Fatty Liver Disease Definition A clinicopathologic syndrome encompassing
- Slides: 18
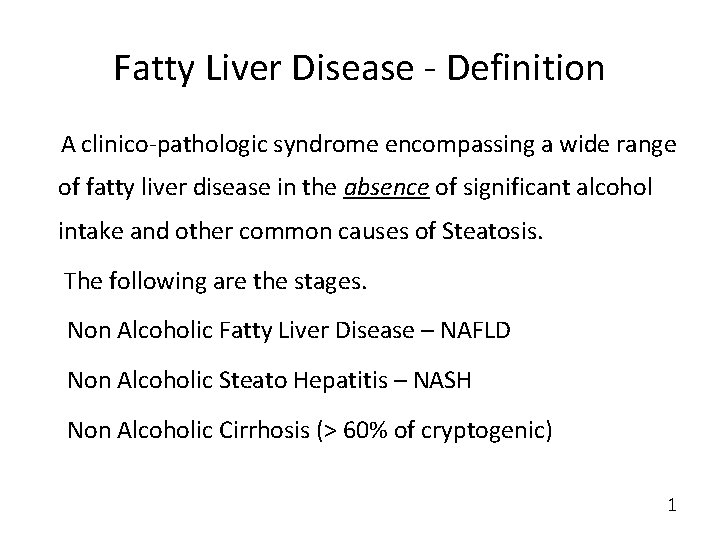
Fatty Liver Disease - Definition A clinico-pathologic syndrome encompassing a wide range of fatty liver disease in the absence of significant alcohol intake and other common causes of Steatosis. The following are the stages. Non Alcoholic Fatty Liver Disease – NAFLD Non Alcoholic Steato Hepatitis – NASH Non Alcoholic Cirrhosis (> 60% of cryptogenic) 1
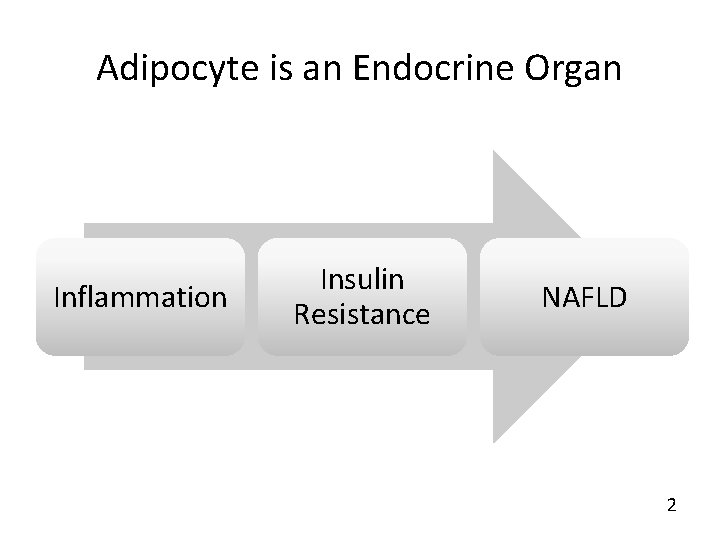
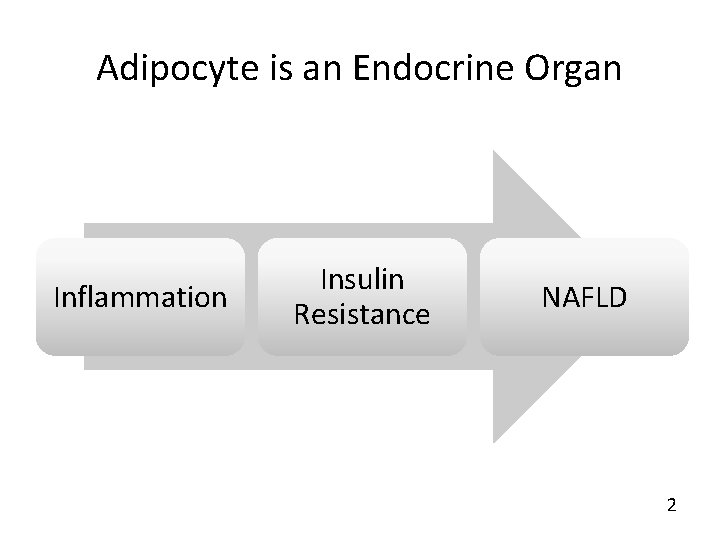
Adipocyte is an Endocrine Organ Inflammation Insulin Resistance NAFLD 2
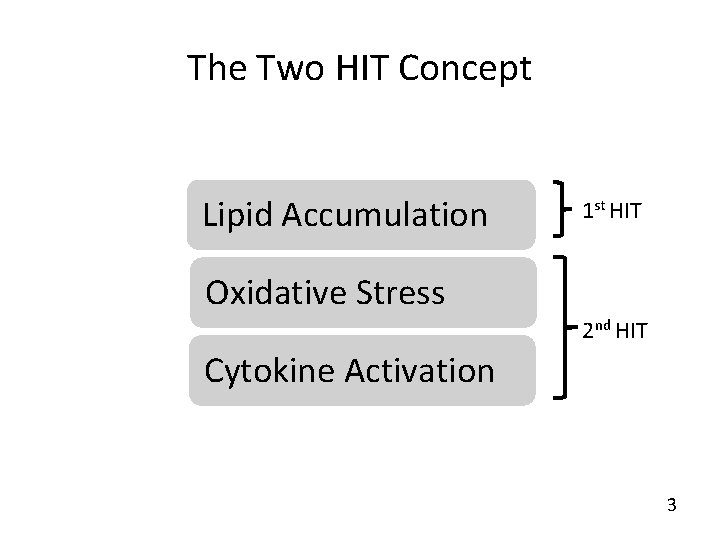
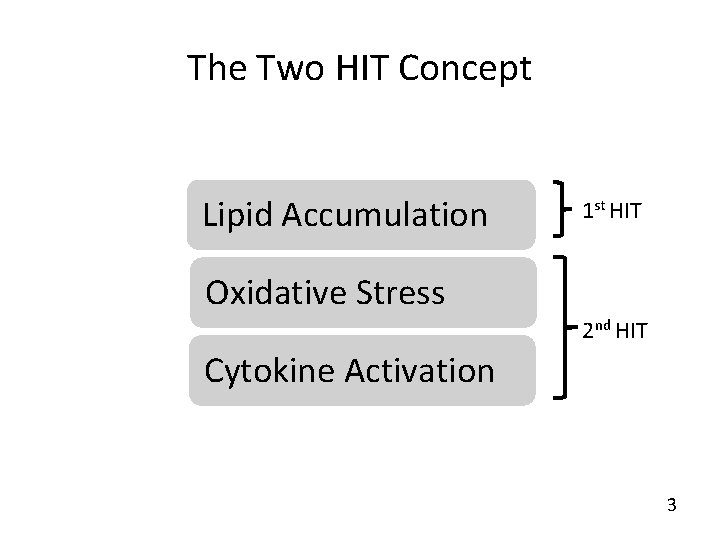
The Two HIT Concept Lipid Accumulation 1 st HIT Oxidative Stress 2 nd HIT Cytokine Activation 3
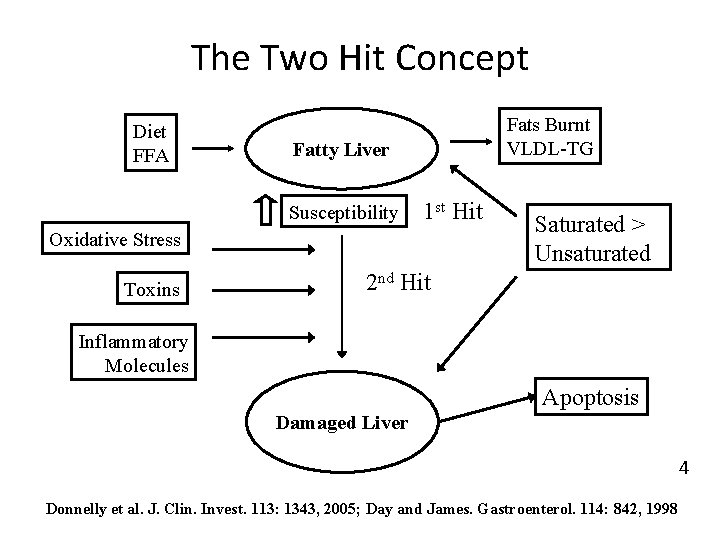
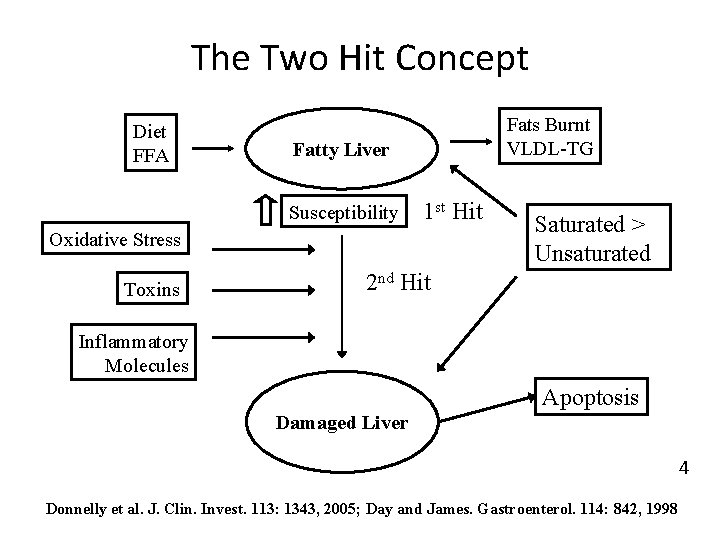
The Two Hit Concept Diet FFA Fats Burnt VLDL-TG Fatty Liver Susceptibility 1 st Hit Oxidative Stress Toxins Saturated > Unsaturated 2 nd Hit Inflammatory Molecules Apoptosis Damaged Liver 4 Donnelly et al. J. Clin. Invest. 113: 1343, 2005; Day and James. Gastroenterol. 114: 842, 1998
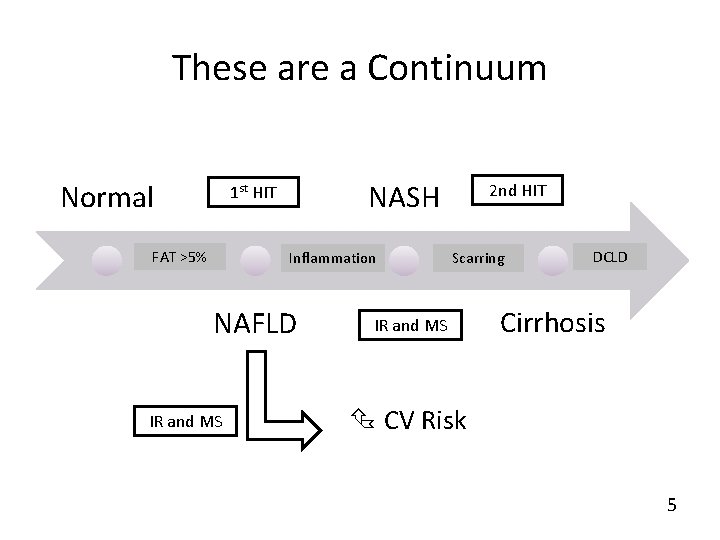
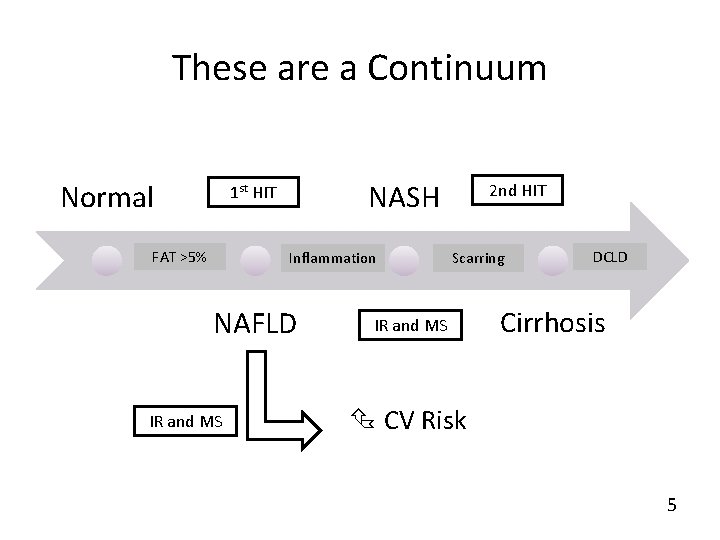
These are a Continuum Normal NASH 1 st HIT FAT >5% Inflammation NAFLD IR and MS 2 nd HIT Scarring IR and MS DCLD Cirrhosis CV Risk 5
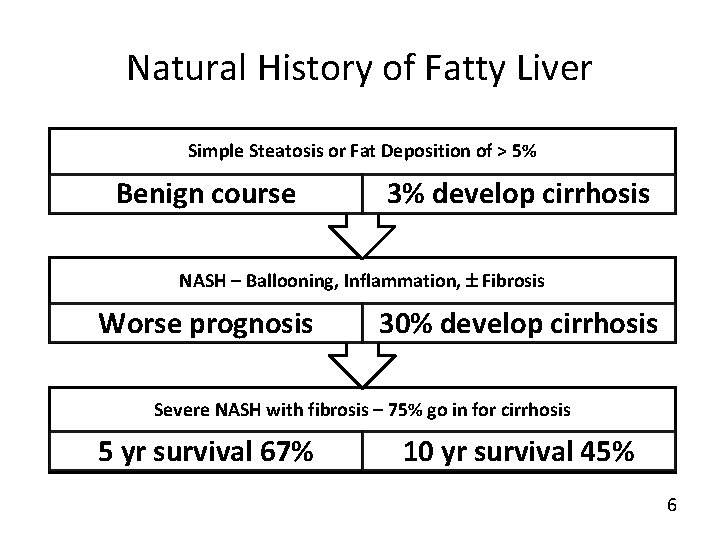
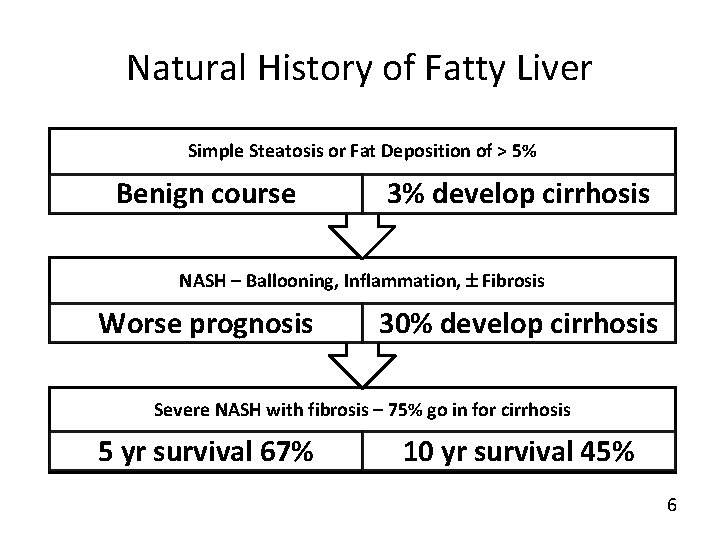
Natural History of Fatty Liver Simple Steatosis or Fat Deposition of > 5% Benign course 3% develop cirrhosis NASH – Ballooning, Inflammation, Fibrosis Worse prognosis 30% develop cirrhosis Severe NASH with fibrosis – 75% go in for cirrhosis 5 yr survival 67% 10 yr survival 45% 6
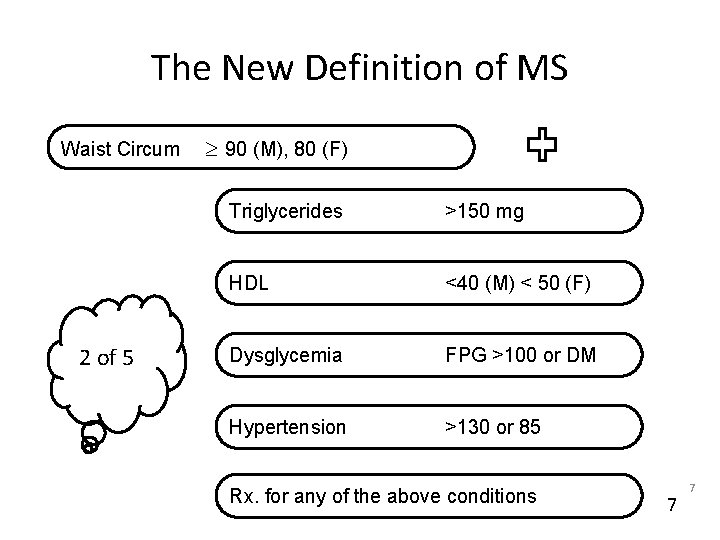
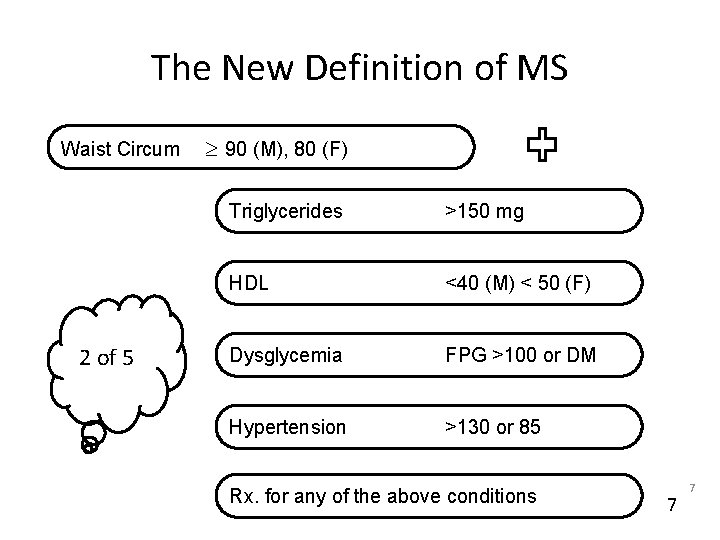
The New Definition of MS Waist Circum 2 of 5 90 (M), 80 (F) Triglycerides >150 mg HDL <40 (M) < 50 (F) Dysglycemia FPG >100 or DM Hypertension >130 or 85 Rx. for any of the above conditions 7 7
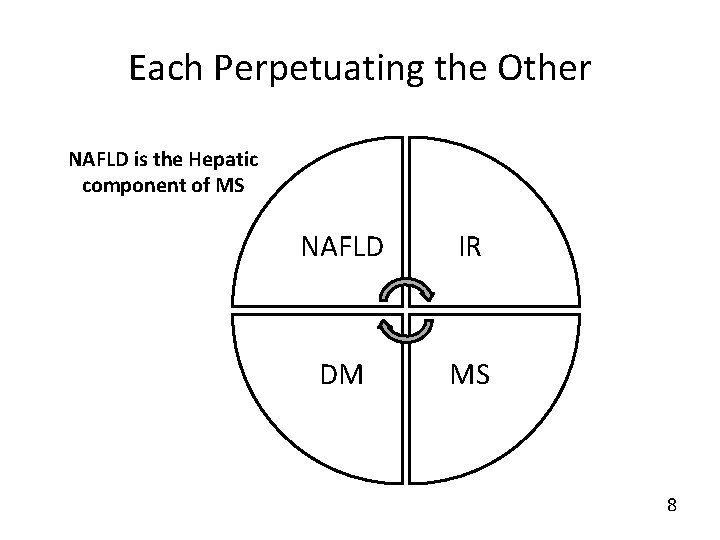
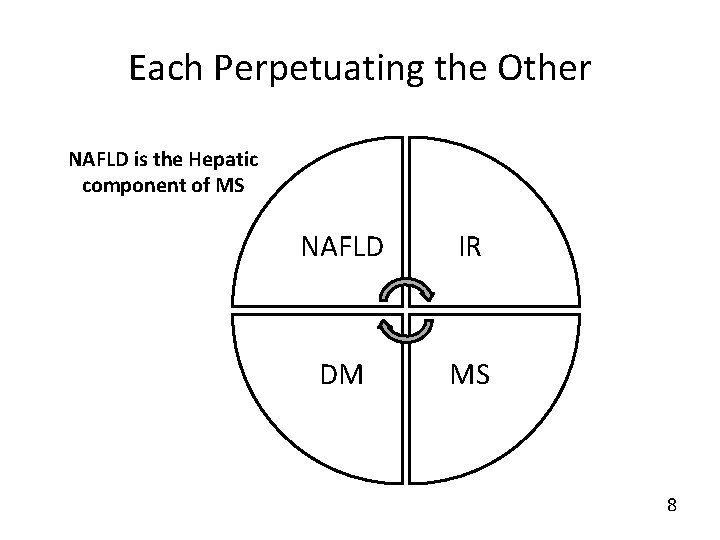
Each Perpetuating the Other NAFLD is the Hepatic component of MS NAFLD IR DM MS 8
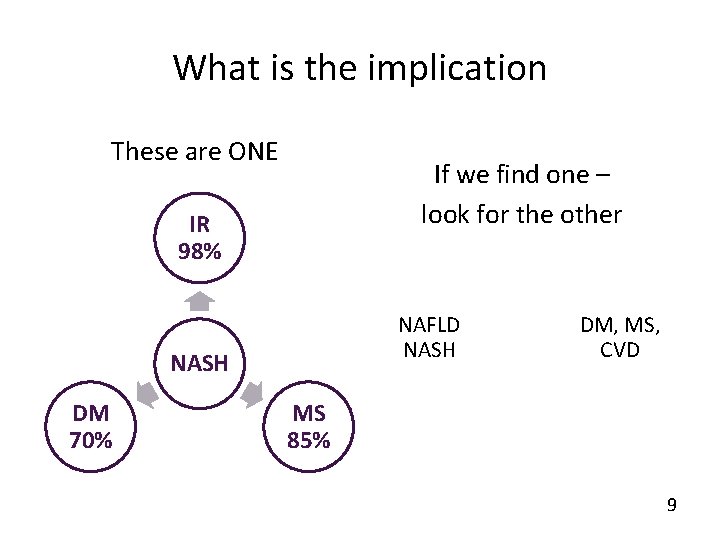
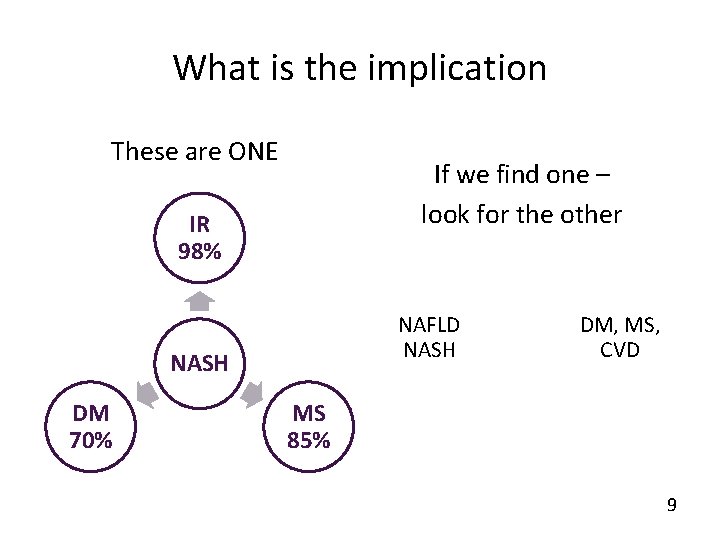
What is the implication These are ONE If we find one – look for the other IR 98% NAFLD NASH DM 70% DM, MS, CVD MS 85% 9
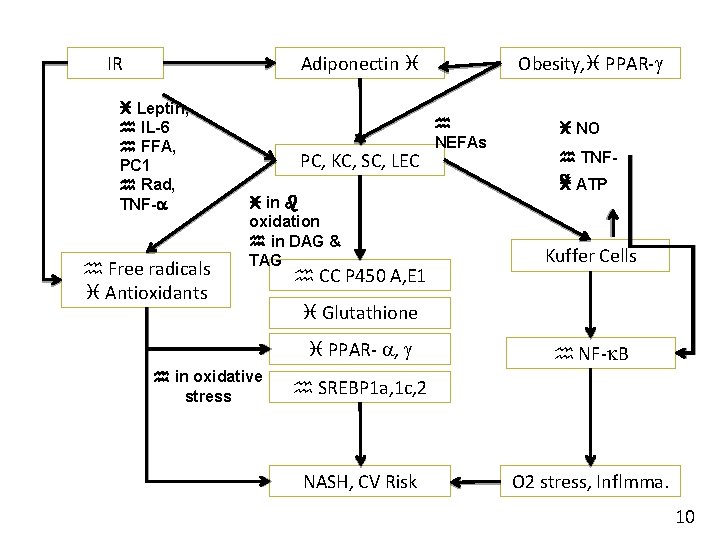
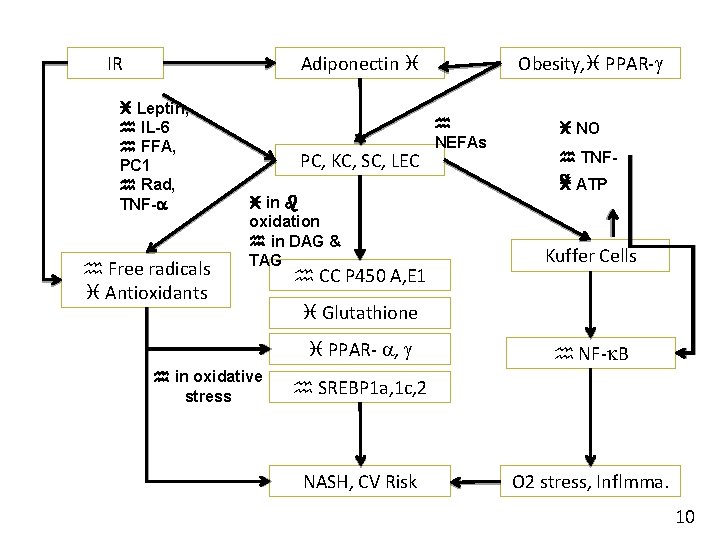
IR Obesity, PPAR- Adiponectin Leptin, IL-6 FFA, PC 1 Rad, TNF- Free radicals Antioxidants PC, KC, SC, LEC in oxidation in DAG & TAG CC P 450 A, E 1 NO TNF ATP Kuffer Cells Glutathione PPAR- , in oxidative stress NEFAs NF- B SREBP 1 a, 1 c, 2 NASH, CV Risk O 2 stress, Inflmma. 10
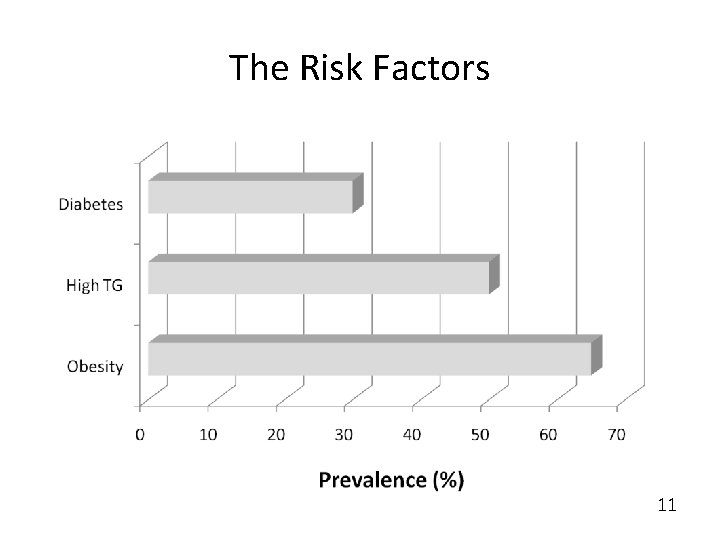
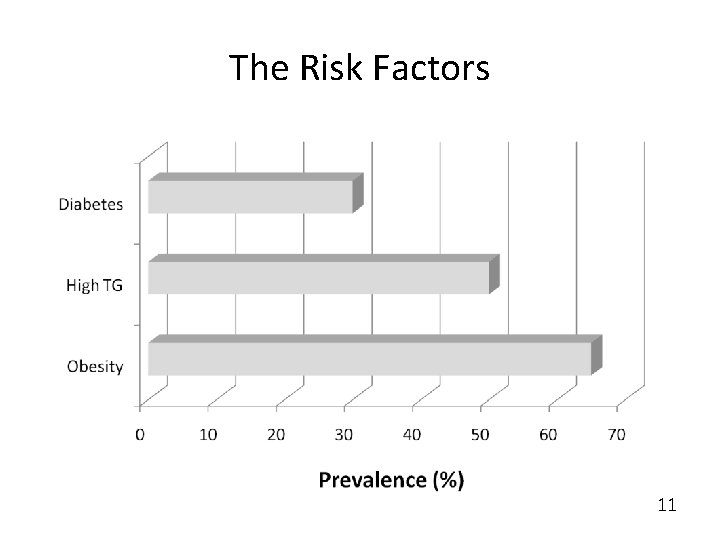
The Risk Factors 11
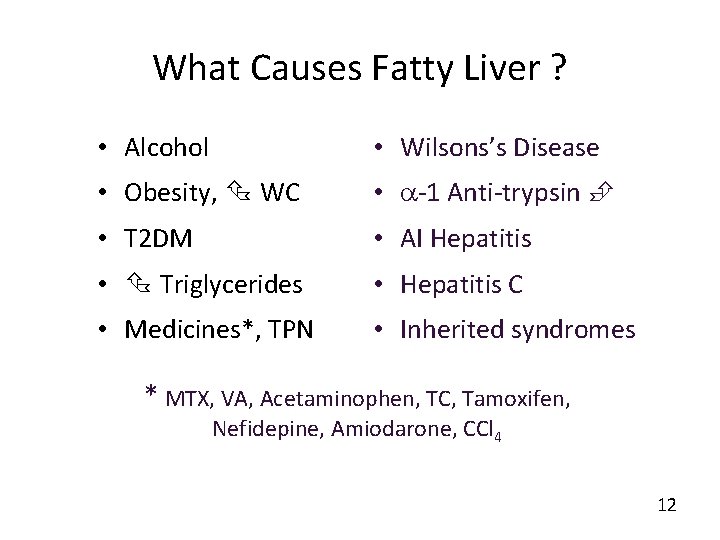
What Causes Fatty Liver ? • Alcohol • Wilsons’s Disease • Obesity, WC • -1 Anti-trypsin • T 2 DM • AI Hepatitis • Triglycerides • Hepatitis C • Medicines*, TPN • Inherited syndromes * MTX, VA, Acetaminophen, TC, Tamoxifen, Nefidepine, Amiodarone, CCl 4 12
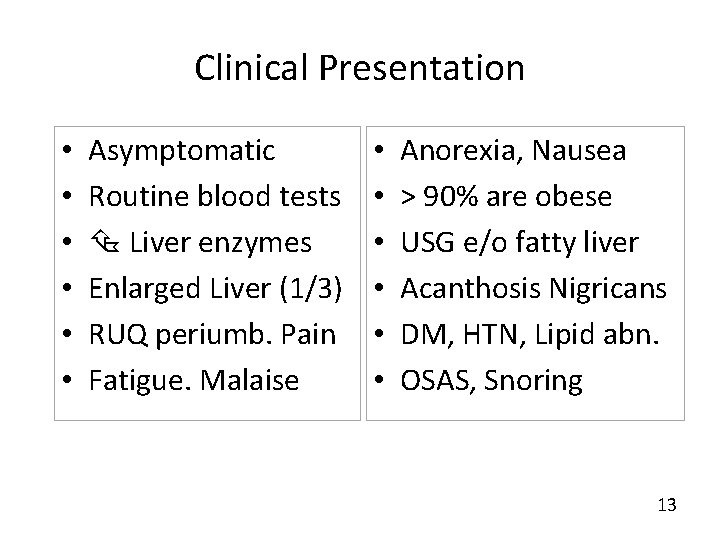
Clinical Presentation • • • Asymptomatic Routine blood tests Liver enzymes Enlarged Liver (1/3) RUQ periumb. Pain Fatigue. Malaise • • • Anorexia, Nausea > 90% are obese USG e/o fatty liver Acanthosis Nigricans DM, HTN, Lipid abn. OSAS, Snoring 13
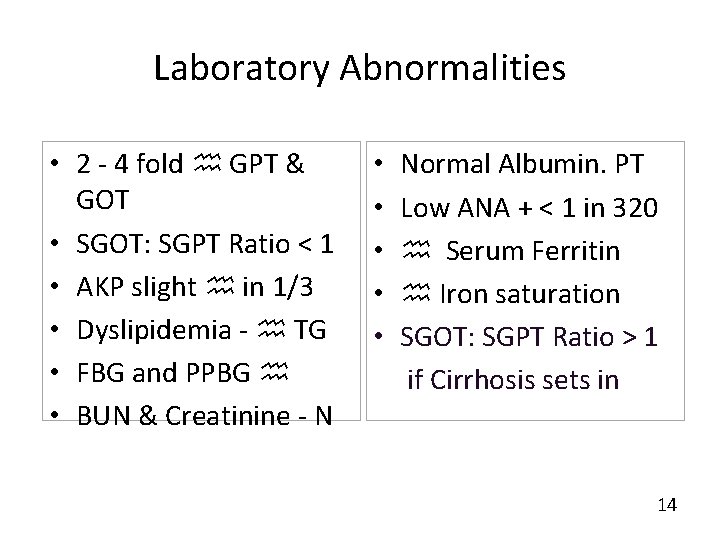
Laboratory Abnormalities • 2 - 4 fold GPT & GOT • SGOT: SGPT Ratio < 1 • AKP slight in 1/3 • Dyslipidemia - TG • FBG and PPBG • BUN & Creatinine - N • • • Normal Albumin. PT Low ANA + < 1 in 320 Serum Ferritin Iron saturation SGOT: SGPT Ratio > 1 if Cirrhosis sets in 14
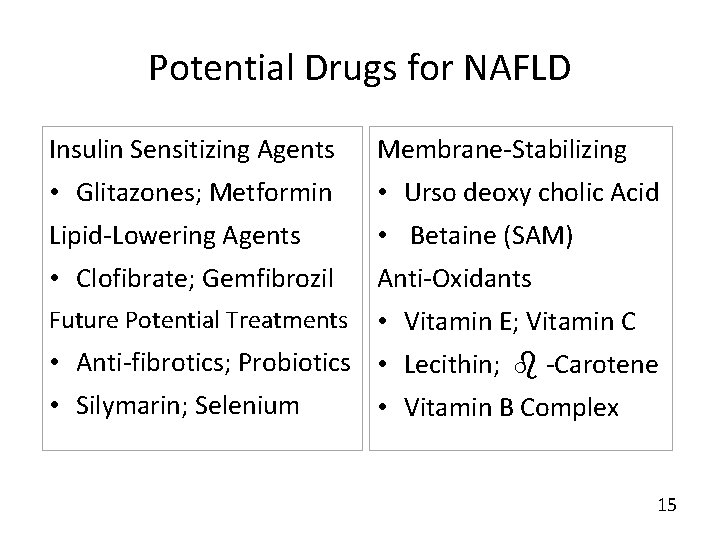
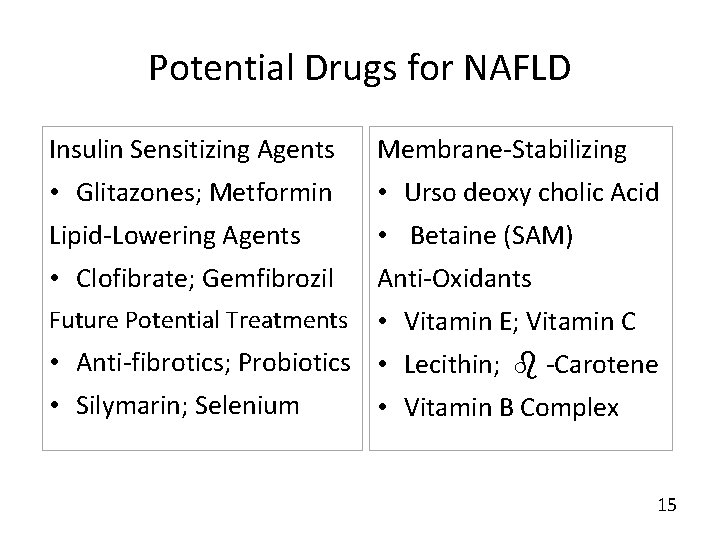
Potential Drugs for NAFLD Insulin Sensitizing Agents Membrane-Stabilizing • Glitazones; Metformin • Urso deoxy cholic Acid Lipid-Lowering Agents • Betaine (SAM) • Clofibrate; Gemfibrozil Anti-Oxidants Future Potential Treatments • Vitamin E; Vitamin C • Anti-fibrotics; Probiotics • Lecithin; -Carotene • Silymarin; Selenium • Vitamin B Complex 15
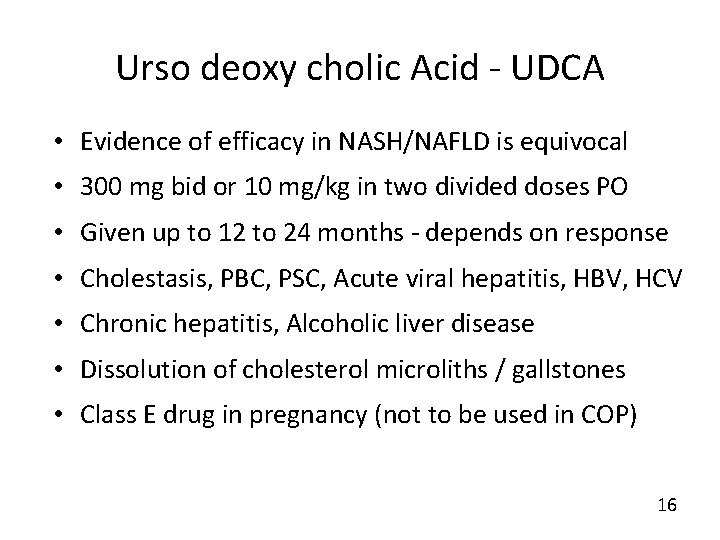
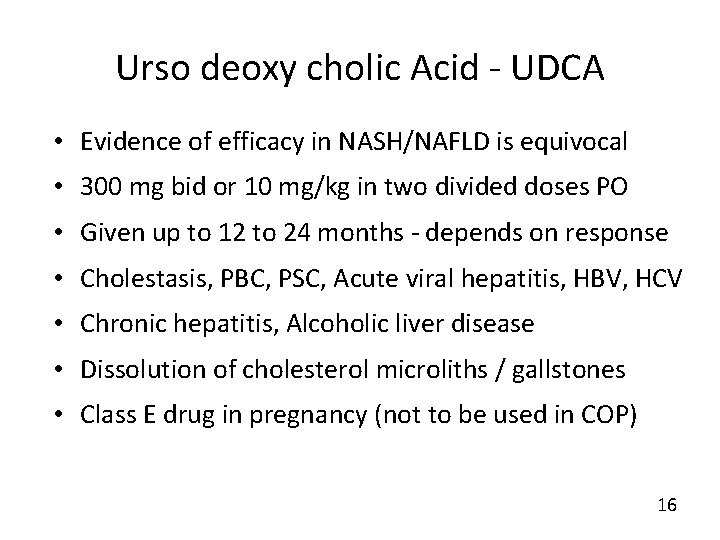
Urso deoxy cholic Acid - UDCA • Evidence of efficacy in NASH/NAFLD is equivocal • 300 mg bid or 10 mg/kg in two divided doses PO • Given up to 12 to 24 months - depends on response • Cholestasis, PBC, PSC, Acute viral hepatitis, HBV, HCV • Chronic hepatitis, Alcoholic liver disease • Dissolution of cholesterol microliths / gallstones • Class E drug in pregnancy (not to be used in COP) 16
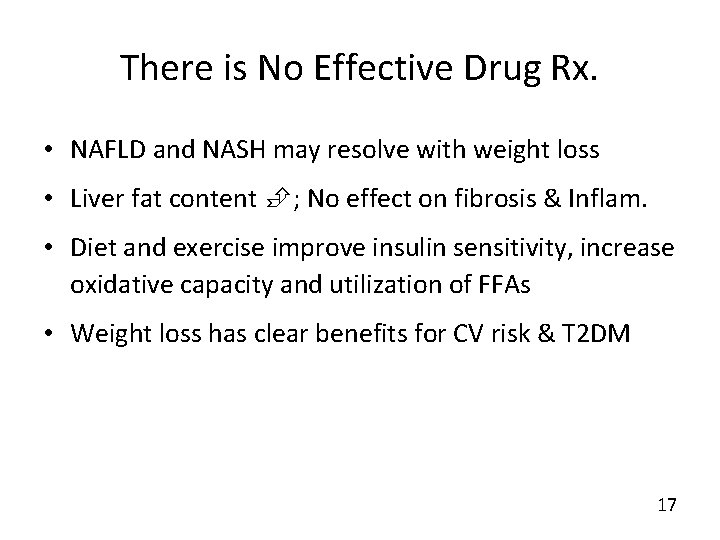
There is No Effective Drug Rx. • NAFLD and NASH may resolve with weight loss • Liver fat content ; No effect on fibrosis & Inflam. • Diet and exercise improve insulin sensitivity, increase oxidative capacity and utilization of FFAs • Weight loss has clear benefits for CV risk & T 2 DM 17
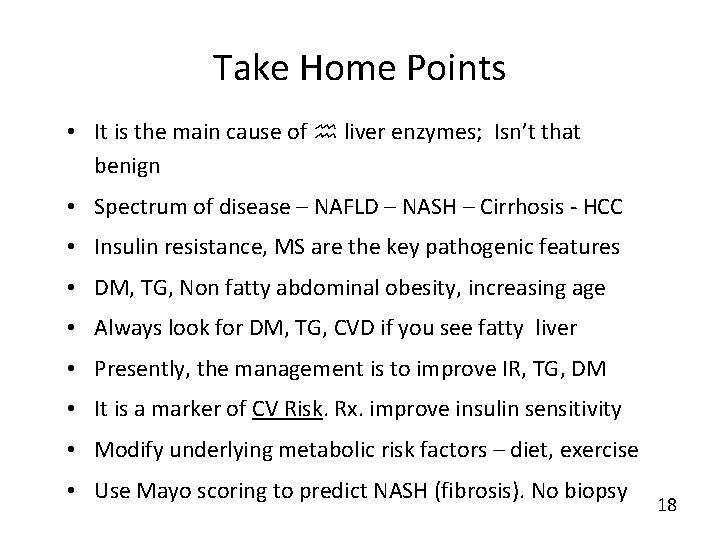
Take Home Points • It is the main cause of liver enzymes; Isn’t that benign • Spectrum of disease – NAFLD – NASH – Cirrhosis - HCC • Insulin resistance, MS are the key pathogenic features • DM, TG, Non fatty abdominal obesity, increasing age • Always look for DM, TG, CVD if you see fatty liver • Presently, the management is to improve IR, TG, DM • It is a marker of CV Risk. Rx. improve insulin sensitivity • Modify underlying metabolic risk factors – diet, exercise • Use Mayo scoring to predict NASH (fibrosis). No biopsy 18
 Non-alcoholic fatty liver disease (nafld)
Non-alcoholic fatty liver disease (nafld) Nonalcoholic fatty liver disease
Nonalcoholic fatty liver disease Encompassing pictures of reality created
Encompassing pictures of reality created Clinicopathologic conference sample
Clinicopathologic conference sample Acute fatty liver of pregnancy
Acute fatty liver of pregnancy Acute fatty liver of pregnancy
Acute fatty liver of pregnancy Lchad deficiency
Lchad deficiency Gastroenterology board review
Gastroenterology board review Stigmata of chronic liver disease
Stigmata of chronic liver disease Portal hypertension
Portal hypertension Chronic liver stigmata
Chronic liver stigmata Peripheral stigmata of cld
Peripheral stigmata of cld Portal hypertension symptoms and signs
Portal hypertension symptoms and signs Stages of cirrosis
Stages of cirrosis Gennifer shafer liver disease
Gennifer shafer liver disease Alcoholic liver disease
Alcoholic liver disease Infiltrative liver disease
Infiltrative liver disease Communicable disease and non communicable disease
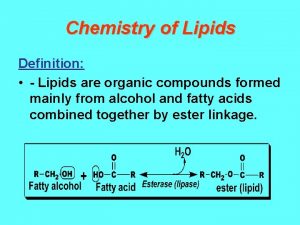
Communicable disease and non communicable disease Define compound lipids
Define compound lipids