Leading Topics Related to the FMV of Healthcare


- Slides: 25

Leading Topics Related to the FMV of Healthcare Arrangements Presenter: Daryl P. Johnson, Health. Care Appraisers, Inc.
Topic No. 1 Investment value vs. fair market value – How do these standards of value differ, and how do the differences affect the valuation of healthcare transactions? 2
No. 1 - Investment Value vs. FMV n n The fair market value standard is a hypothetical willing buyer/willing seller scenario. No consideration is given to any unique attributes or synergies of either party in reaching a determination of value. The investment value standard takes into consideration the unique synergies or attributes that one or both parties may possess. n For example, if a hospital has more favorable reimbursement that will enhance the profitability of a diagnostic cath lab being considered for purchase by the hospital, any valuation consideration of this benefit would reflect investment value, and not FMV. 3
No. 1 - Investment Value vs. FMV (cont. ) n While FMV is the applicable valuation standard for most healthcare transactions, commercial reasonableness may dictate a departure from the strict FMV definition. For example, if a hospital has purchasing economies related to med/surg supplies, any arrangement involving the hospital’s acquisition of these items through an agreement with physicians should give consideration to the hospital’s actual cost (which invokes investment value). 4
Topic No. 2 The OIG precludes the use of potentially “tainted” market values (i. e. , those arrangements that involve physician ownership). What are some of the key implications of this OIG guidance in valuing healthcare transactions? 5
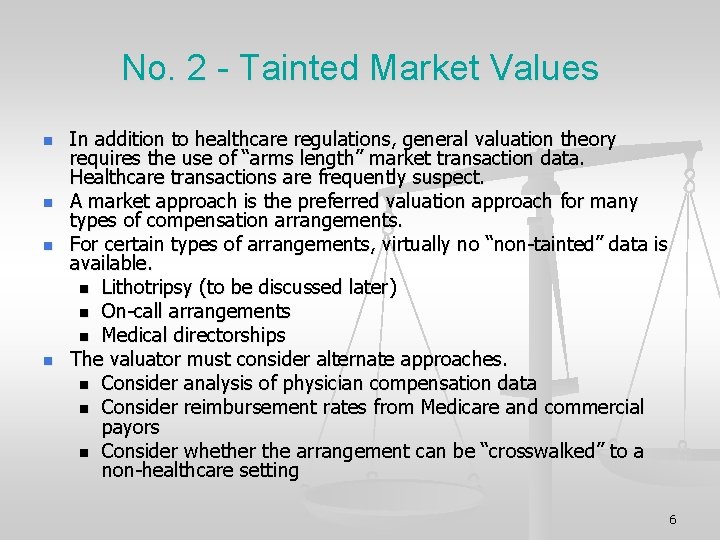
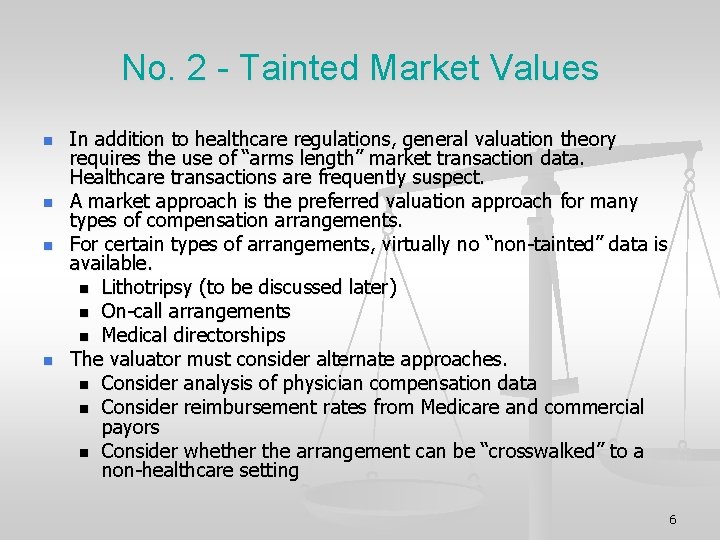
No. 2 - Tainted Market Values n n In addition to healthcare regulations, general valuation theory requires the use of “arms length” market transaction data. Healthcare transactions are frequently suspect. A market approach is the preferred valuation approach for many types of compensation arrangements. For certain types of arrangements, virtually no “non-tainted” data is available. n Lithotripsy (to be discussed later) n On-call arrangements n Medical directorships The valuator must consider alternate approaches. n Consider analysis of physician compensation data n Consider reimbursement rates from Medicare and commercial payors n Consider whether the arrangement can be “crosswalked” to a non-healthcare setting 6
Topic No. 3 What is the “top down” approach in the context of valuing under arrangements, and is such approach a valid valuation approach? 7
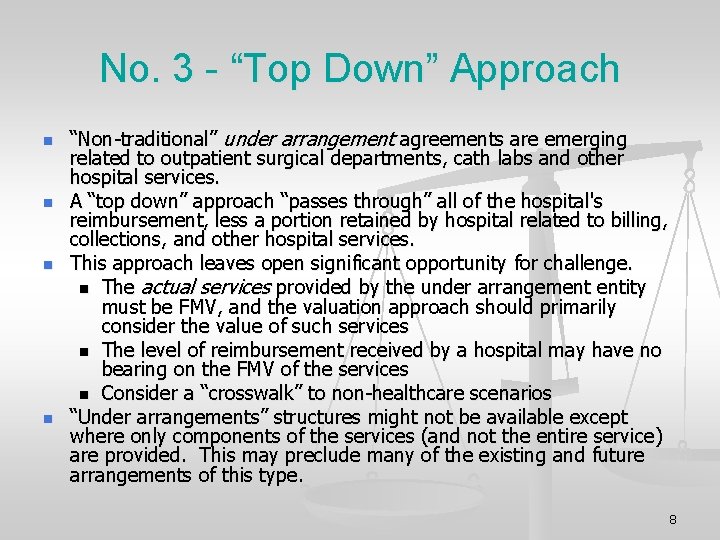
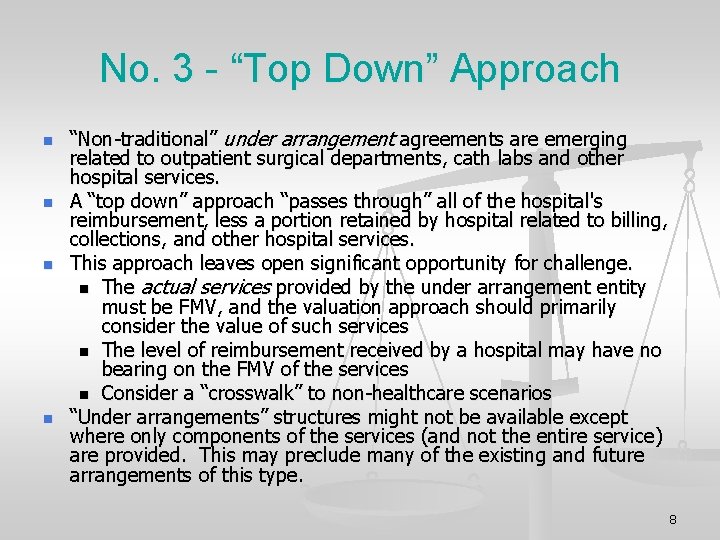
No. 3 - “Top Down” Approach n n “Non-traditional” under arrangement agreements are emerging related to outpatient surgical departments, cath labs and other hospital services. A “top down” approach “passes through” all of the hospital's reimbursement, less a portion retained by hospital related to billing, collections, and other hospital services. This approach leaves open significant opportunity for challenge. n The actual services provided by the under arrangement entity must be FMV, and the valuation approach should primarily consider the value of such services n The level of reimbursement received by a hospital may have no bearing on the FMV of the services n Consider a “crosswalk” to non-healthcare scenarios “Under arrangements” structures might not be available except where only components of the services (and not the entire service) are provided. This may preclude many of the existing and future arrangements of this type. 8
Topic No. 4 Is the concept of a physician’s “opportunity cost” a viable valuation methodology? 9
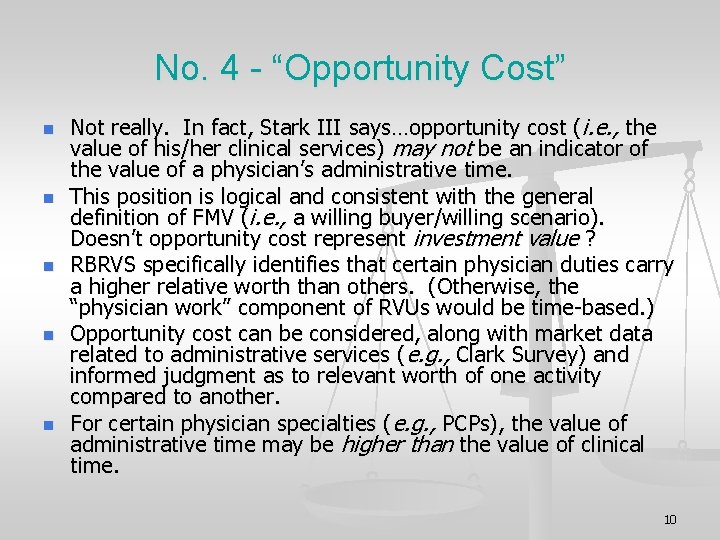
No. 4 - “Opportunity Cost” n n n Not really. In fact, Stark III says…opportunity cost (i. e. , the value of his/her clinical services) may not be an indicator of the value of a physician’s administrative time. This position is logical and consistent with the general definition of FMV (i. e. , a willing buyer/willing scenario). Doesn’t opportunity cost represent investment value ? RBRVS specifically identifies that certain physician duties carry a higher relative worth than others. (Otherwise, the “physician work” component of RVUs would be time-based. ) Opportunity cost can be considered, along with market data related to administrative services (e. g. , Clark Survey) and informed judgment as to relevant worth of one activity compared to another. For certain physician specialties (e. g. , PCPs), the value of administrative time may be higher than the value of clinical time. 10
Topic No. 5 Regarding compensated call coverage arrangements, what are current trends in payment methodologies, and how can these arrangements be valued? 11
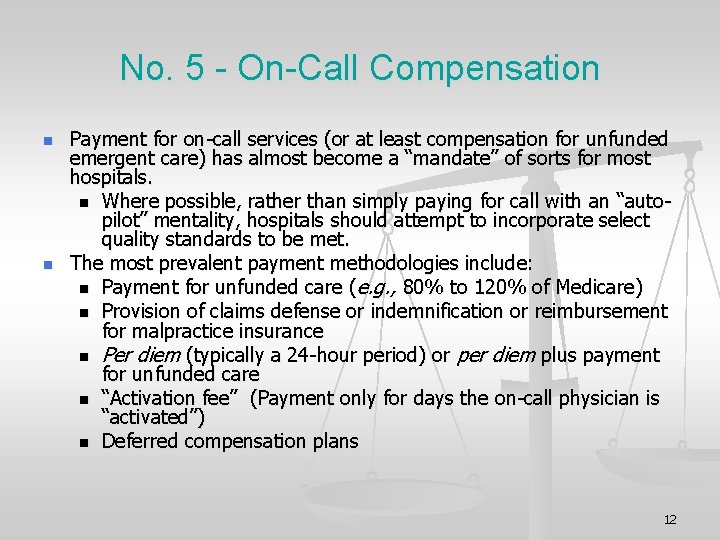
No. 5 - On-Call Compensation n n Payment for on-call services (or at least compensation for unfunded emergent care) has almost become a “mandate” of sorts for most hospitals. n Where possible, rather than simply paying for call with an “autopilot” mentality, hospitals should attempt to incorporate select quality standards to be met. The most prevalent payment methodologies include: n Payment for unfunded care (e. g. , 80% to 120% of Medicare) n Provision of claims defense or indemnification or reimbursement for malpractice insurance n Per diem (typically a 24 -hour period) or per diem plus payment for unfunded care n “Activation fee” (Payment only for days the on-call physician is “activated”) n Deferred compensation plans 12
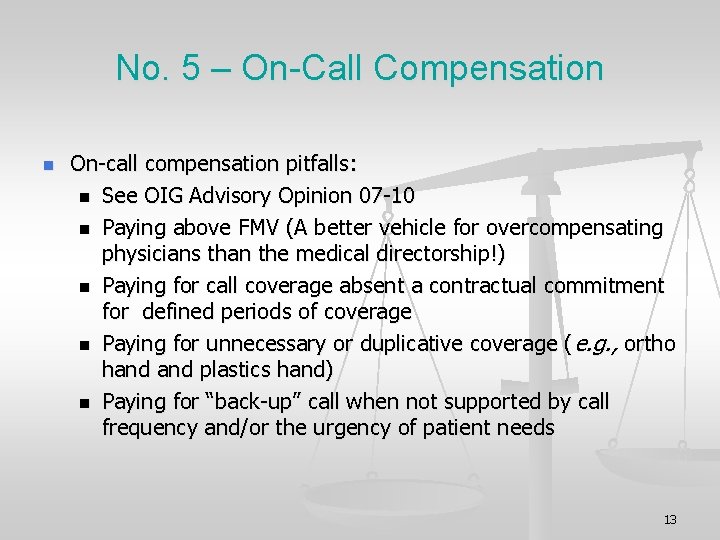
No. 5 – On-Call Compensation n On-call compensation pitfalls: n See OIG Advisory Opinion 07 -10 n Paying above FMV (A better vehicle for overcompensating physicians than the medical directorship!) n Paying for call coverage absent a contractual commitment for defined periods of coverage n Paying for unnecessary or duplicative coverage ( e. g. , ortho hand plastics hand) n Paying for “back-up” call when not supported by call frequency and/or the urgency of patient needs 13
Topic No. 6 What unique issues arise in connection with valuing lithotripsy and other “per click” arrangements, and what should cause concern? 14
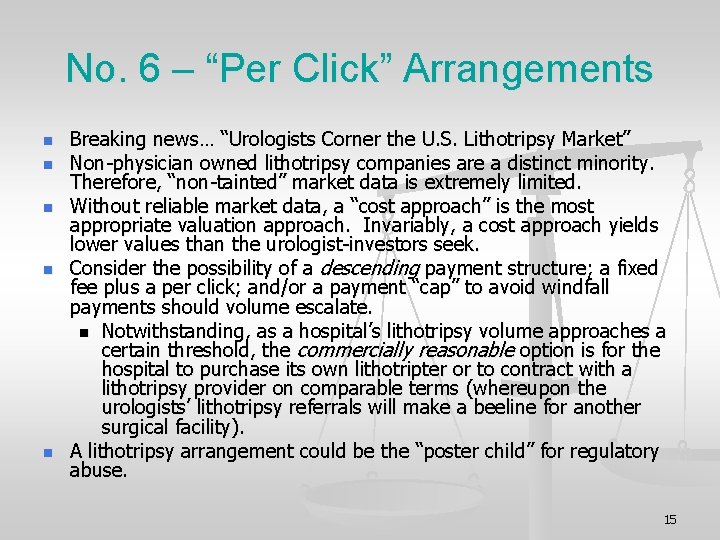
No. 6 – “Per Click” Arrangements n n n Breaking news… “Urologists Corner the U. S. Lithotripsy Market” Non-physician owned lithotripsy companies are a distinct minority. Therefore, “non-tainted” market data is extremely limited. Without reliable market data, a “cost approach” is the most appropriate valuation approach. Invariably, a cost approach yields lower values than the urologist-investors seek. Consider the possibility of a descending payment structure; a fixed fee plus a per click; and/or a payment “cap” to avoid windfall payments should volume escalate. n Notwithstanding, as a hospital’s lithotripsy volume approaches a certain threshold, the commercially reasonable option is for the hospital to purchase its own lithotripter or to contract with a lithotripsy provider on comparable terms (whereupon the urologists’ lithotripsy referrals will make a beeline for another surgical facility). A lithotripsy arrangement could be the “poster child” for regulatory abuse. 15
Topic No. 7 What impact does the elimination of the CMS safe harbor for personally performed physician services have on healthcare organizations? 16
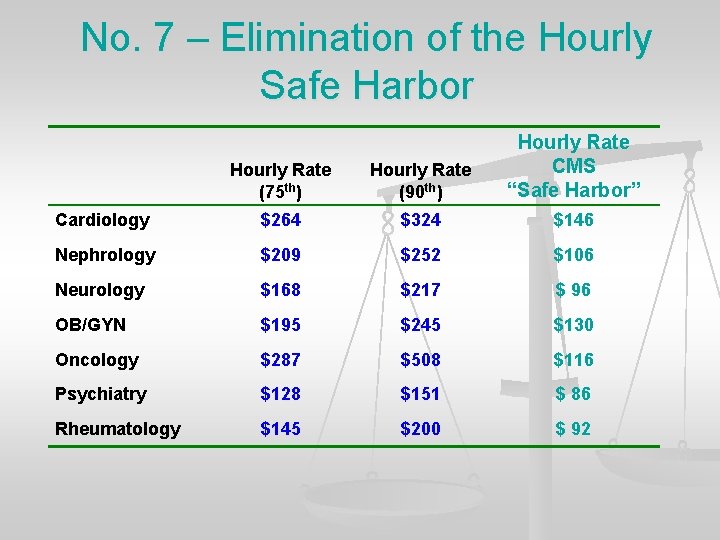
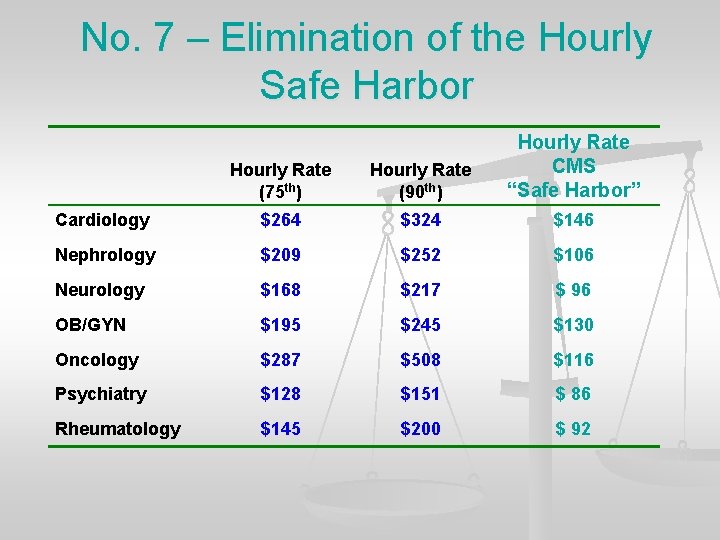
No. 7 – Elimination of the Hourly Safe Harbor Hourly Rate (75 th) Hourly Rate (90 th) Hourly Rate CMS “Safe Harbor” Cardiology $264 $324 $146 Nephrology $209 $252 $106 Neurology $168 $217 $ 96 OB/GYN $195 $245 $130 Oncology $287 $508 $116 Psychiatry $128 $151 $ 86 Rheumatology $145 $200 $ 92
Topic No. 8 “Co-management arrangements” typically involve physician/hospital ventures to manage hospital services lines, with compensation consisting of base and incentive components. What valuation approaches can be used to assess this new breed of management arrangements? 18
No. 8 – Co-Management Arrangements n n Compliance with FMV is critical for regulatory compliance, but also for the ultimate success of the project. Available valuation methodologies are limited and somewhat subjective. In considering the primary valuation approaches (cost, income and market), an income approach can likely be eliminated. Using a cost approach, FMV of the management fee can be established by assessing the required number of work hours needed to provide the management services multiplied by a fair market value hourly rate. n However, the exact number of required work hours cannot reasonably be determined in advance. n Further, a key ideal of most co-management arrangements is to reward results rather than time-based efforts. 19
No. 8 – Co-Management Arrangements n n A market approach recognizes that each co-management arrangement is unique, and reflects specific market and operational factors which are singular to the specific setting. n Break the specific services down into specific tasks and objectives, and then compare to other arrangements n On an item specific basis, assess the relative worth of each task/objective, and determine necessary adjustments to the comparable arrangements. The cost and market valuation methodologies described above must be reconciled to arrive at a final conclusion of value. The FMV of the total management fee must be established, as well as the base and incentive components. Rev Proc. 97 -13 may limit the amount of the incentive fee in relationship to the base fee. 20
Topic No. 9 Discussion of CMS developments related to the permissibility of “per click” compensation arrangements. 21
No. 9 – Status of “Per Clicks” Stark III does not specifically affect per click arrangements, but the proposal in the physician fee schedule rule would prohibit such arrangements with an individual physician or physician group. Joint ventures would still be viable vehicles. 22
…and last… Topic No. 10 In theory, local market data may be the most relevant market data in evaluating physician transactions. However, local data may be difficult to obtain. What implications does this have on the valuation process? 23
No. 10 – Local Market Values n n n Most healthcare providers are reluctant to share their physician compensation data. Even if a few local market values can be obtained, there will undoubtedly be insufficient information to allow reasonable comparisons to a subject arrangement (e. g. , how productive is the OB/GYN being paid $340, 000 in the local market? ). There is no assurance that local data points are free from overcompensation bias. In comparison to the thousands of respondents to at least 6 national salary surveys, local data is generally anecdotal. CMS specifically addresses situations when local data (e. g. , with respect to real estate) is insufficient. FMV of physician compensation may best be determined using national surveys as a starting point. Adjustments from the “norm” can then be made based upon differences in productivity, extent of call coverage and administrative duties, local economics, etc. 24

Questions? 25
 Fmv krigsstab
Fmv krigsstab Bobbin leading principle
Bobbin leading principle Healthcare and the healthcare team chapter 2
Healthcare and the healthcare team chapter 2 Sports medicine meaning
Sports medicine meaning What are the two types of physical components
What are the two types of physical components Fitness related images
Fitness related images Số nguyên tố là số gì
Số nguyên tố là số gì đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Fecboak
Fecboak Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Sơ đồ cơ thể người
Sơ đồ cơ thể người ưu thế lai là gì
ưu thế lai là gì Môn thể thao bắt đầu bằng chữ đua
Môn thể thao bắt đầu bằng chữ đua Tư thế ngồi viết
Tư thế ngồi viết Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Tư thế ngồi viết
Tư thế ngồi viết Thứ tự các dấu thăng giáng ở hóa biểu
Thứ tự các dấu thăng giáng ở hóa biểu Chó sói
Chó sói Thẻ vin
Thẻ vin Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Hổ sinh sản vào mùa nào
Hổ sinh sản vào mùa nào Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu