HELP Strategies for Delirium Prevention The Hospital Elder
- Slides: 22
HELP Strategies for Delirium Prevention The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
HELP Project Planning Tool In this section think about…. Will you start with some or all of the HELP interventions? What HELP interventions will your system find most challenging? What strategies will you use to support their introduction? The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
HELP Protocols The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
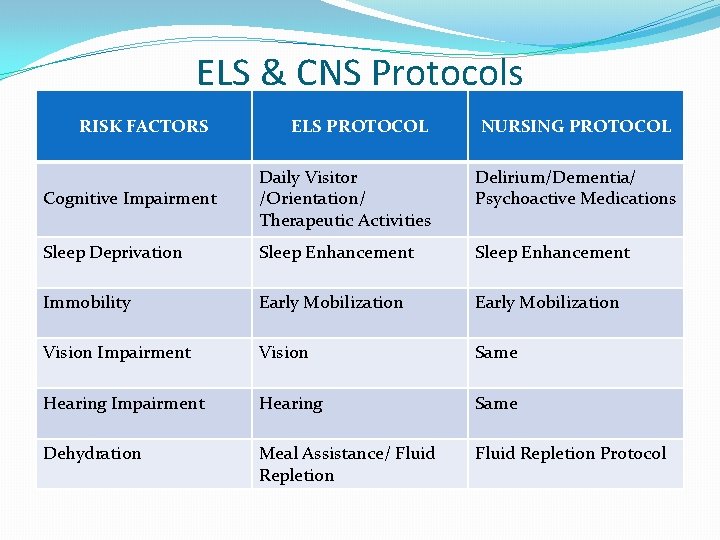
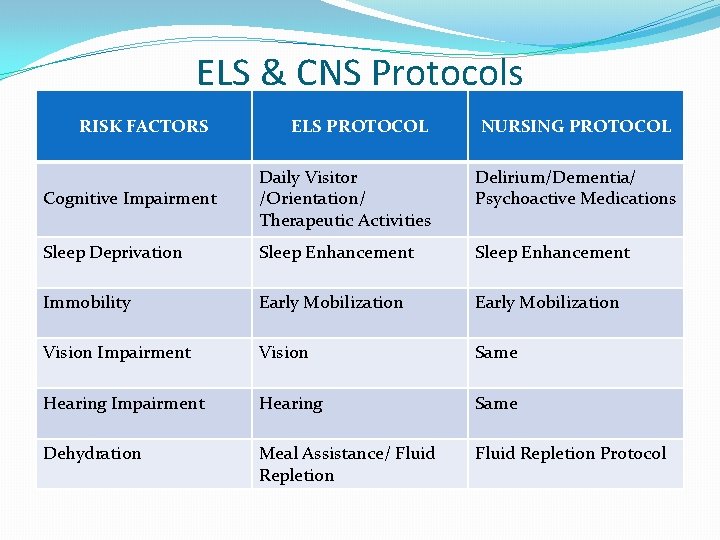
ELS & CNS Protocols RISK FACTORS ELS PROTOCOL NURSING PROTOCOL Cognitive Impairment Daily Visitor /Orientation/ Therapeutic Activities Delirium/Dementia/ Psychoactive Medications Sleep Deprivation Sleep Enhancement Immobility Early Mobilization Vision Impairment Vision Same Hearing Impairment Hearing Same Dehydration Meal Assistance/ Fluid Repletion Protocol
Orientation/Daily Visitor/Therapeutic Activities Criteria- all patients are enrolled Intervention-Orient 1 time per day if SMMSE >20, orient 3 times per day if SMMSE <20 -Explore patient’s interests and possible therapeutic activities -Discuss current events, structured reminiscence, word games (Inouye et al. N. Engl. J. Med. 1999, March 4 340 (9): 669 -676) The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
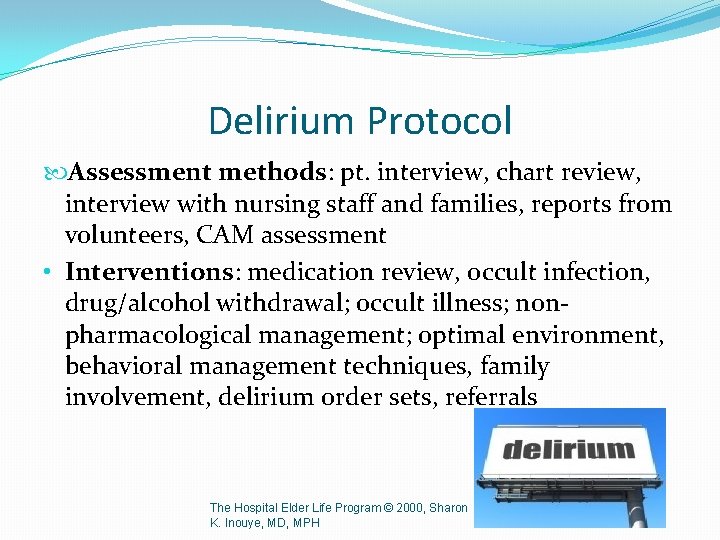
Delirium Protocol Assessment methods: pt. interview, chart review, interview with nursing staff and families, reports from volunteers, CAM assessment • Interventions: medication review, occult infection, drug/alcohol withdrawal; occult illness; nonpharmacological management; optimal environment, behavioral management techniques, family involvement, delirium order sets, referrals The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
More Delirium Interventions Non-Pharmacological Management Education for staff, involve family Optimal environment Strategies to decrease agitation and improve sleep Communication techniques The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
Dementia Protocol • Baseline cognitive status • Baseline screening information (social situation/caregiving needs/ADLs/IADLs/ nutrition, sleep) • Interventions (medical workup, effective behavioral management strategies, nursing education, avoiding psychoactive medications) The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
Psychoactive Medication Protocol Past and current medication use Screening for medications associated with delirium Anticholinergic Cognitive Burden scale Nursing staff education The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
Healthy Vision/Healthy Hearing Vision Criteria- if near vision in both eyes <20/70 Intervention - Eyeglasses clean and on - Magnifying glass Hearing Criteria-<3 whispers from each ear on whisper test Intervention -Hearing aids in and turned on -Consider use of hearing amplifier The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
Healthy Eating/Fluid Repletion Criteria-appetite rated as poor Criteria-clinical evidence of Interventiondehydration and Assist with set-up of meals Urea X 10/Creatinine> 0. 7 Encourage food intake Intervention- Encourage fluids Ensure regular mouth care if not contraindicated Assist with menu completion The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
Fluid Repletion Protocol Assessment: criter; risk factors, postural hypotension Interventions: patient/family education re: fluid intake and postural hypotension; collaboration with nursing and medical staff; direction for volunteers, patient preference ; collaboration with physician if symptoms persist The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
Poor Appetite Further assessment by CNS: Physical appearance Weight loss etiology Weight loss markers CNS’ Interventions: Referrals to RD, OT, MD Communication with nursing staff Communication with families The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
Early Mobilization Criteria- all patients assessed for early mobilization Intervention ELS/CNS consults with Physiotherapist to determine appropriate mobilization protocol: Active range of motion exercises 3 times per day Supervised walking 3 times per day according to PT guidelines The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
Early Mobilization –CNS role Assessment: patient’s self-report of functional abilities, direct mobility assessment, physician order, hospital staff assessment, pain and pain management assessment Intervention: referral to Physiotherapist/OT, patient/family education, staff education (deconditioning, falls prevention) The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
Sleep Enhancement Criteria- difficulty falling asleep or sleeps poorly at home or in hospital Intervention Avoid sleeping pills Instead: Back rub/ hand rub (if not contraindicated) Warm blanket Warm drink such as herbal tea or warm milk Soft music The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
Sleep protocol –CNS role Risk factors Medication Patient/family education on sleep hygiene practices: q. Increase physical activity during the day q. Avoid naps q. Limit caffeine, nicotine intake q. Have light snack before going to bed q. No TV before going to bed The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
At HHS, the HELP nurse ……. Follows HELP delirium protocols Structured cognitive assessment is not carried out daily but on admission and as indicated SMMSE is not done prior to discharge The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
Adherence-What dose of HELP is enough ? The Role of Adherence on the Effectiveness of Nonpharmacologic Interventions Higher levels of adherence resulted in reduced rates of delirium in a directly graded fashion, with extremely low levels of delirium in the highest adherence group. Inouye SK. Arch Intern Med. 2003; 163: 958 -964 The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
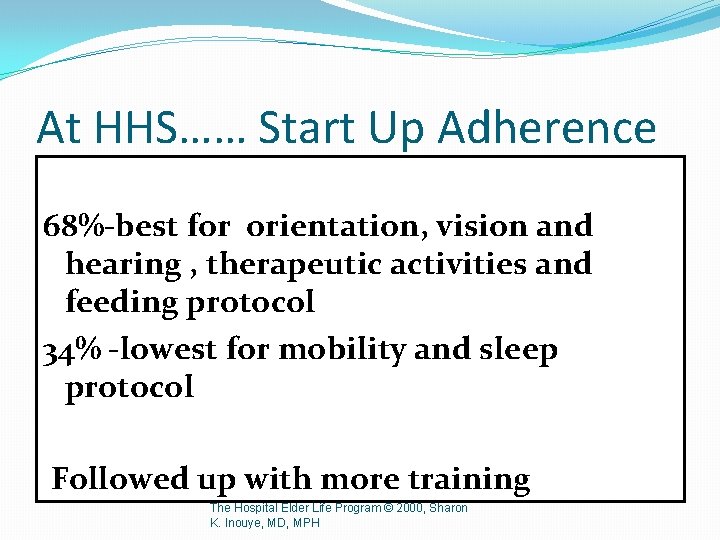
At HHS…… Start Up Adherence 68%-best for orientation, vision and hearing , therapeutic activities and feeding protocol 34% -lowest for mobility and sleep protocol Followed up with more training The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
What factors affect adherence? Are they modifiable? The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
HELP Project Planning Tool Will you start with some or all of the HELP interventions? What HELP interventions will your system find most challenging? What strategies will you use to support their introduction? The Hospital Elder Life Program © 2000, Sharon K. Inouye, MD, MPH
 Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention The hospital elder life program
The hospital elder life program Francisco fernandez md
Francisco fernandez md Flocculation delirium
Flocculation delirium Cam icu escala
Cam icu escala Excited delirium перевод
Excited delirium перевод Sindrom delirium akut
Sindrom delirium akut Gcs somnolen
Gcs somnolen Delirium care pathways
Delirium care pathways Escala rass
Escala rass Nash delirium
Nash delirium Types of amnesia
Types of amnesia Delirium definition
Delirium definition Lucie big delirium
Lucie big delirium Delirium case presentation
Delirium case presentation Terminalt delirium
Terminalt delirium Driver diagram palliative care
Driver diagram palliative care Delirium definition
Delirium definition Difference between dementia and delirium
Difference between dementia and delirium Help us help you
Help us help you Spagetti poem
Spagetti poem Help im being oppressed
Help im being oppressed Question maker face asl
Question maker face asl