Fenomenet agitasjon Hvorfor er dette viktig i klinikken

- Slides: 23
Fenomenet agitasjon. Hvorfor er dette viktig i klinikken? Arne Vaaler
Covering • What is agitation? • Definitions / assessments. • Epidemiological aspects • Clinical consequences / burden of illness. • Suicide and agitation • Conclusions.
What is agitation? - «Something every clinician know when they see it» . Common component of many disorders. Seldom addressed as a unique medical or psychiatric entity. • A cluster of behaviours occuring in a number of clinical situations. • A heterogeneous, dimensional concept crossing multiple diagnostic areas in medicine and psychiatry. Core symptoms: Restlessness, excessive verbal and motor activity, irritability, unability to cooperate, threats… and violent incidents. Vegetative symptoms as decreased sleep. Unstable, fluctuating course with symptoms rapidly changing over time.
Frequent in: • Psychiatric conditions: Schizophrenia, affective disorders, ADHD, personality, anxiety… • Central nervous system diseases: Epilepsy, dementia, Mb Parkinson’ • Medical conditions: Encephalitis, diabetes, thyrotoxicosis, brain trauma. • Substance abuse: Alcohol, methamphetamine, GHB (gamma-hydroxybutyric acid)… • Side effects medication: Antipsychotics and antidepressants. … and combinations of all.
Definitions. A number of often imprecise and/or conflicting defintions. Sachs. J Clin Psychiatry 2006. • «Excessive motor activity associated with a feeling of inner tension» APA. DSM-4. • «Agitation is an non-specific constellation of comparatively unrelated behaviours that possess a risk to the safety of the patient or caregiver, impedes the process of care giving or impairs a person’s function» . Yildis et al. Emerg Med J 2000 • Agitation is «a temporary disruption of the typical phycisian – patient collaboration, which interferes with assessment and treatment, during a period when immediate assessment and treatment are needed» . Allen. J Clin Psychiatry 2000.
Definitions – differences and similarities. • Agitation is seen by many specialists. Psychiatry, emergency medicine, GP, neurology. . • Clinicians view agitation primarily from the perspective of own patient population. -Emergency physicians describe agitation in terms of broader range of symptoms. -Geriatricians describe it reflecting syndromes commonly in the elderly. • The definitions in the literature tend to vary with the illnesses in focus. Shared factors in the different definitions: «Increase in motor activity; aggression; disinhibition and impulsivity; and irritable, anxious or labile mood» . Battaglia. Drugs 2005; 65.
Assessment of agitation. • A number of rating scales in use. Zeller&Rhoades. Clin Ther 2010. • The lack of precision in the definitions of the clinical syndrome is reflected in significant differences in the assessment approaches and rating scales. Sachs. J Clin Psychiatry 2006. • Better utility in the assessment of interventions than in epidemiologic or pathophysiologic research. Lindenmayer. J Clin Psychiatry 2000.
Severity of agitation. • A spectrum of behaviours from mild to severe. . with rapid fluctuations. • Anxiety…. High anxiety…Agitation…Aggression. In some patients: • Agitation a warning sign of aggression. • Severity of untreated agitation increases with time. • Violence in agitated patients preceded by increased pacing and loud speech.
Agitation in psychiatric acute and emergency psychiatry. «Epidemiology» • At present lack of direct epidemiological studies assessing prevalence, clinical impact, short / long time consequences, and financial costs. Sachs. J Clin Psychiatry 2006 • Existing data derived from patients visiting emergency settings. Different populations, rating scales, organization of services… Severity of agitation. Studies with / without informed consent. • The typical contemporary psychiatric intensive care patient presents in severe crisis, often complicated by substance use, polypharmacy, behavioural dyscontrol and multiple axis 1 -2 diagnoses. Zealberg&Brady. Emergency Psychiatry 1999. • Present data an indication of «the burden of illness» .

Epidemiology / «burden of illness» . • Agitated or violent behaviour in 10 % emergency psychiatry visits worldwide. Raveendran et al. BMJ 2007. Mc. Allister-Williams&Ferrier. Br J Psychiatry 2002. Tardiff&Koeningsberg. Am J Psychiatry 1985. Huf et al. Cochrane Database Syst Rev 2005. • 20 – 50 % of emergency patients in US «at risk» for agitation Allen&Currier. Gen Hosp Psych 2005. • 21 % of emergency visits may involve agitated patients with schizophrenia. 13 % bipolar disorders. Marco&Vaughan. Am J Emerg Med 2005. • Total number of emergency visits in US potentially involving agitation 1. 7 million annually. Sachs. J Clin Psychiatry 2006
«The psychiatric emergency research collaboration-01» • Retrospective, structured chart review on psychiatric emergency services patients. . . the interface between community and institution. • Nine US sites. • Agitation in 52 % of the subjects US. • Specific anti-agitation medication in 48 %. Physically restrained 6 %. • Self-harm ideation 55 %. • Admitted to inpatient unit 45 %. Boudreaux et al. Gen Hosp Psychiatry 2009.
Consequences of agitation. Two examples. 1: Coercive measures in inpatient care. Keski-Valkama et al. «The reason for using restraint and seclusion in psychiatric inpatient care: A nationwide 15 -year study» . Nord J Psychiatry 2010; 64. Aims: - To study the reasons for restraint / seclusion, and changes in reasons over a 15 -year period. - Law revisions 1991 and 2001 with explicit aims to reduce restraint / seclusion Method: - A structured postal survey to all actual Finnish hospitals in a predetermined week in 1990, 1991, 1994, 1998 and 2004. - Categories for reason: Actual violence; threatening violence; damaging property; threatening to damage property; agitation / disorientation; unclass.
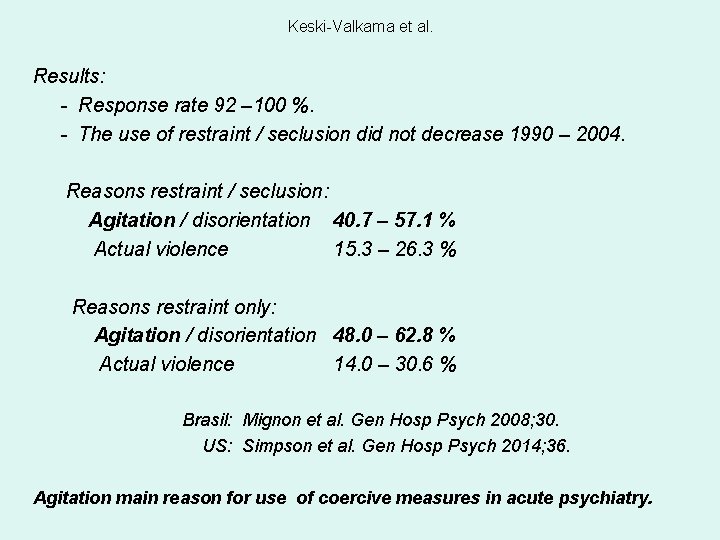
Keski-Valkama et al. Results: - Response rate 92 – 100 %. - The use of restraint / seclusion did not decrease 1990 – 2004. Reasons restraint / seclusion: Agitation / disorientation 40. 7 – 57. 1 % Actual violence 15. 3 – 26. 3 % Reasons restraint only: Agitation / disorientation 48. 0 – 62. 8 % Actual violence 14. 0 – 30. 6 % Brasil: Mignon et al. Gen Hosp Psych 2008; 30. US: Simpson et al. Gen Hosp Psych 2014; 36. Agitation main reason for use of coercive measures in acute psychiatry.
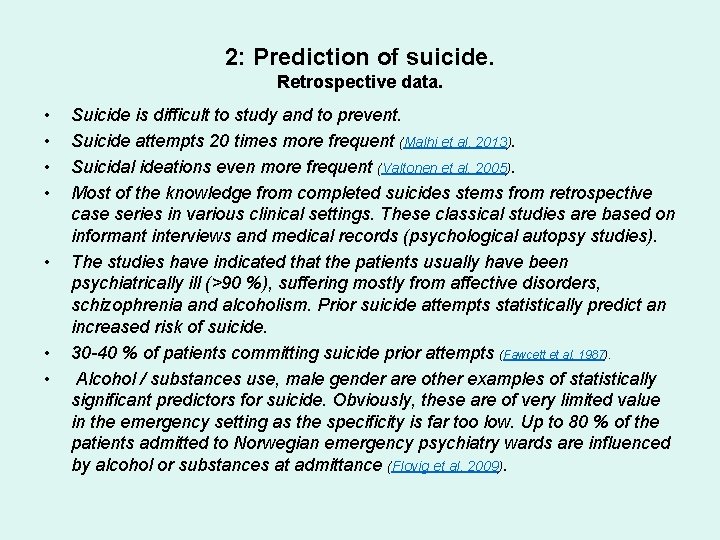
2: Prediction of suicide. Retrospective data. • • Suicide is difficult to study and to prevent. Suicide attempts 20 times more frequent (Malhi et al. 2013). Suicidal ideations even more frequent (Valtonen et al. 2005). Most of the knowledge from completed suicides stems from retrospective case series in various clinical settings. These classical studies are based on informant interviews and medical records (psychological autopsy studies). The studies have indicated that the patients usually have been psychiatrically ill (>90 %), suffering mostly from affective disorders, schizophrenia and alcoholism. Prior suicide attempts statistically predict an increased risk of suicide. 30 -40 % of patients committing suicide prior attempts (Fawcett et al. 1987). Alcohol / substances use, male gender are other examples of statistically significant predictors for suicide. Obviously, these are of very limited value in the emergency setting as the specificity is far too low. Up to 80 % of the patients admitted to Norwegian emergency psychiatry wards are influenced by alcohol or substances at admittance (Flovig et al. 2009).
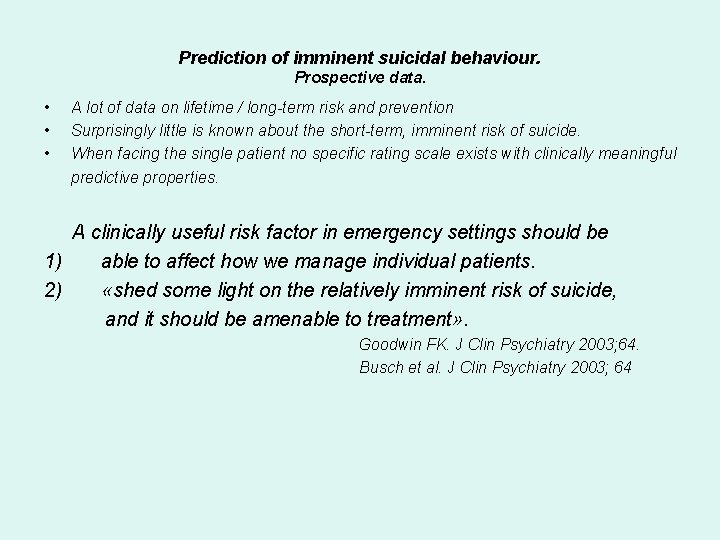
Prediction of imminent suicidal behaviour. Prospective data. • • • A lot of data on lifetime / long-term risk and prevention Surprisingly little is known about the short-term, imminent risk of suicide. When facing the single patient no specific rating scale exists with clinically meaningful predictive properties. A clinically useful risk factor in emergency settings should be 1) able to affect how we manage individual patients. 2) «shed some light on the relatively imminent risk of suicide, and it should be amenable to treatment» . Goodwin FK. J Clin Psychiatry 2003; 64. Busch et al. J Clin Psychiatry 2003; 64
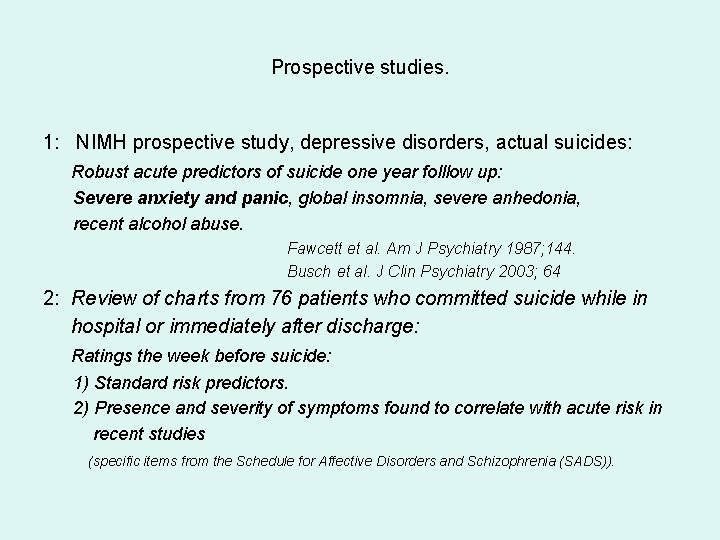
Prospective studies. 1: NIMH prospective study, depressive disorders, actual suicides: Robust acute predictors of suicide one year folllow up: Severe anxiety and panic, global insomnia, severe anhedonia, recent alcohol abuse. Fawcett et al. Am J Psychiatry 1987; 144. Busch et al. J Clin Psychiatry 2003; 64 2: Review of charts from 76 patients who committed suicide while in hospital or immediately after discharge: Ratings the week before suicide: 1) Standard risk predictors. 2) Presence and severity of symptoms found to correlate with acute risk in recent studies (specific items from the Schedule for Affective Disorders and Schizophrenia (SADS)).
Results. - 49 % prior suicide attempt. - 39 % admitted for suicidal ideations. - 78 % denied suicidal ideation in their last communication about the topic. 79 % met criteria for severe or extreme anxiety and/or agitation. • Conclusion: - Standard risk assessments and precautions used were of limited value in protecting the group from suicide. - Adding severity of anxiety and agitation to our current assessment may help identify patients at acute risk and suggest effective treatment interventions. - «Effective anxiolytic medication hardly used at all» .
Sani et al. Psychiatr Clin Neurosci 2011. Aims: Identify predictors for completed suicide. Methods: 4441 inpatients followed for some time during 35 years. Mostly affective disorders. Conclusion: «Suicide is likely to occur in a milieu of agitation, mixed anxiety and depression, and psychosis» . Severe agitation predicts imminent suicidal acts.
Agitasjon og suicid • Medikamenter: Antidepressiva kan utløse og forsterke agitasjon. Vaaler&Fasmer. Tidsskr Nor Legefor 2013 Antidepressiva kan utløse suicidale kriser hos pasienter med agiterte depresjoner. Reeves&Ladner. CNS Neurosci Ther 2010. Primær suicidforebyggende terapi bør fokusere på agitasjon.
Den suicidale «prosess» . • Det er en myte at denne prosessen tar lang tid. • > 50 % < ti minutter. • Alvorlige suicidale handlinger er et impulsivt fenomen. Deisenhammer et al. J Clin Psychiatry 2009. Goodwin. J Clin Psychiatry 2003. Pearson et al. Suicide and life threat behav 2002. «Attempted suicide among rural women in People’s Republic of China: possibilities for prevention» . Alvorlig depresjon med agitasjon krever umiddelbar handling!
Goodwin. «Preventing inpatient suicide» . J Clin Psychiatry 2003. • • Predictors free of recall bias. Male, suicide ideation, prior attempt not associated with acte risk (first year) • A useful clinical predictor should indicate imminent risk, affect management, and be amenable to treatment. • Robuste acute predictors severe anxiety, panic, global insomnia, severe anhedonia, and recent alcohols abuse. • Misleading: Absence of suicidal ideation. Prior attempt. . < 50 %. • Preventive interventions: IO 15 min fell short (50 % suicd). No-harm contracts. • What should work: Aggressive pharmacological management of anxiety, panic, agitation and insomnia.
Språk og holdninger • Selvmord vs suicid. • Norsk vs engelsk…? • Selvmord assosieres med «selvdrap» ? • En aggressiv handling…? • En aggressor. • Overgriper vs offer.
Conclusions. • Regardless of underlaying etiology, severe agitation is an emergency. • A predictor for violence and use of coercive measures. • A very important predictor for imminent suicidal acts. • Immediate interventions to control symptoms and prevent injury. • Together with therapeutic measures like «talking down» fast acting medication is mandatory.
 Hvorfor er mangfold viktig
Hvorfor er mangfold viktig Storbritannien industriella revolutionen
Storbritannien industriella revolutionen Hva er mim
Hva er mim Agitasjon
Agitasjon Dette mezzanine
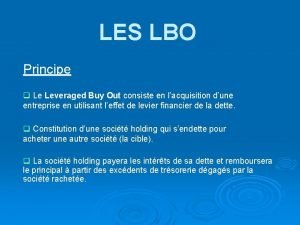
Dette mezzanine Lbo exemple chiffre
Lbo exemple chiffre Dette er min lengsel å ære deg
Dette er min lengsel å ære deg Otera capital
Otera capital Hva betyr dette
Hva betyr dette Markedssegmentering
Markedssegmentering Hvorfor feirer vi 17
Hvorfor feirer vi 17 Hvorfor sluttet den kalde krigen
Hvorfor sluttet den kalde krigen Regresserer
Regresserer Pea hjerterytme
Pea hjerterytme Hvorfor kaldes thisted for en klimakommune
Hvorfor kaldes thisted for en klimakommune Tinderbox målgruppe
Tinderbox målgruppe Hvorfor ser vi farger
Hvorfor ser vi farger Hvorfor pinse
Hvorfor pinse Hvorfor segmentere
Hvorfor segmentere Hinduismen arkitektur
Hinduismen arkitektur Elring uddannelser
Elring uddannelser