Health Center Response to the COVID19 Pandemic The




- Slides: 33
Health Center Response to the COVID-19 Pandemic & The Rural Healthcare Surge Readiness Web Portal Renée Joskow, DDS, MPH, FAGD, FACD, FICD Chief Dental Officer January 21, 2021 Christina Lachance, MPH Bureau of Primary Health Care (BPHC)
Rural Health Webinar Series Title of Presentation: Health Center Response to the COVID-19 Pandemic & The Rural Healthcare Surge Readiness Web Portal Date: January 21, 2021 Presenter(s): Renée Joskow DDS, MPH, FAGD, FACD, FICD Presenter(s) Title/Affiliation: Chief Dental Officer, Health Resources and Services Administration LEARNING OBJECTIVES At the conclusion of this activity, participants will be able to: 1. 2. 3. Summarize COVID-19 specific data collected from rural health centers in New England Reflect on the best practices and innovations implemented by health centers in response to the COVID-19 public health emergency Navigate the Rural Healthcare Surge Readiness web portal to access essential resources, training, and tools to prepare for and respond to COVID-19
Planning Committee & Presenter Declarations The following planning committee members and presenter(s) have disclosed financial interest/arrangements or affiliations with organization(s) that could be perceived as a real or apparent conflict of interest in the context of the subject of their presentation(s). The following *planner(s)/presenter(s) of this activity have disclosed no relevant personal or financial relationships with any commercial interests pertaining to this activity: *Marguerite Urban, MD; *Sara Wall Bollinger, MA; *Ann Marie Day, MBA; *Ashleigh Mc. Gowan, MS Renée Joskow DDS, MPH, FAGD, FACD, FICD
Accreditation/Certification Statements This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of the University of Rochester School of Medicine and Dentistry and New England Rural Health Association, the NYS Association for Rural Health and the Foundation for Community Health. The University of Rochester School of Medicine and Dentistry is accredited by the ACCME to provide continuing medical education for physicians. The University of Rochester School of Medicine and Dentistry designates this live activity for a maximum of 1. 00 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. University of Rochester Medical Center, Center for Experiential Learning is recognized by the New York State Education Department's State Board for Social Work as an approved provider of continuing education for licensed social workers #SW-0005. This course has been approved for 1. 00 contact hours No commercial funding was received to support this activity. ACCME Standards of Commercial Support of CME require that presentations be free of commercial bias and that any information regarding commercial products/services be based on scientific methods generally accepted by the medical community. When discussing therapeutic options, faculty are requested to use only generic names. If they use a trade name, then those of several companies should be used. If a presentation includes discussion of any unlabeled or investigational use of a commercial product, faculty are required to disclose this to the participants.
Health Center Response to the COVID-19 Pandemic & The Rural Healthcare Surge Readiness Web Portal January 21, 2021 New England Rural Health Association & New York State Association for Rural Health Renée Joskow, DDS, MPH, FAGD, FACD, FICD Chief Dental Officer Christina Lachance, MPH Bureau of Primary Health Care (BPHC) Health Resources and Services Administration (HRSA)
Today’s Presentation • HRSA’s Health Center Program • Health Centers’ Response to COVID-19 § Funding and response activities § National data § Rural New England health center data • COVID-19 Response Overview: Healthcare Resilience Working Group • Rural Healthcare Surge Readiness Web Portal 6
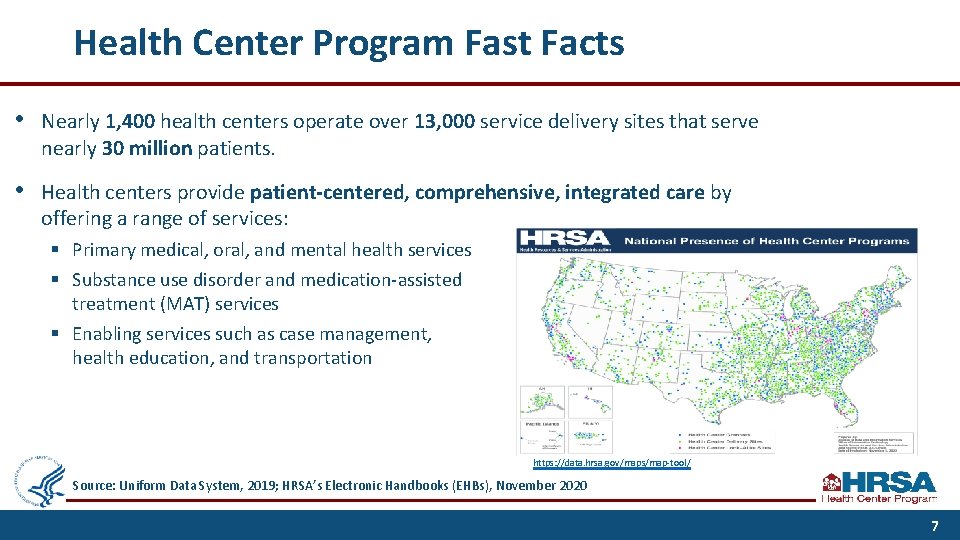
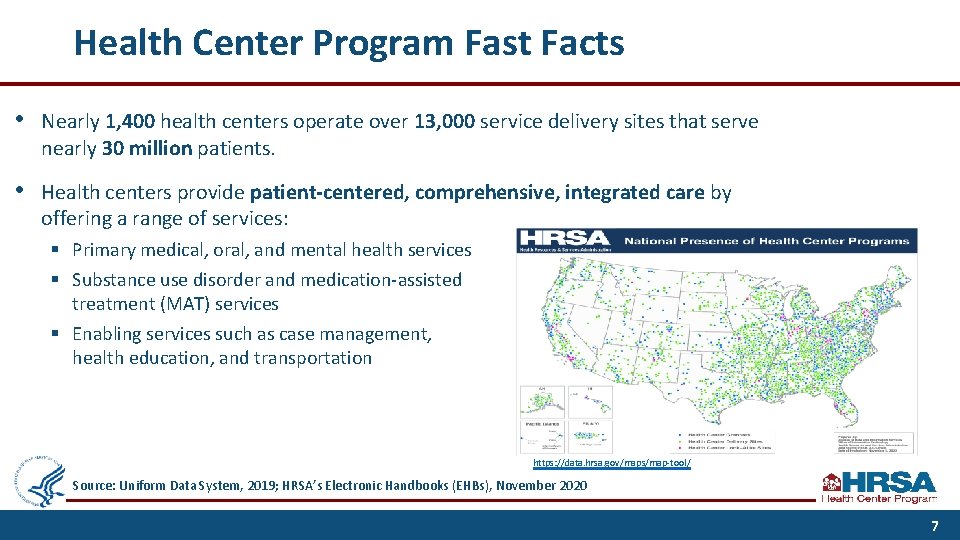
Health Center Program Fast Facts • Nearly 1, 400 health centers operate over 13, 000 service delivery sites that serve nearly 30 million patients. • Health centers provide patient-centered, comprehensive, integrated care by offering a range of services: § Primary medical, oral, and mental health services § Substance use disorder and medication-assisted treatment (MAT) services § Enabling services such as case management, health education, and transportation https: //data. hrsa. gov/maps/map-tool/ Source: Uniform Data System, 2019; HRSA’s Electronic Handbooks (EHBs), November 2020 7
Health Center Program Fundamentals Serve High Need Areas Patient Directed • Must serve a high need community or population (e. g. , HPSA, MUA/P) • Private non-profit or public agency that is governed by a patient-majority community board Comprehensive No One is Turned Away • Provide comprehensive primary care and enabling services (e. g. , education, outreach, and transportation services) • Services are available to all, with fees adjusted based upon ability to pay Collaborative Accountable • Collaborate with other community providers to maximize resources and efficiencies in service delivery • Meet performance and accountability requirements regarding administrative, clinical, and financial operations The Health Center Program is authorized under Section 330 of the Public Health Service (PHS) Act. 8

Health Centers Serve a High Proportion of Low-Income, Minority, Uninsured, and Homeless Patients 100% 91, 1% 80% 59, 0% 60% 40% 28, 9% 27, 8% 22, 7% 20% 0% 9, 1% At or Below 200% of Poverty Racial/Ethnic Minority U. S. Population (2018) Uninsured 0, 2% 4, 9% Homeless Health Center Patient Population (2019) Health center source: Uniform Data System, 2019. National data: https: //www. census. gov/data/tables/time-series/demo/income-poverty/cps-pov/pov-01. 2018. html https: //data. census. gov/cedsci/profile? q=United%20 States&g=0100000 US – excluding “White alone” population https: //www. census. gov/data/tables/time-series/demo/income-poverty/cps-hi/hi. html https: //www. huduser. gov/portal/sites/default/files/pdf/2019 -AHAR-Part-1. pdf 9
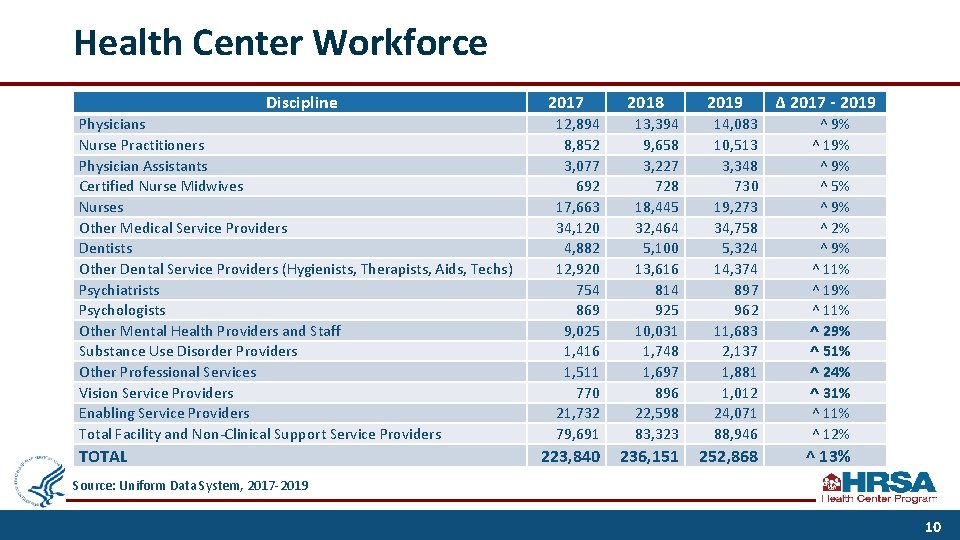
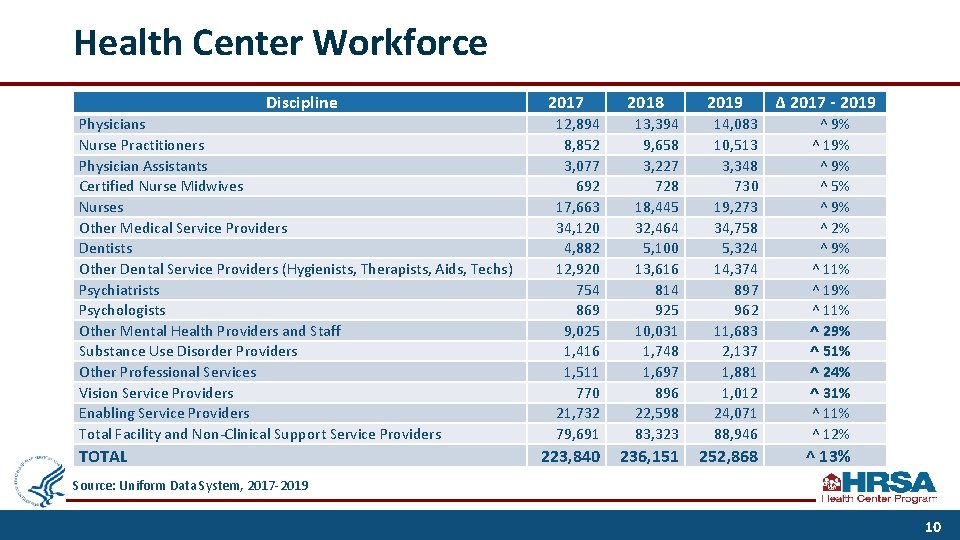
Health Center Workforce Discipline Physicians Nurse Practitioners Physician Assistants Certified Nurse Midwives Nurses Other Medical Service Providers Dentists Other Dental Service Providers (Hygienists, Therapists, Aids, Techs) Psychiatrists Psychologists Other Mental Health Providers and Staff Substance Use Disorder Providers Other Professional Services Vision Service Providers Enabling Service Providers Total Facility and Non-Clinical Support Service Providers TOTAL 2017 2018 2019 Δ 2017 - 2019 12, 894 8, 852 3, 077 692 17, 663 34, 120 4, 882 12, 920 754 869 9, 025 1, 416 1, 511 770 21, 732 79, 691 13, 394 9, 658 3, 227 728 18, 445 32, 464 5, 100 13, 616 814 925 10, 031 1, 748 1, 697 896 22, 598 83, 323 14, 083 10, 513 3, 348 730 19, 273 34, 758 5, 324 14, 374 897 962 11, 683 2, 137 1, 881 1, 012 24, 071 88, 946 ^ 9% ^ 19% ^ 5% ^ 9% ^ 2% ^ 9% ^ 11% ^ 19% ^ 11% ^ 29% ^ 51% ^ 24% ^ 31% ^ 12% 223, 840 236, 151 252, 868 ^ 13% Source: Uniform Data System, 2017 -2019 10
Health Centers’ Response to COVID-19 11
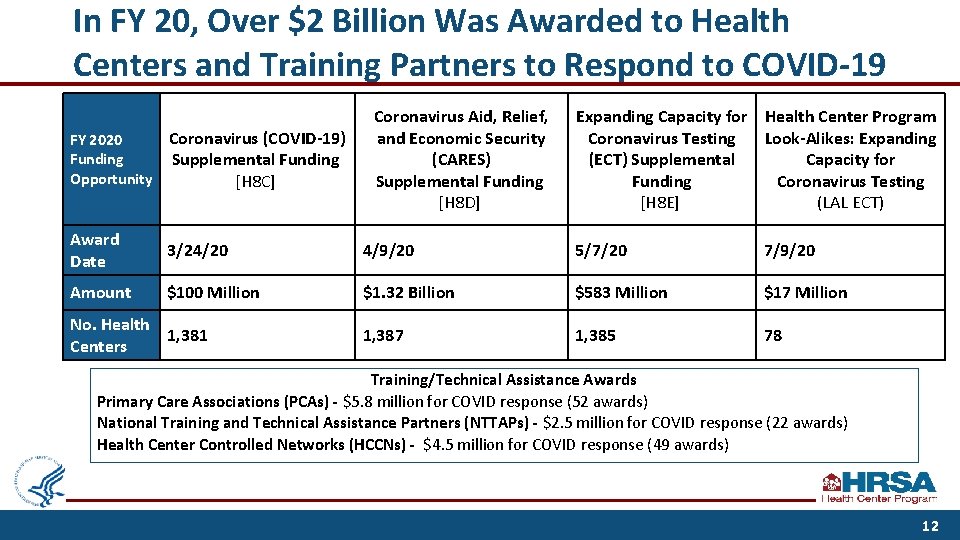
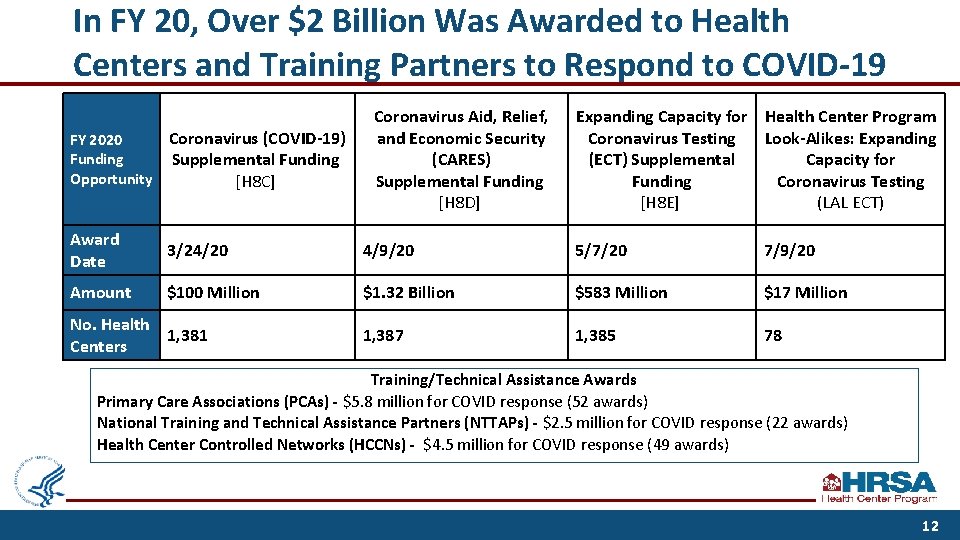
In FY 20, Over $2 Billion Was Awarded to Health Centers and Training Partners to Respond to COVID-19 Coronavirus Aid, Relief, and Economic Security (CARES) Supplemental Funding [H 8 D] Expanding Capacity for Health Center Program Coronavirus Testing Look-Alikes: Expanding (ECT) Supplemental Capacity for Funding Coronavirus Testing [H 8 E] (LAL ECT) FY 2020 Funding Opportunity Coronavirus (COVID-19) Supplemental Funding [H 8 C] Award Date 3/24/20 4/9/20 5/7/20 7/9/20 Amount $100 Million $1. 32 Billion $583 Million $17 Million 1, 387 1, 385 78 No. Health 1, 381 Centers Training/Technical Assistance Awards Primary Care Associations (PCAs) - $5. 8 million for COVID response (52 awards) National Training and Technical Assistance Partners (NTTAPs) - $2. 5 million for COVID response (22 awards) Health Center Controlled Networks (HCCNs) - $4. 5 million for COVID response (49 awards) 12
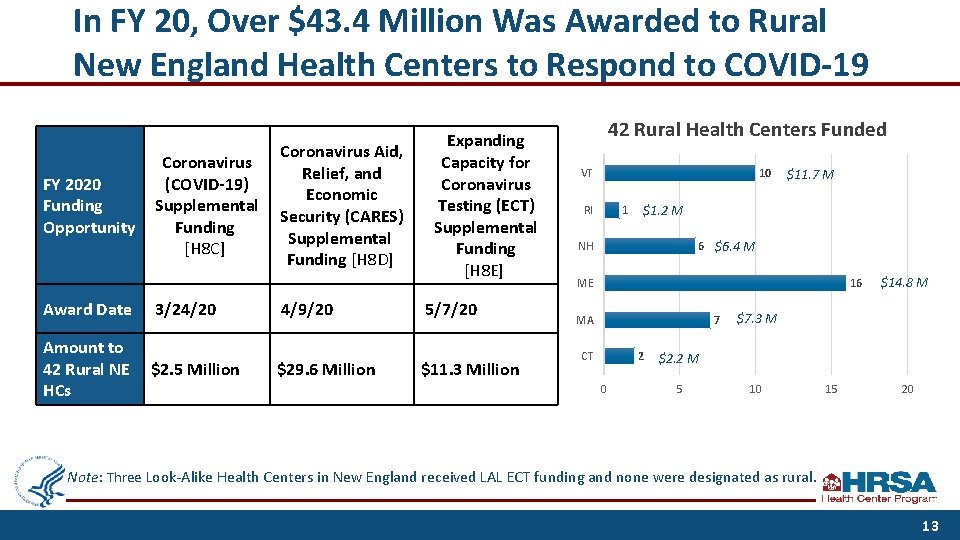
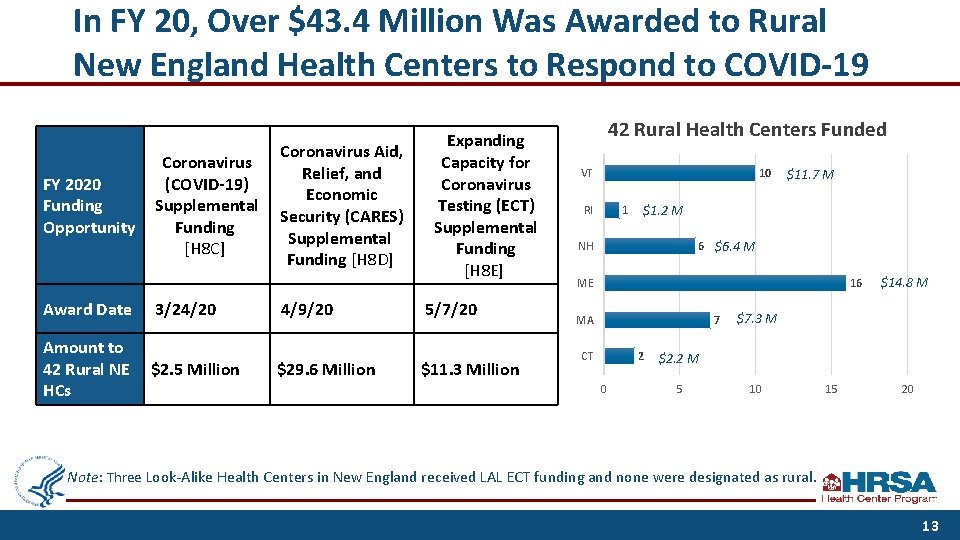
In FY 20, Over $43. 4 Million Was Awarded to Rural New England Health Centers to Respond to COVID-19 FY 2020 Funding Opportunity Coronavirus (COVID-19) Supplemental Funding [H 8 C] Coronavirus Aid, Relief, and Economic Security (CARES) Supplemental Funding [H 8 D] Expanding Capacity for Coronavirus Testing (ECT) Supplemental Funding [H 8 E] Award Date 3/24/20 4/9/20 5/7/20 Amount to 42 Rural NE HCs $2. 5 Million $29. 6 Million $11. 3 Million 42 Rural Health Centers Funded VT 10 RI 1 $11. 7 M $1. 2 M 6 $6. 4 M NH ME 16 MA 7 CT 2 0 $14. 8 M $7. 3 M $2. 2 M 5 10 15 20 Note: Three Look-Alike Health Centers in New England received LAL ECT funding and none were designated as rural. 13
Health Centers and COVID-19 Response • Health centers are on the front lines, delivering critical services, including: § COVID-19 testing; § Monitoring and managing COVID-19 symptoms to alleviate burden on emergency rooms and hospitals; § Coordinating with local and state health departments to support a unified and comprehensive public health response – including enrolling providers to administer COVID-19 vaccines; § Collaborating with federal and academic partners to provide COVID-19 therapeutics to high-risk positive patients; and § Providing ongoing essential primary care services to patients with medical and mental health care needs, including actively managing conditions that put patients at increased risk for COVID-19 complications. 14
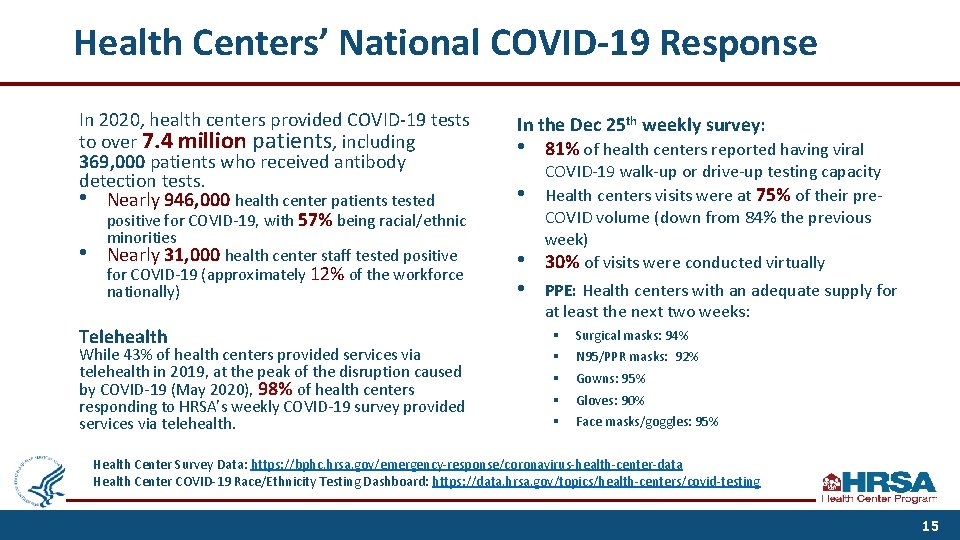
Health Centers’ National COVID-19 Response In 2020, health centers provided COVID-19 tests to over 7. 4 million patients, including 369, 000 patients who received antibody detection tests. • Nearly 946, 000 health center patients tested positive for COVID-19, with 57% being racial/ethnic In the Dec 25 th weekly survey: • 81% of health centers reported having viral • • minorities Nearly 31, 000 health center staff tested positive for COVID-19 (approximately 12% of the workforce nationally) Telehealth While 43% of health centers provided services via telehealth in 2019, at the peak of the disruption caused by COVID-19 (May 2020), 98% of health centers responding to HRSA’s weekly COVID-19 survey provided services via telehealth. • • COVID-19 walk-up or drive-up testing capacity Health centers visits were at 75% of their pre. COVID volume (down from 84% the previous week) 30% of visits were conducted virtually PPE: Health centers with an adequate supply for at least the next two weeks: § § § Surgical masks: 94% N 95/PPR masks: 92% Gowns: 95% Gloves: 90% Face masks/goggles: 95% Health Center Survey Data: https: //bphc. hrsa. gov/emergency-response/coronavirus-health-center-data Health Center COVID-19 Race/Ethnicity Testing Dashboard: https: //data. hrsa. gov/topics/health-centers/covid-testing 15
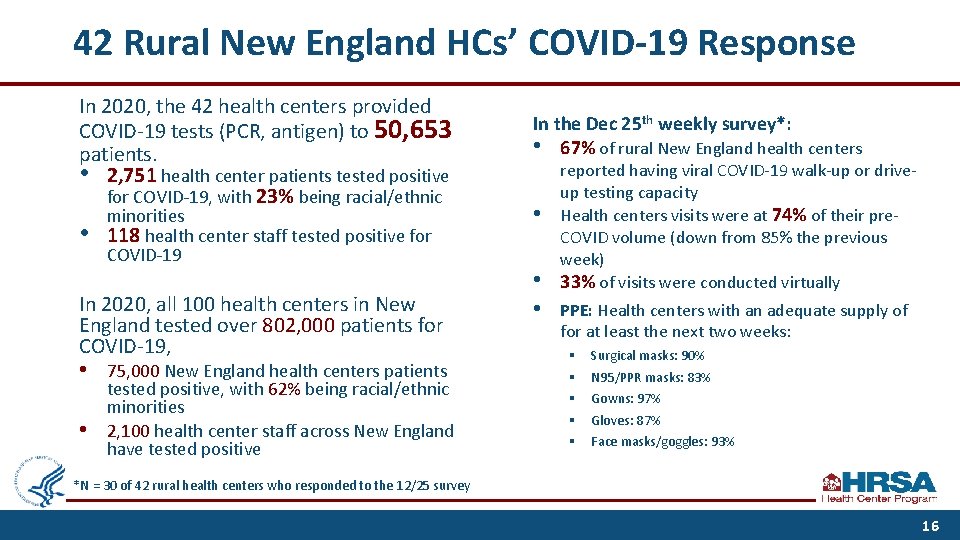
42 Rural New England HCs’ COVID-19 Response In 2020, the 42 health centers provided COVID-19 tests (PCR, antigen) to 50, 653 patients. • 2, 751 health center patients tested positive for COVID-19, with 23% being racial/ethnic • minorities 118 health center staff tested positive for COVID-19 In 2020, all 100 health centers in New England tested over 802, 000 patients for COVID-19, • • 75, 000 New England health centers patients tested positive, with 62% being racial/ethnic minorities 2, 100 health center staff across New England have tested positive In the Dec 25 th weekly survey*: • 67% of rural New England health centers • • • reported having viral COVID-19 walk-up or driveup testing capacity Health centers visits were at 74% of their pre. COVID volume (down from 85% the previous week) 33% of visits were conducted virtually PPE: Health centers with an adequate supply of for at least the next two weeks: § § § Surgical masks: 90% N 95/PPR masks: 83% Gowns: 97% Gloves: 87% Face masks/goggles: 93% *N = 30 of 42 rural health centers who responded to the 12/25 survey 16
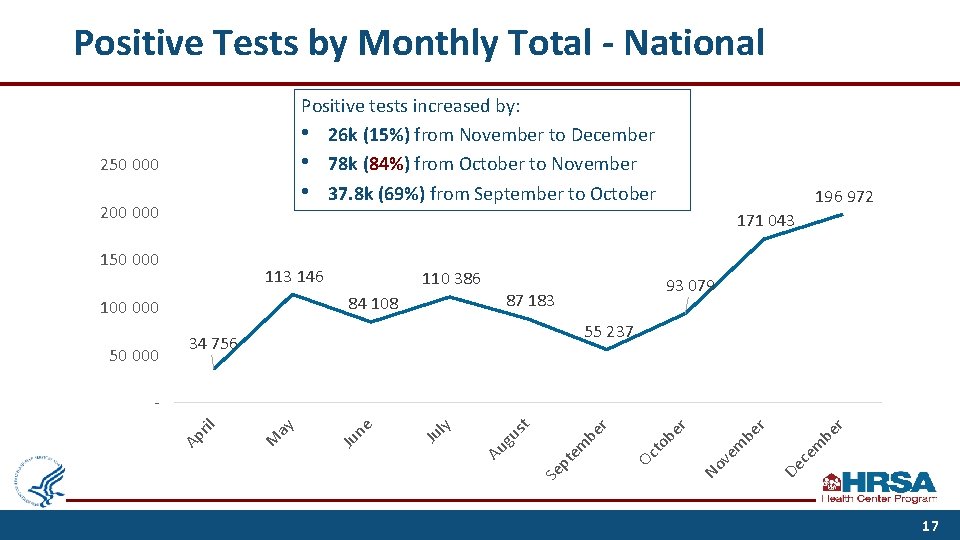
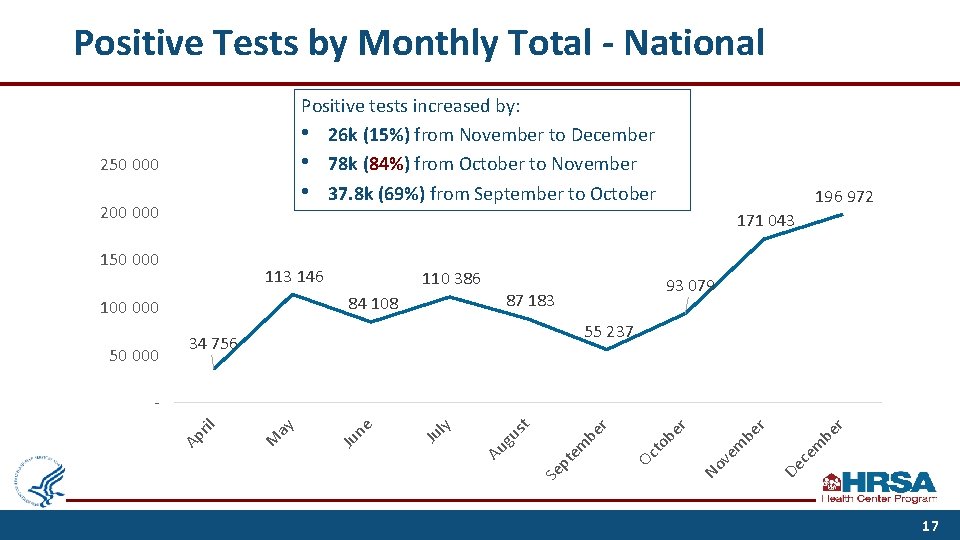
Positive Tests by Monthly Total - National Positive tests increased by: • 26 k (15%) from November to December • 78 k (84%) from October to November • 37. 8 k (69%) from September to October 250 000 200 000 171 043 150 000 113 146 110 386 93 079 87 183 84 108 100 000 50 000 196 972 55 237 34 756 m be ce De be m ve r r r be to Oc No Se pt em be r t us Au g ly Ju ne Ju ay M Ap ril - 17
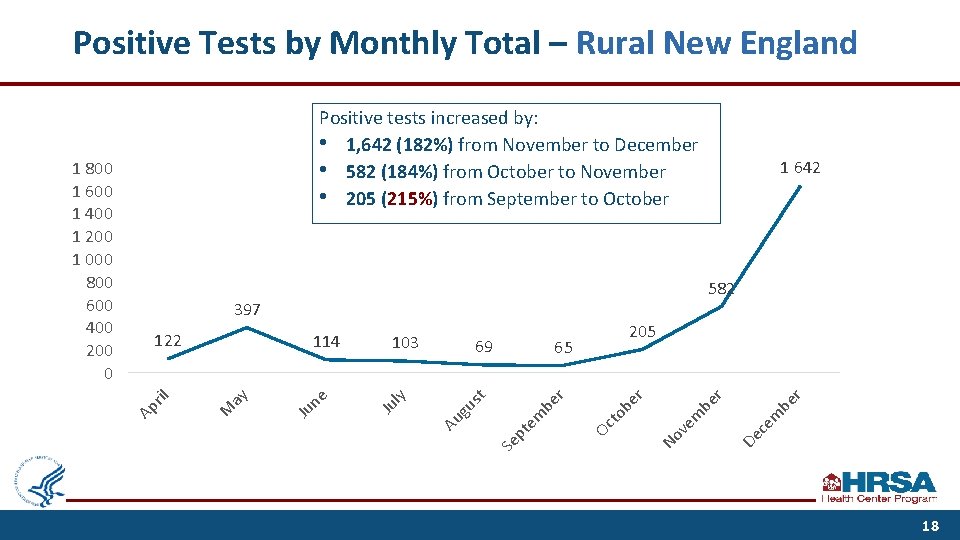
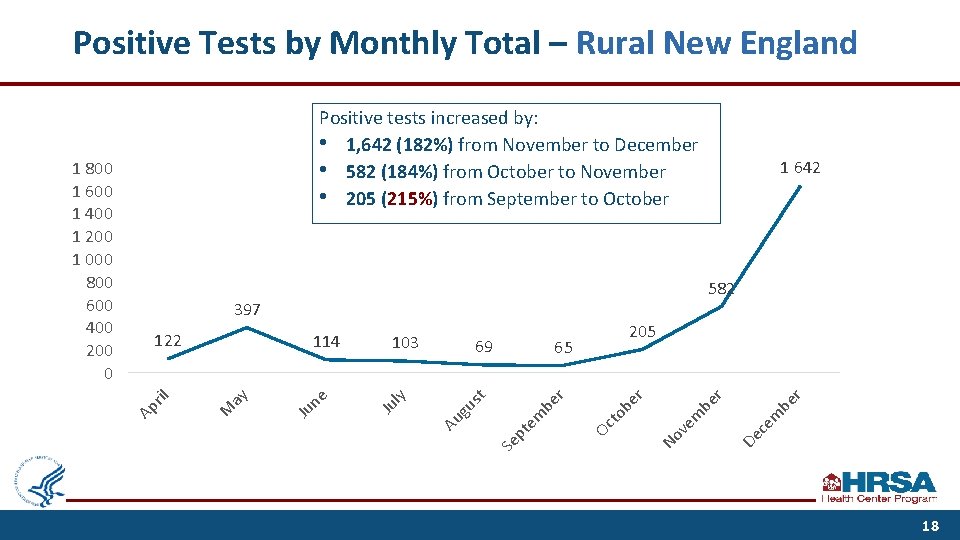
Positive Tests by Monthly Total – Rural New England De ce m be r r ve m be be to Oc r em be pt Se r 65 t us 205 No 69 Au g ly 103 Ju ne Ju ay 114 M ril 122 1 642 582 397 Ap 1 800 1 600 1 400 1 200 1 000 800 600 400 200 0 Positive tests increased by: • 1, 642 (182%) from November to December • 582 (184%) from October to November • 205 (215%) from September to October 18
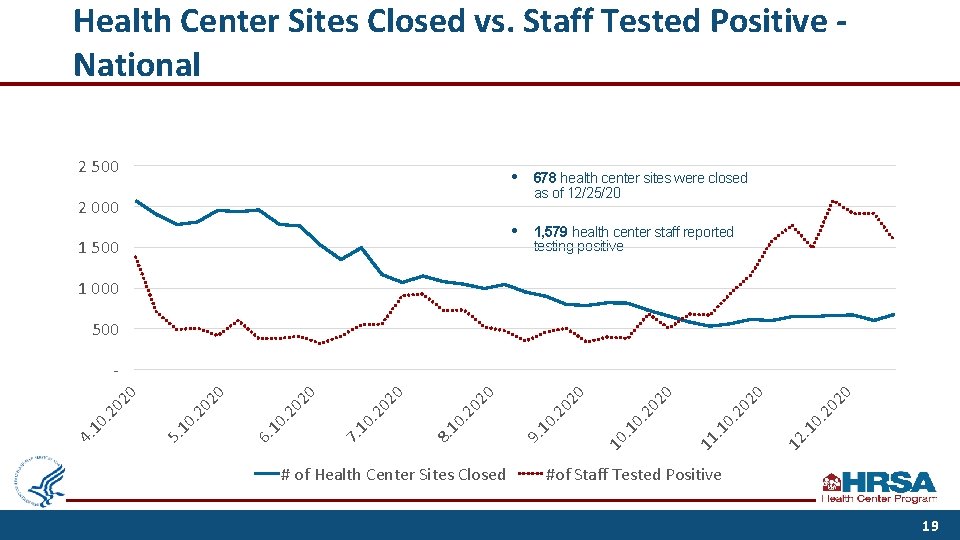
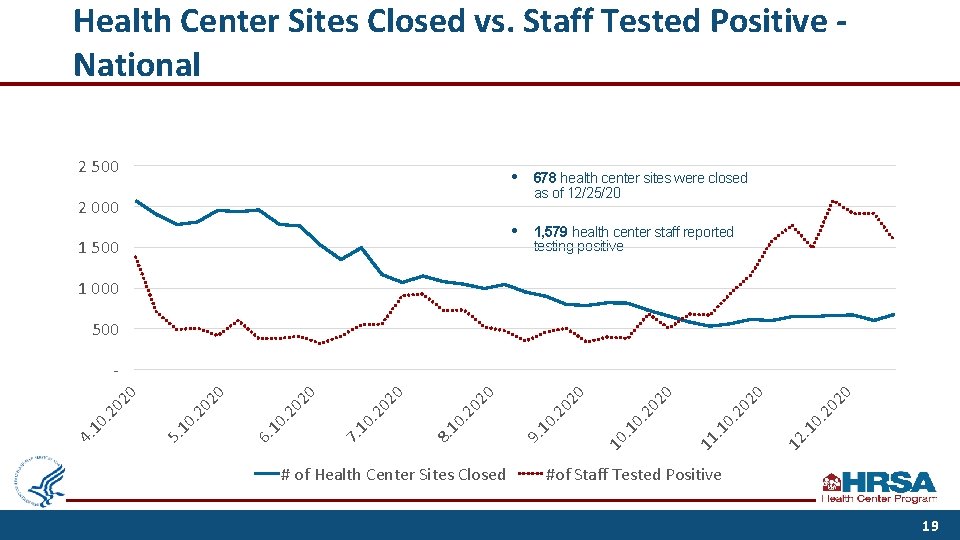
Health Center Sites Closed vs. Staff Tested Positive National 2 500 • 678 health center sites were closed as of 12/25/20 • 1, 579 health center staff reported testing positive 2 000 1 500 1 000 500 # of Health Center Sites Closed 20 20 0. . 1 12 20 0. . 1 11 10 . 1 0. 20 20 20 0 9. 10 . 2 02 0. 2 10 8. 02. 2 10 7. 02 0 0 02. 2 10 6. 02. 2 10 5. 4. 10 . 2 02 0 0 - #of Staff Tested Positive 19
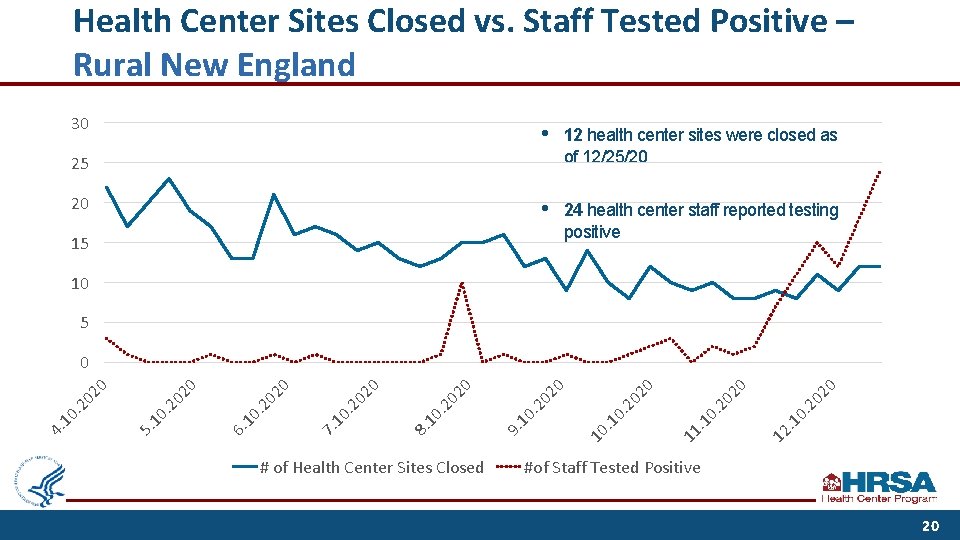
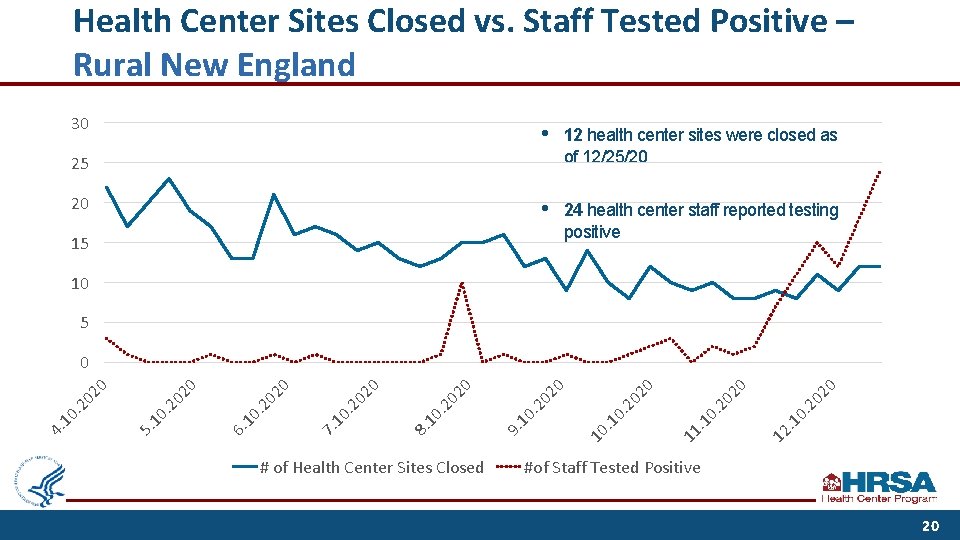
Health Center Sites Closed vs. Staff Tested Positive – Rural New England 30 • 12 health center sites were closed as of 12/25/20 • 24 health center staff reported testing positive 25 20 15 10 5 # of Health Center Sites Closed 20 12 . 1 0. 20 20 0. . 1 11 20 0. . 1 10 20 20 0 9. 10 . 2 02 0 8. 10 . 2 02 0 7. 10 . 2 02 0 6. 10 . 2 02 0 02. 2 10 5. 4. 10 . 2 02 0 0 #of Staff Tested Positive 20
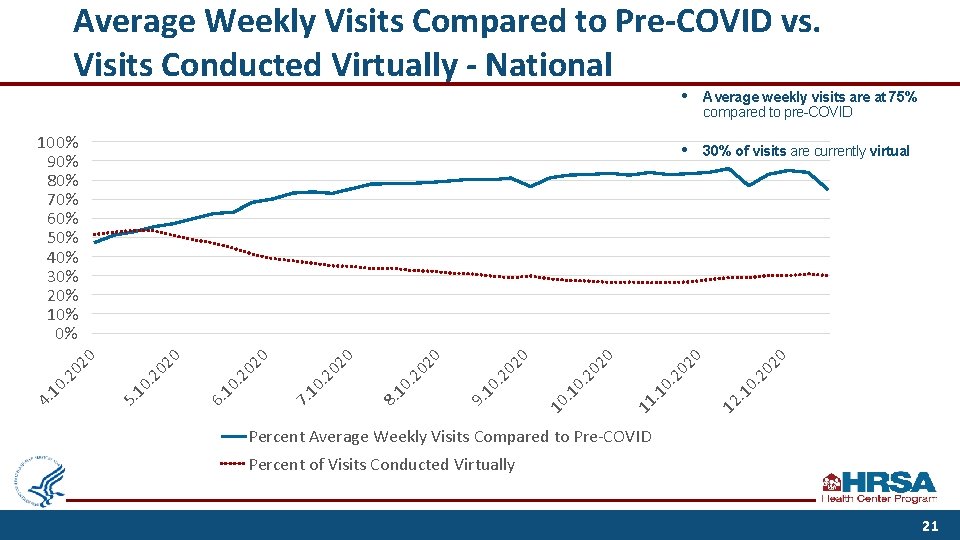
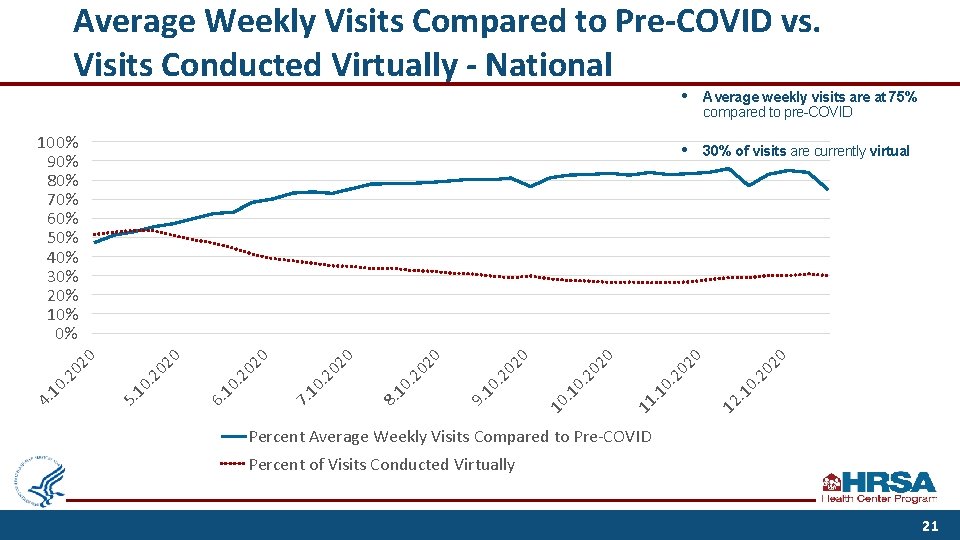
Average Weekly Visits Compared to Pre-COVID vs. Visits Conducted Virtually - National 30% of visits are currently virtual 20 • 12 . 1 0. 20 20 0. . 1 11 20 0. . 1 10 Average weekly visits are at 75% compared to pre-COVID 20 20 0 9. 10 . 2 02 0 8. 10 . 2 02 0 7. 10 . 2 02 0 02 6. 10 . 2 02. 2 10 5. 4. 10 . 2 02 0 0 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% • Percent Average Weekly Visits Compared to Pre-COVID Percent of Visits Conducted Virtually 21
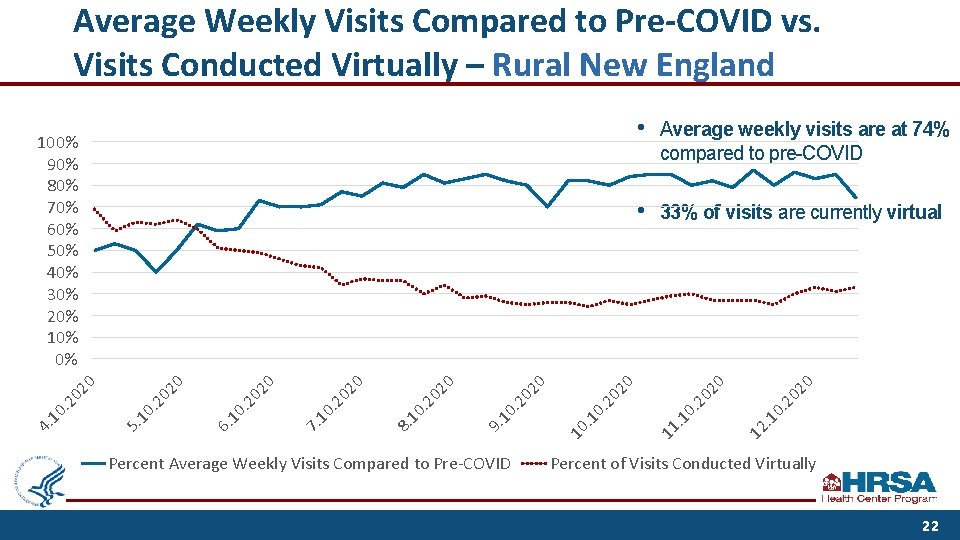
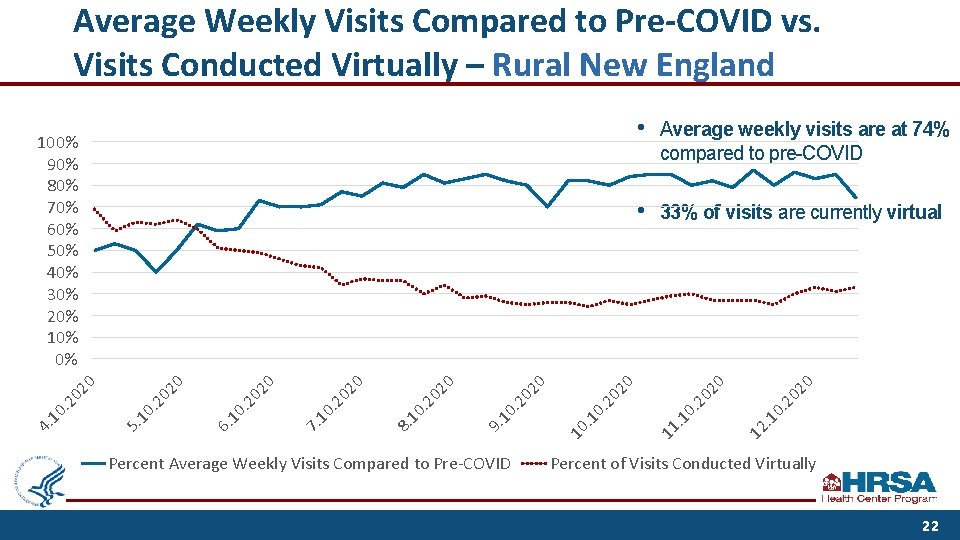
Average Weekly Visits Compared to Pre-COVID vs. Visits Conducted Virtually – Rural New England Percent Average Weekly Visits Compared to Pre-COVID • 33% of visits are currently virtual 20 0. . 1 12 20 0. . 1 11 20 0. . 1 10 20 Average weekly visits are at 74% compared to pre-COVID 20 • 20 0. 2 10 9. 02. 2 10 8. 02 0 0. 2 10 7. 02. 2 10 6. 02 0 0 02. 2 10 5. 4. 10 . 2 02 0 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% Percent of Visits Conducted Virtually 22
COVID-19 Therapeutics • Health centers engaged in clinical research trials to develop COVID-19 treatment therapies and explore their capacity to provide monoclonal antibody (m. Ab) therapeutics to COVID-19 -positive, high risk patients in the outpatient setting. § On November 9, 2020, FDA issued an emergency use authorization for the m. Ab therapy, bamlanivimab, for the treatment of mild-to-moderate COVID-19 in adults and pediatric patients with positive COVID-19 test results who are at high risk for progressing to severe COVID-19 and/or hospitalization. • COVID-19 antibody treatments administered by intravenous (IV) infusion can be considered in-scope of project and subsequently eligible for FTCA malpractice coverage. • Operation Warp Speed is working with 36 health centers to pilot the administration of m. AB therapy to high-risk COVID-19 positive patients in the outpatient setting. 23
COVID-19 Vaccine Distribution Plan Distribution • • • State Primary Care Associations (PCAs) report that they or health center leaders in a majority of states are involved with state health department planning for COVID-19 vaccine deployment and working to enroll as COVID-19 vaccine providers. Health centers are receiving vaccines through their state immunization programs. Depending on the state distribution plan, health centers may be prioritized for the initial allocation of vaccines. Concerns Raised • • • Sufficient PPE and supplies to administer vaccines Paying for staff to administer the vaccine and related operational expenses Workforce operational levels Hesitancy among health center staff and/or patients to receive a COVID-19 vaccine Access and/or transportation barriers due to location 24
Lessons and Innovations • • Standing up a response team that coordinates with state/local public health authorities Increasing capacity for robust virtual care infrastructure § Medical, dental, and behavioral health • Transforming workflows and physical space to accommodate new protocols § Drive-through COVID-19 testing; mobile units; virtual visits • • Leveraging health IT and analytics to support data driven decision-making Deploying multimodal communications Partnerships Implementing workforce supports See NACHC’s Sept 2020 Report: Promising Health Center Practices During COVID-19 https: //cdn 1. digitellinc. com/uploads/nachc/articles/ca 7 da 83 e 629 d 33 a 83 ecc 35 cd 1 b 9 fc 007. pdf and related TA site 25
Supporting Health Center Workforce Resilience • Nearly half of physicians, nurses, and other providers report experiencing job burnout, with these trends further exacerbated during the national response to COVID-19. • In response, BPHC is initiating several efforts to assess the levels of workforce well-being, engagement, and burnout throughout the country, in order to: • • identify the key factors that affect workforce well-being, and facilitate shared learning to improve workforce well-being within the Health Center Program. • BPHC is also investing in Primary Care Associations to assist health centers in assessing readiness for developing and engaging with health professions training programs. • Goal: Enhance health centers’ capabilities to recruit, develop, and retain their workforce by exposing health and allied health professions students, trainees, and residents to education and training programs at health centers. 26
DRAFT COVID-19 Response Overview: Healthcare Resilience Working Group
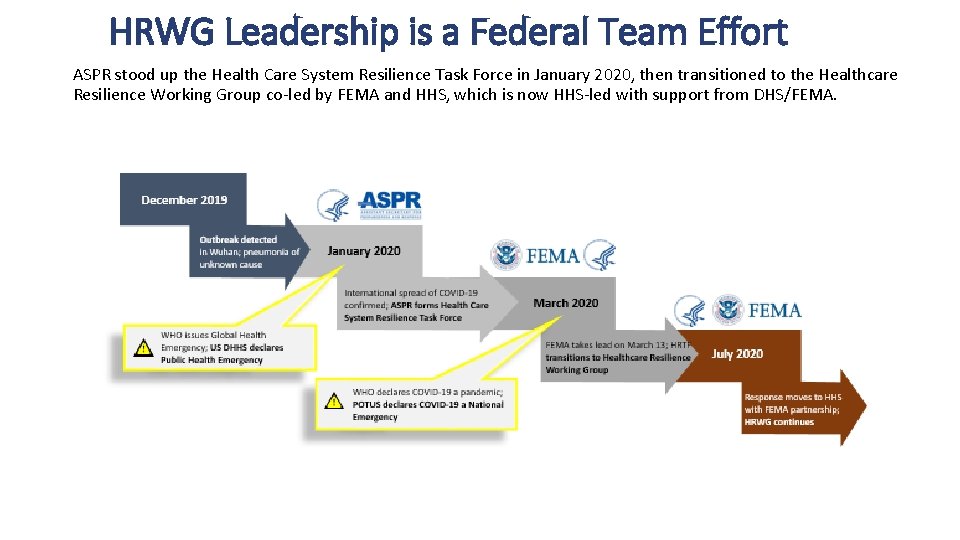
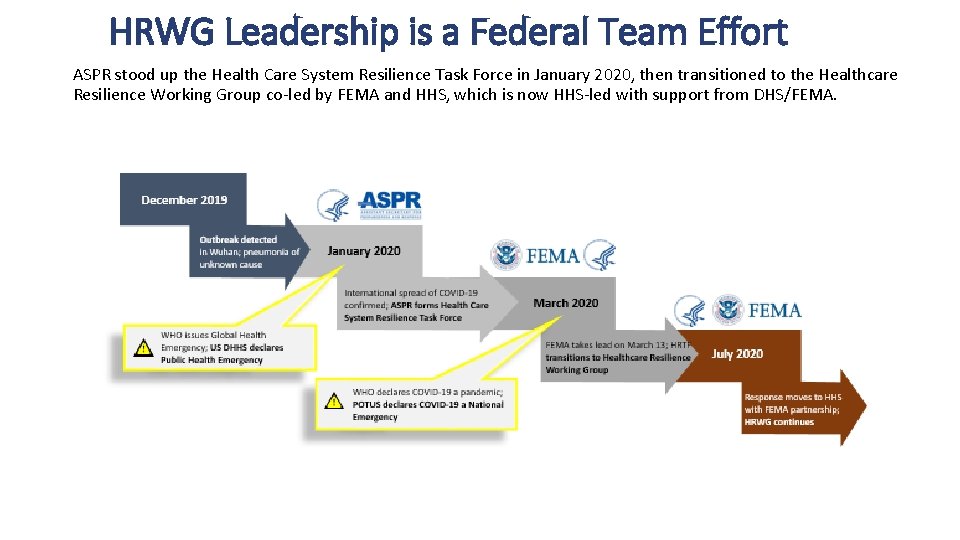
HRWG Leadership is a Federal Team Effort ASPR stood up the Health Care System Resilience Task Force in January 2020, then transitioned to the Healthcare Resilience Working Group co-led by FEMA and HHS, which is now HHS-led with support from DHS/FEMA.

HRWG Values its Association Partners HRWG held regular meetings with key stakeholders including representatives from professional associations, academic institutions, non-government organizations, and private healthcare companies

Rural Healthcare Surge Readiness • Health care entities in rural areas face significant and unique challenges related to COVID-19. • The Rural Healthcare Surge Readiness Web Portal provides a collection of essential resources, tools, and trainings to prepare for and respond to surge events in rural settings. • Searchable by health care sector (pre-hospital, ambulatory, and long-term care) and role (executive, manager, provider). • Also organized by topic area (e. g. , behavioral health, telehealth, regulatory and policy, workforce). • https: //www. ruralhealthinfo. org/healthcaresurge-readiness Utilization: >23, 800 web portal visits including every state in the U. S. • Podcast: Rural Health Resources Roundup: Rural Hospital Resources - collaboration with the HRSA Office of Regional Operations. 30
Rural Healthcare Surge Readiness https: //www. ruralhealthinfo. org/healthcare-surge-readiness Saving Lives. Protecting Americans. 31
Thank You! Christina Lachance, MPH Senior Advisor Bureau of Primary Health Care, HRSA bphcoaa@hrsa. gov Renée Joskow, DDS, MPH, FAGD, FACD, FICD Chief Dental Officer Health Resources and Services Administration HCSRTF-COVID-19@hhs. gov www. hrsa. gov Sign up for the Primary Health Care Digest 32

Connect with HRSA To learn more about our agency, visit www. HRSA. gov Sign up for the HRSA e. News FOLLOW US: 33
 Http//apps.tujuhbukit.com/covid19
Http//apps.tujuhbukit.com/covid19 Do if you covid19
Do if you covid19 Covid19 athome rapid what know
Covid19 athome rapid what know What do if test positive covid19
What do if test positive covid19 Vaksin covid19
Vaksin covid19 Covid 19 pandemic summary
Covid 19 pandemic summary Who pandemic phases
Who pandemic phases Pandemic tabletop exercise template
Pandemic tabletop exercise template Mathalicious pandemic answer key
Mathalicious pandemic answer key Global pandemic preparedness
Global pandemic preparedness Natural response and forced response
Natural response and forced response First order system transfer function
First order system transfer function A subsequent
A subsequent National center for response to intervention
National center for response to intervention Chiang mai azure development
Chiang mai azure development Videofied pricing
Videofied pricing National center on response to intervention
National center on response to intervention Demand response research center
Demand response research center Herds reporting
Herds reporting Role of public health nurse in disaster response
Role of public health nurse in disaster response Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Tư thế worm breton
Tư thế worm breton Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Môn thể thao bắt đầu bằng chữ đua
Môn thể thao bắt đầu bằng chữ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công của trọng lực
Công của trọng lực Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Làm thế nào để 102-1=99
Làm thế nào để 102-1=99