Histosminaire conjoint 27 mai 2009 Dre Katherine Grondin


















- Slides: 48
Histoséminaire conjoint 27 mai 2009 Dre Katherine Grondin Dre Jocelyne Arseneau Pathology dept, RVH Mc. Gill University
48 y. o. woman Adnexal mass, 14 cm
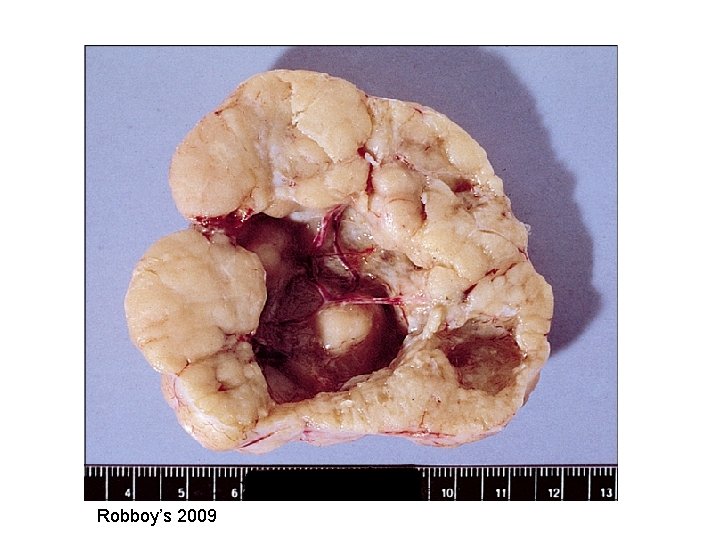
Macroscopy • 14 x 11 x 10 cm mass • Encapsulated, bosselated, multinodular with solid cut surface





Tumors of the Ovary • • • Surface epithelial tumors Germ cell tumors Sex cord-stromal tumors Germ cell sex cord-stromal tumors Rare stuff Metastasis
Tumors of the Ovary • • • Surface epithelial tumors Germ cell tumors Sex cord-stromal tumors Germ cell sex cord-stromal tumors Rare stuff Metastasis
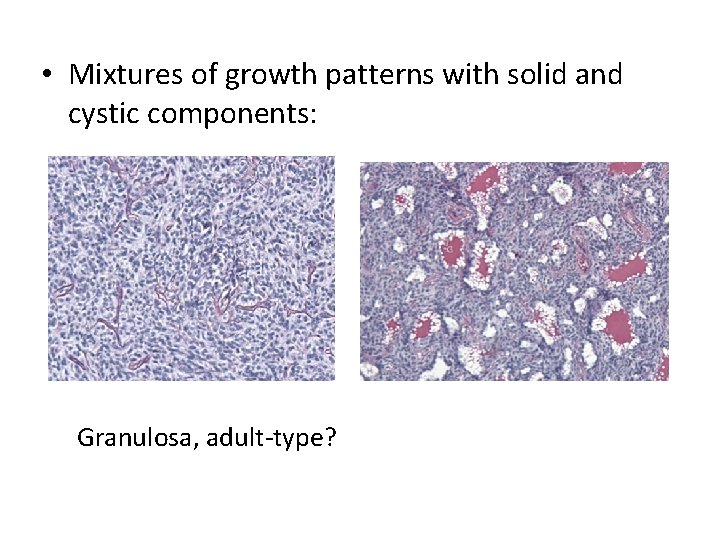
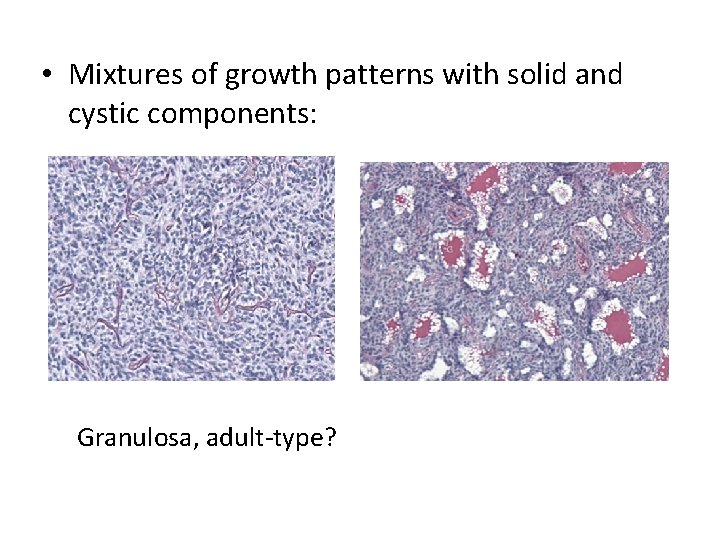
• Mixtures of growth patterns with solid and cystic components: Granulosa, adult-type?
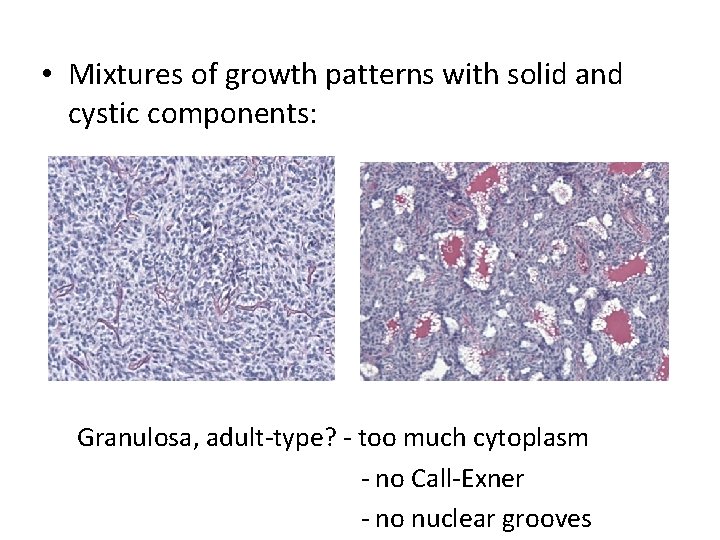
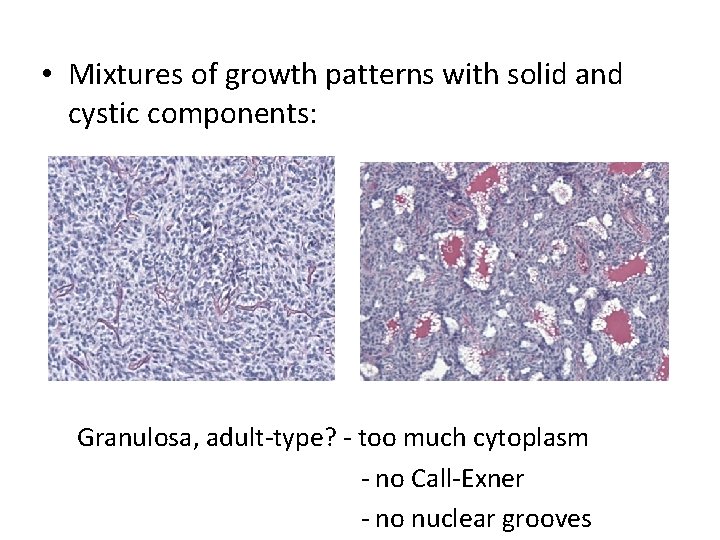
• Mixtures of growth patterns with solid and cystic components: Granulosa, adult-type? - too much cytoplasm - no Call-Exner - no nuclear grooves
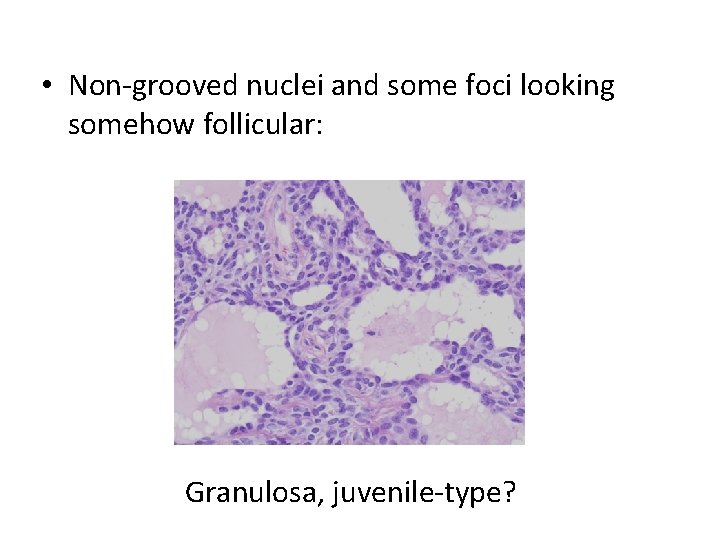
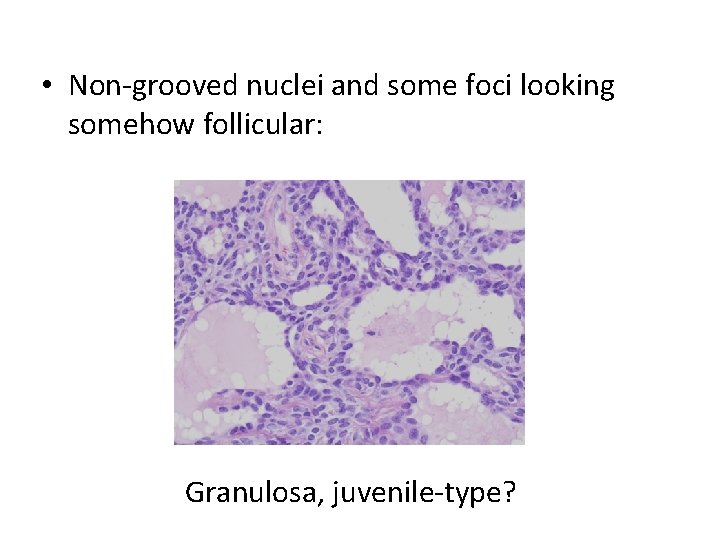
• Non-grooved nuclei and some foci looking somehow follicular: Granulosa, juvenile-type?
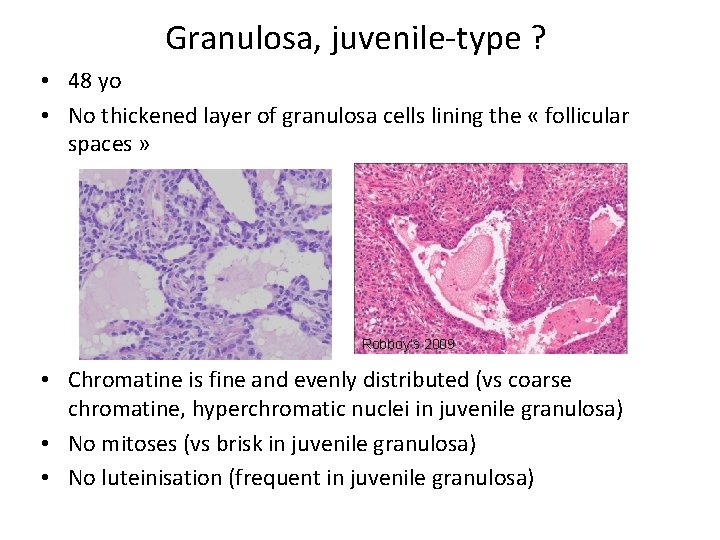
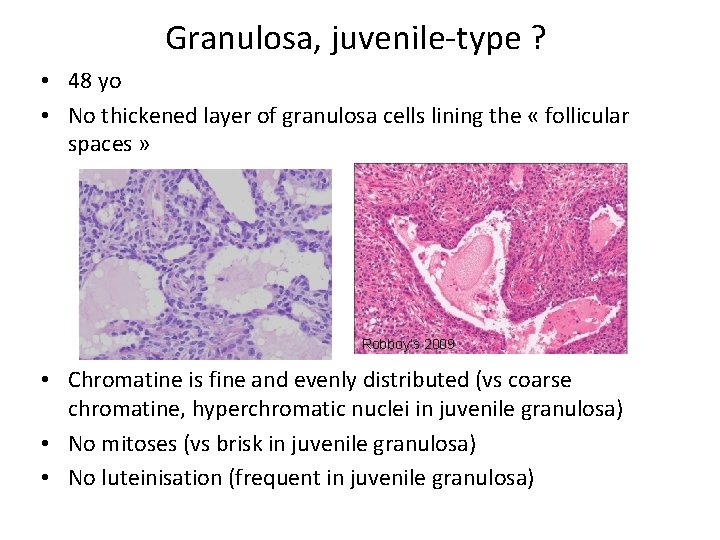
Granulosa, juvenile-type ? • 48 yo • No thickened layer of granulosa cells lining the « follicular spaces » Robboy’s 2009 • Chromatine is fine and evenly distributed (vs coarse chromatine, hyperchromatic nuclei in juvenile granulosa) • No mitoses (vs brisk in juvenile granulosa) • No luteinisation (frequent in juvenile granulosa)
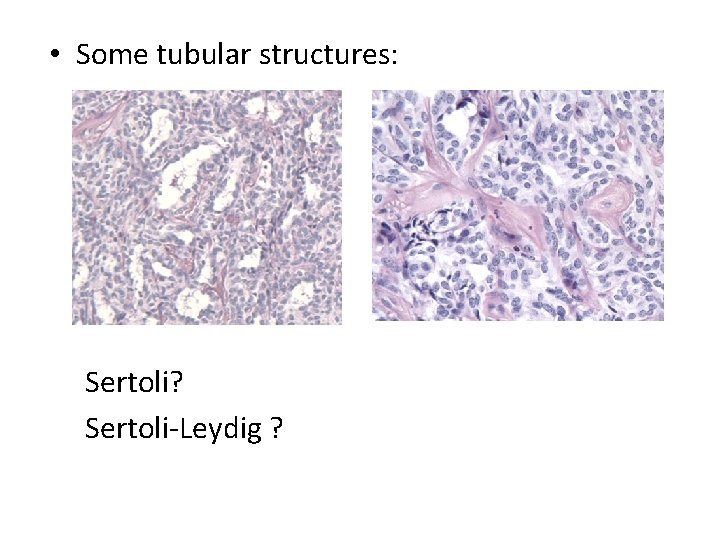
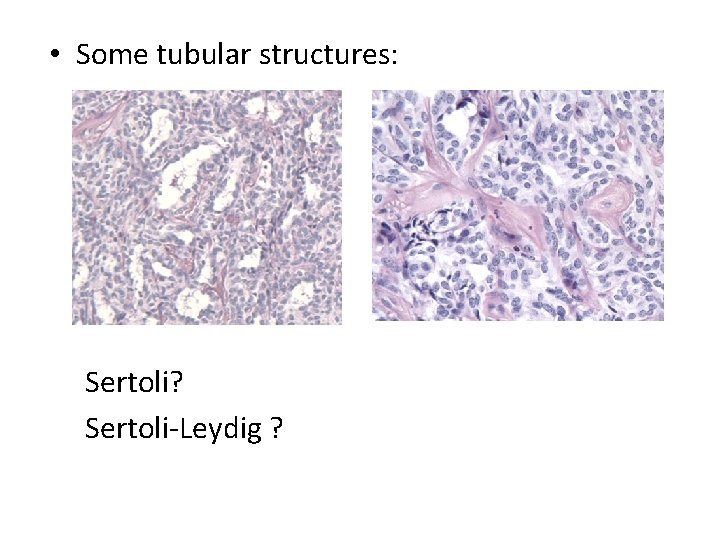
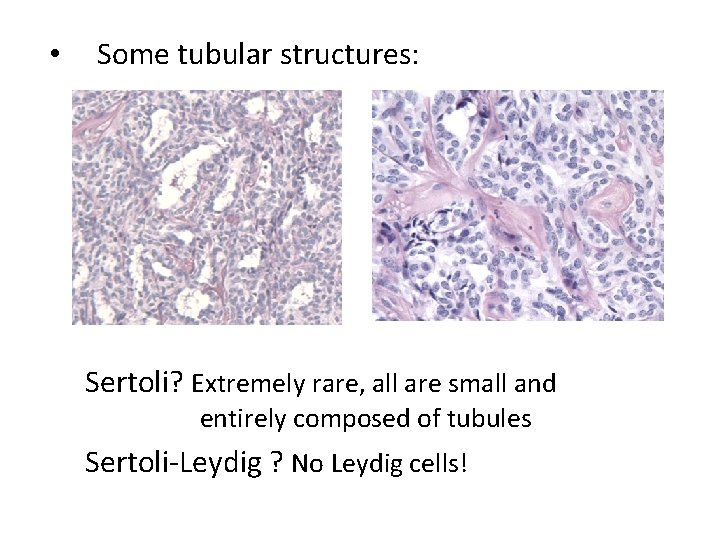
• Some tubular structures: Sertoli? Sertoli-Leydig ?
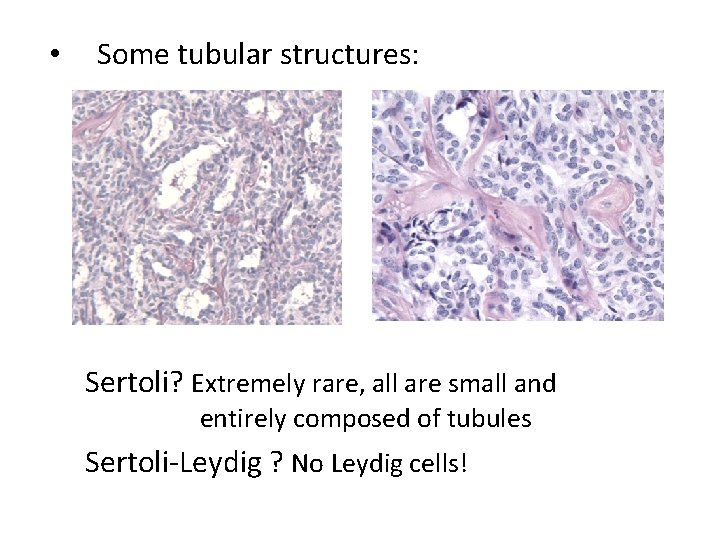
• Some tubular structures: Sertoli? Extremely rare, all are small and entirely composed of tubules Sertoli-Leydig ? No Leydig cells!

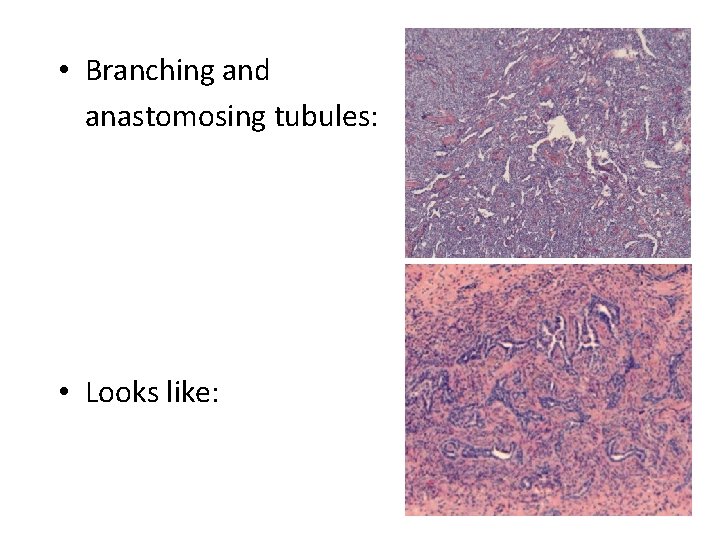
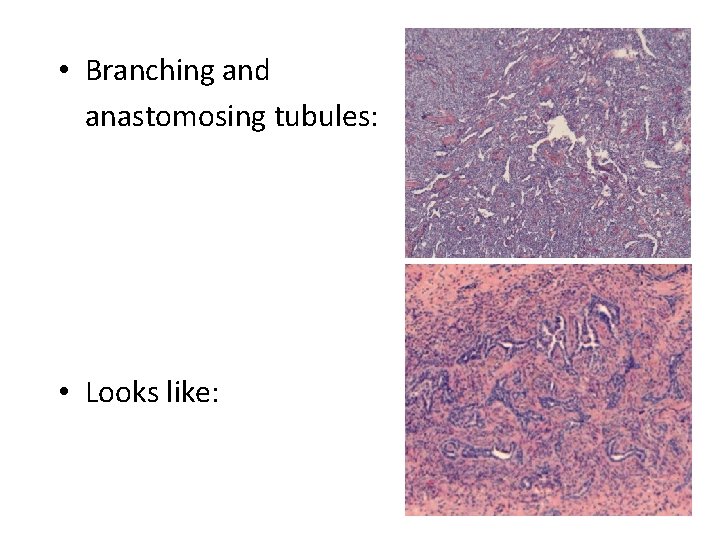
• Branching and anastomosing tubules: • Looks like:
Tumors of the rete ovarii • Cystadenomas, papillary cystadenomas • Rete adenoma • Rete carcinoma • or maybe retiform Sertoli-Leydig Cell tumor
Rete adenoma • Growth patterns described are only tubular and papillary • No solid, no sieve-like patterns


• Looks sex-cord stromal • Looks like rete ovarii • With intraluminal thick eosinophilic secretions
Female adnexal tumor of probable wolffian origin (FATWO) – Most are described in the broad ligament, extremely rare in the ovary

Macroscopy • 14 x 11 x 10 cm mass • Encapsulated, bosselated, multinodular with solid cut surface • Attached to the broad ligament • Totally separated from the ovary (partially cystic, 6 x 4 x 2 cm)
Female Adnexal Tumor of probable Wolffian Origin (FATWO) • First described in 1973 by Kariminejad and Scully • Less 80 cases reported (17 to 83 yrs) • Most benign but ~ 10 cases malignant • All unilateral most often between the leaves of the broad ligament or attached to it or to the fallopian tube by a pedicle • Rare examples in the ovary (rete) and paravaginal
In favor of a wolffian origin • Their location: broad ligament, paratubal, ovary (rete) and paravaginal (where wolffian remnants are located) • Exclusion of other possibilities • Microscopic appearance compatible with such an origin • Compatible IHC (Hum Pathol 1999, 30: 856 -863 (25 cases); Histopathology 2001, 38: 237 -242 (6 cases))

Macroscopy • • 0. 5 -18 cm Cut surface solid or solid and cystic Gray-white to tan or yellow, firm or rubbery Hemorrhage and necrosis occasionally
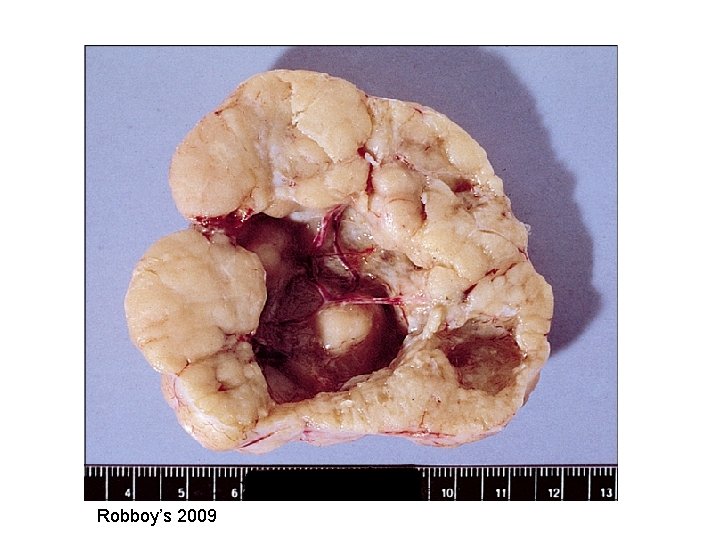
Robboy’s 2009
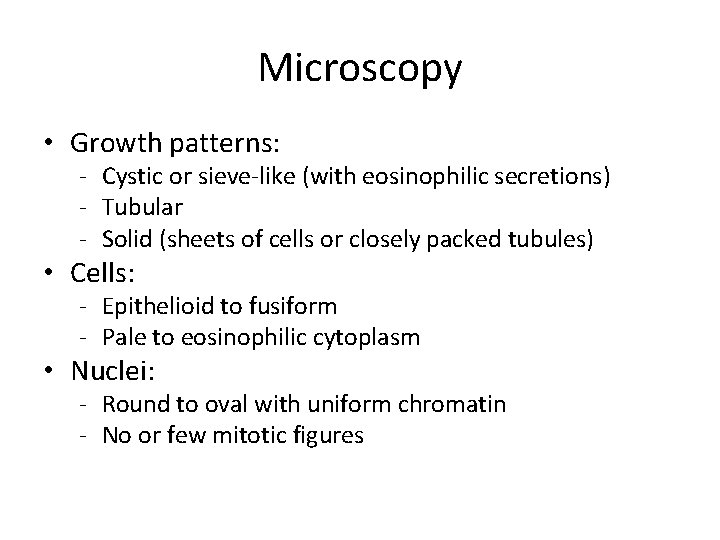
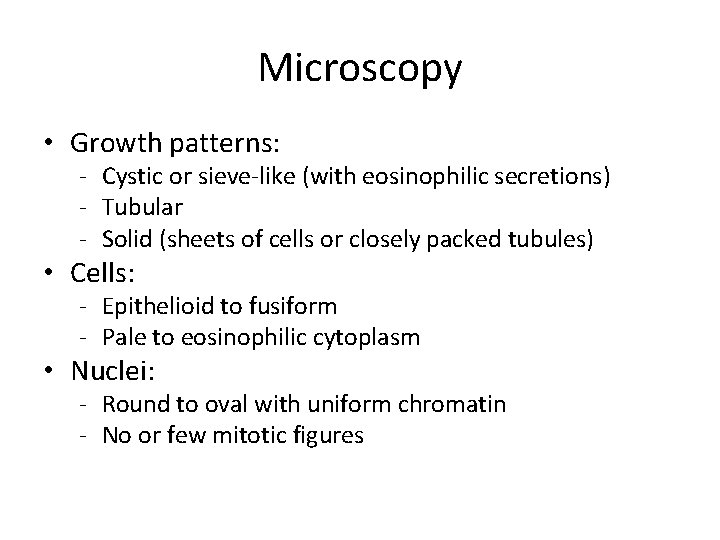
Microscopy • Growth patterns: - Cystic or sieve-like (with eosinophilic secretions) - Tubular - Solid (sheets of cells or closely packed tubules) • Cells: - Epithelioid to fusiform - Pale to eosinophilic cytoplasm • Nuclei: - Round to oval with uniform chromatin - No or few mitotic figures
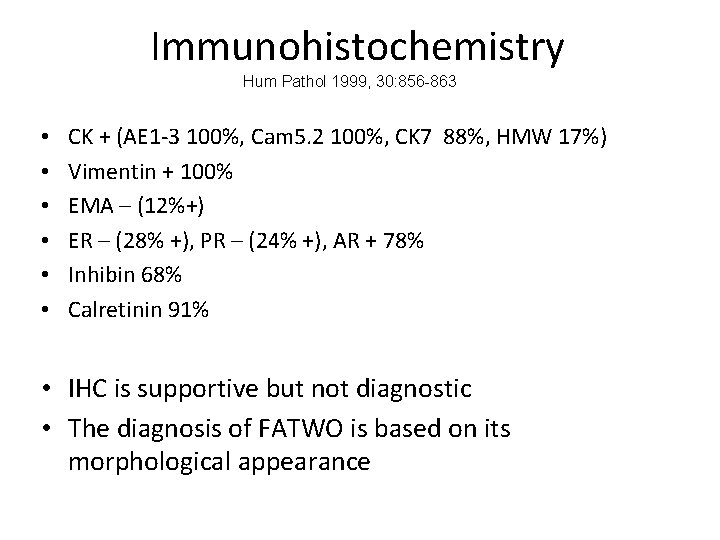
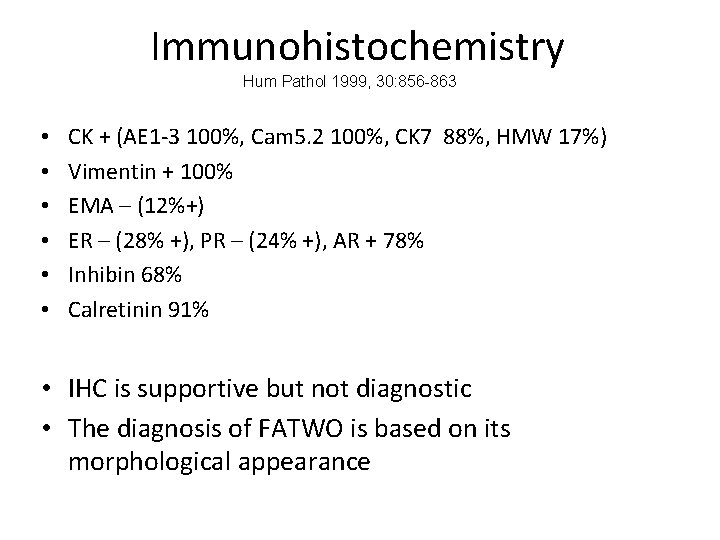
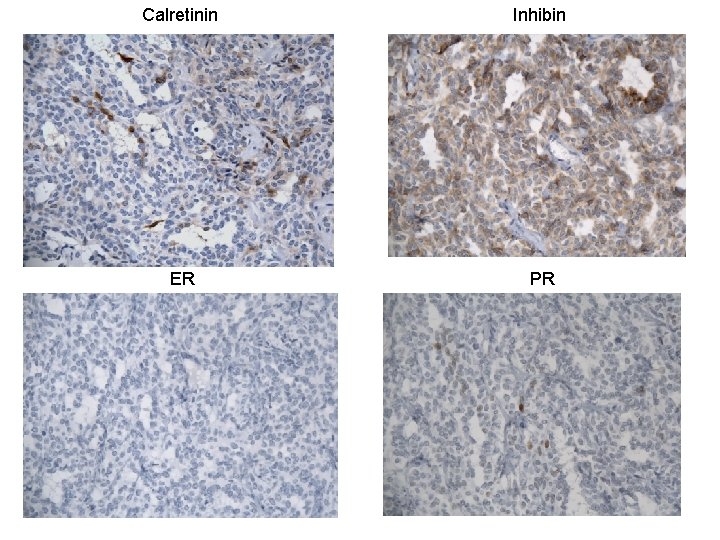
Immunohistochemistry Hum Pathol 1999, 30: 856 -863 • • • CK + (AE 1 -3 100%, Cam 5. 2 100%, CK 7 88%, HMW 17%) Vimentin + 100% EMA – (12%+) ER – (28% +), PR – (24% +), AR + 78% Inhibin 68% Calretinin 91% • IHC is supportive but not diagnostic • The diagnosis of FATWO is based on its morphological appearance

AE 1 -3 EMA Vimentin
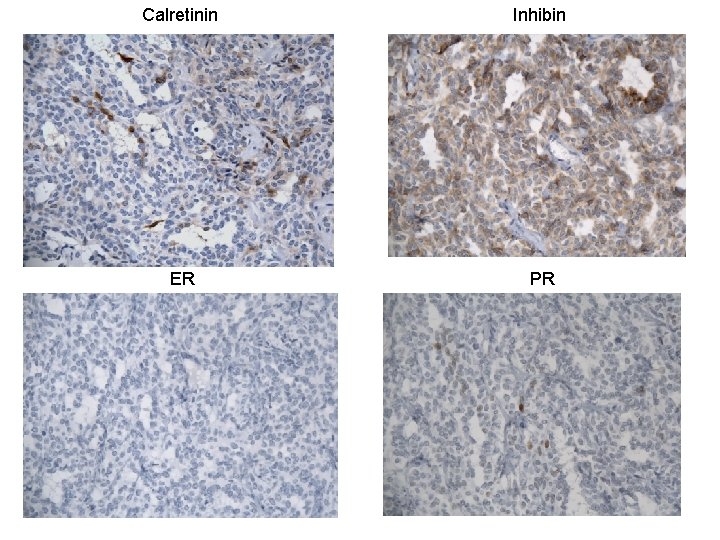
Calretinin Inhibin ER PR
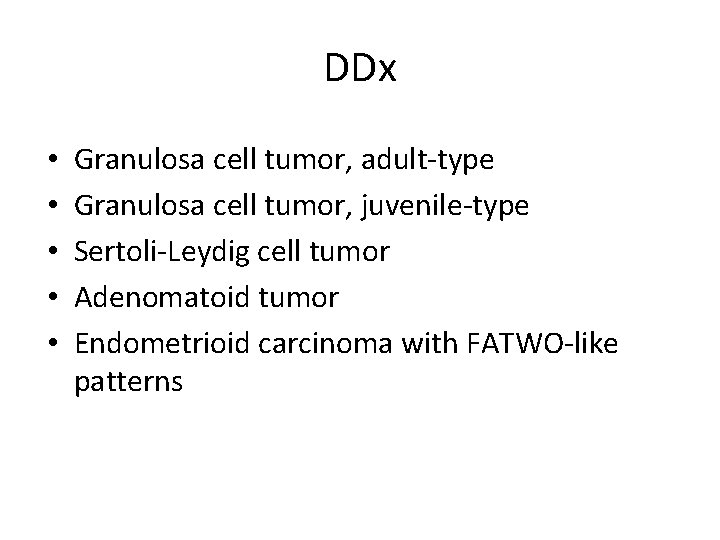
DDx • • • Granulosa cell tumor, adult-type Granulosa cell tumor, juvenile-type Sertoli-Leydig cell tumor Adenomatoid tumor Endometrioid carcinoma with FATWO-like patterns
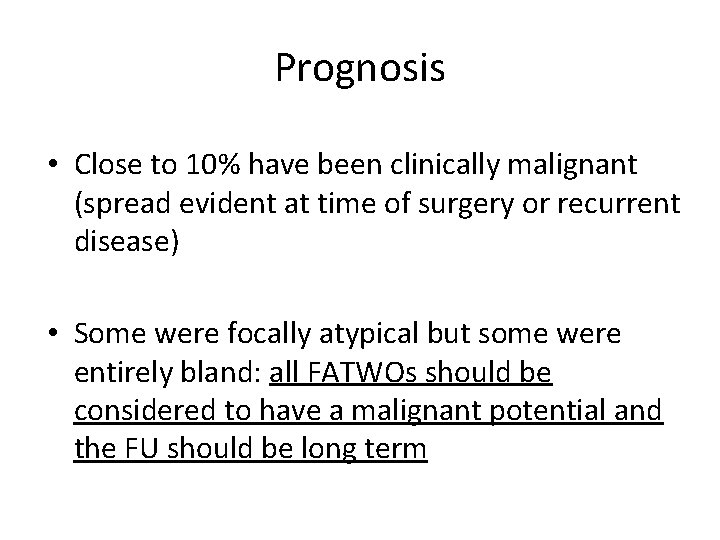
Prognosis • Close to 10% have been clinically malignant (spread evident at time of surgery or recurrent disease) • Some were focally atypical but some were entirely bland: all FATWOs should be considered to have a malignant potential and the FU should be long term
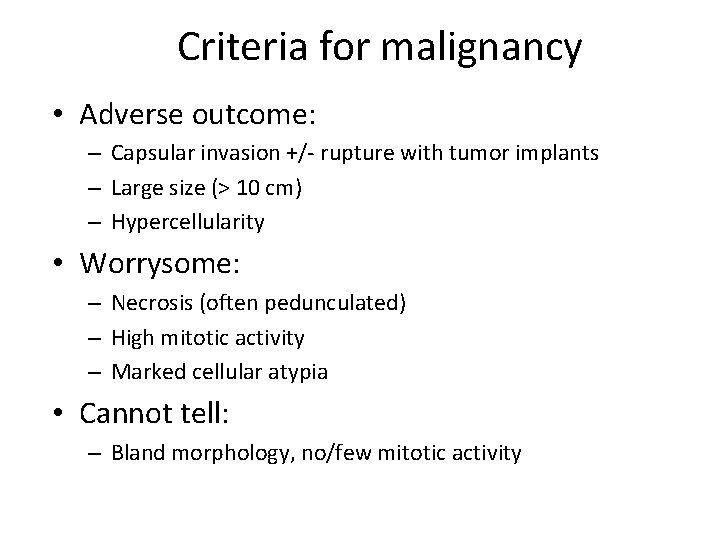
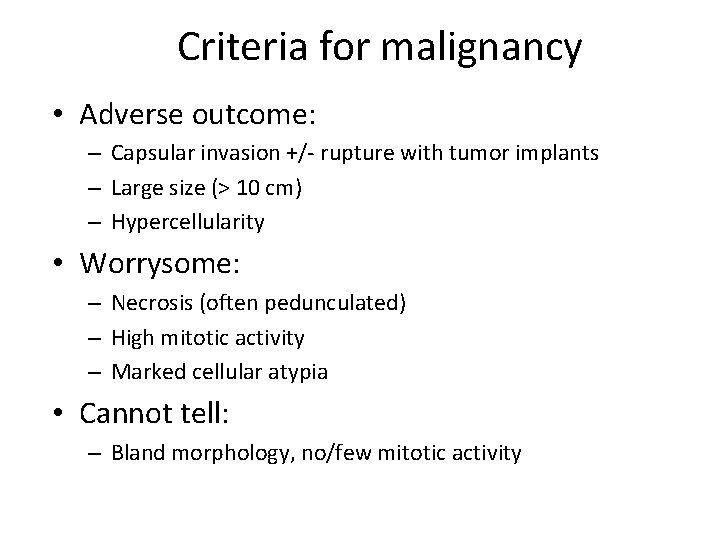
Criteria for malignancy • Adverse outcome: – Capsular invasion +/- rupture with tumor implants – Large size (> 10 cm) – Hypercellularity • Worrysome: – Necrosis (often pedunculated) – High mitotic activity – Marked cellular atypia • Cannot tell: – Bland morphology, no/few mitotic activity
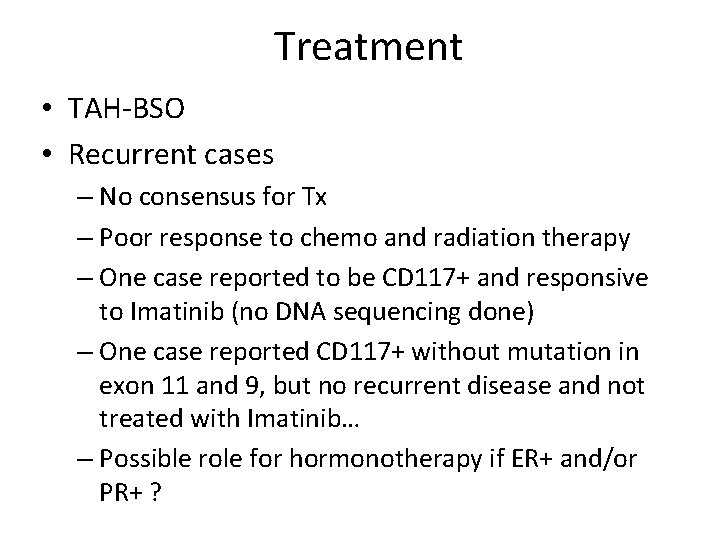
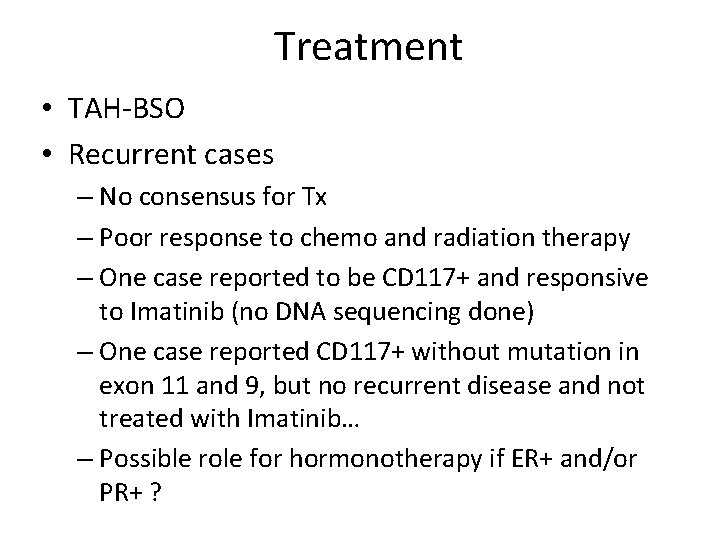
Treatment • TAH-BSO • Recurrent cases – No consensus for Tx – Poor response to chemo and radiation therapy – One case reported to be CD 117+ and responsive to Imatinib (no DNA sequencing done) – One case reported CD 117+ without mutation in exon 11 and 9, but no recurrent disease and not treated with Imatinib… – Possible role for hormonotherapy if ER+ and/or PR+ ?
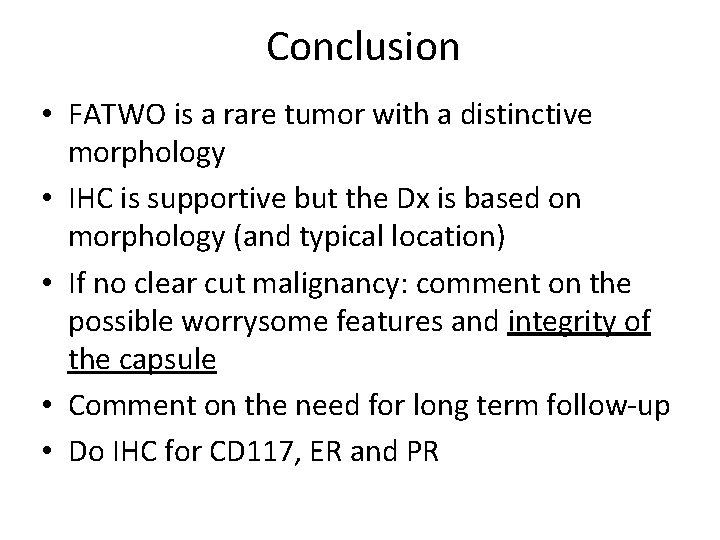
Conclusion • FATWO is a rare tumor with a distinctive morphology • IHC is supportive but the Dx is based on morphology (and typical location) • If no clear cut malignancy: comment on the possible worrysome features and integrity of the capsule • Comment on the need for long term follow-up • Do IHC for CD 117, ER and PR
Merci!




Granulosa, adult-type? No Call-Exner No grooves!
Retiform SLCT • In favor: have retiform pattern and can also have sieve-like pattern BUT: • Retiform SLCT occur at a young age (mean 17 yrs) • Insular, lobulated growth pattern at low power • All are moderately or poorly differentiated SCLT with a component of loose fibrous or fibromyxoid mesenchymal stroma containing Leydig cells separating the epithelial nodules • Almost half of the Retiform variant have heterologous element
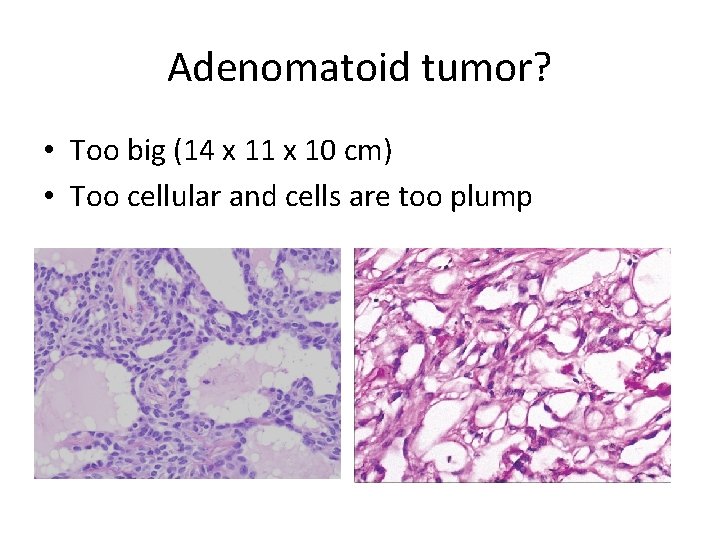
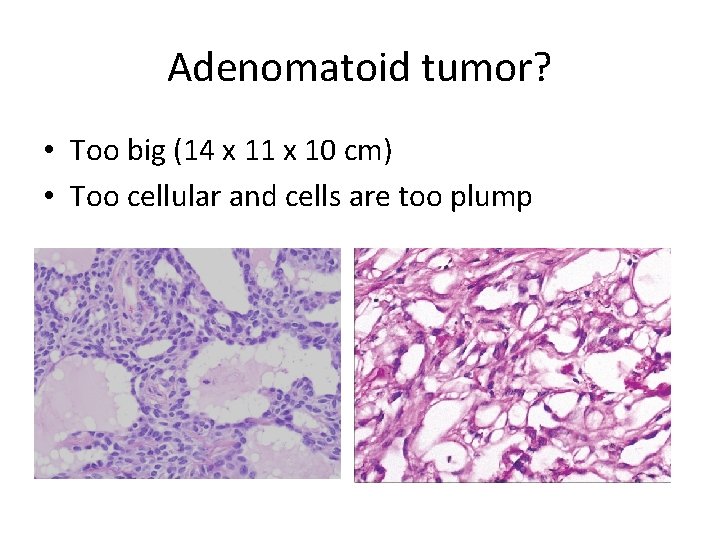
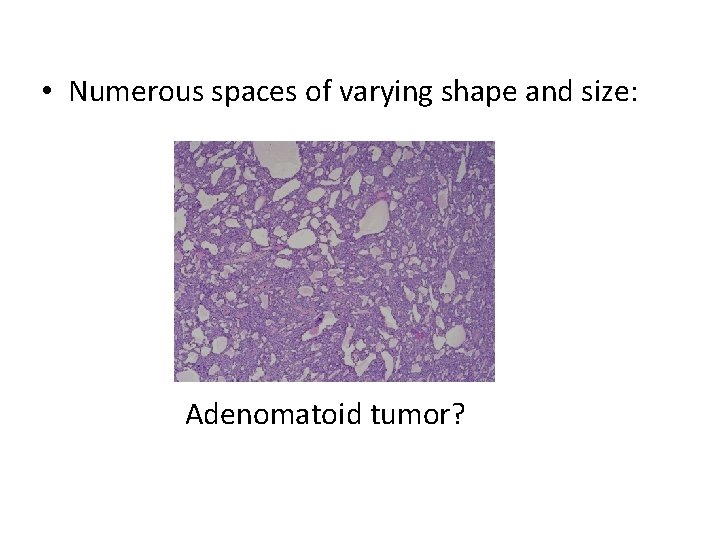
Adenomatoid tumor? • Too big (14 x 11 x 10 cm) • Too cellular and cells are too plump

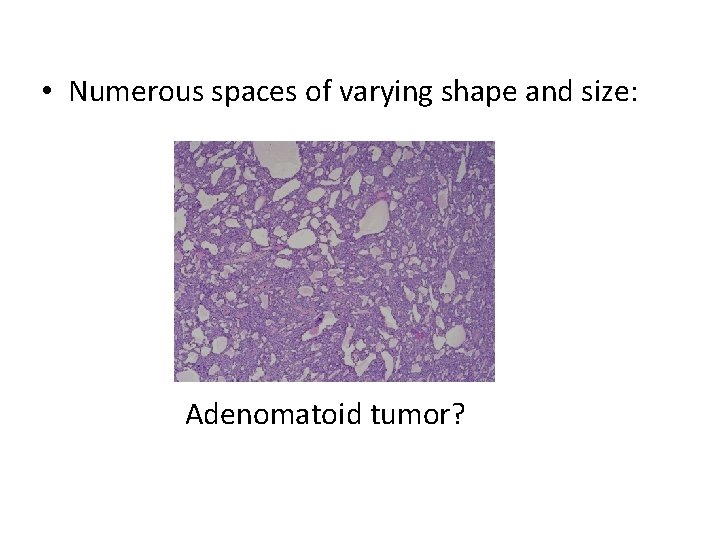
• Numerous spaces of varying shape and size: Adenomatoid tumor?

Adenomatoid tumor? • Too big (14 x 11 x 10 cm) • Cells lining the cystic spaces are too plump

 27 mai 2009
27 mai 2009 Denis grondin
Denis grondin Reo
Reo Mai sus mai sus
Mai sus mai sus Sirul numerelor naturale
Sirul numerelor naturale Decp
Decp Personas gramaticales
Personas gramaticales Dre 12 step process
Dre 12 step process Palabras con pra
Palabras con pra Dre.ca.gov
Dre.ca.gov Se dre
Se dre Drug recognition expert chart
Drug recognition expert chart Logos con z
Logos con z Dre 12 steps
Dre 12 steps Coverings of direct inguinal hernia
Coverings of direct inguinal hernia Conjoint malady in repertory
Conjoint malady in repertory C'est quoi un pronom personnel
C'est quoi un pronom personnel Conjoint analysis output
Conjoint analysis output Applied conjoint analysis
Applied conjoint analysis Conjoint analysis sample size rule of thumb
Conjoint analysis sample size rule of thumb Conjoint analyse vor und nachteile
Conjoint analyse vor und nachteile Adaptive choice based conjoint
Adaptive choice based conjoint Multiplikative preisabsatzfunktion
Multiplikative preisabsatzfunktion Sawtooth conjoint analysis
Sawtooth conjoint analysis Conjoint family drawing
Conjoint family drawing Sustainability conjoint
Sustainability conjoint Conjoint analysis sample size rule of thumb
Conjoint analysis sample size rule of thumb Stata conjoint analysis
Stata conjoint analysis Divergence neurons
Divergence neurons Priyanka ps
Priyanka ps Gabrielle roy conjoint
Gabrielle roy conjoint Applied conjoint analysis
Applied conjoint analysis Conjoint premises
Conjoint premises Conjoint premises
Conjoint premises Marketing analytics software r
Marketing analytics software r Al pacino conjoint
Al pacino conjoint Shutter mechanism of inguinal canal
Shutter mechanism of inguinal canal Videsk
Videsk Conjoint analysis in r
Conjoint analysis in r Katherine hobbs knutson
Katherine hobbs knutson Katherine yuen
Katherine yuen Eecs 183
Eecs 183 The last dog by katherine paterson
The last dog by katherine paterson Pearl fulton bliss
Pearl fulton bliss Katherine mahoney ospi
Katherine mahoney ospi The last dog katherine paterson
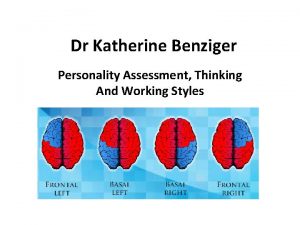
The last dog katherine paterson Katherine benziger
Katherine benziger Jordana abraham
Jordana abraham Katherine thornton statement
Katherine thornton statement