Increased use of Advanced Medical Imaging Radiation Exposure







- Slides: 54
Increased use of Advanced Medical Imaging, Radiation Exposure, and Cancer Risk Diana L. Miglioretti, Ph. D Group Health Research Institute Rebecca Smith-Bindman, MD University of California, San Francisco May 31, 2011 | D. Miglioretti, Ph. D
Outline § Background • Utilization of medical imaging • Cancer risk from radiation • Radiation from medical imaging § Study of dose from CT at 4 San Francisco Bay Area Facilities • Dose from CT is high and variable § Study of imaging at 7 integrated healthcare systems • • Imaging utilization and radiation exposure CT use in children Radiation exposure from CT in children Leukemia risk § Discussion & Conclusions
Benefits of Medical Imaging § Earlier and more accurate diagnosis of disease • Earlier treatment • Improved patient outcomes § Quick diagnosis (e. g. , CT use in ED) § Less invasive diagnosis § Accurate prognosis § Reassurance
Harms Associated with Imaging § Radiation exposure § Doses of common exams (e. g. , CT) in carcinogenic range § Rare - accidental overdose § False positives – Unnecessary follow-up testing, anxiety, cost § Incidental findings – Cascade of testing to rule out disease § Overdiagnosis – Unnecessary treatment § Contrast reactions – Most minor, some major § Healthcare costs § Advanced imaging is expensive
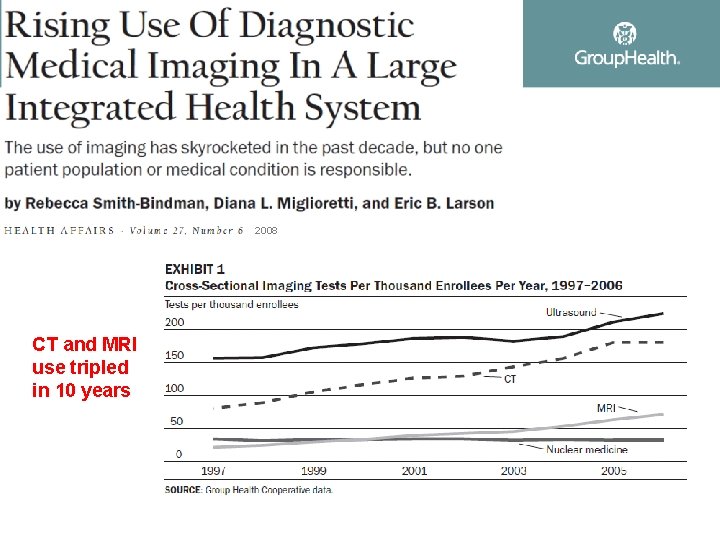
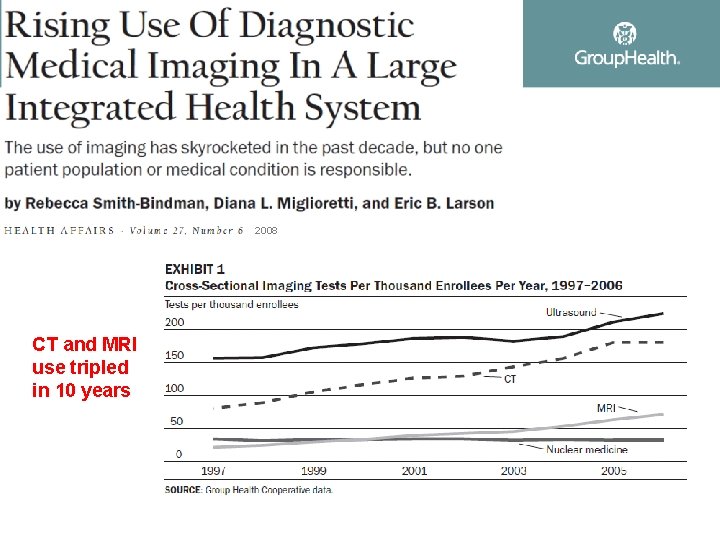
2008 CT and MRI use tripled in 10 years
Radiation and Cancer Risk
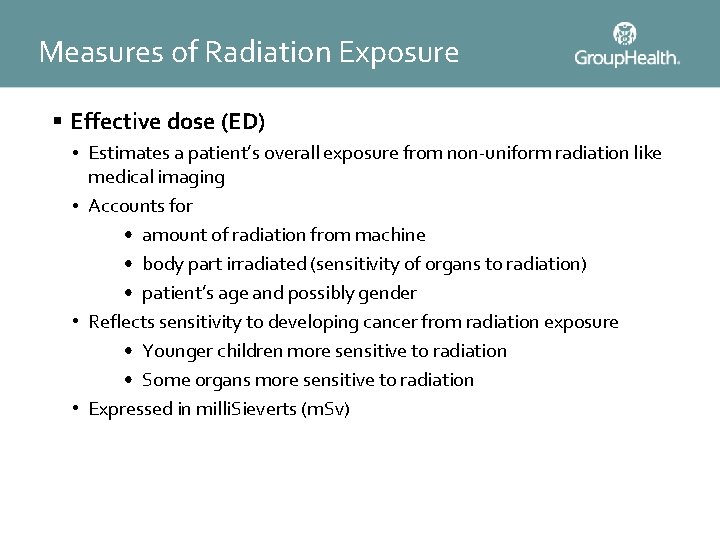
Measures of Radiation Exposure § Effective dose (ED) • Estimates a patient’s overall exposure from non-uniform radiation like medical imaging • Accounts for • amount of radiation from machine • body part irradiated (sensitivity of organs to radiation) • patient’s age and possibly gender • Reflects sensitivity to developing cancer from radiation exposure • Younger children more sensitive to radiation • Some organs more sensitive to radiation • Expressed in milli. Sieverts (m. Sv)
BEIR VII Report § The U. S. National Academies of Sciences Biological Effects of Ionizing Radiation Committee (BEIR) conducted a comprehensive review of literature on health risks of low dose radiation exposure § Members included leading scientists from a broad range of disciplines § Estimated cancer risk based on dose and age at exposure using a variety of studies
Japanese Atomic Bomb Survivors § Life Span Study of the 120, 000 survivors of the atomic bombings in Hiroshima and Nagasaki Japan § The median dose of survivors was 40 m. Sv § Organ specific radiation doses are linked with organ specific cancers for nearly every cancer § Even at low doses (10 m. Sv), survivors were at a significantly increased risk of developing cancer
Medically Irradiated Populations Malignant Disease § Following radiotherapy for malignant disease, there is an elevated risk of second cancers § Second primary malignancies particularly high among survivors of childhood cancer § Among Hodgkin’s survivors, radiation-induced second primary cancers are a leading cause of mortality
Medically Irradiated Populations Benign Disease § Radiation commonly used 1930 -1960 for benign conditions • • Tinea capitis Enlarged tonsils Enlarged thymus Breast conditions (i. e. , post partum mastitis) § Increased risks of radiosensitive cancers • thyroid, salivary gland, central nervous system, skin, and breast
Medically Irradiated Populations Repeated X-rays § Studies have assessed groups who received repeated radiographs • Scoliosis • Tuberculosis • Children with cardiac catheterizations § All significantly more likely to develop cancer
Radiation Workers § 400, 000 radiation workers in the nuclear industry § Average doses of 20 m. Sv § Significant association between exposure (5 - 150 m. Sv) and cancer mortality § Ongoing studies of radiology technologists, physicians who use radiation suggest increase cancer risks
Summary of Evidence of Harmful Effects of Radiation § A large body of epidemiological and biologic evidence links exposure to radiation (even low doses) with development of cancer § The results are highly consistent across studies § “It has not been scientifically demonstrated that any cancer risk exists below 100 m. Sv” is untrue § The A-bomb survivor data provides best dose response data • However, the effect size is consistent across studies
Radiation Exposure from Medical Imaging
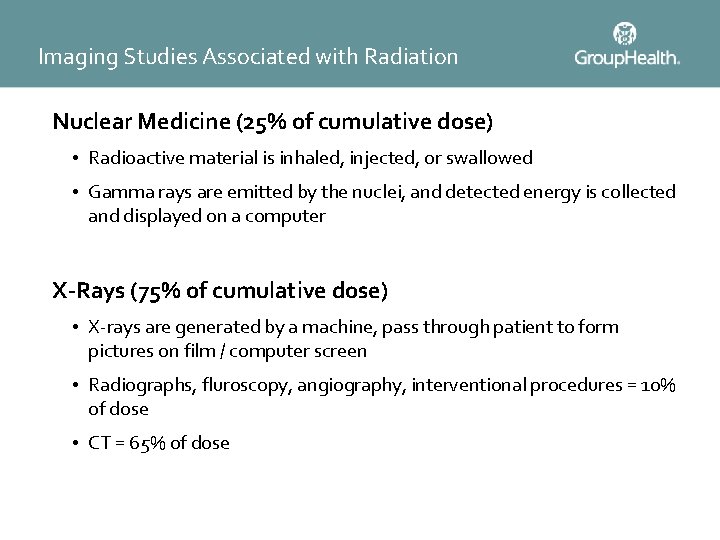
Imaging Studies Associated with Radiation Nuclear Medicine (25% of cumulative dose) • Radioactive material is inhaled, injected, or swallowed • Gamma rays are emitted by the nuclei, and detected energy is collected and displayed on a computer X-Rays (75% of cumulative dose) • X-rays are generated by a machine, pass through patient to form pictures on film / computer screen • Radiographs, fluroscopy, angiography, interventional procedures = 10% of dose • CT = 65% of dose
Medical Radiation § The risks associated with ionizing radiation are not new • Many of the radiology pioneers developed burns or died from radiation -induced cancers § What is new is the dramatic increase in exposures to ionizing radiation from CT
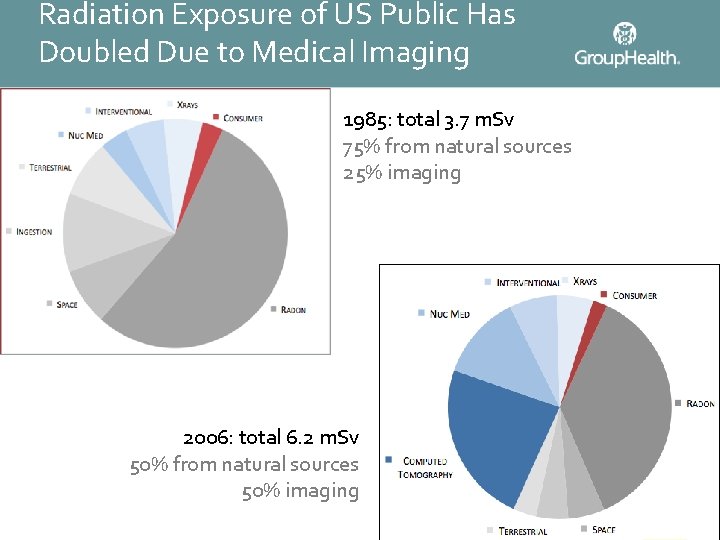
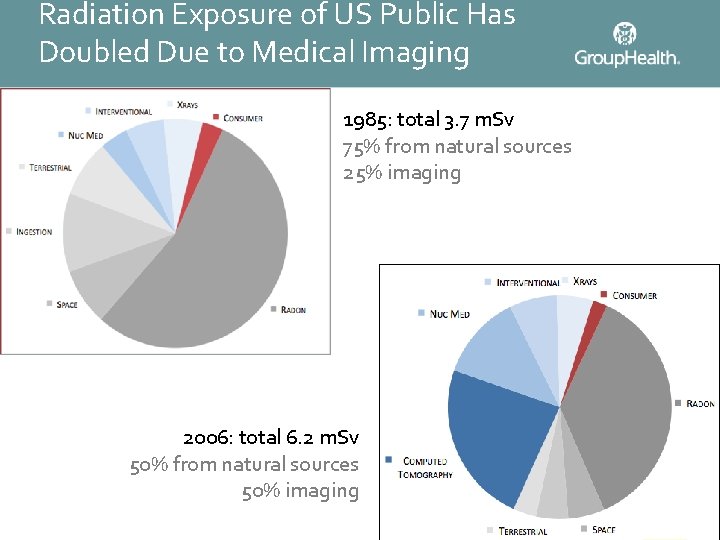
Radiation Exposure of US Public Has Doubled Due to Medical Imaging 1985: total 3. 7 m. Sv 75% from natural sources 25% imaging 2006: total 6. 2 m. Sv 50% from natural sources 50% imaging

Sample Annual Radiation Exposures Source m. Sv Radon 2. 0 Living in Denver 0. 63 Food 0. 40 Sun exposure 0. 27 Dental radiographs (series) 0. 05 Jet travel (6 hours) 0. 03 Airport screening 0. 00001 Chest radiographs (PA & Lat) 0. 06 CT chest 8. 0 CT head, chest, abdomen, pelvis 35 -100
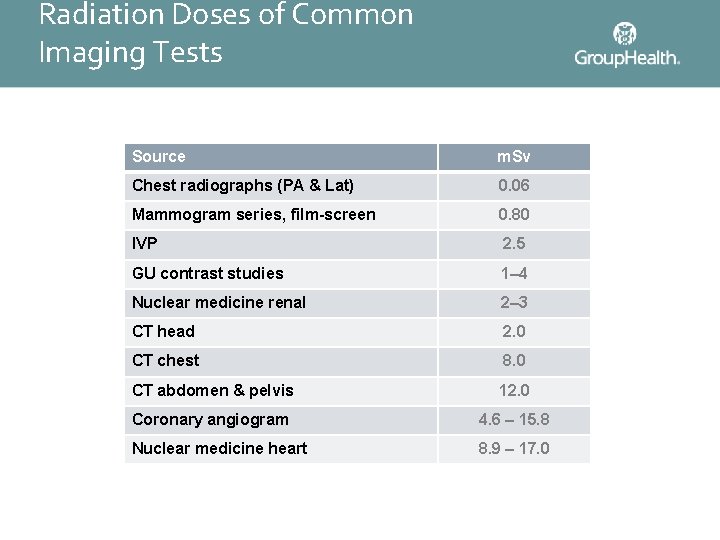
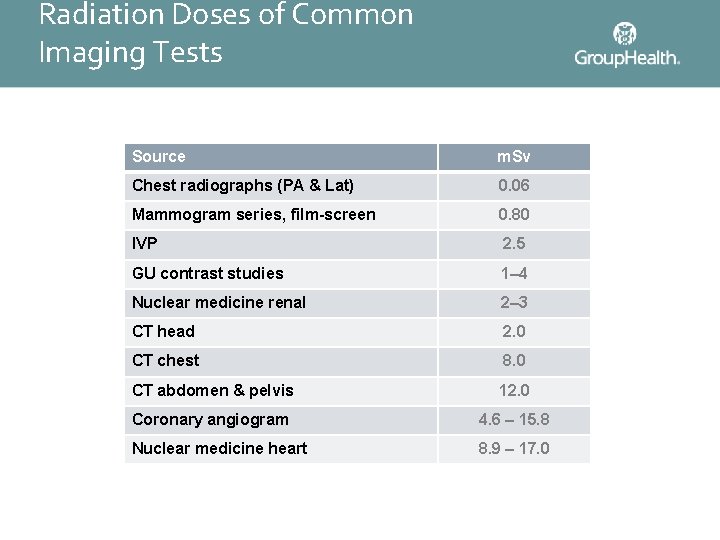
Radiation Doses of Common Imaging Tests Source m. Sv Chest radiographs (PA & Lat) 0. 06 Mammogram series, film-screen 0. 80 IVP 2. 5 GU contrast studies 1– 4 Nuclear medicine renal 2– 3 CT head 2. 0 CT chest 8. 0 CT abdomen & pelvis 12. 0 Coronary angiogram 4. 6 – 15. 8 Nuclear medicine heart 8. 9 – 17. 0
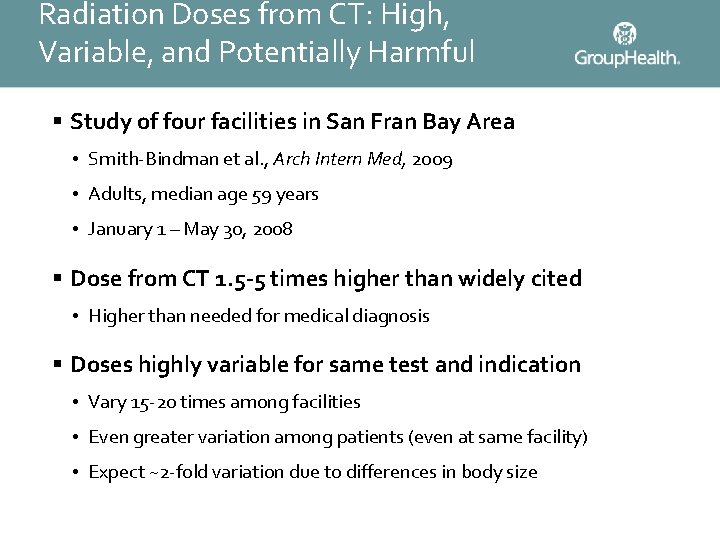
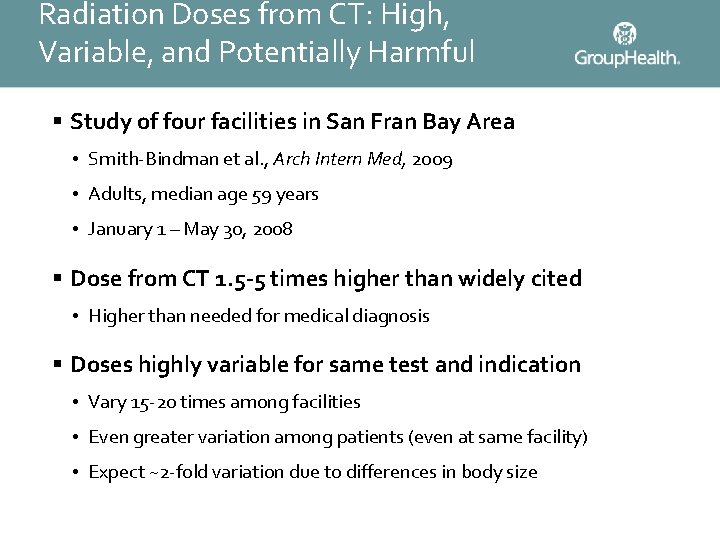
Radiation Doses from CT: High, Variable, and Potentially Harmful § Study of four facilities in San Fran Bay Area • Smith-Bindman et al. , Arch Intern Med, 2009 • Adults, median age 59 years • January 1 – May 30, 2008 § Dose from CT 1. 5 -5 times higher than widely cited • Higher than needed for medical diagnosis § Doses highly variable for same test and indication • Vary 15 -20 times among facilities • Even greater variation among patients (even at same facility) • Expect ~2 -fold variation due to differences in body size
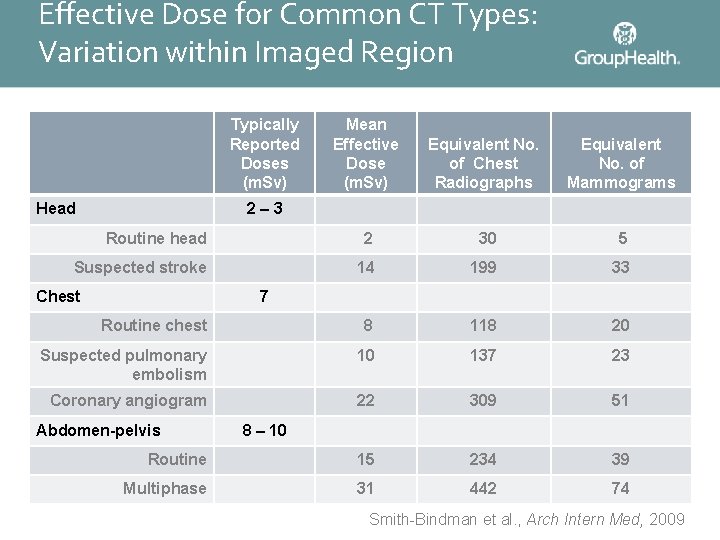
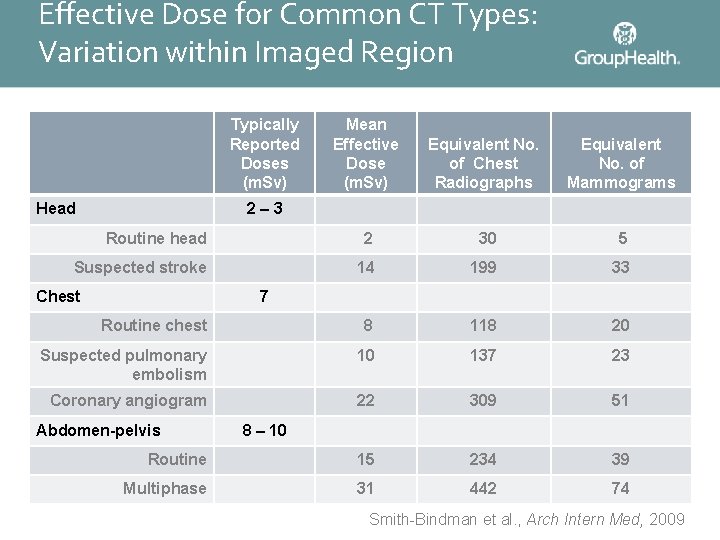
Effective Dose for Common CT Types: Variation within Imaged Region Typically Reported Doses (m. Sv) Mean Effective Dose (m. Sv) Equivalent No. of Chest Radiographs Equivalent No. of Mammograms Routine head 2 30 5 Suspected stroke 14 199 33 Routine chest 8 118 20 Suspected pulmonary embolism 10 137 23 Coronary angiogram 22 309 51 Routine 15 234 39 Multiphase 31 442 74 Head 2– 3 Chest 7 Abdomen-pelvis 8 – 10 Smith-Bindman et al. , Arch Intern Med, 2009
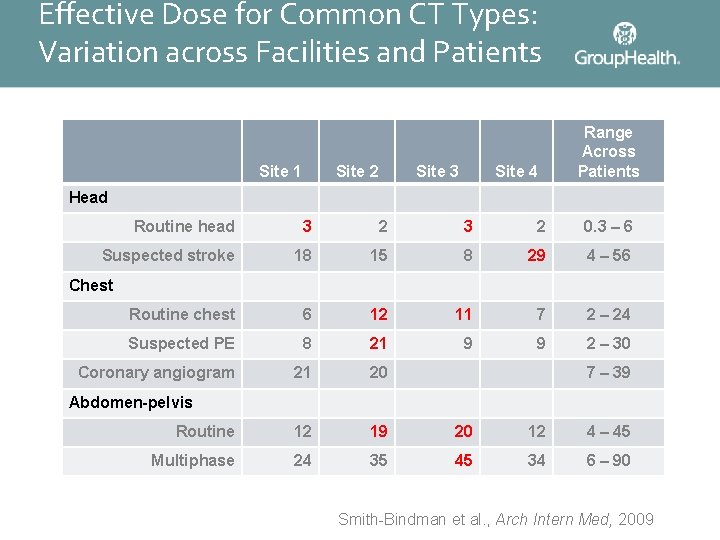
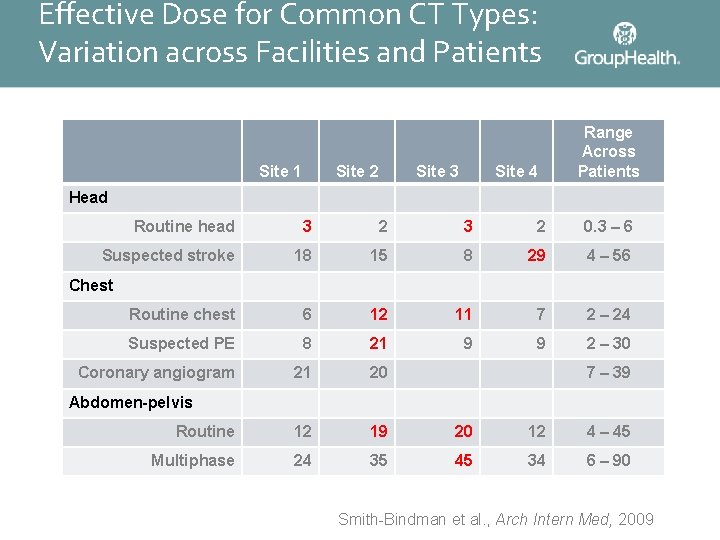
Effective Dose for Common CT Types: Variation across Facilities and Patients Site 1 Site 2 Site 3 Site 4 Range Across Patients Head Routine head 3 2 0. 3 – 6 Suspected stroke 18 15 8 29 4 – 56 Routine chest 6 12 11 7 2 – 24 Suspected PE 8 21 9 9 2 – 30 Coronary angiogram 21 20 Routine 12 19 20 12 4 – 45 Multiphase 24 35 45 34 6 – 90 Chest 7 – 39 Abdomen-pelvis Smith-Bindman et al. , Arch Intern Med, 2009
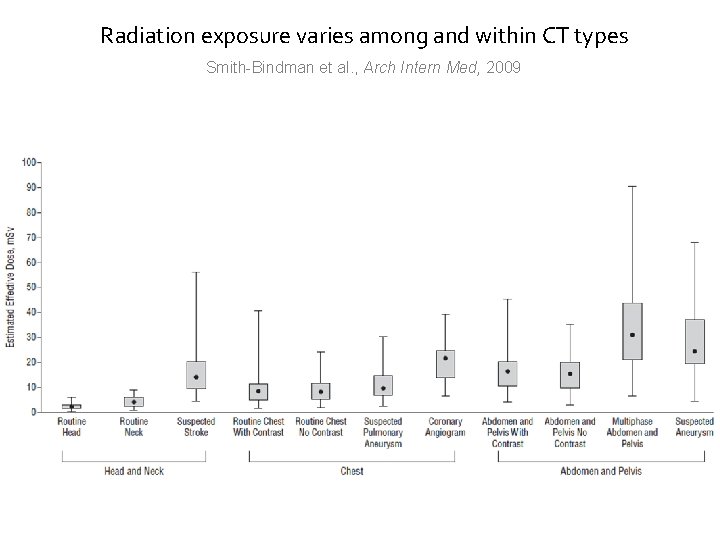
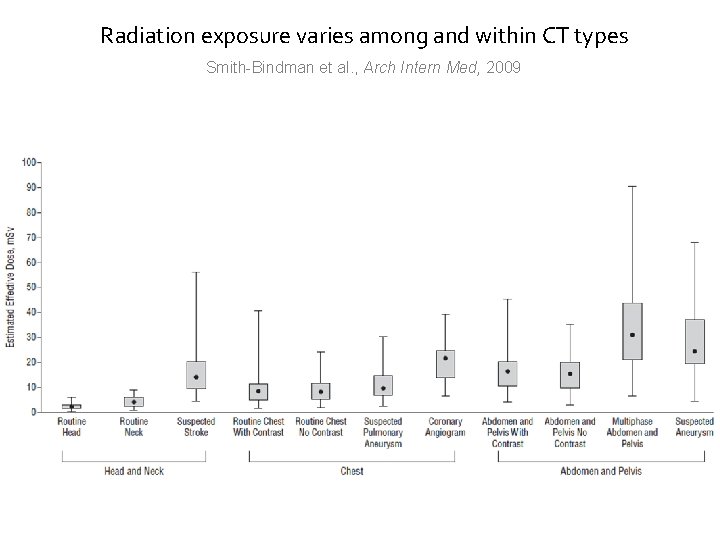
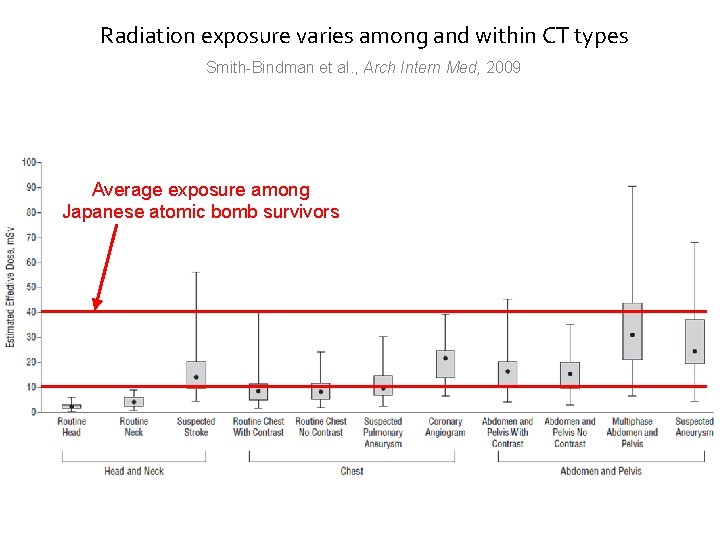
Radiation exposure varies among and within CT types Smith-Bindman et al. , Arch Intern Med, 2009
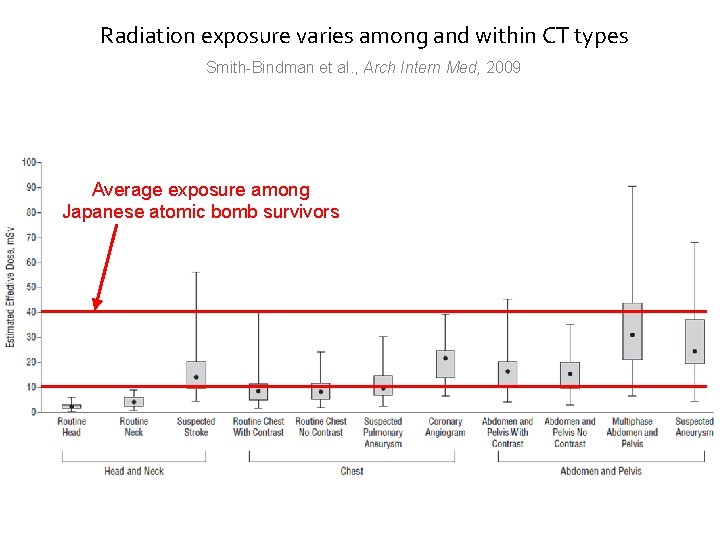
Radiation exposure varies among and within CT types Smith-Bindman et al. , Arch Intern Med, 2009 Average exposure among Japanese atomic bomb survivors
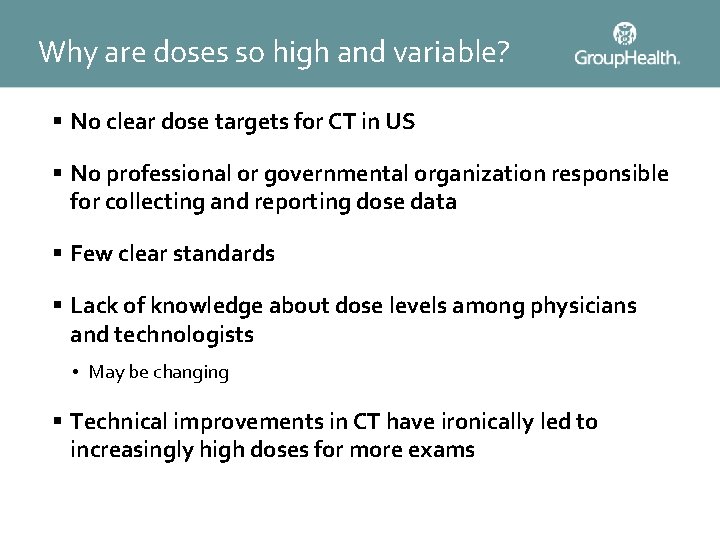
Why are doses so high and variable? § No clear dose targets for CT in US § No professional or governmental organization responsible for collecting and reporting dose data § Few clear standards § Lack of knowledge about dose levels among physicians and technologists • May be changing § Technical improvements in CT have ironically led to increasingly high doses for more exams
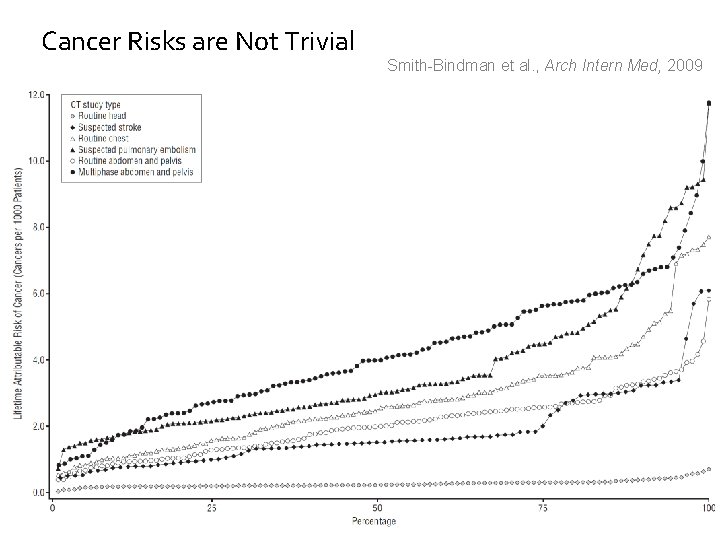
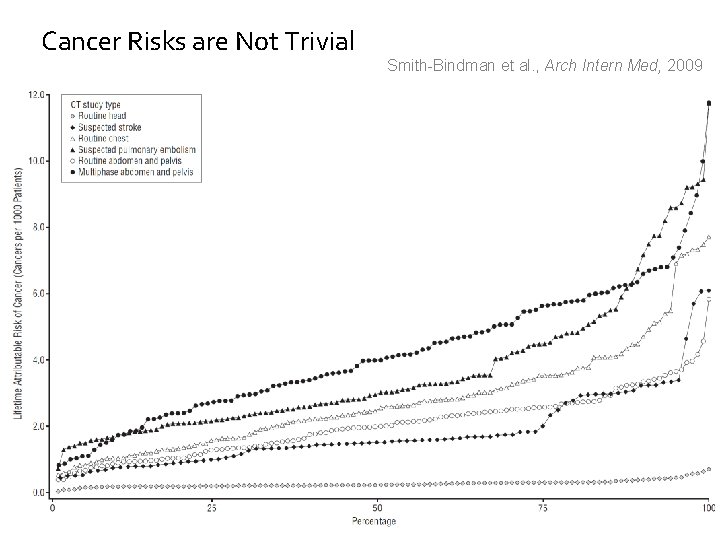
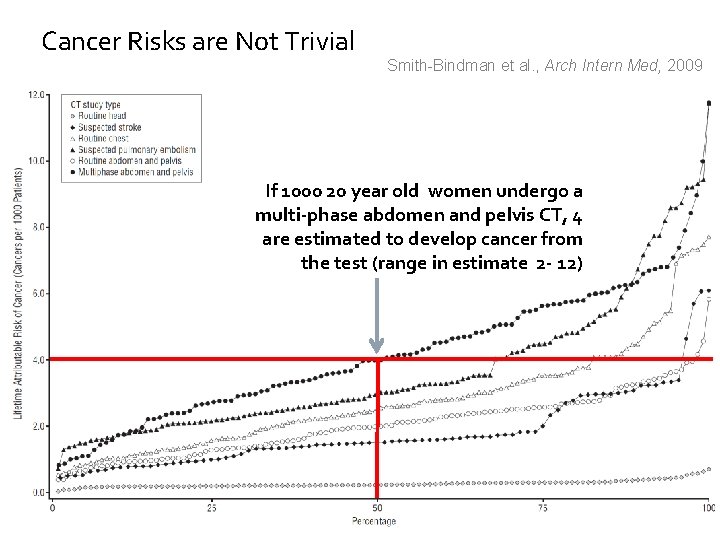
Cancer Risks are Not Trivial Smith-Bindman et al. , Arch Intern Med, 2009
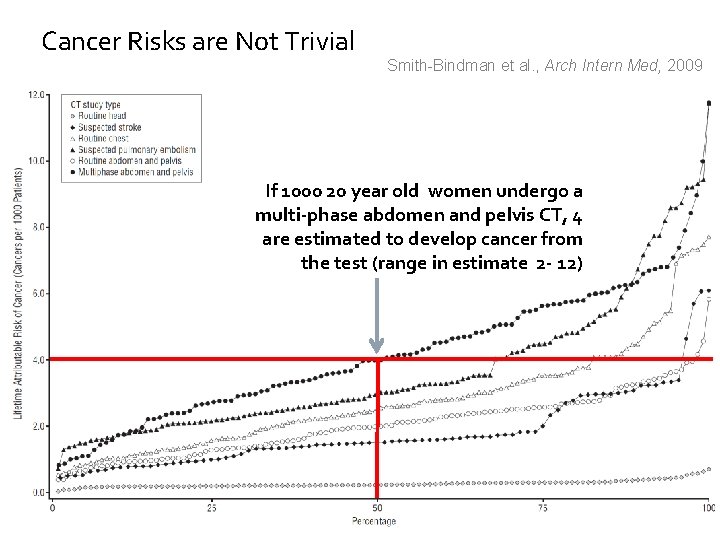
Cancer Risks are Not Trivial Smith-Bindman et al. , Arch Intern Med, 2009 If 1000 20 year old women undergo a multi-phase abdomen and pelvis CT, 4 are estimated to develop cancer from the test (range in estimate 2 - 12)
Image Utilization
Study of Imaging Use § Retrospective observational study § 7 integrated healthcare systems § 1994 -2007 [adding data through 2010] § 2. 5 million members each year
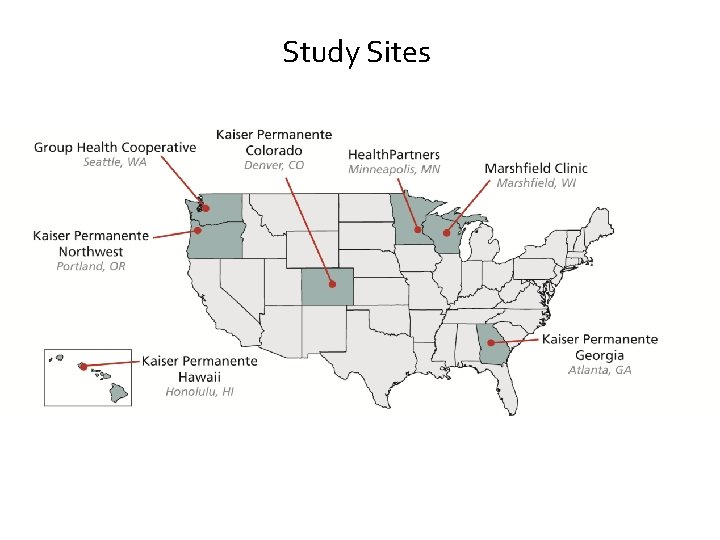
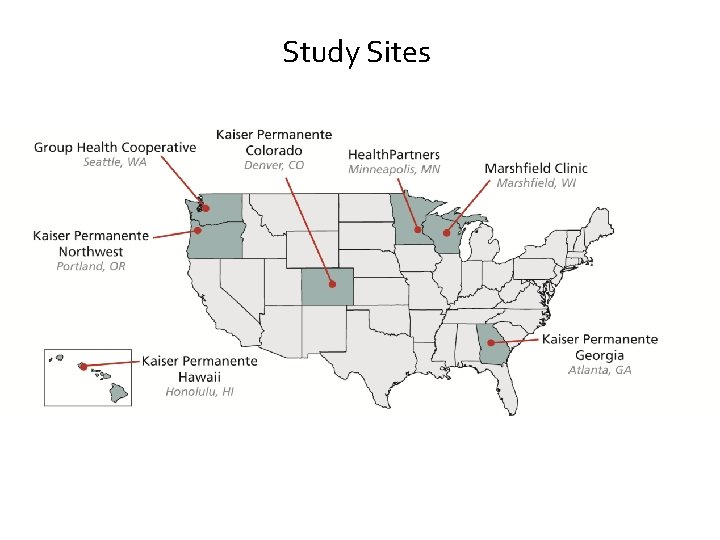
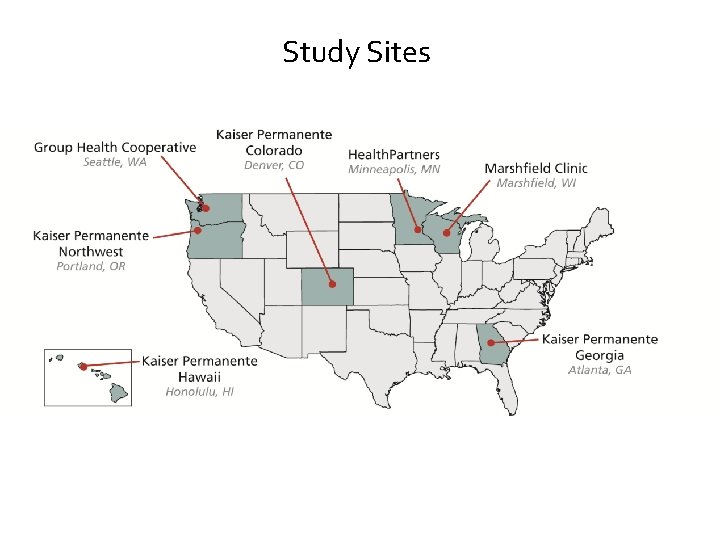
Study Sites
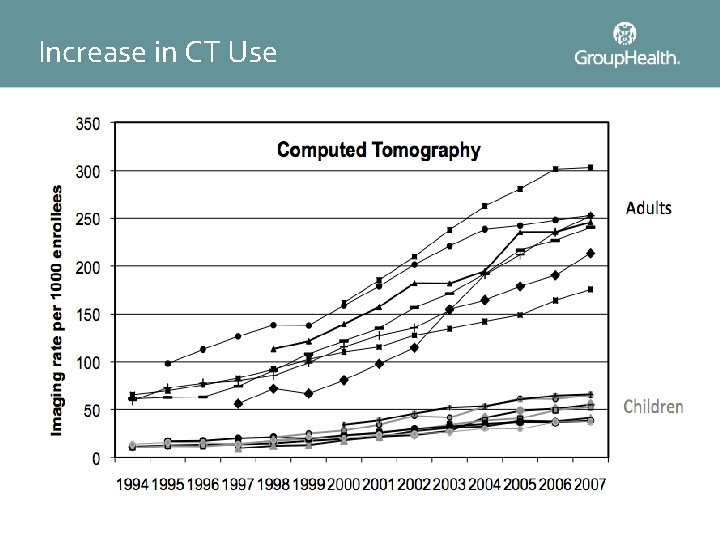
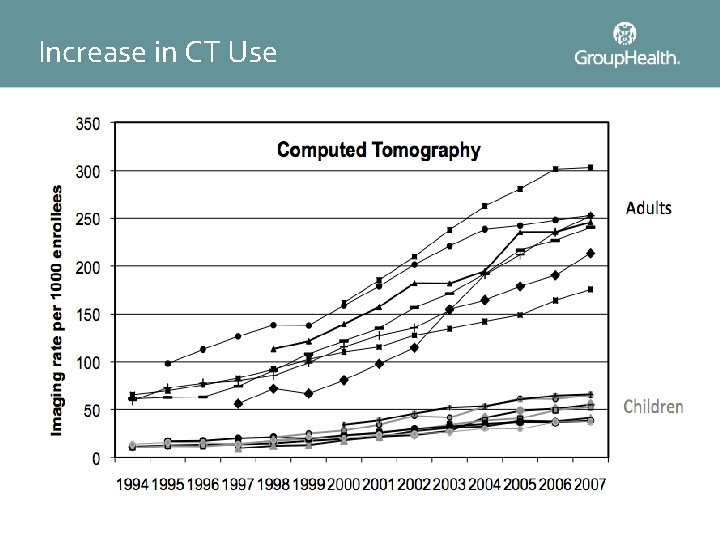
Increase in CT Use
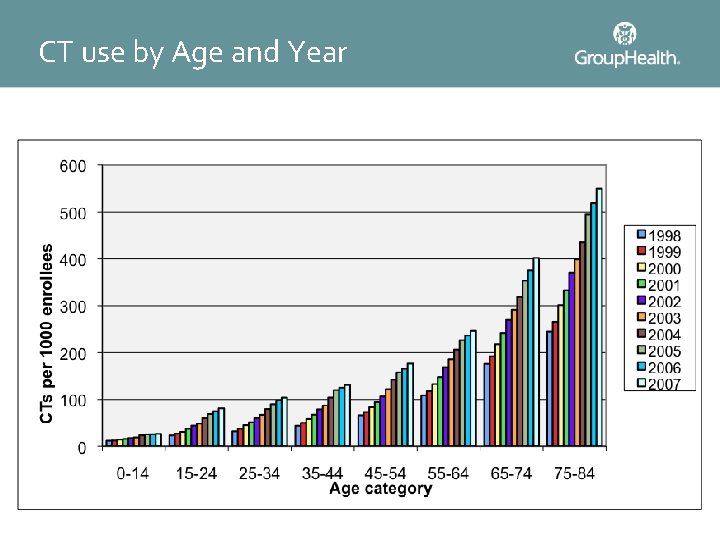
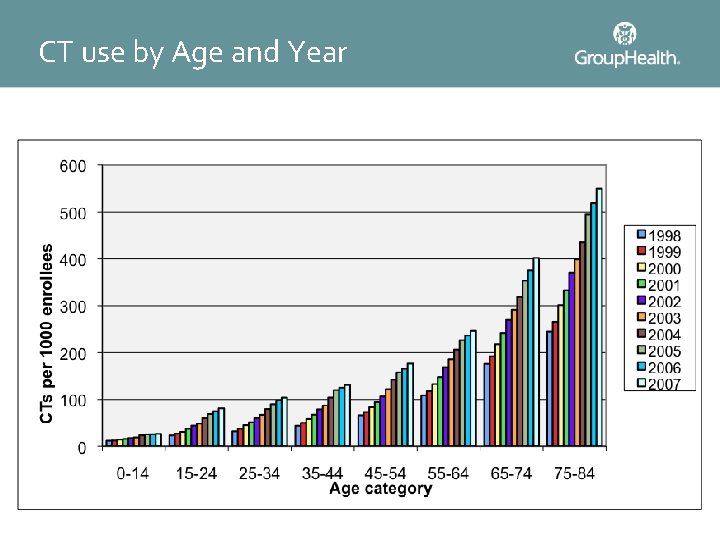
CT use by Age and Year
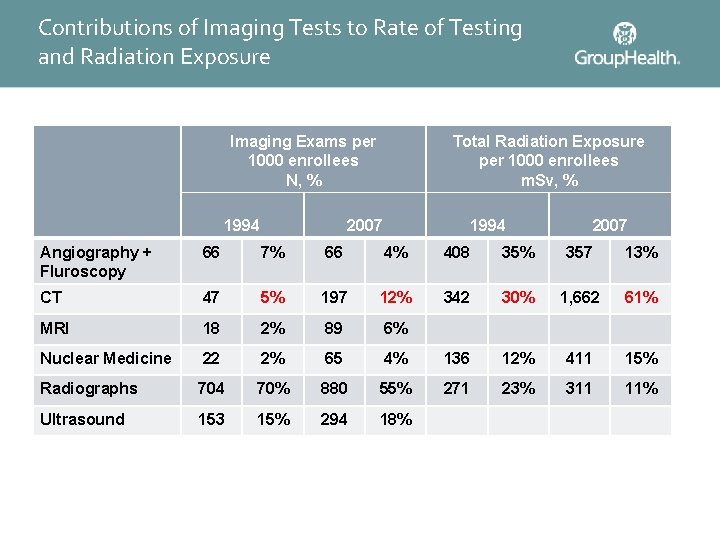
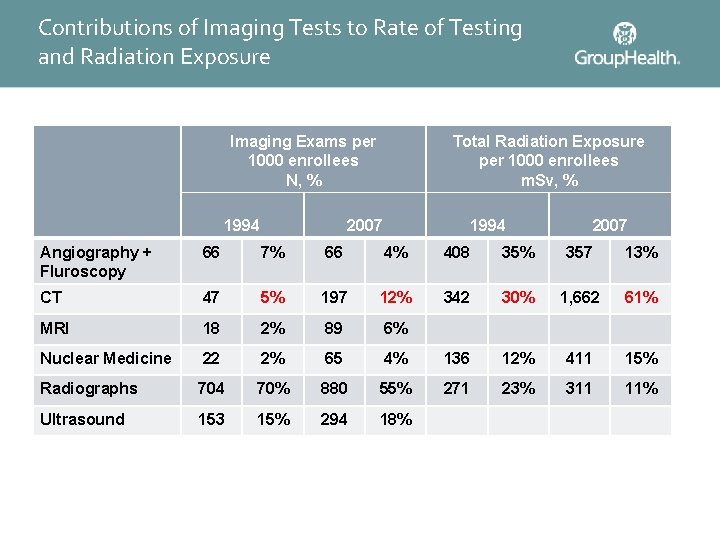
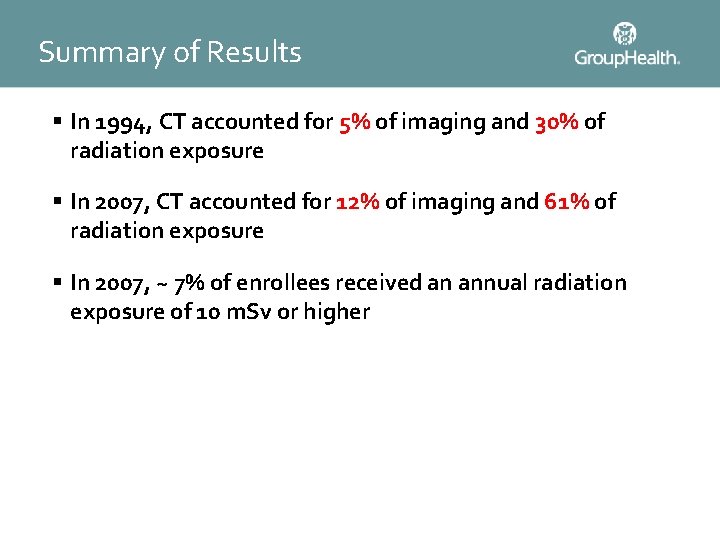
Contributions of Imaging Tests to Rate of Testing and Radiation Exposure Imaging Exams per 1000 enrollees N, % 1994 Total Radiation Exposure per 1000 enrollees m. Sv, % 2007 1994 2007 Angiography + Fluroscopy 66 7% 66 4% 408 35% 357 13% CT 47 5% 197 12% 342 30% 1, 662 61% MRI 18 2% 89 6% Nuclear Medicine 22 2% 65 4% 136 12% 411 15% Radiographs 704 70% 880 55% 271 23% 311 11% Ultrasound 153 15% 294 18%
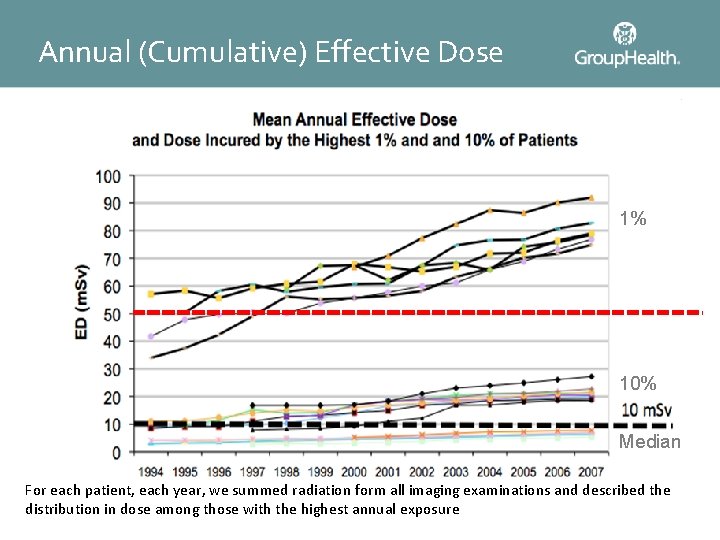
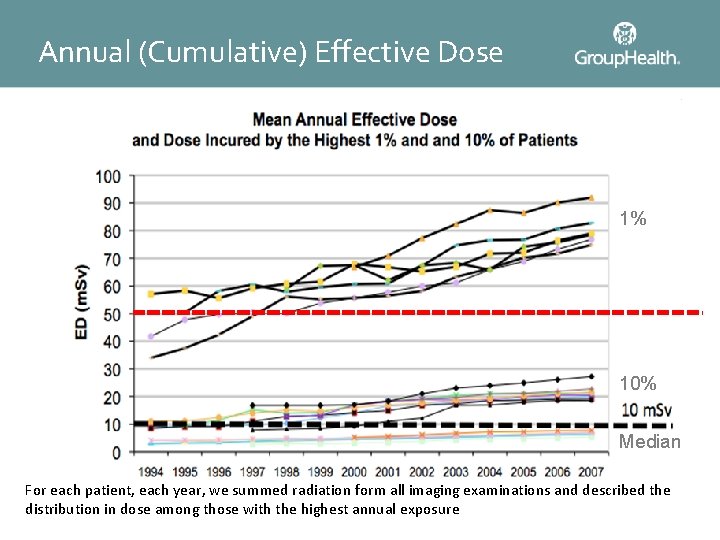
Annual (Cumulative) Effective Dose 1% Hiroshima Survivors 10% Median For each patient, each year, we summed radiation form all imaging examinations and described the distribution in dose among those with the highest annual exposure
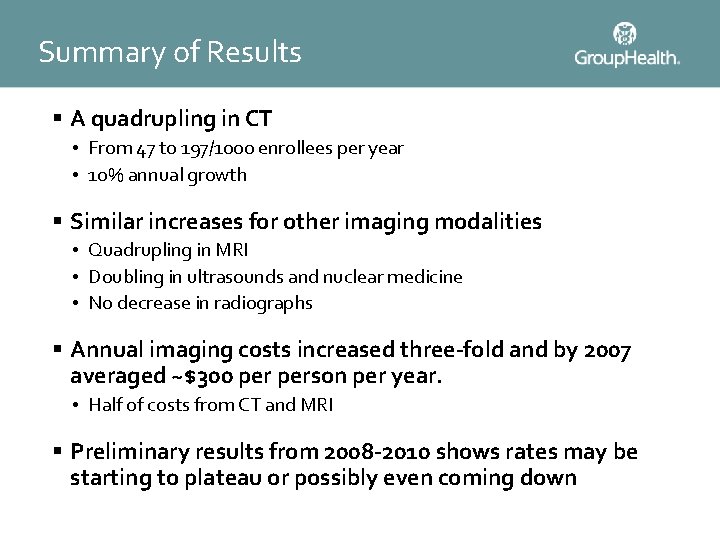
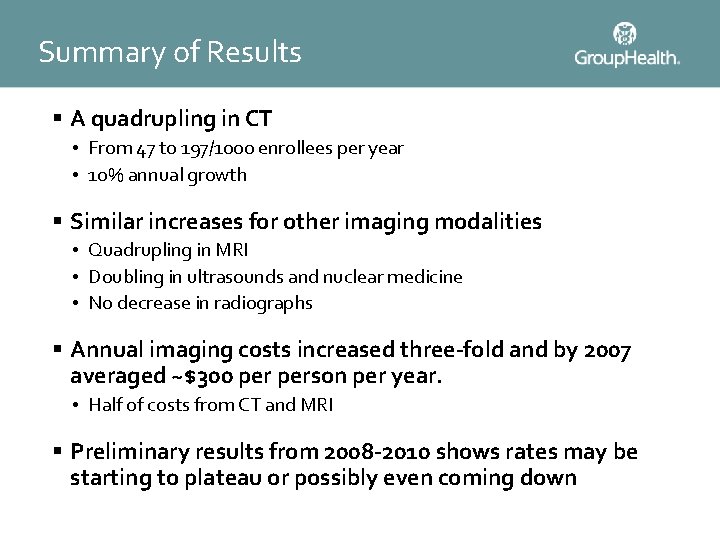
Summary of Results § A quadrupling in CT • From 47 to 197/1000 enrollees per year • 10% annual growth § Similar increases for other imaging modalities • Quadrupling in MRI • Doubling in ultrasounds and nuclear medicine • No decrease in radiographs § Annual imaging costs increased three-fold and by 2007 averaged ~$300 person per year. • Half of costs from CT and MRI § Preliminary results from 2008 -2010 shows rates may be starting to plateau or possibly even coming down
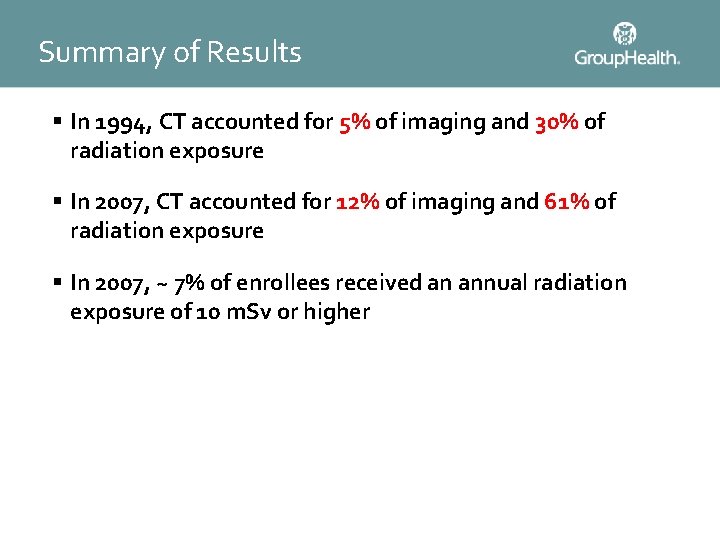
Summary of Results § In 1994, CT accounted for 5% of imaging and 30% of radiation exposure § In 2007, CT accounted for 12% of imaging and 61% of radiation exposure § In 2007, ~ 7% of enrollees received an annual radiation exposure of 10 m. Sv or higher

Pediatric Imaging
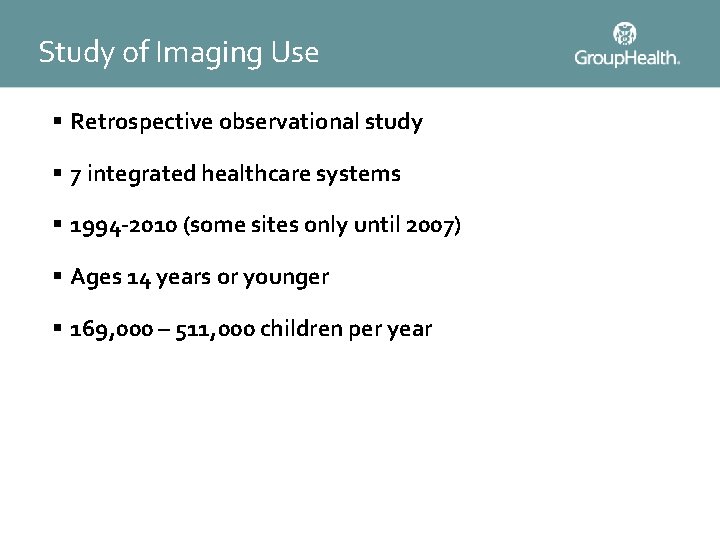
Study of Imaging Use § Retrospective observational study § 7 integrated healthcare systems § 1994 -2010 (some sites only until 2007) § Ages 14 years or younger § 169, 000 – 511, 000 children per year
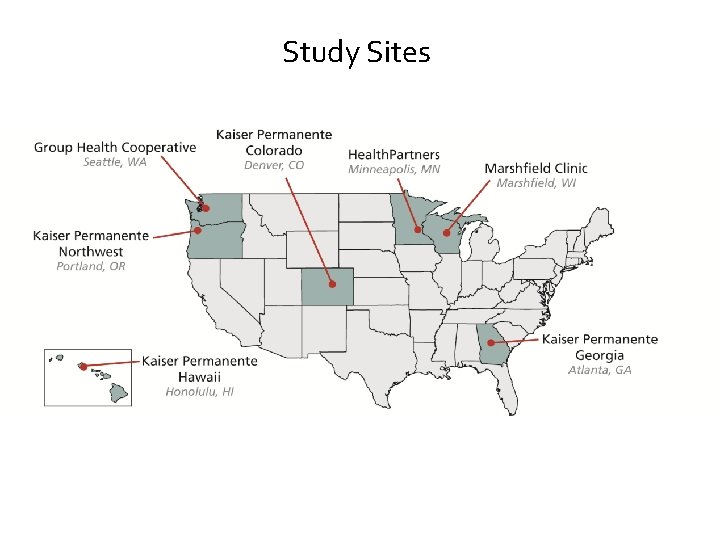
Study Sites
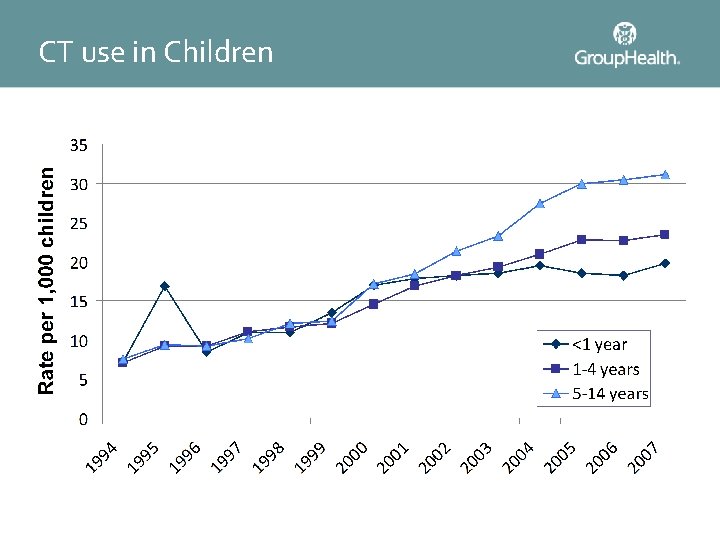
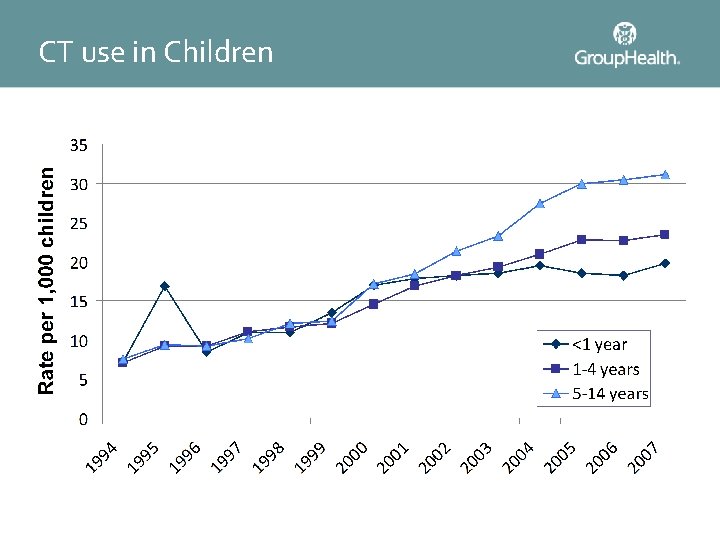
CT use in Children
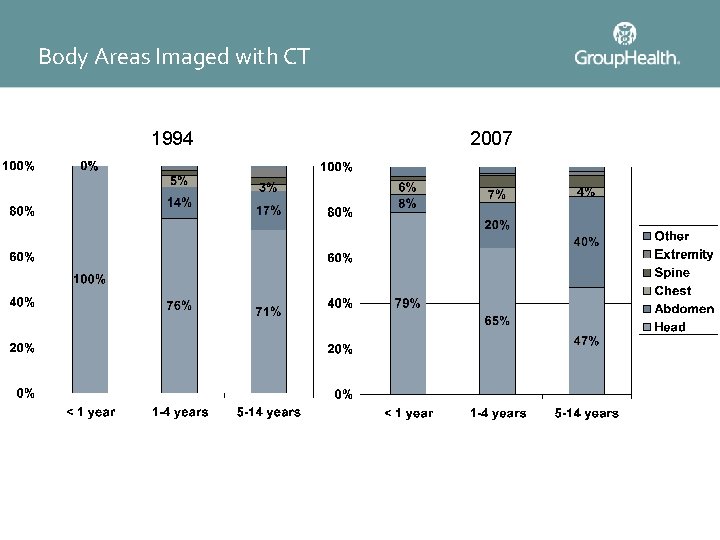
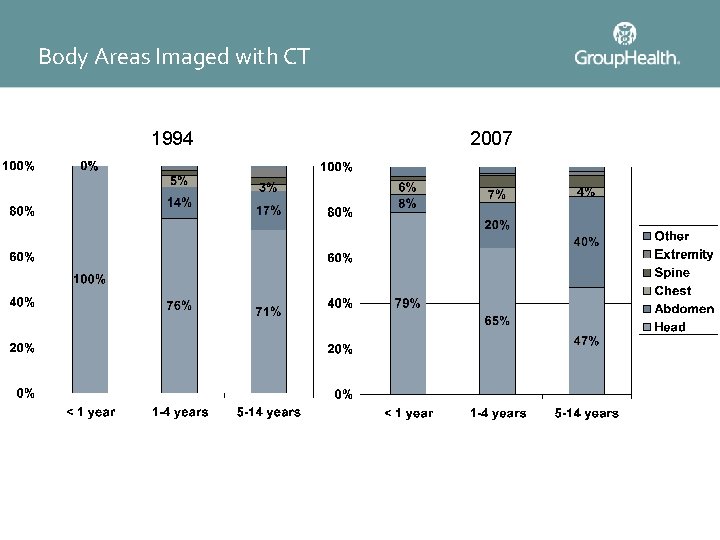
Body Areas Imaged with CT 1994 2007
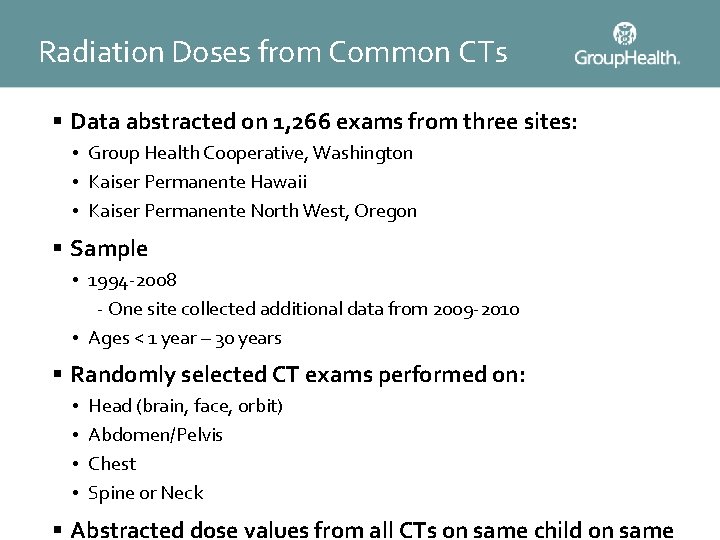
Radiation Doses from Common CTs § Data abstracted on 1, 266 exams from three sites: • Group Health Cooperative, Washington • Kaiser Permanente Hawaii • Kaiser Permanente North West, Oregon § Sample • 1994 -2008 - One site collected additional data from 2009 -2010 • Ages < 1 year – 30 years § Randomly selected CT exams performed on: • • Head (brain, face, orbit) Abdomen/Pelvis Chest Spine or Neck § Abstracted dose values from all CTs on same child on same
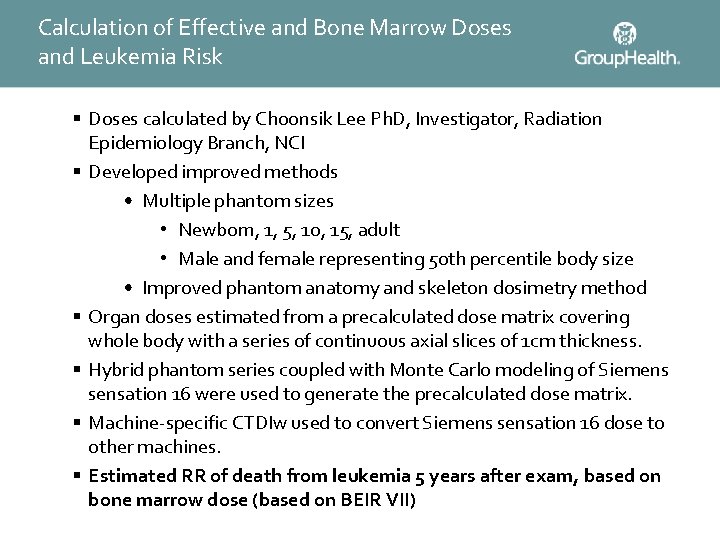
Calculation of Effective and Bone Marrow Doses and Leukemia Risk § Doses calculated by Choonsik Lee Ph. D, Investigator, Radiation Epidemiology Branch, NCI § Developed improved methods • Multiple phantom sizes • Newborn, 1, 5, 10, 15, adult • Male and female representing 50 th percentile body size • Improved phantom anatomy and skeleton dosimetry method § Organ doses estimated from a precalculated dose matrix covering whole body with a series of continuous axial slices of 1 cm thickness. § Hybrid phantom series coupled with Monte Carlo modeling of Siemens sensation 16 were used to generate the precalculated dose matrix. § Machine-specific CTDIw used to convert Siemens sensation 16 dose to other machines. § Estimated RR of death from leukemia 5 years after exam, based on bone marrow dose (based on BEIR VII)



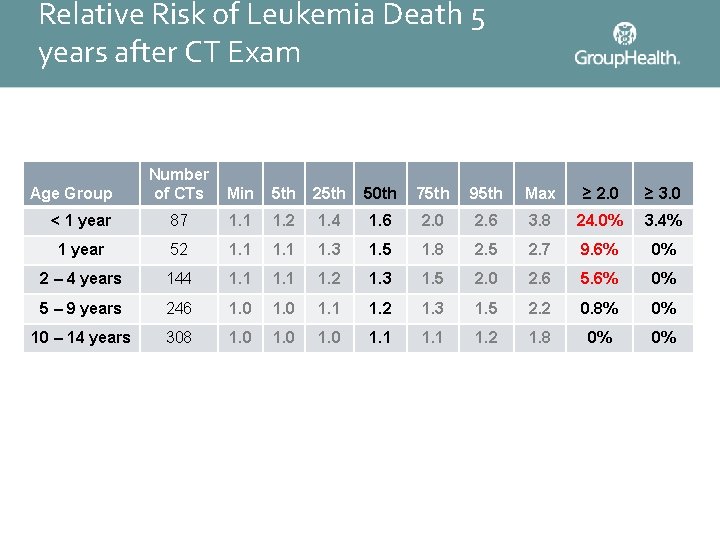
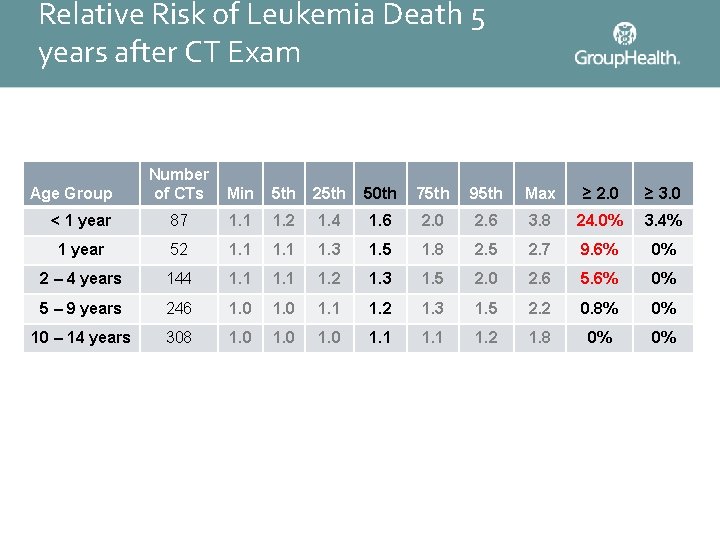
Relative Risk of Leukemia Death 5 years after CT Exam Number of CTs Min 5 th 25 th 50 th 75 th 95 th Max ≥ 2. 0 ≥ 3. 0 < 1 year 87 1. 1 1. 2 1. 4 1. 6 2. 0 2. 6 3. 8 24. 0% 3. 4% 1 year 52 1. 1 1. 3 1. 5 1. 8 2. 5 2. 7 9. 6% 0% 2 – 4 years 144 1. 1 1. 2 1. 3 1. 5 2. 0 2. 6 5. 6% 0% 5 – 9 years 246 1. 0 1. 1 1. 2 1. 3 1. 5 2. 2 0. 8% 0% 10 – 14 years 308 1. 0 1. 1 1. 2 1. 8 0% 0% Age Group
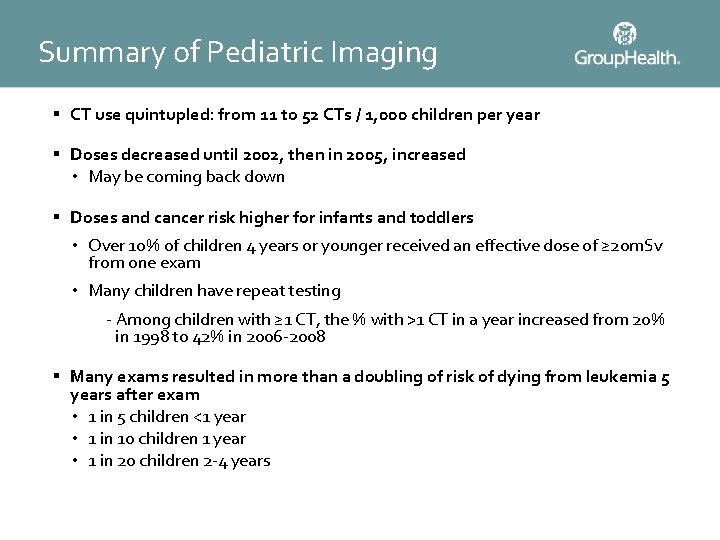
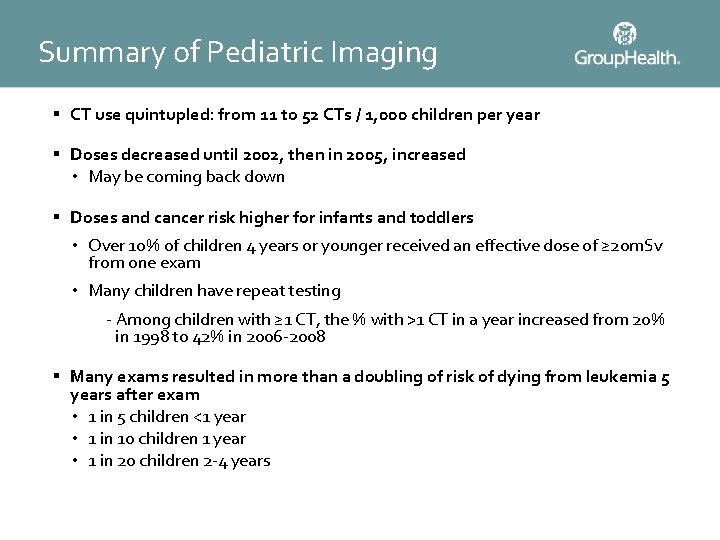
Summary of Pediatric Imaging § CT use quintupled: from 11 to 52 CTs / 1, 000 children per year § Doses decreased until 2002, then in 2005, increased • May be coming back down § Doses and cancer risk higher for infants and toddlers • Over 10% of children 4 years or younger received an effective dose of ≥ 20 m. Sv from one exam • Many children have repeat testing - Among children with ≥ 1 CT, the % with >1 CT in a year increased from 20% in 1998 to 42% in 2006 -2008 § Many exams resulted in more than a doubling of risk of dying from leukemia 5 years after exam • 1 in 5 children <1 year • 1 in 10 children 1 year • 1 in 20 children 2 -4 years

Discussion and Conclusions
Factors Contributing to Increased Advanced Medical Imaging Use § Improvements in technology § Increased capacity § Patient demand – no perceived disincentive § Physician demand • Easy • Lack of tolerance for ambiguity • Limited evidence-based guidelines (or any guidelines) § Malpractice concerns – leads to defensive imaging § High profitability – self-referral
How to Reduce Radiation Exposure § Reduce the number of studies: shared responsibility • Make sure test hasn’t already been done • Need evidence-based guidelines § Reduce doses per test: • Standard protocols • Dose reference levels § Educate physicians and technologists on importance of reducing dose § Educate patients and providers about risks & benefits of imaging § Directly assess the risks /benefits of CT to inform practice
Conclusions § Medical Imaging is an integral component of medical care § However, there are few evidenced based guidelines about when to image, and the default is to over-image § More widespread efforts needed to reduce dose, especially in children, by • Reducing unnecessary exams • Reducing dose when imaging necessary § Research is desperately needed to determine when to image, and how to do so using lowest possible doses

 Frc driver station mac
Frc driver station mac Managing economic exposure and translation exposure
Managing economic exposure and translation exposure Operating exposure vs transaction exposure
Operating exposure vs transaction exposure Transaction exposure and economic exposure
Transaction exposure and economic exposure Managing economic exposure and translation exposure
Managing economic exposure and translation exposure Is2000 the advanced imaging solution
Is2000 the advanced imaging solution Cscc medical imaging
Cscc medical imaging Spie
Spie Medical imaging terminology
Medical imaging terminology Fourier
Fourier Medical imaging software
Medical imaging software Medical imaging workstations
Medical imaging workstations Right arm medical term
Right arm medical term Access to medical and exposure records
Access to medical and exposure records Advanced use case diagram
Advanced use case diagram California medical license for foreign medical graduates
California medical license for foreign medical graduates Gbmc infoweb
Gbmc infoweb Hepburn osteometric board
Hepburn osteometric board Torrance memorial transitional care unit
Torrance memorial transitional care unit Cartersville medical center medical records
Cartersville medical center medical records Principles of individuality
Principles of individuality Increased tactile fremitus occurs with
Increased tactile fremitus occurs with Tactile.fremitus
Tactile.fremitus Causes of increased inr
Causes of increased inr Pas staining principle
Pas staining principle Static lung compliance formula
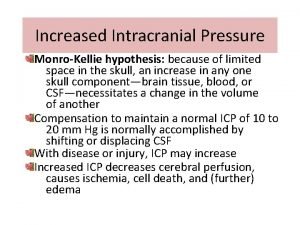
Static lung compliance formula How does meningitis cause increased intracranial pressure
How does meningitis cause increased intracranial pressure Air bronchogram
Air bronchogram Decorticate posturing
Decorticate posturing Increased tactile fremitus
Increased tactile fremitus Tactile fremitus
Tactile fremitus Tactile fremitus increased
Tactile fremitus increased Csf color
Csf color Does constriction increased blood flow
Does constriction increased blood flow Enzyme that conjugates bilirubin
Enzyme that conjugates bilirubin Tactile fremitus location
Tactile fremitus location Why does efferent arteriole constriction increased gfr
Why does efferent arteriole constriction increased gfr Capelaries
Capelaries Alp raised causes
Alp raised causes World history chapter 6 review
World history chapter 6 review The increased wind speed is indeed, accompanied by a
The increased wind speed is indeed, accompanied by a Hexagon shape is used for radio coverage for a cell because
Hexagon shape is used for radio coverage for a cell because Meaning and scope of international finance
Meaning and scope of international finance Signs and symptoms of increased icp
Signs and symptoms of increased icp Increased aerobic and anaerobic enzymes
Increased aerobic and anaerobic enzymes As the safety inventory is increased
As the safety inventory is increased Exploring synonym
Exploring synonym Increased intracranial pressure ati
Increased intracranial pressure ati Windows image acquisition driver
Windows image acquisition driver Quantum imaging with undetected photons
Quantum imaging with undetected photons Affordable hyperspectral imaging
Affordable hyperspectral imaging Live cell imaging applications
Live cell imaging applications Concave mirror ray diagram salt
Concave mirror ray diagram salt Focused imaging learning
Focused imaging learning Direct imaging subsystem
Direct imaging subsystem