Lecture 1 OVERVIEW CELLULAR COMPONENTS Hematopoiesis Chapters 1




- Slides: 67
Lecture 1 OVERVIEW; CELLULAR COMPONENTS; Hematopoiesis Chapters 1, 6, 7 March 7, 2018 Elaine M. Keohane, Ph. D, MLS(ASCP)SH keohanem@shrp. rutgers. edu Rutgers-The State University of New Jersey School of Health Related Professions and Kyung Jin Cho, Ph. D, Professor Emeritus chokj@korea. ac. kr Dept. of Medical Laboratory Science College of Health Sciences, Korea University
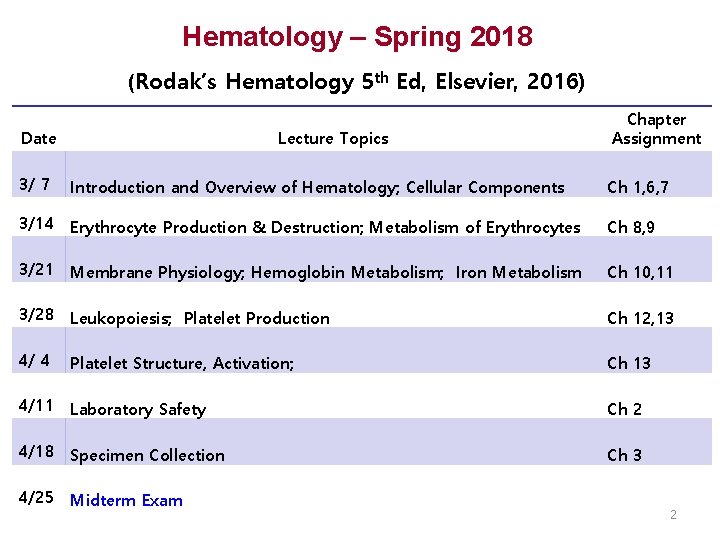
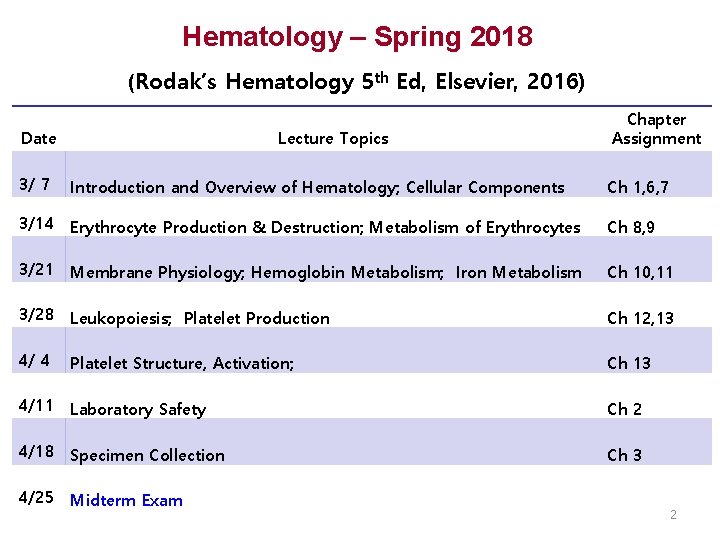
Hematology – Spring 2018 (Rodak’s Hematology 5 th Ed, Elsevier, 2016) Date Lecture Topics Chapter Assignment 3/ 7 Introduction and Overview of Hematology; Cellular Components Ch 1, 6, 7 3/14 Erythrocyte Production & Destruction; Metabolism of Erythrocytes Ch 8, 9 3/21 Membrane Physiology; Hemoglobin Metabolism; Iron Metabolism Ch 10, 11 3/28 Leukopoiesis; Platelet Production Ch 12, 13 4/ 4 Platelet Structure, Activation; Ch 13 4/11 Laboratory Safety Ch 2 4/18 Specimen Collection Ch 3 4/25 Midterm Exam 2
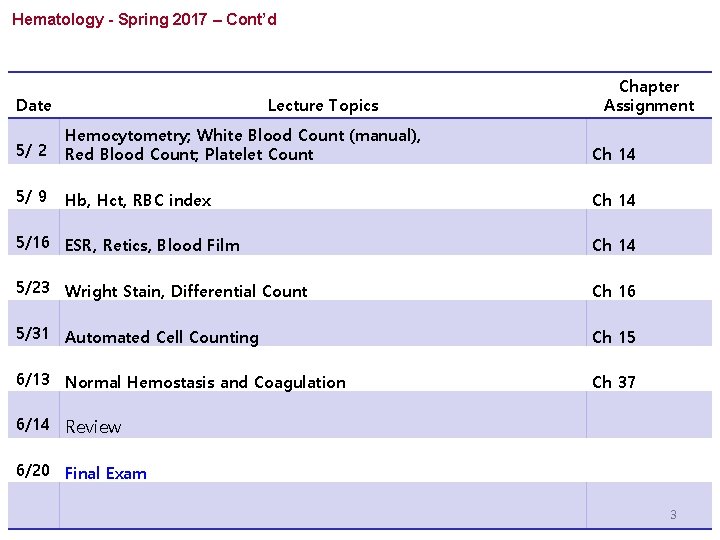
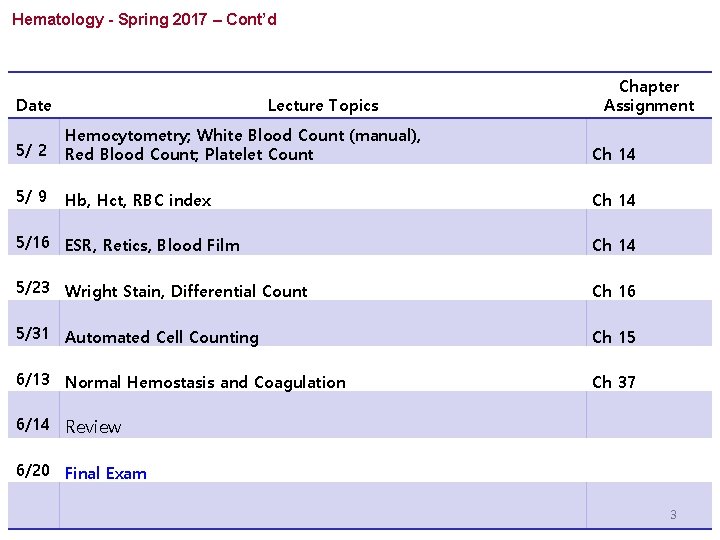
Hematology - Spring 2017 – Cont’d Date Lecture Topics Chapter Assignment 5/ 2 Hemocytometry; White Blood Count (manual), Red Blood Count; Platelet Count Ch 14 5/ 9 Hb, Hct, RBC index Ch 14 5/16 ESR, Retics, Blood Film Ch 14 5/23 Wright Stain, Differential Count Ch 16 5/31 Automated Cell Counting Ch 15 6/13 Normal Hemostasis and Coagulation Ch 37 6/14 Review 6/20 Final Exam 3
OVERVIEW OF CLINICAL LABORATORY HEMATOLOGY Chapter 1 Chapter Author: George A. Fritsma
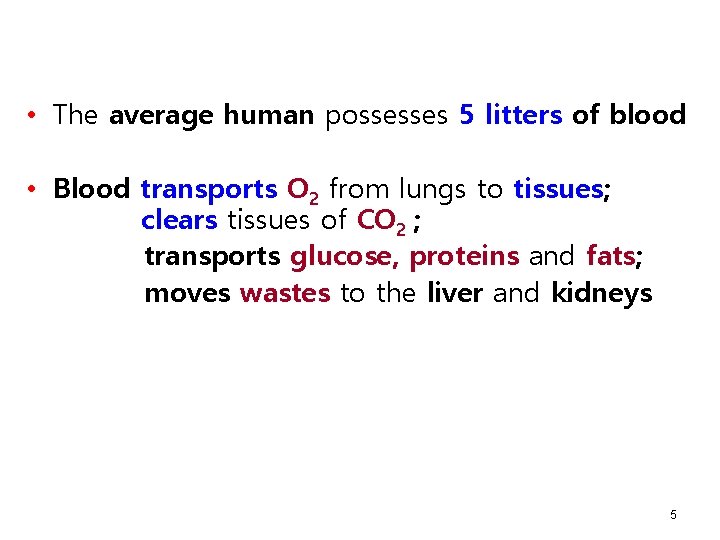
• The average human possesses 5 litters of blood • Blood transports O 2 from lungs to tissues; clears tissues of CO 2 ; transports glucose, proteins and fats; moves wastes to the liver and kidneys 5
• The liquid portion of the blood is plasma, which provides coagulation factors that protect bleeding • Plasma transports and nourishes blood cells: - Red Blood Cells - White Blood Cells: neutrophils, eosinophils, basophils, lymphocytes, monocytes - Platelets 6
• By staining, counting, analyzing and recording the appearance, phenotype, and genotype, the MLS is able to predict, detect, and diagnose blood disease and many systemic diseases that affect blood cells • Physicians rely on hematology laboratory test results to select and monitor therapy for the disorders • Consequently, CBC (complete blood count) is ordered on nearly everyone who visits a physician or is admitted to a hospital 7

History of Hematology • 1657, Kircher A described “worms” in the blood • 1674, Leeuwenhoek AV described RBCs • Late 1800 s, Bizzozero G described platelets • 1902, Wright JH developed Wright Stain, so blood can be examined through microscope. Romanowsky-type stain (polychrome stain): the foundation of blood cell identification 8
History of Hematology – Cont’d • Since before the 1900, physicians and medical laboratory professionals counted RBCs in measured volumes to detect anemias • 1953, Joseph and Wallace Coulter developed automated particle counters • 1958, automated cell counters available in clinical laboratories • 21 stcentury: automated analyzers, flow cytometry, cytogenetics, molecular analysis 9
Clinical Laboratory Hematology • Hematology is the study of the blood cells and the hematopoietic organs that produce them. - Number of specific cells: Cell Counting - Morphology : Cell Size and shape Color and inclusions in Cytoplasm Size, shape, staining features of Nucleus - Function of cells • Advanced study looks at hematologic diseases on a genetic and molecular level 10
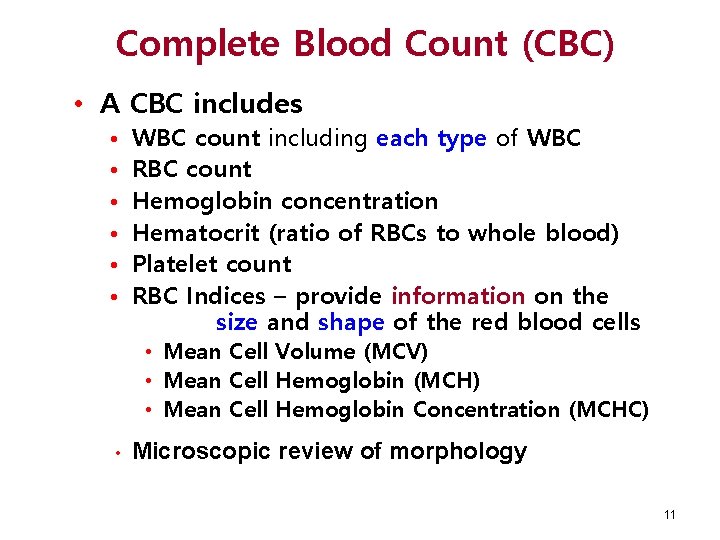
Complete Blood Count (CBC) • A CBC includes • • • WBC count including each type of WBC RBC count Hemoglobin concentration Hematocrit (ratio of RBCs to whole blood) Platelet count RBC Indices – provide information on the size and shape of the red blood cells • Mean Cell Volume (MCV) • Mean Cell Hemoglobin (MCH) • Mean Cell Hemoglobin Concentration (MCHC) • Microscopic review of morphology 11
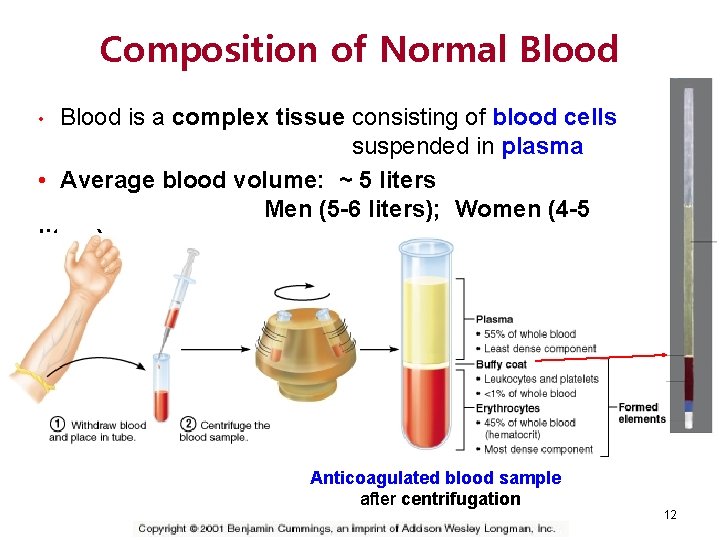
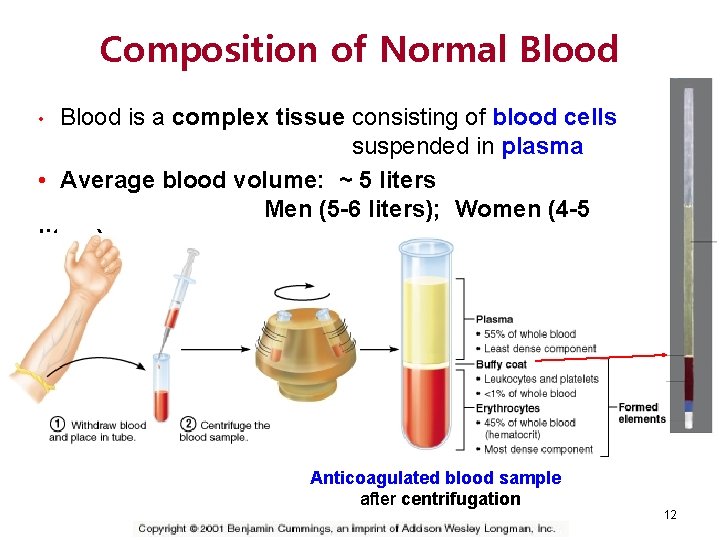
Composition of Normal Blood is a complex tissue consisting of blood cells suspended in plasma • Average blood volume: ~ 5 liters Men (5 -6 liters); Women (4 -5 liters) • Anticoagulated blood sample after centrifugation 12
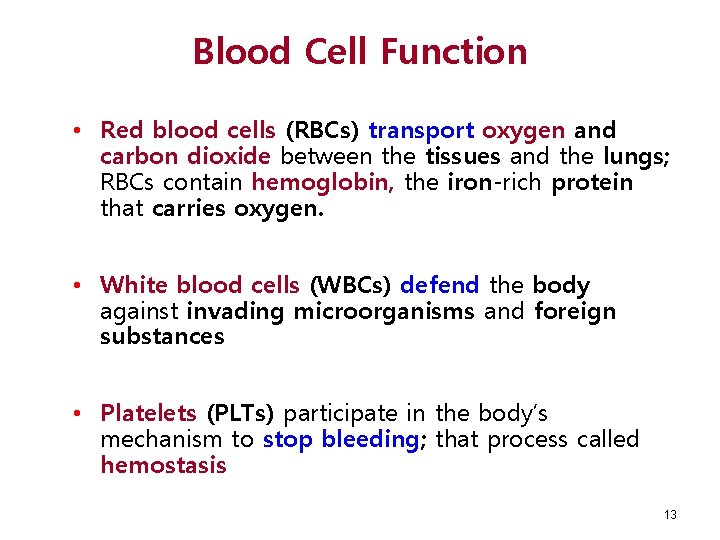
Blood Cell Function • Red blood cells (RBCs) transport oxygen and carbon dioxide between the tissues and the lungs; RBCs contain hemoglobin, the iron-rich protein that carries oxygen. • White blood cells (WBCs) defend the body against invading microorganisms and foreign substances • Platelets (PLTs) participate in the body’s mechanism to stop bleeding; that process called hemostasis 13
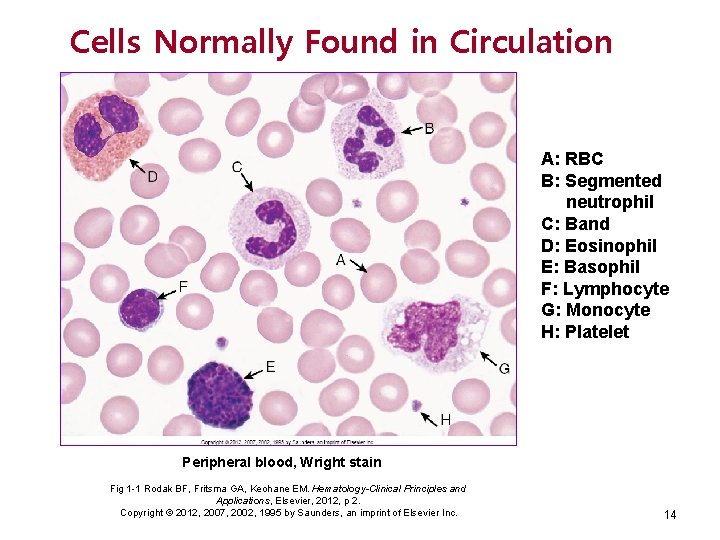
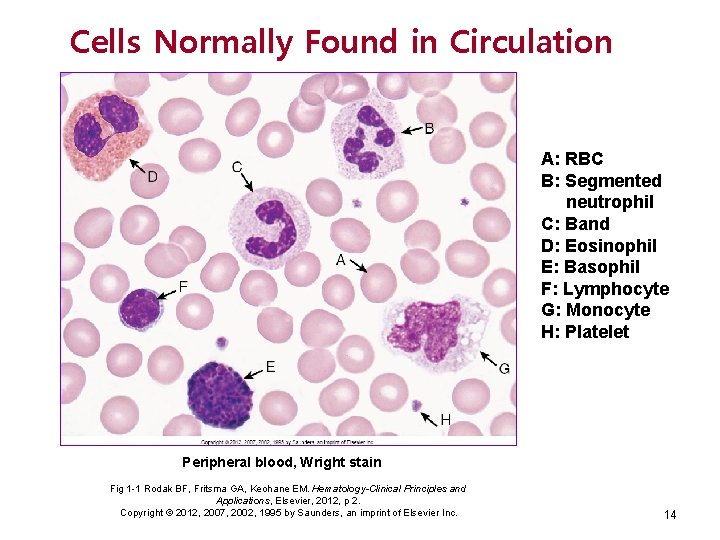
Cells Normally Found in Circulation A: RBC B: Segmented neutrophil C: Band D: Eosinophil E: Basophil F: Lymphocyte G: Monocyte H: Platelet Peripheral blood, Wright stain Fig 1 -1 Rodak BF, Fritsma GA, Keohane EM. Hematology-Clinical Principles and Applications, Elsevier, 2012, p 2. Copyright © 2012, 2007, 2002, 1995 by Saunders, an imprint of Elsevier Inc. 14
Hemostasis • Definition: “stop bleeding” • In laboratory, MLS can test ØPlatelets formation of the primary platelet plug ØCoagulation factors formation of fibrin clot ØRoutine tests Ø PT : prothrombin time Ø APTT: activated partial thromboplastin time ØFibrinolysis of clot when no longer needed 15
Advanced Procedures • Bone Marrow Assays • Aspirates • Biopsies • Cytochemical Stains • • Myeloperoxidase stain (MPO) Sudan Black B stain (SBB) Esterase tests Acid and alkaline phosphatase (LAP) 16
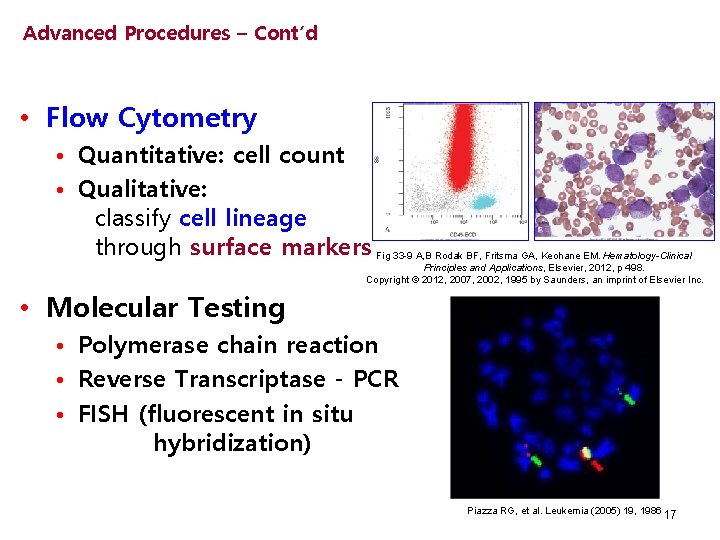
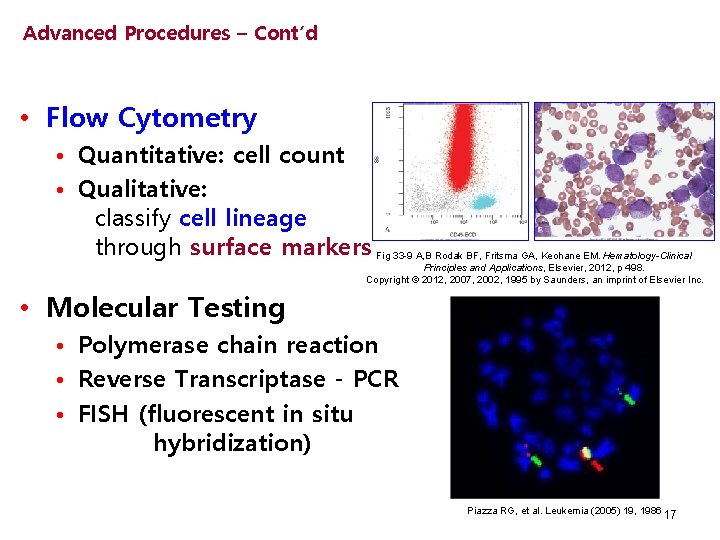
Advanced Procedures – Cont’d • Flow Cytometry • Quantitative: cell count • Qualitative: classify cell lineage through surface markers Fig 33 -9 A, B Rodak BF, Fritsma GA, Keohane EM. Hematology-Clinical Principles and Applications, Elsevier, 2012, p 498. Copyright © 2012, 2007, 2002, 1995 by Saunders, an imprint of Elsevier Inc. • Molecular Testing • Polymerase chain reaction • Reverse Transcriptase - PCR • FISH (fluorescent in situ hybridization) Piazza RG, et al. Leukemia (2005) 19, 1986 17

Any Questions? 18
CELLULAR STRUCTURE AND FUNCTION Chapter 6 Chapter Author: Elaine M. Keohane 19
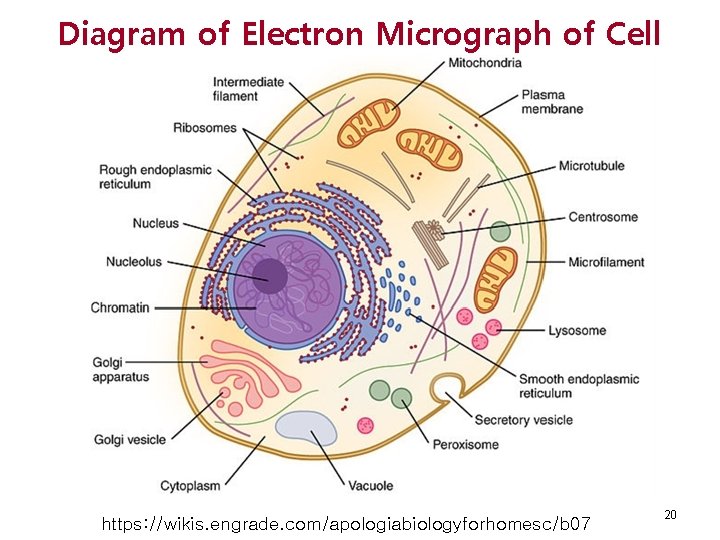
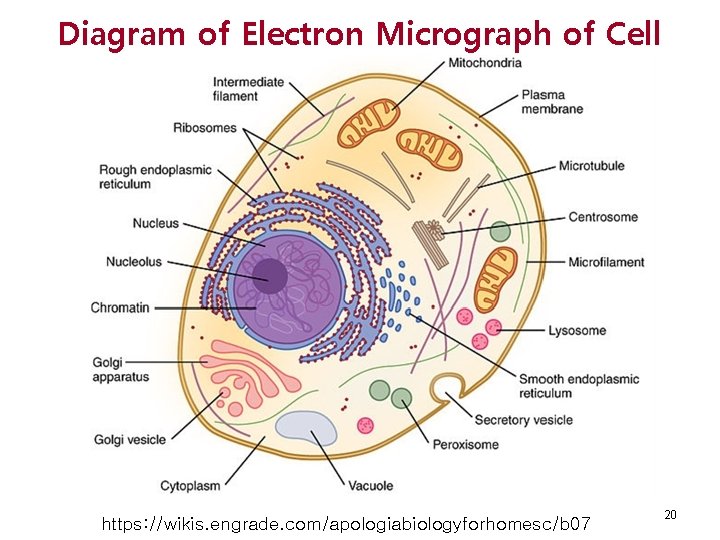
Diagram of Electron Micrograph of Cell https: //wikis. engrade. com/apologiabiologyforhomesc/b 07 20
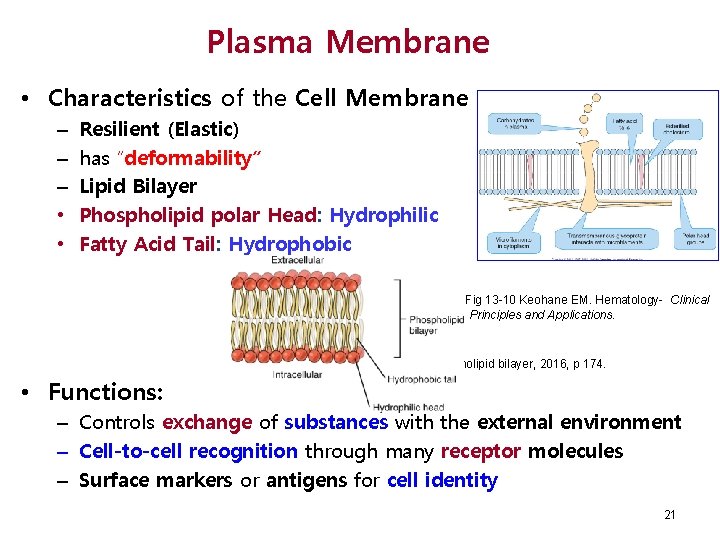
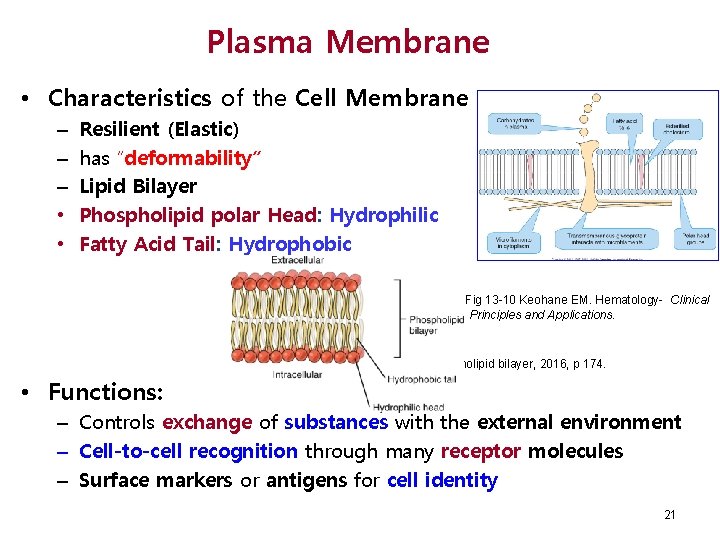
Plasma Membrane • Characteristics of the Cell Membrane – – – • • Resilient (Elastic) has “deformability” Lipid Bilayer Phospholipid polar Head: Hydrophilic Fatty Acid Tail: Hydrophobic Fig 13 -10 Keohane EM. Hematology- Clinical Principles and Applications. Phospholipid bilayer, 2016, p 174. • Functions: – Controls exchange of substances with the external environment – Cell-to-cell recognition through many receptor molecules – Surface markers or antigens for cell identity 21
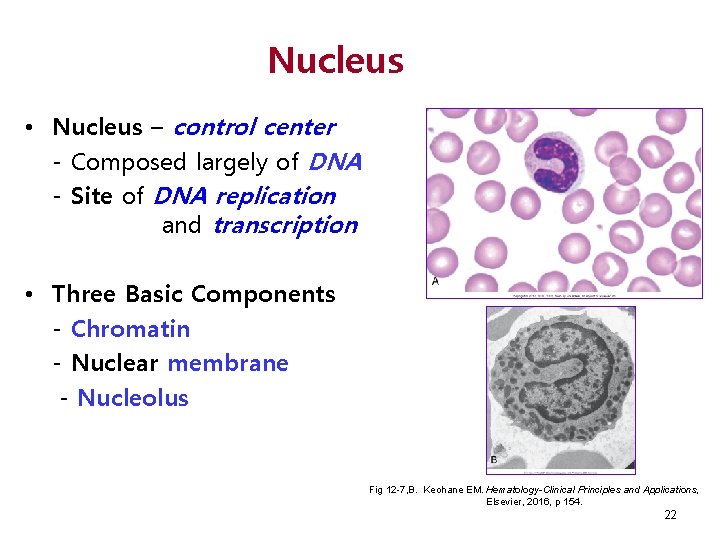
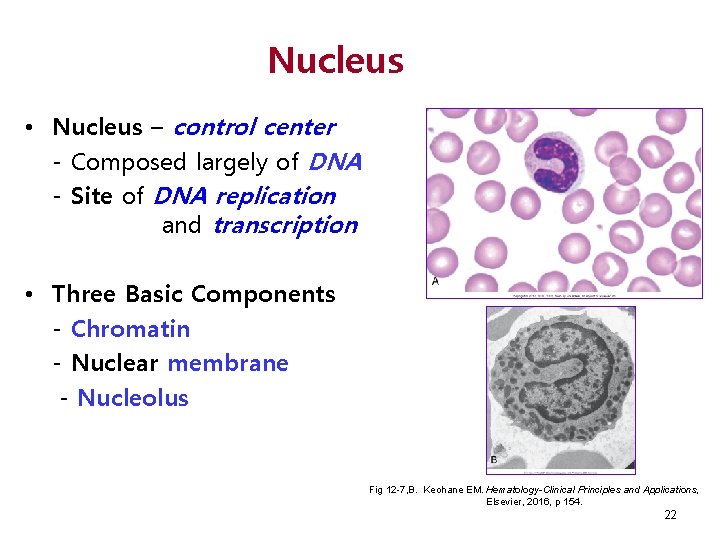
Nucleus • Nucleus – control center - Composed largely of DNA - Site of DNA replication and transcription • Three Basic Components - Chromatin - Nuclear membrane - Nucleolus Fig 12 -7, B. Keohane EM. Hematology-Clinical Principles and Applications, Elsevier, 2016, p 154. 22
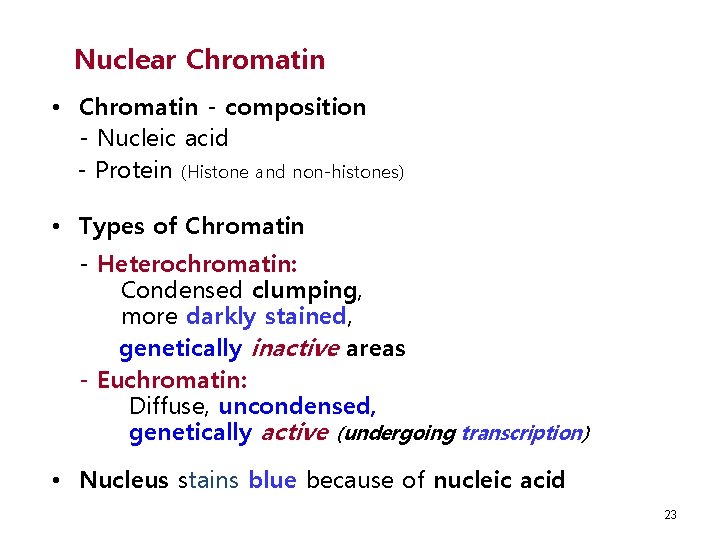
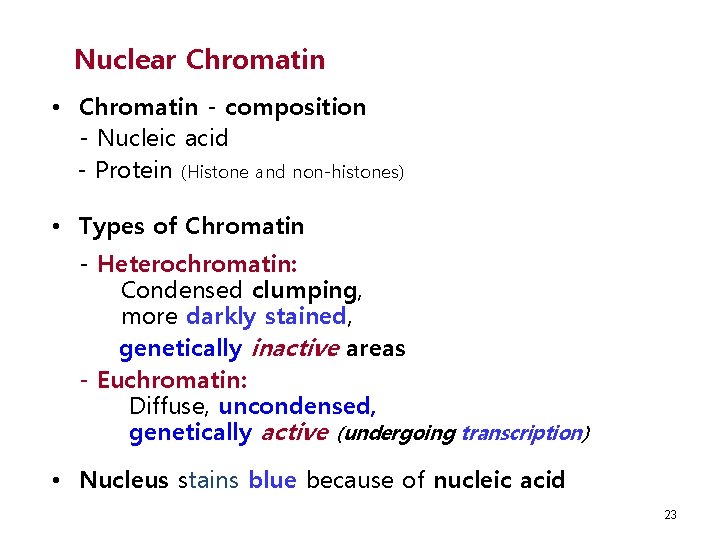
Nuclear Chromatin • Chromatin - composition - Nucleic acid - Protein (Histone and non-histones) • Types of Chromatin - Heterochromatin: Condensed clumping, more darkly stained, genetically inactive areas - Euchromatin: Diffuse, uncondensed, genetically active (undergoing transcription) • Nucleus stains blue because of nucleic acid 23
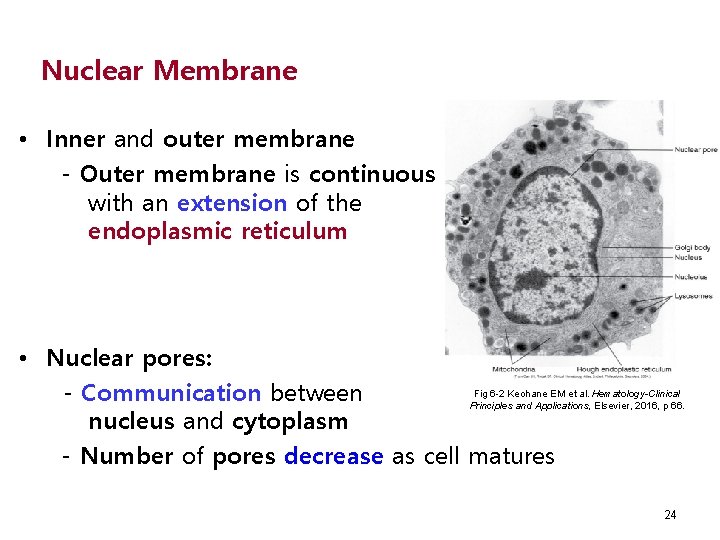
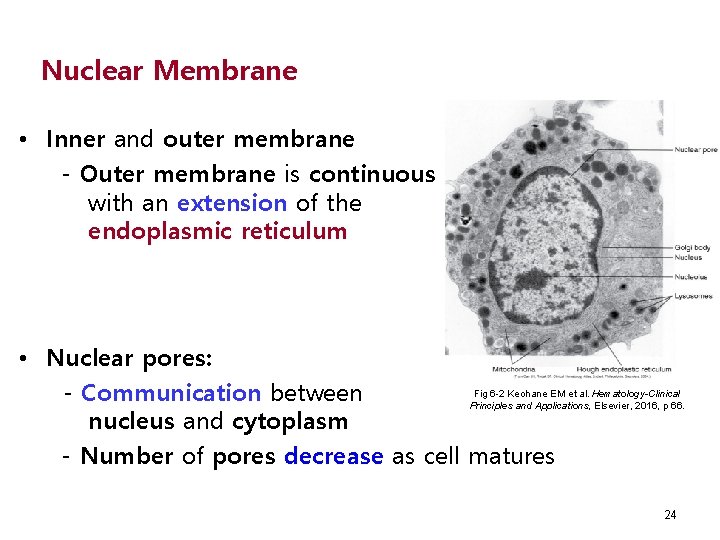
Nuclear Membrane • Inner and outer membrane - Outer membrane is continuous with an extension of the endoplasmic reticulum • Nuclear pores: Fig 6 -2 Keohane EM et al. Hematology-Clinical - Communication between Principles and Applications, Elsevier, 2016, p 66. nucleus and cytoplasm - Number of pores decrease as cell matures 24
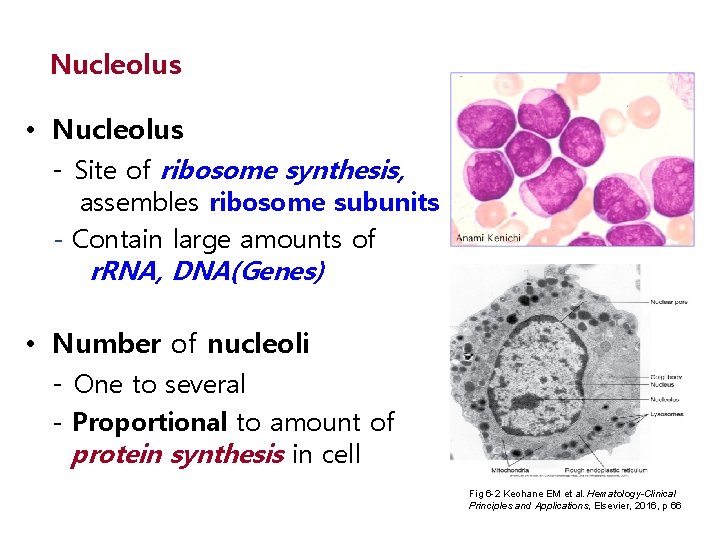
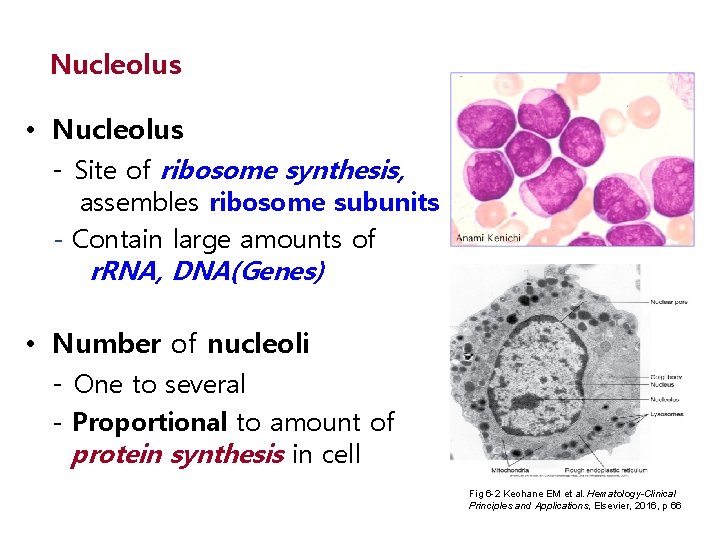
Nucleolus • Nucleolus - Site of ribosome synthesis, assembles ribosome subunits - Contain large amounts of r. RNA, DNA(Genes) • Number of nucleoli - One to several - Proportional to amount of protein synthesis in cell Fig 6 -2 Keohane EM et al. Hematology-Clinical Principles and Applications, Elsevier, 2016, p 66
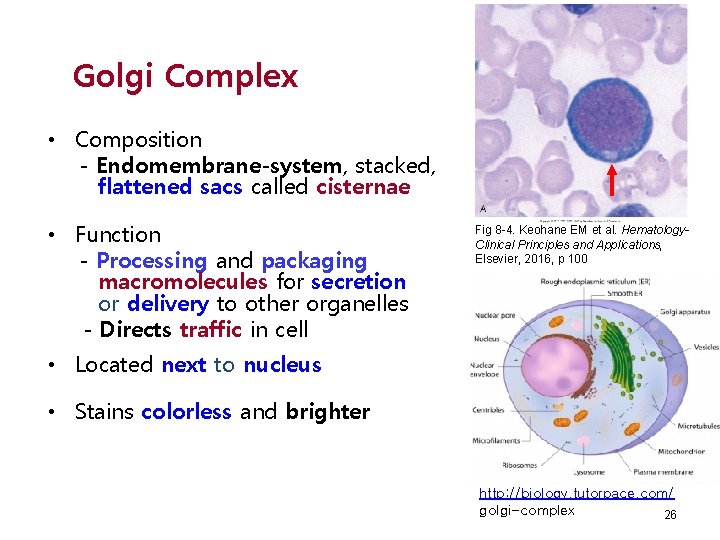
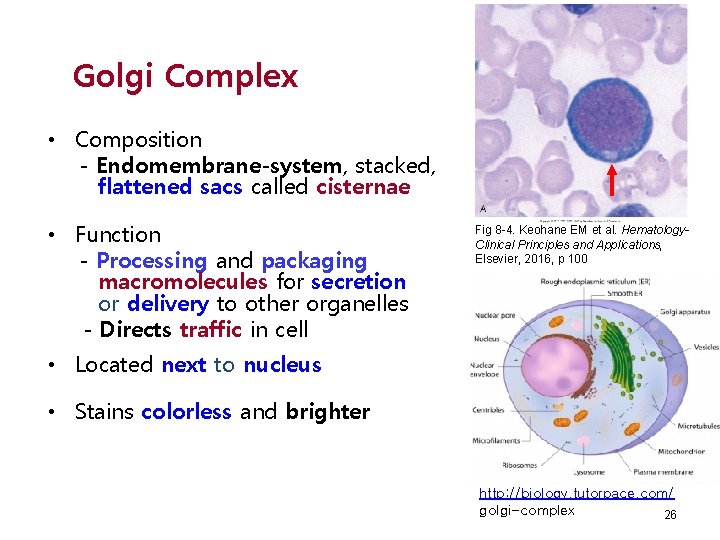
Golgi Complex • Composition - Endomembrane-system, stacked, flattened sacs called cisternae • Function - Processing and packaging macromolecules for secretion or delivery to other organelles - Directs traffic in cell Fig 8 -4. Keohane EM et al. Hematology. Clinical Principles and Applications, Elsevier, 2016, p 100 • Located next to nucleus • Stains colorless and brighter http: //biology. tutorpace. com/ golgi-complex 26
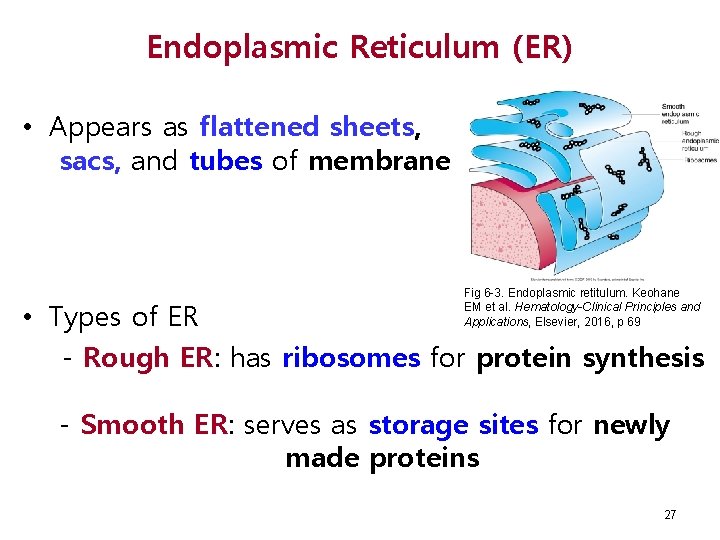
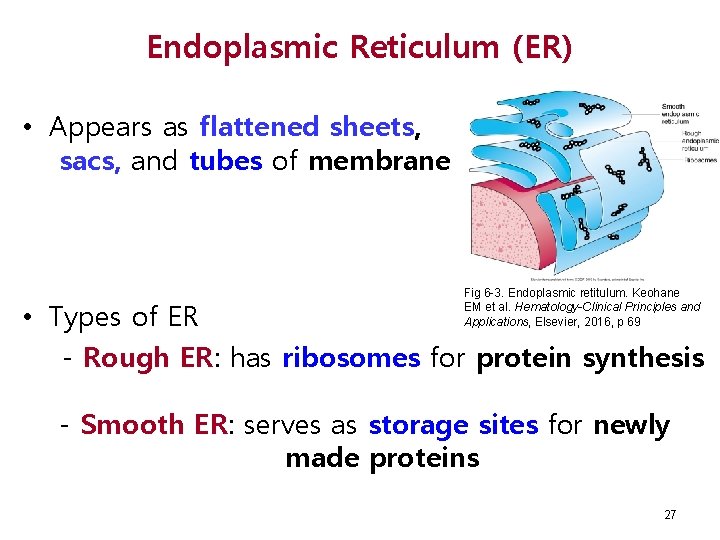
Endoplasmic Reticulum (ER) • Appears as flattened sheets, sacs, and tubes of membrane Fig 6 -3. Endoplasmic retitulum. Keohane EM et al. Hematology-Clinical Principles and Applications, Elsevier, 2016, p 69 • Types of ER - Rough ER: has ribosomes for protein synthesis - Smooth ER: serves as storage sites for newly made proteins 27
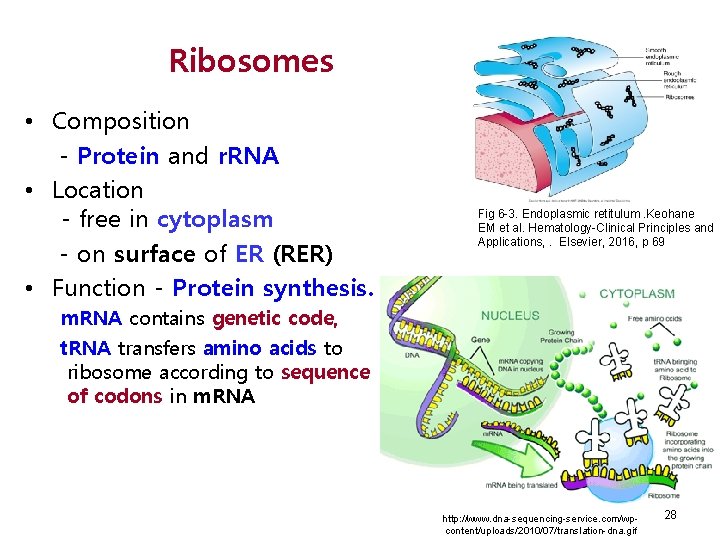
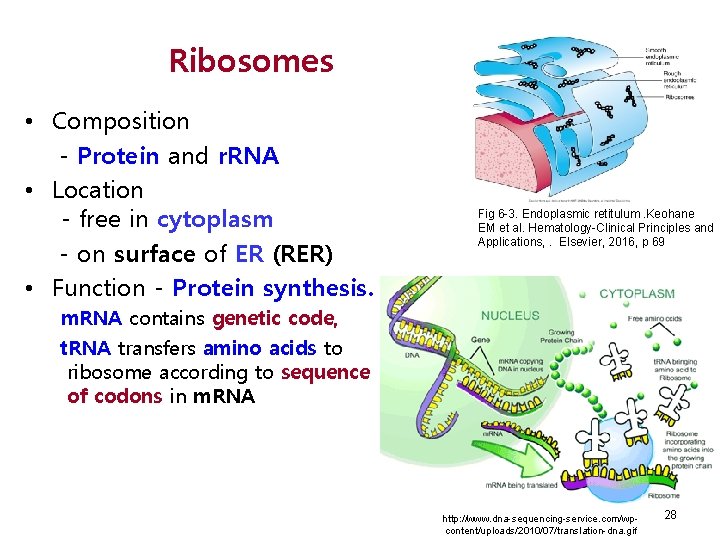
Ribosomes • Composition - Protein and r. RNA • Location - free in cytoplasm - on surface of ER (RER) • Function - Protein synthesis. Fig 6 -3. Endoplasmic retitulum. Keohane EM et al. Hematology-Clinical Principles and Applications, . Elsevier, 2016, p 69 m. RNA contains genetic code, t. RNA transfers amino acids to ribosome according to sequence of codons in m. RNA http: //www. dna-sequencing-service. com/wpcontent/uploads/2010/07/translation-dna. gif 28
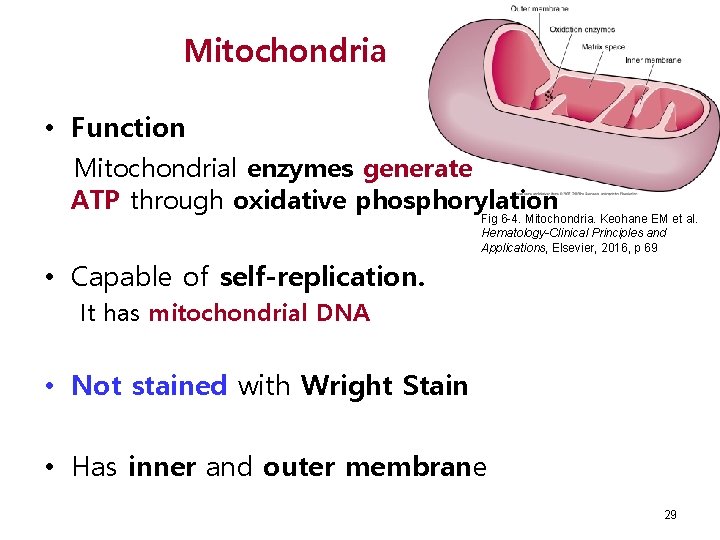
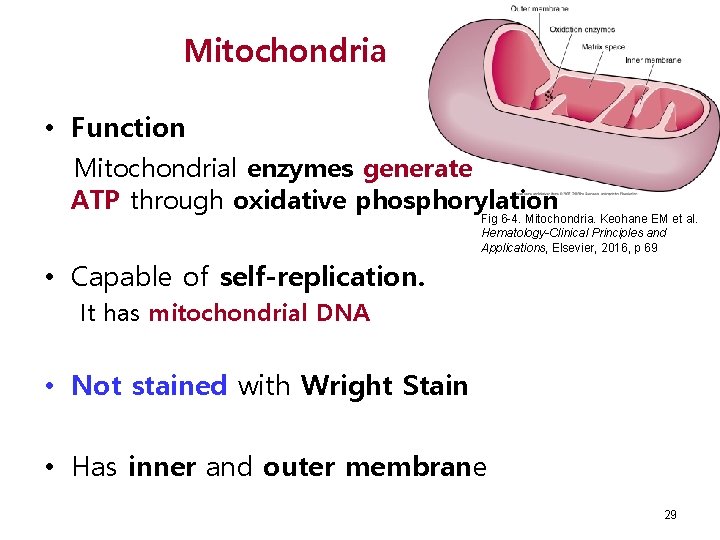
Mitochondria • Function Mitochondrial enzymes generate ATP through oxidative phosphorylation Fig 6 -4. Mitochondria. Keohane EM et al. Hematology-Clinical Principles and Applications, Elsevier, 2016, p 69 • Capable of self-replication. It has mitochondrial DNA • Not stained with Wright Stain • Has inner and outer membrane 29
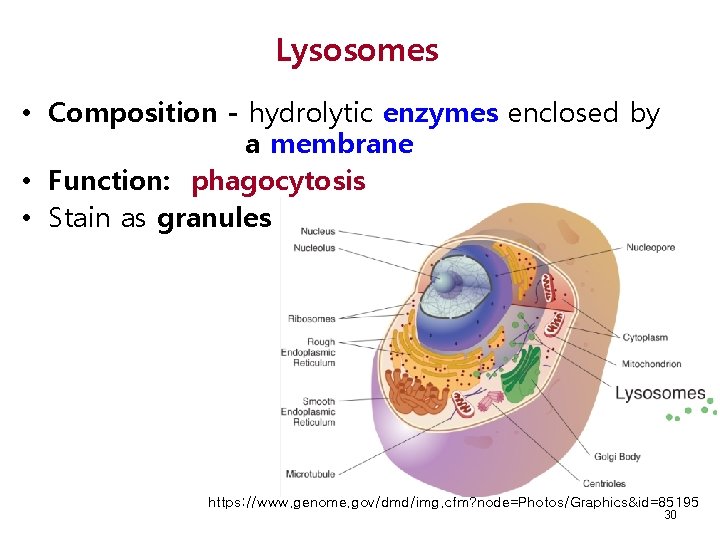
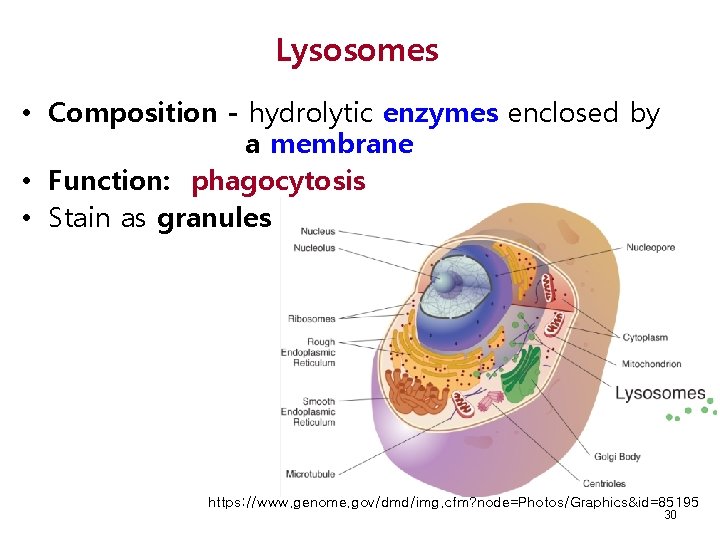
Lysosomes • Composition - hydrolytic enzymes enclosed by a membrane • Function: phagocytosis • Stain as granules https: //www. genome. gov/dmd/img. cfm? node=Photos/Graphics&id=85195 30
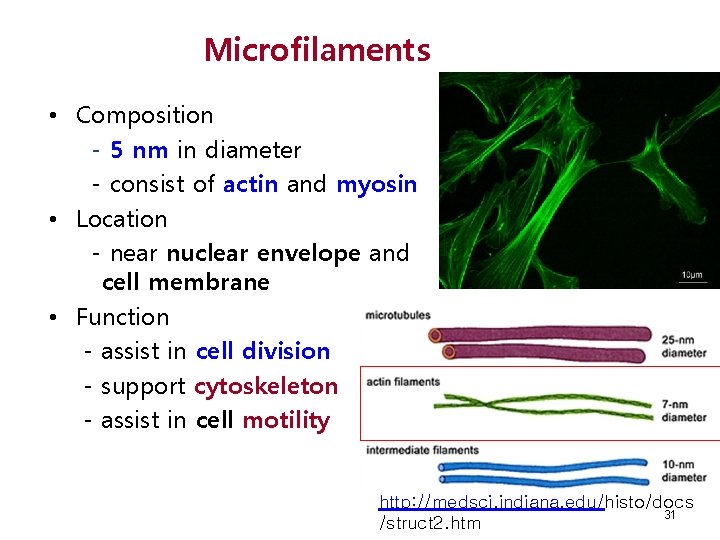
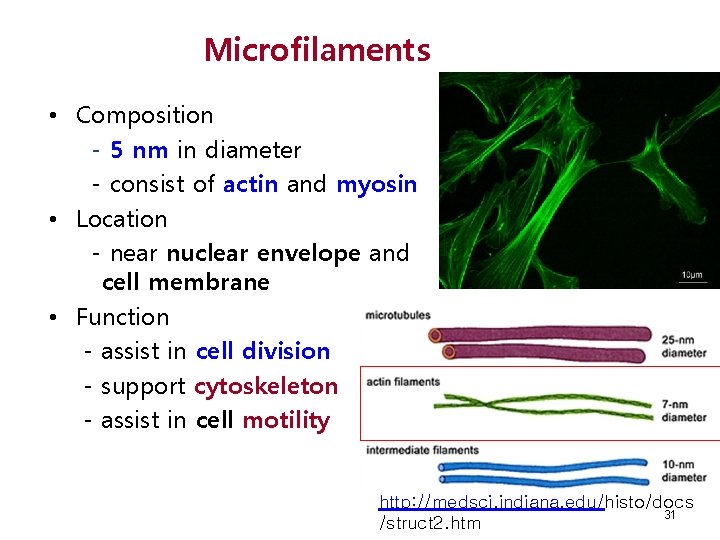
Microfilaments • Composition - 5 nm in diameter - consist of actin and myosin • Location - near nuclear envelope and cell membrane • Function - assist in cell division - support cytoskeleton - assist in cell motility http: //medsci. indiana. edu/histo/docs 31 /struct 2. htm
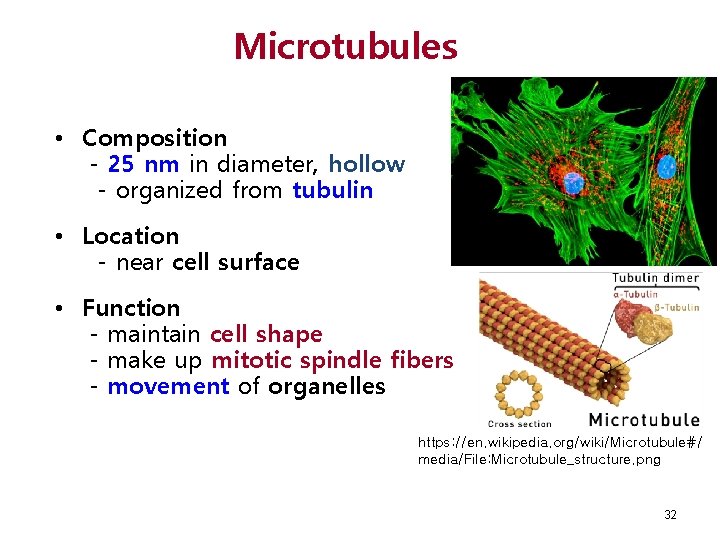
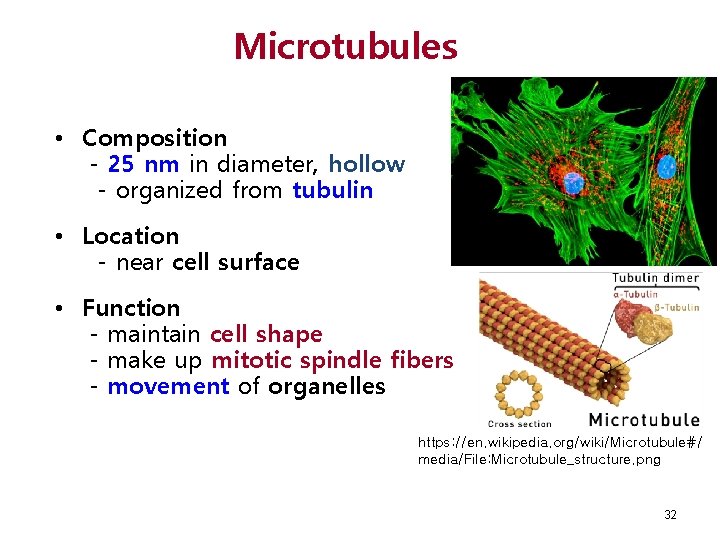
Microtubules • Composition - 25 nm in diameter, hollow - organized from tubulin • Location - near cell surface • Function - maintain cell shape - make up mitotic spindle fibers - movement of organelles https: //en. wikipedia. org/wiki/Microtubule#/ media/File: Microtubule_structure. png 32
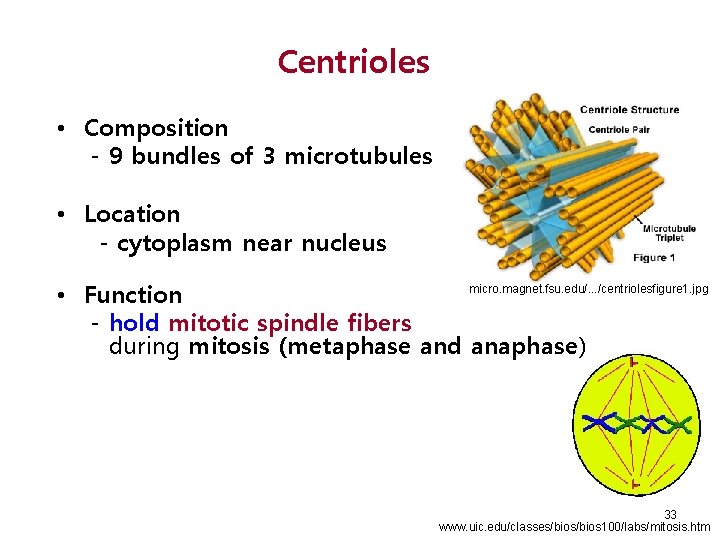
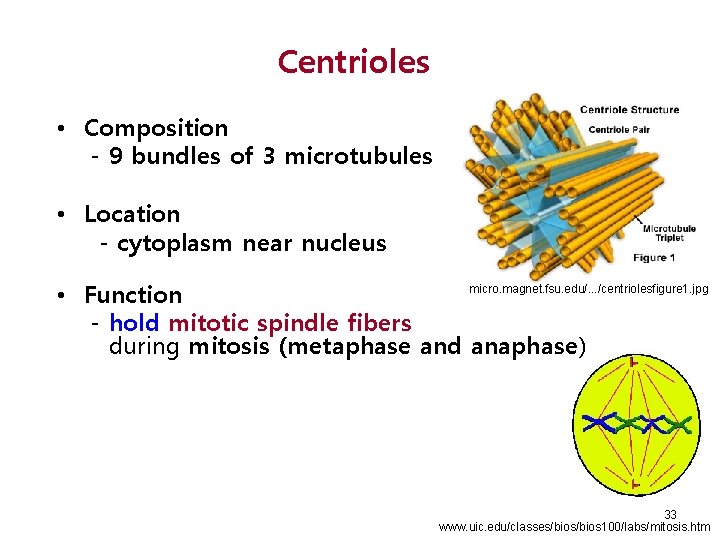
Centrioles • Composition - 9 bundles of 3 microtubules • Location - cytoplasm near nucleus micro. magnet. fsu. edu/. . . /centriolesfigure 1. jpg • Function - hold mitotic spindle fibers during mitosis (metaphase and anaphase) 33 www. uic. edu/classes/bios 100/labs/mitosis. htm

Hematopoietic Microenvironment • BM microenvironment helps for HSCs’ self-renewal, proliferation, differentiation and apoptosis, and support developing progenitor cells • The protective environment is provided by stromal cells (fibroblast etc. ) that secrete substances that form extracellular matrix (ECM) 34
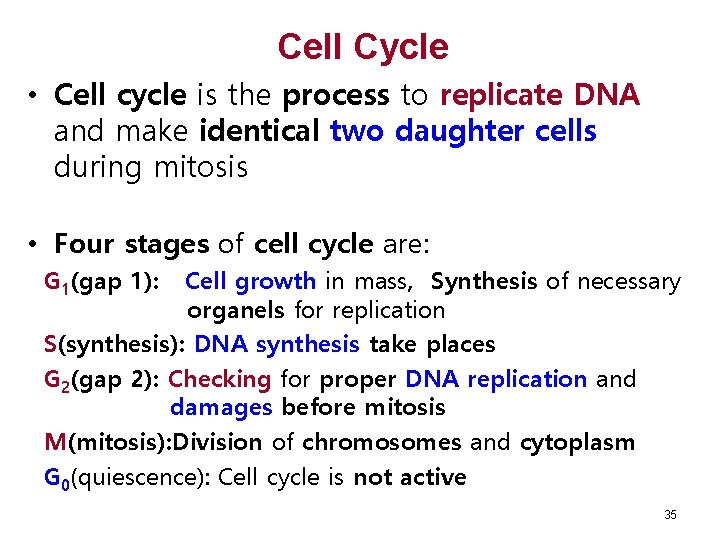
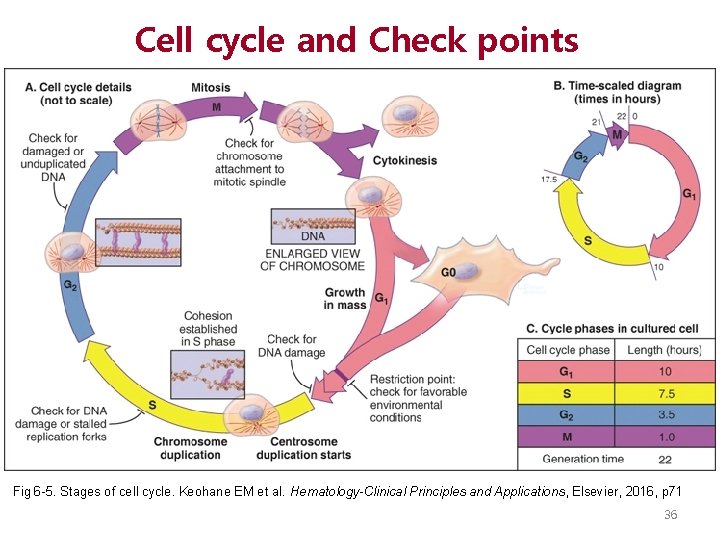
Cell Cycle • Cell cycle is the process to replicate DNA and make identical two daughter cells during mitosis • Four stages of cell cycle are: G 1(gap 1): Cell growth in mass, Synthesis of necessary organels for replication S(synthesis): DNA synthesis take places G 2(gap 2): Checking for proper DNA replication and damages before mitosis M(mitosis): Division of chromosomes and cytoplasm G 0(quiescence): Cell cycle is not active 35
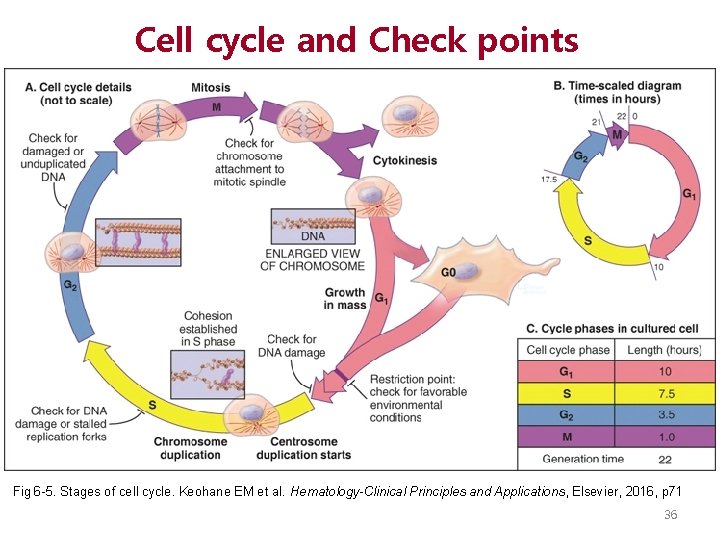
Cell cycle and Check points Fig 6 -5. Stages of cell cycle. Keohane EM et al. Hematology-Clinical Principles and Applications, Elsevier, 2016, p 71 36
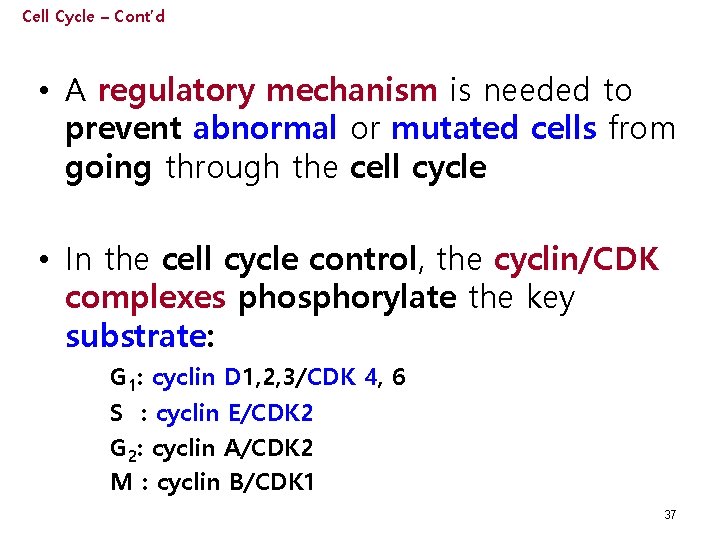
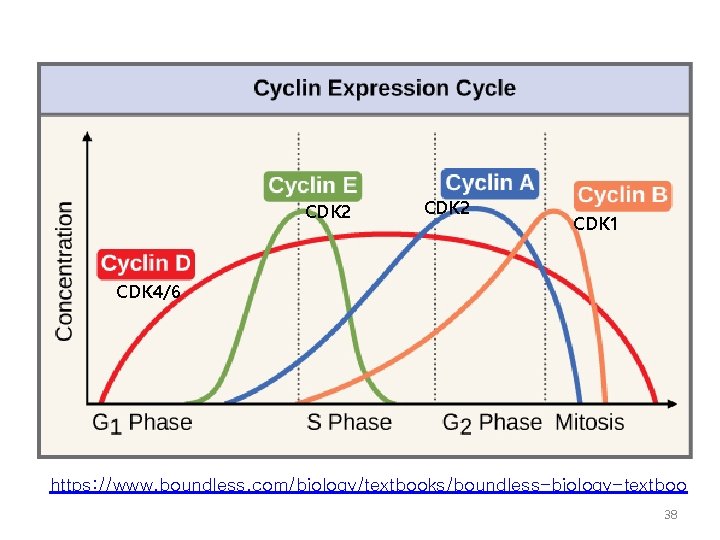
Cell Cycle – Cont’d • A regulatory mechanism is needed to prevent abnormal or mutated cells from going through the cell cycle • In the cell cycle control, the cyclin/CDK complexes phosphorylate the key substrate: G 1: cyclin D 1, 2, 3/CDK 4, 6 S : cyclin E/CDK 2 G 2: cyclin A/CDK 2 M : cyclin B/CDK 1 37
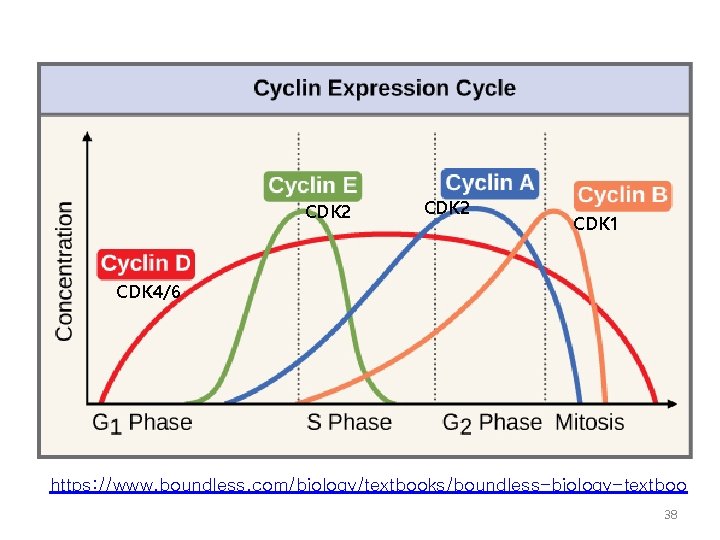
CDK 2 CDK 1 CDK 4/6 https: //www. boundless. com/biology/textbooks/boundless-biology-textboo 38
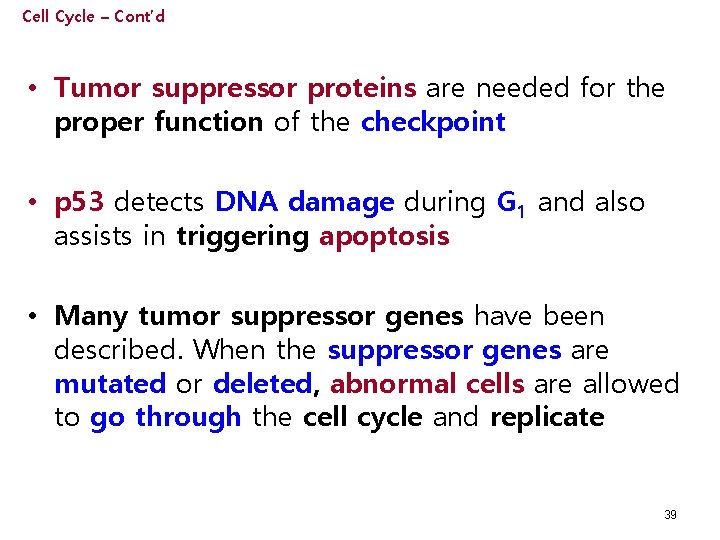
Cell Cycle – Cont’d • Tumor suppressor proteins are needed for the proper function of the checkpoint • p 53 detects DNA damage during G 1 and also assists in triggering apoptosis • Many tumor suppressor genes have been described. When the suppressor genes are mutated or deleted, abnormal cells are allowed to go through the cell cycle and replicate 39

Cell Death • Apoptosis – Cell death by activation of internal pathways – Caused by cell stress, mutations, abnormal growth conditions • Necrosis – Cell death by external damage to cells 40
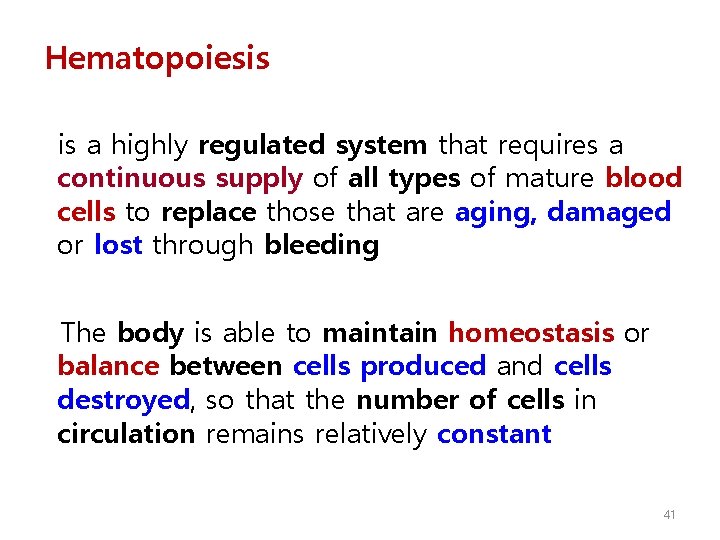
Hematopoiesis is a highly regulated system that requires a continuous supply of all types of mature blood cells to replace those that are aging, damaged or lost through bleeding The body is able to maintain homeostasis or balance between cells produced and cells destroyed, so that the number of cells in circulation remains relatively constant 41
Hematopoiesis – Cont’d Overproduction or underproduction of blood cells has clinical consequences that can be life threatening It has been estimated that the bone marrow of an 60 Kg adult produces approximately 5 million produced per Kg body weight per day: cells per second Cells 3 x 10 RBCs, 2. 5 x 10 Plts, 1. 5 x 10 Granulocytes 9 9 9 The homeostasis can be changed when the BM has to respond to insults such as infection that requires for additional immune cells 42
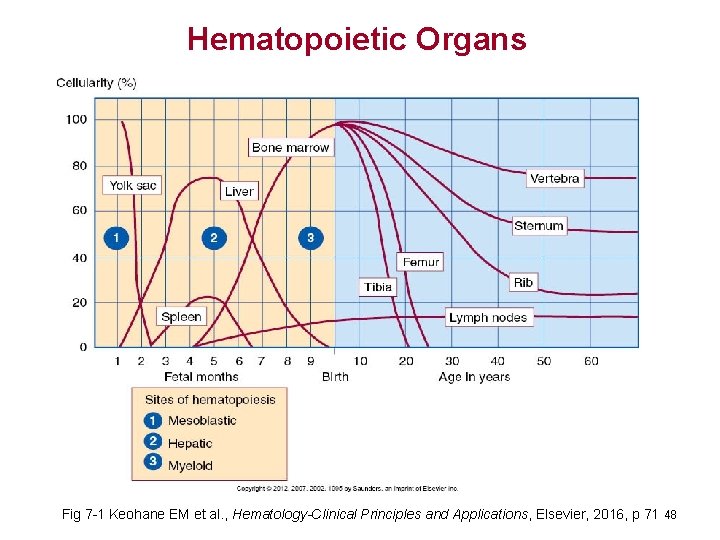
Hematopoiesis – Cont’d • Hematopoietic System • Organs • Bone Marrow • Liver • Spleen • Lymph nodes • Thymus 43
Two signals of the Developing Hematopoietic System • Two signaling: – 1 st Wave: Embryonic wave for embryo support (blood supply). • Hematopoiesis begins in extra-embryonic YS. Yolk Sac is the site of primitive erythropoiesis and macrophage production. – 2 nd Wave: Fetal and adult blood system. • begins in AGM(Aorta-Gonad-Mesonephros) region* where Myeloid and Lymphoid lineages are generated *: Nobuhisa I et al, JEM 2004; 199: 737 44
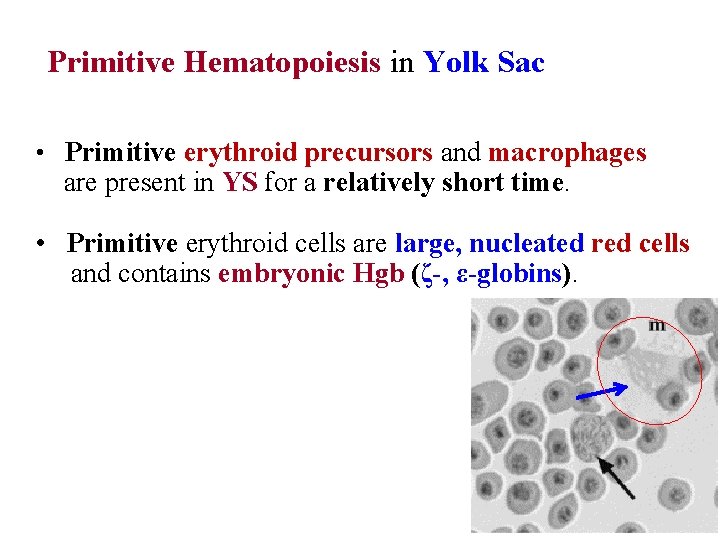
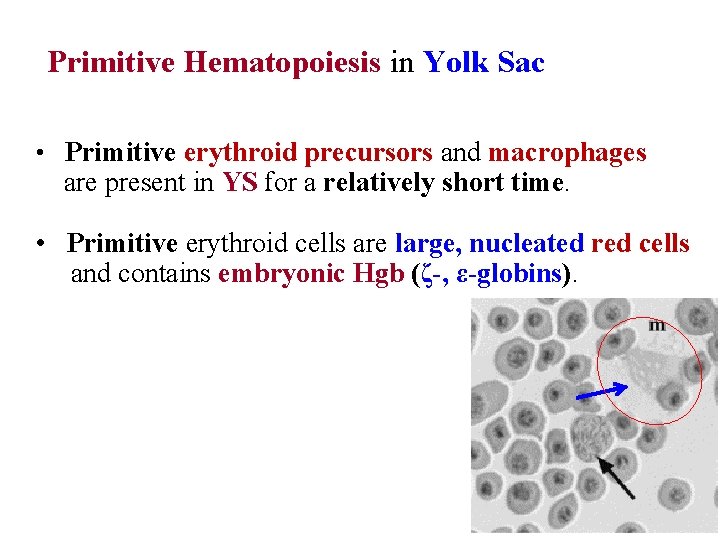
Primitive Hematopoiesis in Yolk Sac • Primitive erythroid precursors and macrophages are present in YS for a relatively short time. • Primitive erythroid cells are large, nucleated red cells and contains embryonic Hgb (ζ-, ε-globins).
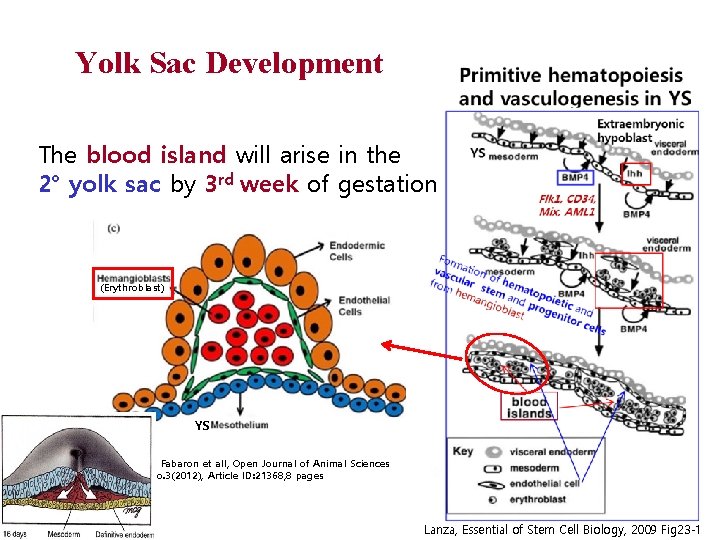
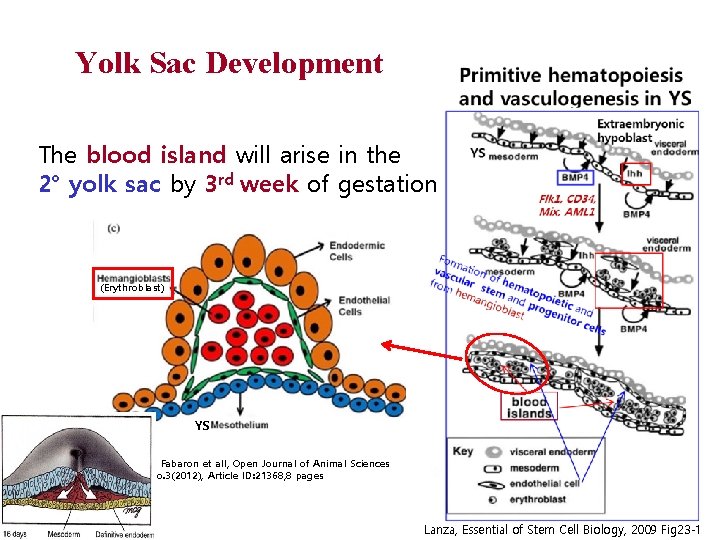
Yolk Sac Development The blood island will arise in the 2° yolk sac by 3 rd week of gestation (Erythroblast) YS Oliveira Fabaron et all, Open Journal of Animal Sciences Vol. 2 No. 3(2012), Article ID: 21368, 8 pages 46 Lanza, Essential of Stem Cell Biology, 2009 Fig 23 -1
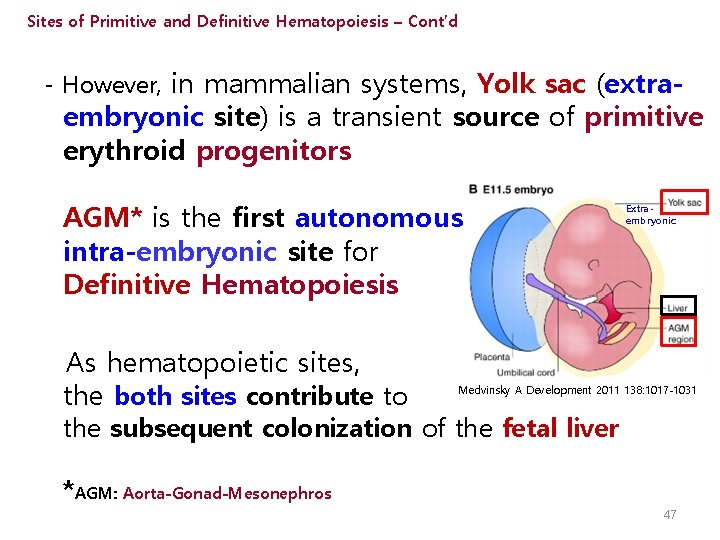
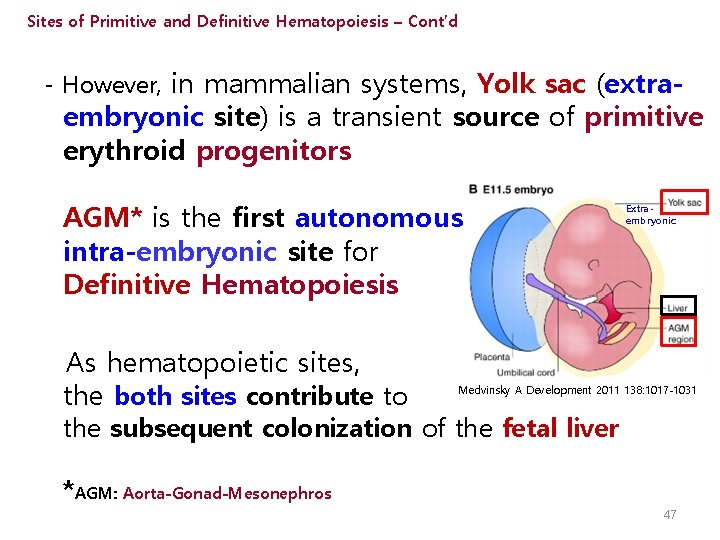
Sites of Primitive and Definitive Hematopoiesis – Cont’d - However, in mammalian systems, Yolk sac (extra- embryonic site) is a transient source of primitive erythroid progenitors AGM* is the first autonomous intra-embryonic site for Definitive Hematopoiesis As hematopoietic sites, the both sites contribute to Extraembryonic Medvinsky A Development 2011 138: 1017 -1031 the subsequent colonization of the fetal liver *AGM: Aorta-Gonad-Mesonephros 47
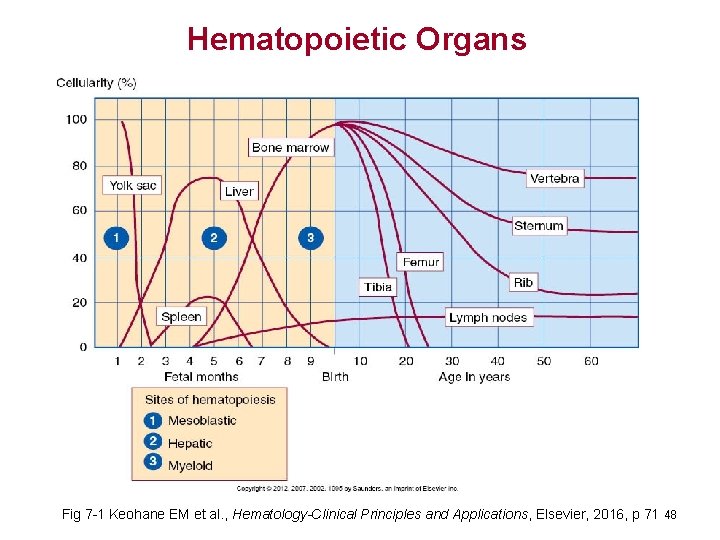
Hematopoietic Organs Fig 7 -1 Keohane EM et al. , Hematology-Clinical Principles and Applications, Elsevier, 2016, p 71 48
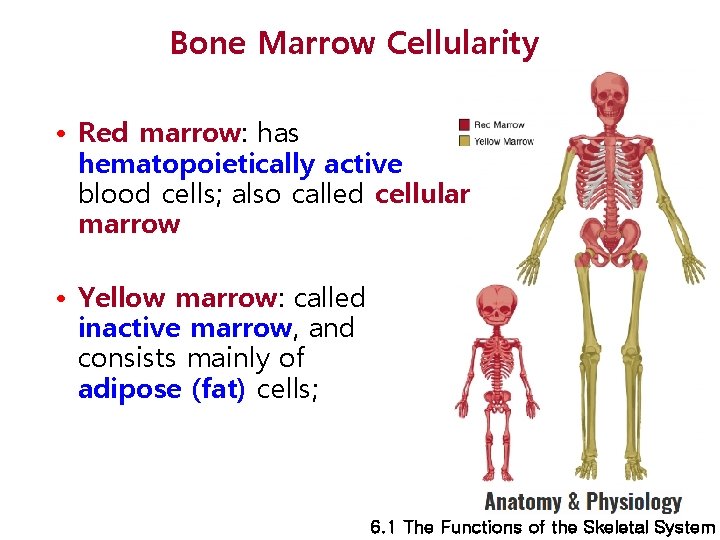
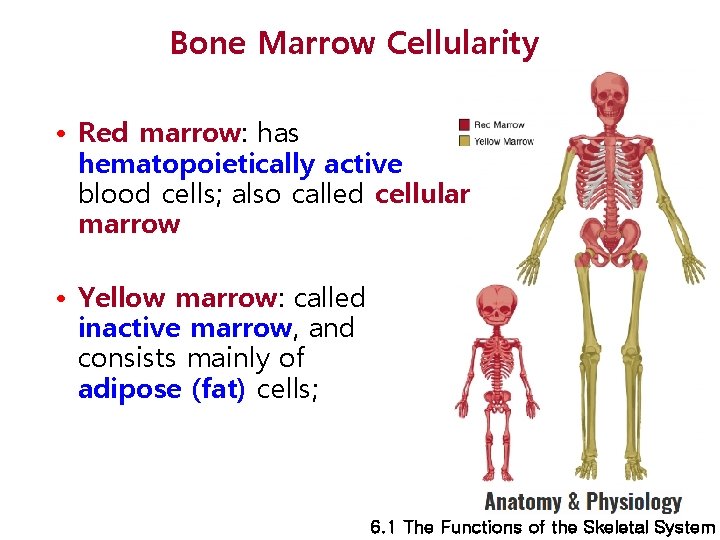
Bone Marrow Cellularity • Red marrow: has hematopoietically active blood cells; also called cellular marrow • Yellow marrow: called inactive marrow, and consists mainly of adipose (fat) cells; 6. 1 The Functions of the Skeletal System
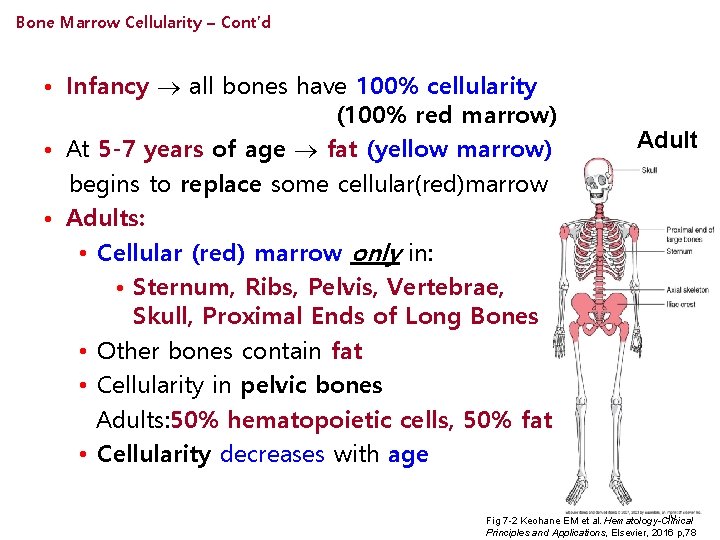
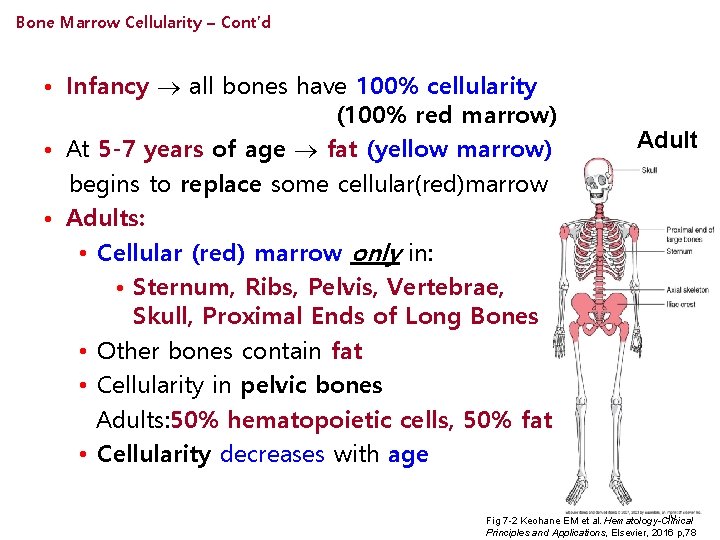
Bone Marrow Cellularity – Cont’d • Infancy all bones have 100% cellularity (100% red marrow) • At 5 -7 years of age fat (yellow marrow) begins to replace some cellular(red)marrow • Adults: • Cellular (red) marrow only in: • Sternum, Ribs, Pelvis, Vertebrae, Skull, Proximal Ends of Long Bones • Other bones contain fat • Cellularity in pelvic bones Adults: 50% hematopoietic cells, 50% fat • Cellularity decreases with age Adult Red areas= cellular marrow White areas= yellow (fat) marrow 50 Fig 7 -2 Keohane EM et al. Hematology-Clinical Principles and Applications, Elsevier, 2016 p, 78
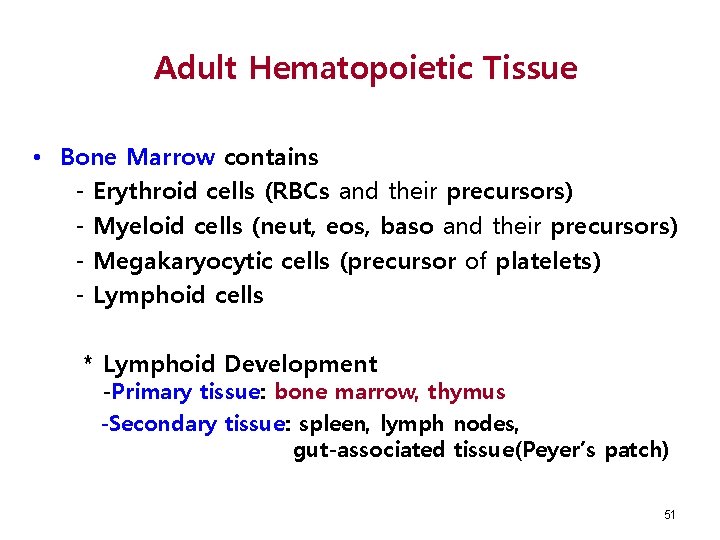
Adult Hematopoietic Tissue • Bone Marrow contains - Erythroid cells (RBCs and their precursors) - Myeloid cells (neut, eos, baso and their precursors) - Megakaryocytic cells (precursor of platelets) - Lymphoid cells * Lymphoid Development -Primary tissue: bone marrow, thymus -Secondary tissue: spleen, lymph nodes, gut-associated tissue(Peyer’s patch) 51
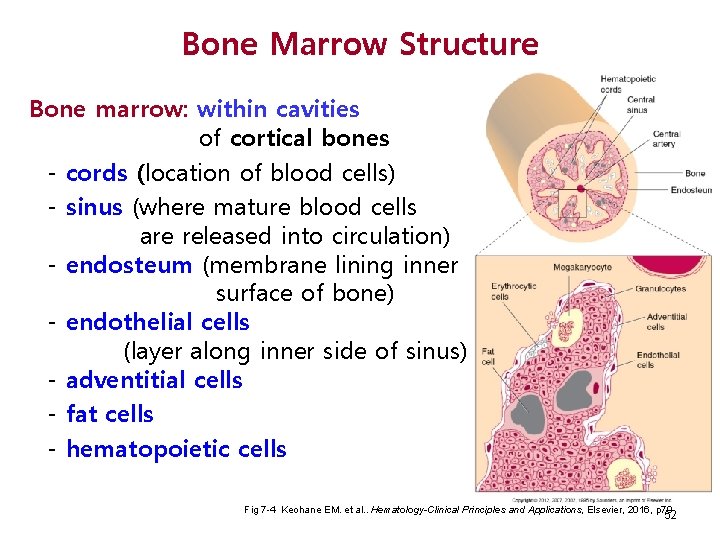
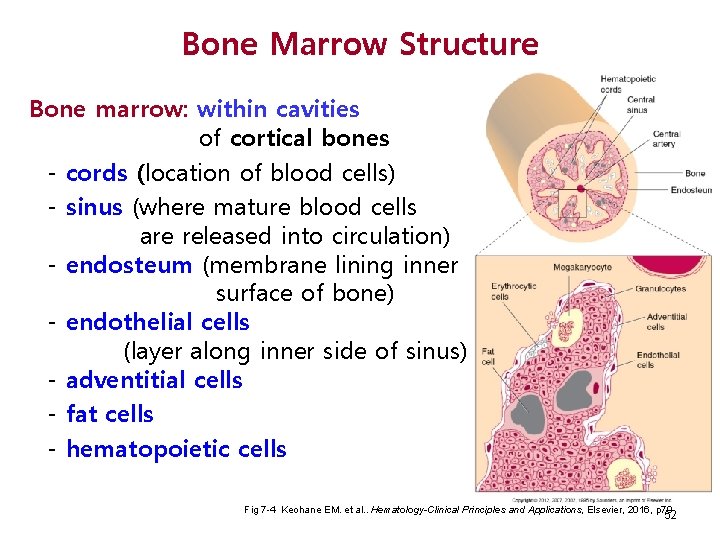
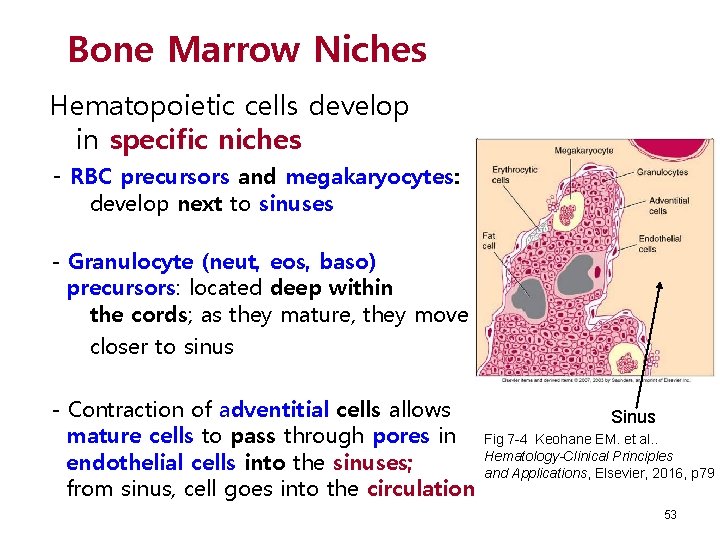
Bone Marrow Structure Bone marrow: within cavities of cortical bones - cords (location of blood cells) - sinus (where mature blood cells are released into circulation) - endosteum (membrane lining inner surface of bone) - endothelial cells (layer along inner side of sinus) - adventitial cells - fat cells - hematopoietic cells Sinus Fig 7 -4 Keohane EM. et al. . Hematology-Clinical Principles and Applications, Elsevier, 2016, p 79 52
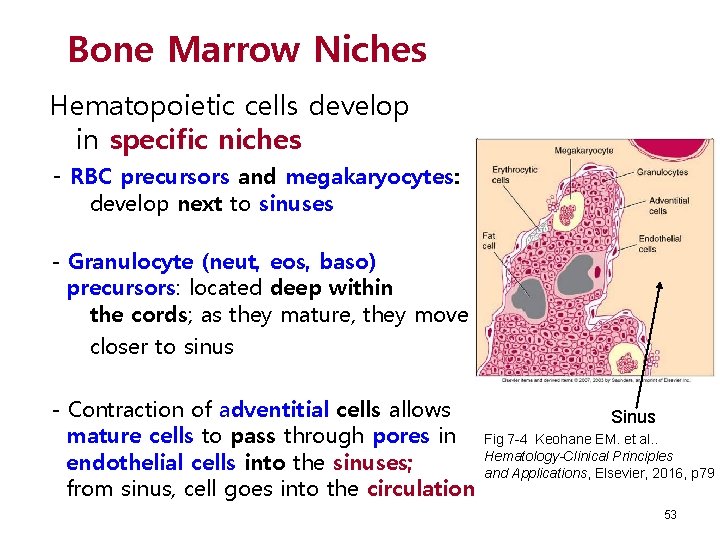
Bone Marrow Niches Hematopoietic cells develop in specific niches - RBC precursors and megakaryocytes: develop next to sinuses - Granulocyte (neut, eos, baso) precursors: located deep within the cords; as they mature, they move closer to sinus - Contraction of adventitial cells allows mature cells to pass through pores in endothelial cells into the sinuses; from sinus, cell goes into the circulation Sinus Fig 7 -4 Keohane EM. et al. . Hematology-Clinical Principles and Applications, Elsevier, 2016, p 79 53
Bone Marrow Microenvironment Consists of Niches • Each niche has specialized stromal cells to maintain favorable microenvironment for a particular type of cell • Stromal cells: • Form semi-fluid extracellular matrix (ECM) for blood cell development • Nurture and protect stem cells and developing blood cells in niches • Help prevent the depletion of stem cells from the bone marrow • Secrete factors that are chemotactic for hematopoietic cells 54
Bone Marrow Stromal Cells • Endothelial cells: cover inner surface of sinus, secrete cytokines • Adipose (fat) cells: secrete adiponectin and other cytokines • Macrophages: phagocytosis; secrete cytokines • Fibroblasts (reticular cells): forms lattice with reticular fibers that supports hematopoietic cells; secretes cytokines • Osteoblasts: bone forming cells • Osteoclasts: bone resorbing cells 55
Extracellular Matrix (ECM) Promotes adhesion of HSCs to matrix Composed of proteins and glycoproteins: – – – Collagen Fibronectin Laminin Hemonectin Thrombospondin 56
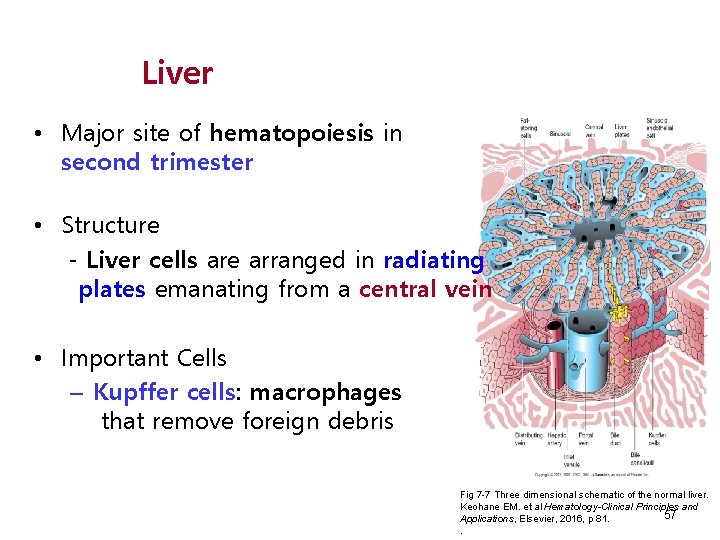
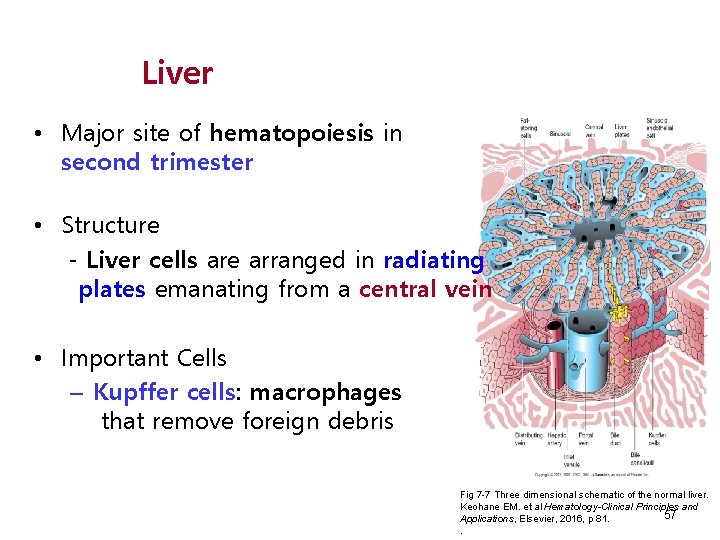
Liver • Major site of hematopoiesis in second trimester • Structure - Liver cells are arranged in radiating plates emanating from a central vein • Important Cells – Kupffer cells: macrophages that remove foreign debris Fig 7 -7 Three dimensional schematic of the normal liver. Keohane EM. et al Hematology-Clinical Principles and 57 Applications, Elsevier, 2016, p 81. .
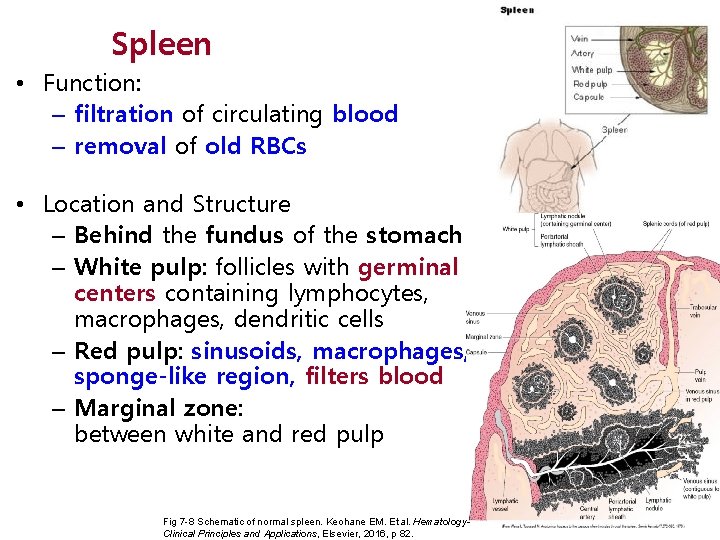
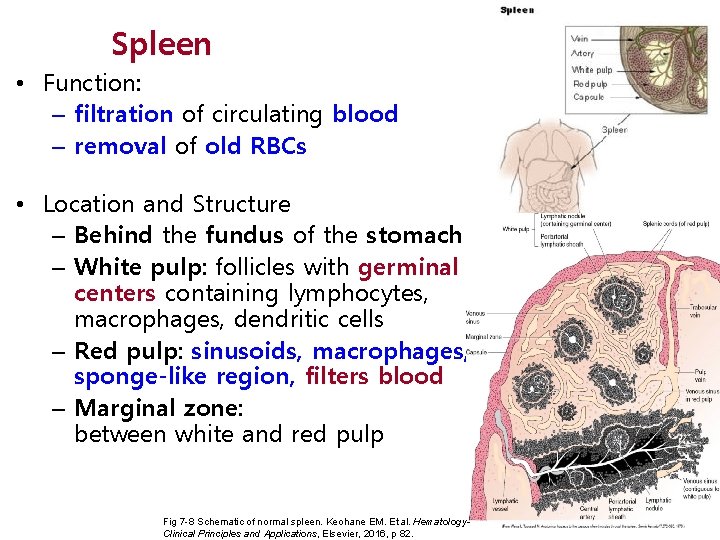
Spleen • Function: – filtration of circulating blood – removal of old RBCs • Location and Structure – Behind the fundus of the stomach – White pulp: follicles with germinal centers containing lymphocytes, macrophages, dendritic cells – Red pulp: sinusoids, macrophages, sponge-like region, filters blood – Marginal zone: between white and red pulp Fig 7 -8 Schematic of normal spleen. Keohane EM. Et al. Hematology. Clinical Principles and Applications, Elsevier, 2016, p 82. 58
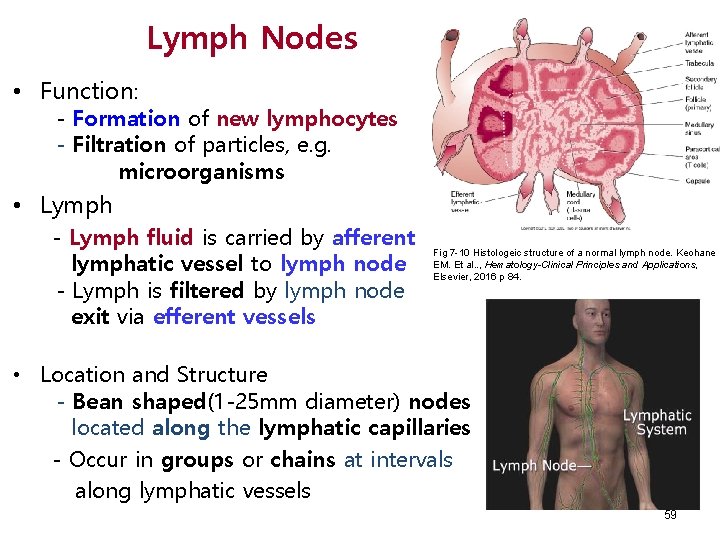
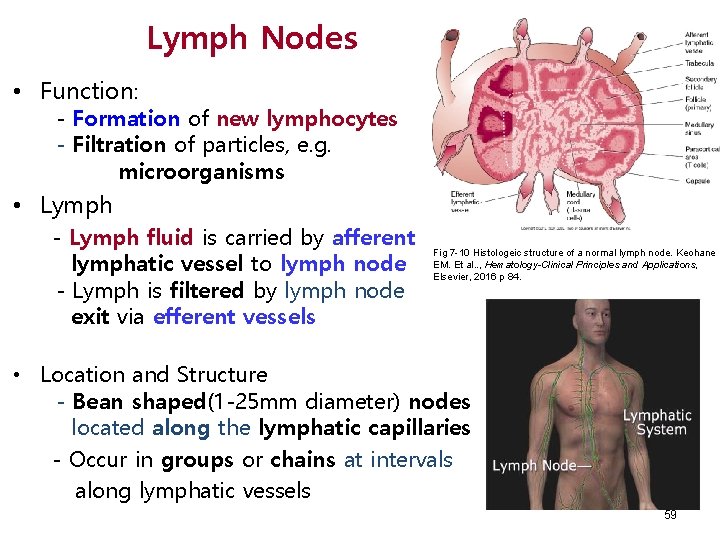
Lymph Nodes • Function: - Formation of new lymphocytes - Filtration of particles, e. g. microorganisms • Lymph - Lymph fluid is carried by afferent lymphatic vessel to lymph node - Lymph is filtered by lymph node exit via efferent vessels Fig 7 -10 Histologeic structure of a normal lymph node. Keohane EM. Et al. . , Hematology-Clinical Principles and Applications, Elsevier, 2016 p 84. • Location and Structure - Bean shaped(1 -25 mm diameter) nodes located along the lymphatic capillaries - Occur in groups or chains at intervals along lymphatic vessels 59
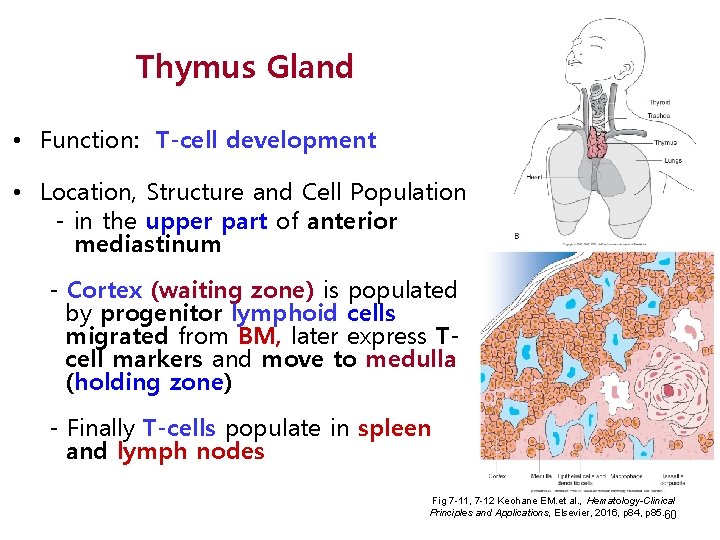
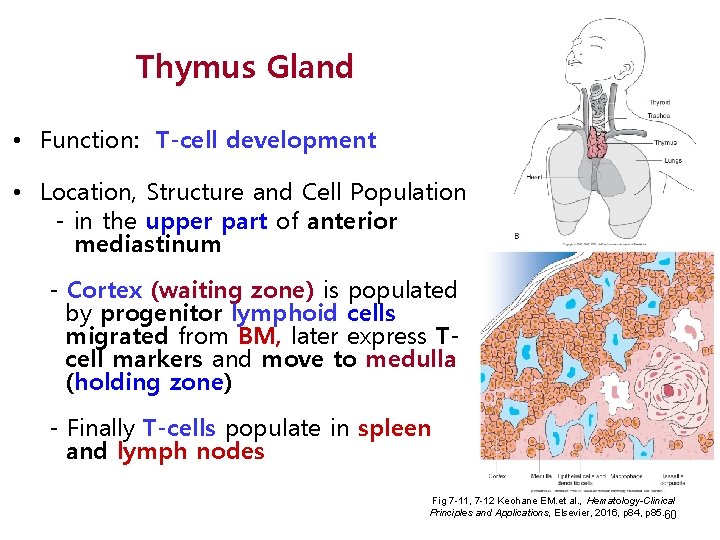
Thymus Gland • Function: T-cell development • Location, Structure and Cell Population - in the upper part of anterior mediastinum - Cortex (waiting zone) is populated by progenitor lymphoid cells migrated from BM, later express Tcell markers and move to medulla (holding zone) - Finally T-cells populate in spleen and lymph nodes Fig 7 -11, 7 -12 Keohane EM. et al. , Hematology-Clinical Principles and Applications, Elsevier, 2016, p 84, p 85. 60
Hematopoietic Cell Compartments • Hematopoietic Stem Cells (HSCs) • Progenitor Cells (PCs) • Committed to certain lineage(s) • Maturing Cells • Morphologically identifyable cells 61
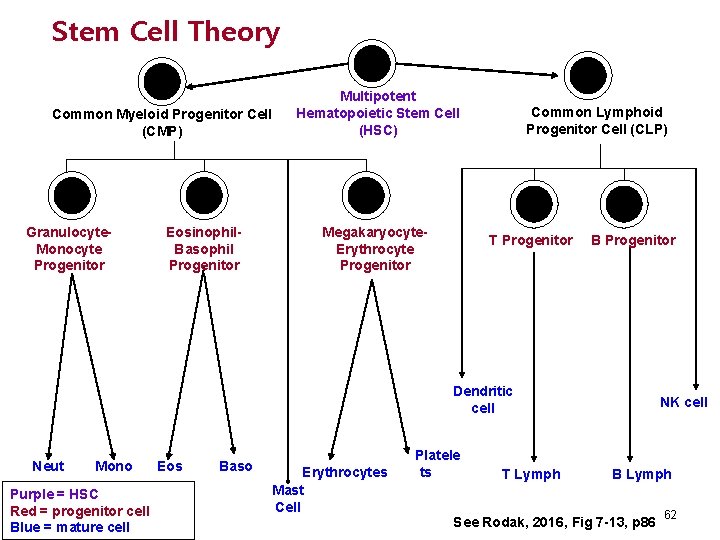
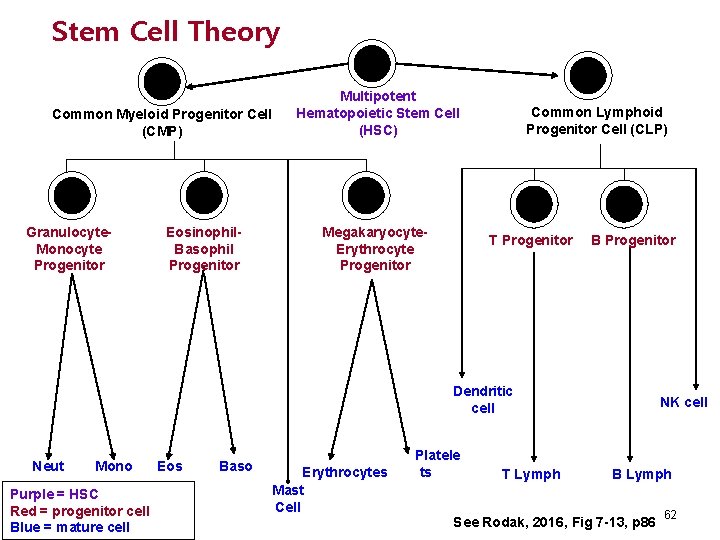
Stem Cell Theory Common Myeloid Progenitor Cell (CMP) Granulocyte. Monocyte Progenitor Eosinophil. Basophil Progenitor Multipotent Hematopoietic Stem Cell (HSC) Megakaryocyte. Erythrocyte Progenitor Common Lymphoid Progenitor Cell (CLP) T Progenitor B Progenitor Dendritic cell Neut Mono Purple = HSC Red = progenitor cell Blue = mature cell Eos Baso Erythrocytes Mast Cell Platele ts T Lymph NK cell B Lymph See Rodak, 2016, Fig 7 -13, p 86 62
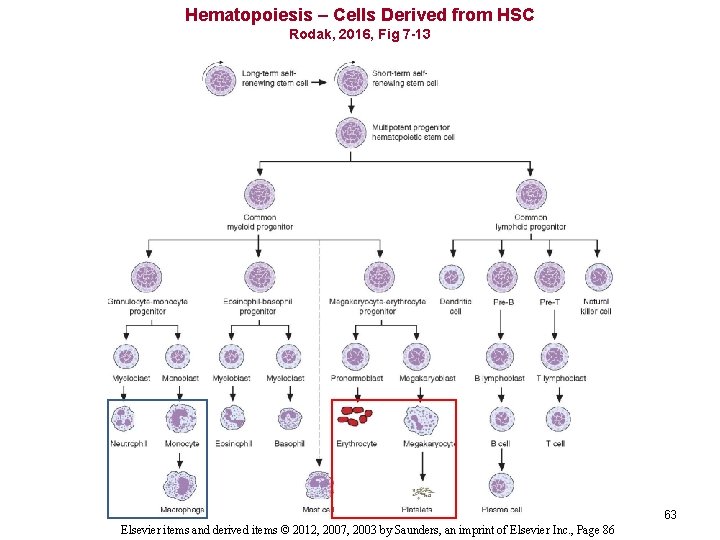
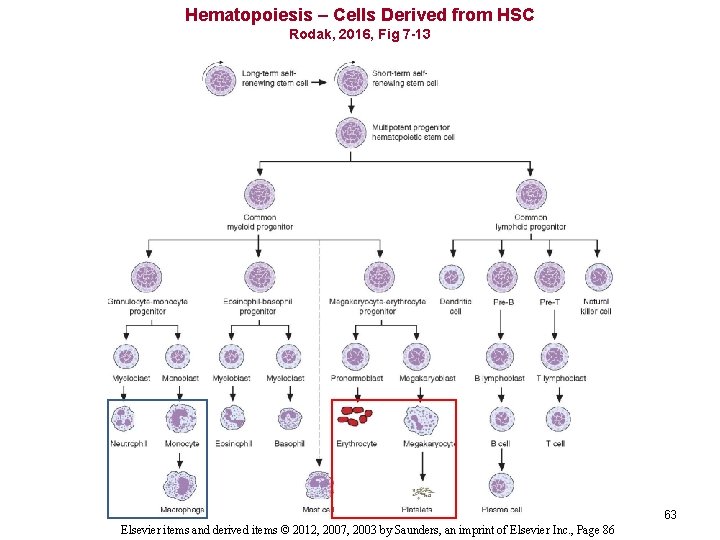
Hematopoiesis – Cells Derived from HSC Rodak, 2016, Fig 7 -13 63 Elsevier items and derived items © 2012, 2007, 2003 by Saunders, an imprint of Elsevier Inc. , Page 86
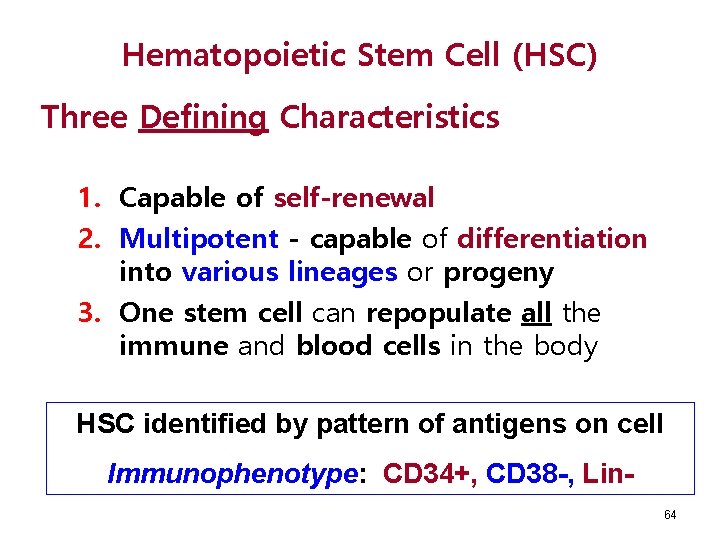
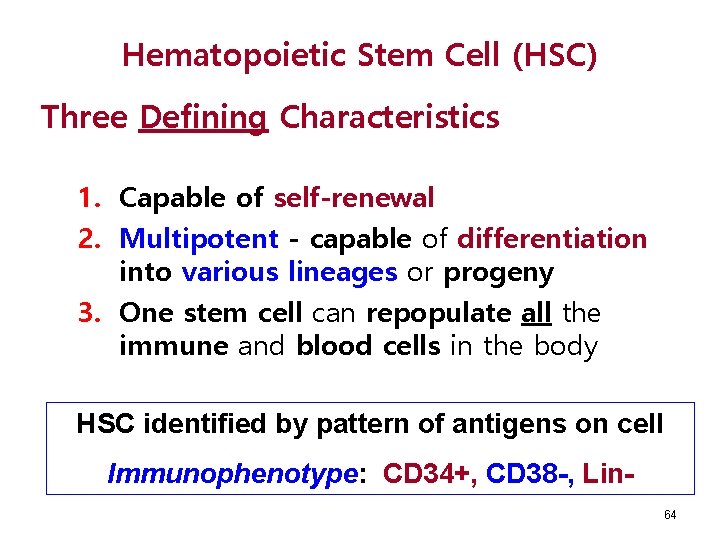
Hematopoietic Stem Cell (HSC) Three Defining Characteristics 1. Capable of self-renewal 2. Multipotent - capable of differentiation into various lineages or progeny 3. One stem cell can repopulate all the immune and blood cells in the body HSC identified by pattern of antigens on cell Immunophenotype: CD 34+, CD 38 -, Lin 64
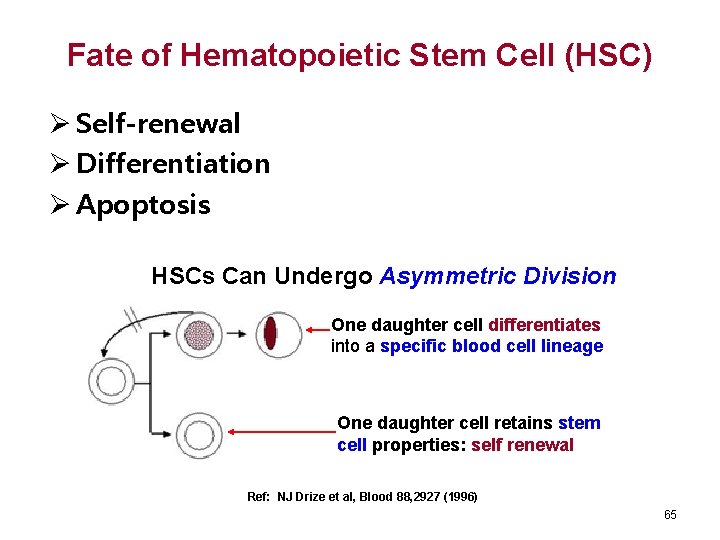
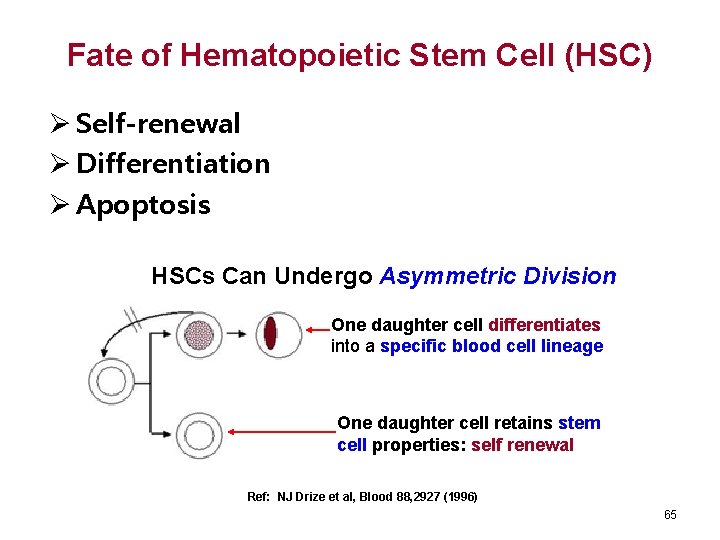
Fate of Hematopoietic Stem Cell (HSC) Ø Self-renewal Ø Differentiation Ø Apoptosis HSCs Can Undergo Asymmetric Division One daughter cell differentiates into a specific blood cell lineage One daughter cell retains stem cell properties: self renewal Ref: NJ Drize et al, Blood 88, 2927 (1996) 65
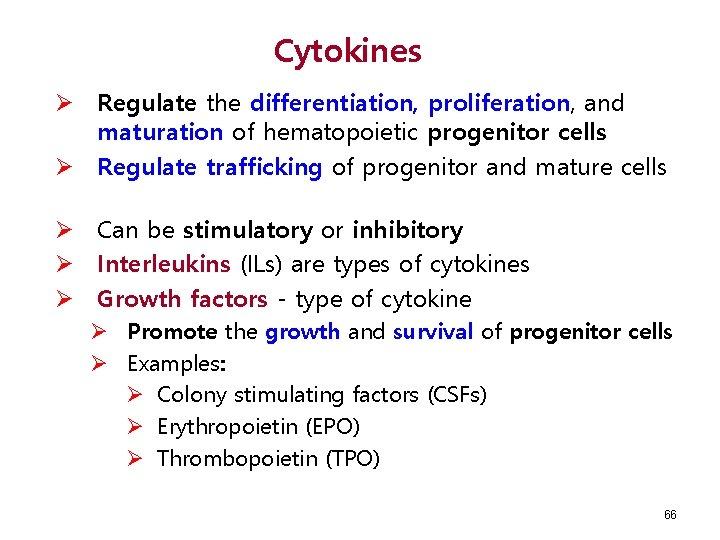
Cytokines Ø Regulate the differentiation, proliferation, and maturation of hematopoietic progenitor cells Ø Regulate trafficking of progenitor and mature cells Ø Can be stimulatory or inhibitory Ø Interleukins (ILs) are types of cytokines Ø Growth factors - type of cytokine Ø Promote the growth and survival of progenitor cells Ø Examples: Ø Colony stimulating factors (CSFs) Ø Erythropoietin (EPO) Ø Thrombopoietin (TPO) 66
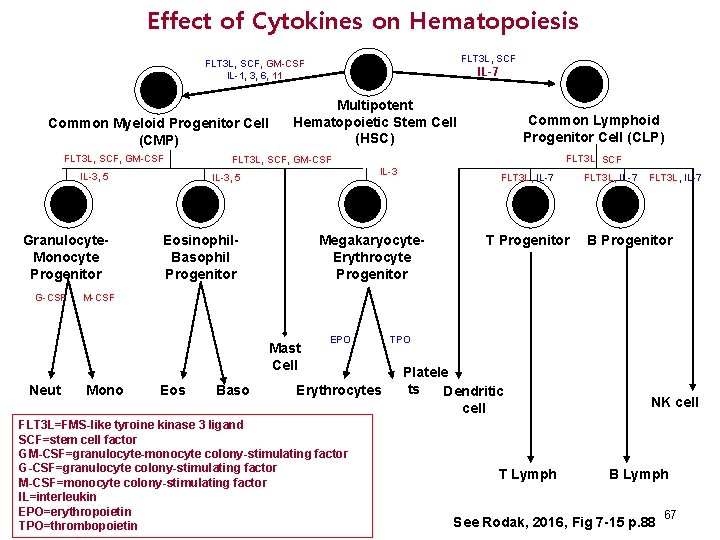
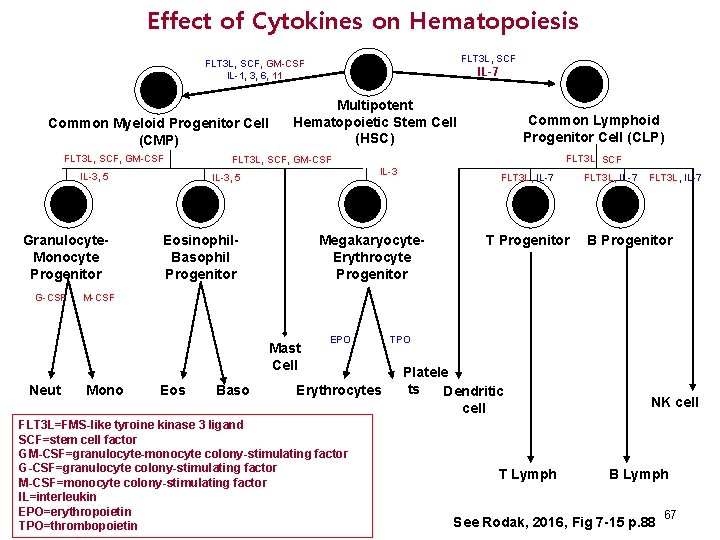
Effect of Cytokines on Hematopoiesis FLT 3 L, SCF, GM-CSF IL-1, 3, 6, 11 Common Myeloid Progenitor Cell (CMP) FLT 3 L, SCF, GM-CSF Multipotent Hematopoietic Stem Cell (HSC) IL-3, 5 Granulocyte. Monocyte Progenitor Eosinophil. Basophil Progenitor FLT 3 L SCF IL-3 FLT 3 L, IL-7 Megakaryocyte. Erythrocyte Progenitor T Progenitor FLT 3 L, IL-7 B Progenitor M-CSF Mast Cell Neut Common Lymphoid Progenitor Cell (CLP) FLT 3 L, SCF, GM-CSF IL-3, 5 G-CSF IL-7 Mono Eos Baso EPO Erythrocytes FLT 3 L=FMS-like tyroine kinase 3 ligand SCF=stem cell factor GM-CSF=granulocyte-monocyte colony-stimulating factor G-CSF=granulocyte colony-stimulating factor M-CSF=monocyte colony-stimulating factor IL=interleukin EPO=erythropoietin TPO=thrombopoietin TPO Platele ts Dendritic cell T Lymph NK cell B Lymph See Rodak, 2016, Fig 7 -15 p. 88 67