Impact of Hospitalization Chapter 1 C Cummings RN


![Depression Watch out for: [1] early morning insomnia [2] excessive daytime sleeping [3] poor Depression Watch out for: [1] early morning insomnia [2] excessive daytime sleeping [3] poor](https://slidetodoc.com/presentation_image_h2/a9b5ecf18ca6366fc2966c08905a749a/image-49.jpg)
![Depression: Treatment [1] Drug therapy [2] Psychotherapy [3] Awareness of depression and eliminate possible Depression: Treatment [1] Drug therapy [2] Psychotherapy [3] Awareness of depression and eliminate possible](https://slidetodoc.com/presentation_image_h2/a9b5ecf18ca6366fc2966c08905a749a/image-50.jpg)
![Cultural Sensitivity/ Considerations [1] Food [2] Attitudes [3] Perceptions [4] TFC Channel Cultural Sensitivity/ Considerations [1] Food [2] Attitudes [3] Perceptions [4] TFC Channel](https://slidetodoc.com/presentation_image_h2/a9b5ecf18ca6366fc2966c08905a749a/image-52.jpg)
![Government and Community Resources Income [1] SSI/SSDI Health Insurance [1] Medicare [2] Medical/Medicaid Housing Government and Community Resources Income [1] SSI/SSDI Health Insurance [1] Medicare [2] Medical/Medicaid Housing](https://slidetodoc.com/presentation_image_h2/a9b5ecf18ca6366fc2966c08905a749a/image-54.jpg)



- Slides: 75
Impact of Hospitalization Chapter 1 C. Cummings, RN, Ed. D
What is Health? • How do you define health? • Health-illness continuum • Is it the ability of one to function in society? • Is it disease free? • Health: free from disease/illness. Different for everyone. • Needs to be their goal for health, not ours.
WHO’s definition of health • State of complete physical, mental and social well-being • Is this realistic? • Holistic health- body, mind and spirit as part of a person’s level of wellness • (not really realistic)
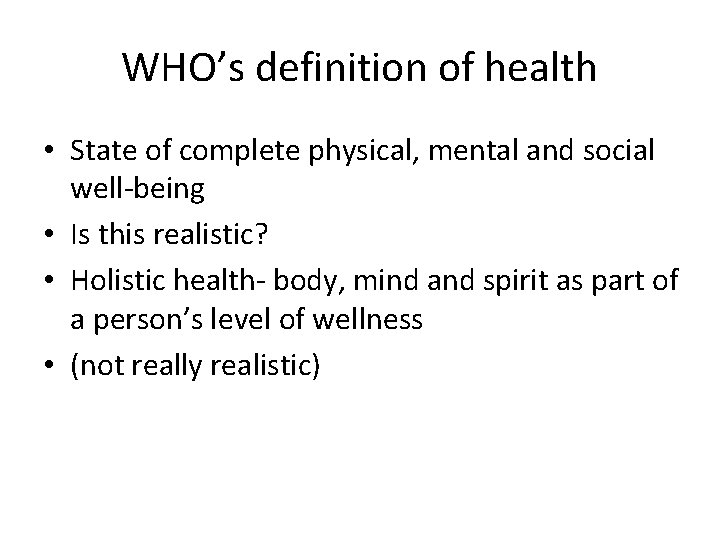
Body-Mind-Spirit connection
Quality of Life • Quality of Life, refers to 2 concepts: – Subjectivity: perceptions of satisfaction with their functional level – Multidimensionality: physical, functional, emotional and social well-being
Health Promotion and Protection • Health Promotion: What is this? • Healthy people 2010: U. S. DHHS – 2 National Goals: • Increase quality and years of healthy life • Eliminate health disparities among demographic groups • Pender (1987) describes health promotion as a positive activity that protects someone against illness • • DRG: diagnosis related group. If you are admitted to hospital… hospital can get a certain amt of money from Medicare for that diagnosis. Hospital has to get every thing that patient needs w/in that amount of money. Now, the patient will add more diagnosis so the patient is able to get more money. Pender (nurse) has written a lot on health promotion
Activities to Promote Health • Name some activities to promote health • Why are the effective and why might they not be? • (exercise, smoking, diet, seat belt, stress relief activities, lower cholesterol, diabetes prevention)
Healthy People 2010 • http: //www. healthypeople. gov/ • Look at leading health indicators. Gov says we have to go by these things! • Physical activity, overweight & obesity, tobacco use, substance abuse, resp sex behavior, mental health, injury & violence, environmental quality, immunization and access to health care.
Healthy People 2010 • What are the 6 target areas of health promotion? • Do you think there is a difference between racial and ethnic groups? • Yes, there is a difference w/ access to care, cultural differences w/ tobacco use or diet, communication issues …

Reasons for Differences • Poor Socioeconomic status • Health beliefs and behaviors • Access to health care • Environmental factors • Direct and indirect manifestations of discrimination • Lack of health insurance • Insufficient transportation • Geographic location • Cost of services • Language barriers • (transportation difficult here in Jax for elders)
Nursing’s Role • What can nurses do to decrease these differences? • What is transcultural nursing? – Area of study that focuses on the care, health and illness patterns as related to one’s cultural beliefs, values and practices • What is cultural competence? • Name some areas that may have differences for a hospitalized patient. • • Being familiar w/ other cultures & groups… being aware, not putting our own prejudices & bias on them. Getting patient to understand meds
Illness Prevention • People must be motivated to prevent an illness from occurring • What do you think motivates them? • What role can you as a nurse play? • The pt has to see it as a problem. Families may motivvate… hopefully as a nurse we motivate.

Three Types of Prevention • Primary Prevention: – Early, health maintenance activities • Secondary Prevention: – Early detection and treatment of a disease or condition (when the person has the disease) • Tertiary prevention: – Rehabilitation once the disease is stabilized – Return to their highest level of functioning
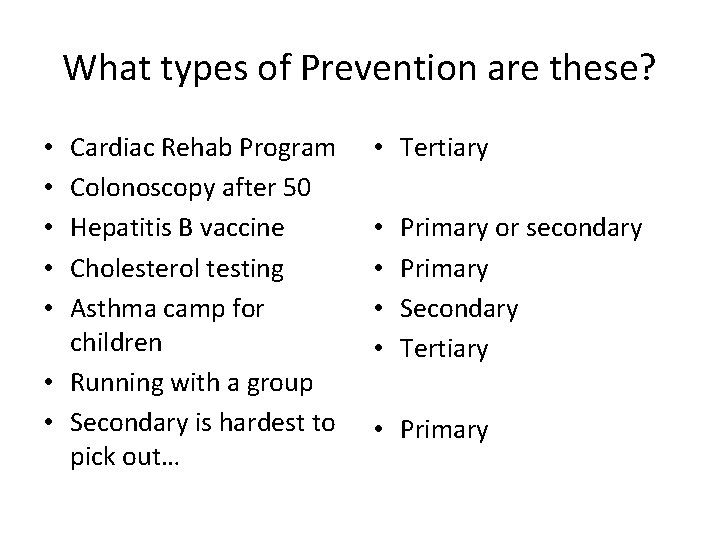
What types of Prevention are these? Cardiac Rehab Program Colonoscopy after 50 Hepatitis B vaccine Cholesterol testing Asthma camp for children • Running with a group • Secondary is hardest to pick out… • • • Tertiary • • Primary or secondary Primary Secondary Tertiary • Primary
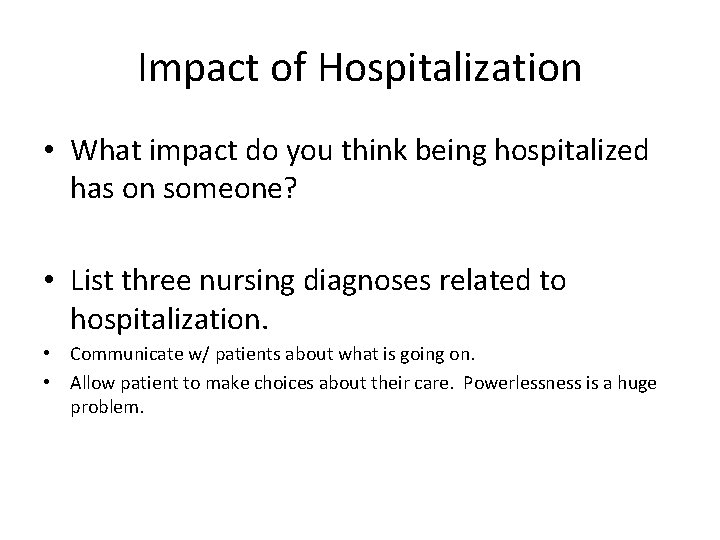
Impact of Hospitalization • What impact do you think being hospitalized has on someone? • List three nursing diagnoses related to hospitalization. • Communicate w/ patients about what is going on. • Allow patient to make choices about their care. Powerlessness is a huge problem.
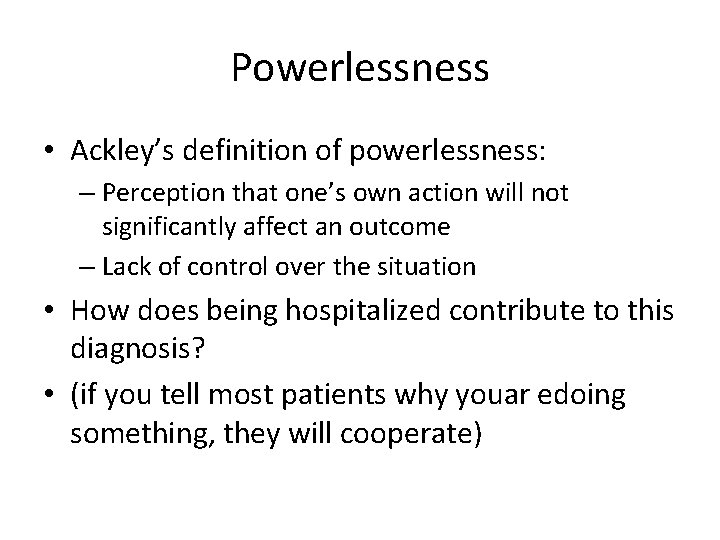
Powerlessness • Ackley’s definition of powerlessness: – Perception that one’s own action will not significantly affect an outcome – Lack of control over the situation • How does being hospitalized contribute to this diagnosis? • (if you tell most patients why youar edoing something, they will cooperate)
Powerlessness • List some patient behaviors that may demonstrate this diagnosis • May be angry… may take the anger out on the nurse… may withdraw or be depressed… • NOC outcomes may be the following: – Health beliefs: Perceived control – Health beliefs: Perceived ability to preform – Participation in health care decisions – Depression level: self-control
Nursing Interventions • List 5 things that nurses can do to help the patient experiencing powerlessness • How can you empower a patient?
Hopelessness • Subjective state in which the person sees limited or no alternatives and is unable to mobilize any energy to correct • What do you see as the difference between hopelessness and powerlessness? • What patient behaviors may be different? • Get a family member in w/ them… Difference: powerlessness; you feel like you can get the control back. Hopelessness: watch for depression & suicidal behavior
Hopelessness • List 4 nursing interventions that may be helpful. • What should the nurse be aware of, if the patient is exhibiting hopelessness? • Talk to them, keep them involved, talk about experiences… long term, be honest but tell that we will do everything we can
Role of the Nurse • What then is the role of the nurse in patient care? – Coordinator of Care – Caregiver – Continuing Care Planner: discharge – Educator – Advocate – Change Agent
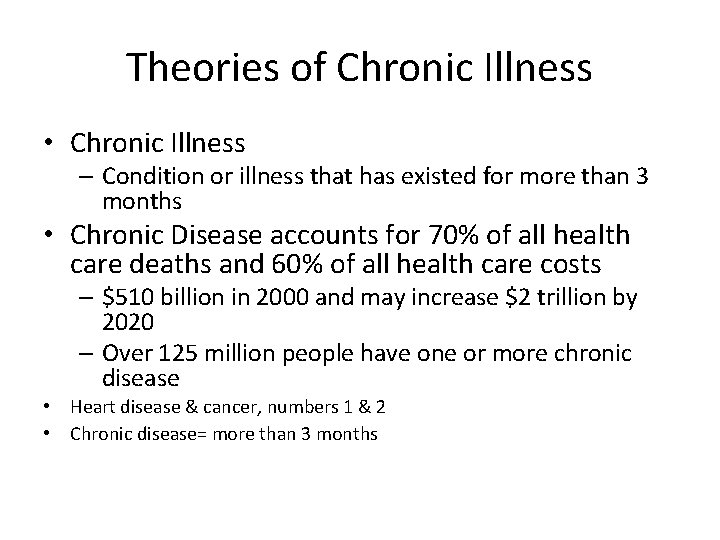
Theories of Chronic Illness • Chronic Illness – Condition or illness that has existed for more than 3 months • Chronic Disease accounts for 70% of all health care deaths and 60% of all health care costs – $510 billion in 2000 and may increase $2 trillion by 2020 – Over 125 million people have one or more chronic disease • Heart disease & cancer, numbers 1 & 2 • Chronic disease= more than 3 months
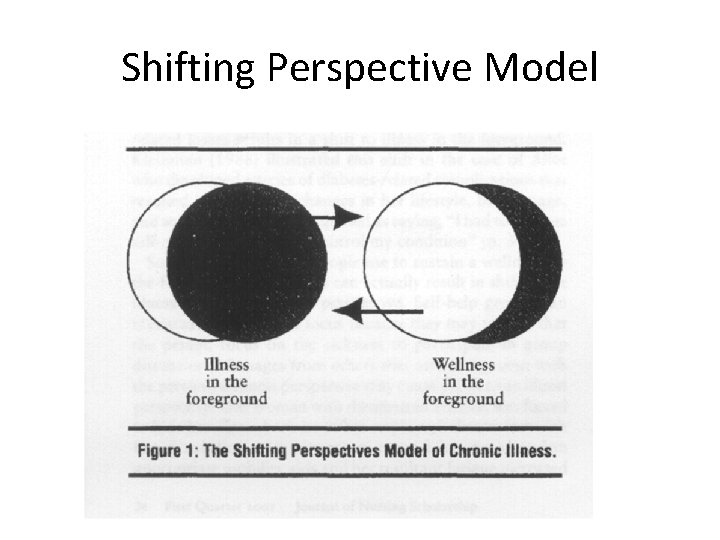
Shifting Perspective Model
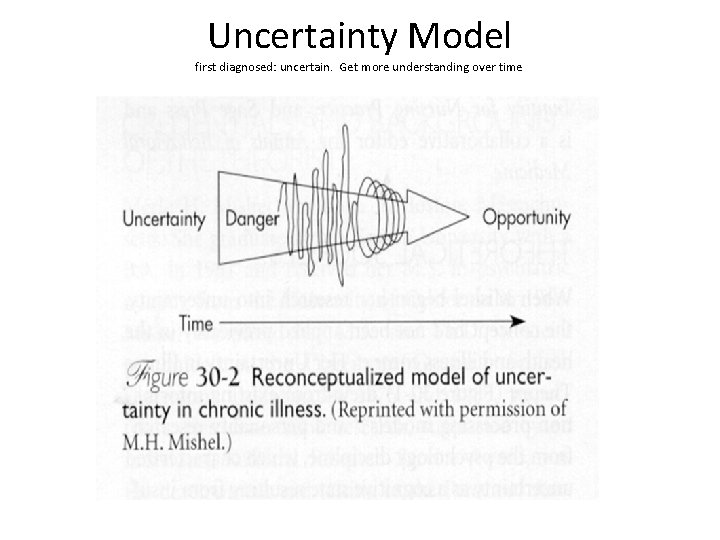
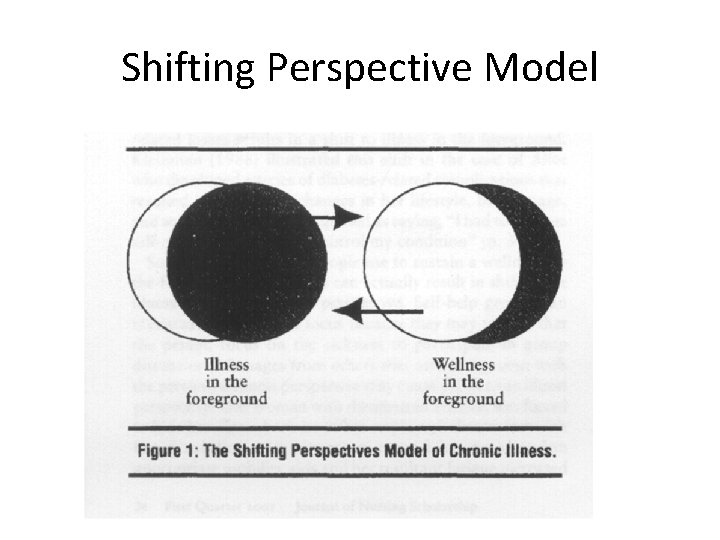
Uncertainty Model first diagnosed: uncertain. Get more understanding over time
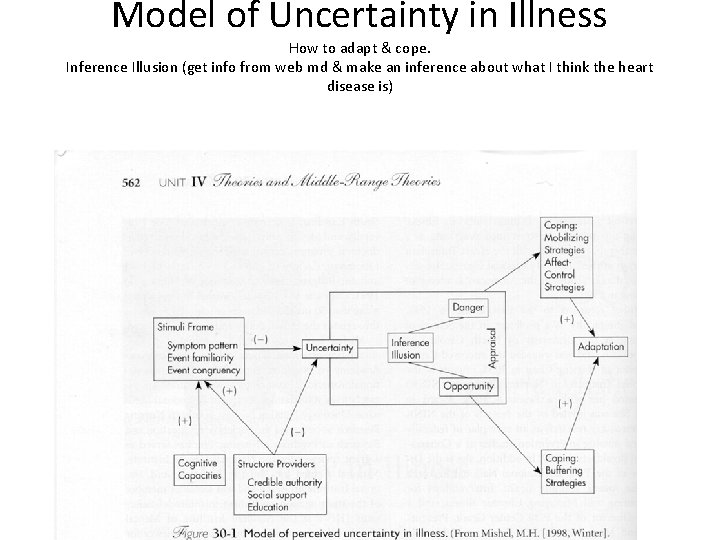
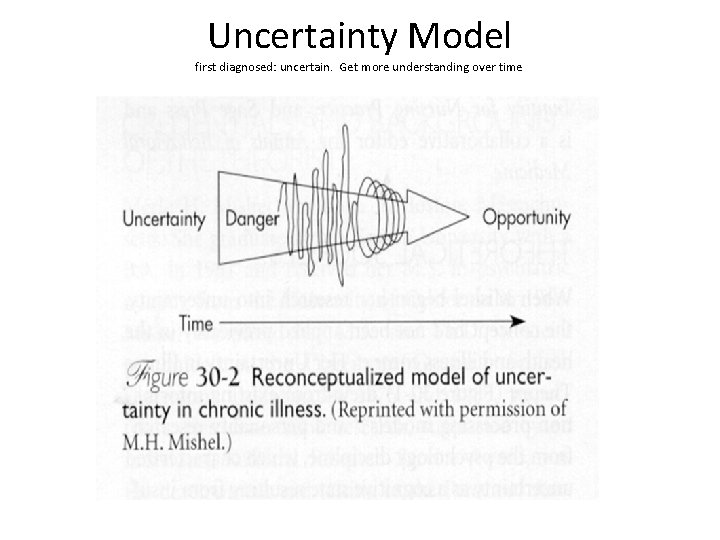
Model of Uncertainty in Illness How to adapt & cope. Inference Illusion (get info from web md & make an inference about what I think the heart disease is)
Chronic Illnesses • List the top 5 common chronic illnesses – 1. – 2. – 3. – 4. – 5. • What is the leading cause of death for those over 65?
Chronic Illnesses • http: //www. cdc. gov/nchs/FASTATS/default. htm • http: //www. ncsl. org/programs/health/phchronic. htm • CDC: leading cause of death: heart disease is number 1, cancer #2, stroke, chronic lower resp disease, accidents, diabetes, alzheimer’s disease, influenza & penumonia, renal syndromes, septicemia • Life expectancy: 77. 7 years • death rate 940 per 100, 000 • NCLS website: state information, website not up right now
Theories of Chronic Illness • Why are some patients more independent than others? – Some illnesses are less debilitating – Some are controlled by medications – Some have the resources to self-manage • Financial • Emotional
Theories of Chronic Illness • Shifting Perspectives – Shift between well and ill – Taking on the Sick Role – Finding meaning, hope and quality of life – Accepting or denying illness
Issues with the Chronically Ill • Education of RN’s about elderly and chronic illness – Only 12% of RN’s are from ethically diverse groups, while 33% of ill are from these groups • Financial issues – Medications, MD visits, home care and ADL’s • Cultural values – Not a priority for family support – Need more nurses from other cultures
Health Care Needs of the Aging Irma B. Ancheta, Ph. D, RN Peggy Mc. Cartt, RN, Ph. D (c), CCRN, ARNP
Learning Objectives • Identify the four subgroups of older adults • Discuss common health issues that may concern the older adult • Explain why older adults are at risk for falls • Discuss polypharmacy in the older adult • Discuss economic issues for older adults • Describe government and community resources for older adults
Four Subgroups of Older Adults • 65 -74 years of age: young old • 75 -84 years of age: middle old • 85 -99 years of age: old • 100 years of age or more: the elite old
Questions About These Groups • Which is the fastest growing of the four subgroups? • What percentage of older adults are living in the community either at home, in assistedliving, or in community retirement complexes? • Old old is the fastest growing • Almost 80% are living in the community. • Page 15 in the book
Health Issues for Older Adults Health Promotion Self-management Nutritional Awareness Physical Fitness and Mobility Stress Management Accidents Drug Use and Misuse Mental Health/Behavioral Health Problems • Elder Neglect and Abuse • (isolation, accidents, falls, leaving stove on, etc…) • •
Relocation Stress Syndrome • “physiological and /or psychological distress following transfer from one environment to another. ” (NANDA, 2003) (transferring from one environment to another is very stressful for elderly… confusing)
Health Promotion Negative Risk Factors for Healthy Aging • • • Alcohol Abuse Smoking Depression Lack of Exercise Obesity
Health Promotion Yearly Influenza Vaccinations Pneumococcal Vaccination Tetanus Immunization Create Hazard Free Environment Wear Seat Belts Install Smoke Detectors Be Cautious About Medication Use • Take One Aspirin a Day • Moderate Alcohol Intake • No Smoking • •
Self-management Find Opportunities to be productive Maintain as much control as possible over their lives Participate in decision making Perform as many tasks as possible (avoid being an enabler)
Nutritional Awareness • Increase Intake of Fiber and Complex Carbohydrates (add Benefiber in coffee) • Decrease Intake of Dietary Fat • Increase Calcium Intake (also need sunlight exposure)
Nutritional Awareness Causes of poor nutrition (not eating/ eating less or overeating) in the elderly: [1] Loneliness (PF) [2] Depression (SB) [3] Boredom ………………. . lose the will to live……
Physical Fitness and Mobility Exercise Regularly (three to five times a week for 30 minutes per session) Some Weight Bearing Exercises (increase strength) Improve regularity of bowel movement
Physical Fitness and Mobility • Use of walker, cane, wheelchair, motorized scooter • Health and beauty trips
Stress Management • Older Adults Cope with Stress as they Did when they were Younger • Awareness of Physical and Economic Constraints • (get stressed that they can’t do what they used to be able to do…. Frustration)
Accidents • Most Accidents are at Home FALLS
Drug Use and Misuse • POLYPHARMACY • (occurs often due to elderly pt receiving a lot of different meds from different pharmacies)
Drug Use and Misuse Older people have less muscle mass…. . ……. inclined to get easily toxic to drugs… ……. beware of how drugs affect the elderly Has more to do with liver involvement, bioavailability. Liver just not as effective. Can also be a renal problem w/ excretion. Statins are really rough on the liver (cholesterol lowering drugs). Tylenol is also rough on the liver.
Mental Health/Behavioral Health Problems • Legally Competent • Clinically Competent • Depression (…the need to be intellectually stimulated) • Dementia/Delirium
![Depression Watch out for 1 early morning insomnia 2 excessive daytime sleeping 3 poor Depression Watch out for: [1] early morning insomnia [2] excessive daytime sleeping [3] poor](https://slidetodoc.com/presentation_image_h2/a9b5ecf18ca6366fc2966c08905a749a/image-49.jpg)
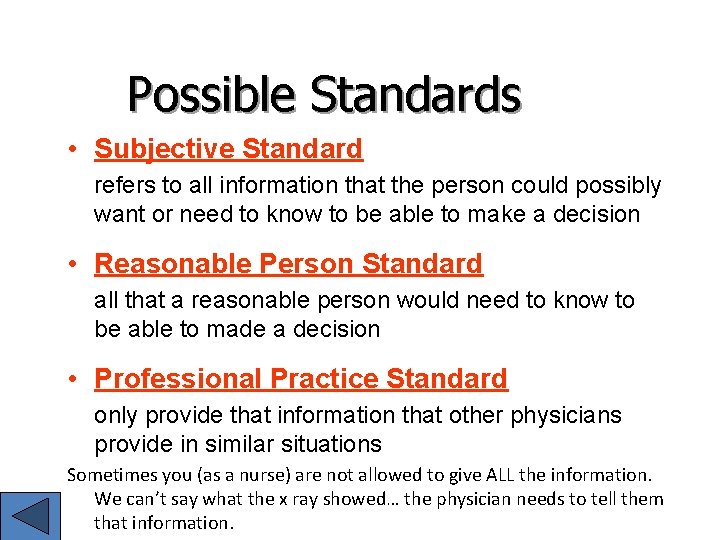
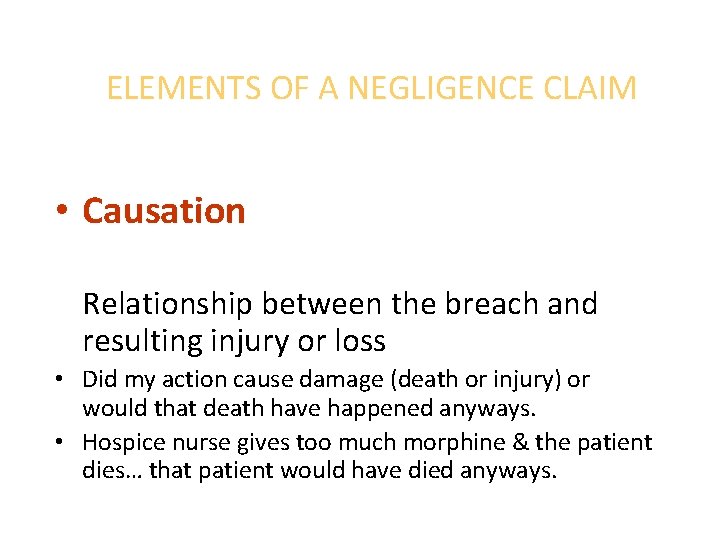
Depression Watch out for: [1] early morning insomnia [2] excessive daytime sleeping [3] poor appetite [4] unwillingness to participate in social and recreational activities Wake up at 3 am, don’t sleep well, sleep throughout the day but not good at night. Depression very common in the elderly.
![Depression Treatment 1 Drug therapy 2 Psychotherapy 3 Awareness of depression and eliminate possible Depression: Treatment [1] Drug therapy [2] Psychotherapy [3] Awareness of depression and eliminate possible](https://slidetodoc.com/presentation_image_h2/a9b5ecf18ca6366fc2966c08905a749a/image-50.jpg)
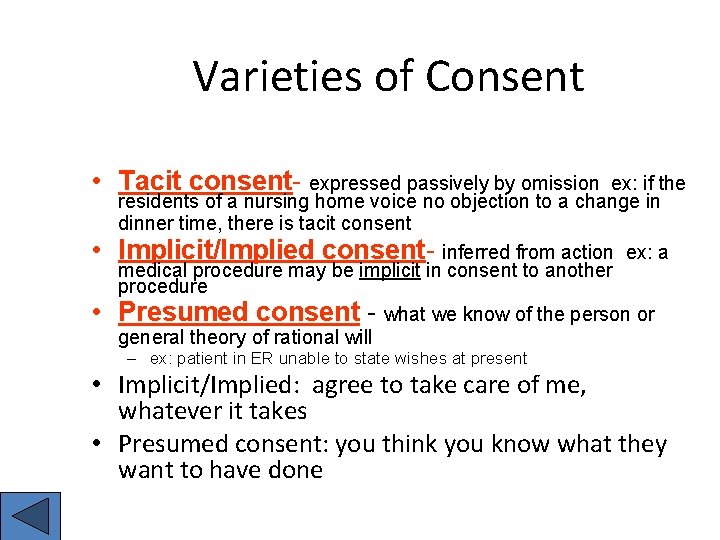
Depression: Treatment [1] Drug therapy [2] Psychotherapy [3] Awareness of depression and eliminate possible causes.
Dementia (OBS) vs. Delirium Chronic Progressive Example: Alzheimer’s disease • Organic brain syndrome = dementia • Delirium = acute & reversible • Pain meds can also cause delirium as well as sleep aids like restoril or ambien. UTIs or sepsis also cause confusion. • Acute • Reversible 2 types: [1] Hyperactive [2] Hypoactive
![Cultural Sensitivity Considerations 1 Food 2 Attitudes 3 Perceptions 4 TFC Channel Cultural Sensitivity/ Considerations [1] Food [2] Attitudes [3] Perceptions [4] TFC Channel](https://slidetodoc.com/presentation_image_h2/a9b5ecf18ca6366fc2966c08905a749a/image-52.jpg)
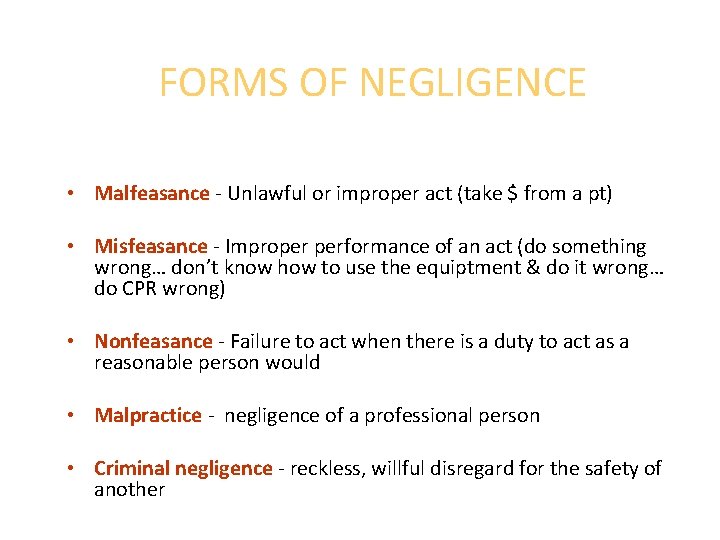
Cultural Sensitivity/ Considerations [1] Food [2] Attitudes [3] Perceptions [4] TFC Channel
Elder Neglect and Abuse • Neglect (failure to provide basic needs) • Physical Abuse (burns) • Financial Abuse (mismanaged property) • Emotional Abuse • (threats, humiliation)
![Government and Community Resources Income 1 SSISSDI Health Insurance 1 Medicare 2 MedicalMedicaid Housing Government and Community Resources Income [1] SSI/SSDI Health Insurance [1] Medicare [2] Medical/Medicaid Housing](https://slidetodoc.com/presentation_image_h2/a9b5ecf18ca6366fc2966c08905a749a/image-54.jpg)
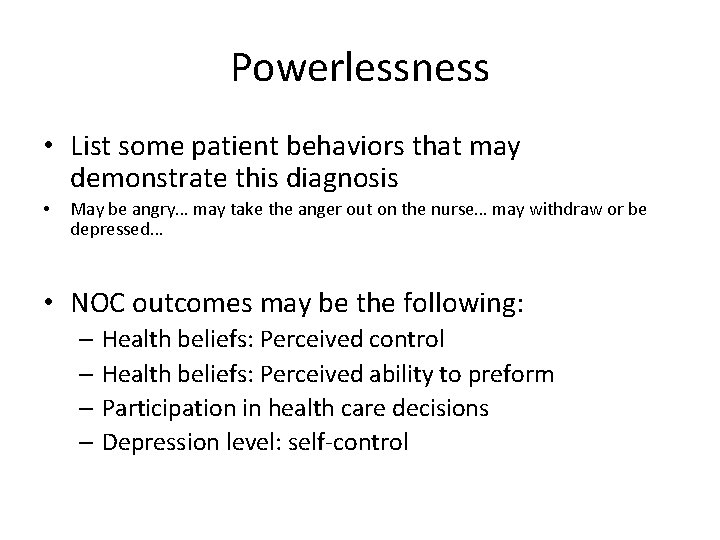
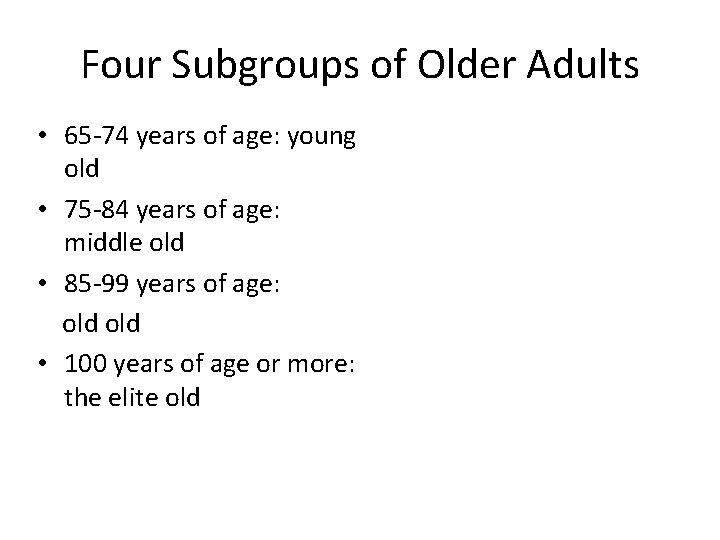
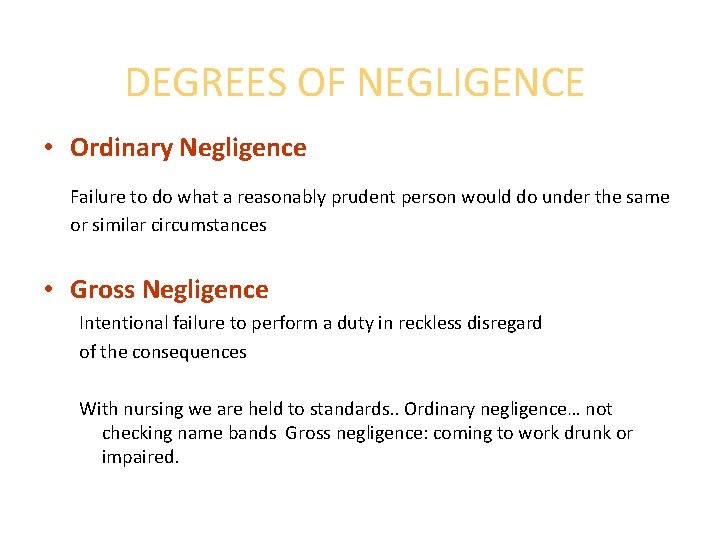
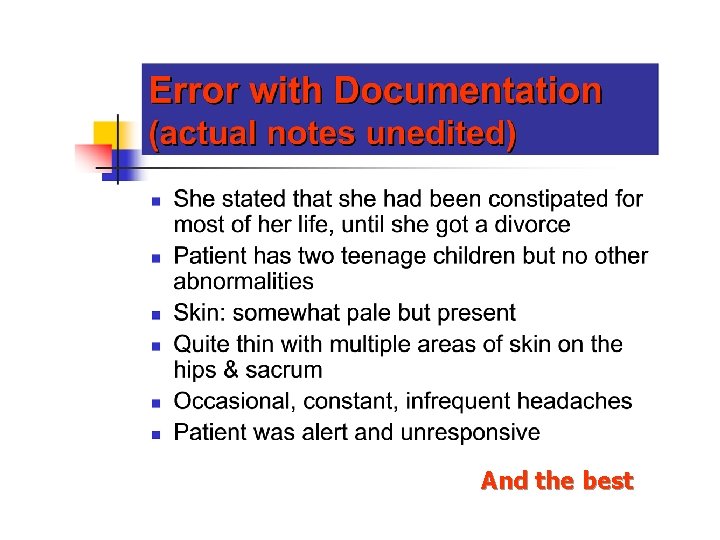
Government and Community Resources Income [1] SSI/SSDI Health Insurance [1] Medicare [2] Medical/Medicaid Housing Programs Social Services Research Agencies Churches Meals on Wheels • Medicaid is state funded • Medicare is federally funded
The Future of Gerontology Nursing • Nurses will practice taking care of older adults in acute care, long term care and community-based settings • Gerontological Certification • Gerontology ARNP
Legal & Ethical Issues in Adult Health Nursing M. Catherine Hough, Ph. D, RN, Associate Professor University of North Florida School of Nursing
Define AUTONOMY?
INFORMED CONSENT • Need informed consent for anything invasive. • Nurses don’t sign this… the physician signs the form. In last 10 years, the physician has to sign the form. • We can witness that the patient is the one that signed, but we give information about the procedure. • Only time you can bypass a blood consent is an emergency. Otherwise you have to give consent. • Basic nursing procedures don’t need informend consent.
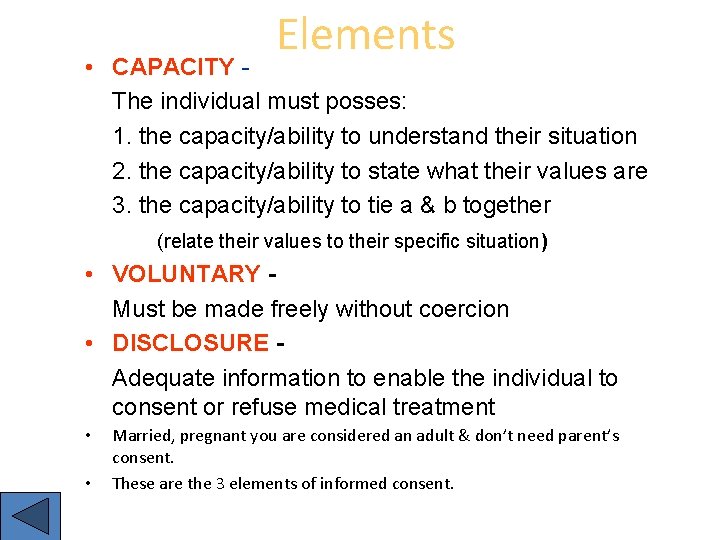
Elements • CAPACITY The individual must posses: 1. the capacity/ability to understand their situation 2. the capacity/ability to state what their values are 3. the capacity/ability to tie a & b together (relate their values to their specific situation) • VOLUNTARY Must be made freely without coercion • DISCLOSURE Adequate information to enable the individual to consent or refuse medical treatment • • Married, pregnant you are considered an adult & don’t need parent’s consent. These are the 3 elements of informed consent.
Possible Standards • Subjective Standard refers to all information that the person could possibly want or need to know to be able to make a decision • Reasonable Person Standard all that a reasonable person would need to know to be able to made a decision • Professional Practice Standard only provide that information that other physicians provide in similar situations Sometimes you (as a nurse) are not allowed to give ALL the information. We can’t say what the x ray showed… the physician needs to tell them that information.
Varieties of Consent • Tacit consent- expressed passively by omission • • ex: if the residents of a nursing home voice no objection to a change in dinner time, there is tacit consent Implicit/Implied consent- inferred from action ex: a medical procedure may be implicit in consent to another procedure Presumed consent - what we know of the person or general theory of rational will – ex: patient in ER unable to state wishes at present • Implicit/Implied: agree to take care of me, whatever it takes • Presumed consent: you think you know what they want to have done
FORMS OF NEGLIGENCE • Malfeasance - Unlawful or improper act (take $ from a pt) • Misfeasance - Improper performance of an act (do something wrong… don’t know how to use the equiptment & do it wrong… do CPR wrong) • Nonfeasance - Failure to act when there is a duty to act as a reasonable person would • Malpractice - negligence of a professional person • Criminal negligence - reckless, willful disregard for the safety of another
DEGREES OF NEGLIGENCE • Ordinary Negligence Failure to do what a reasonably prudent person would do under the same or similar circumstances • Gross Negligence Intentional failure to perform a duty in reckless disregard of the consequences With nursing we are held to standards. . Ordinary negligence… not checking name bands Gross negligence: coming to work drunk or impaired.
Tort Liability for Medical Malpractice TWO PURPOSES: (why people sue) • Compensation • Deterrence
ELEMENTS OF A NEGLIGENCE CLAIM • Duty Existence of a legal obligation to provide care • 4 major elements: • Duty to the patient. I am the person taking care of the person. If a nurse makes a mistake, the doctor is held responsible for that mistake because she is working under the doctor. They can sue the nurse & the charge nurse.
ELEMENTS OF A NEGLIGENCE CLAIM • Breach of duty: as a new nurse, if I can’t handle what is going on, I need to tell the person in charge. Talk to the hospital where you are. • Breach Failure to do what a reasonable professional would do under similar circumstances
ELEMENTS OF A NEGLIGENCE CLAIM • Damages Physical, economic or psychological injury What I did to the patient… did it cause damages. Fall asleep while on duty but there was no injury, can’t really sue for malpractice.
ELEMENTS OF A NEGLIGENCE CLAIM • Causation Relationship between the breach and resulting injury or loss • Did my action cause damage (death or injury) or would that death have happened anyways. • Hospice nurse gives too much morphine & the patient dies… that patient would have died anyways.
ELEMENTS OF A NEGLIGENCE CLAIM • DUTY • BREACH • DAMAGES • CAUSATION

Nursing Documentation
Nursing DOCUMENTATION Part of a legal record Must be factual and objective No spelling errors Must be neat Must correct errors in documentation according to institution policies • NEVER USE WHITE OUT!!!!! • (must be factual… nothing subjective) • • •


And the best
“Large brown stool ambulating in the hall”
 Impact of hospitalisation on child and family
Impact of hospitalisation on child and family Sick child definition
Sick child definition Renal tubule
Renal tubule Somewhere i have never travelled gladly beyond meaning
Somewhere i have never travelled gladly beyond meaning Cummings and worley change model
Cummings and worley change model Ee cummings love is more thicker
Ee cummings love is more thicker Alma cummings dance marathon
Alma cummings dance marathon Ivor cummings
Ivor cummings History of the pinball machine
History of the pinball machine Quick server online
Quick server online Buffalo bill ee cummings
Buffalo bill ee cummings Ashlee_cummings_
Ashlee_cummings_ Clint cummings
Clint cummings Cummings
Cummings Pearson education inc publishing as benjamin cummings
Pearson education inc publishing as benjamin cummings Cummings
Cummings Benjamin cummings
Benjamin cummings Metabolic action of growth hormone
Metabolic action of growth hormone Cummings
Cummings Benjamin cummings
Benjamin cummings Cummings
Cummings Benjamin cummings
Benjamin cummings 1950
1950 Holly cummings
Holly cummings My mane bio
My mane bio Brain stem
Brain stem 2008
2008 Pearson benjamin cummings
Pearson benjamin cummings Ozone layer depletion
Ozone layer depletion Benjamin cummings
Benjamin cummings Cummings et al
Cummings et al The water of ayole
The water of ayole Pearson education 2004
Pearson education 2004 The furthest distance ive travelled poem
The furthest distance ive travelled poem Function of the cell wall
Function of the cell wall Matter anything that
Matter anything that Maddie cummings
Maddie cummings Sttranslate
Sttranslate Chapter 27 human impact on earth resources
Chapter 27 human impact on earth resources Chapter 16 the impact of technology
Chapter 16 the impact of technology Chapter 16 human impact on ecosystems
Chapter 16 human impact on ecosystems Chapter 7 lesson 4 the war's impact
Chapter 7 lesson 4 the war's impact Chapter 16 human impact on ecosystems
Chapter 16 human impact on ecosystems Chapter 21 lesson 3 the impact of alcohol abuse
Chapter 21 lesson 3 the impact of alcohol abuse Impact of wwi
Impact of wwi Nunavut impact review board
Nunavut impact review board Cross impact matrix
Cross impact matrix Trans pecos weathering erosion and deposition
Trans pecos weathering erosion and deposition Pollution effects on ecosystems
Pollution effects on ecosystems What was the impact of the beer hall putsch?
What was the impact of the beer hall putsch? Impact cad software
Impact cad software Types of publications
Types of publications Tone and figurative language
Tone and figurative language Who was the defendant in tinker v des moines
Who was the defendant in tinker v des moines Societal impact of pain
Societal impact of pain Positive impacts of ict
Positive impacts of ict Social impact of ict
Social impact of ict Benito mussolini impact
Benito mussolini impact Social media good and bad effects
Social media good and bad effects The impact of a godly woman
The impact of a godly woman How did the gaa impact irish life
How did the gaa impact irish life Impact of hr practices on employee performance
Impact of hr practices on employee performance Impact of computers in today's society
Impact of computers in today's society How did the great depression impact the world
How did the great depression impact the world Human movement science impact factor
Human movement science impact factor Sustainable engineering ktu syllabus
Sustainable engineering ktu syllabus Stem impact toolkit
Stem impact toolkit Highest impact factor journal
Highest impact factor journal Hydrobiologia editorial manager
Hydrobiologia editorial manager Chaparral biome distribution
Chaparral biome distribution Characteristics of renaissance
Characteristics of renaissance Mst physics 1135
Mst physics 1135 Ijmpa impact factor
Ijmpa impact factor Cross impact matrix
Cross impact matrix Ibm enterprise data management
Ibm enterprise data management Projected bloodstain pattern
Projected bloodstain pattern