How Nutrition Plays a Role in Wound Healing


- Slides: 50
How Nutrition Plays a Role in Wound Healing Kelsey L. Puffe Concordia College, Moorhead, MN September 25, 2008
Objectives: § § Be able to describe pressure ulcers Identify contributing factors to development of pressure ulcers Identify the different stages of pressure ulcers Identify recommended treatment and nutritional treatment for pressure ulcers
Bed Sore or Pressure Ulcers n Pressure Ulcers- begin as tender, inflamed patches that develops when a person’s weight rests against a hard surface, exerting pressure on the skin and soft tissue over bony parts of the body. n 95% develop on the lower part of the body Skin Problems & Treatments Health Center: Pressure Ulcers (2007): 15 Sept. 2008 http: //www. webmd. com/skin-problems-and-treatments/tc/pressure-sores
Cause n This is most likely to happen when the person is confined to a bed or wheelchair for long periods of time and is relatively immobile. n n Constant pressure on the skin and tissues Sliding down in a bed or chair, forcing the skin to fold over itself Being pulled across bed sheets or other surfaces Moisture that stays on the skin
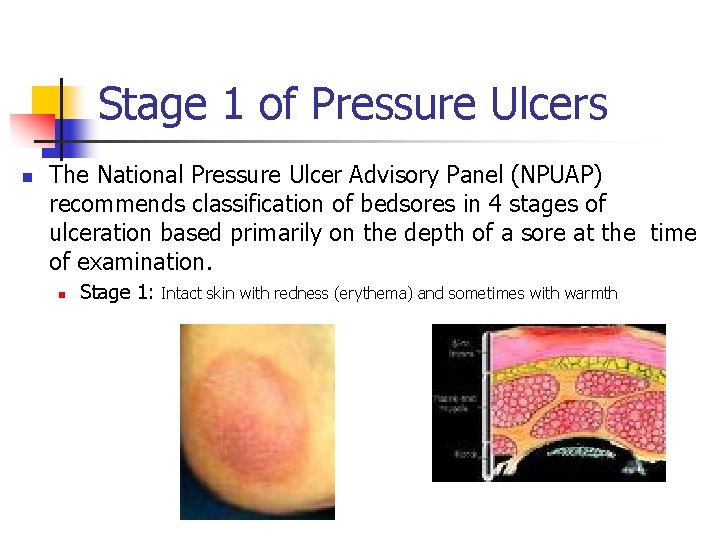
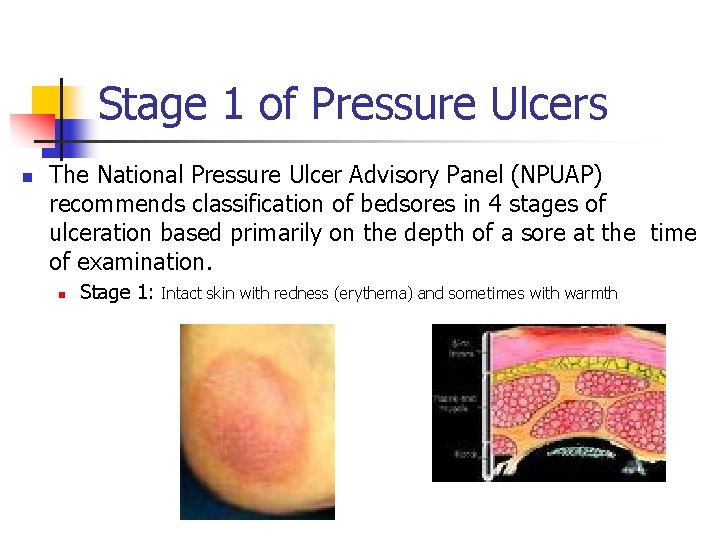
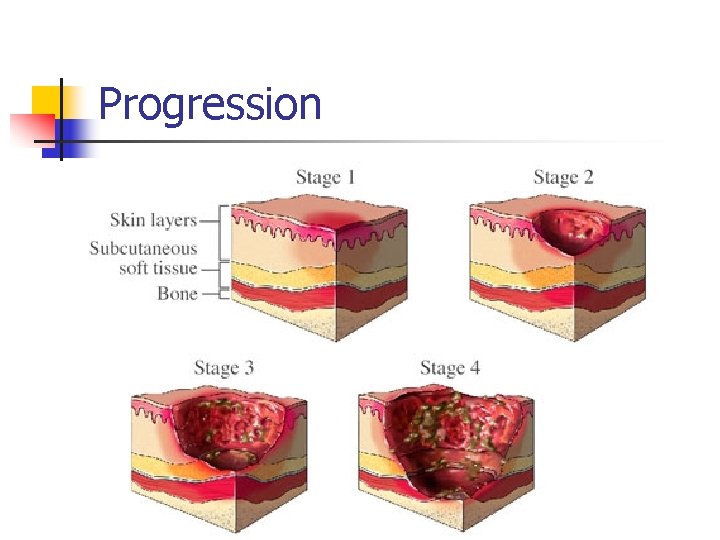
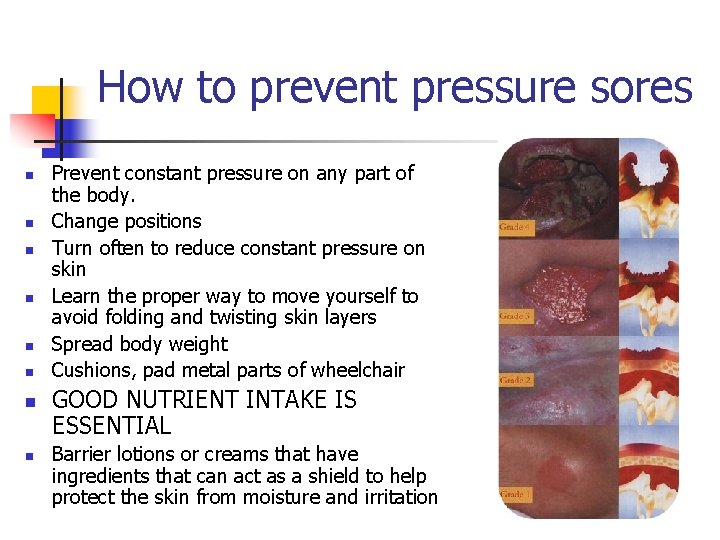
Stage 1 of Pressure Ulcers n The National Pressure Ulcer Advisory Panel (NPUAP) recommends classification of bedsores in 4 stages of ulceration based primarily on the depth of a sore at the time of examination. n Stage 1: Intact skin with redness (erythema) and sometimes with warmth
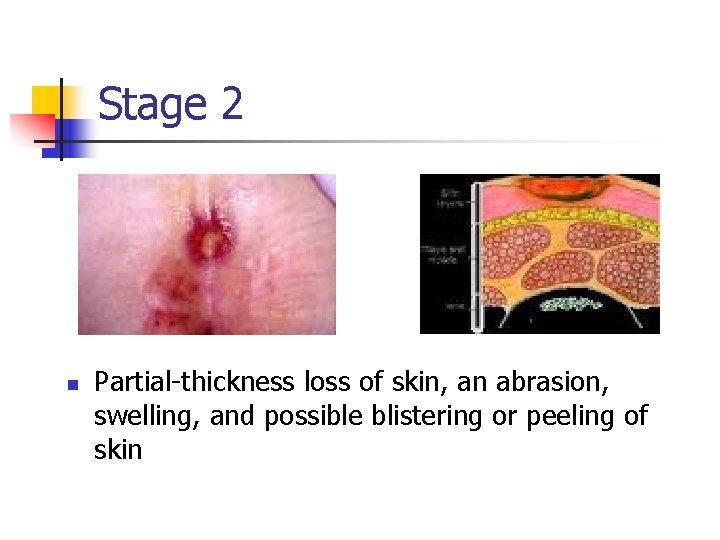
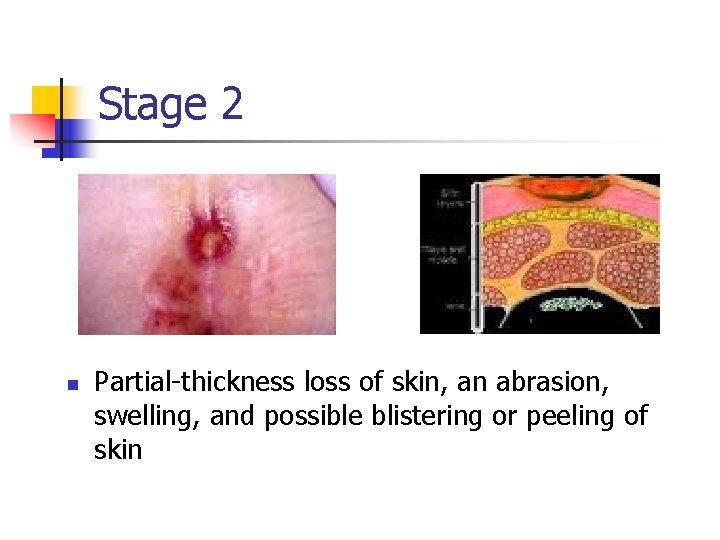
Stage 2 n Partial-thickness loss of skin, an abrasion, swelling, and possible blistering or peeling of skin

Stage 3 n Full-thickness loss of skin, open wound (crater), and possible exposed under layer.
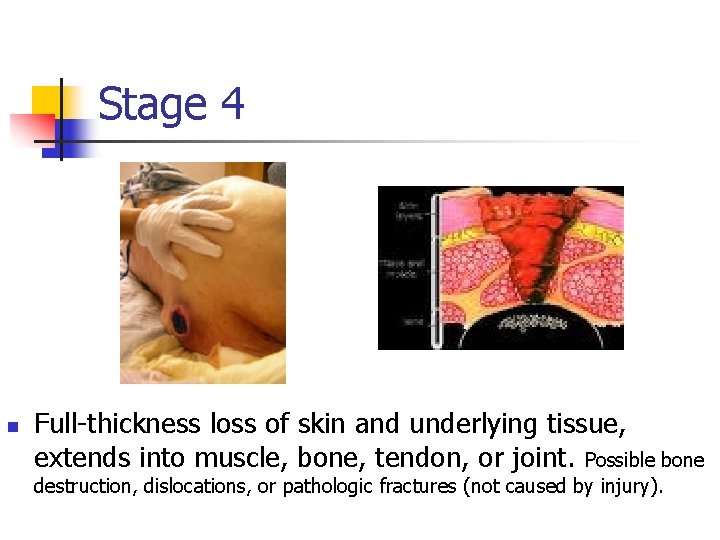
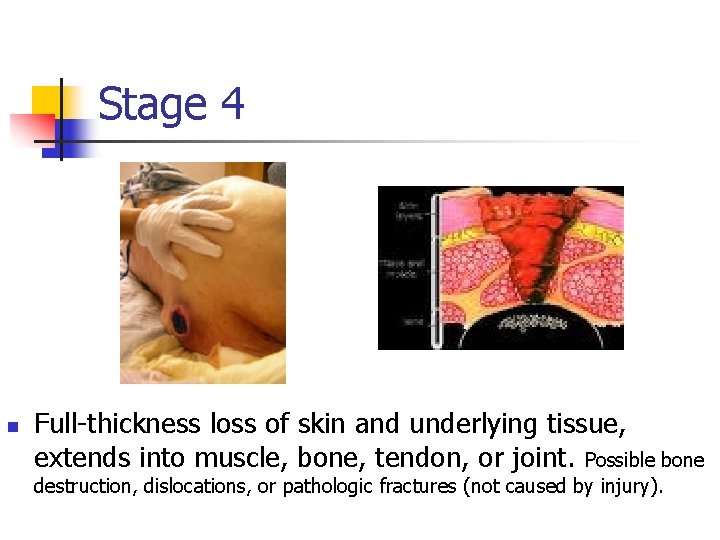
Stage 4 n Full-thickness loss of skin and underlying tissue, extends into muscle, bone, tendon, or joint. Possible bone destruction, dislocations, or pathologic fractures (not caused by injury).
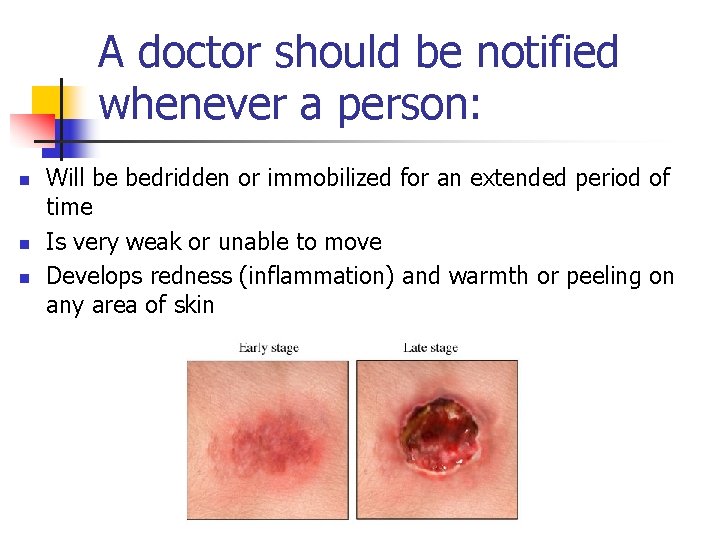
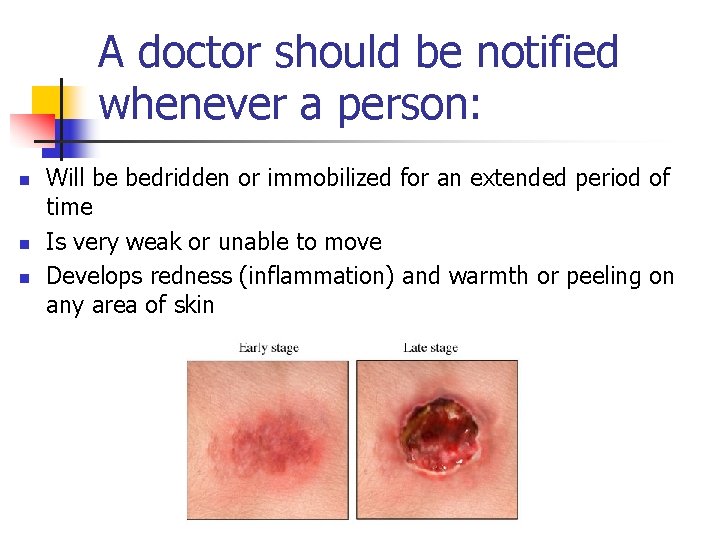
A doctor should be notified whenever a person: n n n Will be bedridden or immobilized for an extended period of time Is very weak or unable to move Develops redness (inflammation) and warmth or peeling on any area of skin
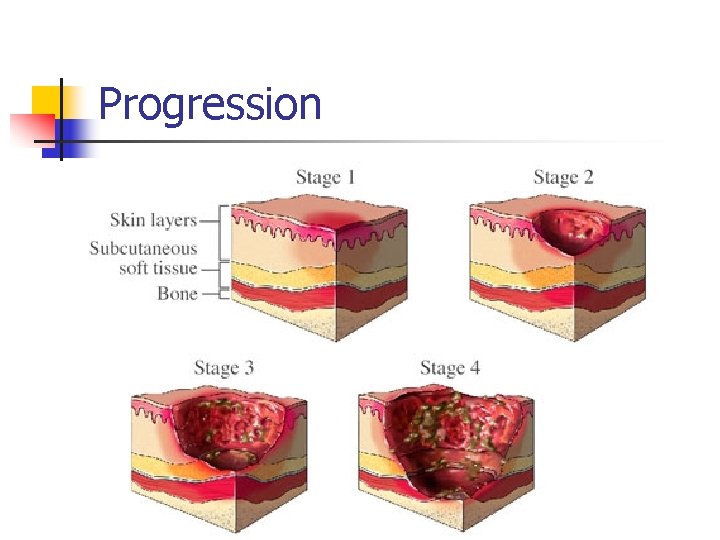
Progression
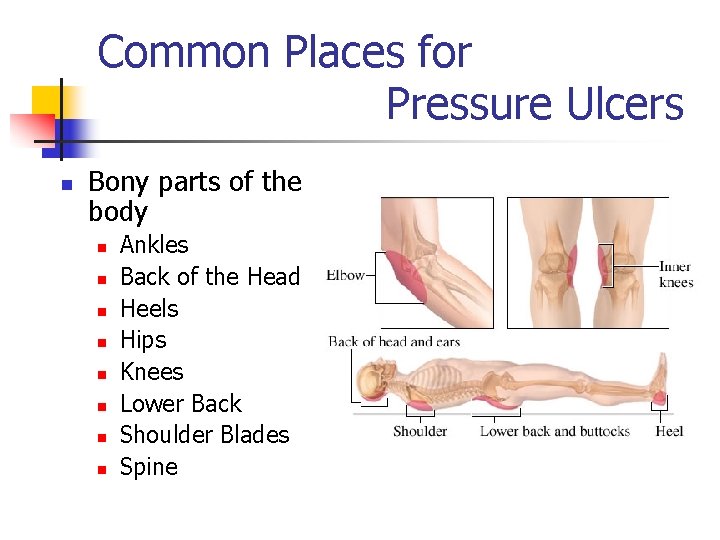
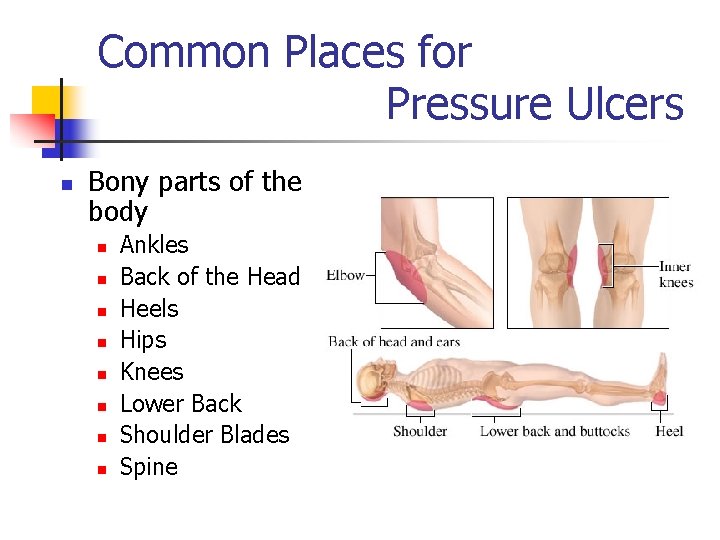
Common Places for Pressure Ulcers n Bony parts of the body n n n n Ankles Back of the Head Heels Hips Knees Lower Back Shoulder Blades Spine
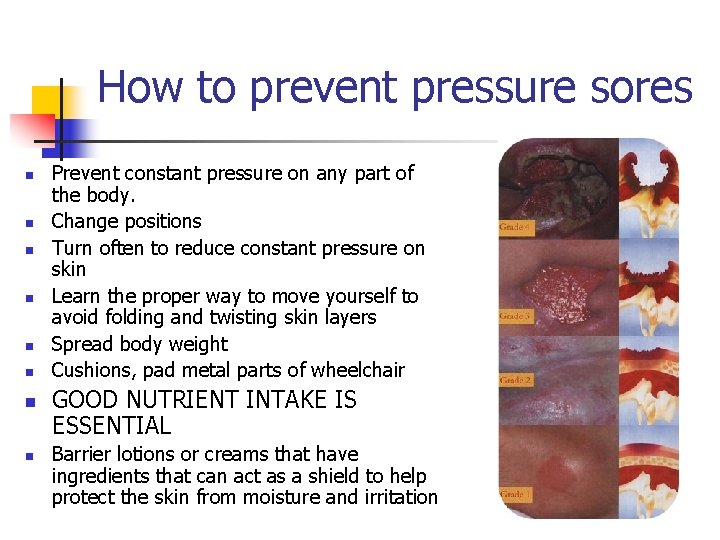
How to prevent pressure sores n n n n Prevent constant pressure on any part of the body. Change positions Turn often to reduce constant pressure on skin Learn the proper way to move yourself to avoid folding and twisting skin layers Spread body weight Cushions, pad metal parts of wheelchair GOOD NUTRIENT INTAKE IS ESSENTIAL Barrier lotions or creams that have ingredients that can act as a shield to help protect the skin from moisture and irritation
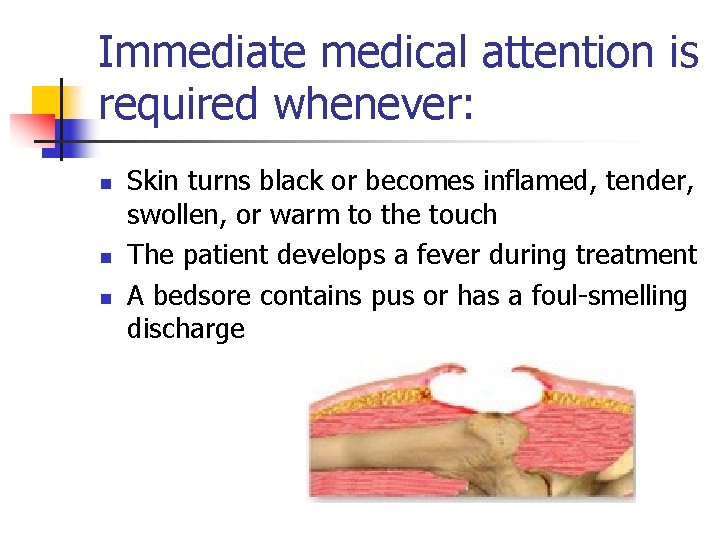
Immediate medical attention is required whenever: n n n Skin turns black or becomes inflamed, tender, swollen, or warm to the touch The patient develops a fever during treatment A bedsore contains pus or has a foul-smelling discharge
Risk Factors for Impaired Healing n n n n n Advanced age Diabetes Impaired immunity Underweight Obesity Malnutrition Medications Infections Moisture Cognitive impairment/ altered sensory perception
Who is typically affected? n n n Older people and individuals with spinal cord injuries Malnutrition, immobility, pressure, shear forces, friction, sensory perception, and skin exposure to moisture can contribute to pressure ulcer incidence Bed-Bound Paralyzed Elderly patients undergoing treatment for other diseases Poor physical function, less able to perform self-care, less mobile
Statistics n n One million people in the United States develop bedsores at a treatment cost of $1 billion Two thirds of all bedsores occur in people over age 70 Pressure sores have been noted as a direct cause of death in about 8% of paraplegics 1992, Federal Agency for Health Care Policy and Research reported that bedsores afflicted n 10% of all hospital patients n 25% of nursing home residents n 60% of quadriplegics Bedsores (2007): 15 Sept. 2008 http: //www. surgeryencyclopedia. com/A-Ce/Bedsores. html
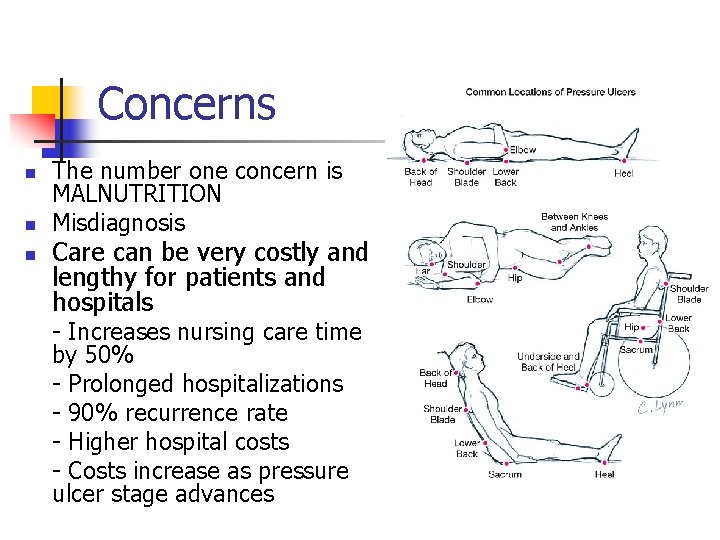
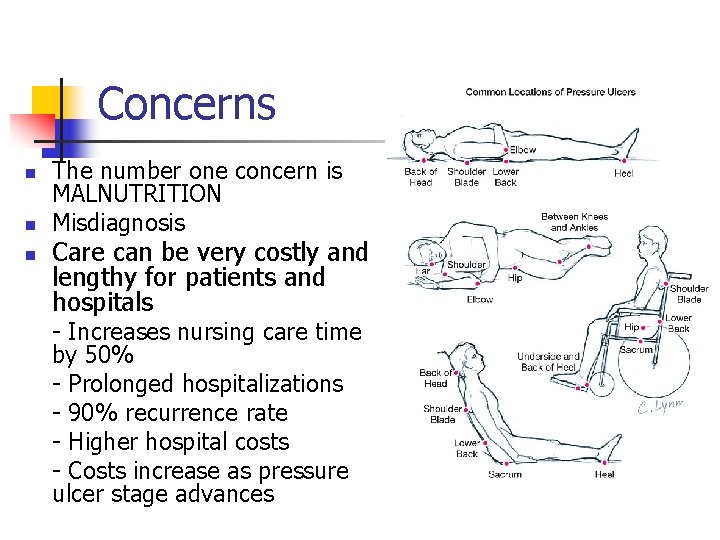
Concerns n n n The number one concern is MALNUTRITION Misdiagnosis Care can be very costly and lengthy for patients and hospitals - Increases nursing care time by 50% - Prolonged hospitalizations - 90% recurrence rate - Higher hospital costs - Costs increase as pressure ulcer stage advances
Consequences n n n Cellulitus- acute infection of connective tissue Bone and joint infections Necrotizing fasciitis- destroys tissues around muscle n n n Gas gangrene Sepsis- blood infection Cancer
Ethical Issues n n n Knowing that Pressure Ulcers are preventable Nutrition Intervention is a great approach Knowledge of how to prevent and treat Pressure Ulcers Recognizing that hospitalized and wheelchair people are more susceptible to Pressure Ulcers Reluctance of health care providers to diagnose Pressure Ulcers & at a early enough stage n n Don’t want to take the blame for development Increasing demands of healthcare intervention accountability by legal professionals
Treatment n Focuses on preventing a sore from getting worse and on making the skin healthy again n n Relieving pressure on the area by changing positions often and spreading body weight evenly with special mattresses Keeping the sore clean and covered, not letting it dry out Eating a healthy diet with enough protein to help the skin heal Keeping healthy tissue around a pressure sore clean and dry Removing dead tissue and applying medicated ointments or creams to reduce the risk of infection.

Treatment n n n Most stage 1 and 2 pressure sores will heal within 60 days with proper treatment Stage 3 and 4 can take months or even years to heal Progress is slow, continued care and treatment can prevent complications such as further tissue damage, infection, and pain
Home Treatment n n n n n Use cushions Use sheepskin layers or foam alternatives on chairs and beds At least every 2 hours, reposition yourself Avoid using doughnut-type devices or boots fill with air to support heals Keep yourself active Inspect skin daily, learn to recognize what a pressure ulcer is Keep skin clean and free of sweat, wound drainage, urine, and feces Moisturize skin with lotion, limited exposure to dry cold weather Provide good nutrition through a healthy diet with enough protein to keep skin healthy and able to heal more quickly Maintain a healthy weight
“Effective nutritional assessment and subsequent support are essential to the prevention and treatment of pressure ulcers. ” Marti Andrews, Ph. D, RD
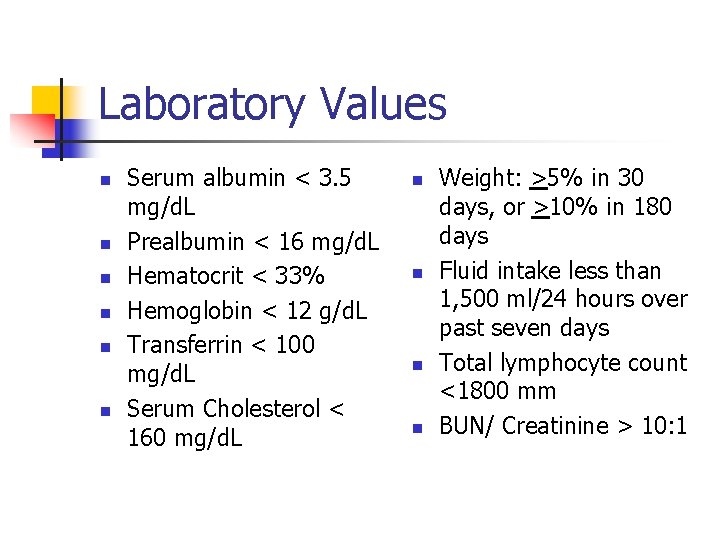
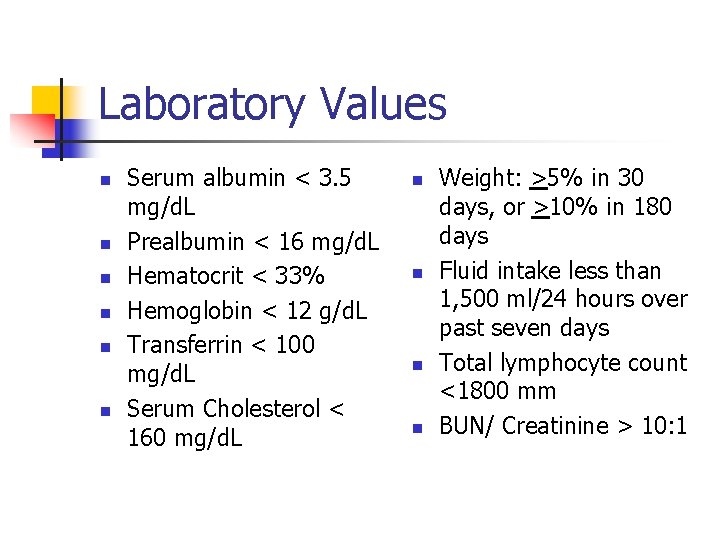
Laboratory Values n n n Serum albumin < 3. 5 mg/d. L Prealbumin < 16 mg/d. L Hematocrit < 33% Hemoglobin < 12 g/d. L Transferrin < 100 mg/d. L Serum Cholesterol < 160 mg/d. L n n Weight: >5% in 30 days, or >10% in 180 days Fluid intake less than 1, 500 ml/24 hours over past seven days Total lymphocyte count <1800 mm BUN/ Creatinine > 10: 1
Nutrition Care n n Patient screening and assessment Nutrition Intervention Monitor Reassess
Nutrition Goals n n Provide adequate calories Prevent/Treat protein-calorie malnutrition Promote wound healing Provide adequate macro and micronutrients during all stages of the wound-care process
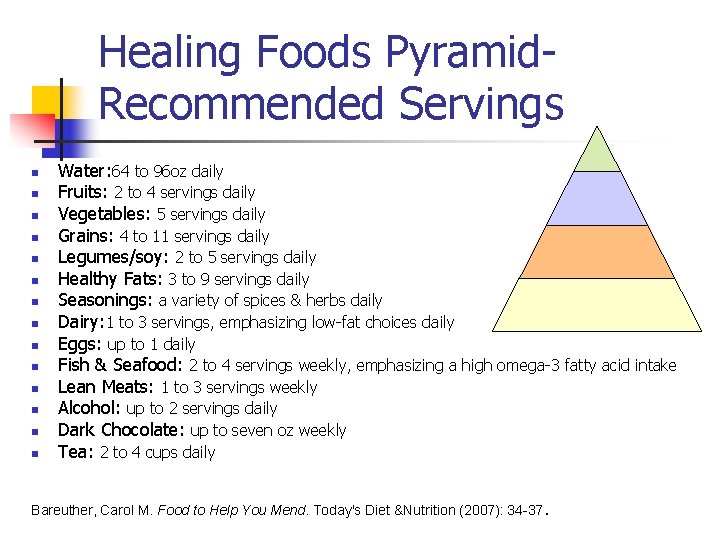
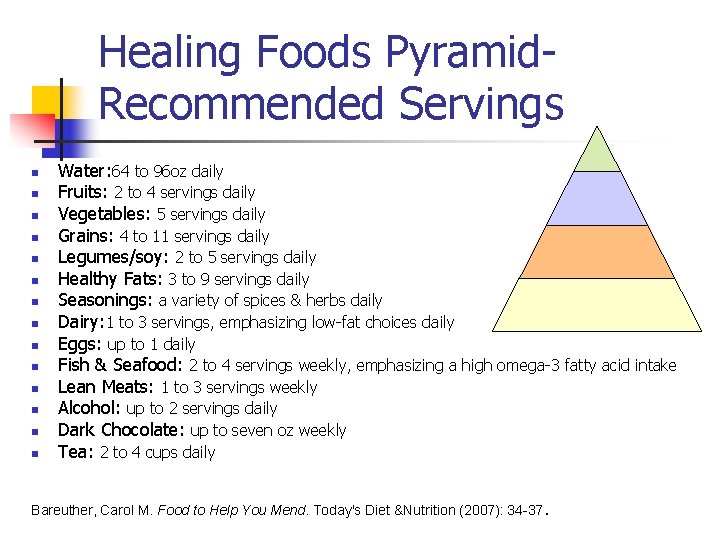
Healing Foods Pyramid. Recommended Servings n n n n Water: 64 to 96 oz daily Fruits: 2 to 4 servings daily Vegetables: 5 servings daily Grains: 4 to 11 servings daily Legumes/soy: 2 to 5 servings daily Healthy Fats: 3 to 9 servings daily Seasonings: a variety of spices & herbs daily Dairy: 1 to 3 servings, emphasizing low-fat choices daily Eggs: up to 1 daily Fish & Seafood: 2 to 4 servings weekly, emphasizing a high omega-3 fatty acid intake Lean Meats: 1 to 3 servings weekly Alcohol: up to 2 servings daily Dark Chocolate: up to seven oz weekly Tea: 2 to 4 cups daily Bareuther, Carol M. Food to Help You Mend. Today's Diet &Nutrition (2007): 34 -37.
Calories n n n Poor calorie intake is associated with poor protein, vitamin and mineral intake. Calories equal energy and it takes a lot of energy to heal a wound. Eat enough calories to “spare” the use of protein for energy. Calories in your diet should come from a variety of “healthy sources” 30 kcal/kg to 35 kcal/kg body weight n n n n Lean meat Beans Legumes Whole grains/cereals Milk and milk products Fruits Vegetables
Basic Principles—CHO & Energy n n n Carbohydrate 55 -60% of diet Provide as complex CHO n n n Glucose is the main energy source for cells Give insulin for glucose >250 mg/d. L and decrease intake if severe hyperglycemia Energy May need to increase calorie intake by 50% or more depending on the severity of the wound. Minimum of 30 -40 kcals/kg/day Use the Harris-Benedict formula to figure the energy need
Basic Principles--Protein n n 20 -25% of diet from protein The “building blocks” for tissue and wound repair. Is involved in the making of cells, enzymes (for chemical reactions) and building connective tissue. Increased protein intake decreases the net nitrogen losses by increasing the amino acid flow into the protein synthesis channel 1. 2 g to 1. 5 g of protein/kg body weight Stage n I- 1. 0 g/kg II- 1. 0 -1. 2 g/kg III- 1. 25 -1. 5 g/kg IV- 1. 5 -2. 0 g/kg Foods that are good sources of protein n All meats, Cheese, Cottage Cheese, Milk, Dry Milk Powder, Instant Breakfast, Egg, Beans, Pudding/custard, Peanut butter, Yogurt, Ensure HP, Boost Merit. Care
Basic Principles--Fat n n 25 -30% of diet Essential for cell membranes and required for the absorption and function of fat-soluble vitamins Fatty acid deficiency disrupts skin integrity Need to keep triglycerides in check
Basic Principles-Fatty Acids/Omega 3 n n n Type of polyunsaturated fatty acid Essential fat because the body cant make it Proper brain growth and development An anti-inflammatory Regulate mood by increasing serotonin levels Recommended 2 to 3 oz servings of fatty fish per week n Cold water fish, wild game, walnuts, leafy greens, canola oil, flaxseed
Basic Principles -Micronutrient Support n Vitamin A n n Important for maintaining healthy skin and mucous membranes Plays a important role in our immune system RDA is 5000 iu In wound healing- take 3 - 4 times the recommended RDA for 1 -2 weeks n Tomato Juice, Apricots, Cantaloupe, Nectarine, Green Beans, Broccoli, Carrots, Squash, Brussels Sprouts, Yams, Sweet Potatoes Merit. Care
Basic Principles - Micronutrient Support n Vitamin C n n Plays an important role in the formation of collagen and cell production RDA is 60 milligrams Daily supplement of 500 mg may be beneficial if a patient is deficient in Vit. C or has pressure ulcers In wound healing- requirement is much greater. May be advised to take additional vitamin C in a pill form. n Orange Juice, Cranberry Juice, Honey dew, Tangerine, Brussels sprouts, Grapefruit, Kiwi fruit, Strawberries, Broccoli, V-8 Juices Merit. Care
Basic Principles - Micronutrient Support n Calcium n n n A cofactor for some collagenases during remodeling Necessary for normal blood coagulation Dietary Nucleotides n n Building blocks for DNA/RNA Improve immune function Assist in wound healing Found in any animal protein
Basic Principles - Micronutrient Support n Vitamin E n n n Important role as an “anti-oxidant” Anti-oxidants help to protect cells from destruction In wound healing- role in reducing atherosclerosis (heart disease) RDA is 10 mg for men & 8 mg for women To much may interfere with wound healing n n Unprocessed whole grains, vegetable oils, margarine, salad dressings, nuts, poultry, fish, seeds, and eggs Copper n n Involved in making of red blood cells, absorption and transportation of iron, wound healing, RNA synthesis and making of collagen RDA is 1. 5 -3. 0 mg/day n Legumes, seafood, shellfish, whole grains, nuts, seeds, and vegetables Merit. Care
Basic Principles - Micronutrient Support n Zinc n n n Involved in over 200 enzyme systems, functions of the immune system, heals wounds, enhances ability to taste food Necessary for metabolism of protein Toxic if too much RDA is 12 -15 mg Can safely take up to 50 mg daily for a 3 month time period to assist with wound healing n Seafood, meats, whole grains, milk & milk products, legumes Merit. Care
Basic Principles - Micronutrient Support n Magnesium n n n Involved in 300 enzyme systems Important for protein metabolism Low levels can occur with diuretics, vomiting, diarrhea, stress on the body Important in glucose and blood pressure control RDA is 280 -350 mg n n Iron n n Unprocessed whole grains, legumes, buts, chocolate, dark green vegetables, and bananas Merit. Care Involved in the electron transport chain, oxidative burst in phagocytosis, part of hemoglobin which transports oxygen to tissues Inadequate iron decreases oxygen delivery to tissues & impairs the ability of leukocytes to kill bacteria, increasing risk of wound infection RDA is 8 mg/day for men and postmenopausal women, 18 mg/day for premenopausal women Iron supplementation should NOT be given to individuals with an active infection-can make it worse Bacteria will use the iron-making it more difficult to fight the infection
Basic Principles- Micronutrient Support n Arginine n n Plays a role in lymphocyte production, RNA synthesis, collagen disposition, improved tensile wound strength, and bacterial killing by macrophages. 17 to 24 g/day for two weeks will improve the wound strength and collagen deposition in artificial wounds Still need to meet energy and protein needs Not for everyone especially those with renal and liver dysfunction. Kline, Dale A. Healing From the Inside Out. Today’s Dietitian (2008): 12 -17.
Basic Principles- Micronutrient Support n Glutamine n n n Plays a central role in many of the metabolic pathways involved in wound healing- acting as a building block or substrate for many rapidly proliferating cells in the healing process RDA is 0. 57 g/kg of body weight/day in divided doses Should NOT be given to people with renal or liver impairments
Basic Principles- Micronutrient Support n Fluids n n n n Too little fluid impairs wound healing-same as too much Dehydrations reduces the supply of oxygen & nutrients to the wound Over hydration compromises the integrity of the skin and slows the inflammatory phase of wound healing RDA is minimum of 1, 500 m. L or 30 m. L/body weight or an amount equal to kilocalorie requirements Water acts as a solvent for minerals, vitamins, amino acids, glucose-enabling them to diffuse in and out of the cells Water transports vital materials to cells and waste away from cells Maintains blood volume
Guidelines: < 10% Wt. Loss Uncomplicated Stage 1 & 2 n n n n Daily high potency vitamin-mineral 20% above RDA Vitamin C= 500 mg Vitamin A= 5000 IU Zinc sulfate = 220 mg Weekly weight Weekly wound healing measurements De. Santi, L. Involuntary Weight loss and the Nonhealing Wound. Advanced in Skin & Wound Care. 2000 Jan -Feb; Volume 13, Supplement 1: 11 -20
Guidelines: < 10% Weight loss Healing Stages 3 & 4 n n n n 2 high potency vitamin-minerals > 1. 5 g/kg a day (with a protein supplements) Vitamin C = 1 g a day Vitamin A = 400 IU Zinc sulfate = 220 mg Weight weekly Weekly wound healing measurement De. Santi, L. Involuntary Weight loss and the Nonhealing Wound. Advanced in Skin & Wound Care. 2000 Jan-Feb; Volume 13, Supplement 1: 11 -20
Guidelines: > 10% Weight Loss On going Catabolism n n n n Calories: 35 -40 kcal/kg/d Protein: 1. 5 -2. 0 g/kg/d Glutamine: 10 -20 g/d Zinc sulfate: 220 mg Oxandrolone: 10 mg Weekly weight and wound measurements De. Santi, L. Involuntary Weight loss and the Nonhealing Wound. Advanced in Skin & Wound Care. 2000 Jan -Feb; Volume 13, Supplement 1: 11 -20
Standards of Practice n n n Nutrition Monitoring Weight Laboratory Values Calorie, protein, fluids, and proper nutrient intake Wound healing
In Summary n n Pressure Ulcer is an area of the skin that breaks down when you stay in one position for too long without shifting your weight. Prevention n n Monitor your Nutrition Be active If you need to sit or be on bony parts of your body for a long time make sure its cushioned To treat pressure ulcers relieve pressure regularly n n n Don’t sit or lie on the sore Use pillows & cushions Cleaning the sore regularly See a doctor Proper nutrition
Questions
References n n n n n Bareuther, Carol M. Food to Help You Mend. Today's Diet &Nutrition (2007): 3437. Bedsores (2007): 15 Sept. 2008 http: //www. surgeryencyclopedia. com/ACe/Bedsores. html De. Santi, L. Involuntary Weight loss and the Nonhealing Wound. Advanced in Skin & Wound Care. 2000 Jan-Feb; Volume 13, Supplement 1: 11 -20 Dorner, Becky. Medical Nutrition Therapy for Pressure Ulcers (2005): 1 -9. Science Direct. Concordia College. Dorner, Becky. NPUANewly Revised Pressure P's Ulcer Staging System. Today's Dietitian (2007): 24 -25. Fleishman, Amy. Adult Wound Care. Today's Dietitian 7 (2005): 38 -42. Science Direct. EBSCO. Concordia College, Moorhead. 17 Sept. 2008. Hurd, Theresa. Nutrition and Wound-Care Management/Prevention. Wound Care Canada 2: 20 -24. Science Direct. EBSCO. Concordia College, Moorhead. 17 Sept. 2008. American Dietetics Association. "Nutrition Guidelines for Pressure Ulcers. " Kline, Dale A. Healing From the Inside Out. Today’s Dietitian (2008): 12 -17.
References n n n n Krasner, Diane. Chronic Wound Care. Baltimore: Health Management Publications, 1990. 189 -212. Lewicki, Linda & et al. (1997). Potential Risk Factors for Pressure Ulcers During Cardiac Surgery. AORN Journal, 65. 933 -942. Mackay, Douglas, and Alan L. Miller. "Nutritional Support for Wound Healing. " Alternative Medicine Review 8 (2003): 359 -377. Elsevier. EBSCO. Concordia, Moorhead. 17 Sept. 2008. Merit. Care. “Nutrition and Wound Healing. ” Sollinger, Christine. “Pressure Ulcers. ” Today’s Dietitian (1999): 31 -34. Skin Problems & Treatments Health Center: Pressure Ulcers (2007): 15 Sept. 2008 http: //www. webmd. com/skin-problems-and-treatments/tc/pressure-sores 3 M Innovation. Skin Health: A 3 M Guide to Understanding Pressure Ulcers. 1998.
References n n n n Pictures www. selectmedical. co. uk/images/Shop/pug. jpg www. usc. edu/. . . /pups/images/stage 1. gif http: //www. revolutionhealth. com/articles/stages-of-pressuresores/zm 2442 http: //catalog. nucleusinc. com/generateexhibit. php? ID=9476 www. answers. com/topic/bedsore www. napnes. org/etraining/courses. php jama. ama-assn. org/cgi/content/extract/296/8/1020
 What is miracle and morality plays
What is miracle and morality plays Wound healing nutrition handout
Wound healing nutrition handout Factors affecting wound healing ppt
Factors affecting wound healing ppt Local and systemic factors affecting wound healing
Local and systemic factors affecting wound healing Concealed stab wound
Concealed stab wound Types of inflammation
Types of inflammation Primary union wound healing
Primary union wound healing Wound healing definition
Wound healing definition Molding a person meaning
Molding a person meaning Describe the role competition plays in shaping communities.
Describe the role competition plays in shaping communities. Forecasting plays an important role in
Forecasting plays an important role in How to win a deca role play
How to win a deca role play Nonverbal communication plays an important role in
Nonverbal communication plays an important role in Dignity its essential role in resolving conflict
Dignity its essential role in resolving conflict Deca role play tips
Deca role play tips Learning activity examples
Learning activity examples Communication plays a very important role in
Communication plays a very important role in Statuses and their related roles determine
Statuses and their related roles determine Worker role azure
Worker role azure Lothar krappmann
Lothar krappmann Paronychia healing stages pictures
Paronychia healing stages pictures Hroc target
Hroc target Perkins formula fracture
Perkins formula fracture Jeremiah ancient paths
Jeremiah ancient paths Quantum edge healing institute
Quantum edge healing institute Jesus heals 10 lepers lesson
Jesus heals 10 lepers lesson Creator mantra
Creator mantra Perkins timetable fracture healing
Perkins timetable fracture healing Trauma healing centers
Trauma healing centers Institute of health and healing
Institute of health and healing When the healer needs healing
When the healer needs healing Medical sheepskin healing
Medical sheepskin healing 4 r's of fracture management
4 r's of fracture management Egyptian goddess of medicine
Egyptian goddess of medicine Diagram microscopic structure of bone
Diagram microscopic structure of bone Lessons from naaman
Lessons from naaman Hindrances to healing
Hindrances to healing Healing beyond borders
Healing beyond borders Healing miracles of jesus
Healing miracles of jesus Enaahtig healing lodge
Enaahtig healing lodge Native american healing prayers for the sick
Native american healing prayers for the sick Global quantum healing
Global quantum healing Went about doing good
Went about doing good Healing by listening to quran
Healing by listening to quran Jesus healing the lepers
Jesus healing the lepers Tandorosti
Tandorosti Marumali
Marumali Jesus healing quotes
Jesus healing quotes Gtr indications
Gtr indications Jesus healing the lepers
Jesus healing the lepers Healing is a process not an event
Healing is a process not an event