FALLS IN THE PSYCHIATRIC INPATIENT POPULATION AND PREVENTATIVE






- Slides: 36
FALLS IN THE PSYCHIATRIC INPATIENT POPULATION AND PREVENTATIVE MEASURES THROUGH MULTIMEDIA EDUCATION Maria Bartlett, Alisa Foote, Kylie Griffin, Laura Lazzareschi, Emily Ycasas
PROBLEM IDENTIFICATION & EVIDENCE-BASE
Problem Identification Patients suffer: • Increased morbidity + mortality • Loss of trust • Impaired sense of safety
Problem Identification For every fall, there are: • Delays in throughput and access • Unused resources • Costs not reimbursed by Medicare
Problem Identification “Psychiatric units are the second most common setting for falls in the hospital. ” (Kerzman, Cherit, Brin & Toren, 2003)
PICO Question In inpatient psychiatric patients, are fall prevention strategies more effective at decreasing patient fall rates than using no formal patient strategies?
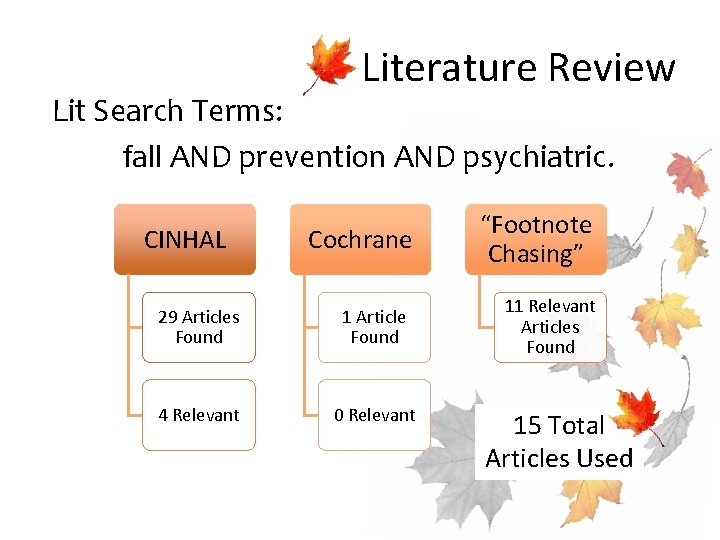
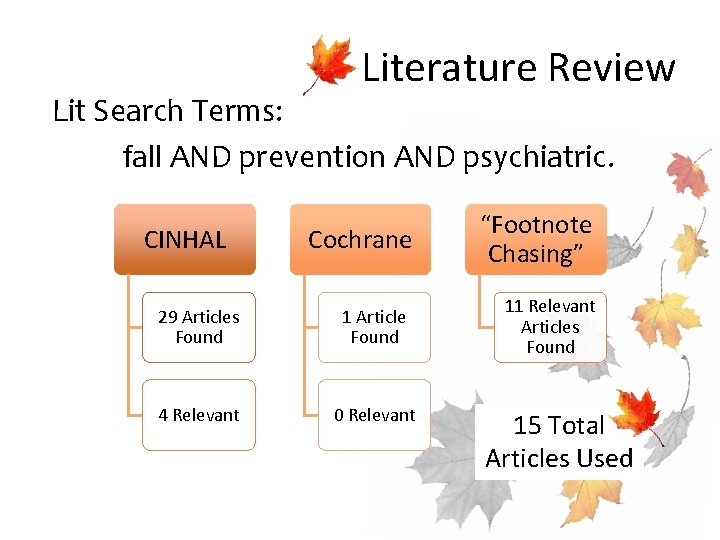
Literature Review Lit Search Terms: fall AND prevention AND psychiatric. Cochrane “Footnote Chasing” 29 Articles Found 1 Article Found 11 Relevant Articles Found 4 Relevant 0 Relevant CINHAL 15 Total Articles Used

Fall Risk Factors • Physical Environment – Poor Lighting – Raised Bed – Improper Equipment • Risky Behavior of Patient • Others: female gender, age, abnormal balance and gait, arthritis, blindness, increased length of stay, h/o prior falls.

Fall Risk Factors: Psychiatric • Psychiatric dx increased risk of falling. – Depression + Psychotic at highest risk. • Related risk factors include: – Cognitive impairment – Dementia – Orthostatic Hypotension – Parkinsonism – Polypharmacy – Sedatives
Fall Risk Factors: Meds • Medications associated with higher fall risk: – Benzodiazepines – Atypical Antidepressants – Anticonvulsants • Fall risk rises with increasing doses of antipsychotics, anxiolytic, hypnotics, sedatives, and antidepressants. • Any combination of above drugs also increase fall risk.
Falls at SMV • Inpatient falls = potentially preventable. – Elimination could mean a 7% reduction in length of stay. • Current fall evaluation: – Schmid Fall Risk Assessment Tool – Get Up and Go Test (mobility assessment) • Universal Fall Precaution or High Fall Risk protocol then implemented.
High Fall Risk Protocol • Interventions include: – Yellow armbands on patients – Falling leaf place card on room – “Fall risk” on brain + rounds board. – Routine orthostatic BP monitoring – RASS scale monitoring – Utilization of individualized interventions from the Interdisciplinary Plan of Care (IPOC)
EBP Suggestions • Causes of falls are multifactorial, so prevention must be also. – Educational programs: Written information + one-on-one follow up • 50% reduction in fall in people with impaired cognitive function. – Utilization of equipment: tab alarms, bed alarms, other restraint-free devices. – Hip protectors in geriatric population – Consider Physical Therapy consult
Education • Primary means of fall risk reduction. • Patient: – Video education regarding epidemiology of falls, self reflection of individualized risk, problem area identification, development of preventative strategies + behaviors, goal setting, and goal review. – Use of multimedia: written, video, professional follow up decreases fall rates!
Education • Staff: – Continuing the change in culture • Changing attitudes • Changing approach – Increased visual aids, media modalities will help staff educate patients and remain aware of the potentially devastating consequences of falls.

SIMPLIFIED FALL PREVENTION POSTER

SMV FALL VIDEO SDSU SON '12 FALL REDUCTION VIDEO PROTOTYPE

IMPLEMENTATION STRATEGY
Protocol for Change • Educate staff: – Communicate necessity – Communicate vision – Communicate practice (Gesme, D. , & Wiseman, M. (2010). How to implement change in practice. Journal of Oncology Practice, 6(5), 257 -259. doi: 10. 1200/JOP. 000089)
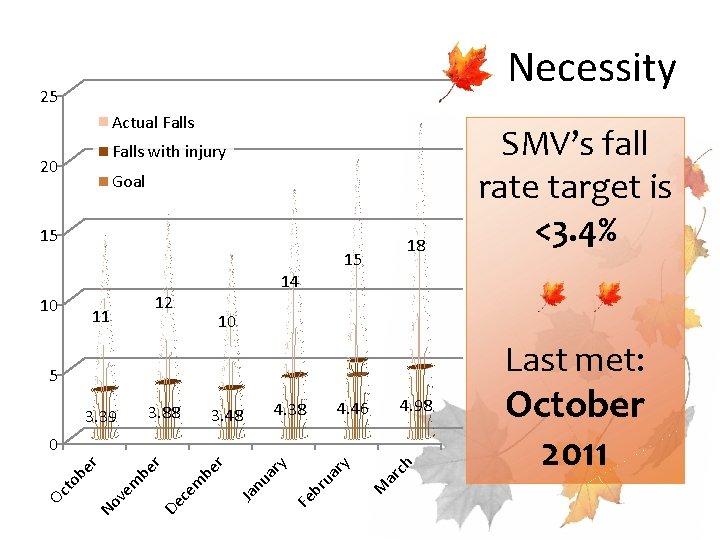
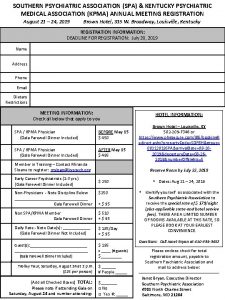
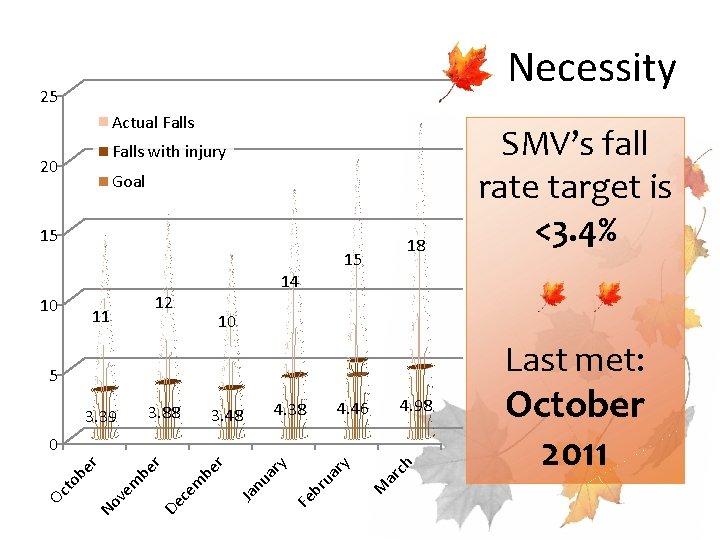
Necessity 25 Actual Falls with injury 20 Goal 15 18 15 10 11 12 14 10 Last met: 5 3. 39 3. 88 4. 98 4. 46 4. 38 3. 48 ar ch M ua ry br Fe ar y nu Ja em be r r De c em be No v to b er 0 Oc SMV’s fall rate target is <3. 4% October 2011
Vision • Nurses and Mental Health workers are to ensure video is shown upon admission. – Evidence shows multimedia education with 1: 1 follow up decreases falls. • RN + MHW can have follow up discussions regarding video with patients.
Practice • Leadership can help by informing staff early and often about new practice. – Make video easy to access. – Reward staff for input. – Use email, telephone, face-to-face communication – Explain who, what, where, and why behind practice change.
Protocol for Change • Foster Team Culture: – Develop Team aimed at common goal: Patient Safety! – Set clear expectations + educate staff towards a sense of shared accountability.
Protocol for Change • Identify + Empower Champions – Empower individuals to lead others • Look for individuals with natural leadership skills • Identify innovators/technologically-friendly
Protocol for Change • Provide feedback + positive reinforcement – Continue data collection – Reward (WOWs!) staff proactive in implementing new policy. – Survey interdisciplinary team + patients for input on video/improvements for future – Evaluate data from before + after video implementation.
Protocol for Change • Provide feedback + positive reinforcement – Continue data collection – Reward (WOWs!) staff proactive in implementing new policy. – Survey interdisciplinary team + patients for input on video/improvements for future – Evaluate data from before + after video implementation.
Change Theory • Seven Phases of Planned Change by Lippitt, Watson, and Westley – “Change Agents”: SDSU SON leadership students • Present Change concept including benefits + appraisal • Cover change forces + resistance forces • Ideally create more change agents to further change potential
Change Theory • Seven Phases of Planned Change 1. Becoming aware of need for change 2. Client system and change agents develop a relationship 3. Change problem is identified 4. Change goals are set and achievement options explored
Change Theory • Seven Phases of Planned Change 5. Plan for change is implemented 6. Change is accepted and stabilized 7. Change entities redefine their relationship Wise, P. S. (2011). Leading and managing in nursing (4 th ed. ). St. Louis, Mo. : Mosby/Elsevier.
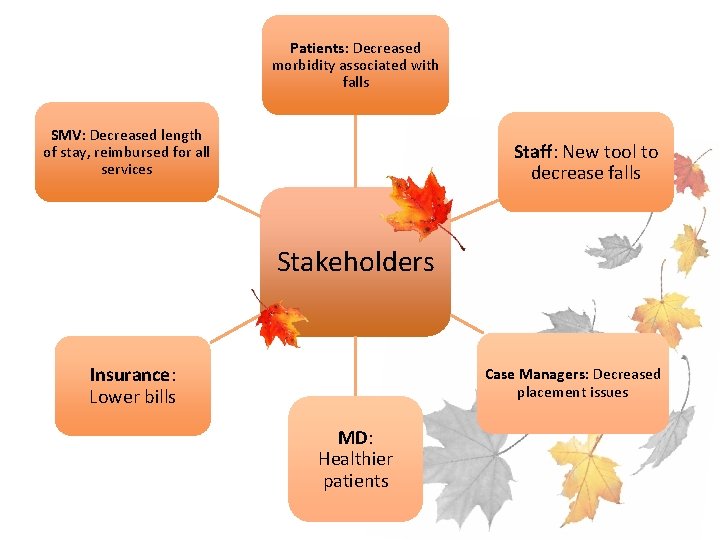
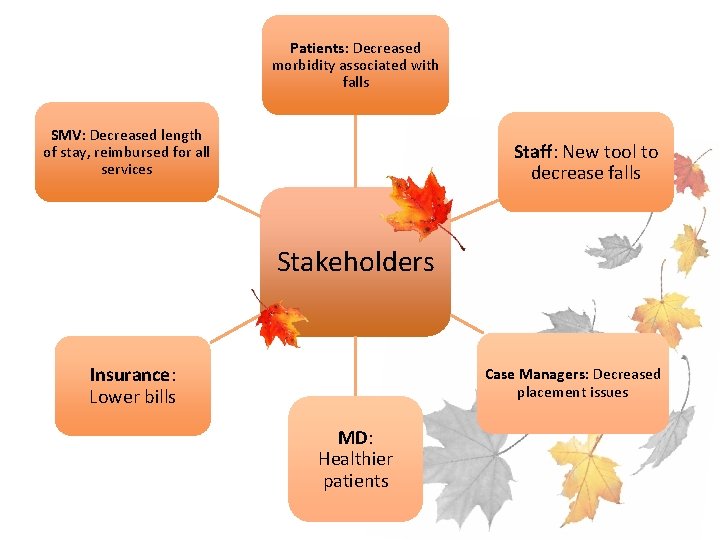
Patients: Decreased morbidity associated with falls SMV: Decreased length of stay, reimbursed for all services Staff: New tool to decrease falls Stakeholders Insurance: Lower bills Case Managers: Decreased placement issues MD: Healthier patients
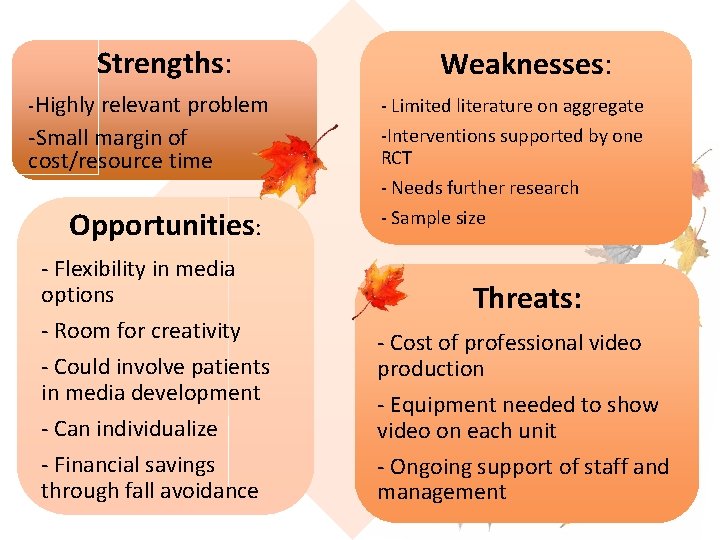
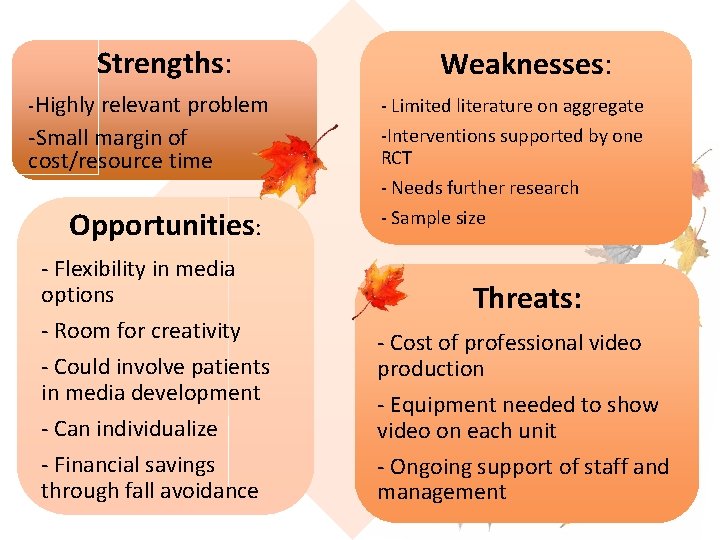
Strengths: -Highly relevant problem -Small margin of cost/resource time Opportunities: - Flexibility in media options - Room for creativity - Could involve patients in media development - Can individualize - Financial savings through fall avoidance Weaknesses: SWOT Analysis - Limited literature on aggregate -Interventions supported by one RCT - Needs further research - Sample size Threats: - Cost of professional video production - Equipment needed to show video on each unit - Ongoing support of staff and management
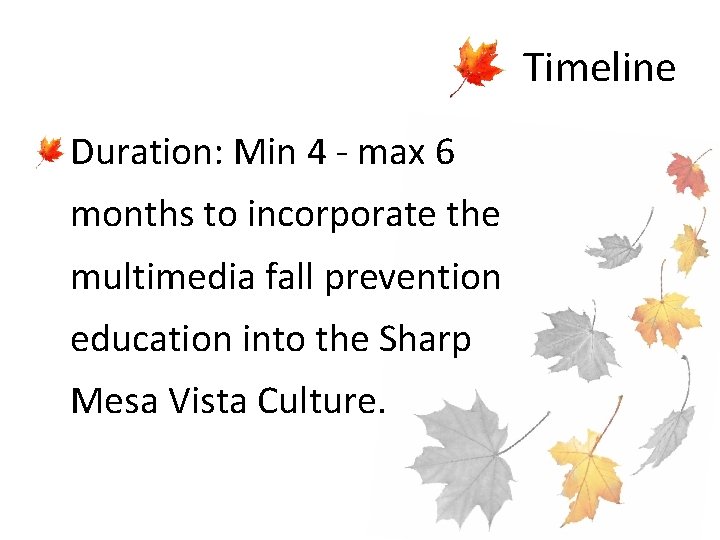
Timeline • Duration: Min 4 - max 6 months to incorporate the multimedia fall prevention education into the Sharp Mesa Vista Culture.
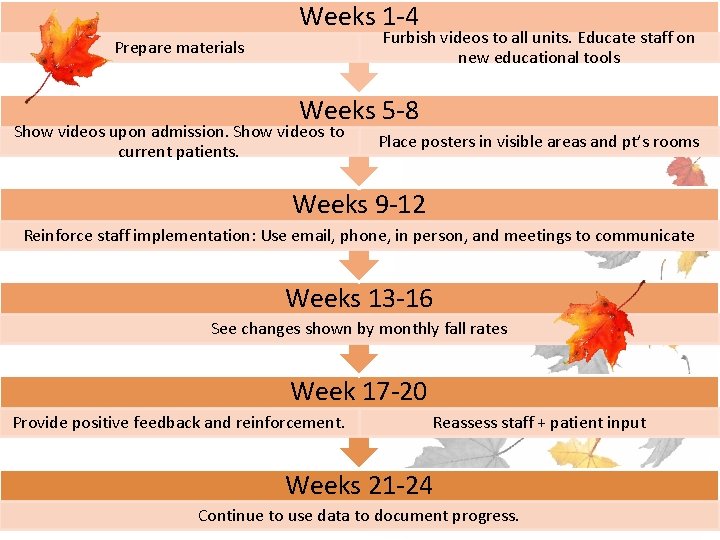
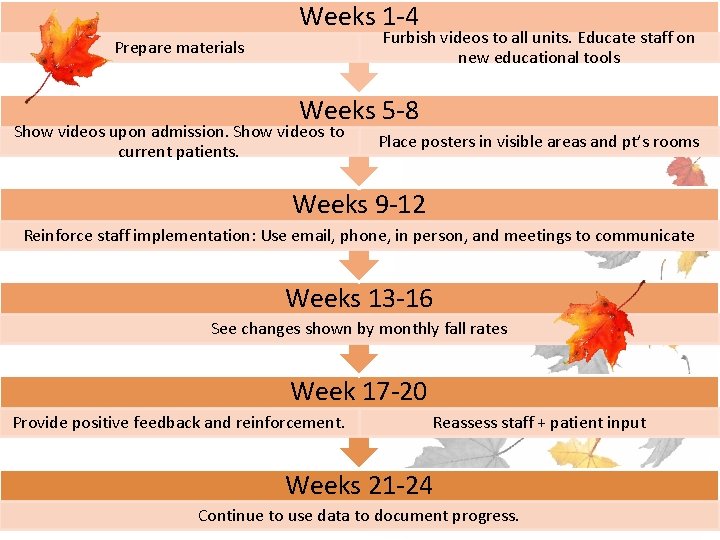
Weeks 1 -4 Furbish videos to all units. Educate staff on new educational tools Prepare materials Weeks 5 -8 Show videos upon admission. Show videos to current patients. Place posters in visible areas and pt’s rooms Weeks 9 -12 Reinforce staff implementation: Use email, phone, in person, and meetings to communicate Weeks 13 -16 See changes shown by monthly fall rates Week 17 -20 Provide positive feedback and reinforcement. Reassess staff + patient input Weeks 21 -24 Continue to use data to document progress.
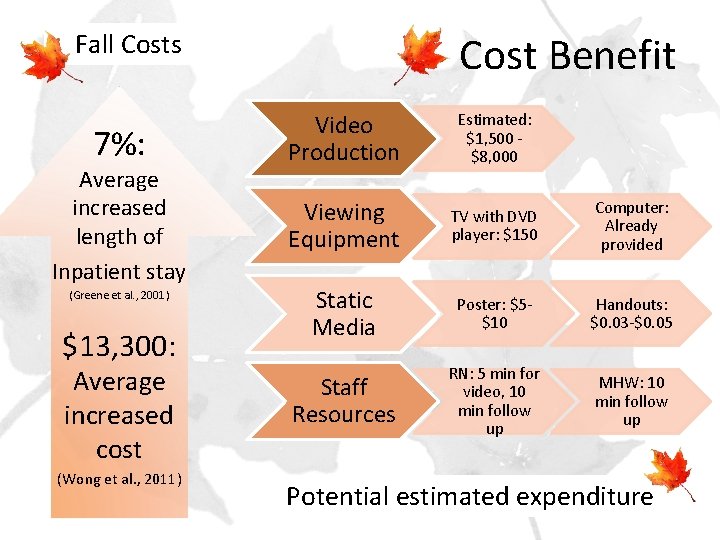
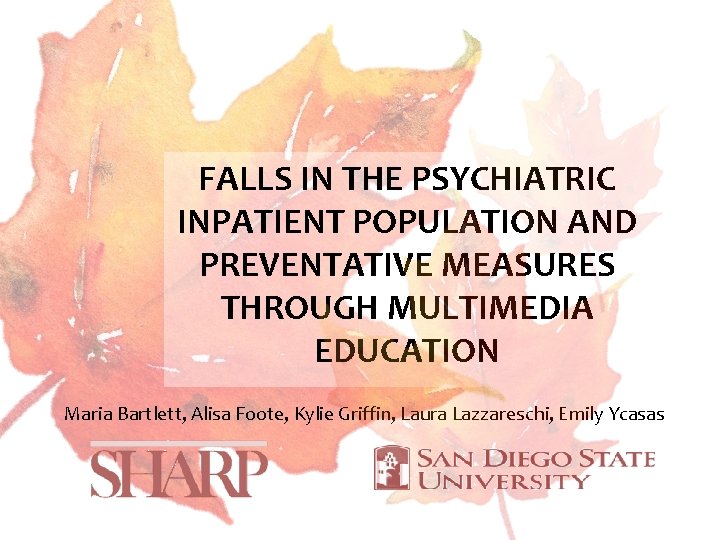
Fall Costs 7%: Average increased length of Inpatient stay (Greene et al. , 2001) $13, 300: Average increased cost (Wong et al. , 2011) Cost Benefit Video Production Estimated: $1, 500 - $8, 000 Viewing Equipment TV with DVD player: $150 Computer: Already provided Static Media Poster: $5$10 Handouts: $0. 03 -$0. 05 Staff Resources RN: 5 min for video, 10 min follow up MHW: 10 min follow up Potential estimated expenditure
References • • • • • Ang, E. , Mordiffi, S. , & Wong, H. (2011). Evaluating the use of a targeted multiple intervention strategy in reducing patient falls in an acute care hospital: a randomized controlled trial. Journal Of Advanced Nursing, 67(9), 1984 -1992. Anonymous. (2010). Multimedia patient education prevents falls. Irish Medical Times, 44(49), 41. Blair, E. , & Szared, B. (2008). Exploring relationship of psychotropic medications to fall events in an inpatient geriatric psychiatric population. International Journal Of Psychiatric Nursing Research, 14(1), 1698 -1710. Centers for Medicare & Medicaid Services. (2008). Changes to the hospital inpatient prospective payment systems and fiscal year 2009 rates. Baltimore, MD: Centers for Medicare & Medicaid Services. De Carle, J. , & Kohn, R. (2001). Risk factors for falling in a psychogeriatric unit. International Journal Of Geriatric Psychiatry, 16(8), 762 -767. doi: 10. 1002/gps. 40 Fontenot-Miller, C. , Lee, T. , Mendoza, C. , Ray, M. (2011). Results of Sharp Mesa Vista’s current fall protocol versus their previous fall protocol in reducing patient falls. San Diego State University: School of Nursing. Greene, E. , Cunningham, C. J. , Eustace, A. , Kidd, W. , Clare, A. W. , & Lawlor, B. A. , (2001). Recurrent falls are associated with increased length of stay in elderly psychiatric inpatients. International Journal Of Geriatric Psychiatry, 16(10), 965 -968. doi: 10. 1002/gps. 463 Haines, T. P. , Hill, A-M. , Hill, K. D. , Mc. Phail, S. , Oliver, D. , Brauer, S… Beer, C. (2011). Pt education to prevent falls among older hospital inpatients. Archives of Internal Medicine, 171(6), 516 -524. Kerzman, H. , Chetrit, A. , Brin, L. , & Toren, O. (2004). Characteristics of falls in hospitalized patients. Journal Of Advanced Nursing, 47(2), 223 -229. doi: 10. 1111/j. 1365 -2648. 2004. 03080. x Knight, M. , & Coakley, C. (2010). Fall risk in pts w/ acute psychosis. Journal of Nursing Care Quality, 25(3), 208 -215. Lavsa, S. , Fabian, T. , Saul, M. , Corman, S. , & Coley, K. (2010). Influence of medications & diagnoses on fall risk in psychiatric inpatients. American Journal of Health-system Pharmacy : AJHP : Official Journal of the American Society of Health-System Pharmacists, 67(15), 1274 -1280. Neyens, J. , Dijcks, B. , Twisk, J. , Schols, J. , van Haastregt, J. , WJ, & de Witte, L. (2009). A multifactorial intervention for the prevention of falls in psychogeriatric nursing home pts, a randomised controlled trial (RCT). Age & Ageing, 38(2), 194 -199. doi: 10. 1093/ageing/afn 297 Poe, S. , Cvach, M. , Gartrell, D. , Radzik, B. , & Joy, T. (2005). An evidence-based approach to fall risk assessment, prevention, & management: lessons learned. Journal Of Nursing Care Quality, 20(2), 107 -118. Semin-Goossens, A. , van der Helm, J. M. J. , & Bossuyt, P. M. (2003). A failed model-based attempt to implement an evidence-based nursing guideline for fall prevention. Journal of Nursing Care Quality, 18(3), 217 -255. Sharp Mesa Vista (2011). Fiscal Year Report Sheet. (Unpublished fiscal year report). San Diego, CA. Spoelstra, S. , Given, B. , & Given, C. (2012). Fall prevention in hospitals: An integrative review. Clinical Nursing Research, 21(1), 92. Sterke, C. , van Beeck, E. , van der Velde, N. , Ziere, G. , Petrovic, M. , et al. (2011). New insights: Dose-response relationship between psychotropic drugs and falls: D study in nursing home residents with dementia. The Journal of Clinical Pharmacology. Tzeng, H. (2011). Nurses' Caring Attitude: Fall Prevention Program Implementation as an Example of Its Importance. Nursing Forum, 46(3), 137 -145. doi: 10. 1111/j. 1744 -6198. 2011. 00222. x Vaughn, K. , Young, B. , Rice, F. , & Stoner, M. (1993). A retrospective study of pt falls in a psychiatric hospital. Journal Of Psychosocial Nursing & Mental Health Services, 31(9), 37. Wong, C. A. , and others. The cost of serious fall-related injuries at three Midwestern hospitals. The Joint Commission Journal on Quality and Patient Safety. 37(2): 81 -87, February 2011

DISCUSSION QUESTIONS
 Politeness theory in communication
Politeness theory in communication Milling machine maintenance
Milling machine maintenance Preventative system
Preventative system Miracles wichita, ks
Miracles wichita, ks Inpatient in nh
Inpatient in nh Dshs irb
Dshs irb Poa indicators are assigned in the inpatient setting for
Poa indicators are assigned in the inpatient setting for Inpatient pharmacy workflow
Inpatient pharmacy workflow Ethical and legal issues in psychiatric nursing
Ethical and legal issues in psychiatric nursing Chapter 4 section 1 population dynamics study guide
Chapter 4 section 1 population dynamics study guide Section 1 population dynamics answer key
Section 1 population dynamics answer key Population ecology section 1 population dynamics
Population ecology section 1 population dynamics Population ecology section 1 population dynamics answer key
Population ecology section 1 population dynamics answer key Definition of psychiatric nursing
Definition of psychiatric nursing Mse psych
Mse psych Psychiatric nursing diagnosis
Psychiatric nursing diagnosis History of psychiatric nursing
History of psychiatric nursing Psychological disorders
Psychological disorders Cmc psychiatric hospital
Cmc psychiatric hospital Role of psychiatric nurse
Role of psychiatric nurse Chapter 22 psychiatric emergencies
Chapter 22 psychiatric emergencies Psychiatric security review board
Psychiatric security review board Psychiatric rehabilitation
Psychiatric rehabilitation American nurses association illinois
American nurses association illinois American psychiatric association annual meeting 2020
American psychiatric association annual meeting 2020 Northeast florida psychiatric associationinc
Northeast florida psychiatric associationinc Liberty hill academy
Liberty hill academy Southern psychiatric association
Southern psychiatric association Chronic insomnia
Chronic insomnia Nursing process in psychiatric nursing
Nursing process in psychiatric nursing Psychiatric emergency
Psychiatric emergency Psychiatric emergency
Psychiatric emergency Calgary family assessment model
Calgary family assessment model Ethical issues in psychiatric nursing
Ethical issues in psychiatric nursing Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Ng-html
Ng-html Bổ thể
Bổ thể