Hypoxia types effects Cyanosis Hypercapnia Dyspnea Asphyxia Dr
- Slides: 32
Hypoxia: types & effects, Cyanosis, Hypercapnia, Dyspnea, Asphyxia Dr. Samina Malik
TYPES OF HYPOXIA: There are 4 types of hypoxia: 1. Hypoxic Hypoxia 2. Anemic Hypoxia 3. Stagnant / Ischemic Hypoxia 4. Histotoxic Hypoxia
HYPOXIC HYPOXIA: • Decreased arterial partial pressure of oxygen. • In other types of hypoxia, PO 2 is normal. CAUSES: • High altitude decreased PO 2 in atmospheric air. • Depression of Respiratory centre (disease / drug).
HYPOXIC HYPOXIA: (continued) CAUSES: • Respiratory muscle paralysis. • Obstructive lung disease (COPD). • Restrictive lung disease (pulmonary fibrosis, pneumothorax). • Congenital heart diseases.
Clinical features of Hypoxic Hypoxia: • Due to decrease arterial PO 2 Interstitial cells in peritubular capillaries secrete Erythropoietin polycythemia • Hypoxia pulm. V. C Pulm. Hypertension Rt. Vent. Hypertrophy Rt. Vent. Failure. TREATMENT: O 2 treatment is most effective in this type of hypoxia.
ANEMIC HYPOXIA: • Arterial PO 2 is normal but inadequate O 2 carrying capacity of blood because of decrease in Hb conc. or due to presence of abnormal Hb like met-Hb or Hb-S or if binding site of Hb for oxygen is not available such as in carbon monoxide poisoning.
• CO is produced due to incomplete combustion of carbon. • Hb has 250 times more affinity to bind with CO as compared to O 2. • Carbon monoxide Hb shifts the oxy-Hb curve to left O 2 dissociation becomes difficult. • CO also inhibits cytochromes. • When there is 70% carbon monoxy Hb in blood death occurs. • CO is colorless & odourless. • In CO poisoning, skin is cherry red colored. • There is no stim. of resp. centre, because arterial PO 2 is normal.
Treatment: • Remove the subject from source of exposure. • 100% oxygen therapy can help. • Hyper-barric O 2 can help (O 2 with increased pressure = 2 -3 atmospheric pressure)
STAGNANT / ISCHEMIC HYPOXIA: CAUSES: • Decreased cardiac output / sluggish blood flow due heart failure, hemorrhage, circulatory shock and venous obstruction. • Blood remains in tissues for longer time, so tissue extracts increased oxygen from blood more arteriovenous difference of oxygen concentration. • So PCO 2 increases, it facilitates unloading of oxygen from hemoglobin (shifts the oxy-hemoglobin association dissociation curve to right).
HISTOTOXIC HYPOXIA: (poverty amongst plenty) DEFINITION: Inability of the tissues to utilize oxygen inspite of normal arterial PO 2 and oxygen carrying capacity. CAUSES: • Cyanide poisoning (it inhibits cytochrome oxidases oxidative process is inhibited). • Narcotic overdosage (it inactivates the enzyme dehydrogenase inhibition of tissue oxygenation). • Beri-beri (it is deficiency of thymine co-enzyme which is required for many oxidative reactions). TREATMENT: • Methylene blue or nitrites. These convert hemoglobin methemoglobin. • Cyanide + met-hemoglobin cyn-met-hemoglobin (non-toxic compound).
CYANOSIS: • Definition: Bluish discoloration of skin & mucus membrane, when conc. of deoxy-Hb in small blood vessels like capillaries is more than 5 g / dl.
Types of Cyanosis: • Peripheral: • Seen on exposure to moderate cold & in case of stagnant hypoxia. • Seen in fingers, outer surface of lips. • Arterial PO 2 remains normal. • Central: • Seen in case of Congenital heart diseases & chronic lung disease. • Mostly Arterial PO 2 is below normal (due to hypoxic hypoxia).
Conditions in which Cyanosis does not occur: • Severe anemia (less than 5 g Hb / dl) • CO poisoning (masked due to cherry red complexion) • Met-Hemoglobinemia (chocolate brown discoloration)
DYSPNEA = Air Hunger: DEFINITION: • Mental anguish associated with inability to ventilate enough to satisfy the demand for air.
3 factors that develop the sensation of dyspnea: 1) Abnormality of respiratory gases in body fluids (mainly hypercapnia & partly hypoxia) 2) Work of ventilation by respiratory muscles 3) State of Mind (neurogenic / emotional dyspnea)
Abnormality of respiratory gases • A person may become very dyspneic due to excess rise of CO 2 in body fluids.
Work of ventilation • Sometimes the levels of CO 2 & O 2 are normal but to achieve this normality of respiratory gases, a person has to breathe forcefully feeling of dyspnea.
Neurogenic / Emotional dyspnea • Respiratory functions may be normal but still dyspnea may be experienced due to abnormal state of mind. • More enhanced in people who are claustrophobic (fear of not being able to receive a sufficient quantity of air e. g. , small or crowded places).
HYPERCAPNIA: DEFINITION: • Excess CO 2 in body fluids. (Hypercapnia + Hypoxia): Only when hypoxia is caused by hypoventilation or circulatory deficiency.
Causes of hypoxia in the absence of hypercapnia: Hypoxia caused by: too little oxygen in the air, too little Hb, poisoning of oxidative enzymes
Causes of hypoxia in the absence of serious hypercapnia: • In hypoxia due to poor diffusion through the pulmonary Membrane or tissues (serious hypercapnia does not occur because CO 2 diffuses 20 times as rapidly as O 2). • If hypercapnia begin to occur simultaneously stimulate pulm. Vent. correction of hypercapnia but not necessarily hypoxia.
Causes of hypoxia + hypercapnia (simultaneously): • In hypoxia due to hypoventilation, CO 2 transfer between alveoli & atmosphere is affected as much as is oxygen transfer. • In circulatory deficiency decreased blood flow decreased removal of CO 2 from the tissues tissue hypercapnia + hypoxia. • But transport capacity of blood for CO 2 is more than 3 times that for O 2, so resulting tissue hypercapnia in much less than tissue hypoxia.
Severe Dyspnea: • When alveolar PCO 2 rises above about 60 -75 mm Hg air hunger / dyspnea becomes severe. • If PCO 2 rises to 80 -100 mm Hg lethargy, +/semicomatose • If PCO 2 rises to 120 to 150 mm Hg +/anesthesia & death • At such high PCO 2 Resp. Centre is depressed rather than stimulated vicious circle:
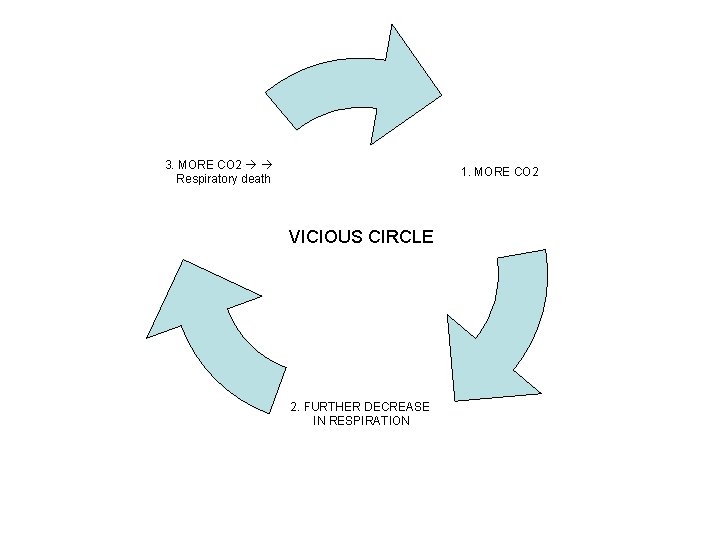
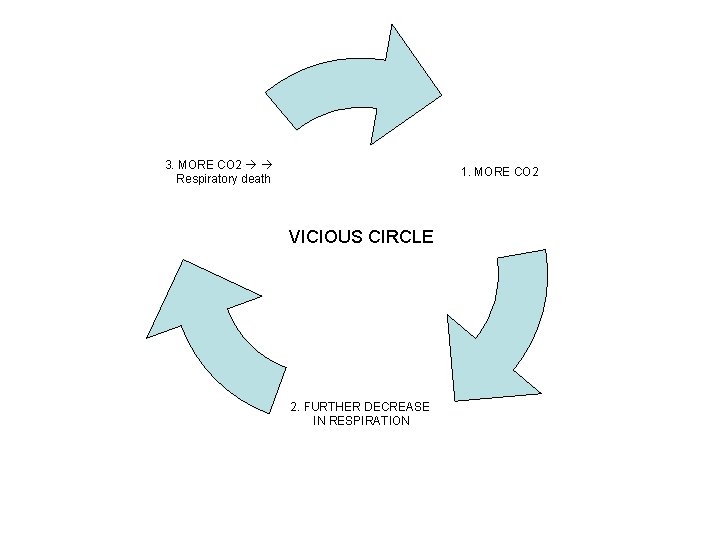
3. MORE CO 2 Respiratory death 1. MORE CO 2 VICIOUS CIRCLE 2. FURTHER DECREASE IN RESPIRATION
ASPHYXIA: DEFINITION: Simultanoeus acute hypoxia & hypercapnia. CAUSES: • Acute airway obstruction • When a person is forced to re-breathe his own air in a confined space.
Mechanism: • During asphyxia hypoxia + hypercapnia = hypercarbia strong stimulation of respiratory centre & violent inspiratory efforts heart rate increases, BP increases, CATS increase from adrenal medulla (increase in nor-epinephrine > epinephrine) unconsciousness, convulsions & decrease in respiratory rate death.
O 2 THERAPY: (3 ways) • 1) O 2 mask on nose • 2) Intra-nasal tube • 3) O 2 tent (newborn) When O 2 is given for longer period toxic effects.
100% O 2 treatment for over 8 hrs: Features of airway irritation sore throat substernal distress nasal congestion coughing
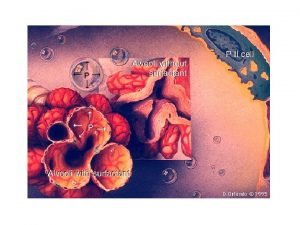
100% O 2 treatment for 24 -48 hrs: Toxic effects start like lung damage, decreased ability of alveolar macrophages to kill bacteria, decrease in surfactant secretion, cyst formation in lung may occur, Retrolental fibroplasia in infants kept in O 2 tents for long.
Cause of toxic effects of oxygen: • Formation of certain ions: • Super-oxide ions (O 2 -) • Hydrogen peroxide (H 2 O 2)
Prevention of toxic effects of oxygen: • By anti-oxidants like vitamin E.
Benefit of Oxygen therapy: • • • Helpful in some types of hypoxia. Most helpful in hypoxic hypoxia. May be helpful in cyanide or CO poisoning May be helpful in case of Gas Gangrene. No use in Anemic & Ischemic (stagnant) hypoxia.
 Ards permissive hypercapnia
Ards permissive hypercapnia Hypercapnia
Hypercapnia Permissive hypercapnia
Permissive hypercapnia Cyanosis types
Cyanosis types Two types of cyanosis
Two types of cyanosis Decrd
Decrd Dead space vs shunt
Dead space vs shunt Intra plural pressure
Intra plural pressure Baltic sea hypoxia
Baltic sea hypoxia Magzati hypoxia
Magzati hypoxia Haemoglobin
Haemoglobin Diffusion hypoxia slideshare
Diffusion hypoxia slideshare Second gas effect
Second gas effect Hemoglobina
Hemoglobina Hypoximia
Hypoximia Eisenmenger syndrome
Eisenmenger syndrome Cyanosis
Cyanosis Cynosis
Cynosis Decardron
Decardron Causes of cyanosis
Causes of cyanosis Central cyanosis in newborn when crying
Central cyanosis in newborn when crying Approach to dyspnea
Approach to dyspnea Borg breathlessness scale
Borg breathlessness scale Modified borg scale
Modified borg scale Paroxysmal nocturnal dyspnea pathophysiology
Paroxysmal nocturnal dyspnea pathophysiology Dyspnea grading nyha
Dyspnea grading nyha Faacvpr
Faacvpr Cardiac vs pulmonary dyspnea
Cardiac vs pulmonary dyspnea Dr marwa a. ahmed
Dr marwa a. ahmed Dyspnea exertion scale
Dyspnea exertion scale Define dyspnea
Define dyspnea Complications of respiratory failure
Complications of respiratory failure Grades of dyspnea
Grades of dyspnea