Examination of the arteries veins and lymphatics Dr







- Slides: 26
Examination of the arteries, veins and lymphatics Dr Abdul. Qader Said Murshed Consultant General, G. I. , & Laparoscoic Surgeon FRCS Glasg, FRCSI, Jordanian Board Monday, 16/7/2018
The arteries lower limb • • Inspection Colour Vascular angle Venous filling Pressure areas
• Colour ischaemic limb, or varyis whiteing degrees of redness or blueness more obvious in the lower leg and the toes. In acutely ischaemic legs, blue streaks around white patches produce a mottled discolouration. When the cyanotic areas become fixed, the ischaemia is irreversible. Gangrene turns the skin a permanent blue–black colour, usually first seen in the toes.
• Vascular angle: The vascular angle, which is also called Buerger’s angle, is the angle to which the leg has to be raised before it becomes white. -In a limb with a normal circulation, the toes stay pink even when the limb is raised by 90°. -In an ischaemic leg, elevation to 15° or 30° for 30– 60 seconds may cause pallor. -A vascular angle of less than 20° indicates severe ischaemia. -(after elevation) to pink and then take on a suffused purple–red colour. The latter is caused by deoxygenated blood filling the dilated capillaries.
• Venous filling: In a warm room, the veins of a normal foot are dilated and full of blood, even when the patient is lying horizontally. – In an ischaemic foot, the veins collapse and sink below the skin surface to look like pale blue gutters. This appearance is called guttering of the veins.
• Pressure areas: Inspect all areas subjected to pressure or trauma during walking or bed rest very carefully, because these are the first sites to show evidence of trophic changes, ulceration and gangrene.
• • Palpation Temperature Capillary refilling Feel all the pulses Test the muscles and nerves
Temperature: The skin temperature can only be assessed reliably if both lower limbs have been exposed to the same ambient temperature for a full 5 minutes. A blue or even red foot can be very cold.
Capillary refilling: Press on the pulp of a toe or finger for two seconds, and then observe the time taken for the blanched area to turn pink after you have stopped pressing. This gives a crude indication of the rate of blood flow in the capillaries and the pressure within them.
• Feel all the pulses: Pulses are most easily felt where an artery is superficial and crosses a bone. -the carotid, subclavian, brachial and both wris arteries are close to the skin and easy to palpate. -The femoral pulse in the groin lies half way between the symphysis pubis (in the midline) and the anterior superior iliac spine (the mid-inguinal point). -The dorsalis pedis artery runs from a point on the anterior surface of the ankle joint, midway between the malleoli, towards the cleft between the first and second metatarsal bones. - In 10 per cent of subjects, the anterior tibial artery is absent and replaced by a branch of the peroneal artery. -The posterior tibial artery lies one-third of the way along a line between the tip of the medial malleolus and the point of the heel, but is easier to feel 2. 5 cm higher up, where it lies just behind the medial malleolus.
• Feel all the pulses The popliteal pulse is difficult to feel becauseit does not cross a prominent bone and is not superficial. There are three ways to feel it, and all three may have to be tried before deciding that the pulse is present or absent: -extend the patient’s knee fully and place both hands around the top of the calf, with the thumbs placed on the tibial tuberosity and the tips of the fingers of each hand touching behind the knee, over the lower part of the popliteal fossa. -Flexing the knee to 135° loosens the deep fascia and may make the lower half of the artery easier to feel. -It is sometimes worth turning the patient into the prone position and feeling along the course of the artery with the fingertips of both hands.
• Test the muscles and nerves: Severe ischaemia causes a loss of muscle and nerve function, ultimately producing an immobile, numb limb.
Auscultation: -listen along the course of all the major arteries, especially if the pulses are weak. - Bruits are caused by turbulent flow beyond a stenosis, or an irregularity in the artery wall. - Do not press too hard over a superficial artery with the bell of your stethoscope. - Before finishing the physical examination of the lower limb, you should always measure the blood pressure in both arms to exclude significant subclavian or innominate artery disease.
• Before finishing the physical examination of the lower limb, you should always measure the blood pressure in both arms to exclude significant subclavian or innominate artery disease.

• Pressure measurement with the Doppler flow detector
• • • The symptoms and signs of acute ischaemia: Pain. Paraesthesia and numbness Paralysis. Pallor. Pulseless. Perishing cold.
• • • Causes of acute arterial ischaemia: An arterial embolus. Thrombosis on an atheromatous plaque. Thrombosis of an aneurysm (usually popliteal) Arterial dissection (usually aortic). Traumatic disruption. External compression, e. g. a cervical rib or popliteal entrapment.
Symptoms of chronic arterial insufficiency of the lower limb: • Intermittent claudication • Rest pain
• Intermittent claudication






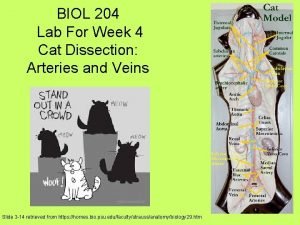
 Cat dissection arteries
Cat dissection arteries Cardiopulmonary circulation
Cardiopulmonary circulation Lower extremity arteries and veins
Lower extremity arteries and veins Difference between arteries veins and capillaries
Difference between arteries veins and capillaries Traube space
Traube space Blood
Blood Facial vein and facial artery
Facial vein and facial artery Blood pressure
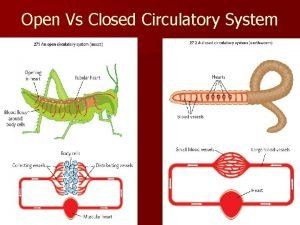
Blood pressure Open circulatory system vs closed
Open circulatory system vs closed Arterioles capillaries venules
Arterioles capillaries venules Youtube.com
Youtube.com Infraclavicular lymph nodes
Infraclavicular lymph nodes Veins of upper limb
Veins of upper limb Efferent lymphatic vessel
Efferent lymphatic vessel Short gastric arteries
Short gastric arteries Major arteries of the systemic circulation
Major arteries of the systemic circulation Posterior circulation
Posterior circulation Anterior choroidal artery
Anterior choroidal artery Hemiazygos vein
Hemiazygos vein Layers of chest wall
Layers of chest wall Aorta branches
Aorta branches Arteries of thoracic wall
Arteries of thoracic wall Posterior tibial arter
Posterior tibial arter Arteries of the upper limb
Arteries of the upper limb Thoracic anatomy
Thoracic anatomy Lymph nodes in buttocks
Lymph nodes in buttocks Systemic veins
Systemic veins