CIRRHOSIS Dr akhondei cirrhosis Cirrhosis is a pathologically








- Slides: 111
CIRRHOSIS Dr akhondei
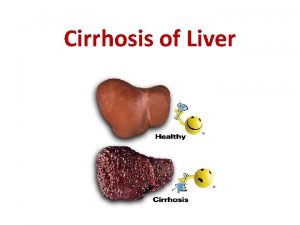
cirrhosis Cirrhosis is a pathologically defined entity that is associated with a spectrum of characteristic clininical manifestation 1 -Irreversible chronic injury of the hepatic parenchyma 2 -Extensive fibrosis 3 -formation of regenerative nodules

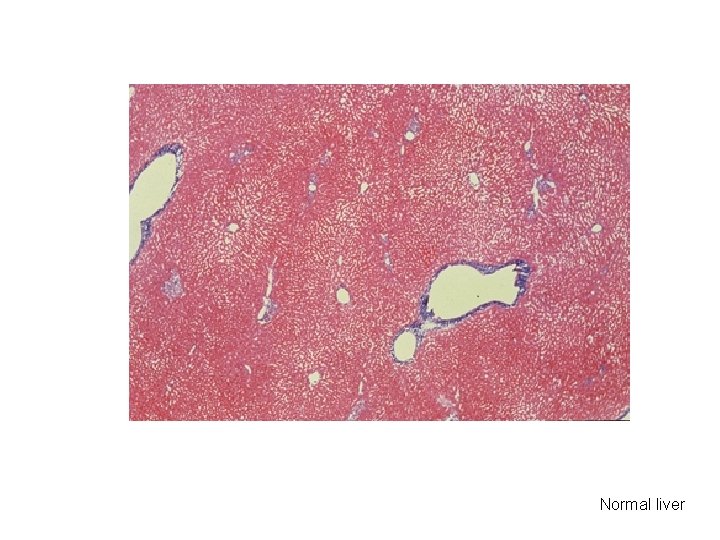
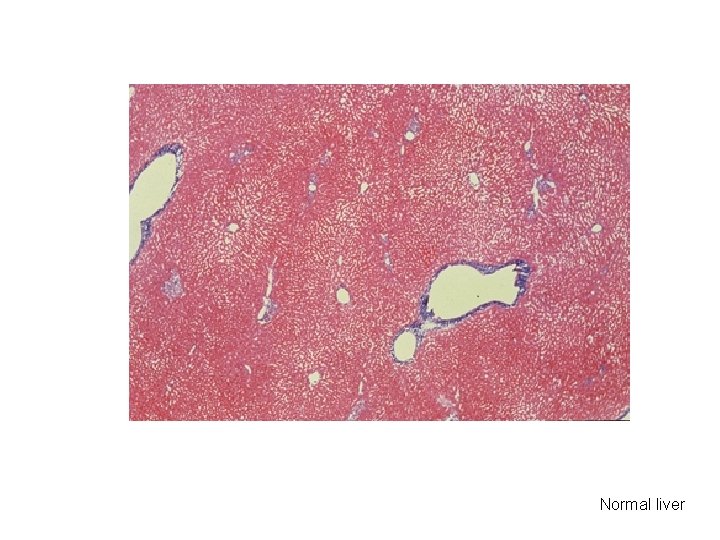
Normal liver


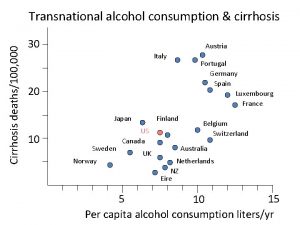
Cirrhosis of the liver is the third leading cause of death in people between the ages of 25 and 65 years, exceeded only by cardiovascular disease and cancer.
The cost of cirrhosis in terms of human suffering, financial burden, and loss of productive life is devastating.
Patients with cirrhosis may present in a variety of ways. Variceal bleeding New onset of ascites Hepatomegaly and/or splenomegaly
Patients with cirrhosis may present in a variety of ways. Incidental Discovery Of Abnormal Laboratory Tests Serum Aminotransferases, Hypoalbuminemia, Prolonged Prothrombin Time, Hrombocytopenia)
Patients with cirrhosis may present in a variety of ways. Detection of the peripheral stigmata of chronic liver disease such as v Jaundice, v Dupuytren's contracture, v Manifestations related to hyperestrogenemia such as o Spider angiomata, o Palmar erythema, o Gynecomastia, and testicular atrophy which may also be related to low testosterone concentrations
Patients with cirrhosis may present in a variety of ways. hepatic encephalopathy or one or more complications or systemic manifestations of hepatocellular carcinoma Some patients never come to clinical attention. In older reviews, cirrhosis was diagnosed at autopsy in up to 30 to 40 percent of patients
Cirrhosis represents the terminal stage of a number of chronic liver diseases including those caused by excessive ethanol consumption Viral hepatitis Drugs and toxins, Vascular Autoimmune Metabolic disorders Cryptogenic. In some cases, no cause can be determined and the cirrhosis is
Early cirrhosis may be asymptomatic and undetectable except by biopsy. However, by the time cirrhosis becomes clinically apparent, hepatic functional reserve is markedly impaired. If liver injury cannot be arrested, the prognosis without intervention is poor
The onset of complications (eg, ascites, encephalopathy, variceal hemorrhage) indicates a more advanced stage of disease and a poorer prognosis, with median survival of about 5 years or less.
CIRRHOSIS & PORTAL HYPERTENSION
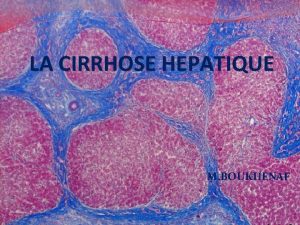
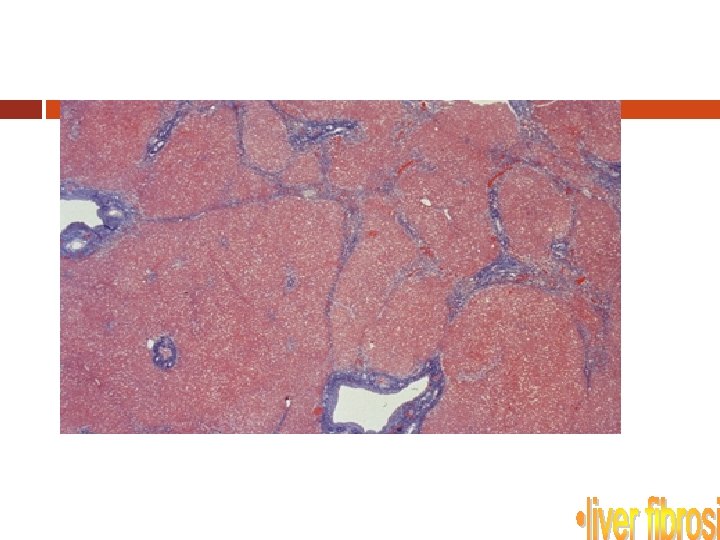
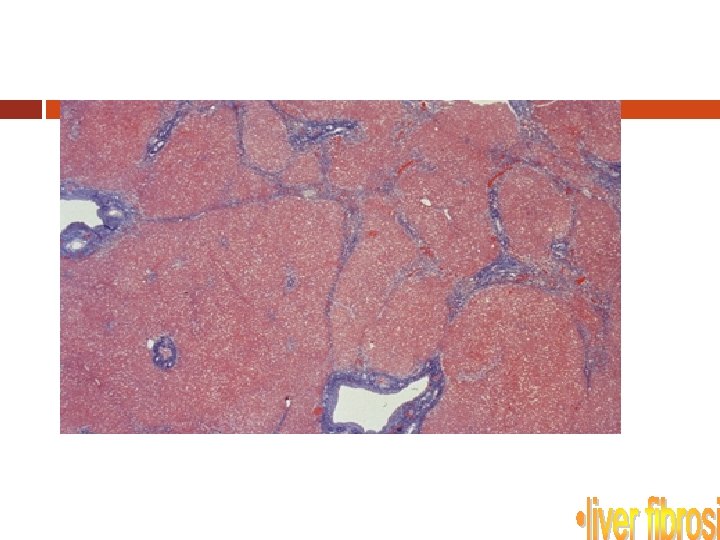
CIRRHOSIS Term was 1 st coined by Laennec in 1826 Many definitions but common theme is injury, repair, regeneration and scarring NOT a localized process; involves entire liver Primary histologic features: 1. 2. 3. 4. Marked fibrosis Destruction of vascular & biliary elements Regeneration Nodule formation
Cirrhosis: Pathophysiology Primary event is injury to hepatocellular elements Initiates inflammatory response with cytokine release->toxic substances Destruction of hepatocytes, bile duct cells, vascular endothelial cells Repair thru cellular proliferation and regeneration Formation of fibrous scar
Cirrhosis: Pathophysiology Primary cell responsible for fibrosis is stellate cell Become activated in response to injury and lead to ed expression of fibril-forming collagen Above process is influenced by Kupffer cells which activate stellate cells by eliciting production of cytokines Sinusoidal fenestrations are obliterated because of ed collagen and EC matrix synthesis
Cirrhosis: Pathophysiology Prevents normal flow of nutrients to hepatocytes and increases vascular resistance Initially, fibrosis may be reversible if inciting events are removed With sustained injury, process of fibrosis becomes irreversible and leads to cirrhosis
Causes of Cirrhosis Alcohol Viral hepatitis Biliary obstruction Veno-occlusive disease Hemochromatosis Wilson’s disease Autommune Drugs and toxins Metabolic diseases Idiopathic
Classification of Cirrhosis WHO divided cirrhosis into 3 categories based on morphological characteristics of the hepatic nodules 1. 2. 3. Micronodular Macronodular Mixed
Micronodular Cirrhosis Nodules are <3 mm in diameter Relatively uniform in size Distributed throughout the liver Rarely contain portal tracts or efferent veins Liver is of uniform size or mildly enlarged Reflect relatively early disease
Macronodular & Mixed Cirrhosis Nodules are >3 mm in diameter and vary considerably in size Usually contain portal tracts and efferent veins Liver is usually normal or reduced in size Mixed pattern if both type of nodules are present in equal proportions
Cirrhosis - Alcohol Also known as Laennec’s cirrhosis >50% of pts. with alcoholic cirrhosis die within 4 yrs of diagnosis Develops in only 10% to 30% of heavy drinkers Morphologically, micronodular pattern Multifactorial - genetic, nutritional, drug use and viral
Cirrhosis - Alcohol Fatty liver, alcoholic hepatitis Histology - megamitochondria, Mallory bodies, inflammation, necrosis, fibrosis Key mediator is acetaldehyde (ADH), the product of alcohol metabolism by alcohol dehydrogenase ADH directly activates stellate cells, inhibits DNA repair and damage microtubules
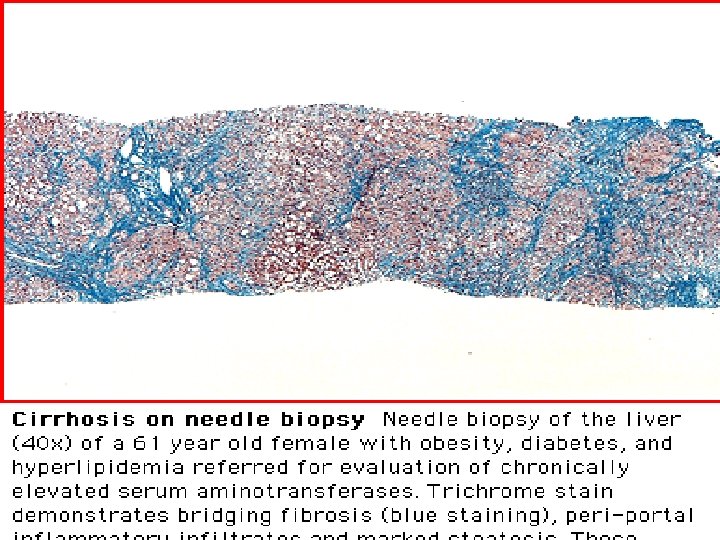
NAFLD/NASH Nonalcoholic Fatty Liver Disease and Steatohepatitis Becoming more common Infiltration of the liver with fat ± inflammation Pathologically similar to alcoholic liver but in absence of alcohol Associated with obesity, hyperlipidemia, NIDDM,
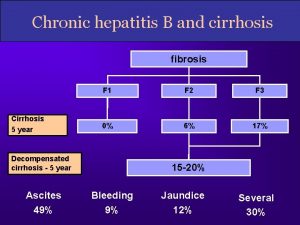
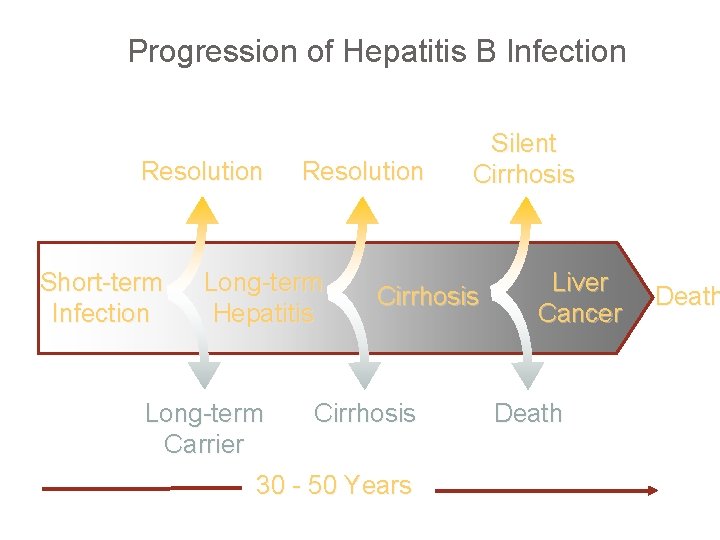
Viral Hepatitis Most common cause of cirrhosis worldwide (>50% of cases) Incidence of cirrhosis in Hepatitis B pts. is 1% and 10% in Hepatitis C pts. Incidence increases to 70 -80% in HBV +ve pts. who are superinfected with HDV
DIAGNOSIS Can be asymptomatic for decades History Physical findings: Hepatomegaly, jaundice, ascites, spider angioma, splenomegaly, palmar erythema, fetor hepaticus, purpura etc. Elevated LFTs, thrombocytopenia,
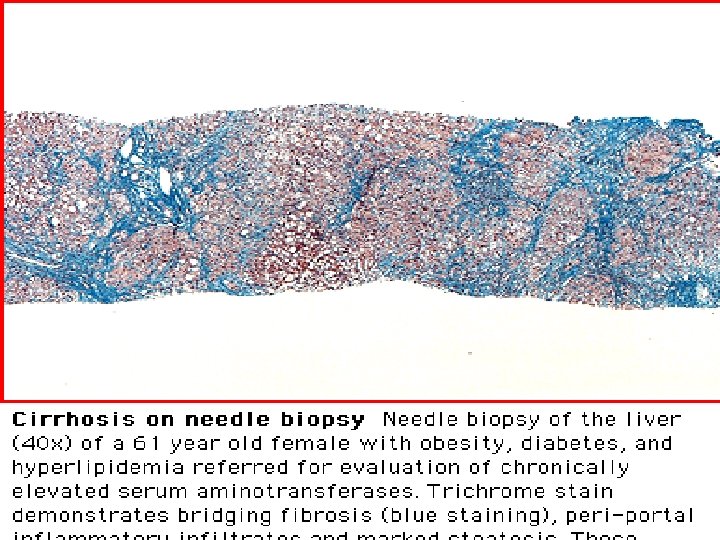
DIAGNOSIS Definitive diagnosis is by biopsy or gross inspection of liver Noninvasive methods include US, CT scan, MRI Indirect evidence - esophageal varices seen during endoscopy
Manifestations of Cirrhosis Hepatorenal syndrome Hepatic encephalopathy Portal hypertension Water retention Hematologic Hepatocellular carcinoma
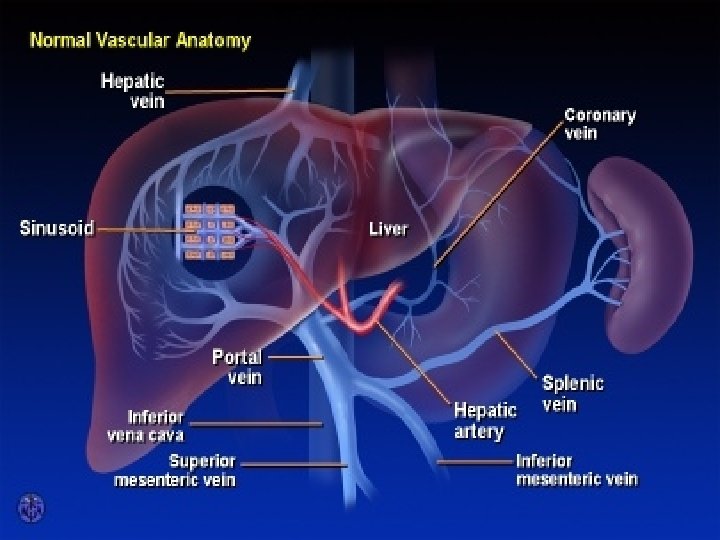
Portal Hypertension (PH) Portal vein pressure above the normal range of 5 to 8 mm Hg Portal vein - Hepatic vein pressure gradient greater than 5 mm Hg (>12 clinically significant) Represents an increase of the hydrostatic pressure within the portal vein or its tributaries
Pathophysiology of PH Cirrhosis results in scarring (perisinusoidal deposition of collagen) Scarring narrows and compresses hepatic sinusoids (fibrosis) Progressive increase in resistance to portal venous blood flow results in PH Portal vein thrombosis, or hepatic venous obstruction also cause PH by increasing the resistance to portal blood flow
Pathophysiology of PH As pressure increases, blood flow decreases and the pressure in the portal system is transmitted to its branches Results in dilation of venous tributaries Increased blood flow through collaterals and subsequently increased venous return cause an increase in cardiac output and total blood volume and a decrease in systemic vascular resistance With progression of disease, blood pressure usually falls
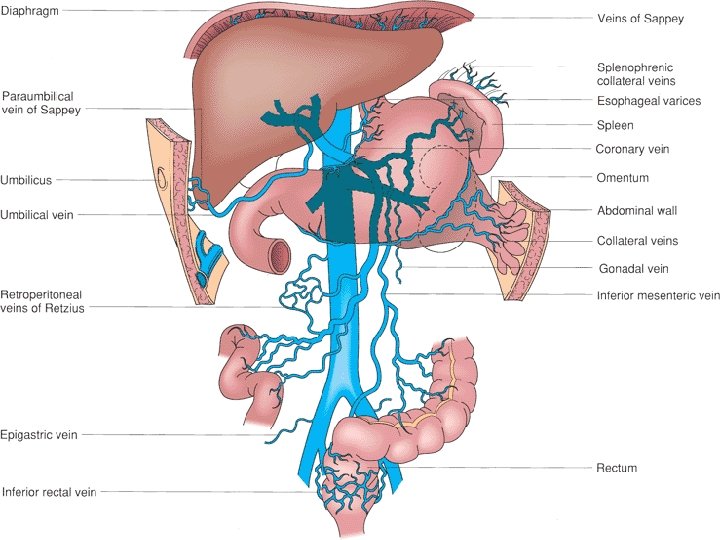
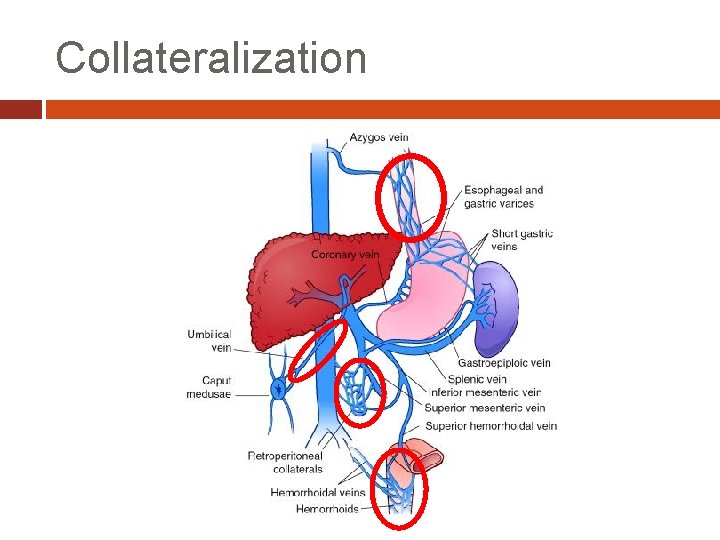
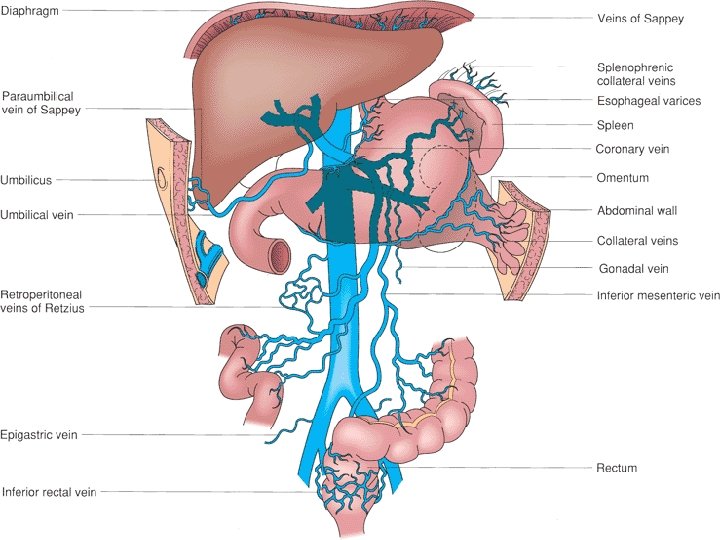
Portal Vein Collaterals Coronary vein and short gastric veins -> veins of the lesser curve of the stomach and the esophagus, leading to the formation of varices Inferior mesenteric vein -> rectal branches which, when distended, form hemorrhoids Umbilical vein ->epigastric venous system around the umbilicus (caput medusae) Retroperitoneal collaterals ->gastrointestinal veins through the bare areas of the liver
Etiology of PH Causes of PH can be divided into 1. Pre-hepatic 2. Intra-hepatic 3. Post-hepatic
Pre-hepatic PH Caused by obstruction to blood flow at the level of portal vein Examples: congenital atresia, extrinsic compression, schistosomiasis, portal, superior mesenteric, or splenic vein thrombosis
Post-hepatic Caused by obstruction to blood flow at the level of hepatic vein Examples: Budd-Chiari syndrome, chronic heart failure, constrictive pericarditis, vena cava webs
Budd-Chiari Syndrome Caused by hepatic venous obstruction At the level of the inferior vena cava, the hepatic veins, or the central veins within the liver itself result of congenital webs (in Africa and Asia), acute or chronic thrombosis (in the West), and malignancy
Budd-Chiari Syndrome Acute symptoms include hepatomegaly, RUQ abdominal pain, nausea, vomiting, ascites Chronic form present with the sequelae of cirrhosis and portal hypertension, including variceal bleeding, ascites, spontaneous bacterial peritonitis, fatigue, and encephalopathy Diagnosis is most often made by US evaluation of the liver and its vasculature Cross-sectional imaging using contrastenhanced CT or MRI
Budd-Chiari Syndrome Gold standard for the diagnosis has been angiography Management has traditionally been surgical intervention (surgical decompression with a side -to-side portosystemic shunt) Minimally invasive treatment using TIPS may be first-line therapy now Response rates to medical therapy are poor
Portal Vein Thrombosis Most common cause in children (fewer than 10% of adult pts. ) Normal liver function and not as susceptible to the development of complications, such as encephalopathy Diagnosis by sonography, CT and MRI Often, the initial manifestation of portal vein thrombosis is variceal bleeding in a noncirrhotic patient with normal liver function
Portal Vein Thrombosis Causes Umbilical vein infection (the most common cause in children) Coagulopathies (protein C and antithrombin III deficiency), Hepatic malignancy, myeloproliferative disorders Inflammatory bowel disease pancreatitis trauma Most cases in adults are idiopathic
Portal Vein Thrombosis Therapeutic options are esophageal variceal ligation and sclerotherapy Distal splenorenal shunt Rex shunt in patients whose intrahepatic portal vein is patent (most commonly children)
Splenic Vein Thrombosis Most often caused by disorders of the pancreas (acute and chronic pancreatitis, trauma, pancreatic malignancy, and pseudocysts) Related to the location of the splenic vein Gastric varices are present in 80% of patients Occurs in the setting of normal liver function Readily cured with splenectomy (variceal hemorrhage), although observation for asymptomatic patients is acceptable.

Complications of PH GI bleeding due to gastric and esophageal varices Ascites Hepatic encephalopathy
Varices Most life threatening complication is bleeding from esophageal varices Distal 5 cm of esophagus Usually the portal vein-hepatic vein pressure gradient >12 mm Hg Bleeding occurs in 25 -35% of pts. With varices and risk is highest in 1 st yr.
Prevention of Varices Primary prophylaxis: prevent 1 st episode of bleeding Secondary prophylaxis: prevent recurrent episodes of bleeding Include control of underlying cause of cirrhosis and pharmacological, surgical interventions to lower portal pressure
Prevention of Varices Beta blockade: Beta blockade (Nadolol, Propranolol) Nitrates: Organic nitrates Surgery: No longer performed* Endoscopy: Sclerotherapy (no longer used*) and variceal ligation * Refers to primary prophylaxis
Treatment of Varices Initial Management: 1. 2. 3. 4. 5. 6. Airway control Hemodynamic monitoring Placement of large bore IV lines Full lab investigation (Hct, Coags, LFTs, ) Administration of blood products ICU monitoring
Pharmacologic Treatment of Varices Decreases the rate of bleeding Enhances the endoscopic ability to visualize the site of bleeding Vasopressin - potent splanchnic vasoconstrictor; decreases portal venous blood flow and pressure Somatostatin: decrease splanchnic blood flow indirectly; fewer side effects Octreotide: Initial drug of choice for acute variceal bleeding
Endoscopic Therapy for Varices Endoscopic Sclerotherapy: complications occur in 10 -30% and include fever, retrosternal chest pain, dysphagia, perforation Endoscopic variceal ligation: becoming the initial intervention of choice; success rates range from 80 -100%
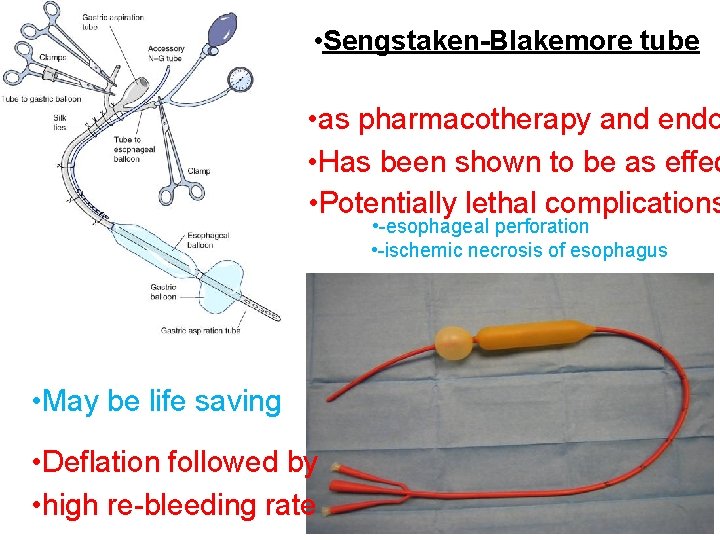
Balloon Tamponade Sengstaken-Blakemore tube Minnesota tube Alternative therapy for pts. who fail pharmacologic or endoscopic therapy Complications: aspiration, perforation, necrosis Limited to 24 hrs; works in 70 -80%
TIPS Transjugular inrahepatic portasystemic shunt 1 st line treatment for bleeding esophageal varices when earlier-mentioned methods fail Performed in IR Success rates 90 -100% Significant complication is hepatic encephalopathy
Surgical Intervention Liver transplantation: only definitive procedure for PH caused by cirrhosis Shunts Totally diverting (end-side portacaval) Partially diverting (side-side portacaval) Selective (distal splenorenal shunt) Devascularization
Severe complications such as spontaneous bacterial peritonitis or ascites that is refractory to diuretic therapy, occur in the most advanced disease and are associated with a median life expectancy of less than 1 year.
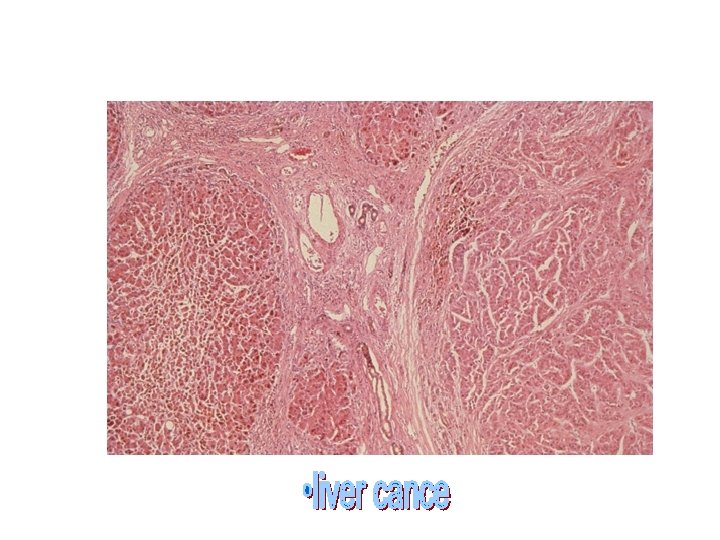
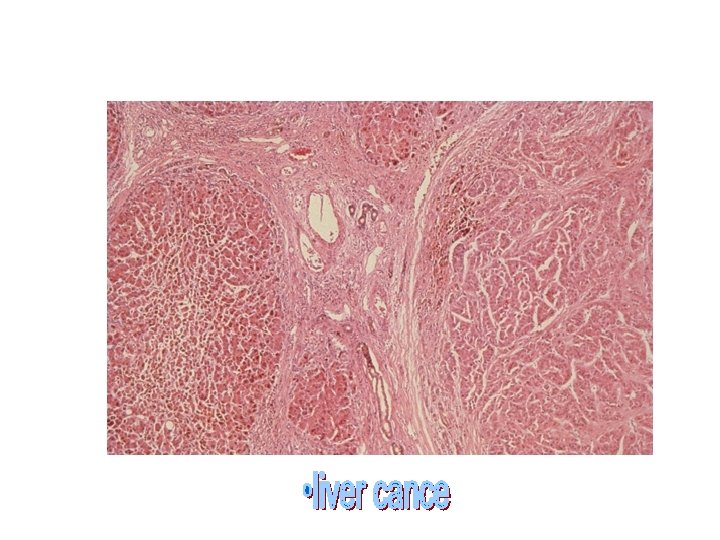
Cirrhosis, even if early and stable, predisposes to development of primary hepatocellular carcinoma in as many as 3% of patients per year.
Until recently, little could be done to alter the prognosis of patients with cirrhosis and most died of complications. Today, the outlook has begun to change because of advances in orthotopic liver transplantation and development of therapies to prevent and treat complications.
Biologic Basis of hepatic fibrosis Hepatic fibrosis is a wound-healing response The same cell type produce hepatic fibrosis regardless of the underling cause. hepatic fibrosis follows chronic, but not selflimited, injury. Fibrosis occurs earliest in regions where injury is most severe.
Antifibrotic therapies : Rationale and specific Agent The paradigm of satellite cell activation provides an important framework to define potential sites of antifibrotic therapy follows 1. Cure the primary disease to prevent injury. 2. Reduce inflammation or the host response to avoid stimulating satellite cells. 3. Directly down –regulate stellate cell activation
Antifibrotic therapies : Rationale and specific Agent 4. Neutralize the proliferative, fibrogenic, contractile, and proinflammatory responses of stellate cells. 5. Stimulate apoptosis of stellate cells. 6. Increase the degradation of scar martix, either by stimulating cells that produce matrix proteases, down-regulating their inhibitors , or directly administering matrix proteases.
DIAGNOSTIC APPROACH Unless the diagnosis is already established, specific serologic tests and often a liver biopsy are required to establish the cause of the cirrhosis.
DIAGNOSTIC APPROACH In addition, patients should undergo laboratory testing to document the severity of the disease and assessment of whether ascites or hepatic encephalopathy is present. .
DIAGNOSTIC APPROACH Obtaining this information helps to determine prognosis, the possibility of specific therapy, and the possible necessity for screening family members for inherited diseases or chronic viral hepatitis
specific therapy may be indicated Antiviral therapy for chronic hepatitis C and B, Corticosteroids (with or without immunosuppressive therapy) for autoimmune hepatitis, Phlebotomy for hereditary hemochromatosis, Penicillamine for Wilson's disease.
In some cases, even hepatic fibrosis can be reversed; examples include abstinence from alcohol in alcoholic liver disease and immunosuppressive therapy in autoimmune hepatitis
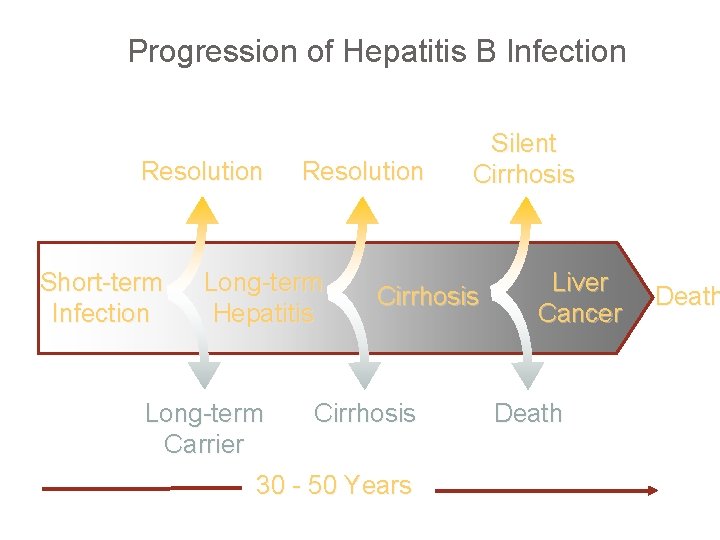
Progression of Hepatitis B Infection Resolution Short-term Infection Resolution Long-term Hepatitis Long-term Carrier Silent Cirrhosis 30 - 50 Years Liver Cancer Death
initial testing should consist of the following Measurement of serum aminotransferases, bilirubin, alkaline phosphatase, albumin, creatinine, and sodium (otherwise unexplained hyponatremia is a marker of severe disease), the blood urea nitrogen, platelet count, and prothrombin time.

initial testing should consist of the following • Abdominal ultrasonography to assess the portal circulation. In one study, the severity of liver disease correlated with portal vein blood velocity as determined by ultrasound
Portal hypertension is the most common and lethal complication of chronic liver disease Esophageal varices and hemorrhage ascites renal dysfunction hypersplenism portalsystemic encephalopathy P H. . PPG>5 mm. Hg
Hepatocellular carcinoma The issue of periodic surveillance of such patients with serum alphafetoprotein (AFP) measurements (values above 20 µg/L being abnormal) and ultrasound examinations remains a contentious issue from the viewpoint of cost-effectiveness since an improvement in survival has not yet been demonstrate
All patients with cirrhosis should be evaluated for the presence of varices because of the beneficial effect of prophylaxis with propranolol or nadolol
Patients with most forms of cirrhosis, particularly due to hepatitis B and C, hereditary hemochromatosis, and alcoholic liver disease, are at high risk (1 to 6 percent per year) for the development of hepatocellular carcinoma
A. Cure the primary disease Clear chronic viral infection Abstinence from alcohol, stop toxic drugs Remove iron , copper in overload disease Eradicate schistosomiasis Reverse biliary obstruction Revers jejunoileal bypass

Nonalcoholic steatohepatitis NASH is a disorder diagnosed by liver biopsy. The biopsy findings are indistinguishable from those of alcoholic hepatitis described above but the patient lacks a history of significant alcohol consumption. The liver disease is stable in most patients but a minority progress to cirrhosis
CIRRHOSIS & PORTAL HYPERTENSION SURGICAL COMPLICATIONS Turner Lisle Resident Teaching Conference May 2008
Cirrhosis End result of anything that causes hepatocellular injury Toxins, viruses, prolonged cholestasis, autoimmunity, metabolic disorders Pathologic response is uniform Hepatocellular necrosis Fibrosis Nodular regeneration
Cirrhosis - why do we care Hepatic failure Portal hypertension - variceal bleeding Ischemia & autoimmune factors thought to play a role, although mechanism is not clear
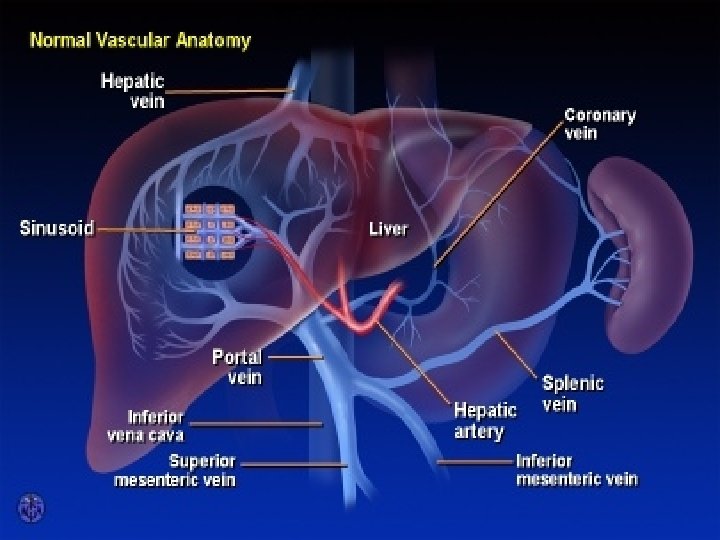
Anatomy Dual blood supply Hepatic arterial Portal venous Total hepatic blood flow ~1500 m. L/min or 25% of cardiac output Portal vein 2/3 of total hepatic blood flow Hepatic artery >1/2 of O 2
Portal Hypertension Usually due to increased portal venous resistance Classification based on site of increased resistance Prehepatic Intrahepatic
Prehepatic Portal HTN Portal vein thrombosis most common Isolated splenic vein thrombosis Usually caused by pancreatic inflammation or neoplasm Results in gastrosplenic HTN with ensuing formation of gastric varices Normal superior mesenteric & portal vein pressure Easily reversed by splenectomy alone
Intrahepatic Portal HTN Often a combination of pre-, intra-, or post-sinusoidal Presinusoidal Schistosomiasis Nonalcoholic cirrhosis Sinusoidal Et. OH Postsinusoidal - overall rare Et. OH Budd-Chiari syndrome (hepatic vein thrombosis) Constrictive pericarditis Heart failure
Portal Hypertension Portal pressure > 5 mm. Hg Portal pressure > 8 mm. Hg needed for collateralization
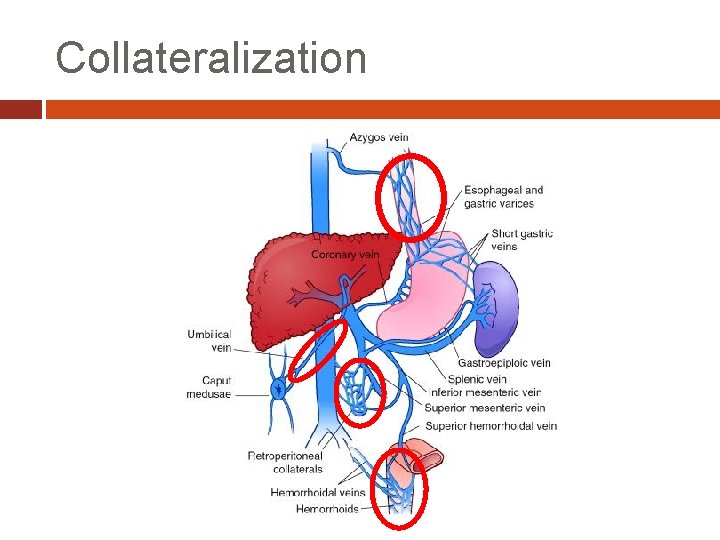
Collateralization
Evaluation of the Cirrhotic 1) 2) 3) 4) 5) Dx of underlying liver disease Estimation of fxn hepatic reserve Definition of portal venous anatomy Hepatic hemodynamic evaluation If present, identification of site of UGI bleeding
Evaluation of the Cirrhotic Physical Exam Jaundice Ascites Caput medusae Asterixis Spider angiomas Palmer erythema Testicular atrophy Gynecomastia +/- Palpable spleen (portal HTN) Lab tests Anemia Thrombocytopenia Coagulopathy Hypoalbuminemia AST/ALT Bili Alk Phos GGT Hepatitis serologies -fetoprotein
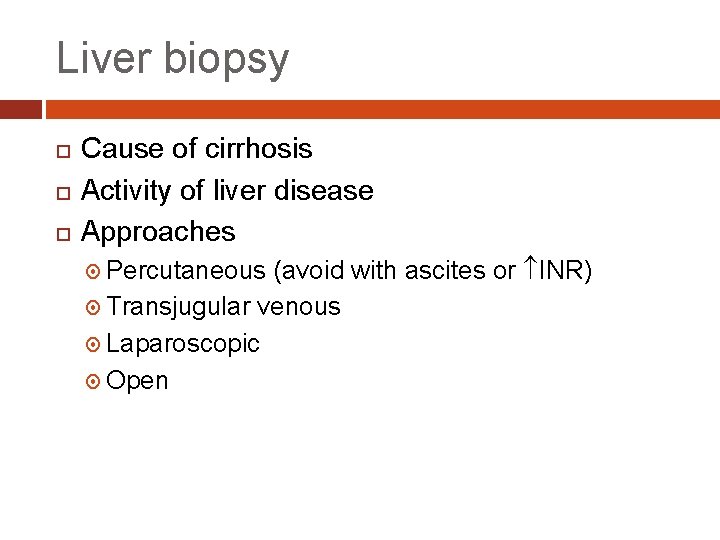
Liver biopsy Cause of cirrhosis Activity of liver disease Approaches (avoid with ascites or INR) Transjugular venous Laparoscopic Open Percutaneous
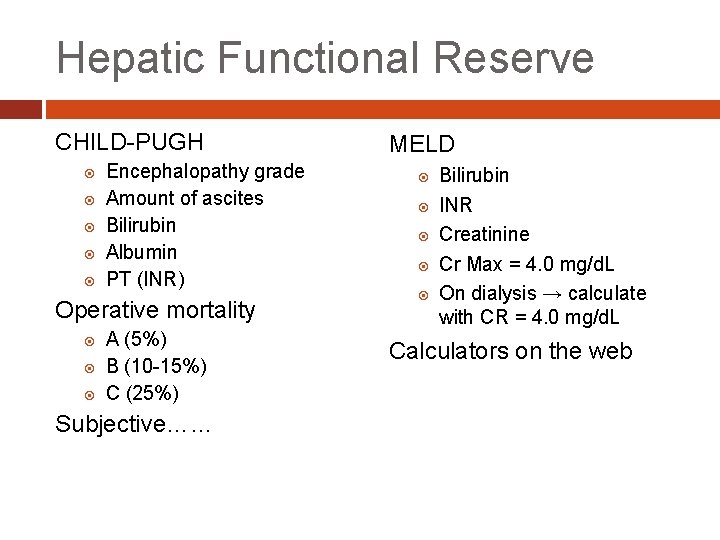
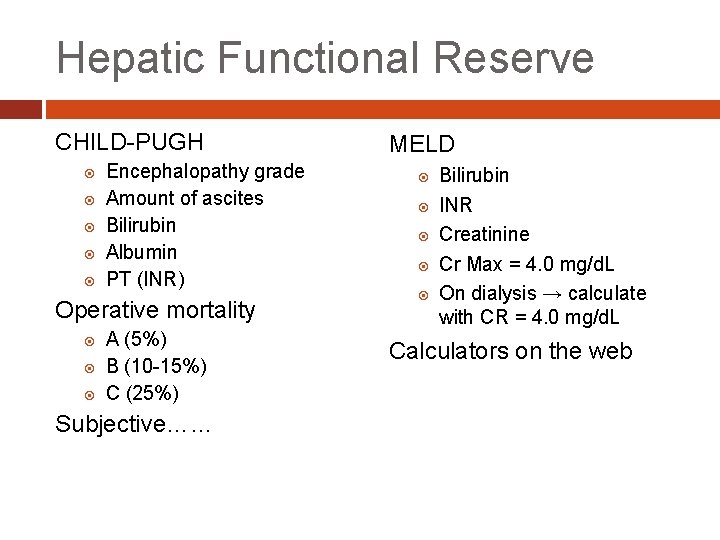
Hepatic Functional Reserve CHILD-PUGH Encephalopathy grade Amount of ascites Bilirubin Albumin PT (INR) Operative mortality A (5%) B (10 -15%) C (25%) Subjective…… MELD Bilirubin INR Creatinine Cr Max = 4. 0 mg/d. L On dialysis → calculate with CR = 4. 0 mg/d. L Calculators on the web
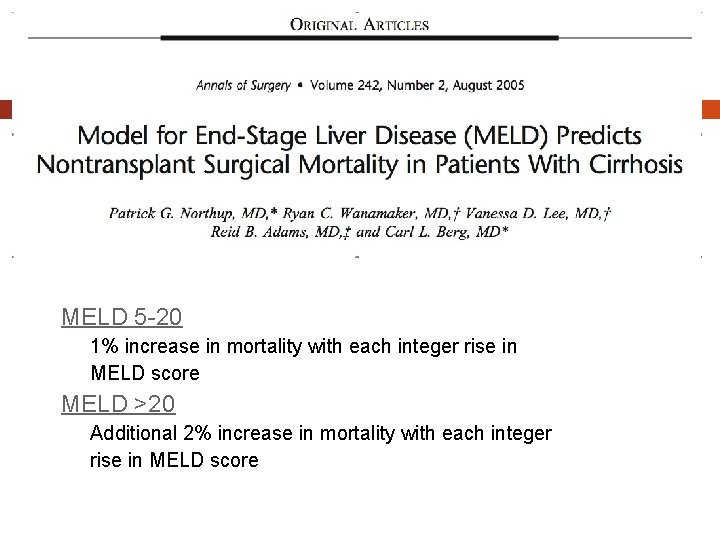
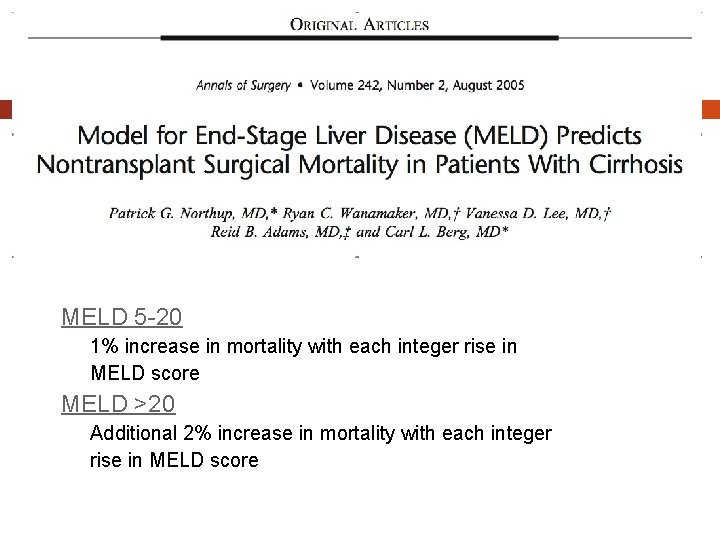
MELD 5 -20 1% increase in mortality with each integer rise in MELD score MELD >20 Additional 2% increase in mortality with each integer rise in MELD score
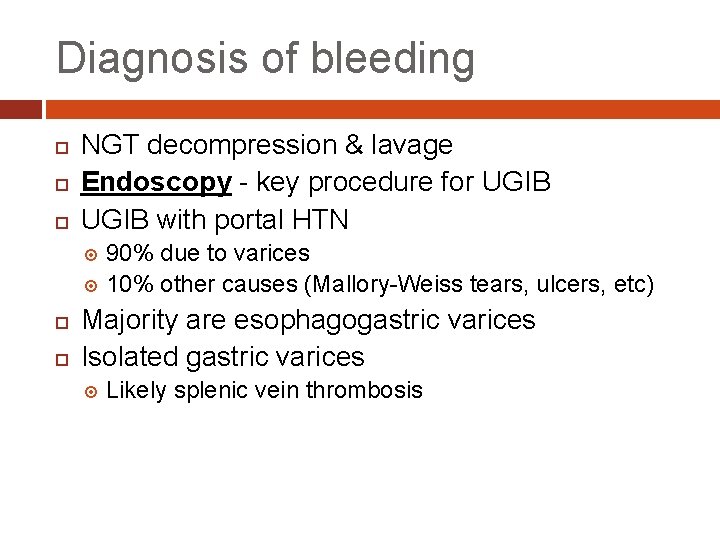
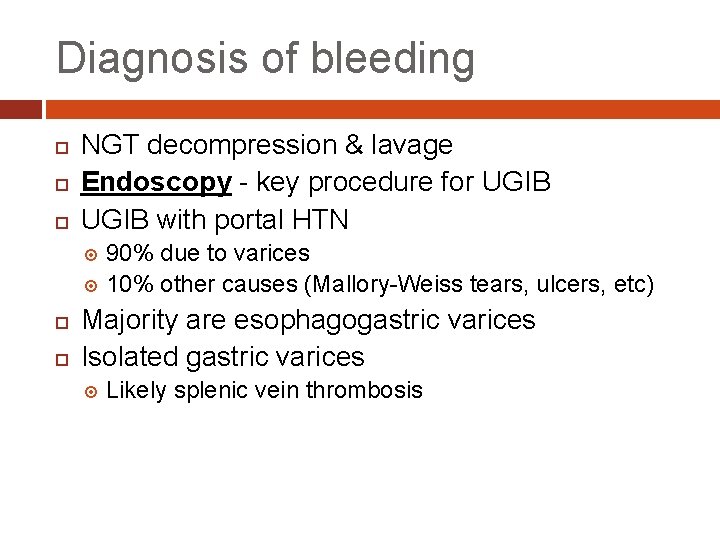
Diagnosis of bleeding NGT decompression & lavage Endoscopy - key procedure for UGIB with portal HTN 90% due to varices 10% other causes (Mallory-Weiss tears, ulcers, etc) Majority are esophagogastric varices Isolated gastric varices Likely splenic vein thrombosis
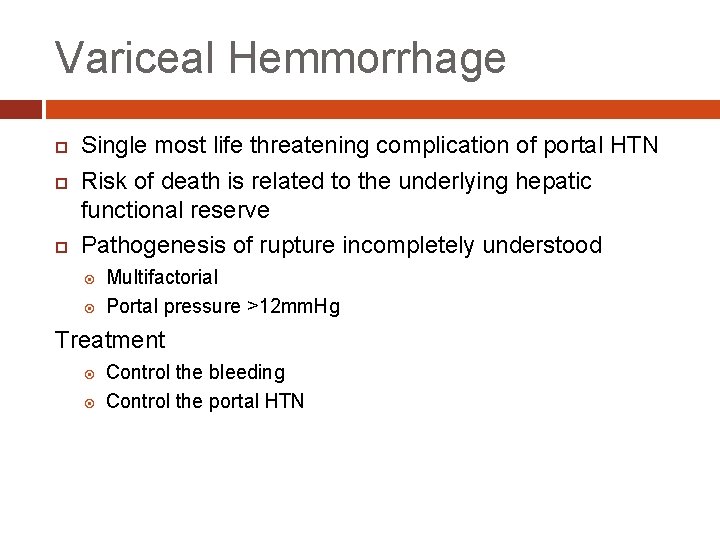
Variceal Hemmorrhage Single most life threatening complication of portal HTN Risk of death is related to the underlying hepatic functional reserve Pathogenesis of rupture incompletely understood Multifactorial Portal pressure >12 mm. Hg Treatment Control the bleeding Control the portal HTN
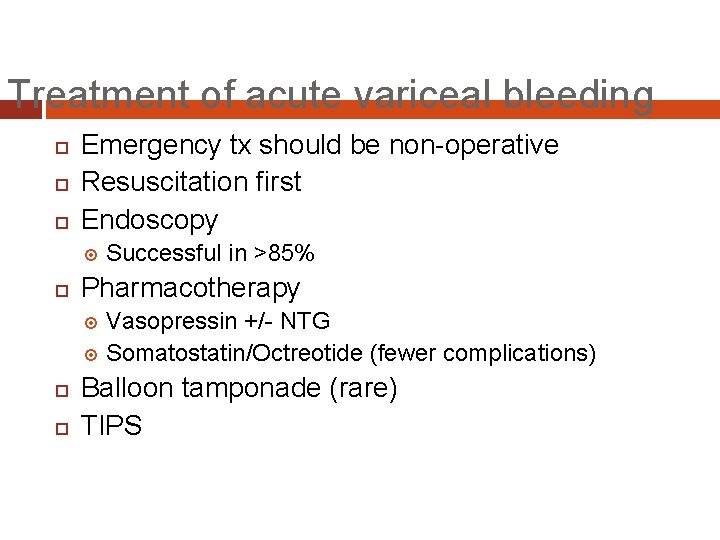
Treatment of acute variceal bleeding Emergency tx should be non-operative Resuscitation first Endoscopy Successful in >85% Pharmacotherapy Vasopressin +/- NTG Somatostatin/Octreotide (fewer complications) Balloon tamponade (rare) TIPS
Endoscopic treatment Most common treatment modality for acute bleeding as well as prevention Sclerosis Ligation • Equally efficacious (80 -9 Complications Esophageal ulceration Perforation Worsening hemorrhage Aspiration Failure after two unsuccessful attempts
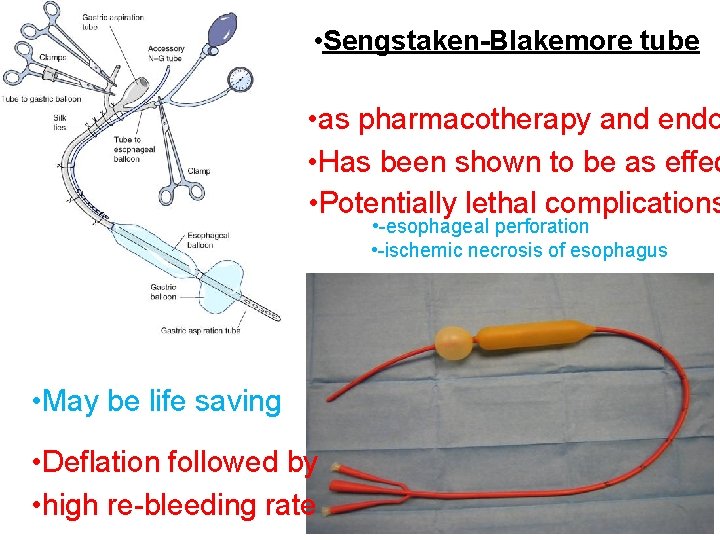
• Sengstaken-Blakemore tube • as pharmacotherapy and endo • Has been shown to be as effec • Potentially lethal complications • -esophageal perforation • -ischemic necrosis of esophagus • May be life saving • Deflation followed by • high re-bleeding rate
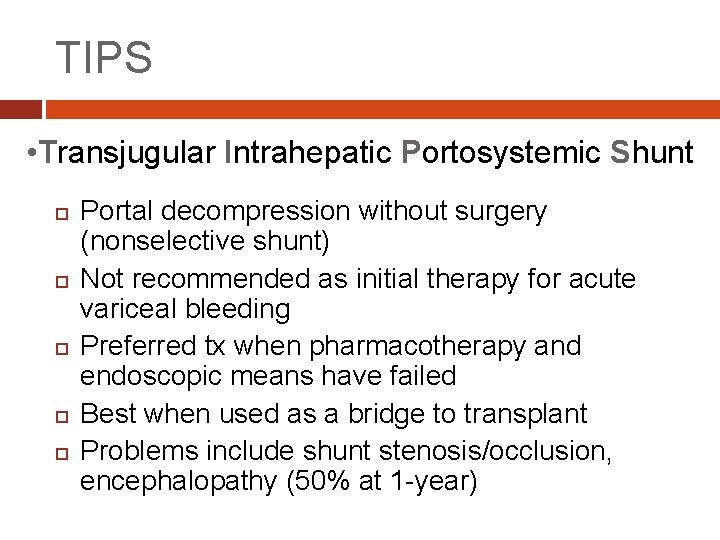
TIPS • Transjugular Intrahepatic Portosystemic Shunt Portal decompression without surgery (nonselective shunt) Not recommended as initial therapy for acute variceal bleeding Preferred tx when pharmacotherapy and endoscopic means have failed Best when used as a bridge to transplant Problems include shunt stenosis/occlusion, encephalopathy (50% at 1 -year)
Emergency surgery Indications Failure of acute endoscopic tx Failure of TIPS placement Hemorrhage from gastric varices Esophageal transection rapid/simple Portacaval shunt or splenorenal shunt Operative mortality >25% in most series
Prevention of recurrent hemorrhage Likelihood of repeat episodes >70% Goals Prevention of recurrent bleeding Maintenance of satisfactory hepatic function Options Pharmacotherapy ( -blockers +/- nitrates) Chronic endoscopy (successful in 2/3) TIPS (less bleeding, more encephalopathy) Operative shunts Transplantation
Portosystemic shunts Most effective means of preventing recurrent bleeding in patients with portal hypertension Problems Encephalopathy Accelerated hepatic failure Types Nonselective - End-to-end/side portocaval Selective - Distal splenorenal Partial - Small diameter PTFE
Nonshunt procedures Objectives Ablation of varices Extensive interruption of collateral vessels Options Transection and reanastamosis of the distal esophagus Extensive esophagogastric devascularization + esophageal transection and splenectomy Rebleeding rates similar to endoscopic experience

Ascites Usually an indicator of advanced cirrhosis Initiated by altered hepatic and splanchnic hemodynamics Intravascular volume deficit resulting in increased aldosterone…. . Central goal is to achieve a NEGATIVE sodium balance
Ascites treatment Dietary restriction + Diuretics spironolactone +/- lasix 5 -10% are refractory Intermittent paracentesis TIPS Peritoneovenous “Denver” shunt (rarely used) SBP PMN >250/mm 3 or positive culture
Encephalopathy Variety of manifestations Pathogenesis - circulating cerebral toxins Precipitated by multiple factors Ammonia Mercaptans -aminobutyric acid Shunts, hemorrhage, excessive diuresis, azotemia, infection, increased dietary protein, sedatives Management Eliminate/treat precipitating factors Lactulose, neomycin (decrease absorption of intestinal ammonia)
Questions

 Nursing management of cirrhosis of liver
Nursing management of cirrhosis of liver Cirrhosis
Cirrhosis Symptoms liver cirrhosis
Symptoms liver cirrhosis Mild hepatic steatosis
Mild hepatic steatosis Psc disease
Psc disease What is cirrhosis
What is cirrhosis Complication of liver cirrhosis
Complication of liver cirrhosis Easl guidelines decompensated cirrhosis
Easl guidelines decompensated cirrhosis Necrotic cell
Necrotic cell Hyperestrinism cirrhosis
Hyperestrinism cirrhosis Complications of cirrhosis
Complications of cirrhosis Can ct scan miss cirrhosis
Can ct scan miss cirrhosis Cirrhosis pathogenesis
Cirrhosis pathogenesis Types of cirrhosis
Types of cirrhosis Pes statement for liver cirrhosis
Pes statement for liver cirrhosis Pes statement for cirrhosis
Pes statement for cirrhosis Complication of liver cirrhosis
Complication of liver cirrhosis Cirrhosis
Cirrhosis Micronodular cirrhosis vs macronodular
Micronodular cirrhosis vs macronodular Diet for hepatitis c
Diet for hepatitis c Gastrointestinalis
Gastrointestinalis Cirrhosis care near woodland
Cirrhosis care near woodland What causes liver cirrhosis
What causes liver cirrhosis