Inguinal Hernia of Premature Infants 20050203 R 1

- Slides: 21
Inguinal Hernia of Premature Infants 2005/02/03 R 1林群博
Brief History n n 2 months old male infant G 3 P 1 AA 2 GA: 28 weeks+6 Birth body weight: 1302 gm
Brief History n n n Maternal APH, PPROM, placental abruptio C/S on 2004/11/11 Apgar score: 7→ 8
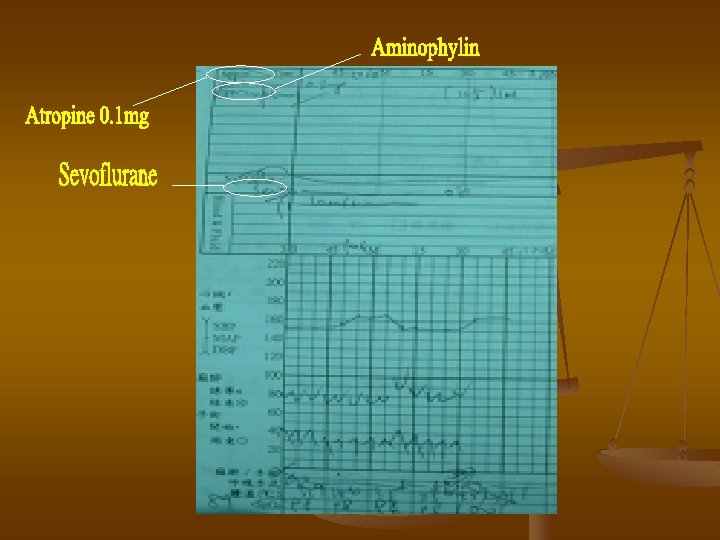
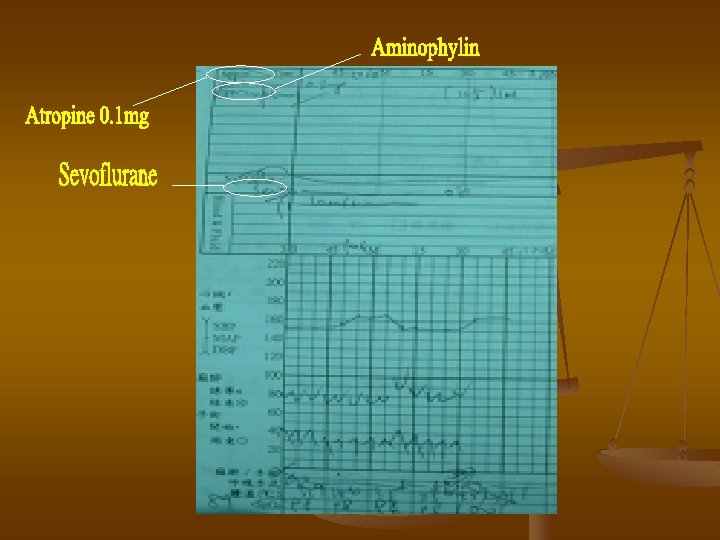
Brief History n n Frequent apnea episodes on 11/13 -14 and aminophylline was given Abscess and osteomyelitis in 2005/12 Pre-op: BW: 2644 gm Herniorraphy for umbilical and right inguinal hernia on 2005/1/21
Discussion n 1. When should repair of inguinal hernia be done? 2. Anesthetic risks for surgery of premature infants 3. What kind of anesthetic technique is better?
Inguinal Hernia in Prematurity n n n Incidence: 14 -30%(children: 2%) Higher incidence of incarceration in infants Hernia repair when ready for discharge has be accepted Pediatr Surg Int (1999) 15: 36 -39
Inguinal Hernia in Prematurity n n VLBW infants had a longer operation time and a longer waiting period Preoperative medical complication: RDS, sepsis, and cardiac failure→ considered to delay surgery The shorting waiting group had shorter operation time No correlation between operation time and body weight at surgery
Inguinal Hernia in Prematurity n n For long waits for surgery in VLBW infants: hernia sac may grow large and thick, and fibrous adhesions may develop Difficult surgical repair and the risk of gonadal ischemia may be increased
The Most Common Medical Problems in Prematurity n n n Respiratory distress syndrome (RDS) Apnea of prematurity Anemia of prematurity Patent ductus arteriosus Intraventricular hemorrhage
The Formerly Premature Infant n Bronchopulmonary dysplasia (BPD): 1. the sequelae of RDS 2. the leading cause of chronic lung disease during infancy 3. periodic episodes of bronchospasm, especially during URI
Anesthetic Management of Infants with BPD n n n Optimization of respiratory status Deep extubation to avoid bronchospasm Regional analgesia in abdominal procedures for pain control
Laryngeal and Tracheal Injury n n Prolonged intubation and mechanical ventilation Subglottic stenosis Smaller ET tube when intubation Stridor following extubation
Postoperative Apnea n n n May be accompanied by bradycardia Probably related to the effects of general anesthetic agents on the immature respiratory control center Low gestational age, low postconceptional age, preoperative apnea of prematurity
General VS Spinal Anesthesia n n n GA<36 wks and post-conceptual age (PCA)<46 wks Exclude preexisting cardiac, neuromuscular or metabolic diseases Preoperative hemoglobin and a history of preexisting abnormal respiratory function British Journal of Anaesthesia 86 (3): 366 -71 (2001)
General Anesthesia (Group 1) n n Induction: 2 MAC sevoflurane and atracurium 0. 5 mg/kg Maintenance: 0. 5 -1. 0 MAC sevoflurane until completion of skin closure Reversed with neostigmine 50 μg/kg and glycopyrrolate 10 μg/kg Caudal epidural injection with 0. 25% bupivacaine 2 mg/kg
Spinal Anesthesia (Group 2) n n 0. 5% bupivacaine 1 mg/kg Caudal epidural injection with 0. 25% bupivacaine 2 mg/kg
Results n n n Spinal anesthesia was attempted unsuccessfully in four patients in group 2 5 patients in group 1 demonstrated an excess number of episodes of postoperative cardiopulmonary complications 3 patients had preexisting abnormal respiratory function and accounted for 80% of the episodes
Prevention of Postoperative Apnea n n n Performing a regional anesthetic instead of a general anesthetic Perioperative administration of caffeine Selection of general anesthetic agents or opoids that are characterized by their limited duration of action
Regional Anesthesia n n n Lower incidence (not complete absence) of postoperative apnea The risk is similar to general anesthesia hen adding systemic sedatives Potentially stressful for the infant and associated with a clinically significant failure rate

Thanks for Your Attention!!
 Difference between direct and indirect hernia ppt
Difference between direct and indirect hernia ppt Hernia inguinal derecha
Hernia inguinal derecha Inguinal hernia are a female reproductive health issue
Inguinal hernia are a female reproductive health issue Sublingual hernia
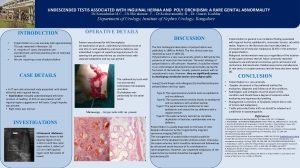
Sublingual hernia Funiculus spermaticus canalis inguinalis
Funiculus spermaticus canalis inguinalis Hernia inguinal videolaparoscopia
Hernia inguinal videolaparoscopia Indirect vs direct hernia
Indirect vs direct hernia Ileopubico
Ileopubico Malgaigne’s bulgings
Malgaigne’s bulgings Pediatric surgery
Pediatric surgery Spermatic cord layers
Spermatic cord layers Inguinal hernia definition
Inguinal hernia definition Conjoint tendon
Conjoint tendon Layers of spermatic fascia
Layers of spermatic fascia Nyhus
Nyhus Fisiopatologia hernia inguinal
Fisiopatologia hernia inguinal Triangle defenition
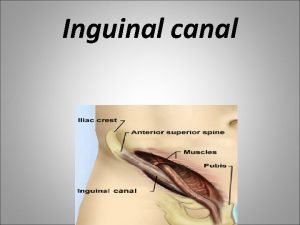
Triangle defenition Inguinal canal
Inguinal canal Exomphalos vs omphalocele
Exomphalos vs omphalocele Hiatus subinguinalis
Hiatus subinguinalis Triangulo miopectineo de fruchaud
Triangulo miopectineo de fruchaud Maniobra de landivar
Maniobra de landivar