • Best therapy is liver transplantation
Hepatic Encephalopathy • Defined as an alteration in mental status and cognitive function occurring in the presence of liver failure • Results from accumulation of gut derived neurotoxins • Ammonia levels are typically elevated
Hepatic Encephalopathy • Clinical Features – Changes in mental status occurs within weeks to months – Brain edema is usually present – Usually precipitated by: • • • Hypokalemia Infection Dehydration Increase dietary protein load Electrolyte imbalance
Hepatic Encephalopathy • Treatment – Hydration and correction of electrolyte imbalance – Mainstay of treatment is lactulose – Zinc supplementation can sometimes be helpful
 Paul f gerrard
Paul f gerrard Gerrard
Gerrard It is a collection of well-defined objects.
It is a collection of well-defined objects. Cirrhosis
Cirrhosis Pes statement for cirrhosis
Pes statement for cirrhosis Micronodular cirrhosis vs macronodular
Micronodular cirrhosis vs macronodular Hepatic coma diet
Hepatic coma diet Cirrhosis care near woodland
Cirrhosis care near woodland S.terre hepatic
S.terre hepatic Nursing care plan for liver cirrhosis
Nursing care plan for liver cirrhosis Sindrome hepatorrenal
Sindrome hepatorrenal Hepatocirrosis
Hepatocirrosis Primary biliary cirrhosis
Primary biliary cirrhosis Chronic liver desease
Chronic liver desease Simtuzumab
Simtuzumab What is cirrhosis
What is cirrhosis Hyperestrinism cirrhosis
Hyperestrinism cirrhosis Easl guidelines 2018
Easl guidelines 2018 Liquefactive necrosis
Liquefactive necrosis Complication of liver cirrhosis
Complication of liver cirrhosis Can ct scan miss cirrhosis
Can ct scan miss cirrhosis Hyperestrinism cirrhosis
Hyperestrinism cirrhosis Primary biliary cholangitis skin
Primary biliary cholangitis skin Types of cirrhosis
Types of cirrhosis Pes statement for liver cirrhosis
Pes statement for liver cirrhosis Complication of liver cirrhosis
Complication of liver cirrhosis Recursively defined procedure
Recursively defined procedure Material management definition
Material management definition Sales resistance is defined as a buyer's:
Sales resistance is defined as a buyer's: How is personality defined module 55
How is personality defined module 55 An opsec indicator is defined as:
An opsec indicator is defined as: Sdn introduction
Sdn introduction Elixir definition
Elixir definition Match the correct etvx criteria
Match the correct etvx criteria Customer defined service standards
Customer defined service standards Relationship between maturation and learning
Relationship between maturation and learning