Group 5 Heather Donaldson Jatna Azuri Marcia Powell





- Slides: 49
Group 5: Heather Donaldson Jatna Azuri Marcia Powell Christina Ramotar Tiffany Wood Alicia Mendoza Katherine Riedi
Definitions • Morals- principles on which one’s judgments of right and wrong are based. More abstract, subjective, and often personal or religion-based. • Ethics- principles of right conduct. More practical, conceived as shared principles promoting fairness in social and business interactions ▫ Ethics is also a field of philosophical study.
Step 1: Ethical Questions
1. In all circumstances, doctors and nurses should do everything possible to save the life of a patient. 2. Sometimes there are circumstances where a patient should be allowed to die.
When a person has a disease that cannot be cured and is living in severe pain, do you think doctors should or should not be allowed by law to assist the patient to commit suicide if the patient requests it? I. Should? II. Should not?
Do you think a person has a moral right to end his or her own life under any of the following circumstances? I. When this person has a disease that is incurable II. When this person is suffering great pain and has no hope of improvement III. When this person is an extremely heavy burden on his or her family IV. When this person is ready to die because living has become a burden
u o y d w? i D o n K Step 2: What are the Facts?
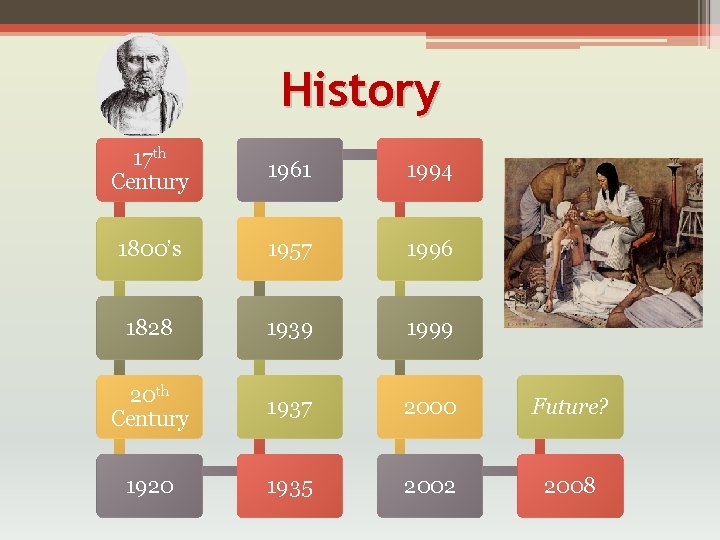
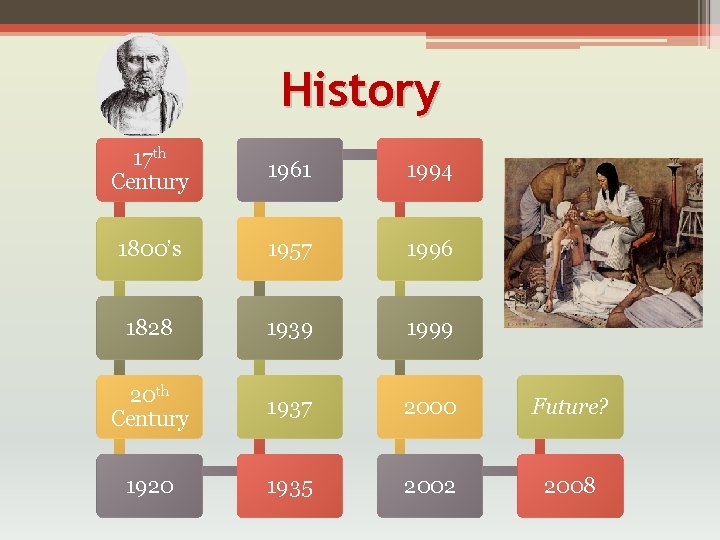
History 17 th Century 1961 1994 1800’s 1957 1996 1828 1939 1999 20 th Century 1937 2000 Future? 1920 1935 2002 2008


Forms of Euthanasia It Can Be: Passive Or Active
Other Forms of Euthanasia • Indirect euthanasia ▫ Providing treatment that has the side effect of speeding the patient's death ▫ Primary intention is not to kill • Assisted suicide ▫ Who is going to die needs help to kill themselves and asks for it ▫ Getting drugs for the person and putting them within their reach
Classification of Euthanasia • Voluntary ▫ Occurs at the request of the person who dies • Non-Voluntary ▫ When the person is unable to make a choice • Involuntary ▫ When the person who dies chooses life and is killed anyway ▫ Usually called murder ▫ An appropriate person takes the decision on their behalf.
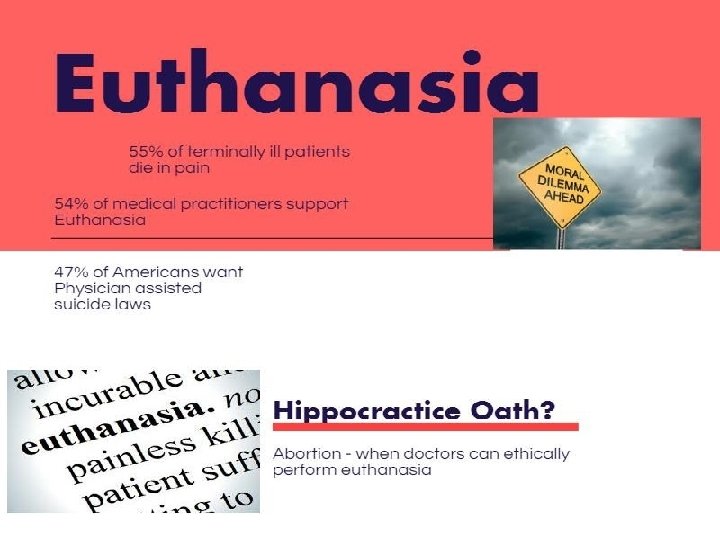
For Euthanasia • Right to choose when to die • Dignified death • End pain and suffering • Promotes quality of life • Save money on drugs and medical bills
a i s a n a h t u E t s n i a Ag • Act of Murder or Suicide • Religious beliefs • Devalues human life • Promotes quantity of life • Misused or manipulation • Hinders further medical developments

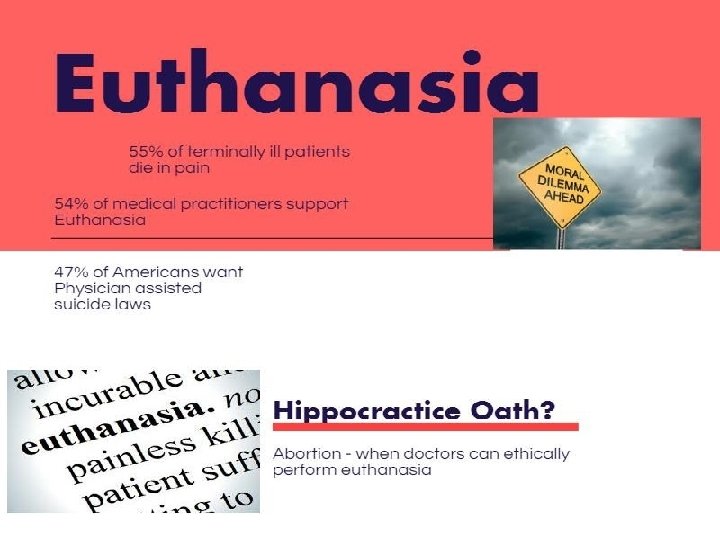
• “I will give no deadly medicine to any one if asked, nor suggest any such counsel”(Hippocrates).
Step 3: Identify the Stakeholders
Terminally ill patients • Individuals who are terminally ill do not want to die, but at the same time, they do not want to suffer terribly either. Family Members • Many family members would prefer to take the time to care for their terminally ill loved ones, but it is not their choice.
Physicians • Have been taught to heal and not do harm to patients. • Faced with the prospect of: ▫ Having to forego what they were taught ▫ Ignore their moral values of respecting each individual human life. The Society • Faced with the dilemma of: ▫ Whether a person should be allowed to choose to die with dignity. ▫ Get relief from pain and suffering and die a natural death.
Religion • Most religions disapprove of euthanasia. ▫ Some of them absolutely forbid it. ▫ “You must not kill‘” kill • Some Eastern religions take a different approach. ▫ Their attitudes to death are achieving freedom from mortal life, and not-harming living beings.
Step 4: What are the Options for this Case?
Options for Euthanasia • Pain Killer or Medication Overdose ▫ Also known as active euthanasia ▫ Physician’s are not actively “killing”, but aware of inaction on their behalf will ultimately be the death of the patient. • Lethal Injection • Withdrawal of Treatment/Withholding Treatment ▫ Passive Euthanasia
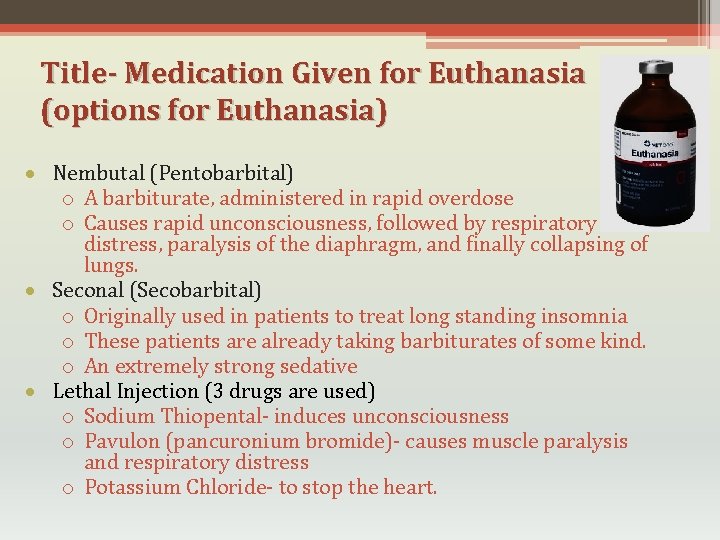
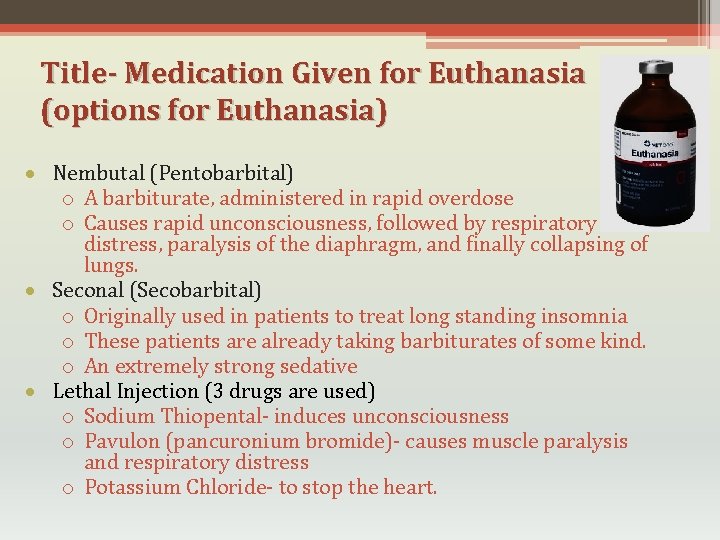
Title- Medication Given for Euthanasia (options for Euthanasia) Nembutal (Pentobarbital) o A barbiturate, administered in rapid overdose o Causes rapid unconsciousness, followed by respiratory distress, paralysis of the diaphragm, and finally collapsing of lungs. Seconal (Secobarbital) o Originally used in patients to treat long standing insomnia o These patients are already taking barbiturates of some kind. o An extremely strong sedative Lethal Injection (3 drugs are used) o Sodium Thiopental- induces unconsciousness o Pavulon (pancuronium bromide)- causes muscle paralysis and respiratory distress o Potassium Chloride- to stop the heart.
Other Options • Pain Management ▫ Palliative Sedation • Withdrawing life-sustaining treatments ▫ dialysis, where a machine takes over the functions of your kidneys ▫ ventilators, where a machine takes over your breathing
Other Options • Refusing Treatment • Advance Directive ▫ allows you to document your wishes concerning medical treatments at the end of life. • DNR Order (Do Not Resuscitate) ▫ Not to do cardiopulmonary resuscitation (CPR)
Step 5: What should be done?

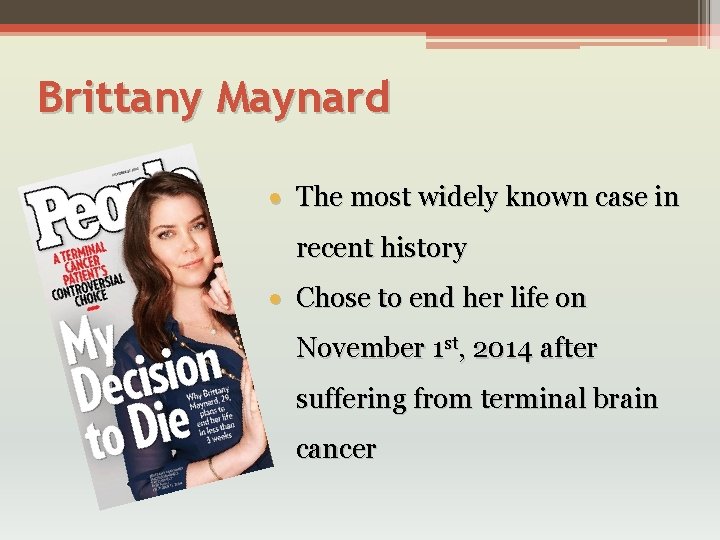
Brittany Maynard The most widely known case in recent history Chose to end her life on November 1 st, 2014 after suffering from terminal brain cancer
Ethan Remmel • Psychology Professor • Diagnosed with terminal colon cancer • Did not want his children to see him deteriorate or suffer and remember him that way • Obtained the meds and held onto them until he felt it was time • His wife said to NBC “We obviously didn’t want him to die, but he was dying anyways”
Barbara Mancini • Father suffered from Kidney and Cardiovascular problems along with others • Accused of helping her father commit suicide by a lethal dosage of morphine • Handed him the bottle of morphine not knowing what he was planning to do with it • Her father had a DNR and made it clear that he did not want to be in the hospital • Eventually the case was dismissed
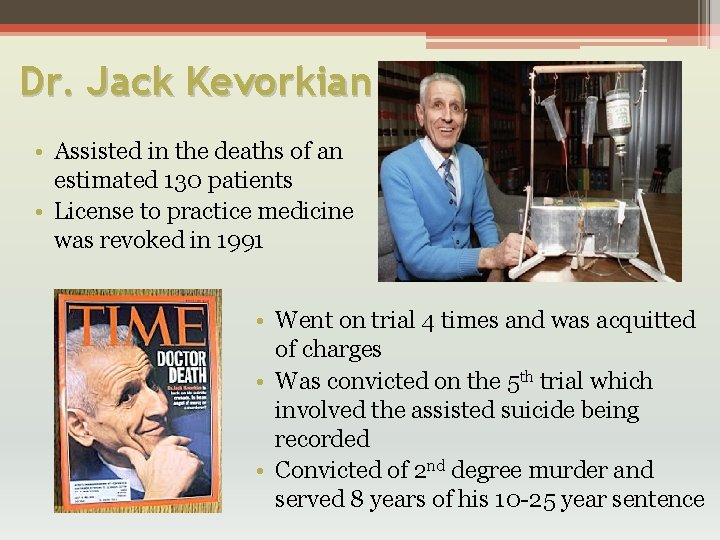
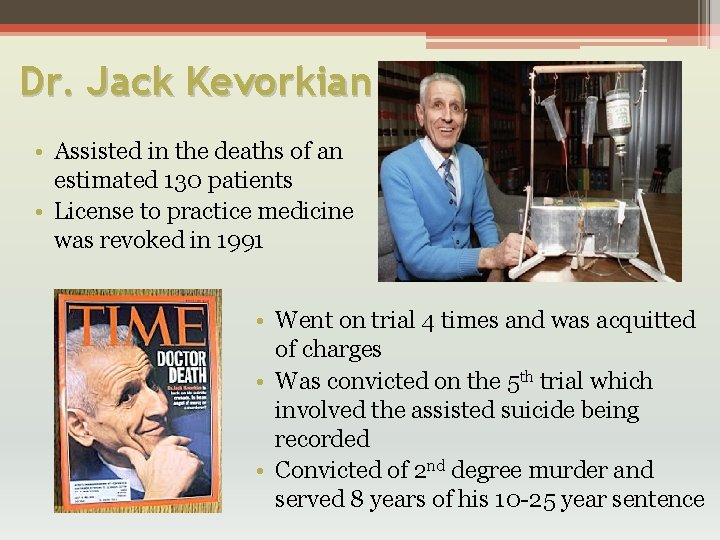
Dr. Jack Kevorkian • Assisted in the deaths of an estimated 130 patients • License to practice medicine was revoked in 1991 • Went on trial 4 times and was acquitted of charges • Was convicted on the 5 th trial which involved the assisted suicide being recorded • Convicted of 2 nd degree murder and served 8 years of his 10 -25 year sentence
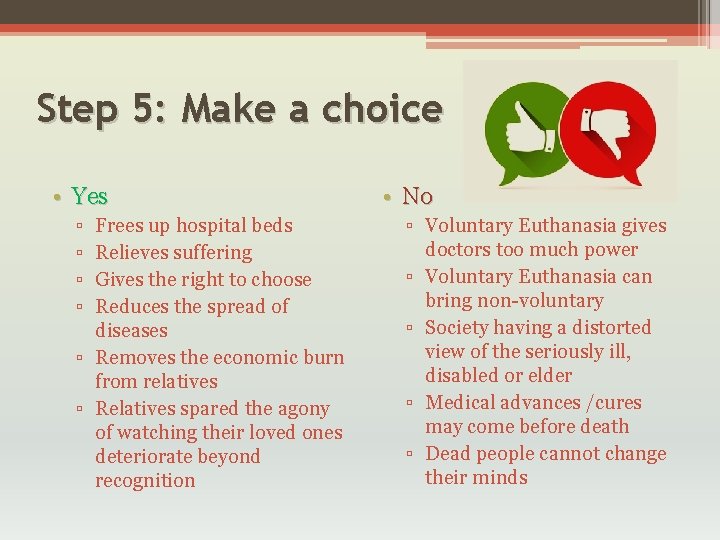
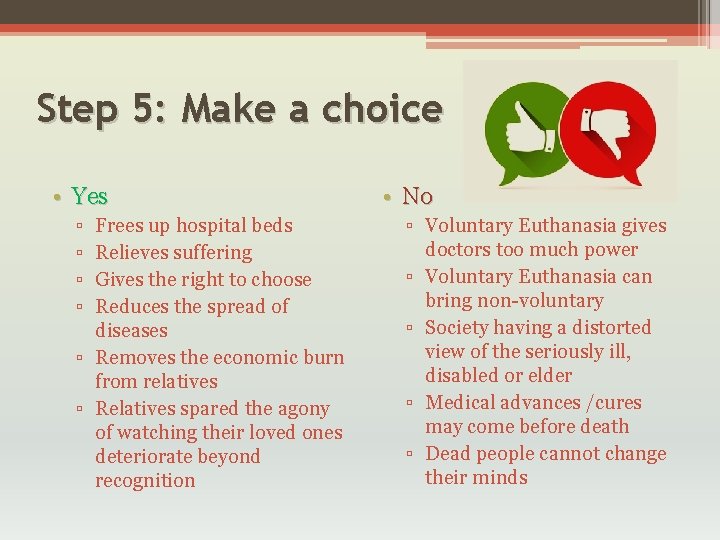
Step 5: Make a choice • Yes ▫ ▫ Frees up hospital beds Relieves suffering Gives the right to choose Reduces the spread of diseases ▫ Removes the economic burn from relatives ▫ Relatives spared the agony of watching their loved ones deteriorate beyond recognition • No ▫ Voluntary Euthanasia gives doctors too much power ▫ Voluntary Euthanasia can bring non-voluntary ▫ Society having a distorted view of the seriously ill, disabled or elder ▫ Medical advances /cures may come before death ▫ Dead people cannot change their minds
Results are in: Legalize Voluntary Euthanasia only Group 5
Step 6: What Justifies your Choice?
• We are “for Euthanasia” depending on the circumstance Because ▫ Examples: Terminally ill patients that have terminal • It provides a way to cancer, end stage renal relieve extreme pain disease, advanced heart • It provides a way of relief disease…Basically any when a person's quality of incurable disease life is low • Frees up medical funds to help other people • It is another case of freedom of choice
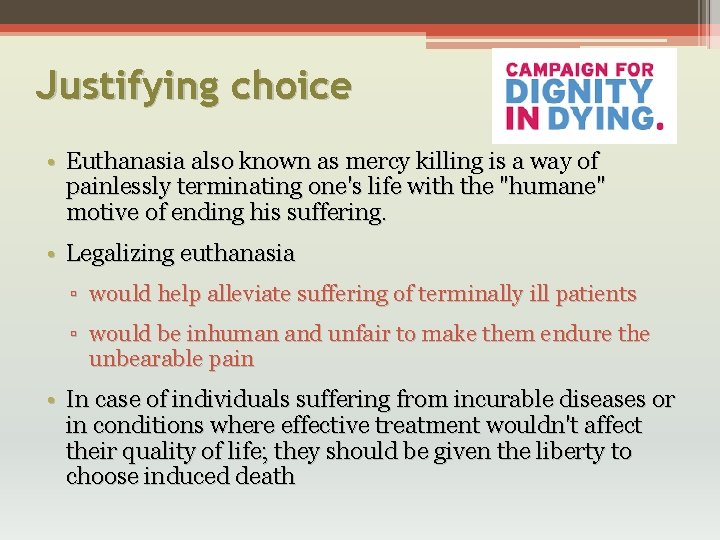
Justifying choice • Euthanasia also known as mercy killing is a way of painlessly terminating one's life with the "humane" motive of ending his suffering. • Legalizing euthanasia ▫ would help alleviate suffering of terminally ill patients ▫ would be inhuman and unfair to make them endure the unbearable pain • In case of individuals suffering from incurable diseases or in conditions where effective treatment wouldn't affect their quality of life; they should be given the liberty to choose induced death
If the patient has the right to discontinue treatment why would he not have the right to shorten his lifetime to escape the intolerable anguish? Isn't the pain of waiting for death frightening and traumatic?
• "The victim should have the right to end his life, if he wants. But I think it would be a great mistake. However a bad life may seem, there is always something you can do, and succeed at. While there's life, there is hope. “ (Stephen Hawking)
Step 7: How can this Problem be Prevented?
Prevention in Unnecessary Deaths • A patient must be given 6 months or less to live • Medical and Technological advances • Advances in palliative medications have been able to relieve pain
Prevention Time Constraint • Terminally Ill patients lose motivation • Takes time for medical advances • Is 6 months long enough?
Prevention Examples of Medical Advances • Here are some examples of Medical Advances over the last decade: • Smoke Free Laws • Targeted Cancer Therapies
Can a Child Choose the Right to Die? • If a child is suffering and in pain, do the same concepts apply? • Should parents be able to make the decision for the child? • This all depends on the age that the child fully grasps the concept of death
How can this be Prevented? • Better training in long-term pain management • Developing treatments with less debilitating side effects
What to Do? • • Help them feel useful Give love Encourage them to live Educate yourself to make the right decision

References • American Brain Tumor Association. (n. d. ). Glioblastoma (GBM). Retrieved March 10, 2016, from http: //www. abta. org/brain-tumor-information/types-oftumors/glioblastoma. html? referrer=https: //www. google. com/ • Bulger, M. (2015). Can a Child Choose the Right to Die? The Humanist. Retrieved March 16, 2016 • Ethics vs. morals. (n. d. ). Retrieved March 19, 2016, from http: //grammarist. com/usage/ethics-morals/ • Euthanasia. (2014). Retrieved March 6, 2016, from http: //www. bbc. co. uk/ethics/euthanasia/ • Euthanasia. (n. d. ). Retrieved March 06, 2016, from http: //www. life. org. nz/euthanasia/ • Fieser, J. (2015, January 01). From Moral Issues that Divide Us and Applied Ethics: A Sourcebook. Retrieved March 03, 2016, from https: //www. utm. edu/staff/jfieser/class/160/6 -euthanasia. htm • History of Euthanasia. (n. d. ). Retrieved March 14, 2016, from www. euthanasia. com/historyeuthanasia. html • Nordqvist, C. (2015, October 30). Euthanasia and Assisted Suicide. Retrieved March 12, 2016, from www. medicalnewstoday. com/articles/182951. php? page=2
References • Oregon Health Authority. (n. d. ). Death with Dignity Act. Retrieved March 08, 2016, from https: //public. health. oregon. gov/Provider. Partner. Resources/Evaluation. Research/Dea thwith. Dignity. Act/Pages/index. aspx • Prokopetz, J. , & Lehmann, L. (2012). Redefining Physicians' Role in Assisted Dying. New England Journal of Medicine. Retrieved March 16, 2016. • What are Advance Directives? (n. d. ). Retrieved March 15, 2016, from http: //www. caringinfo. org/i 4 a/pages/index. cfm? pageid=3285 • N/A. (n. d. ). Euthanasia & assisted suicide. Retrieved from Lost All Hope: http: //lostallhope. com/suicide-methods • N/A. (n. d. ). Nembutal. Retrieved from Drugs. com: http: //www. drugs. com/mtm/nembutal. html • N/A. (n. d. ). Secobarbital. Retrieved from Drugs. com: http: //www. drugs. com/mtm/secobarbital. html • Unknown. (n. d. ). Euthanasia and physician assisted suicide. Retrieved from BBC: http: //www. bbc. co. uk/ethics/euthanasia/
 Prof jatna supriatna
Prof jatna supriatna Conor donaldson
Conor donaldson Donaldson
Donaldson Dr donaldson urology
Dr donaldson urology Collin donaldson
Collin donaldson Collin donaldson
Collin donaldson Anita donaldson
Anita donaldson Mercurys surface
Mercurys surface Jenna donaldson
Jenna donaldson Collin donaldson
Collin donaldson Donaldson toolbox
Donaldson toolbox Suzanne donaldson
Suzanne donaldson Africa's plea questions
Africa's plea questions Bergie web
Bergie web Colegio baden powell preparatoria
Colegio baden powell preparatoria Welsh powell algorithm python
Welsh powell algorithm python Mekanisme mesin powell
Mekanisme mesin powell Contoh lintasan terpendek
Contoh lintasan terpendek Brett powell
Brett powell Recursos interpretativos
Recursos interpretativos Lake powell and lake mead
Lake powell and lake mead Edwin powell hubble biography
Edwin powell hubble biography Royal college of nursing v dhss 1981
Royal college of nursing v dhss 1981 Algoritma welch powell
Algoritma welch powell Kategori budaya politik dari almond dan powell
Kategori budaya politik dari almond dan powell Budaya politik dari almond dan powell
Budaya politik dari almond dan powell Joe satriani top gun
Joe satriani top gun Beth powell
Beth powell Maggy powell
Maggy powell Brooke powell engaged
Brooke powell engaged Lake powell and lake mead
Lake powell and lake mead Dax powell
Dax powell Gimc eye clinic
Gimc eye clinic![Barton v armstrong [1976] Barton v armstrong [1976]](data:image/svg+xml,%3Csvg%20xmlns=%22http://www.w3.org/2000/svg%22%20viewBox=%220%200%20200%20200%22%3E%3C/svg%3E) Barton v armstrong [1976]
Barton v armstrong [1976] Almond e powell
Almond e powell Powell colin a leadership primer
Powell colin a leadership primer Colin powell 18 rules of leadership
Colin powell 18 rules of leadership Colin powell maud arial
Colin powell maud arial Literal rule in law
Literal rule in law Thermenklinikum baden
Thermenklinikum baden Brief history of scouting
Brief history of scouting Lunch pail inventor
Lunch pail inventor Aldonsa tejada
Aldonsa tejada Welsh-powell algorithm
Welsh-powell algorithm Discus tutorial
Discus tutorial Bayard powell
Bayard powell Powell v alabama
Powell v alabama Brooks secondary powell river
Brooks secondary powell river Neoistituzionalismo
Neoistituzionalismo John powell escritor
John powell escritor











![Barton v armstrong [1976] Barton v armstrong [1976]](https://slidetodoc.com/wp-content/uploads/2020/10/1247166_1fd9c72ecbff2a0a7f2b19308714c341-300x225.jpg)