Fever of Unknown Origin in a 79 year



- Slides: 50
Fever of Unknown Origin in a 79 year old woman Katy Moran, MD September 9, 2003
History § 79 yr old WF admitted to PHD 8/8/03 § CC: intermittant high fevers x 2 weeks § Pt has had approx 2 weeks with high spiking fever 102§ § § 104° F, chills, drenching night sweats, malaise Pt stopped taking methotrexate 3 weeks ago that she has been on for 4 months for rheumatoid arthritis – SE nausea, malaise. Pt has decreased appetite, wt loss 5 -10 lbs over 4 mo. , fatigue, HA when temperature is high, occasional joint pain and stiffness, nausea, weakness, constipation. Denies cough, dyspnea, chest pain, abd pain, urinary sx, neck pain, visual change.
§ PMHx: § § RA dx 4/03, on MTX until 3 weeks ago COPD, spastic dysphonia, hypothyroidism, HTN 1968 - TAH 1981 – Non small cell lung CA s/p LUL resection and radiation § 1989 – Double mastectomy for “precancerous lesions, ” s/p bilateral breast implants § 1999 – CVA § Meds: § Synthroid 75 mcg qd, Advair Diskus bid, Folic acid, Norvasc 10 mg qd, Premarin. 625 mg qd, Plavix 75 mg qd, Leukovorin 5 mg qd day 3/7. Recent d/c MTX 10 mg q week § Allergies: codeine, ASA, PCN
§ SH: § Widowed, lives independently at Medistone apts, quit smoking in 1978 - prior to that smoked heavily. No Et. OH, no drugs. § FH: § Parents and siblings died of heart disease. § ROS: § Occasional sore throat, dizziness. No congestion, diarrhea, rash, SOB, cough, sore throat, recent travel.
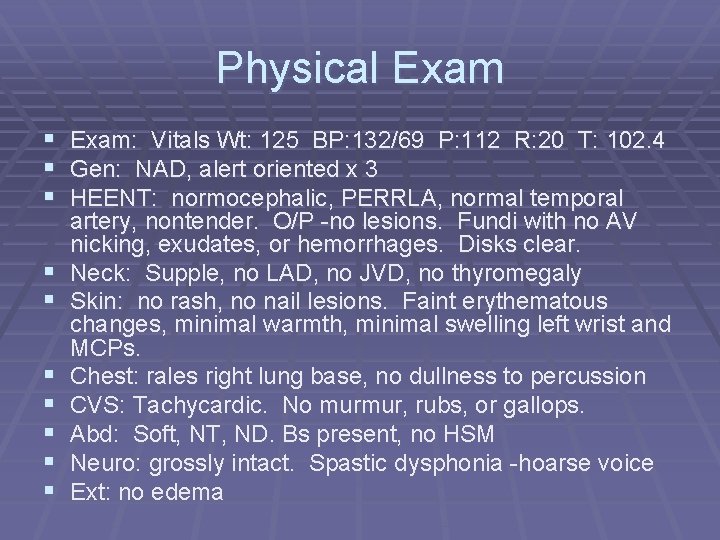
Physical Exam § Exam: Vitals Wt: 125 BP: 132/69 P: 112 R: 20 T: 102. 4 § Gen: NAD, alert oriented x 3 § HEENT: normocephalic, PERRLA, normal temporal § § § § artery, nontender. O/P -no lesions. Fundi with no AV nicking, exudates, or hemorrhages. Disks clear. Neck: Supple, no LAD, no JVD, no thyromegaly Skin: no rash, no nail lesions. Faint erythematous changes, minimal warmth, minimal swelling left wrist and MCPs. Chest: rales right lung base, no dullness to percussion CVS: Tachycardic. No murmur, rubs, or gallops. Abd: Soft, NT, ND. Bs present, no HSM Neuro: grossly intact. Spastic dysphonia -hoarse voice Ext: no edema
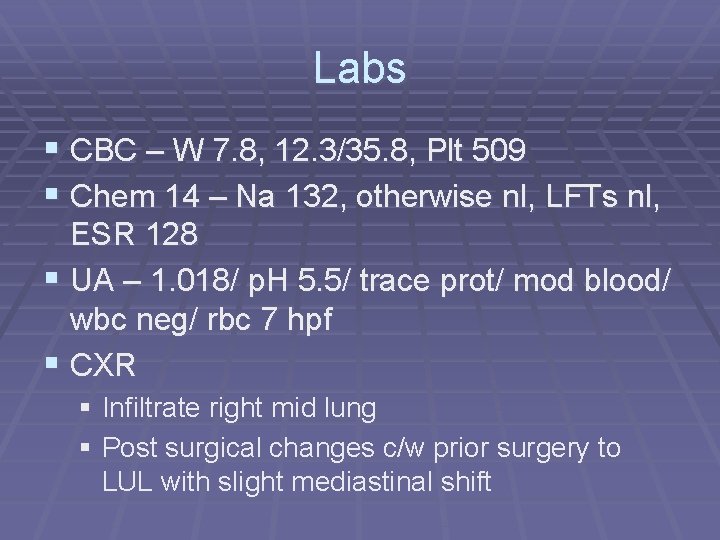
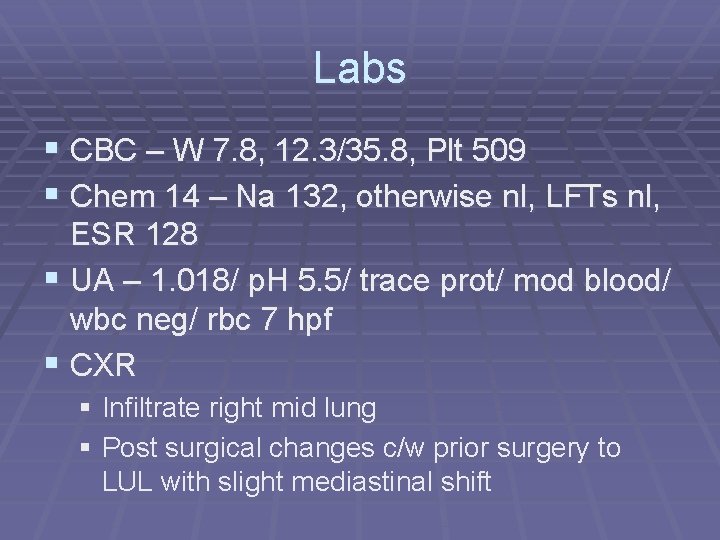
Labs § CBC – W 7. 8, 12. 3/35. 8, Plt 509 § Chem 14 – Na 132, otherwise nl, LFTs nl, ESR 128 § UA – 1. 018/ p. H 5. 5/ trace prot/ mod blood/ wbc neg/ rbc 7 hpf § CXR § Infiltrate right mid lung § Post surgical changes c/w prior surgery to LUL with slight mediastinal shift
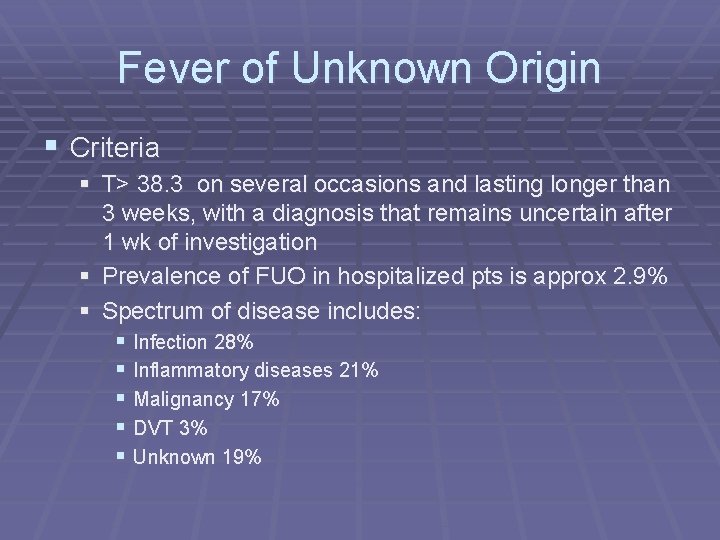
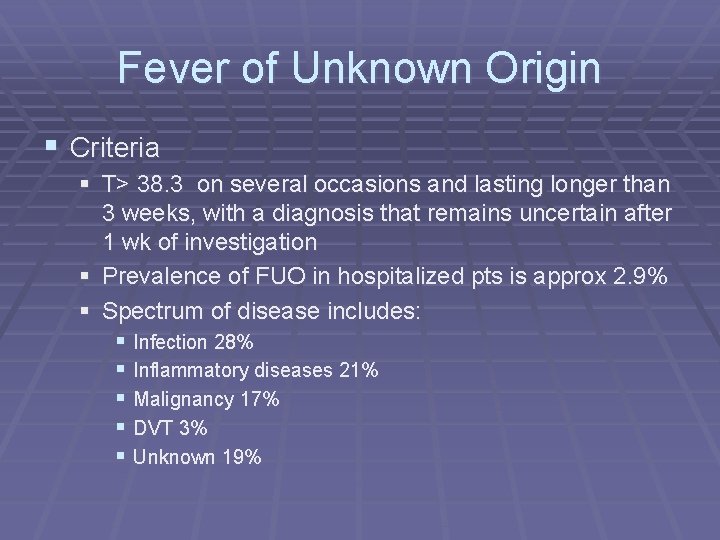
Fever of Unknown Origin § Criteria § T> 38. 3 on several occasions and lasting longer than 3 weeks, with a diagnosis that remains uncertain after 1 wk of investigation § Prevalence of FUO in hospitalized pts is approx 2. 9% § Spectrum of disease includes: § Infection 28% § Inflammatory diseases 21% § Malignancy 17% § DVT 3% § Unknown 19%
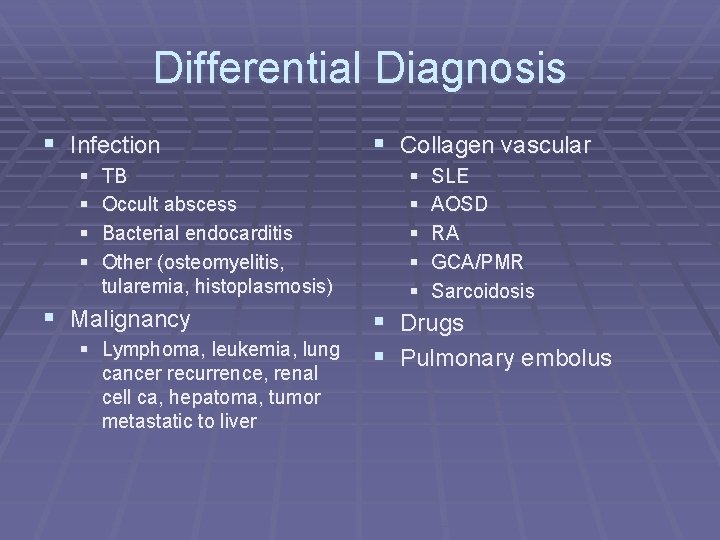
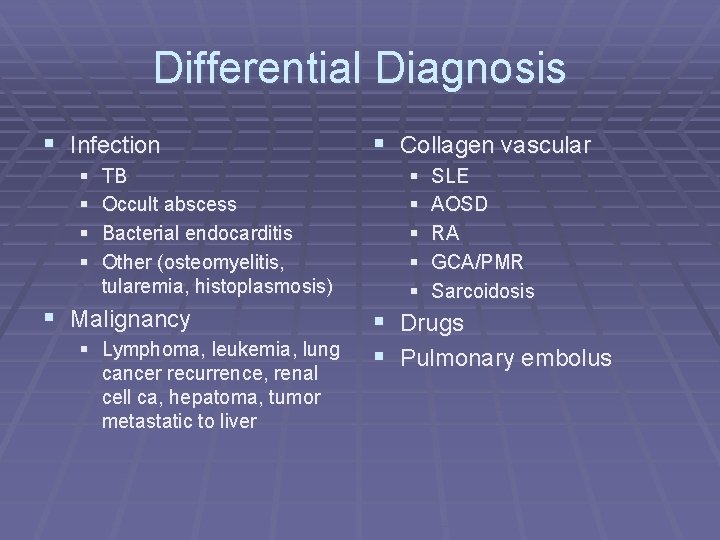
Differential Diagnosis § Infection § § TB Occult abscess Bacterial endocarditis Other (osteomyelitis, tularemia, histoplasmosis) § Malignancy § Lymphoma, leukemia, lung cancer recurrence, renal cell ca, hepatoma, tumor metastatic to liver § Collagen vascular § § § SLE AOSD RA GCA/PMR Sarcoidosis § Drugs § Pulmonary embolus
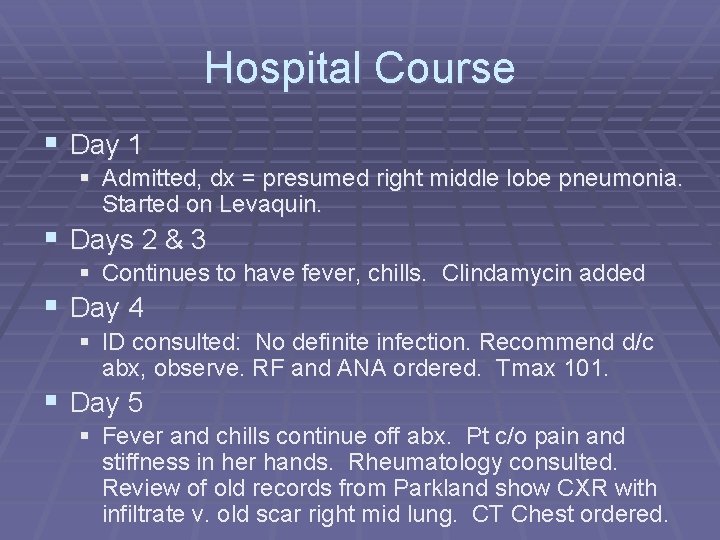
Hospital Course § Day 1 § Admitted, dx = presumed right middle lobe pneumonia. Started on Levaquin. § Days 2 & 3 § Continues to have fever, chills. Clindamycin added § Day 4 § ID consulted: No definite infection. Recommend d/c abx, observe. RF and ANA ordered. Tmax 101. § Day 5 § Fever and chills continue off abx. Pt c/o pain and stiffness in her hands. Rheumatology consulted. Review of old records from Parkland show CXR with infiltrate v. old scar right mid lung. CT Chest ordered.
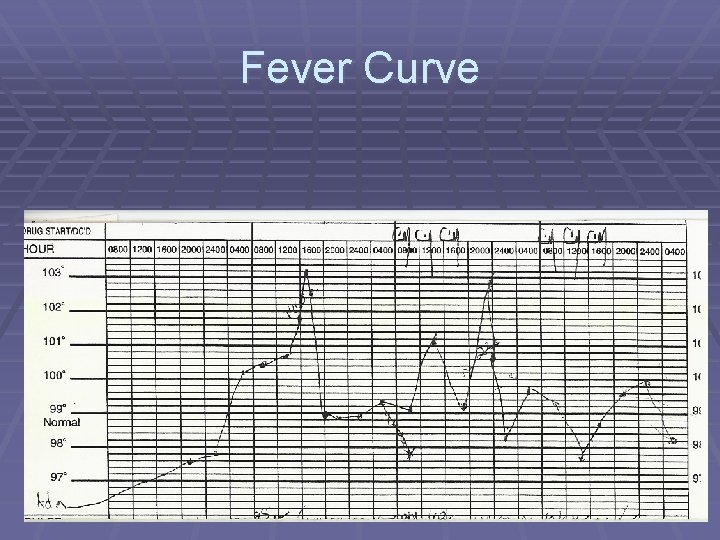
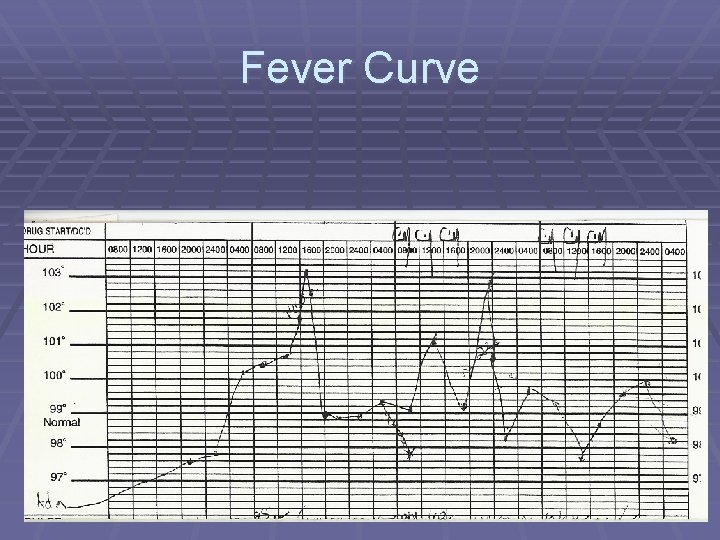
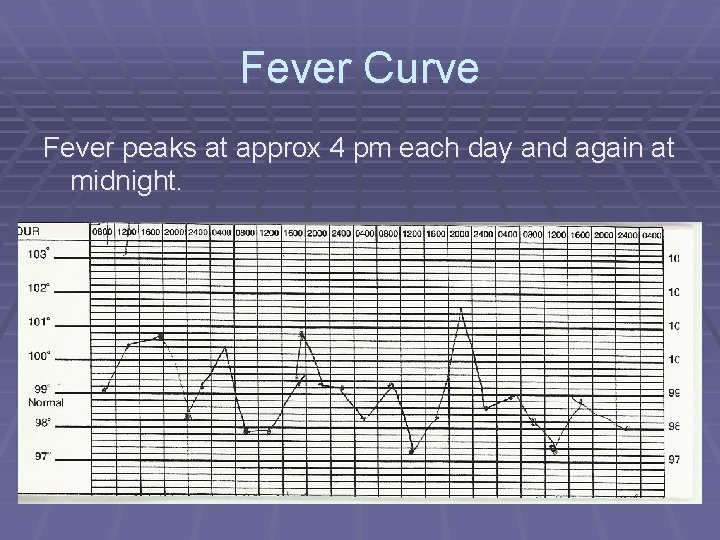
Fever Curve
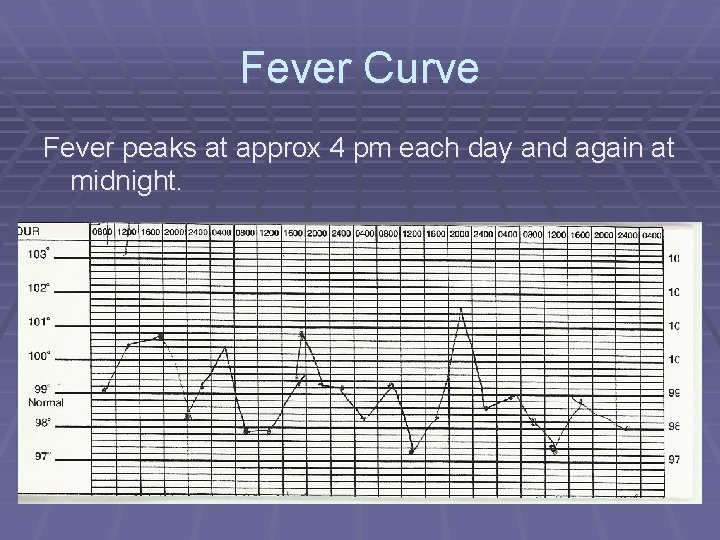
Fever Curve Fever peaks at approx 4 pm each day and again at midnight.
Rheum Evaluation § On further questioning, pt states that since Jan 03 she § § has had several episodes of excruciating pain in her hands. These “attacks” include pain, warmth, and swelling in her MCPs and PIPs. The pain lasts approx 12 hours and is somewhat relieved by Tylenol. Warmth and swelling decrease over a few days. Two ER visits over the last few months when the pain became unbearable Referred to a rheumatologist in the area where she lives, was dx with RA and started MTX. RF was 1: 160. Joint symptoms have improved somewhat over the last few months, but malaise, dyspnea, anorexia, and nausea worsened. Also states she had “black stools” for one week.
Rheum Evaluation § Physical exam § Asymmetric oligoarticular joint swelling in left wrist, right shoulder, right first CMC and MCP, Heberden and Bouchard nodes present bilaterally

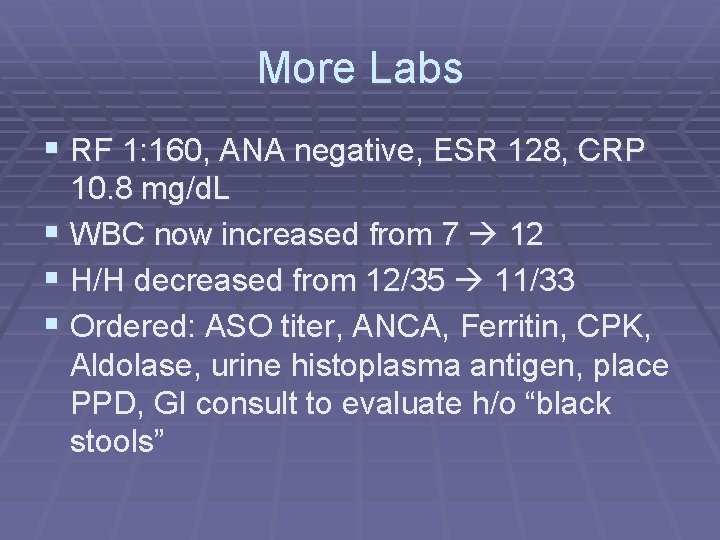
More Labs § RF 1: 160, ANA negative, ESR 128, CRP 10. 8 mg/d. L § WBC now increased from 7 12 § H/H decreased from 12/35 11/33 § Ordered: ASO titer, ANCA, Ferritin, CPK, Aldolase, urine histoplasma antigen, place PPD, GI consult to evaluate h/o “black stools”
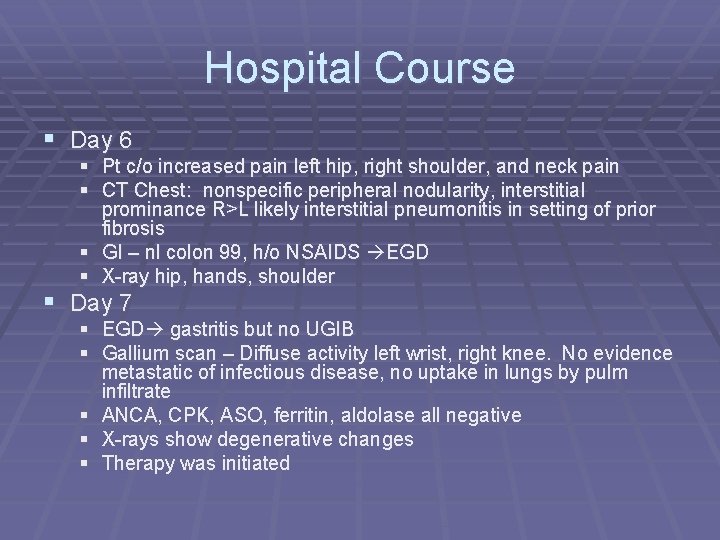
Hospital Course § Day 6 § Pt c/o increased pain left hip, right shoulder, and neck pain § CT Chest: nonspecific peripheral nodularity, interstitial prominance R>L likely interstitial pneumonitis in setting of prior fibrosis § GI – nl colon 99, h/o NSAIDS EGD § X-ray hip, hands, shoulder § Day 7 § EGD gastritis but no UGIB § Gallium scan – Diffuse activity left wrist, right knee. No evidence metastatic of infectious disease, no uptake in lungs by pulm infiltrate § ANCA, CPK, ASO, ferritin, aldolase all negative § X-rays show degenerative changes § Therapy was initiated
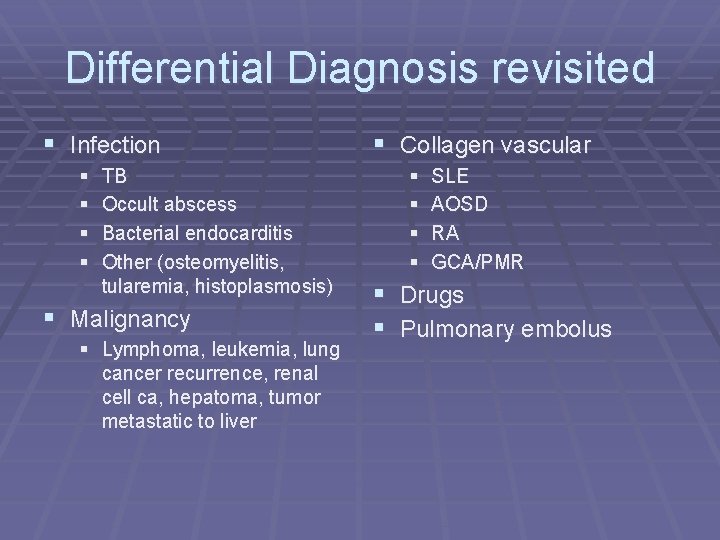
Differential Diagnosis revisited § Infection § § TB Occult abscess Bacterial endocarditis Other (osteomyelitis, tularemia, histoplasmosis) § Malignancy § Lymphoma, leukemia, lung cancer recurrence, renal cell ca, hepatoma, tumor metastatic to liver § Collagen vascular § § SLE AOSD RA GCA/PMR § Drugs § Pulmonary embolus
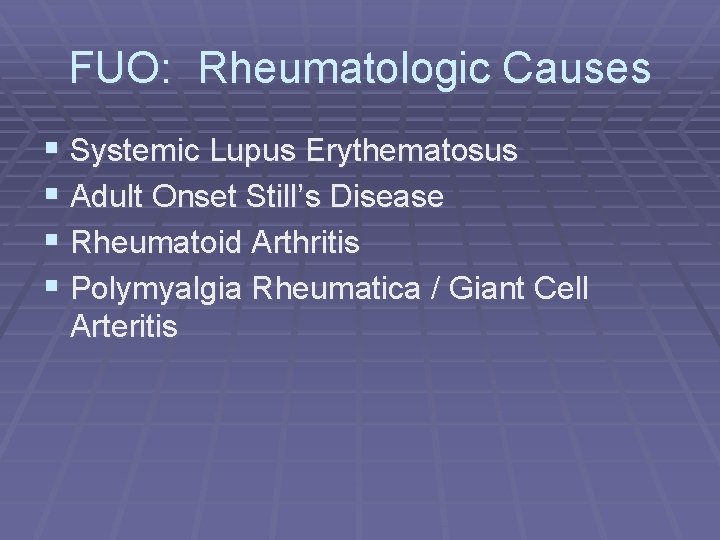
FUO: Rheumatologic Causes § Systemic Lupus Erythematosus § Adult Onset Still’s Disease § Rheumatoid Arthritis § Polymyalgia Rheumatica / Giant Cell Arteritis
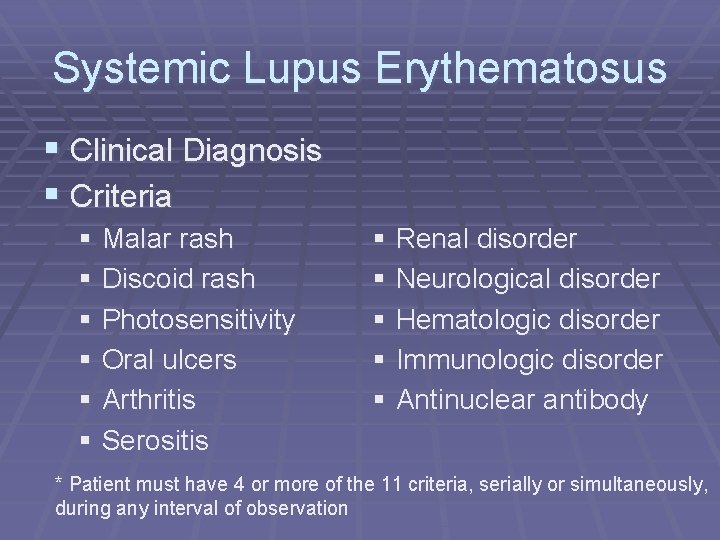
Systemic Lupus Erythematosus § Clinical Diagnosis § Criteria § Malar rash § Discoid rash § Photosensitivity § Oral ulcers § Arthritis § Serositis § Renal disorder § Neurological disorder § Hematologic disorder § Immunologic disorder § Antinuclear antibody * Patient must have 4 or more of the 11 criteria, serially or simultaneously, during any interval of observation
Systemic Lupus Erythematosus § Demographics: § Peak incidence 15 -40 yrs § Female to male ratio 5: 1 § ANA is positive in >95% of cases
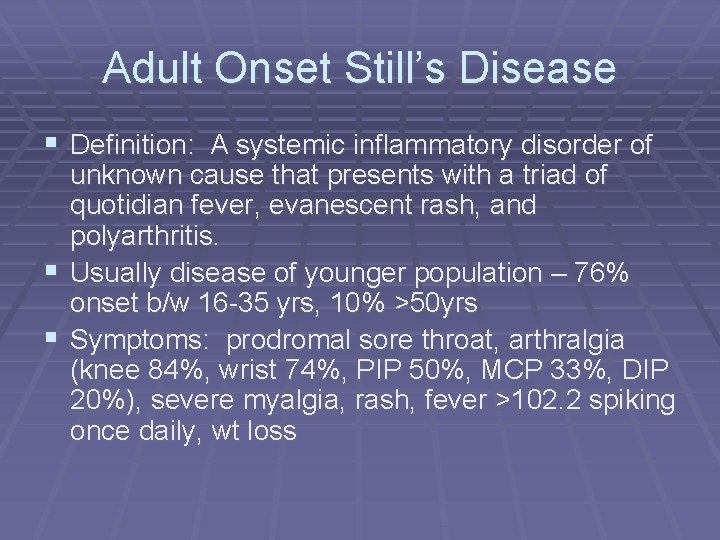
Adult Onset Still’s Disease § Definition: A systemic inflammatory disorder of unknown cause that presents with a triad of quotidian fever, evanescent rash, and polyarthritis. § Usually disease of younger population – 76% onset b/w 16 -35 yrs, 10% >50 yrs § Symptoms: prodromal sore throat, arthralgia (knee 84%, wrist 74%, PIP 50%, MCP 33%, DIP 20%), severe myalgia, rash, fever >102. 2 spiking once daily, wt loss
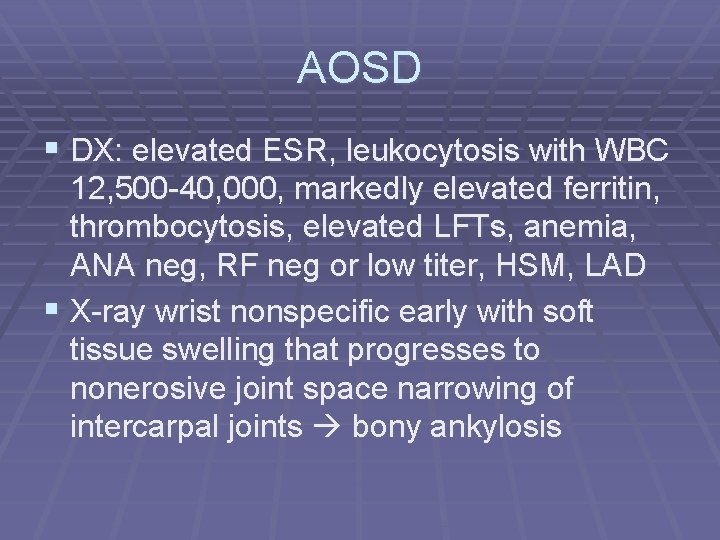
AOSD § DX: elevated ESR, leukocytosis with WBC 12, 500 -40, 000, markedly elevated ferritin, thrombocytosis, elevated LFTs, anemia, ANA neg, RF neg or low titer, HSM, LAD § X-ray wrist nonspecific early with soft tissue swelling that progresses to nonerosive joint space narrowing of intercarpal joints bony ankylosis
AOSD § Most common rheumatologic cause of FUO according to several case series § Clin Rheumatology. 2003 May; 22(2): 8993. § Studied 130 pts with FUO, 36 had collagen vascular disease, of these 36 patients 20 had AOSD according to criteria by Cush, et al. § Intern Med. 1994 Feb; 33 (2): 65 -66.
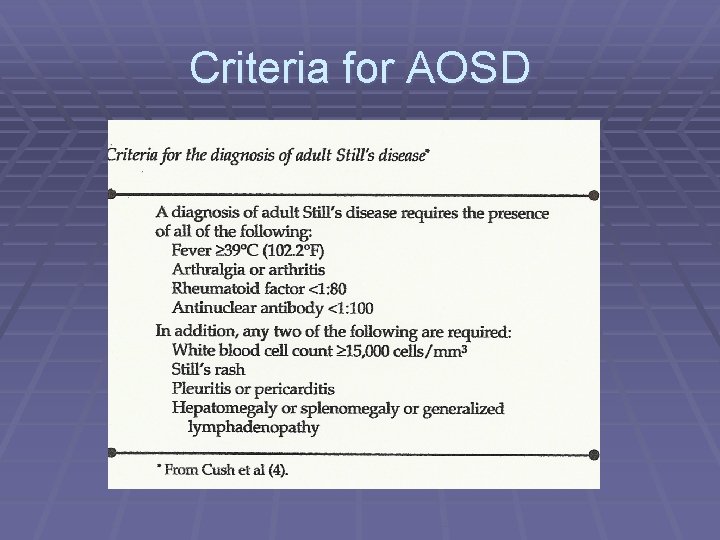
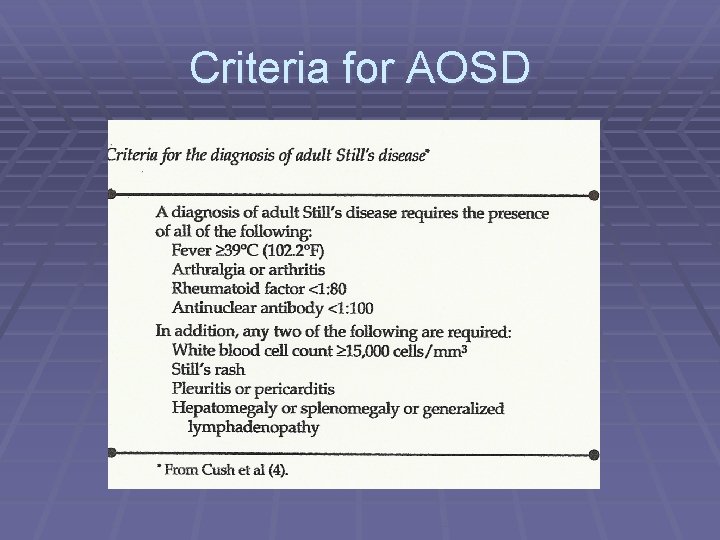
Criteria for AOSD
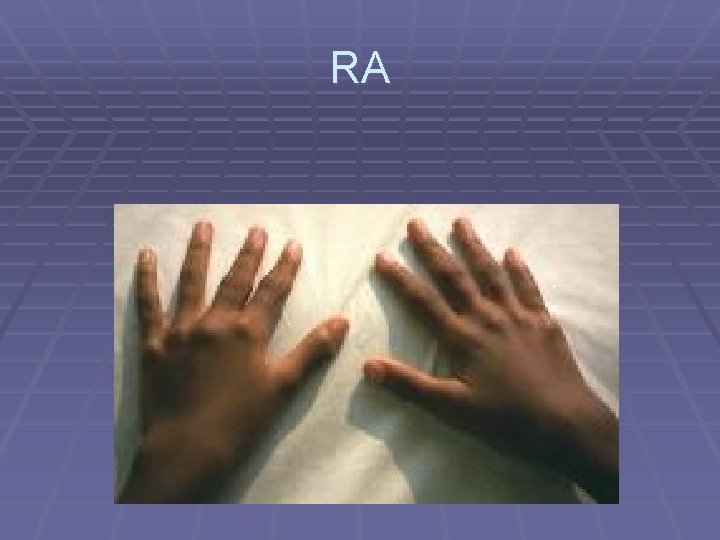
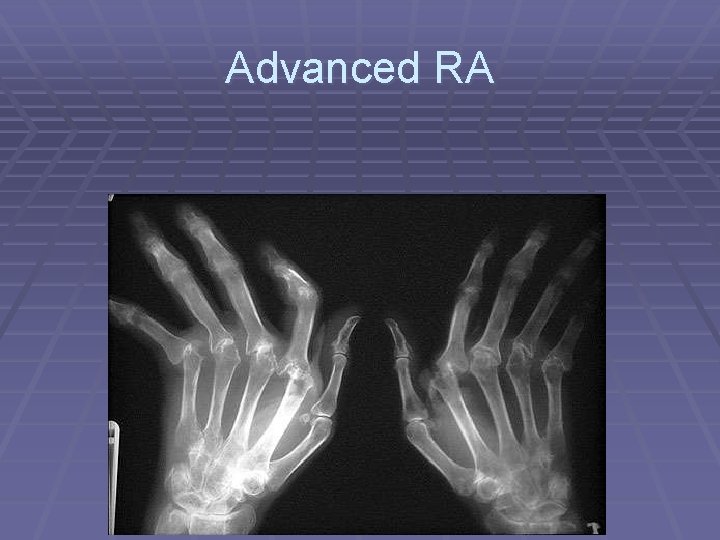
Rheumatoid Arthritis § Definition: Chronic, systemic inflammatory disease with persistent and progressive synovitis in peripheral joints § Peak incidence 4 th-6 th decades § Associated with HLA DR 4 § Sx: Affects small joints of hands and feet. Pts c/o difficulty with tasks like buttoning clothes
Rheumatoid Arthritis § Rheumatoid Factor § Autoantibody with specificity for Fc portion of Ig G § Associated with severe disease § Present in patients with extra articular manifestations such as nodules § Not specific for RA - Detected in normal individuals as well as pts with chronic inflammatory rheumatic diseases, chronic bacterial infection, transplanted organs
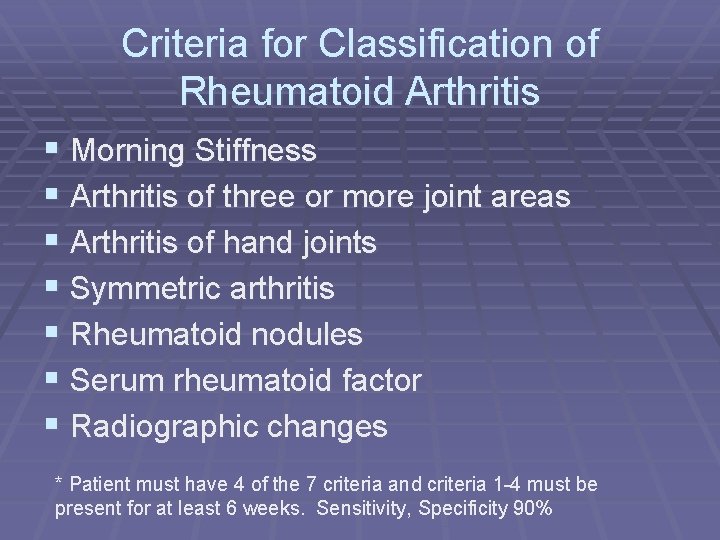
Criteria for Classification of Rheumatoid Arthritis § Morning Stiffness § Arthritis of three or more joint areas § Arthritis of hand joints § Symmetric arthritis § Rheumatoid nodules § Serum rheumatoid factor § Radiographic changes * Patient must have 4 of the 7 criteria and criteria 1 -4 must be present for at least 6 weeks. Sensitivity, Specificity 90%
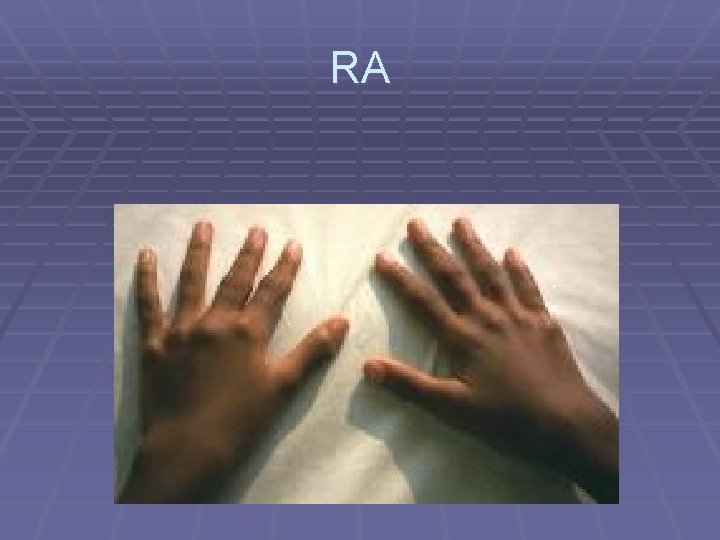
RA
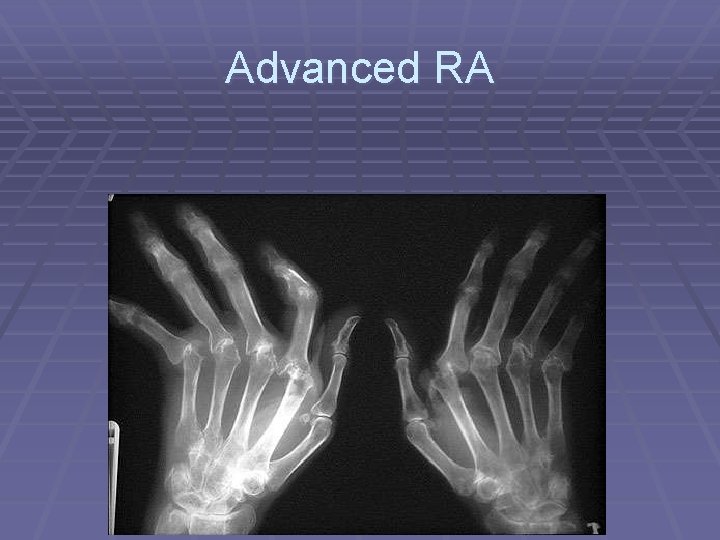
Advanced RA
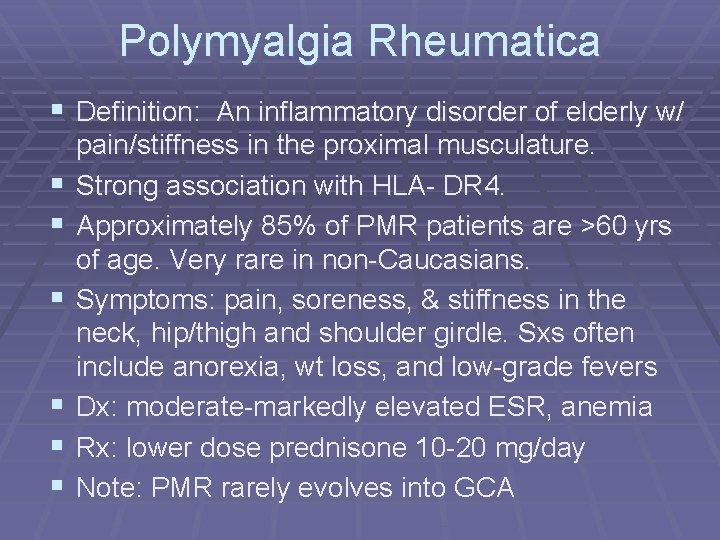
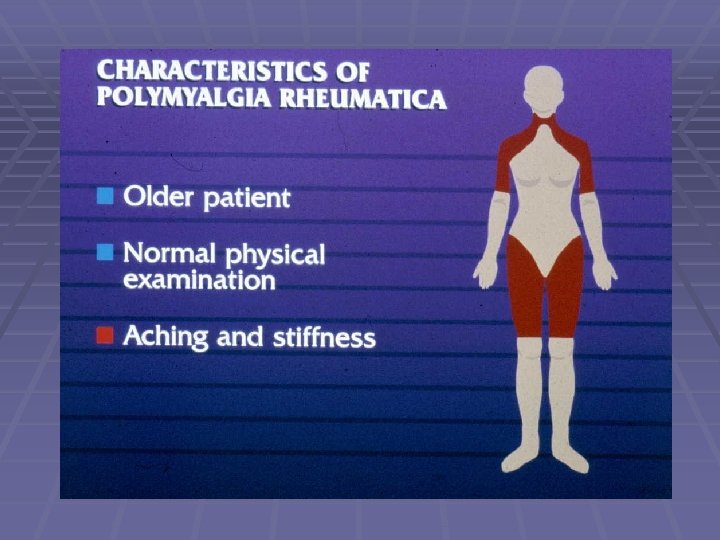
Polymyalgia Rheumatica § Definition: An inflammatory disorder of elderly w/ § § § pain/stiffness in the proximal musculature. Strong association with HLA- DR 4. Approximately 85% of PMR patients are >60 yrs of age. Very rare in non-Caucasians. Symptoms: pain, soreness, & stiffness in the neck, hip/thigh and shoulder girdle. Sxs often include anorexia, wt loss, and low-grade fevers Dx: moderate-markedly elevated ESR, anemia Rx: lower dose prednisone 10 -20 mg/day Note: PMR rarely evolves into GCA
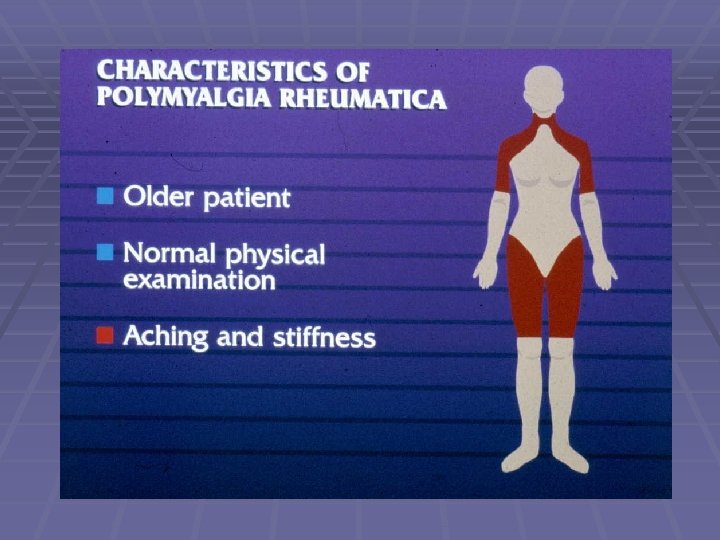
Polymyalgia Rheumatica § Morning stiffness § Prominent finding, lasting 1 -4 hours § Pain and stiffness in shoulder and hip girdle § Problems getting out of bed, rising from a chair, combing hair § In 33% of pts aching is so severe that self care becomes difficult § Low grade fever is most frequent sx, then wt loss, fatigue § If muscles of neck and shoulder are involved pts may be misdiagnosed with frozen shoulder or cervical myelopathy
Polymyalgia Rheumatica § Clinical criteria § Pain, stiffness in at least 2 large muscle groups § Duration >2 weeks without clinical evidence of infection, RA, SLE, PAN, or malignancy § Elevated ESR § Age > 50 § Rapid, lasting relief of symptoms after institution of corticosteroid therapy
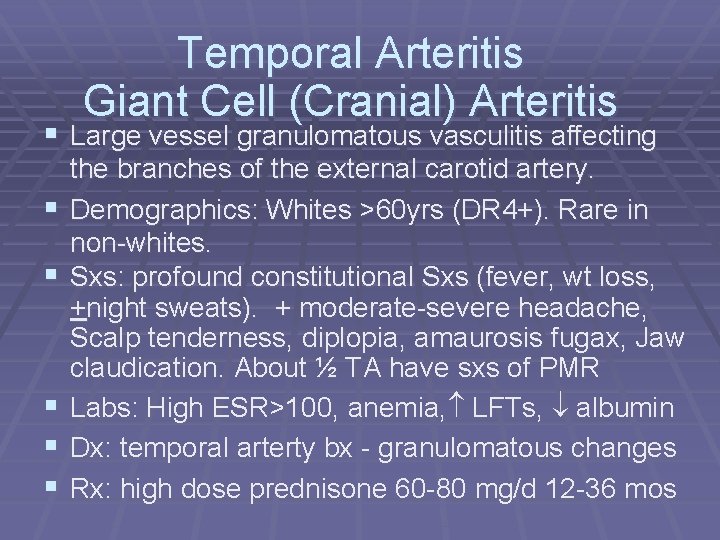
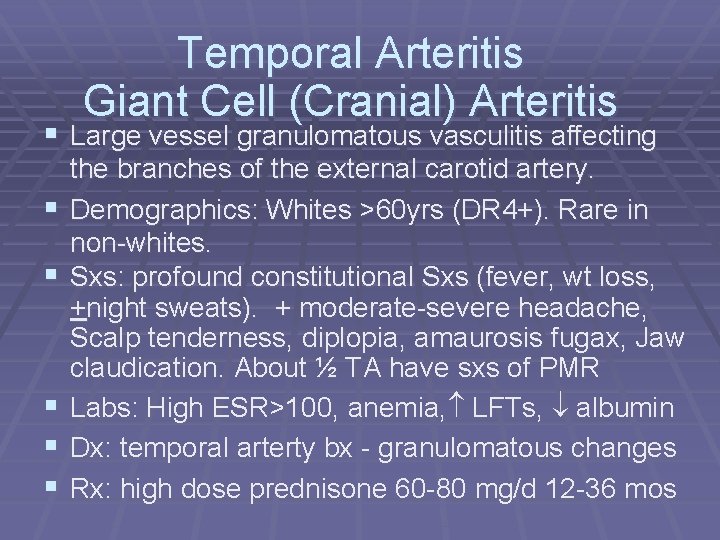
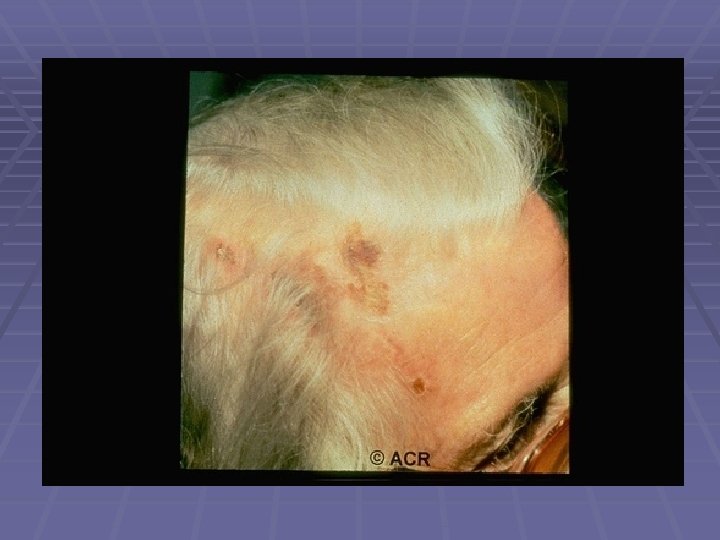
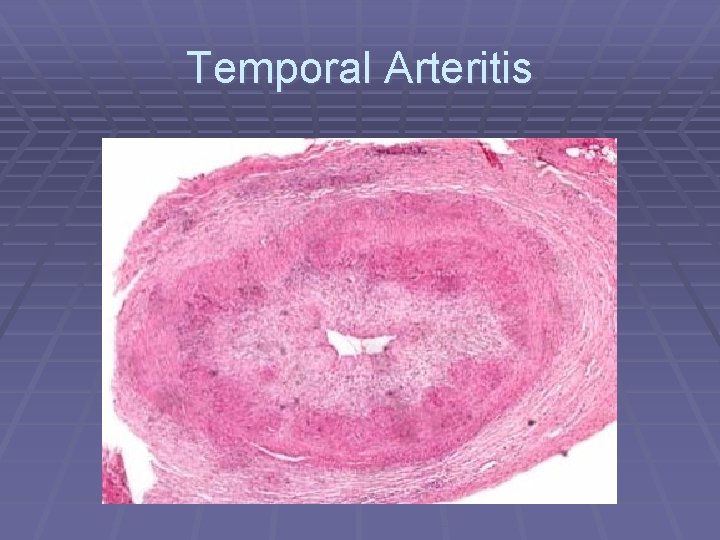
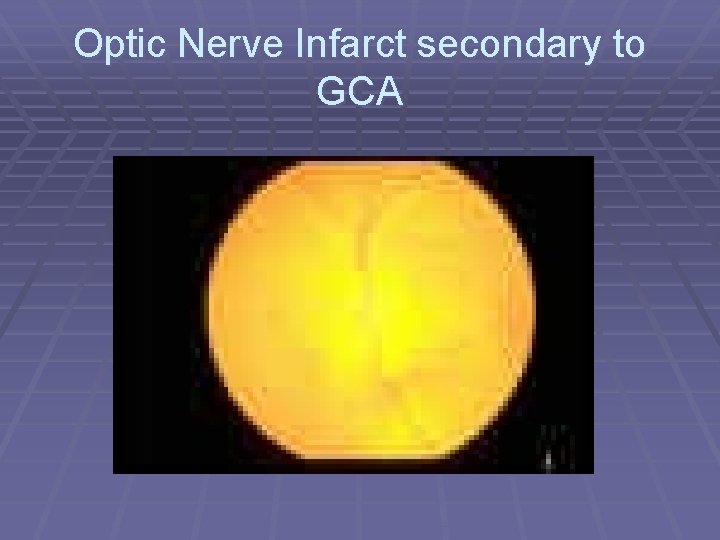
Temporal Arteritis Giant Cell (Cranial) Arteritis § Large vessel granulomatous vasculitis affecting § § § the branches of the external carotid artery. Demographics: Whites >60 yrs (DR 4+). Rare in non-whites. Sxs: profound constitutional Sxs (fever, wt loss, +night sweats). + moderate-severe headache, Scalp tenderness, diplopia, amaurosis fugax, Jaw claudication. About ½ TA have sxs of PMR Labs: High ESR>100, anemia, LFTs, albumin Dx: temporal arterty bx - granulomatous changes Rx: high dose prednisone 60 -80 mg/d 12 -36 mos
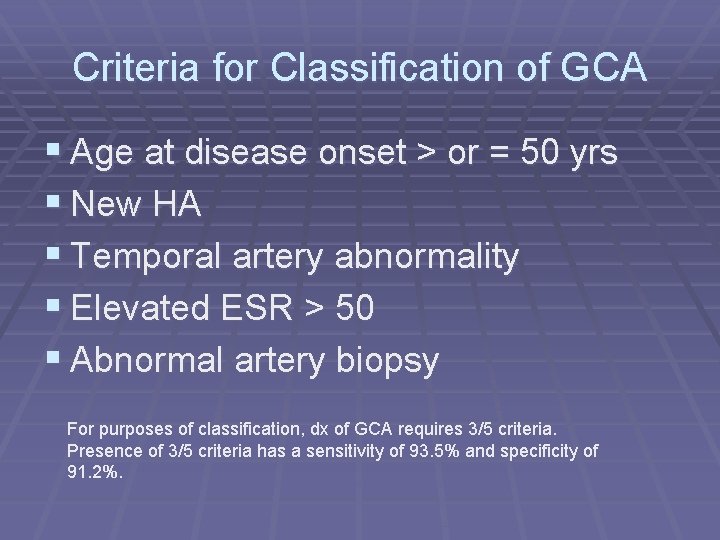
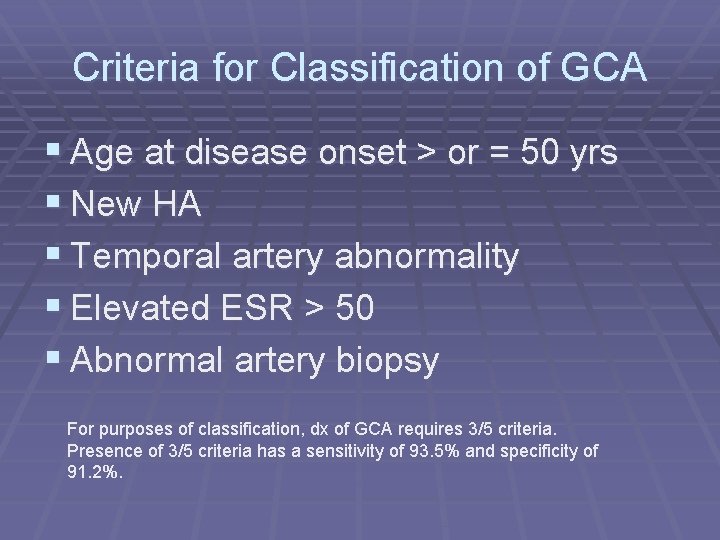
Criteria for Classification of GCA § Age at disease onset > or = 50 yrs § New HA § Temporal artery abnormality § Elevated ESR > 50 § Abnormal artery biopsy For purposes of classification, dx of GCA requires 3/5 criteria. Presence of 3/5 criteria has a sensitivity of 93. 5% and specificity of 91. 2%.
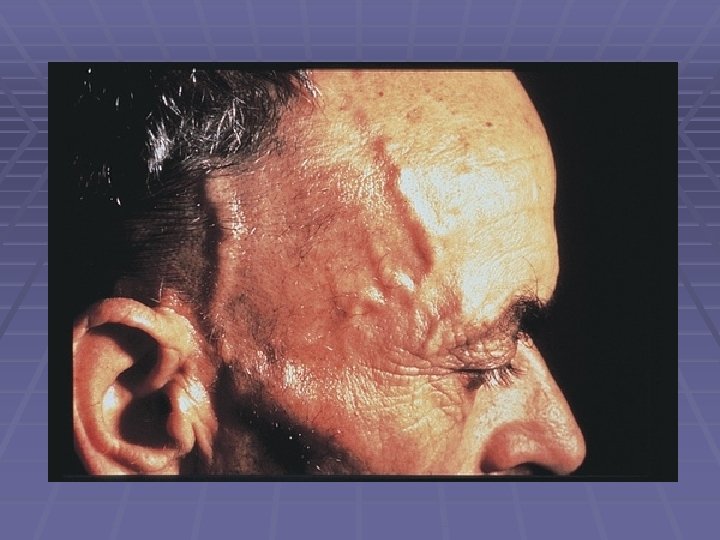
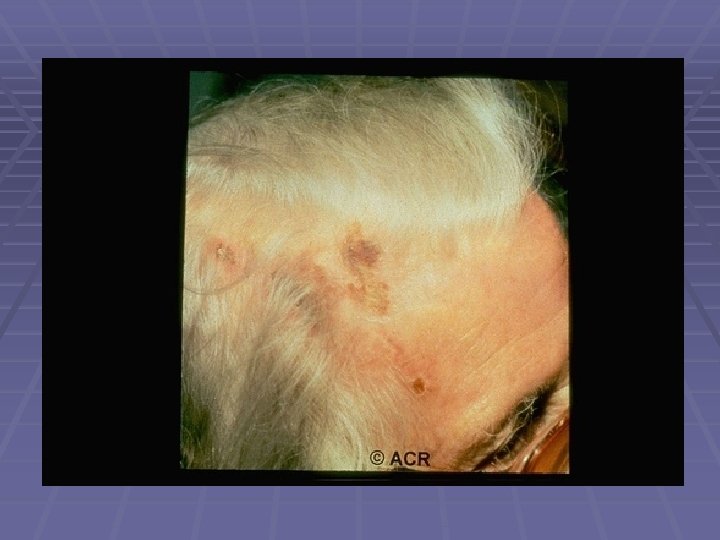
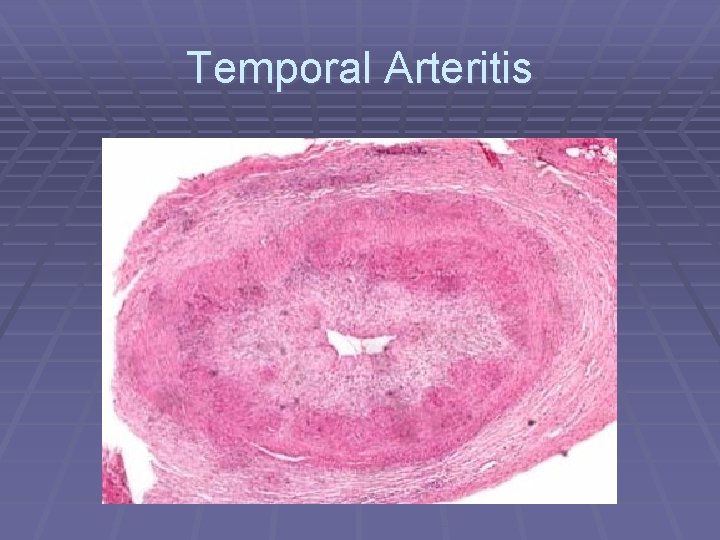
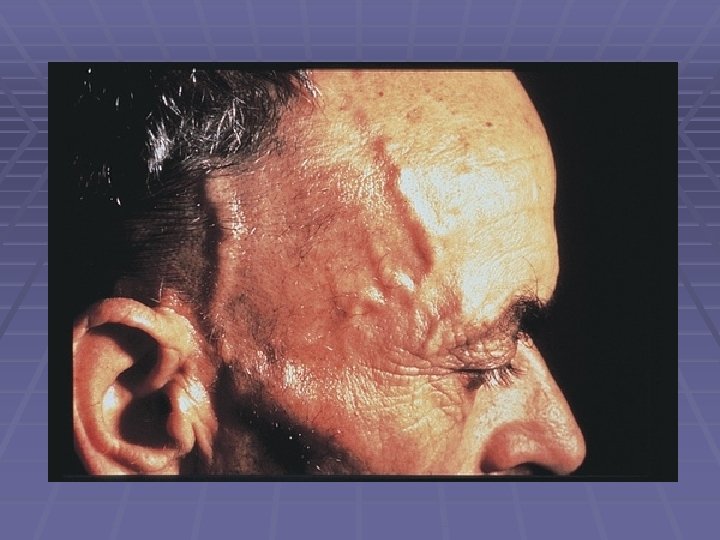
Temporal Arteritis

Temporal Arteritis
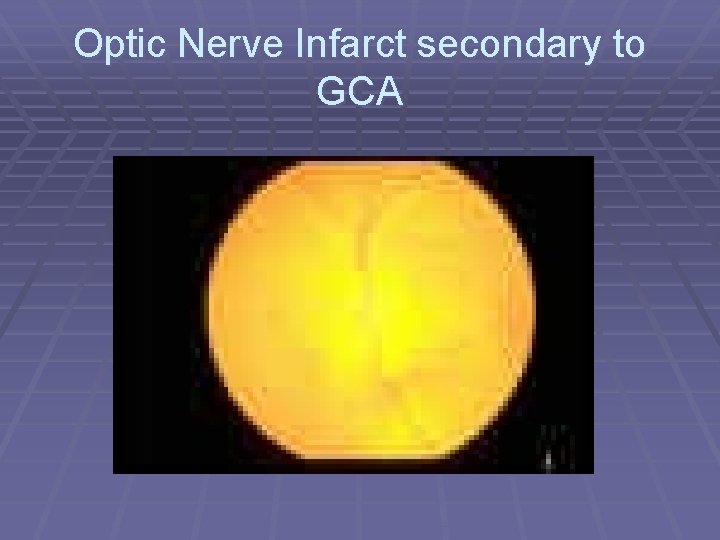
Optic Nerve Infarct secondary to GCA
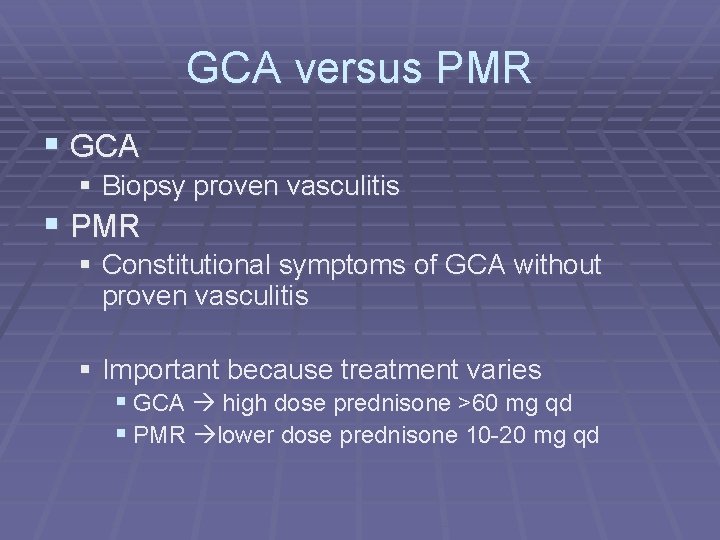
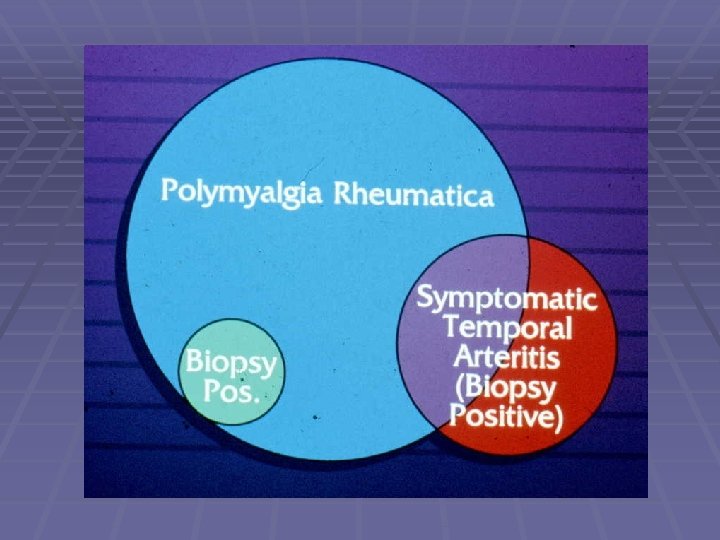
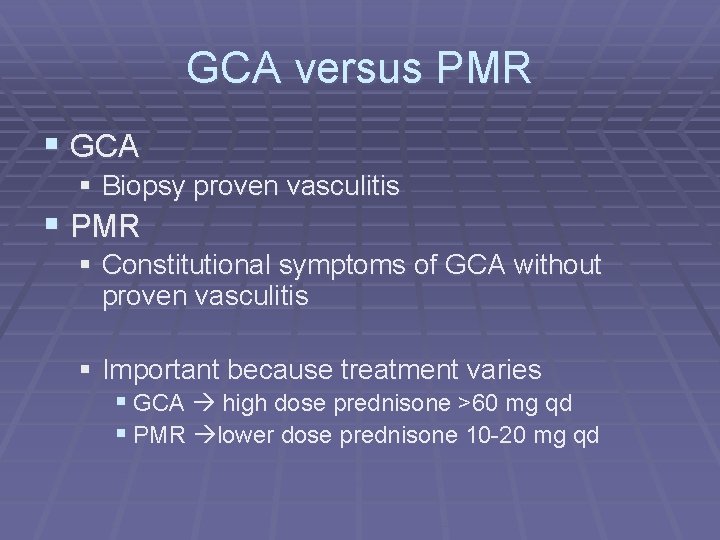
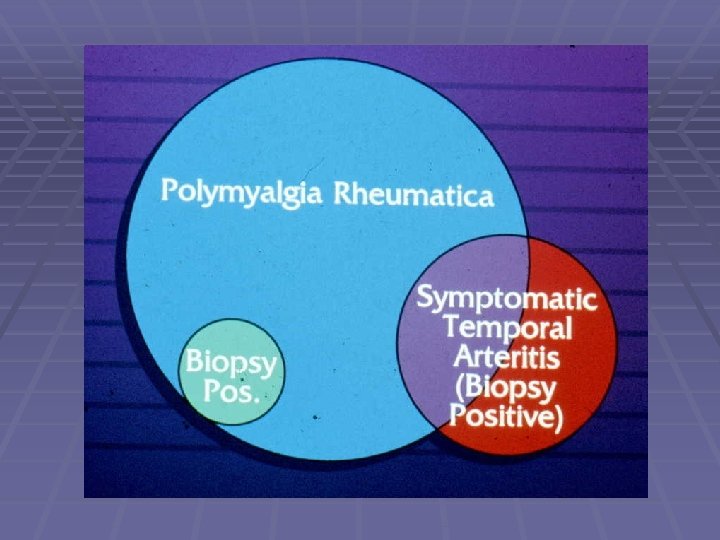
GCA versus PMR § GCA § Biopsy proven vasculitis § PMR § Constitutional symptoms of GCA without proven vasculitis § Important because treatment varies § GCA high dose prednisone >60 mg qd § PMR lower dose prednisone 10 -20 mg qd
GCA versus PMR § Prospective study of 287 patients with PMR and GCA evaluating clinical and lab manifestations at disease onset and at the time of diagnosis § Peripheral arthritis 24% of pts with PMR, none of the patients with GCA § Random sample of 68 pts with “pure” PMR temporal artery biopsy revealed inflammatory changes in 3 pts (4. 4%) § Br J Rheum 1996 Nov; 35(11): 1161 -8.
GCA versus PMR § About half of pts with PMR have distal manifestations in addition to the classic pain and soreness in the proximal joints and muscles § Included are the following: § nonerosive, self-limited, asymmetric peripheral arthritis, especially of the knees and wrists § Carpal tunnel syndrome § Swelling and pitting edema of the dorsum of the hands and wrists

Rheumatologic Comparison AM stiffness Proximal Pain Hand Arthritis Symmetric ESR>80 X-ray Prednisone 10 mg/day Weight loss, anemia PMR RA AOSD ++++ ++/+++ ++ + + +++ pain swelling ++++ ++ ++++ normal abnormal ++++ ++ +/- +++ + +++
§ Day 9 § Pt started on Prednisone 20 mg po qd and had a rapid, dramatic improvement in her sx § 48 hour gallium scan no uptake in lungs, PPD negative, d/c home on Prednisone 20 mg qd with diagnosis of polymyalgia rheumatica
Treatment § GCA Tx: Does adding MTX to prednisone reduce the incidence of GCA relapse? Does it diminish cumulative steroid dose or decrease morbidity resulting from long term steroid therapy? § Evidence is conflicting depending on the study § Annals of Int Med Jan 01 – Small trial that found MTX plus steroid as a safe alternative to prednisone alone with more effective disease control. Double blind placebo controlled § Arthritis Rheumatology April 02 – Larger trial, multicenter, randomized, double blind, placebo controlled. Results did not support the use of MTX as adjunct tx.
Objectives § Rheumatologic causes of FUO § PMR § GCA
Resources § Primer on Rheumatic Disease, Klippel et al. § Fever of unknown origin in elderly patients. J Am Geriatric Soc. 1993 Nov; 41 (11): 1187 -92. § Fever of unknown origin in a 71 year old woman. Am J Med 1985 Sep; 79 (3): 373 -84. § Fever of unknown origin: a review of 20 patients with AOSD. Clin Rheumatol. 2003 May; 22(2): 89 -93. § Fever of unknown origin: a review of 80 patients from the Sin’etsu area of Japan from 1986 -1992. Intern Med. 1994 Feb; 33(2): 65 -66.
Resources § Fever of unknown origin: a changing diagnostic spectrum. § § § Intern Med 1994 Feb; 33(2): 65 -6. Pyrexia of unknown origin. BMJ 1997 Feb; 314: 583 -6. A comprehensive evidence based approach to FUO. Arch Intern Med 2003 Mar 10; 163 (5): 545 -51. Clinical problem- solving. Diagnosis still in question. N Engl J Med 2002 Jun 6; 346 (23): 1813 -6. Medium and Large Vessel Vasculitis. N Engl J Med 2003 July 10; 349 (2) : 160 -9. Medical Progress: PMR and GCA. N Engl J Med 2002 July 25; 347(4): 261 -71. Approach to the pt with FUO. Br J Rheum 1996 Nov; 35(11): 1161 -8.