Infection control for house officers at the Omaha




- Slides: 42
Infection control for house officers at the Omaha VA Medical Center Infection Control Practitioner Pager 13 -485 ext. 3319 MRSA Prevention Coordinator Pager 13 -323 ext. 4226 Hospital Epidemiologist Ext. 5606
Omaha VA uses n n Standard and Transmission-Based Precautions Based on current guideline of the Centers for Disease Control and Prevention (CDC)
Standard Precautions Protective barriers for ALL potential contact with: n All body fluids n n n Blood All secretions All excretions (except sweat) Mucus membranes Non intact skin
Follow CDC 2002 hand hygiene guideline n n No artificial nails, no chipped nail polish Natural nail no longer than 0. 25 inch Wash hands with antimicrobial soap and water if visibly soiled or after caring for Clostridium difficile patients Hand hygiene before and after patient contact, including after removal of gloves. Generally use alcohol handrub.
Personal Protective Equipment (PPE) n What is available for your use? n n n Surgical masks N-95 respirators (must be fit tested) Gloves Gowns Eye protection

Alcohol dispensers often near sinks & in every patient room

Purell alcohol handrub
Transmission based Precautions n n Contact Enhanced contact Airborne Droplet
Contact precautions n Examples of Diseases in this category: n n Drug-resistant organisms (eg MRSA, VRE) SARS (also needs airborne precautions, eye protection)
Contact precautions includes n n n Gown Gloves Hand hygiene Dedicated equipment in the room (including stethoscope, blood pressure cuff) Terminally clean room on discharge of patient from the room
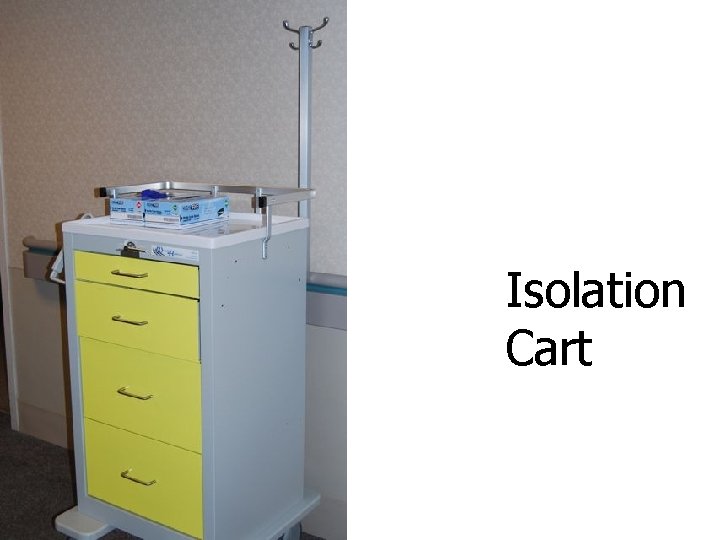
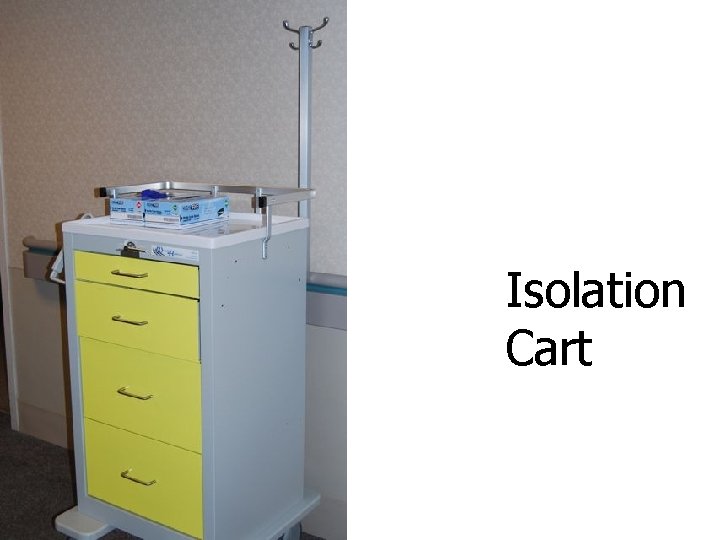
Isolation Cart
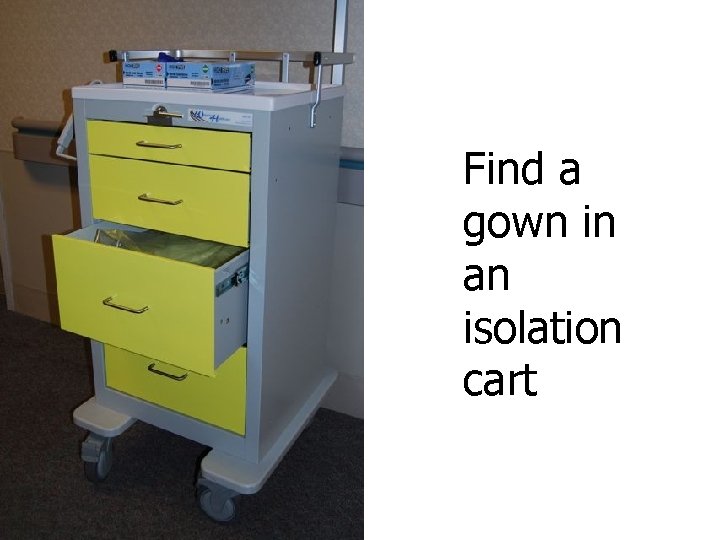
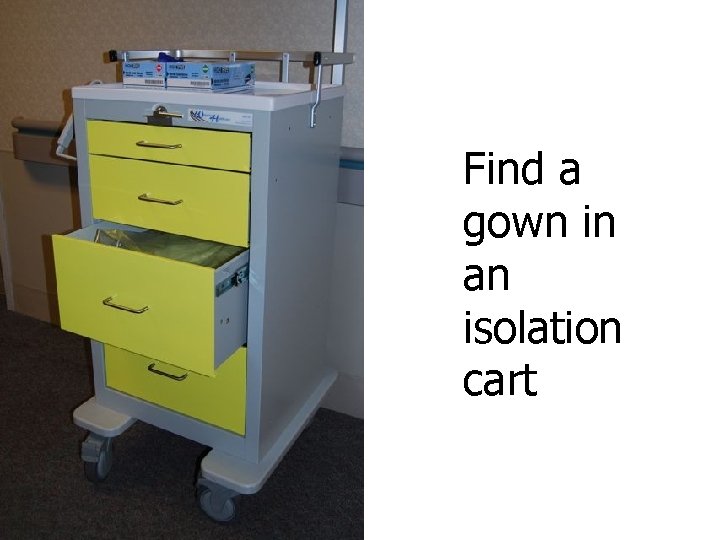
Find a gown in an isolation cart
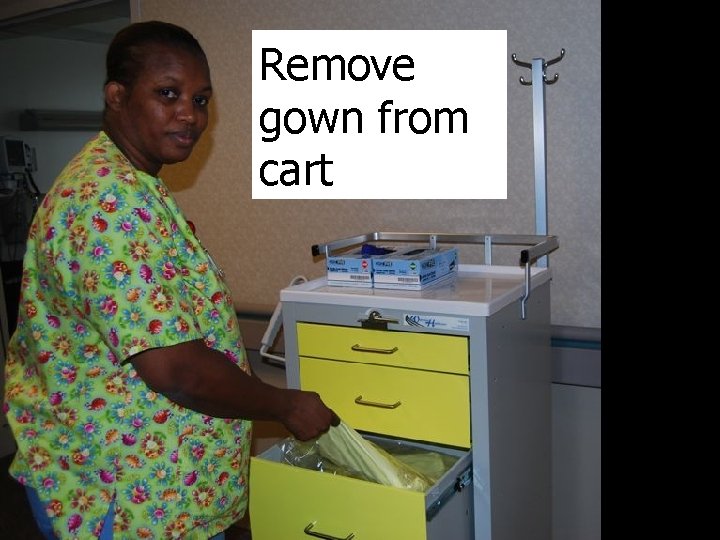
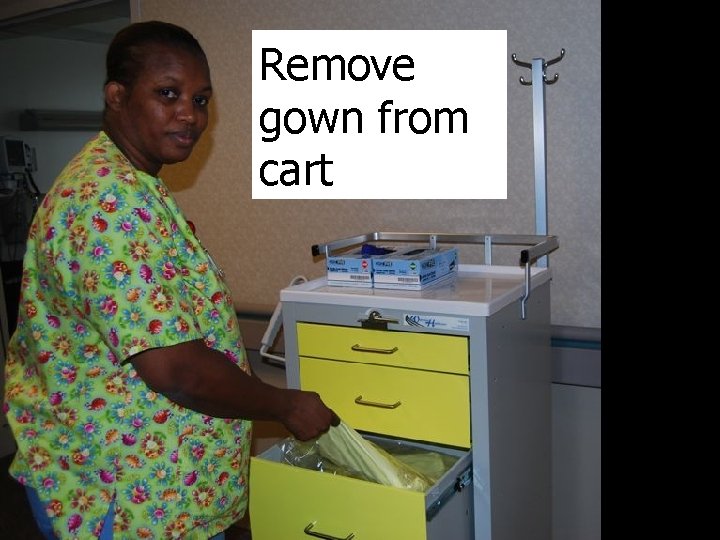
Remove gown from cart
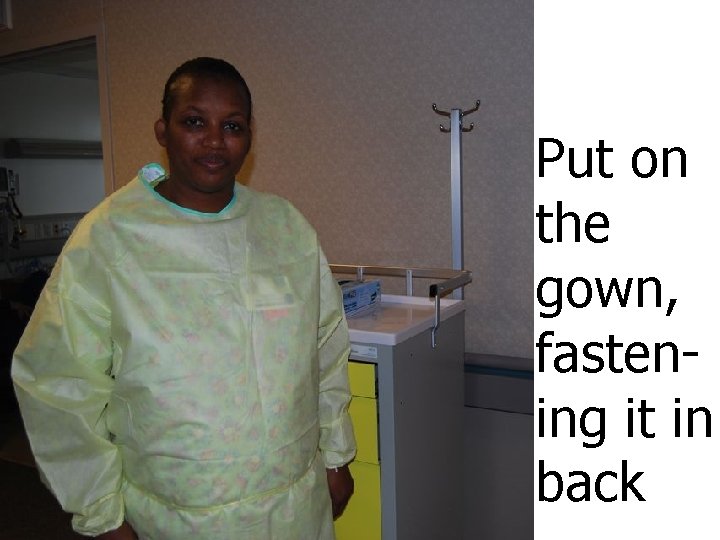
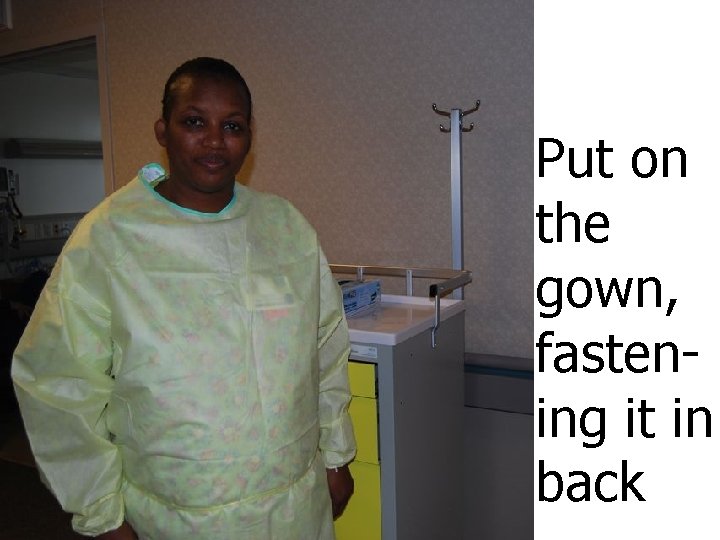
Put on the gown, fastening it in back
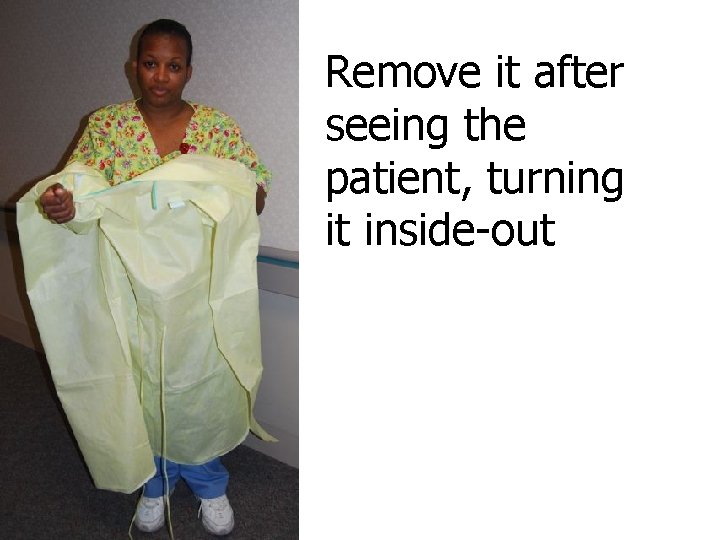
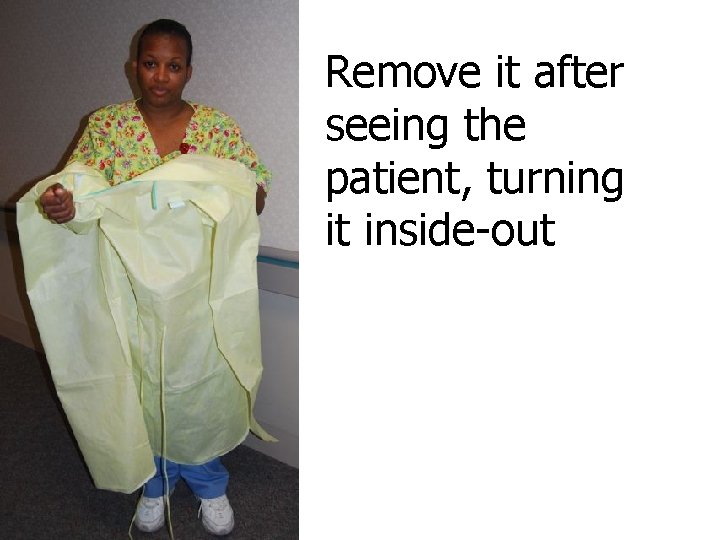
Remove it after seeing the patient, turning it inside-out
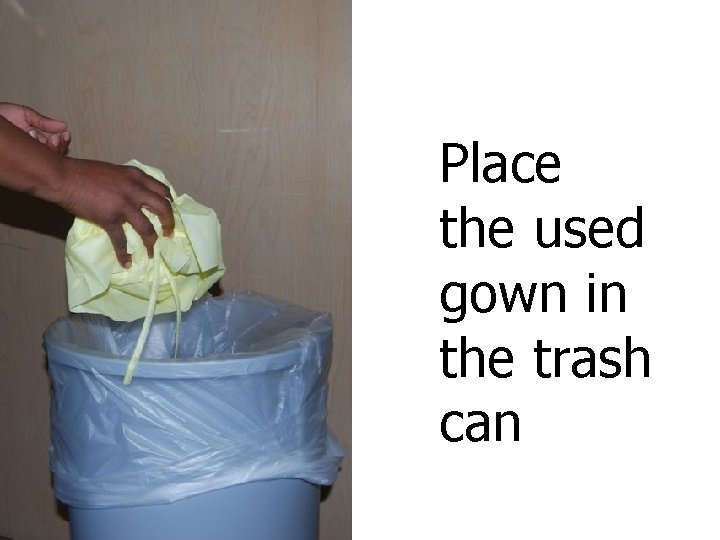
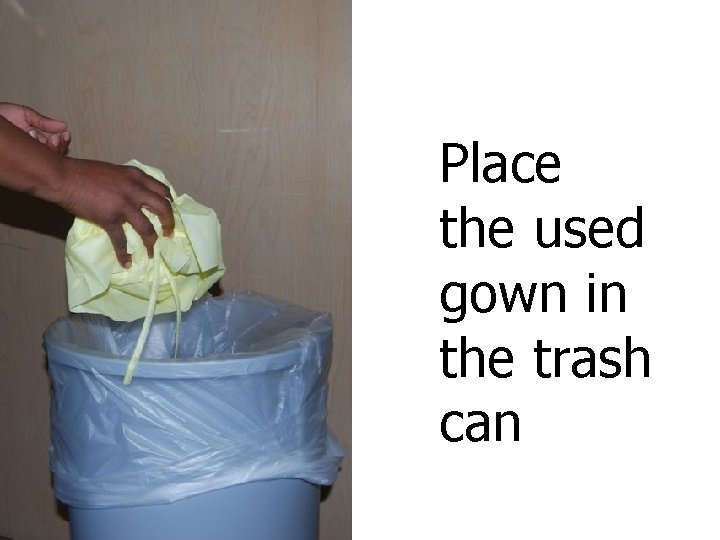
Place the used gown in the trash can
Enhanced contact precautions n Examples of diseases in this category: n n Clostridium difficile Norovirus
Actions: Enhanced contact precautions n n Disinfect hands with antimicrobial soap and water (rather than alcohol gel) Housekeeping staff use special cleaning methods involving bleach
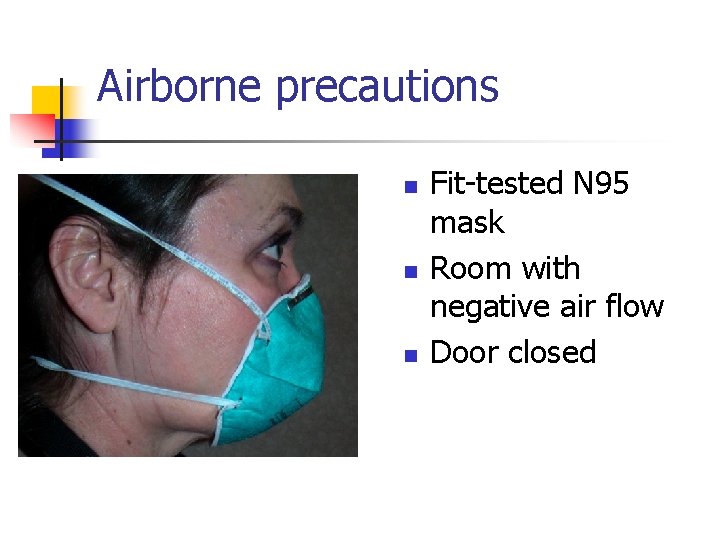
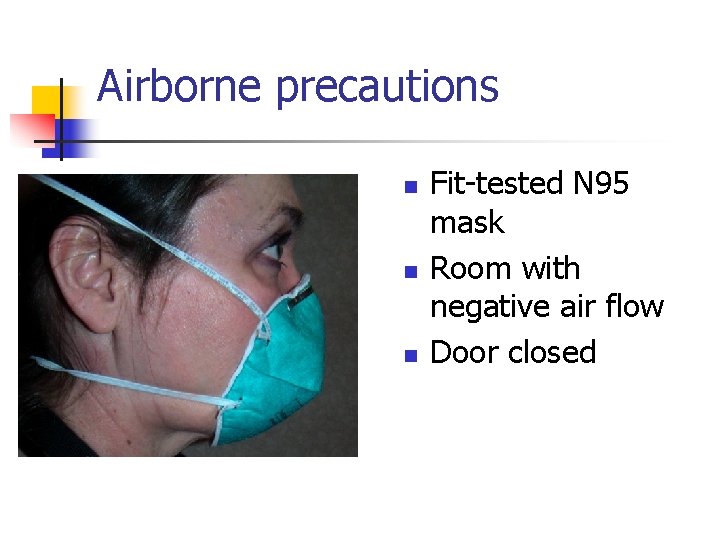
Airborne precautions n n n Fit-tested N 95 mask Room with negative air flow Door closed
Airborne Precautions n Examples of Diseases in this category: n n Tuberculosis Varicella Measles SARS (also needs contact precautions and eye protection)
Common questions on airborne precautions: PPD n n Q. “My patient has a positive tuberculin skin test (PPD test). Is this an indication for airborne precautions? ” A. No, only patients suspected of having active tuberculosis or proven to have active tuberculosis need airborne precautions.
Common questions on airborne precautions: AFB n n Q. “My patient has a laboratory test showing acid-fast bacilli (AFB) in the sputum. Does this mean the patient has tuberculosis? ” A. Not always. So-called atypical mycobacteria that are not causing tuberculosis can result in a lab report of AFB in the sputum and isolation is not indicated.
Rooms for airborne precautions n n n 8 rooms available (includes 2 each in Emergency, ICU, 6 E, and 7 E) Specially equipped to maintain negative flow Reduces risk of pathogens drifting in air currents from infected patient to other patient rooms
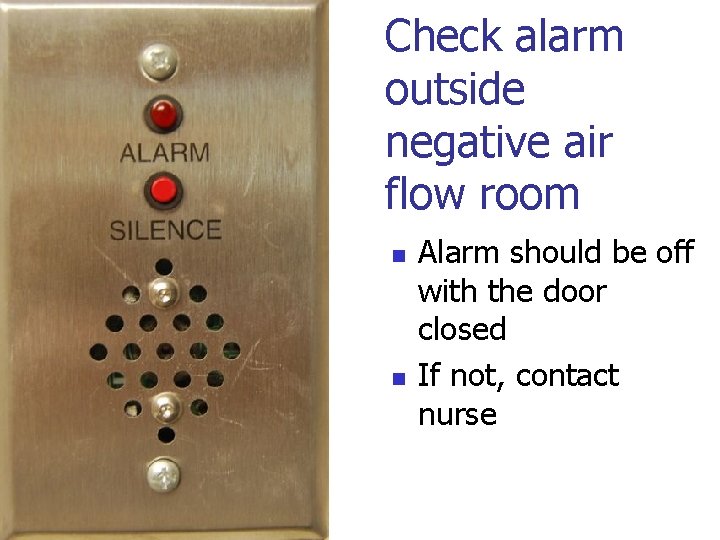
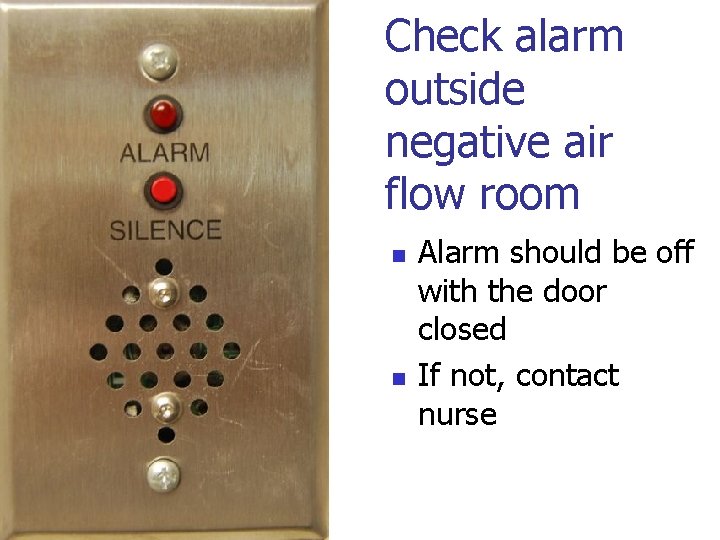
Check alarm outside negative air flow room n n Alarm should be off with the door closed If not, contact nurse
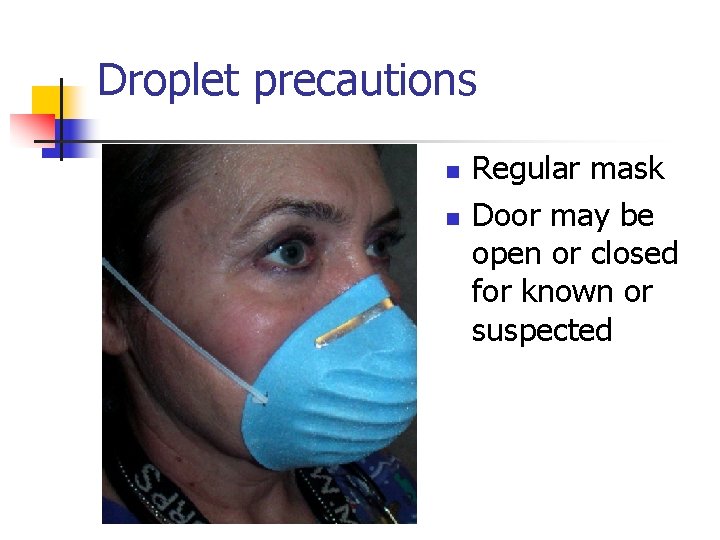
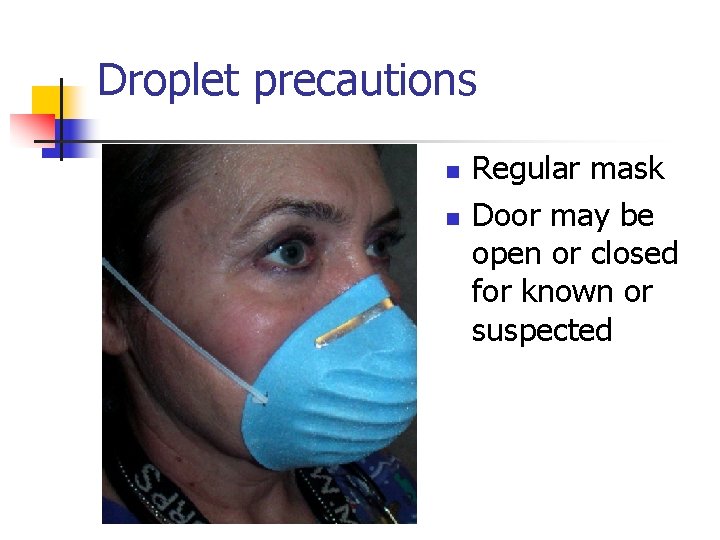
Droplet precautions n n Regular mask Door may be open or closed for known or suspected
Droplet Precautions n Examples of disease in this category: n Influenza Pertussis n Neisseria meningitidis n
Employee Health Issues n Blood and body fluid exposure n n n Immediately notify supervisor Immediately call Occupational Health (5825) during day hours or go to Urgent Care area after hours Do so immediately since post exposure prophylaxis for HIV should be started, ideally within an hour FREE influenza vaccine provided for all Tuberculin skin test annually at host institution: CUMC or UNMC Hepatitis B vaccine at host institution
All blood and body fluid exposures are important n Sharps Injuries n n n Needle stick Scalpel cut Pipette break Any injury that breaks the skin in the presence of body fluids Mucous membrane exposure

If a Blood Exposure Occurs: n n Clean the exposed area with soap and water. For exposed mucous membranes, flush with water. DO NOT use bleach or surface disinfectants. Report incident to supervisor immediately. Report to Employee Health or Urgent Care area as previously described. Fill out an Incident Report via the electronic reporting system - ASISTS
Follow-up of blood or body fluid exposure n n n Follow-up after initial visit to Urgent Care Occupational health nurse practitioner Call 3209 to schedule visit
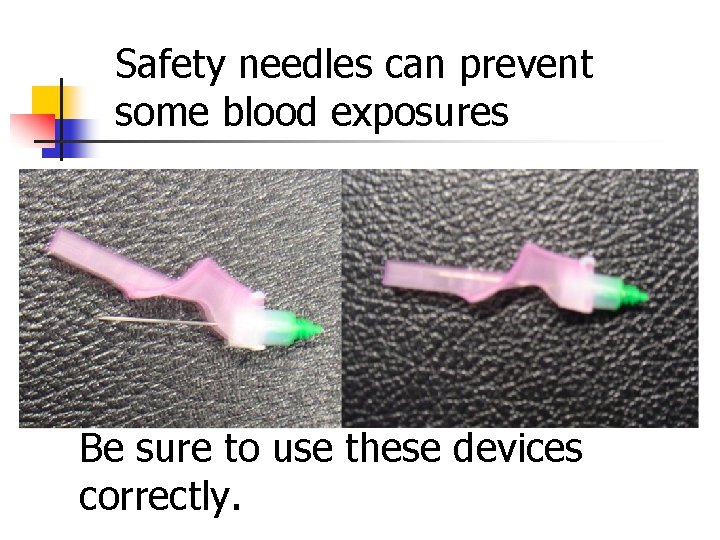
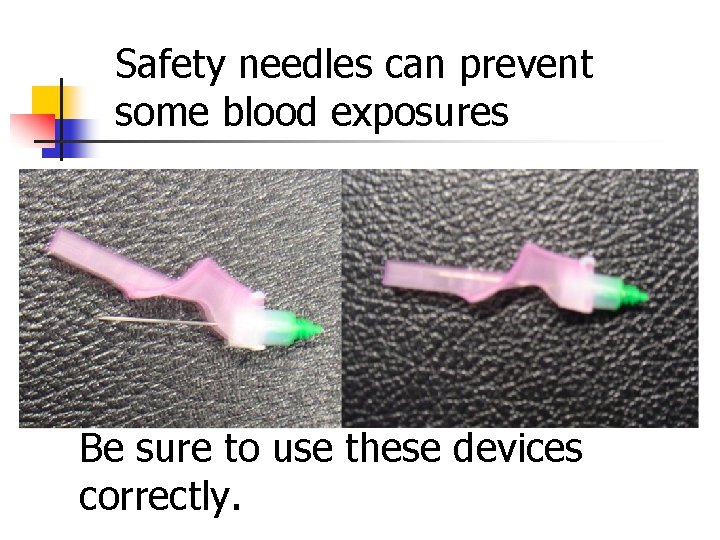
Safety needles can prevent some blood exposures Be sure to use these devices correctly.

Sharps disposal containers in each room
Needle/Sharps Disposal n n n DO activate safety device DO locate the disposal container closest to your work area DO look to be sure that the opening of the box is clear of sharps Do NOT recap by hand Do NOT bend, clip or break
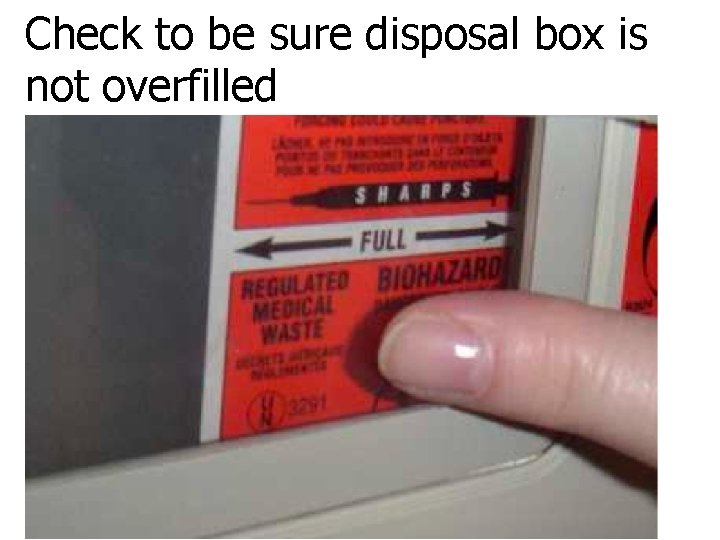
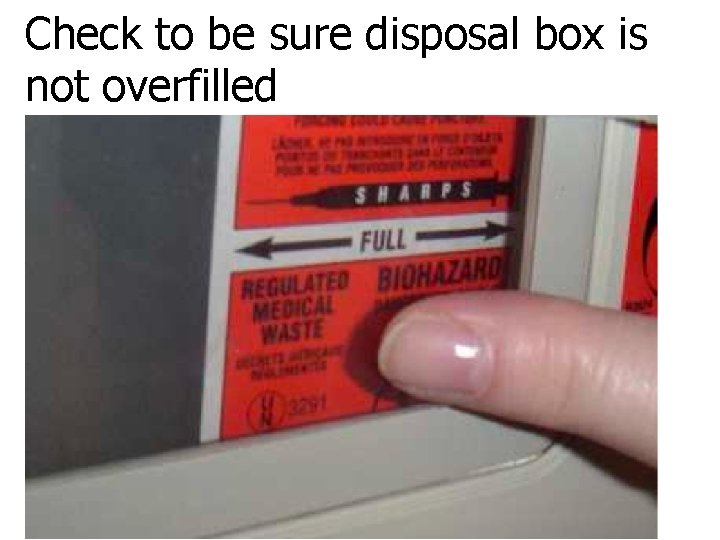
Check to be sure disposal box is not overfilled
Aims of OSHA bloodborne pathogens standard n To protect employees from n Occupational exposure to blood or other potentially infectious materials n Transmission of bloodborne diseases
Bloodborne diseases of concern Human immunodeficiency virus (HIV) n Hepatitis B (HBV) n Hepatitis C (HCV) n
Transmission in the workplace occurs by: n Parenteral Exposure Needle stick, blood transmission n Mucous Membrane Exposure n n n Mouth, eyes In the community, they may be transmitted through IV drug use and from mother to baby.
Human Immunodeficiency Virus (HIV) n n Virus that causes AIDS Attacks the immune system May be no obvious signs of infection Can transmit virus before illness known
Hepatitis B (HBV) n Symptoms if liver damage develops: n n n n Poor appetite Fatigue Abdominal discomfort Jaundice 125, 000 people infected yearly in US 5 -10% become chronic carriers 5 -10% of those advance to liver disease Hepatitis B Vaccine is available to prevent disease
Hepatitis C (HCV) n n n Symptoms same as Hepatitis B Antibodies may not provide immunity Up to 85% will develop chronic hepatitis 3. 9 million chronically infected in US Sexual transmission uncertain
Respiratory etiquette to prevent transmission n n Cover your cough or sneeze Deposit tissues directly into the trash Clean hands after use of tissues or cough/sneeze Offer tissues or mask to others with coughing or sneezing Remind them to clean hands
Infection Control is Everyone’s Responsibility!
 Dental radiography ppt
Dental radiography ppt Chemical germicides formulated for use on skin
Chemical germicides formulated for use on skin Chapter 16 infection control and standard precautions
Chapter 16 infection control and standard precautions Chapter 16 infection control and standard precautions
Chapter 16 infection control and standard precautions Chapter 15:3 washing hands
Chapter 15:3 washing hands Chapter 15 infection control
Chapter 15 infection control Certification in infection control cic
Certification in infection control cic Infection control definition
Infection control definition Infection control in dental radiology
Infection control in dental radiology Learning objectives for infection control
Learning objectives for infection control Conclusion of infection
Conclusion of infection Cna infection control
Cna infection control Cbic recertification
Cbic recertification Infection control is everyone's responsibility
Infection control is everyone's responsibility Infection control
Infection control Tier 1 standard precautions
Tier 1 standard precautions Infection control information
Infection control information Root locus drawer
Root locus drawer Infection control orientation
Infection control orientation Infection control
Infection control Infection control audits
Infection control audits Environmental controls infection control
Environmental controls infection control Another name for customer service
Another name for customer service Infection control committee
Infection control committee Conclusion of infection control
Conclusion of infection control Rigid thinking examples
Rigid thinking examples Infection control champion
Infection control champion Unit 13 infection control
Unit 13 infection control Infection control surveyor worksheet
Infection control surveyor worksheet Chapter 10 infection control
Chapter 10 infection control Bel retired officers association bangalore
Bel retired officers association bangalore Community college business officers
Community college business officers Ft belvoir officers club
Ft belvoir officers club Chief instructional officers california community colleges
Chief instructional officers california community colleges California community college chief instructional officers
California community college chief instructional officers International foundation for protection officers
International foundation for protection officers Uk chief medical officers' physical activity guidelines
Uk chief medical officers' physical activity guidelines 36 officers problem
36 officers problem The police officers pledge
The police officers pledge Short choppy sentences in the tell tale heart
Short choppy sentences in the tell tale heart Ra 6975
Ra 6975 What were the military duties of ranked officers othello
What were the military duties of ranked officers othello Canton police officers
Canton police officers