Hypoglycemia Driving Implications for Medical Reporting Priya Narula

- Slides: 41
Hypoglycemia & Driving Implications for Medical Reporting… Priya Narula, CCPA Manager, Medical Services Ronnie Aronson MD, FRCPC, FACE Executive Director, LMC Diabetes
Objectives • Define hypoglycemia and severe hypoglycemia and review treatment of each • Review current process of license suspension in Ontario • Understand differentiate the 3 supporting documents: CCMTA, CDA and the CMA Driver’s Guide • Discuss the duty to report across Canada • Define “fitness to drive” • Summarize the Ombudsman report: Better Safe than Sorry
Sources • Determining Driver Fitness in Canada: CCMTA, Ed. 13. August 2013. Canadian Council of Motor Transport Administrators • Better Safe than Sorry Ombudsman Report, April 2014 • CMA Driver’s Guide: Determining Medical Fitness to Operate Motor Vehicles, 8 th edition Canadian Medical Association • CDA CPG’s for Diabetes and Private and Commercial Driving. Begg et al, CJD 2003; 27(2): 128 -140 • The Practice Guide. CPSO College of Physicians and Surgeons of Ontario
Definitions of Hypoglycemia • Mild Hypoglycemia • Severe Hypoglycemia • Hypoglycemia Unawareness
Case Study # 1 54 y/o male with T 1 D for 30 years using MDI therapy. Generally very well-controlled glycemia with minimal mild hypoglycemic event and no hypoglycemia unawareness.
Case Study # 1 He had a severe hypoglycemic episode overnight as he mistakenly took his bolus insulin as his basal. His wife tried to provide him Dextrose tabs however he had passed out and instead paramedics were called. He is otherwise healthy with no co-morbidities and this is the first severe hypoglycemic episode.
Case Study # 1 • Question: – Will you report to the Ministry of Transportation or not?
Case Study # 2 58 year old male with 25 years of well controlled T 1 D using Lantus and Humalog. He has hypoglycemia unawareness however has never had a severe hypoglycemic episode. He checks his blood sugars before he drives.
Case Study # 2 He comes to see you and you notice multiple hypoglycemic episodes, as low as 1. 7 which you start to question. He was at the airport, waiting for his flight home. He explains that he did not have any classic symptoms of hypoglycemia however a passenger noticed him sweating profusely which prompted him to check his blood sugar.
Case Study # 2 He immediately asked the passenger to call for help as he did not have any fast-acting carbohydrates. He was unable to take anything by mouth and there fore was given glucagon by paramedics.
Case Study # 2 While in your office now, you notice him slightly disoriented and again profusely sweating. When you check his blood sugar it is 1. 9. You treat as per your clinic protocol and his sugars after 30 min are at 5. 6. What are your next steps?
Case Study # 3 67 year old male with type 2 diabetes using Apidra and Lantus. In general, he has not been controlled well due to much variation in his diet. He would have mild hypoglycemic events which he would treat appropriately and these events were related to delayed meal.
Case Study # 3 He comes to you for a follow up and explains he was in a car accident with no casualties or injuries. When paramedics arrived his blood sugar was 2. 7. He does not recall any warning symptoms. Prior to driving he checked his blood sugar which was 7. 8, however 1 hour before driving.
Case # 3 • What would you do?
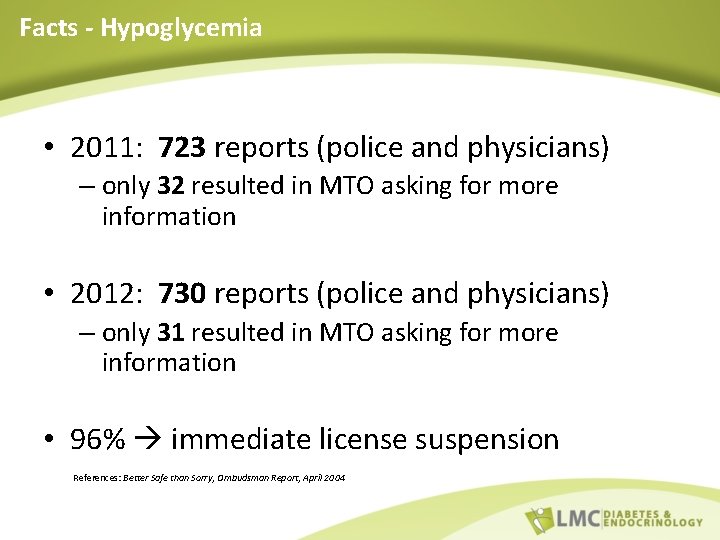
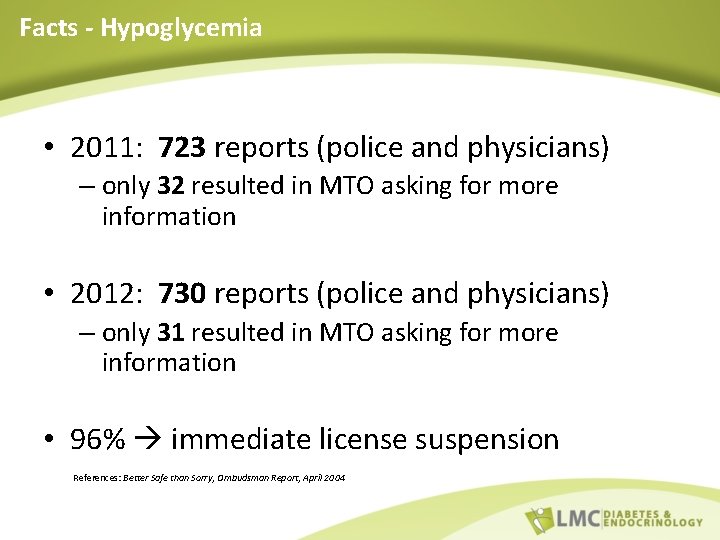
Facts - Hypoglycemia • 2011: 723 reports (police and physicians) – only 32 resulted in MTO asking for more information • 2012: 730 reports (police and physicians) – only 31 resulted in MTO asking for more information • 96% immediate license suspension References: Better Safe than Sorry, Ombudsman Report, April 2004
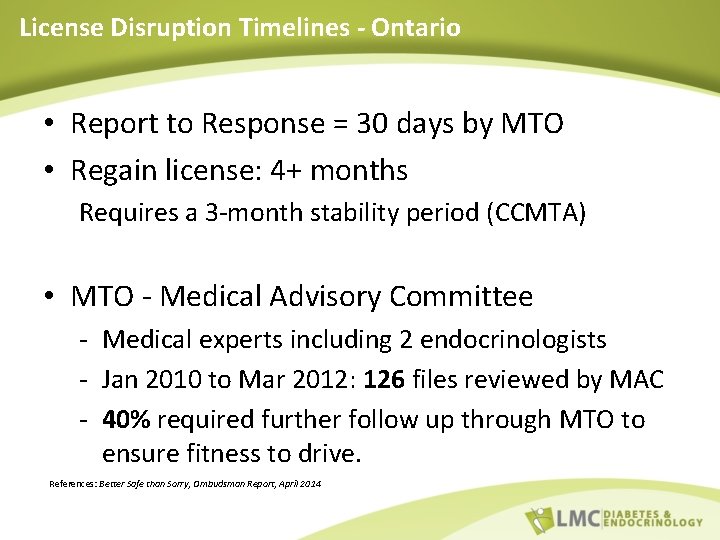
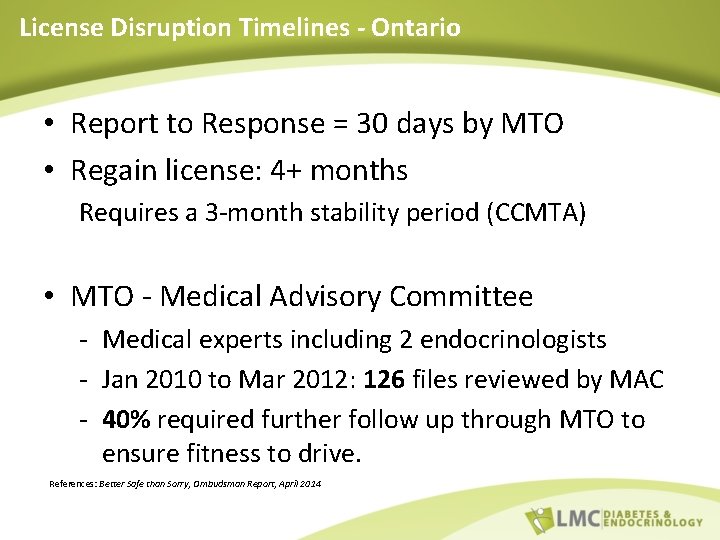
License Disruption Timelines - Ontario • Report to Response = 30 days by MTO • Regain license: 4+ months Requires a 3 -month stability period (CCMTA) • MTO - Medical Advisory Committee - Medical experts including 2 endocrinologists - Jan 2010 to Mar 2012: 126 files reviewed by MAC - 40% required further follow up through MTO to ensure fitness to drive. References: Better Safe than Sorry, Ombudsman Report, April 2014
Conditions & Guidelines
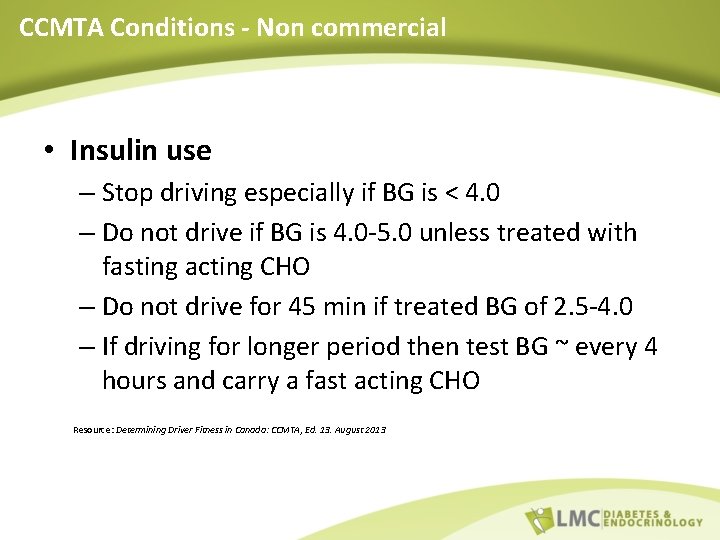
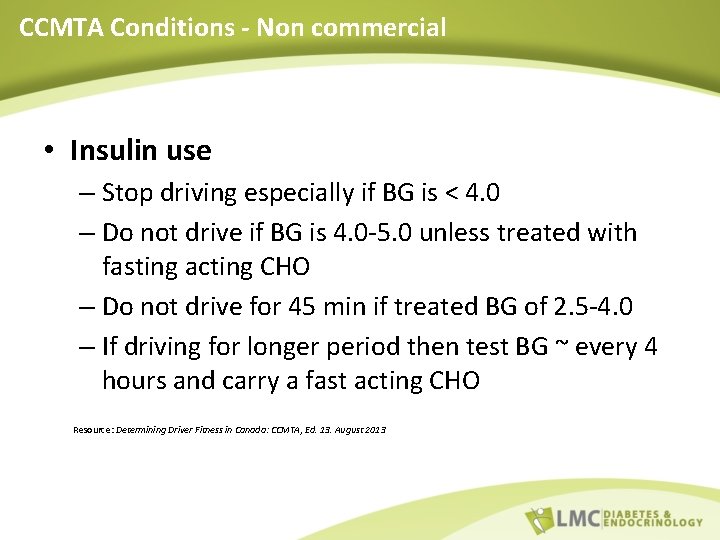
CCMTA Conditions - Non commercial • Insulin use – Stop driving especially if BG is < 4. 0 – Do not drive if BG is 4. 0 -5. 0 unless treated with fasting acting CHO – Do not drive for 45 min if treated BG of 2. 5 -4. 0 – If driving for longer period then test BG ~ every 4 hours and carry a fast acting CHO Resource: Determining Driver Fitness in Canada: CCMTA, Ed. 13. August 2013
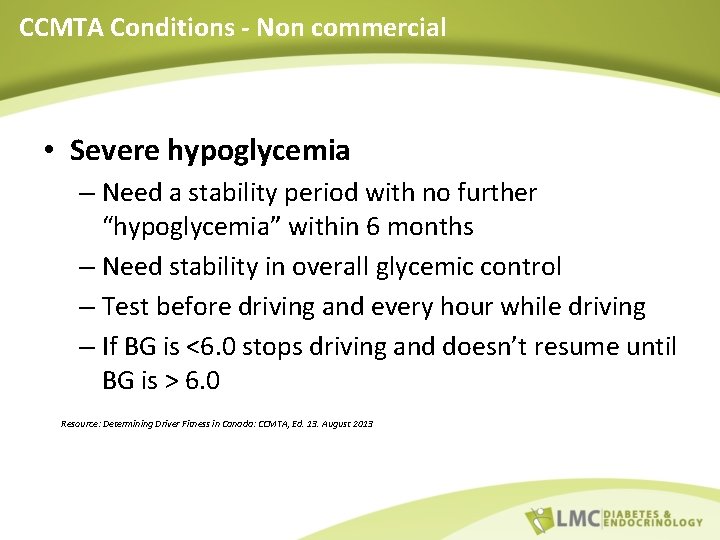
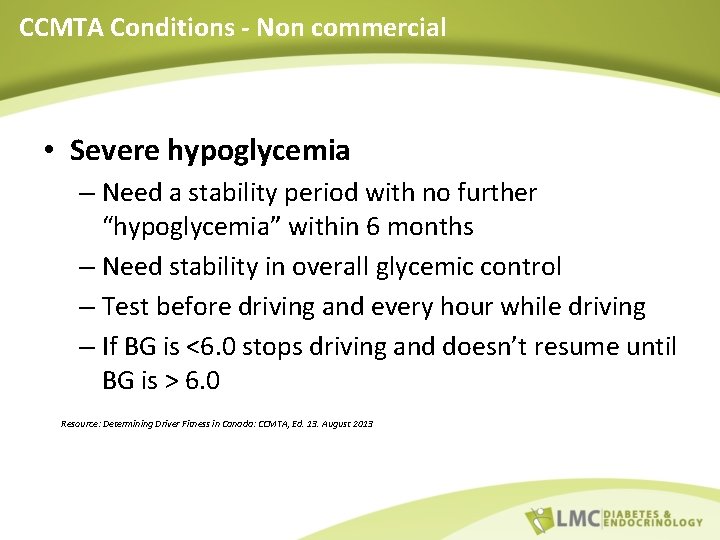
CCMTA Conditions - Non commercial • Severe hypoglycemia – Need a stability period with no further “hypoglycemia” within 6 months – Need stability in overall glycemic control – Test before driving and every hour while driving – If BG is <6. 0 stops driving and doesn’t resume until BG is > 6. 0 Resource: Determining Driver Fitness in Canada: CCMTA, Ed. 13. August 2013
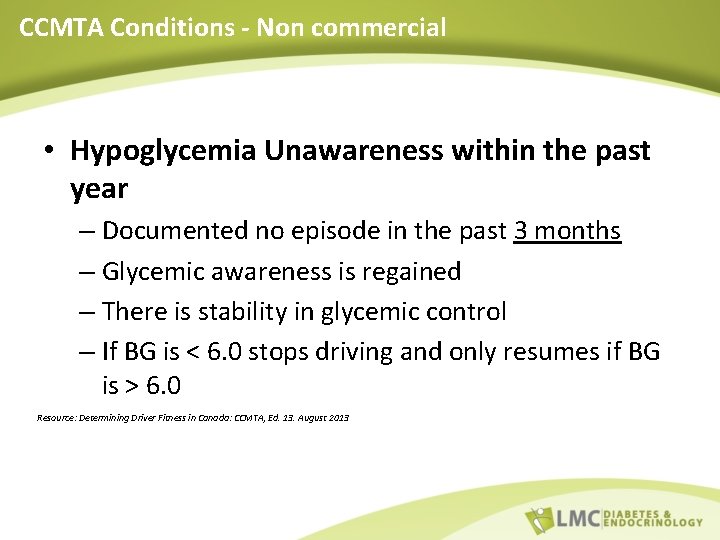
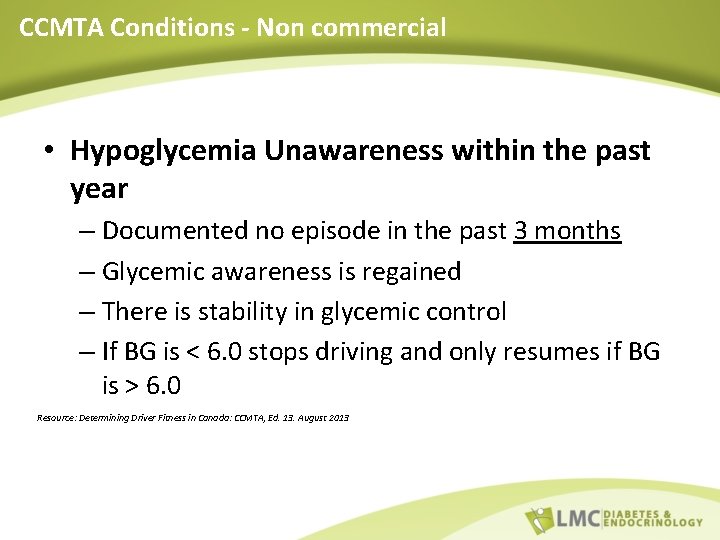
CCMTA Conditions - Non commercial • Hypoglycemia Unawareness within the past year – Documented no episode in the past 3 months – Glycemic awareness is regained – There is stability in glycemic control – If BG is < 6. 0 stops driving and only resumes if BG is > 6. 0 Resource: Determining Driver Fitness in Canada: CCMTA, Ed. 13. August 2013
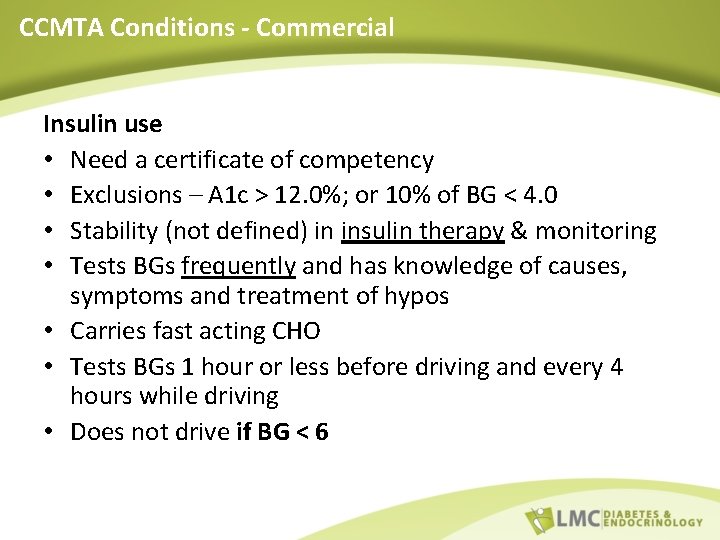
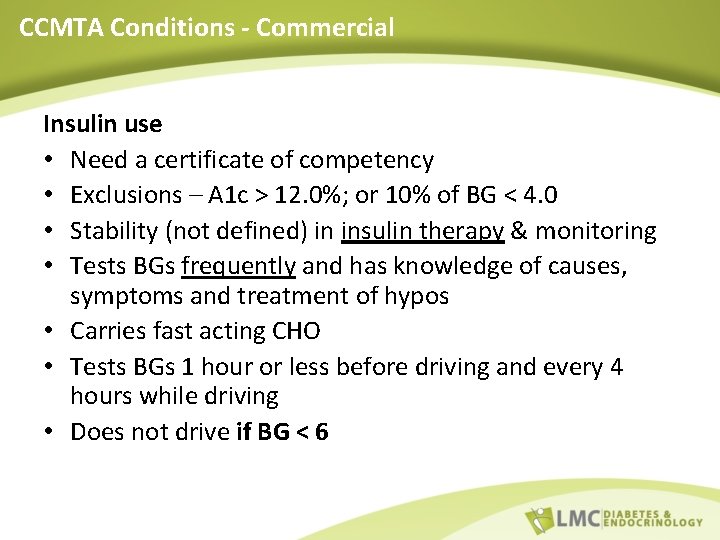
CCMTA Conditions - Commercial Insulin use • Need a certificate of competency • Exclusions – A 1 c > 12. 0%; or 10% of BG < 4. 0 • Stability (not defined) in insulin therapy & monitoring • Tests BGs frequently and has knowledge of causes, symptoms and treatment of hypos • Carries fast acting CHO • Tests BGs 1 hour or less before driving and every 4 hours while driving • Does not drive if BG < 6
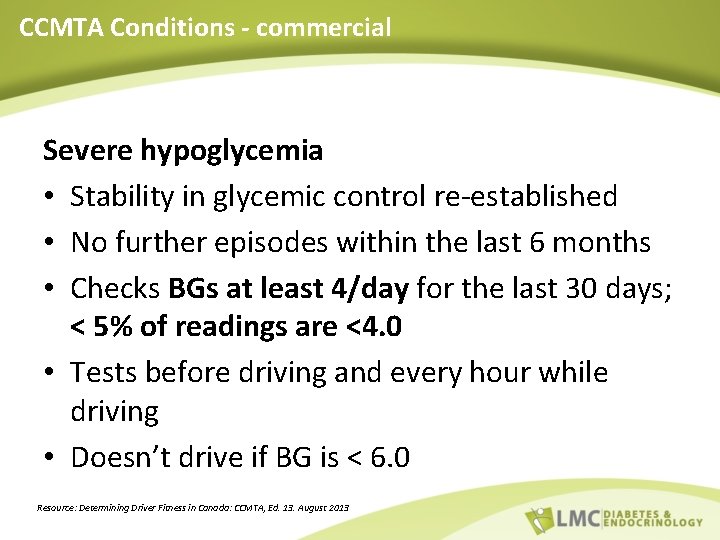
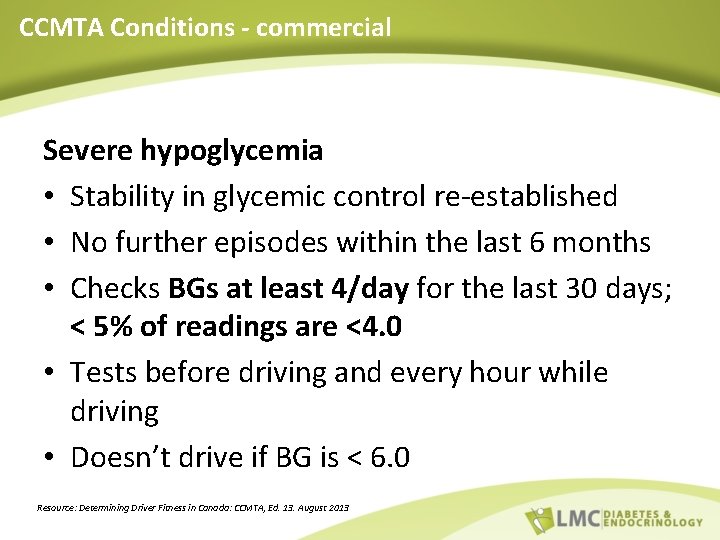
CCMTA Conditions - commercial Severe hypoglycemia • Stability in glycemic control re-established • No further episodes within the last 6 months • Checks BGs at least 4/day for the last 30 days; < 5% of readings are <4. 0 • Tests before driving and every hour while driving • Doesn’t drive if BG is < 6. 0 Resource: Determining Driver Fitness in Canada: CCMTA, Ed. 13. August 2013
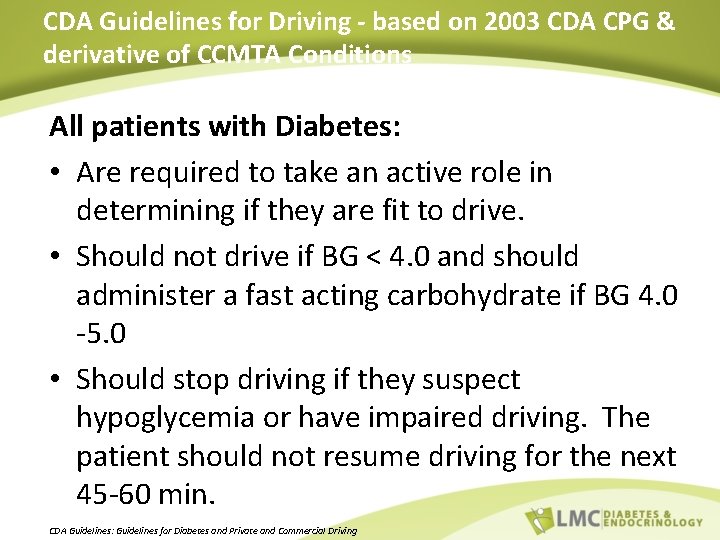
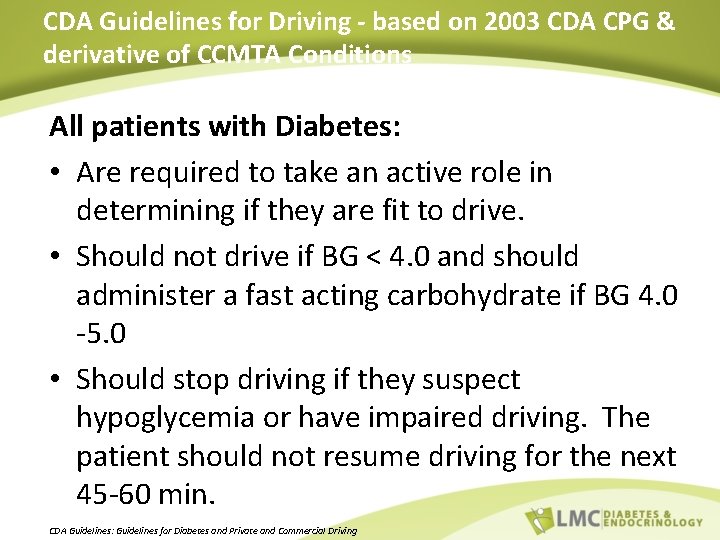
CDA Guidelines for Driving - based on 2003 CDA CPG & derivative of CCMTA Conditions All patients with Diabetes: • Are required to take an active role in determining if they are fit to drive. • Should not drive if BG < 4. 0 and should administer a fast acting carbohydrate if BG 4. 0 -5. 0 • Should stop driving if they suspect hypoglycemia or have impaired driving. The patient should not resume driving for the next 45 -60 min. CDA Guidelines: Guidelines for Diabetes and Private and Commercial Driving
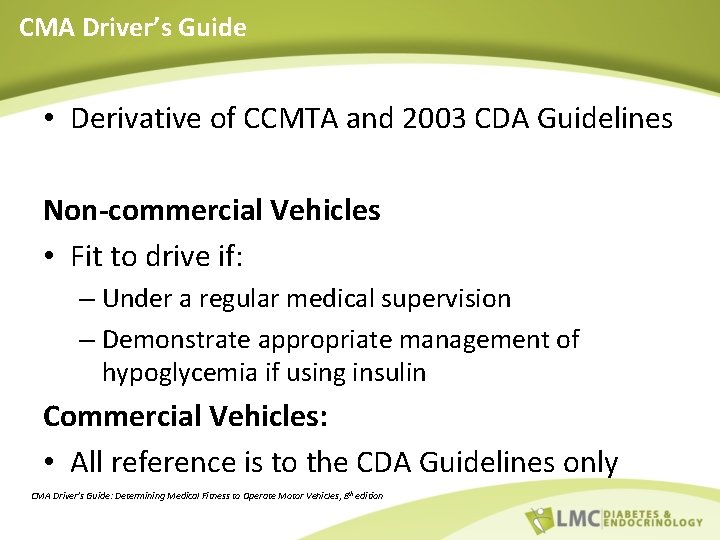
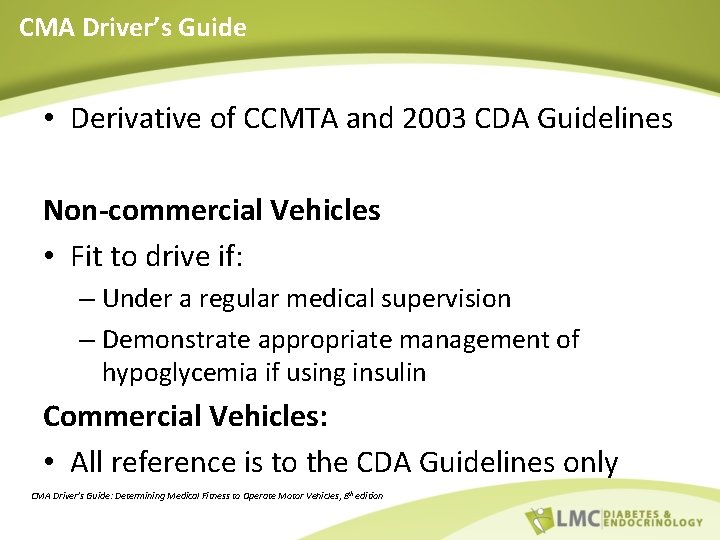
CMA Driver’s Guide • Derivative of CCMTA and 2003 CDA Guidelines Non-commercial Vehicles • Fit to drive if: – Under a regular medical supervision – Demonstrate appropriate management of hypoglycemia if using insulin Commercial Vehicles: • All reference is to the CDA Guidelines only CMA Driver’s Guide: Determining Medical Fitness to Operate Motor Vehicles, 8 th edition
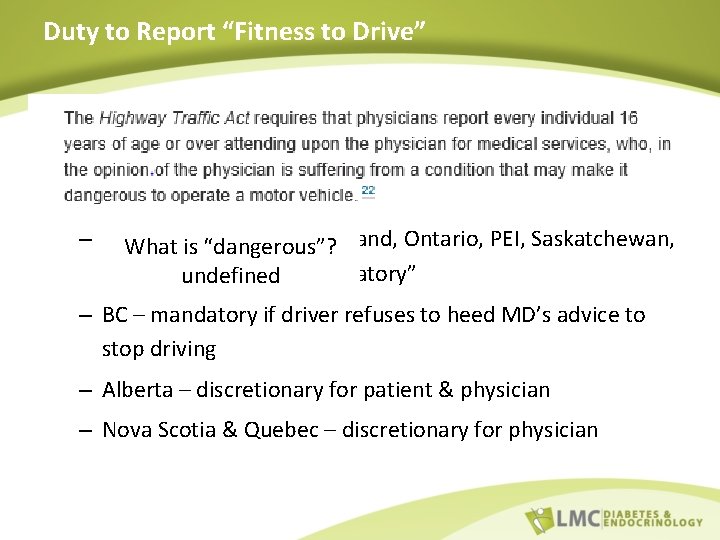
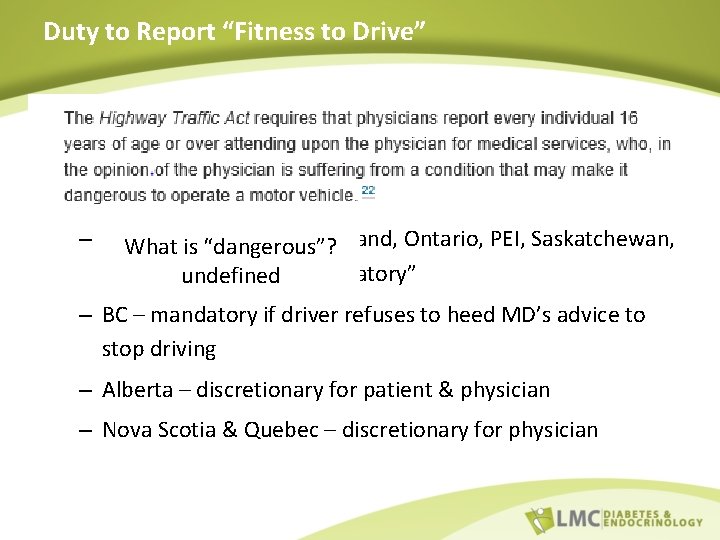
Duty to Report “Fitness to Drive” • CCMTA – silent on duty to report • CDA Guidelines – silent on duty to report other than to refer to provincial legislation: – Manitoba, NB, Newfoundland, Ontario, PEI, Saskatchewan, What is “dangerous”? NWT – “reporting undefinedis mandatory” – BC – mandatory if driver refuses to heed MD’s advice to stop driving – Alberta – discretionary for patient & physician – Nova Scotia & Quebec – discretionary for physician
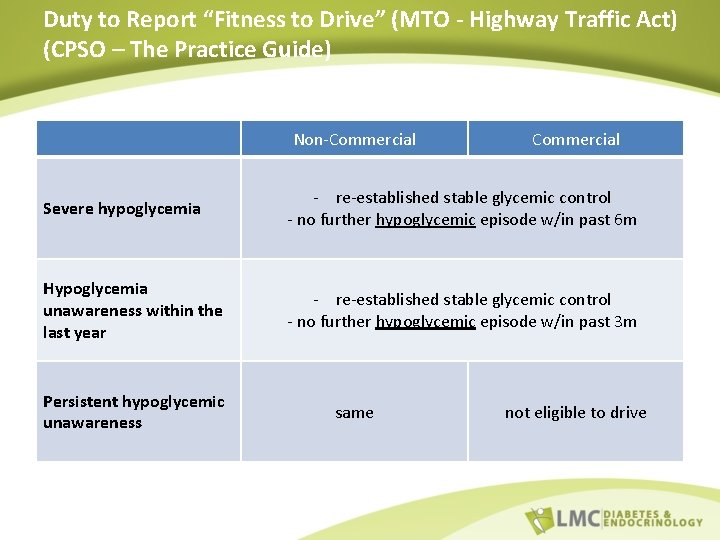
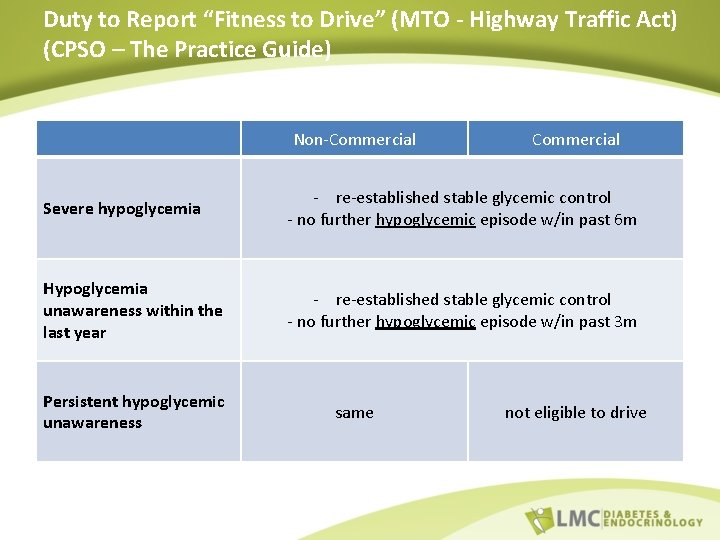
Duty to Report “Fitness to Drive” (MTO - Highway Traffic Act) (CPSO – The Practice Guide) Non-Commercial Severe hypoglycemia - re-established stable glycemic control - no further hypoglycemic episode w/in past 6 m Hypoglycemia unawareness within the last year - re-established stable glycemic control - no further hypoglycemic episode w/in past 3 m Persistent hypoglycemic unawareness same not eligible to drive
Better Safe than Sorry Ombudsman Report April 2014
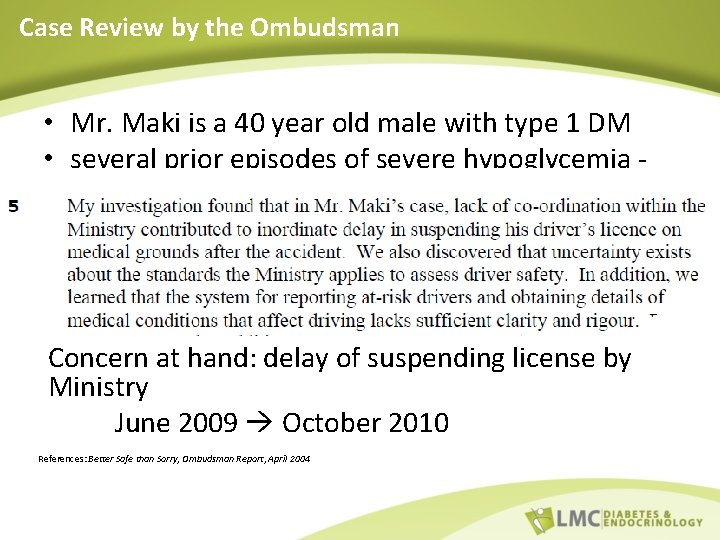
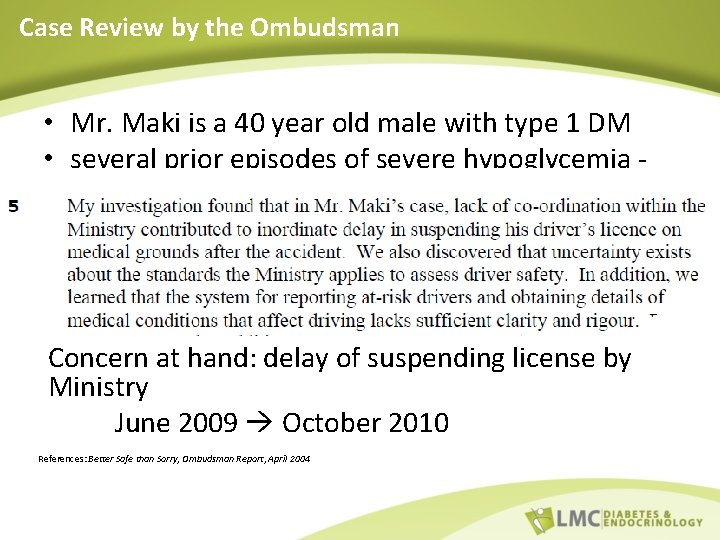
Case Review by the Ombudsman • Mr. Maki is a 40 year old male with type 1 DM • several prior episodes of severe hypoglycemia unknown if his physicians were aware • Day of incident: – BG tested before driving was hypo - treated – did not wait to retest BG MVA - 3 fatalities Concern at hand: delay of suspending license by Ministry June 2009 October 2010 References: Better Safe than Sorry, Ombudsman Report, April 2004

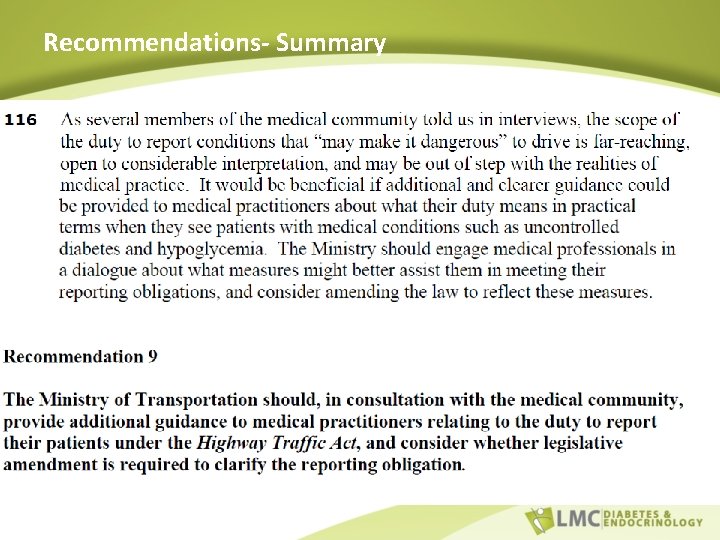
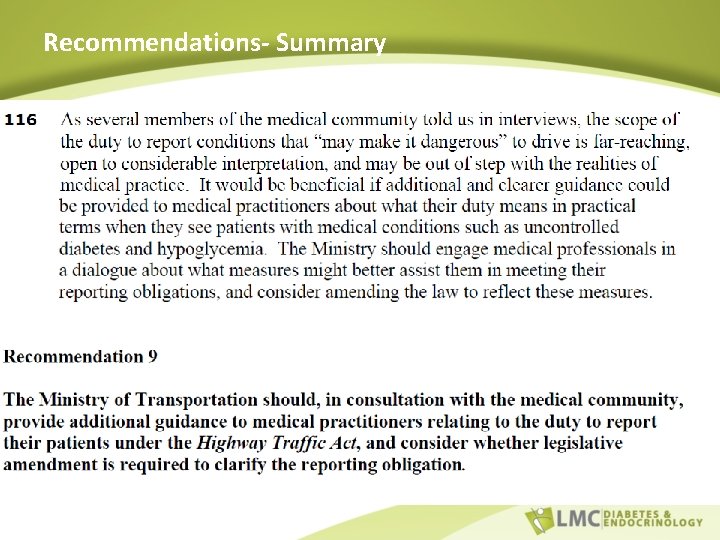
Recommendations- Summary
REVISIT CASE STUDIES
Case Study # 1 54 y/o male with T 1 D for 30 years using MDI therapy. Generally very well-controlled glycemia with minimal mild hypoglycemic event and no hypoglycemia unawareness.
Case Study # 1 He had a severe hypoglycemic episode overnight as he mistakenly took his bolus insulin as his basal. His wife tried to provide him Dextrose tabs however he had passed out and instead paramedics were called. He is otherwise healthy with no co-morbidities and this is the first severe hypoglycemic episode. What are your next steps?
Case Study # 2 58 year old male with 25 years of well controlled T 1 D using Lantus and Humalog. He has hypoglycemia unawareness however has never had a severe hypoglycemic episode. He checks his blood sugars before he drives.
Case Study # 2 He comes to see you and you notice multiple hypoglycemic episodes, as low as 1. 7 which you start to question. He was at the airport, waiting for his flight home. He explains that he did not have any classic symptoms of hypoglycemia however a passenger noticed him sweating profusely which prompted him to check his blood sugar.
Case Study # 2 He immediately asked the passenger to call for help as he did not have any fast-acting carbohydrates. He was unable to take anything by mouth and there fore was given glucagon by paramedics.
Case Study # 2 While in your office now, you notice him slightly disoriented and again profusely sweating. When you check his blood sugar it is 1. 9. You treat as per your clinic protocol and his sugars after 30 min are at 5. 6. What are your next steps?
Case Study # 3 67 year old male with type 2 diabetes using Apidra and Lantus. In general, he has not been controlled well due to much variation in his diet. He would have mild hypoglycemic events which he would treat appropriately and these events were related to delayed meal.
Case Study # 3 • He comes to you for a follow up and explains he was in a car accident with no casualties or injuries. When paramedics arrived his blood sugar was 2. 7. He does not recall any warning symptoms. • Prior to driving he checked his blood sugar which was 7. 8, however 1 hour before driving.
Case # 3 • What would you do?
Contact details Thank you! Priya Narula, BSc, CCPA Manager, Medical Services LMC Diabetes & Endocrinology Priya. narula@lmc. ca For further information www. lmc. ca www. Diabetessource. ca