Integrated Medical and Dental Care for Population Management

- Slides: 43
Integrated Medical and Dental Care for Population Management of Periodontal Disease Oregon Oral Health Coalition Jeff Hummel, MD, MPH November 2, 2018
Goals • Population management of periodontal disease to improve CVD outcomes • QI methodology for a disease that straddles the Medical-Dental divide • Dentists and Medical Clinicians must be full partners in care • Practice transformation as a strategy to improve quality and reduce cost
What is the problem we are trying to solve? A Prevention Gap • Caries and periodontal disease are preventable chronic infectious diseases • Unacceptably high burden of disease nationwide that mirrors other health disparities • Dental care is the most common unmet health need • The healthcare system, as currently configured, fails to reach the populations with the highest burden of disease that perpetuates health disparities and wasteful spending 3
The Burden of Oral Disease: Adults 40% of adults suffer from periodontal diseases Up to 60% of adults in disadvantaged communities Cumulative Result? By age 65, 25% of Americans have no natural teeth 4
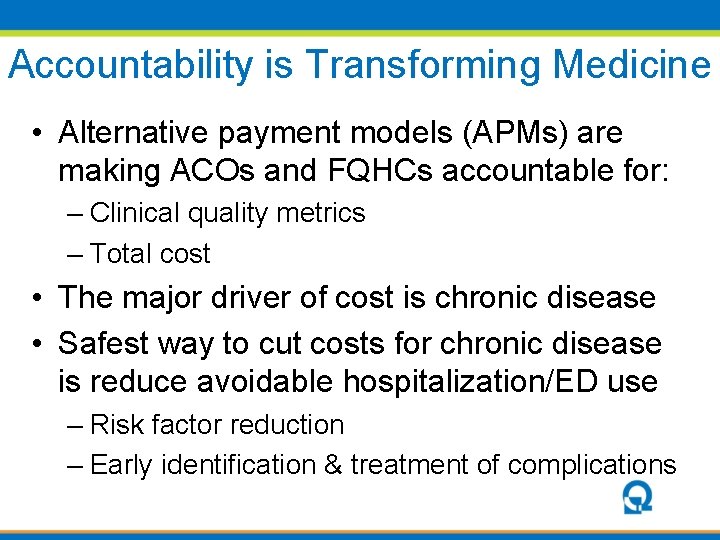
Accountability is Transforming Medicine • Alternative payment models (APMs) are making ACOs and FQHCs accountable for: – Clinical quality metrics – Total cost • The major driver of cost is chronic disease • Safest way to cut costs for chronic disease is reduce avoidable hospitalization/ED use – Risk factor reduction – Early identification & treatment of complications
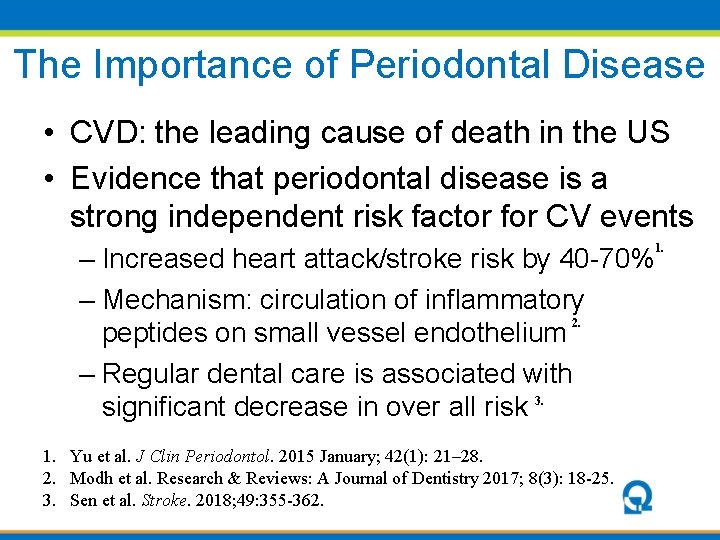
The Importance of Periodontal Disease • CVD: the leading cause of death in the US • Evidence that periodontal disease is a strong independent risk factor for CV events 1. – Increased heart attack/stroke risk by 40 -70% – Mechanism: circulation of inflammatory 2. peptides on small vessel endothelium – Regular dental care is associated with significant decrease in over all risk 3. 1. Yu et al. J Clin Periodontol. 2015 January; 42(1): 21– 28. 2. Modh et al. Research & Reviews: A Journal of Dentistry 2017; 8(3): 18 -25. 3. Sen et al. Stroke. 2018; 49: 355 -362.
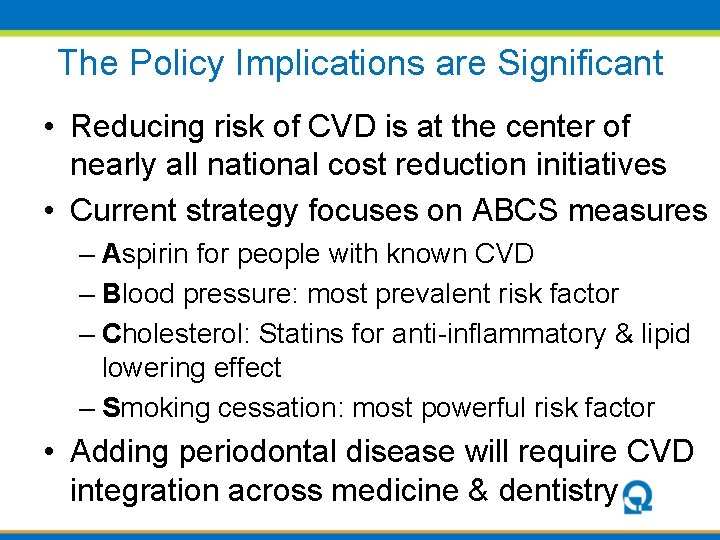
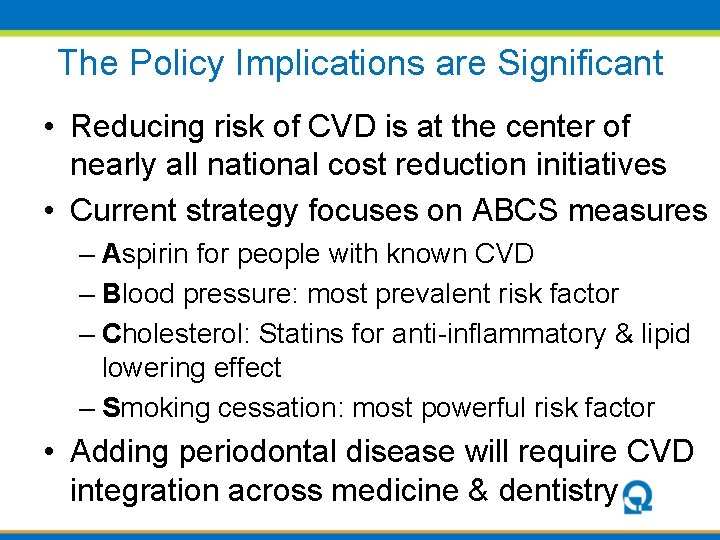
The Policy Implications are Significant • Reducing risk of CVD is at the center of nearly all national cost reduction initiatives • Current strategy focuses on ABCS measures – Aspirin for people with known CVD – Blood pressure: most prevalent risk factor – Cholesterol: Statins for anti-inflammatory & lipid lowering effect – Smoking cessation: most powerful risk factor • Adding periodontal disease will require CVD integration across medicine & dentistry

A Quality Improvement Perspective What are we trying to accomplish? • Reduce the burden of periodontal disease How will we know a change is an improvement? • Measure evidence-based process measures • Use Dental diagnostic codes to track population disease severity What can we change to cause an improvement? • Integrate oral health into medical care • Implement upstream preventive interventions on a population level
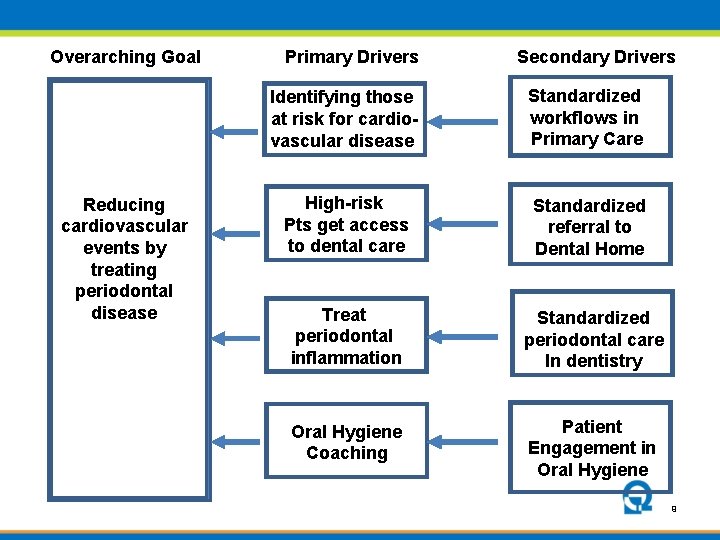
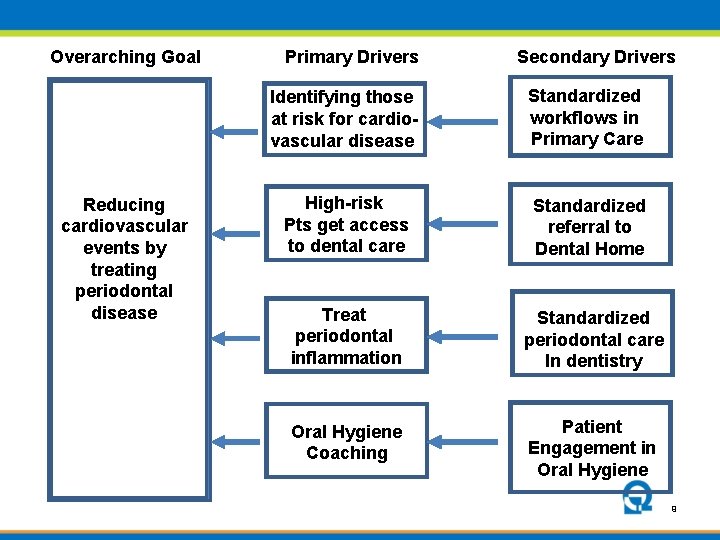
Overarching Goal Reducing cardiovascular events by treating periodontal disease Primary Drivers Secondary Drivers Identifying those at risk for cardiovascular disease Standardized workflows in Primary Care High-risk Pts get access to dental care Standardized referral to Dental Home Treat periodontal inflammation Standardized periodontal care In dentistry Oral Hygiene Coaching Patient Engagement in Oral Hygiene 9
What are we trying to accomplish? 10
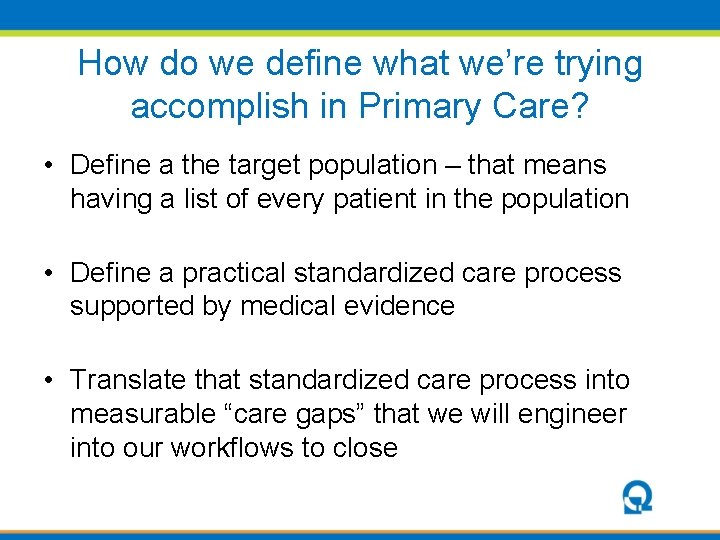
How do we define what we’re trying accomplish in Primary Care? • Define a the target population – that means having a list of every patient in the population • Define a practical standardized care process supported by medical evidence • Translate that standardized care process into measurable “care gaps” that we will engineer into our workflows to close
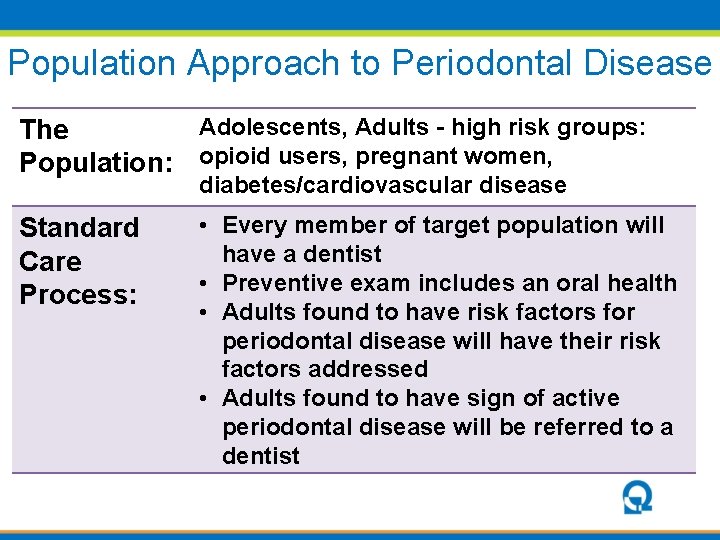
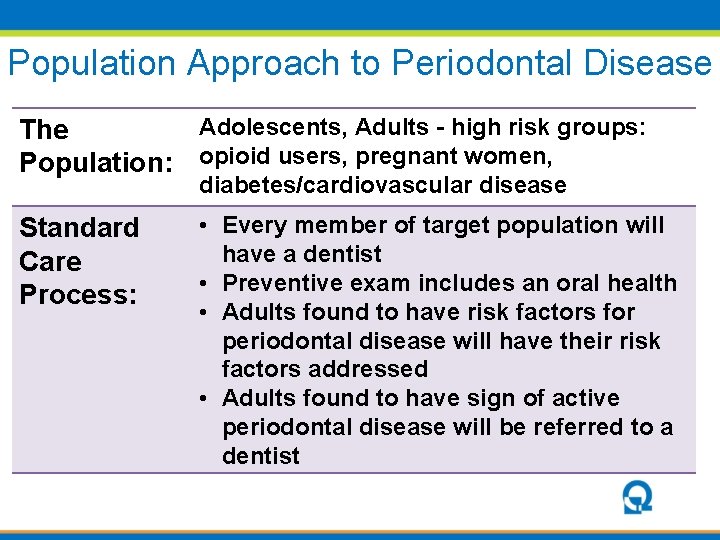
Population Approach to Periodontal Disease Adolescents, Adults - high risk groups: The Population: opioid users, pregnant women, diabetes/cardiovascular disease Standard Care Process: • Every member of target population will have a dentist • Preventive exam includes an oral health • Adults found to have risk factors for periodontal disease will have their risk factors addressed • Adults found to have sign of active periodontal disease will be referred to a dentist
How will we know a change is an improvement? 13
Why is it so important to measure improvement? • Usually we jump to solutions • All of the solutions we will think of will entail change, which threatens the status quo • It is very easy to think of reasons to resist threats to the status quo, particularly if the goal isn’t clear • Without a clear goal and ways to measure improvement, efforts to implement solutions bog down in resistance
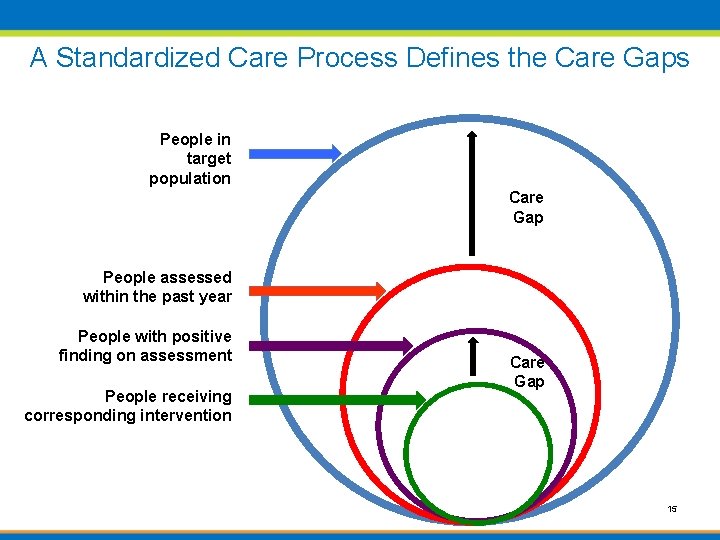
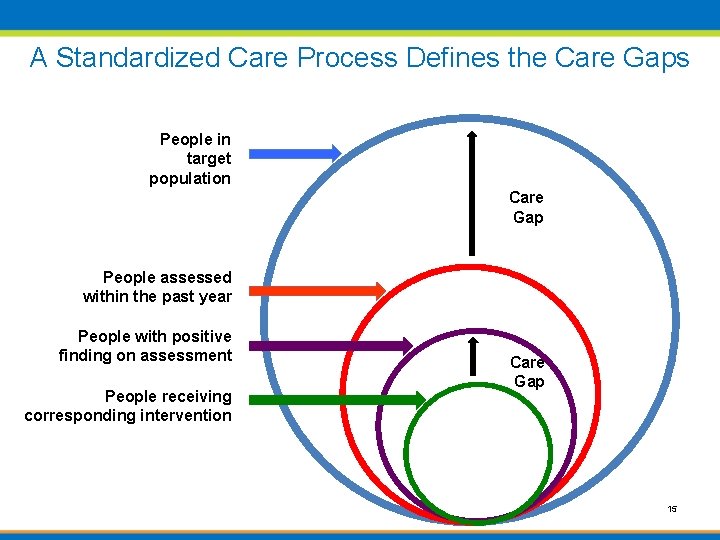
A Standardized Care Process Defines the Care Gaps People in target population Care Gap People assessed within the past year People with positive finding on assessment People receiving corresponding intervention Care Gap 15
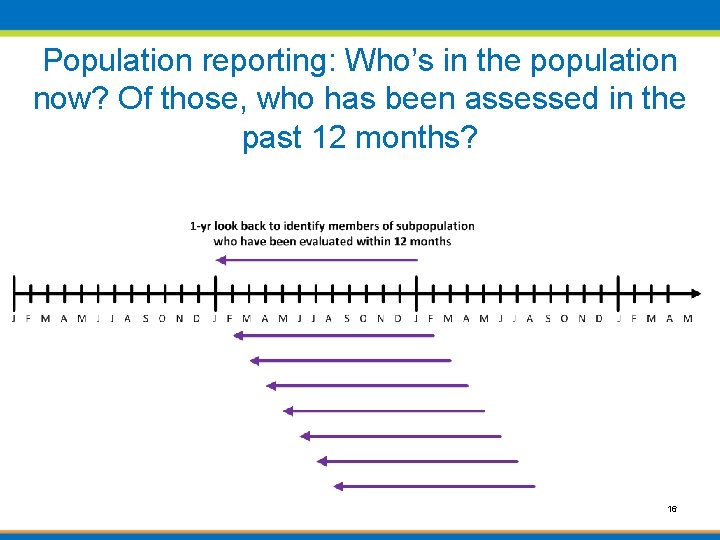
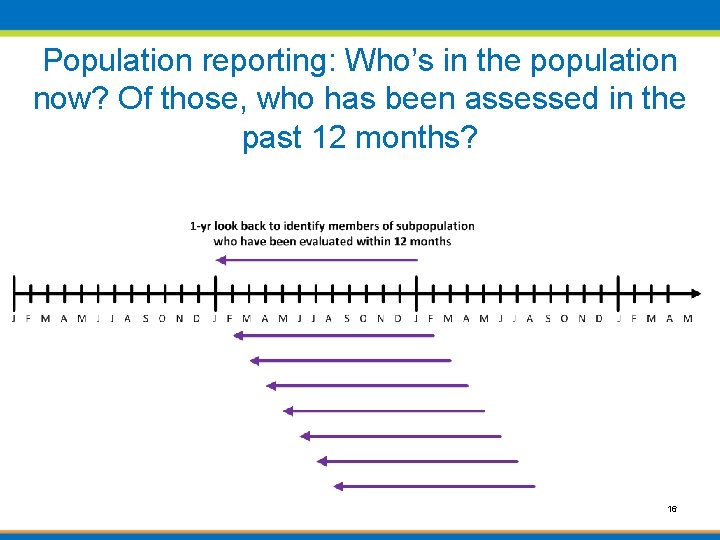
Population reporting: Who’s in the population now? Of those, who has been assessed in the past 12 months? 16
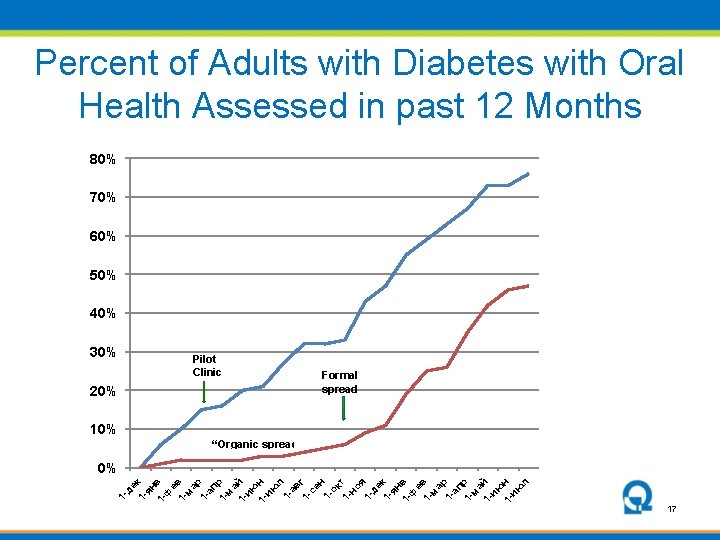
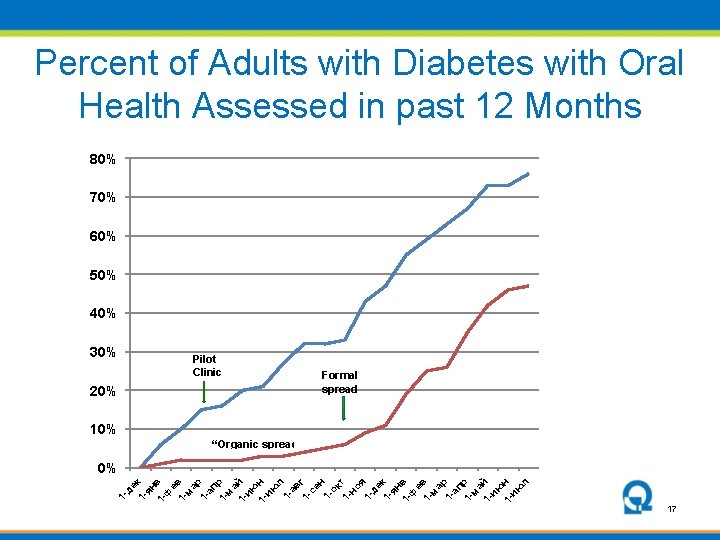
Percent of Adults with Diabetes with Oral Health Assessed in past 12 Months 80% 70% 60% 50% 40% 30% Pilot Clinic 20% Formal spread 10% “Organic spread” 1 - де 1 - к ян 1 - в ф е 1 - в м а 1 - р ап 1 - р м а 1 - й ию 1 - н ию л 1 ав 1 - г се н 1 ок 1 - т но я 1 де 1 - к ян 1 - в ф е 1 - в м а 1 - р ап 1 - р м а 1 - й ию 1 - н ию л 0% 17
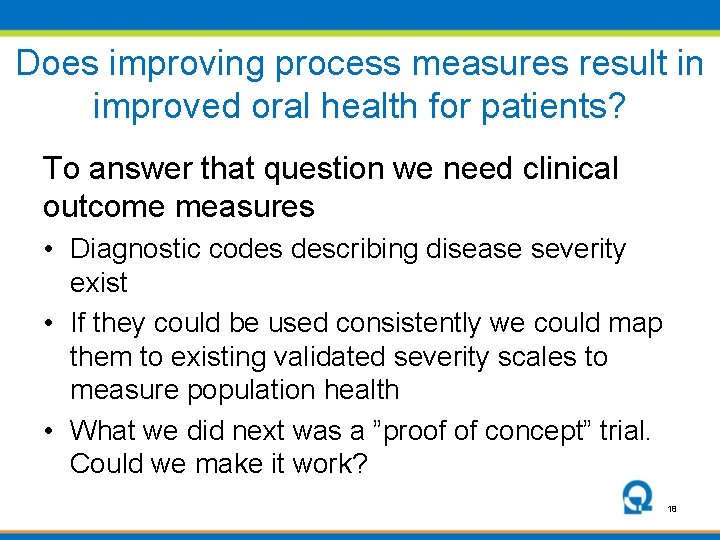
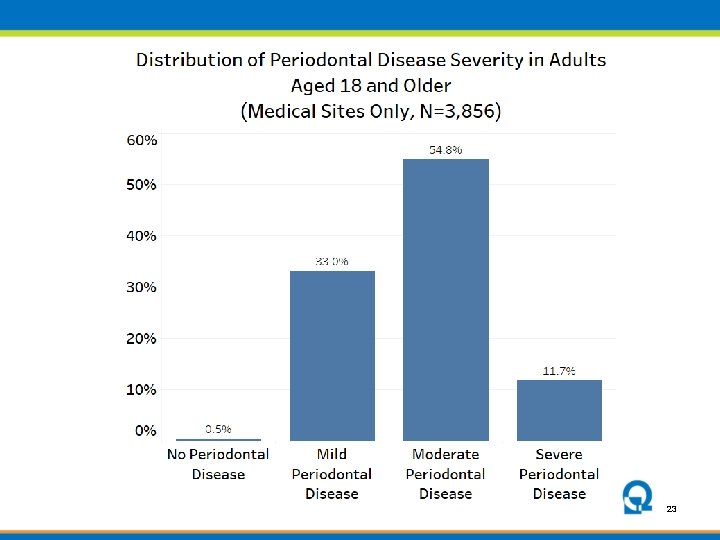
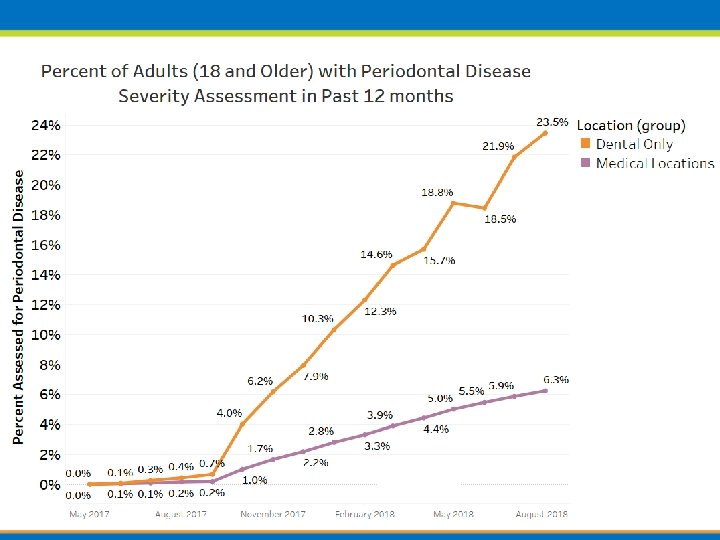
Does improving process measures result in improved oral health for patients? To answer that question we need clinical outcome measures • Diagnostic codes describing disease severity exist • If they could be used consistently we could map them to existing validated severity scales to measure population health • What we did next was a ”proof of concept” trial. Could we make it work? 18
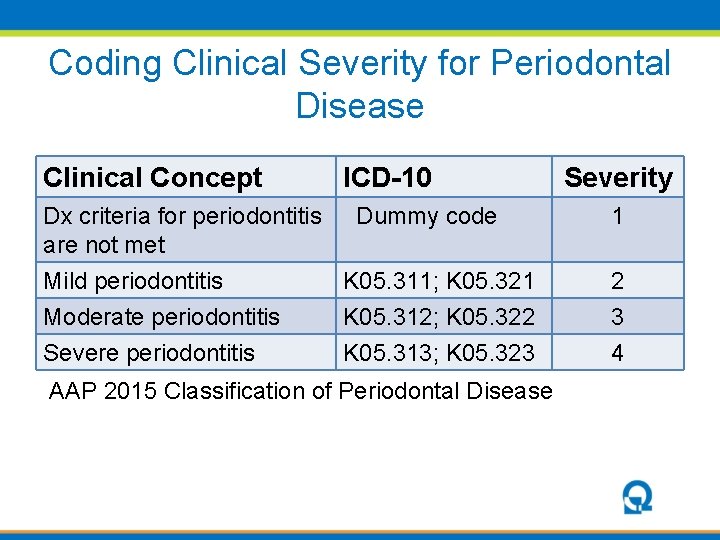
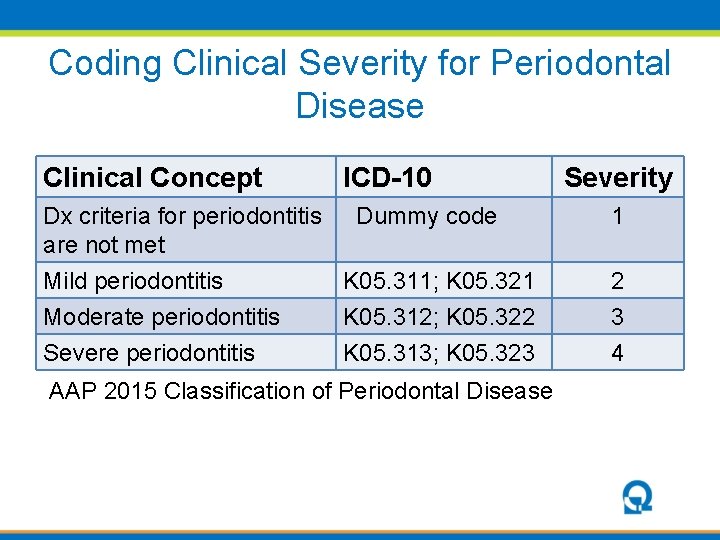
Coding Clinical Severity for Periodontal Disease Clinical Concept ICD-10 Severity Dx criteria for periodontitis Dummy code are not met Mild periodontitis K 05. 311; K 05. 321 1 Moderate periodontitis Severe periodontitis 3 4 K 05. 312; K 05. 322 K 05. 313; K 05. 323 AAP 2015 Classification of Periodontal Disease 2
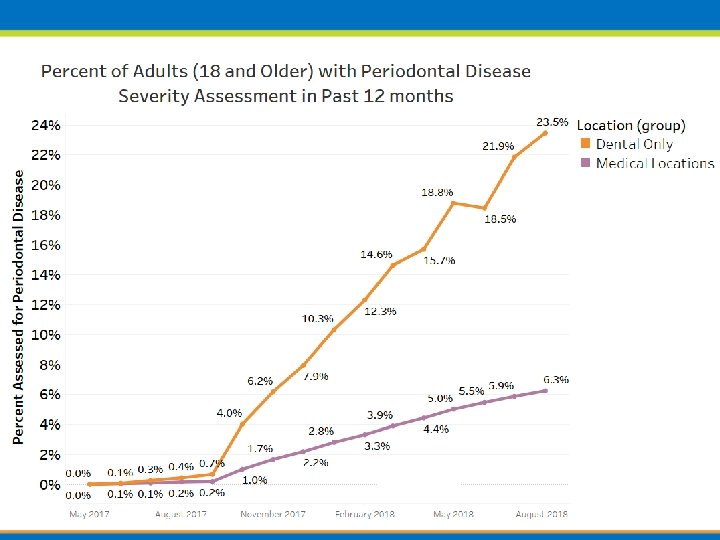
Proof of Concept: Can we make this work? Health. Point FQHC • 10 Primary Care sites & 7 with colocated Dental • 86, 000 medical Pts • 12, 000 (16%) receive dental care Goal: Use ICD-10 Coding in dentistry to measure the oral disease of the population 20
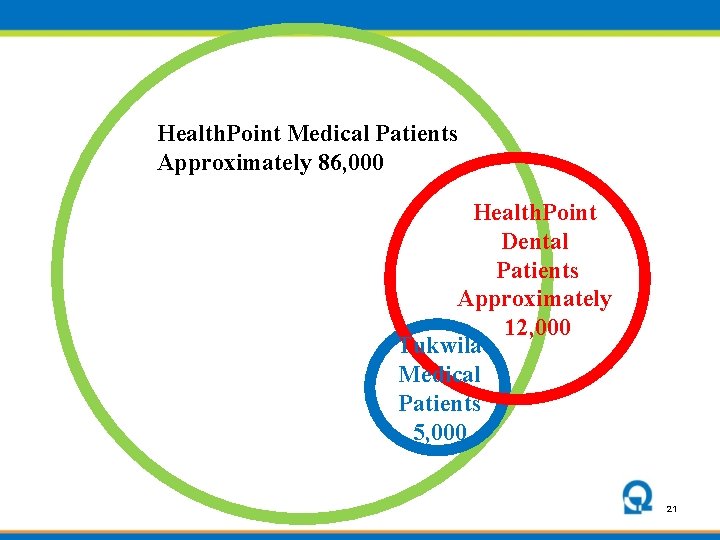
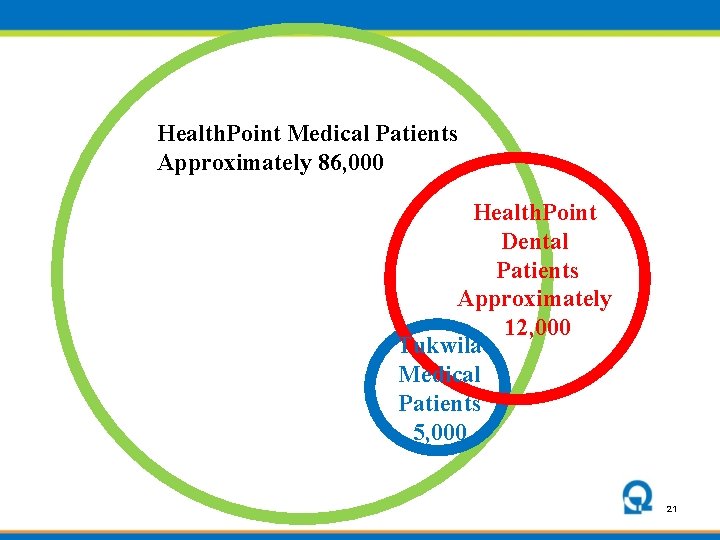
Health. Point Medical Patients Approximately 86, 000 Health. Point Dental Patients Approximately 12, 000 Tukwila Medical Patients 5, 000 21
22
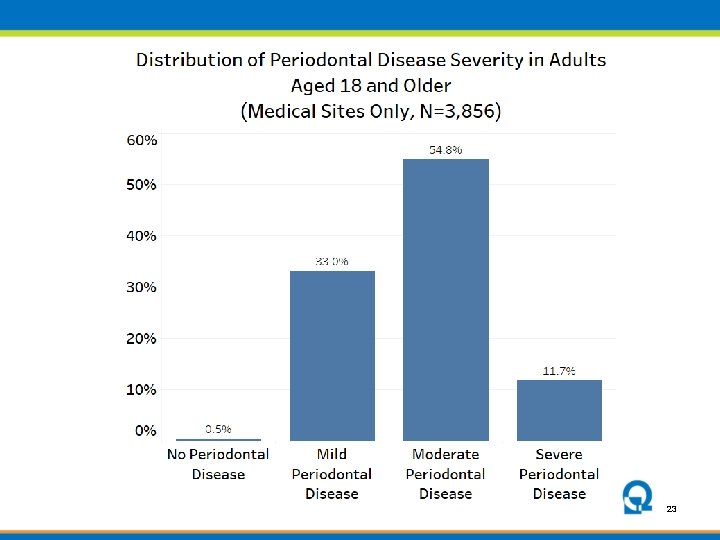
23
What changes could be make that would result in an improvement? 24
What would it take to change the medical standard of care? 1. Clear definition of what can be done in the primary care setting to protect and promote oral health 2. Streamlined process for fitting oral health into an already packed primary care workflow 3. Practical model for a close collaboration between medicine and dentistry
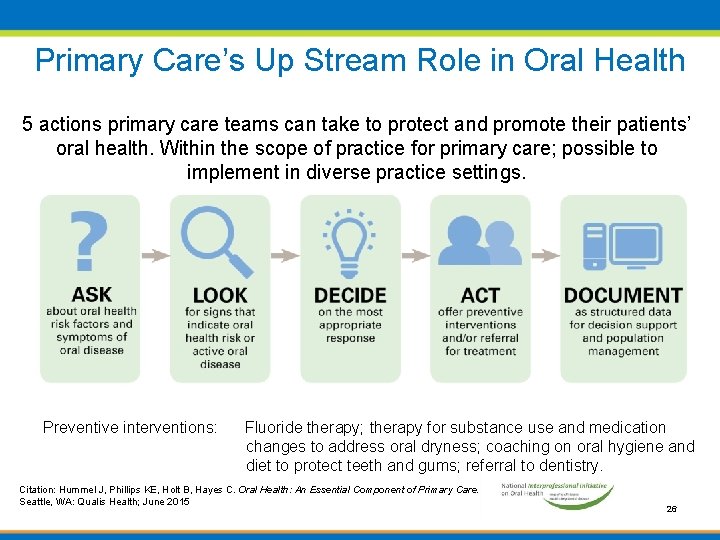
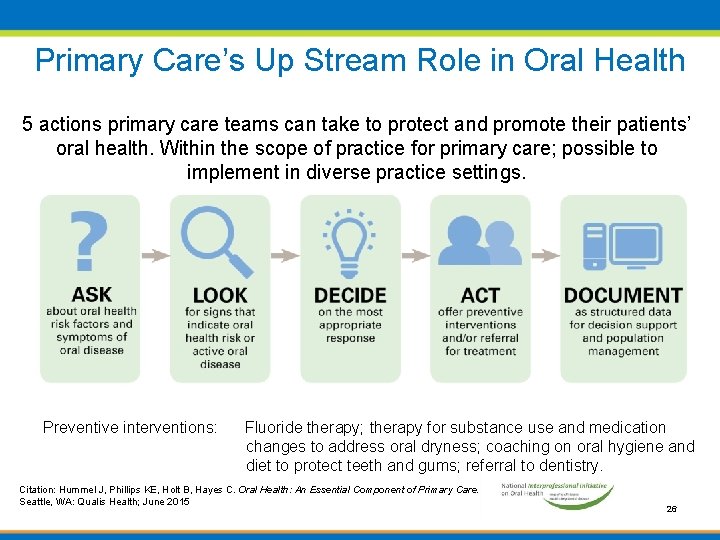
Primary Care’s Up Stream Role in Oral Health 5 actions primary care teams can take to protect and promote their patients’ oral health. Within the scope of practice for primary care; possible to implement in diverse practice settings. Preventive interventions: Fluoride therapy; therapy for substance use and medication changes to address oral dryness; coaching on oral hygiene and diet to protect teeth and gums; referral to dentistry. Citation: Hummel J, Phillips KE, Holt B, Hayes C. Oral Health: An Essential Component of Primary Care. Seattle, WA: Qualis Health; June 2015 26
An Example from the Front Lines • George is 45 years old and is having his planned diabetes visit. • George tells the doctor about a bleeding in his gums. • After ordering the Hb. A 1 c, dilated retinal exam, Alb/Cr ratio, etc George is told to make an appointment upstairs with dentistry. • There is a line at the desk and he has to get back to work so he leaves. He remembers the next week and calls to make the appointment • 2 months later George has a complete dental exam. The dentist finds George has moderate periodontal disease, with severe disease in one quadrant in which a tooth shows some mobility. • He returns the following month to have a single quadrant scaling. • What’s wrong with that? Isn’t that how it works?
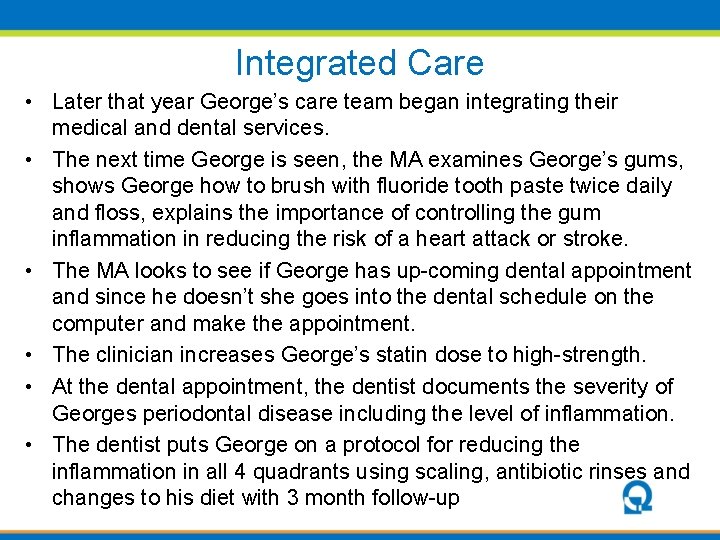
Integrated Care • Later that year George’s care team began integrating their medical and dental services. • The next time George is seen, the MA examines George’s gums, shows George how to brush with fluoride tooth paste twice daily and floss, explains the importance of controlling the gum inflammation in reducing the risk of a heart attack or stroke. • The MA looks to see if George has up-coming dental appointment and since he doesn’t she goes into the dental schedule on the computer and make the appointment. • The clinician increases George’s statin dose to high-strength. • At the dental appointment, the dentist documents the severity of Georges periodontal disease including the level of inflammation. • The dentist puts George on a protocol for reducing the inflammation in all 4 quadrants using scaling, antibiotic rinses and changes to his diet with 3 month follow-up
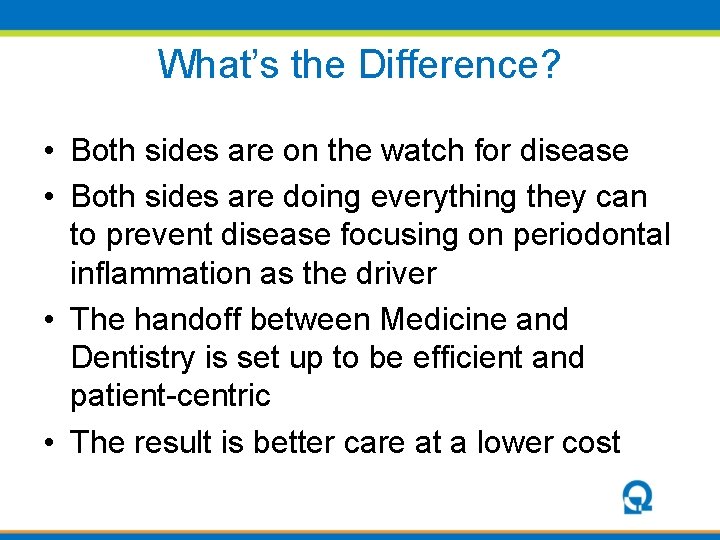
What’s the Difference? • Both sides are on the watch for disease • Both sides are doing everything they can to prevent disease focusing on periodontal inflammation as the driver • The handoff between Medicine and Dentistry is set up to be efficient and patient-centric • The result is better care at a lower cost
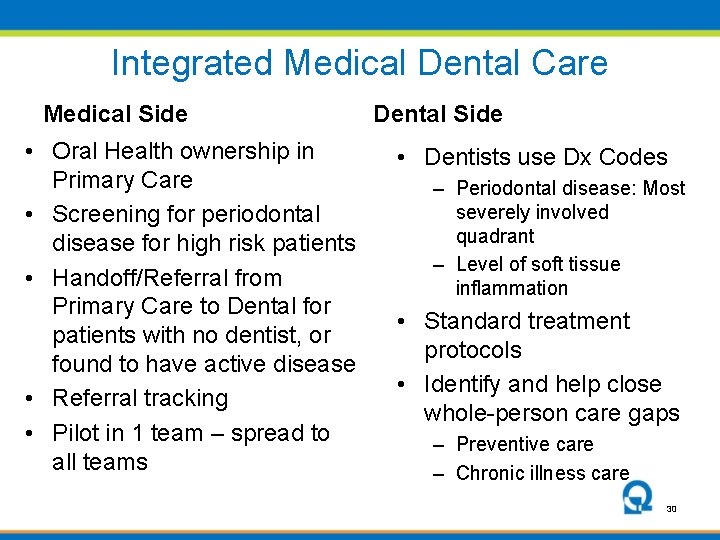
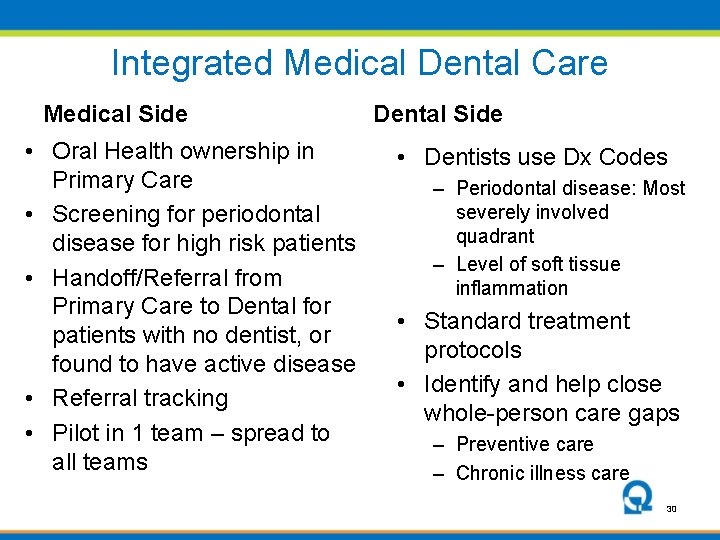
Integrated Medical Dental Care Medical Side • Oral Health ownership in Primary Care • Screening for periodontal disease for high risk patients • Handoff/Referral from Primary Care to Dental for patients with no dentist, or found to have active disease • Referral tracking • Pilot in 1 team – spread to all teams Dental Side • Dentists use Dx Codes – Periodontal disease: Most severely involved quadrant – Level of soft tissue inflammation • Standard treatment protocols • Identify and help close whole-person care gaps – Preventive care – Chronic illness care 30
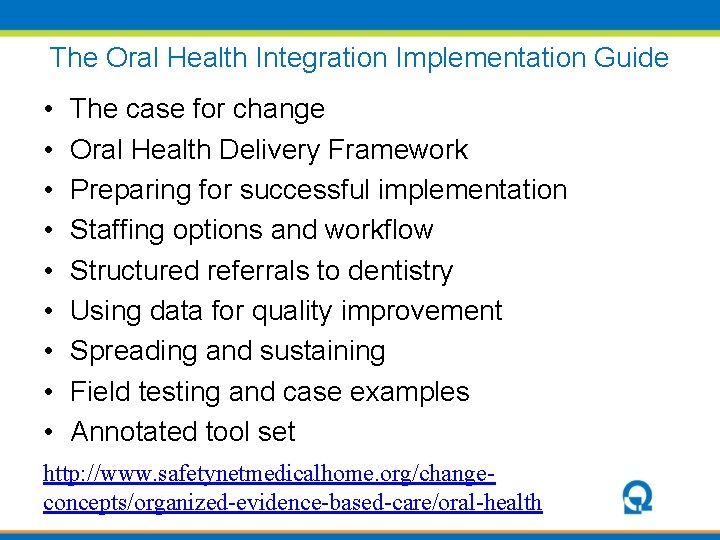
The Oral Health Integration Implementation Guide • • • The case for change Oral Health Delivery Framework Preparing for successful implementation Staffing options and workflow Structured referrals to dentistry Using data for quality improvement Spreading and sustaining Field testing and case examples Annotated tool set http: //www. safetynetmedicalhome. org/changeconcepts/organized-evidence-based-care/oral-health
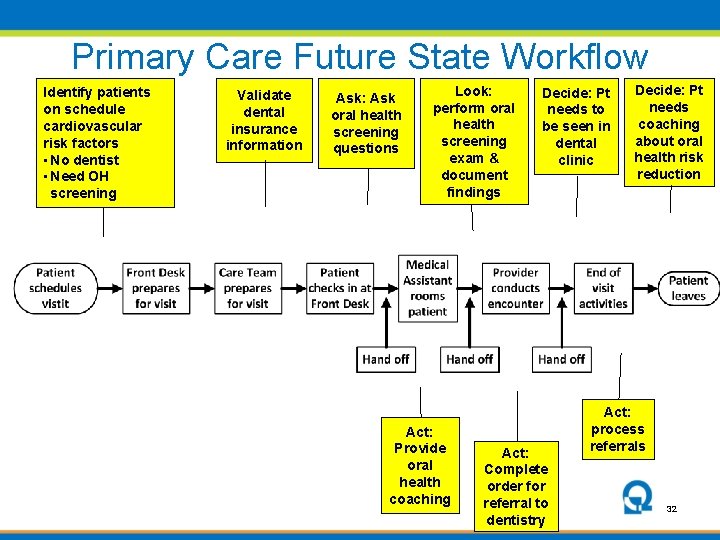
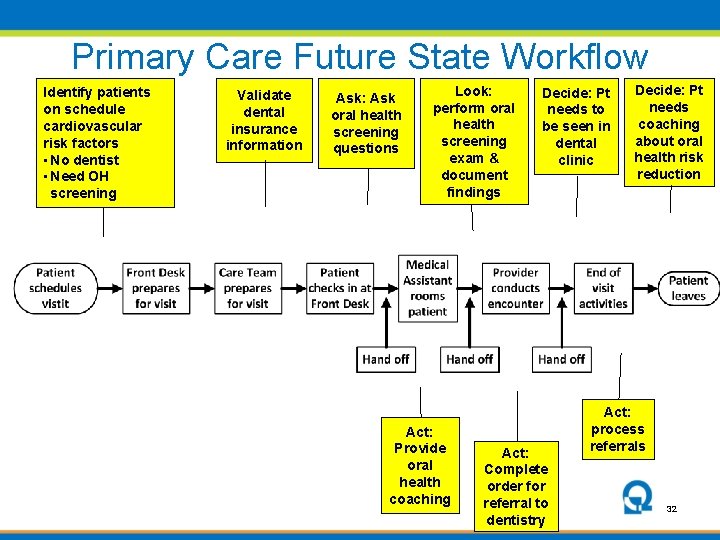
Primary Care Future State Workflow Identify patients on schedule cardiovascular risk factors • No dentist • Need OH screening Validate dental insurance information Ask: Ask oral health screening questions Look: perform oral health screening exam & document findings Act: Provide oral health coaching Decide: Pt needs to be seen in dental clinic Act: Complete order for referral to dentistry Decide: Pt needs coaching about oral health risk reduction Act: process referrals 32
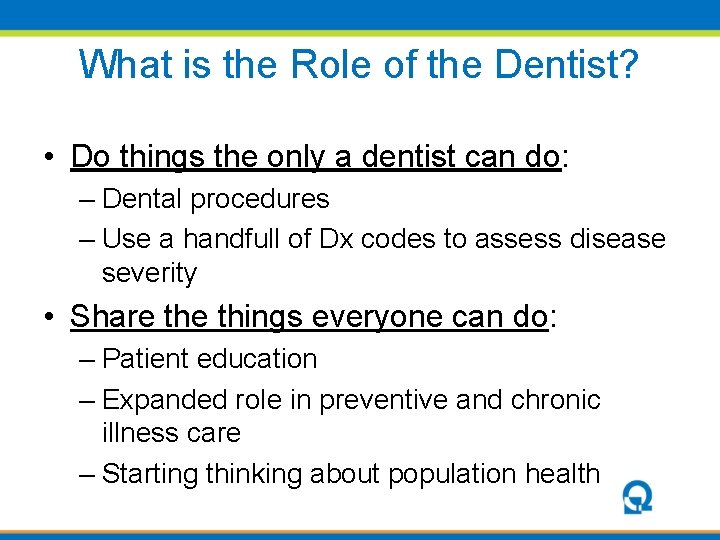
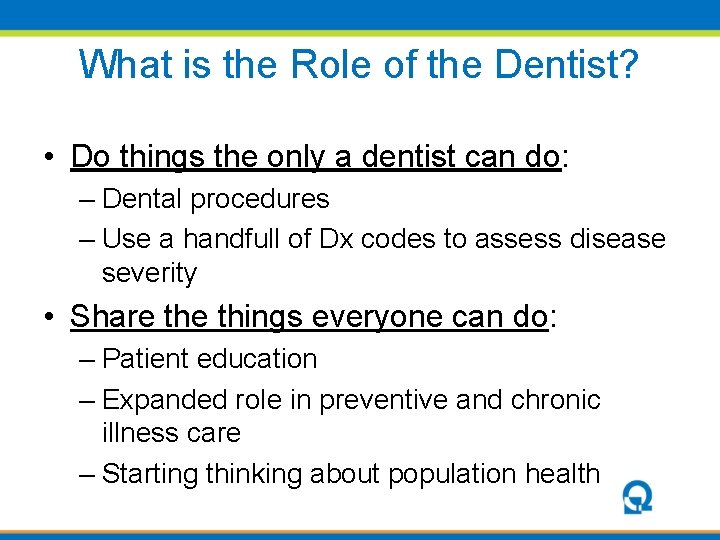
What is the Role of the Dentist? • Do things the only a dentist can do: – Dental procedures – Use a handfull of Dx codes to assess disease severity • Share things everyone can do: – Patient education – Expanded role in preventive and chronic illness care – Starting thinking about population health
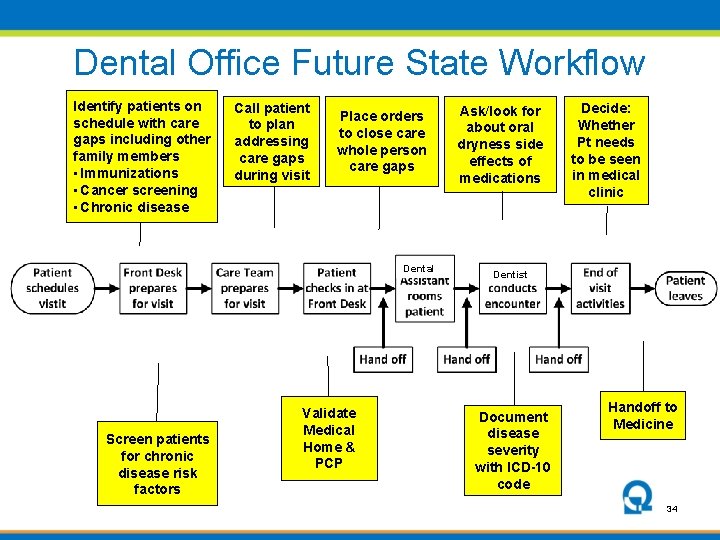
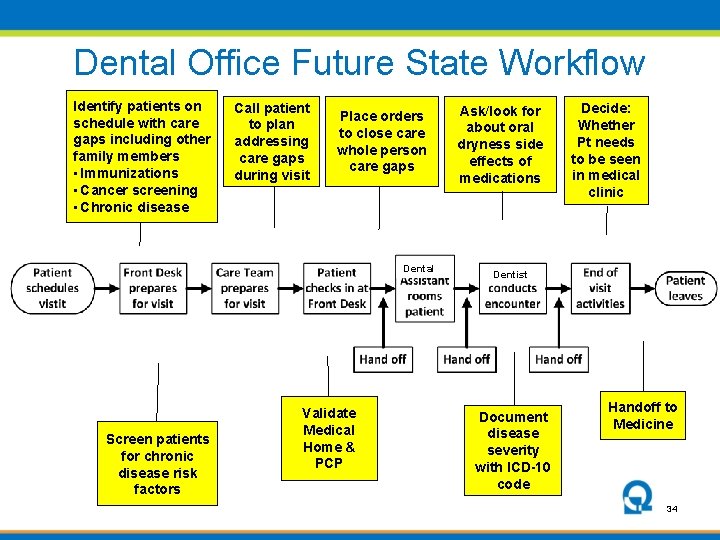
Dental Office Future State Workflow Identify patients on schedule with care gaps including other family members • Immunizations • Cancer screening • Chronic disease Call patient to plan addressing care gaps during visit Place orders to close care whole person care gaps Dental Screen patients for chronic disease risk factors Validate Medical Home & PCP Ask/look for about oral dryness side effects of medications Decide: Whether Pt needs to be seen in medical clinic Dentist Document disease severity with ICD-10 code Handoff to Medicine 34
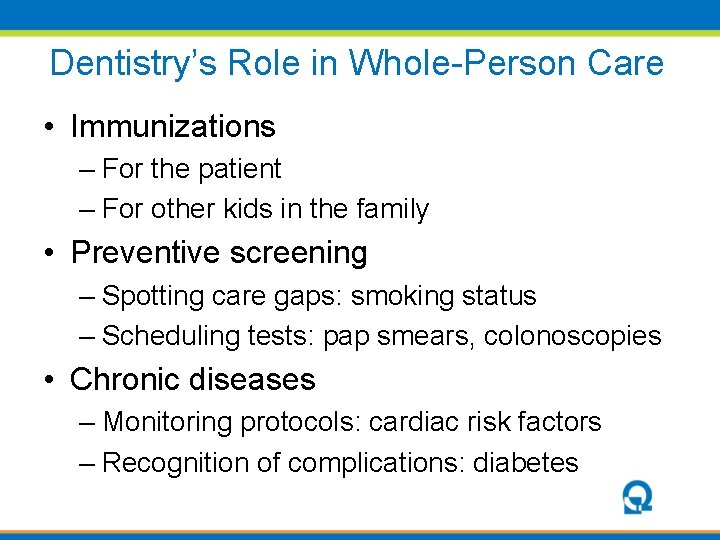
Dentistry’s Role in Whole-Person Care • Immunizations – For the patient – For other kids in the family • Preventive screening – Spotting care gaps: smoking status – Scheduling tests: pap smears, colonoscopies • Chronic diseases – Monitoring protocols: cardiac risk factors – Recognition of complications: diabetes
From Co-Location to Integration • Co-location has the potential for: – Population management of oral health care – Warm handoffs and cross scheduling – Opportunity for dental teams to participate in care beyond the mouth • Full integration: – Shared patient panel – Shared workspace – Seamless care
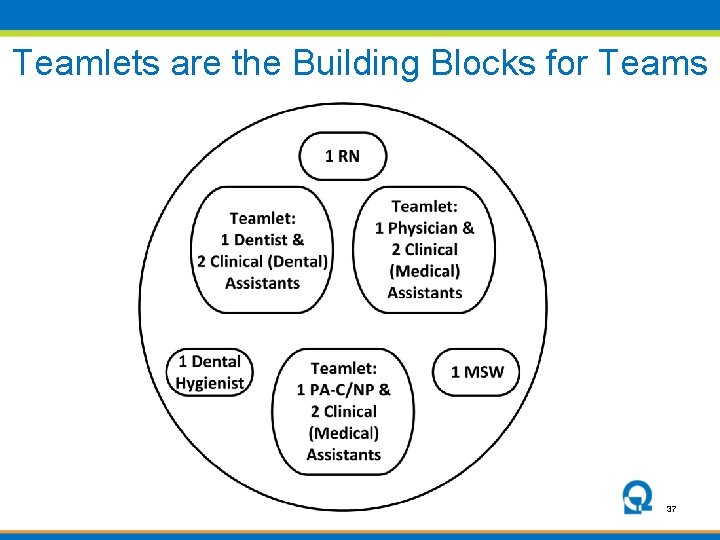
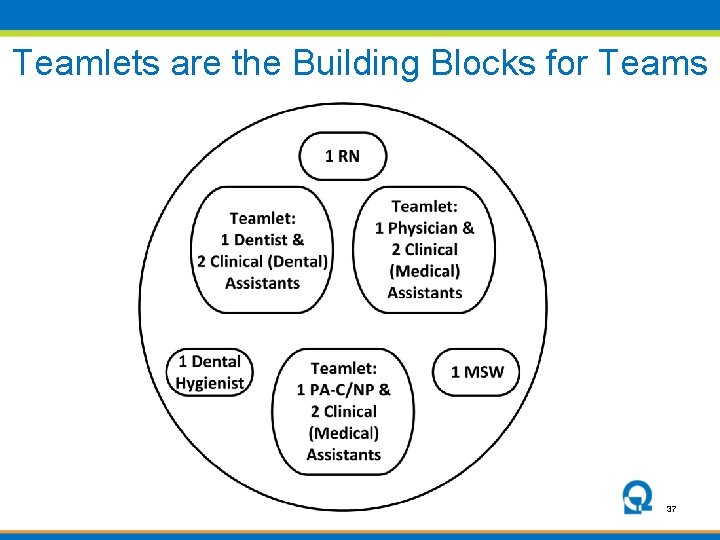
Teamlets are the Building Blocks for Teams 37
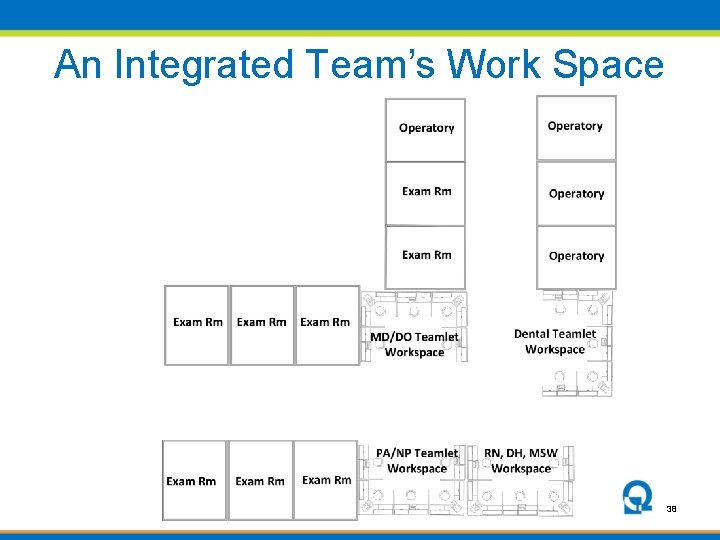
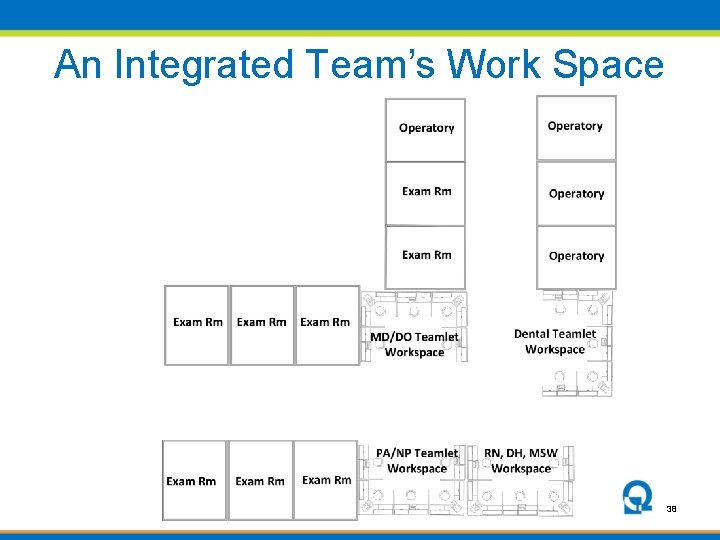
An Integrated Team’s Work Space 38
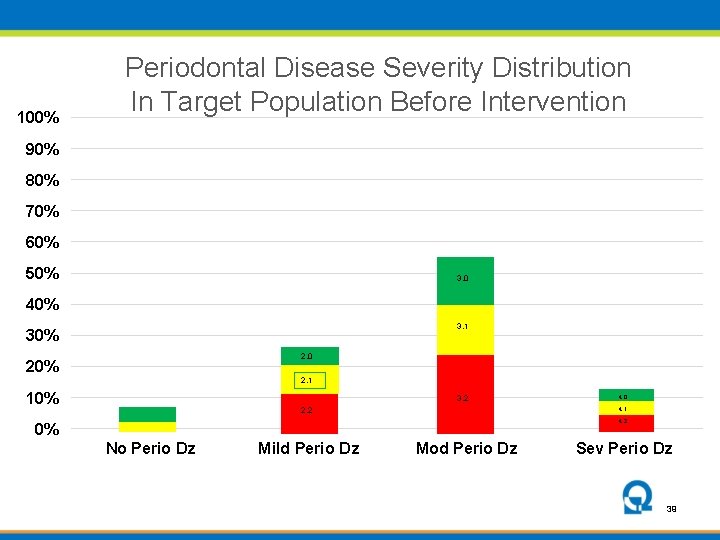
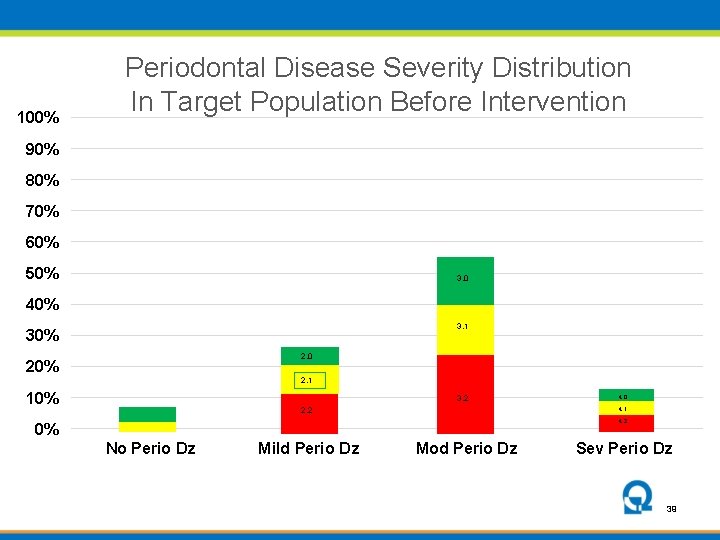
100% Periodontal Disease Severity Distribution In Target Population Before Intervention 90% 80% 70% 60% 50% 3. 0 40% 3. 1 30% 2. 0 20% 2. 1 10% 3. 2 4. 0 4. 1 2. 2 4. 2 0% No Perio Dz Mild Perio Dz Mod Perio Dz Sev Perio Dz 39
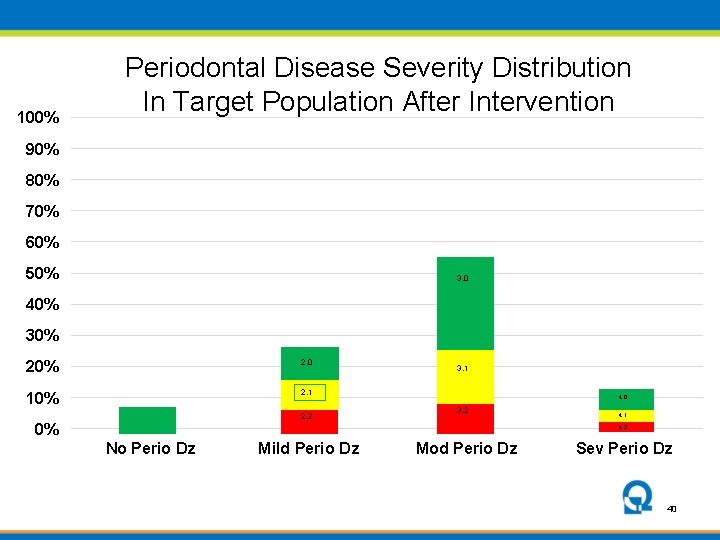
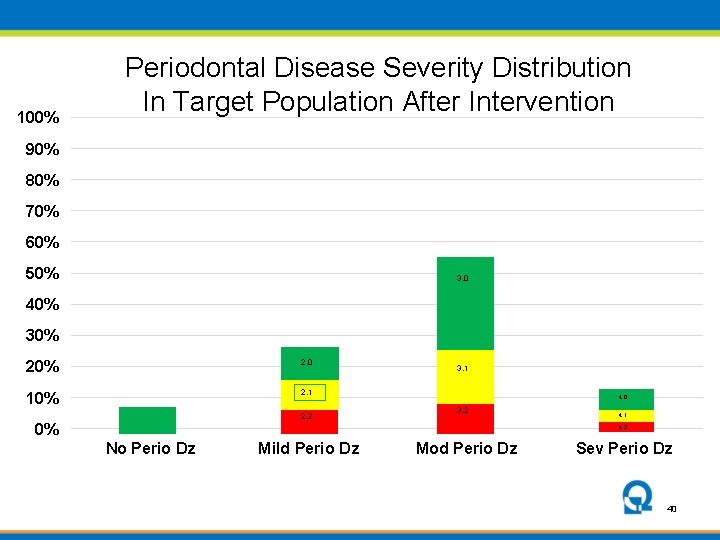
100% Periodontal Disease Severity Distribution In Target Population After Intervention 90% 80% 70% 60% 50% 3. 0 40% 30% 2. 0 10% 2. 1 2. 2 0% 3. 1 4. 0 3. 2 4. 1 4. 2 No Perio Dz Mild Perio Dz Mod Perio Dz Sev Perio Dz 40
Next Steps • Work with ADA to improve ICD-10 codes – Distinguish between caries requiring cutting the tooth and caries that don’t – Add a modifier to periodontal disease to document control of gingival inflammation • Expanding to FQHCs across Washington • Offering MOC IV credit for QI efforts focusing on oral health in primary care
Conclusion • We’re not going to fully address cardiovascular disease without medical dental integration • The tools and skills needed to do that exist • They will be easiest to use in sites with colocated medical-dental services (FQHCs) • Value-based reimbursement will drive this
Learn More Resources available at Qualis Health: White Paper www. Qualis. Health. org/whitepaper Implementation Guide and Toolkit: http: //www. safetynetmedicalhome. org/change -concepts/organized-evidence-basedcare/oral-health Jeff Hummel, MD, MPH e-mail: jeffh@qualishealth. org 43
 Levels of care primary secondary tertiary
Levels of care primary secondary tertiary Chapter test a chapter 4 population ecology answer key
Chapter test a chapter 4 population ecology answer key Section 1 population dynamics
Section 1 population dynamics Population ecology section 1 population dynamics
Population ecology section 1 population dynamics Chapter 4 population ecology section 1 population dynamics
Chapter 4 population ecology section 1 population dynamics Dental defence union
Dental defence union Cumbria and north east ics
Cumbria and north east ics Integrated electronic medical record
Integrated electronic medical record Mercy maricopa behavioral health
Mercy maricopa behavioral health Outcome measures traduzione
Outcome measures traduzione Cissbury integrated care
Cissbury integrated care Integrated care system definition
Integrated care system definition St charles integrated care centre
St charles integrated care centre Rainbow model of integrated care
Rainbow model of integrated care Imcc emory
Imcc emory Family integrated care
Family integrated care Integrated primary health care model
Integrated primary health care model Mhc fully integrated managed care
Mhc fully integrated managed care Hepburn osteometric board
Hepburn osteometric board Green mountain care dental
Green mountain care dental Chapter 33 delivering dental care
Chapter 33 delivering dental care Dr. dalia dental care
Dr. dalia dental care Dalia in the bible
Dalia in the bible Dr. dalia dental care
Dr. dalia dental care Albany area primary health care dental
Albany area primary health care dental Disadvantages of iwm
Disadvantages of iwm Formuö
Formuö Novell typiska drag
Novell typiska drag Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens Returpilarna
Returpilarna Varför kallas perioden 1918-1939 för mellankrigstiden?
Varför kallas perioden 1918-1939 för mellankrigstiden? En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Särskild löneskatt för pensionskostnader
Särskild löneskatt för pensionskostnader Personlig tidbok för yrkesförare
Personlig tidbok för yrkesförare A gastrica
A gastrica Densitet vatten
Densitet vatten Datorkunskap för nybörjare
Datorkunskap för nybörjare Boverket ka
Boverket ka Debatt mall
Debatt mall Autokratiskt ledarskap
Autokratiskt ledarskap Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Påbyggnader för flakfordon
Påbyggnader för flakfordon Vätsketryck formel
Vätsketryck formel Publik sektor
Publik sektor