Hypoxia Prof K Sivapalan Hypoxia It is deficiency
![Respiratory Adjustment to High Altitude [Acclimatization] • At 3000 meters, alveolar PO 2 is Respiratory Adjustment to High Altitude [Acclimatization] • At 3000 meters, alveolar PO 2 is](https://slidetodoc.com/presentation_image_h2/50829b870bf42251bc3746ca87ec5637/image-5.jpg)
![Hypoxic Hypoxia due to Disease • Respiratory problems [benefitted by breathing 100% oxygen] – Hypoxic Hypoxia due to Disease • Respiratory problems [benefitted by breathing 100% oxygen] –](https://slidetodoc.com/presentation_image_h2/50829b870bf42251bc3746ca87ec5637/image-6.jpg)
![Stagnant [Hypoperfusion] Hypoxia • In adequate blood flow to tissues and inability to deliver Stagnant [Hypoperfusion] Hypoxia • In adequate blood flow to tissues and inability to deliver](https://slidetodoc.com/presentation_image_h2/50829b870bf42251bc3746ca87ec5637/image-9.jpg)
- Slides: 13
Hypoxia Prof. K. Sivapalan
Hypoxia • It is deficiency of oxygen at tissue level. • In brain, mild hypoxia causes impaired judgment, drowsiness, reduced pain sensitivity, excitement, disorientation, loss of time sense and headache. • Anorexia, nausea, vomiting, tachycardia, hypertension and tachypnoea. • If PO 2 is less than 20 mm Hg, loss of consciousness in 10 -20 seconds and death in 4 -5 minutes. 2013 Hypoxia 2
Classification • Hypoxic hypoxia- arterial PO 2 reduced • Anaemic hypoxia- arterial PO 2 normal but not enough haemoglobin • Stagnant or hypoperfusion hypoxiaarterial PO 2 and Hb are normal but reduced blood flow • Histotoxic hypoxia- O 2 delivery is normal but the tissues are unable to use it. 2013 Hypoxia 3
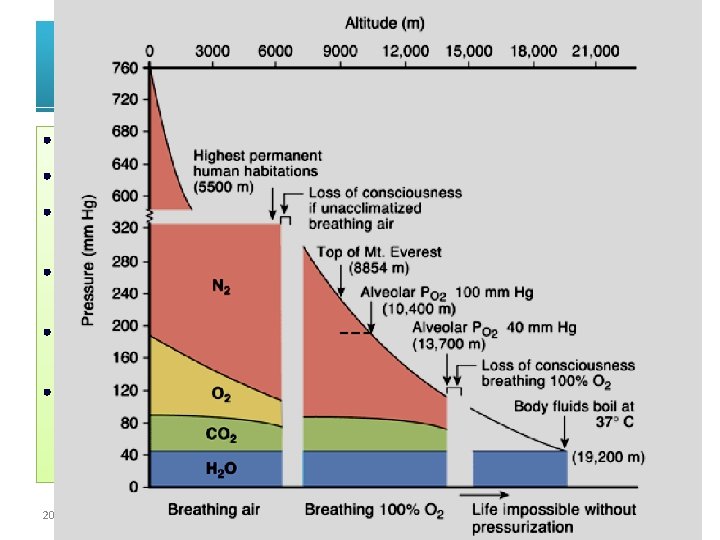
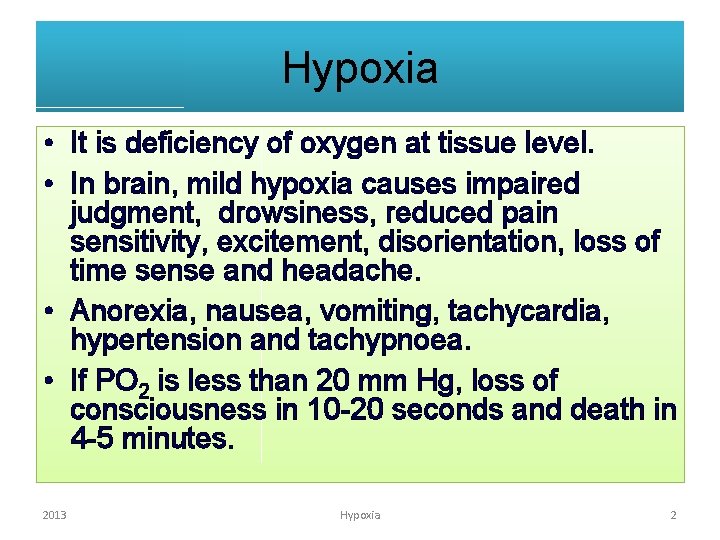
Decreased Barometric Pressure • High altitude is one cause. • Water vapor pressure remains 47 at all altitudes. • Carbon dioxide remains close to 40 mm Hg. Small decrease if hyper ventilation occurs. • The nitrogen and oxygen pressures keep decreasing as altitude increases • At 6000 meters, PO 2 is about 40 m Hg – loss of consciousness without pure oxygen • With pure oxygen, alveolar oxygen will be 100 mm Hg at 10, 400 M. 2013 Hypoxia 4
![Respiratory Adjustment to High Altitude Acclimatization At 3000 meters alveolar PO 2 is Respiratory Adjustment to High Altitude [Acclimatization] • At 3000 meters, alveolar PO 2 is](https://slidetodoc.com/presentation_image_h2/50829b870bf42251bc3746ca87ec5637/image-5.jpg)
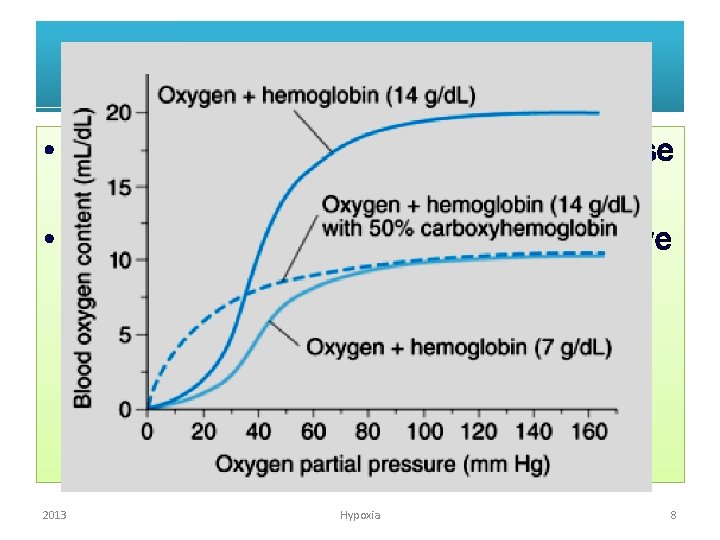
Respiratory Adjustment to High Altitude [Acclimatization] • At 3000 meters, alveolar PO 2 is 60 mm. Hg • Hypoxia stimulates peripheral chemo receptors and hyper ventilation occurs • This washes CO 2 and causes respiratory alkalosis, depresses respiration. • Net effect is no change in respiration immediately • 2 -3 BPG increases and balances the increased affinity of Hb due to alkalosis- small increase in P 50. • Over the next few days CSF p. H normalizes and hypoxic drive causes hyperventilation. [It takes years to adapt to hypoxia] • Erythropoiten causes polycythaemia, myoglobin and mytochondria increase in tissues 2013 Hypoxia 5
![Hypoxic Hypoxia due to Disease Respiratory problems benefitted by breathing 100 oxygen Hypoxic Hypoxia due to Disease • Respiratory problems [benefitted by breathing 100% oxygen] –](https://slidetodoc.com/presentation_image_h2/50829b870bf42251bc3746ca87ec5637/image-6.jpg)
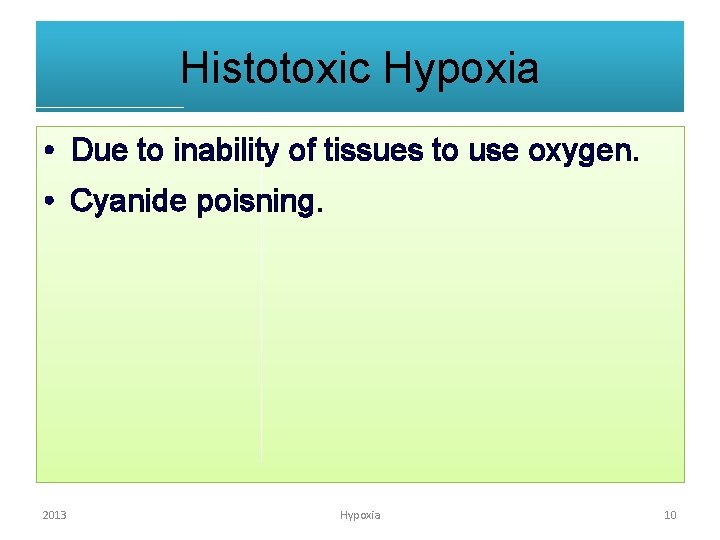
Hypoxic Hypoxia due to Disease • Respiratory problems [benefitted by breathing 100% oxygen] – – – Pulmonary fibrosis causing capillary block Pneumothorax bronchial obstruction Depressed respiratory centre by drugs Altered ventilation perfusion ratio- no use of oxygen therapy • Shunt of venous blood- not benefitted by oxygen therapy – Cyanotic heart diseases 2013 Hypoxia 6
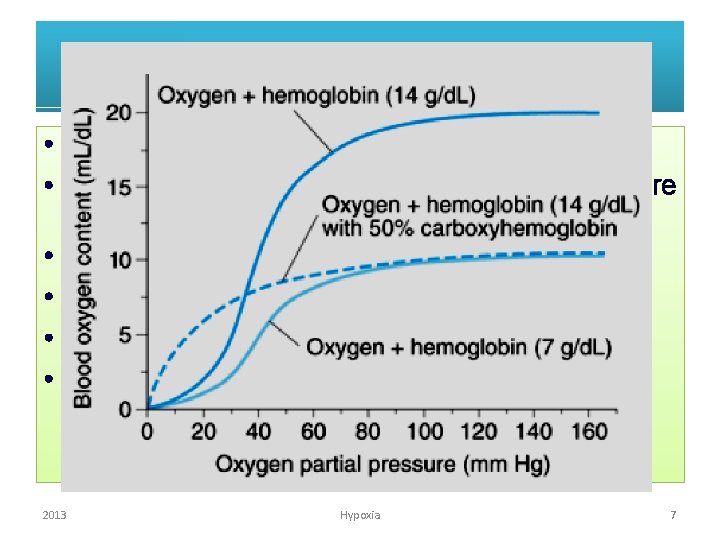
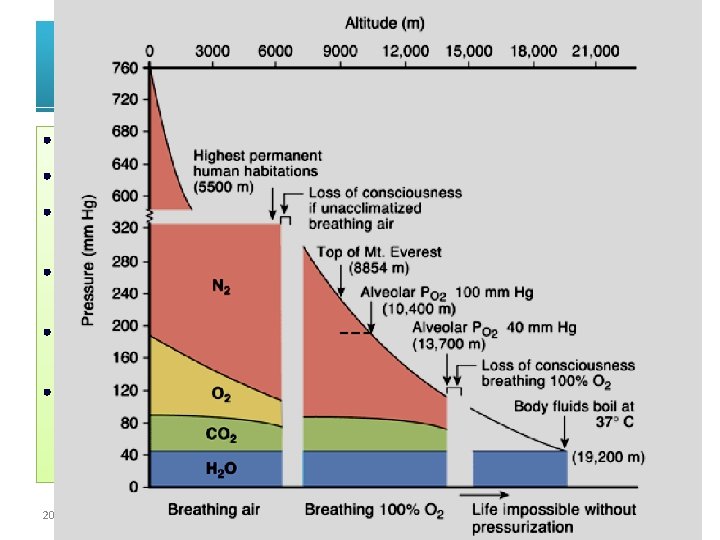
Anaemic Hypoxia • Haemoglobin concentration reduced. • Oxygen and carbon dioxide carrying capacities are reduced. • Arterial PO 2 and PCO 2 not changed • Chemoreceptors are not stimulated. • No change in respiration at rest. • Tissue hypoxia and hypercapnoea along with increased acidity causes Local Vaso dilation leading to cardio-vascular responses. 2013 Hypoxia 7
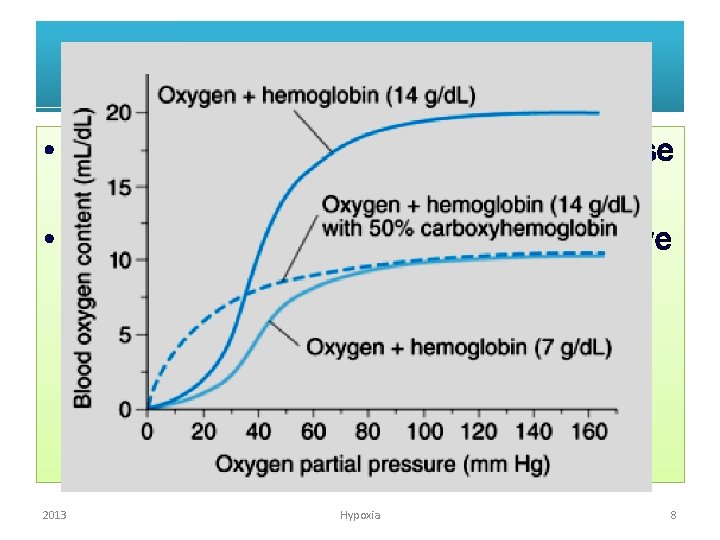
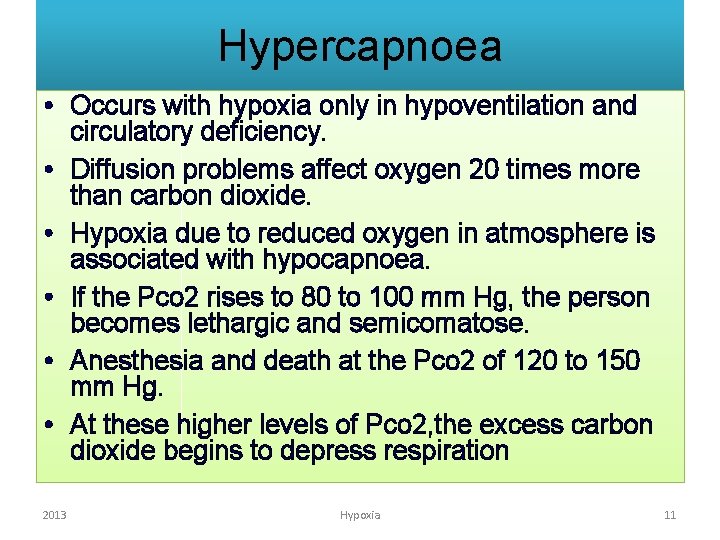
CO poisning • CO also causes anaemic hypoxia because available haemoglobin reduced. • CO also reduces release of O 2 [shift curve to right] 2013 Hypoxia 8
![Stagnant Hypoperfusion Hypoxia In adequate blood flow to tissues and inability to deliver Stagnant [Hypoperfusion] Hypoxia • In adequate blood flow to tissues and inability to deliver](https://slidetodoc.com/presentation_image_h2/50829b870bf42251bc3746ca87ec5637/image-9.jpg)
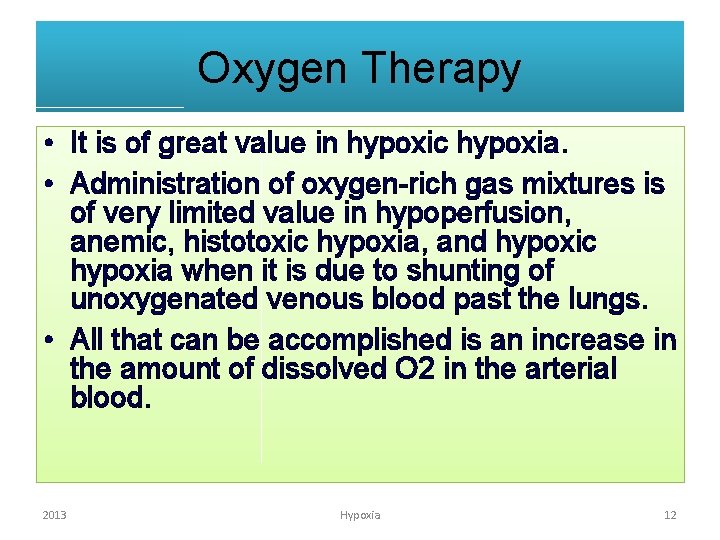
Stagnant [Hypoperfusion] Hypoxia • In adequate blood flow to tissues and inability to deliver adequate oxygen. • Due to circulatory problems– Myocardial infarction – Congestive heart failure – Haemorrhage • Organs most affected are the ones that do not get adequate blood and high metabolic rate- kidney, heart, brain. 2013 Hypoxia 9
Histotoxic Hypoxia • Due to inability of tissues to use oxygen. • Cyanide poisning. 2013 Hypoxia 10
Hypercapnoea • Occurs with hypoxia only in hypoventilation and circulatory deficiency. • Diffusion problems affect oxygen 20 times more than carbon dioxide. • Hypoxia due to reduced oxygen in atmosphere is associated with hypocapnoea. • If the Pco 2 rises to 80 to 100 mm Hg, the person becomes lethargic and semicomatose. • Anesthesia and death at the Pco 2 of 120 to 150 mm Hg. • At these higher levels of Pco 2, the excess carbon dioxide begins to depress respiration 2013 Hypoxia 11
Oxygen Therapy • It is of great value in hypoxic hypoxia. • Administration of oxygen-rich gas mixtures is of very limited value in hypoperfusion, anemic, histotoxic hypoxia, and hypoxic hypoxia when it is due to shunting of unoxygenated venous blood past the lungs. • All that can be accomplished is an increase in the amount of dissolved O 2 in the arterial blood. 2013 Hypoxia 12
Oxygen Toxicity • The toxicity seems to be due to production of reactive oxygen species including superoxide anion (O 2–) and H 2 O 2. • When 80– 100% O 2 is administered to humans for periods of 8 h or more, the respiratory passages become irritated, causing substernal distress, nasal congestion, sore throat, and coughing. • In patients with chronic hypercapnoea oxygen therapy may remove the hypoxic drive of respiration. 2013 Hypoxia 13