Dyspnoea III Pulmonary oedema EMC SDMH 2015 Define


- Slides: 20
Dyspnoea III – Pulmonary oedema { EMC SDMH 2015
Define the pulmonary oedema syndrome and understand differing aetiologies Recognise predisposing and precipitating factors in cardiogenic pulmonary oedema Outline ED treatment modalities Objectives
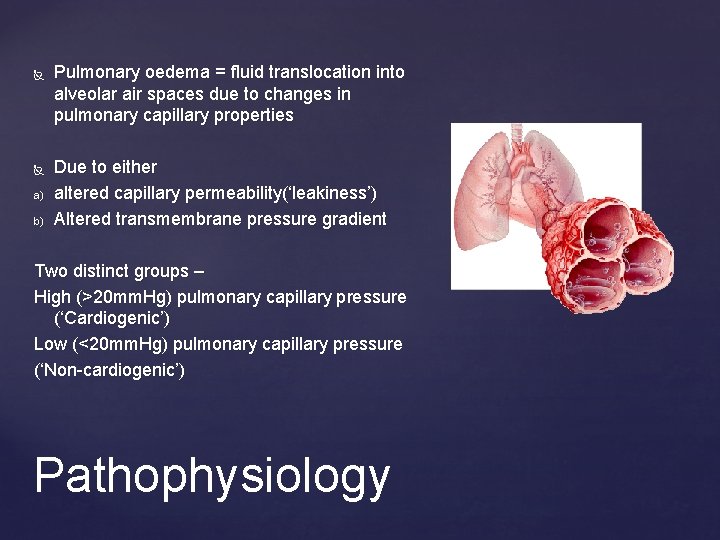
a) b) Pulmonary oedema = fluid translocation into alveolar air spaces due to changes in pulmonary capillary properties Due to either altered capillary permeability(‘leakiness’) Altered transmembrane pressure gradient Two distinct groups – High (>20 mm. Hg) pulmonary capillary pressure (‘Cardiogenic’) Low (<20 mm. Hg) pulmonary capillary pressure (‘Non-cardiogenic’) Pathophysiology
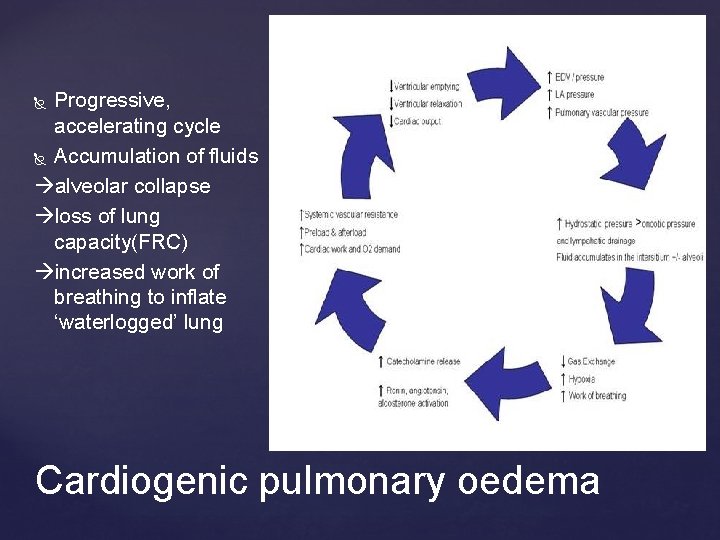
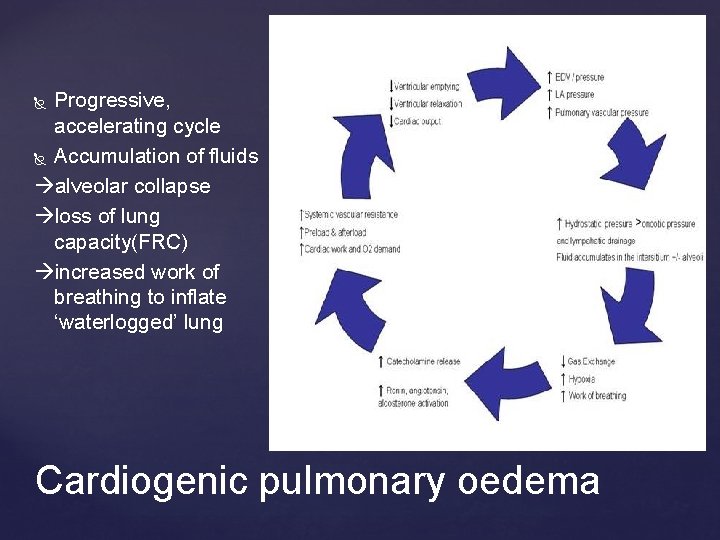
Progressive, accelerating cycle Accumulation of fluids alveolar collapse loss of lung capacity(FRC) increased work of breathing to inflate ‘waterlogged’ lung Cardiogenic pulmonary oedema
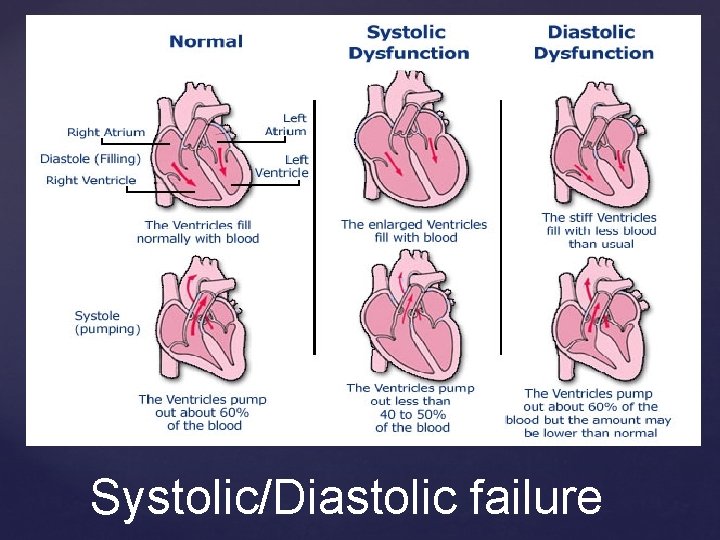
Cardiogenic pulmonary oedema = syndrome of ‘transient’ LV failure WHY does this individual have cardiogenic pulmonary oedema? ~40 -60% will have normal LVEF; not oedematous NOT synonymous with ‘CHF’ Raises concept of ‘diastolic’ vs ‘systolic’ LV failure Cardiac failure?
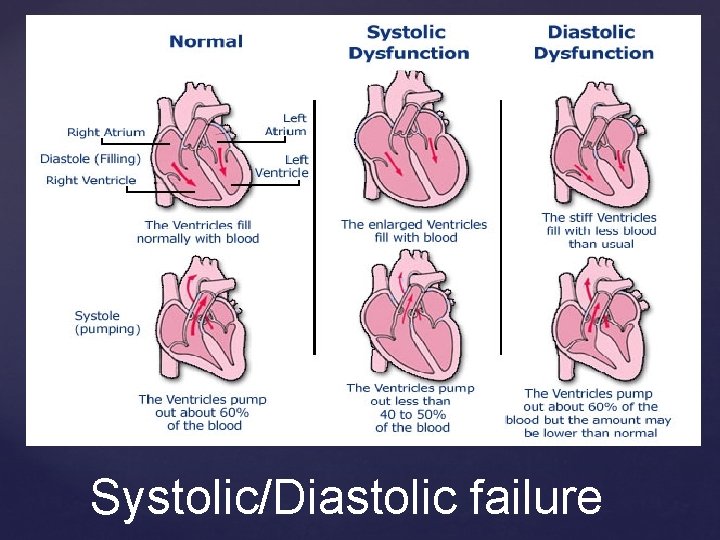
Systolic/Diastolic failure
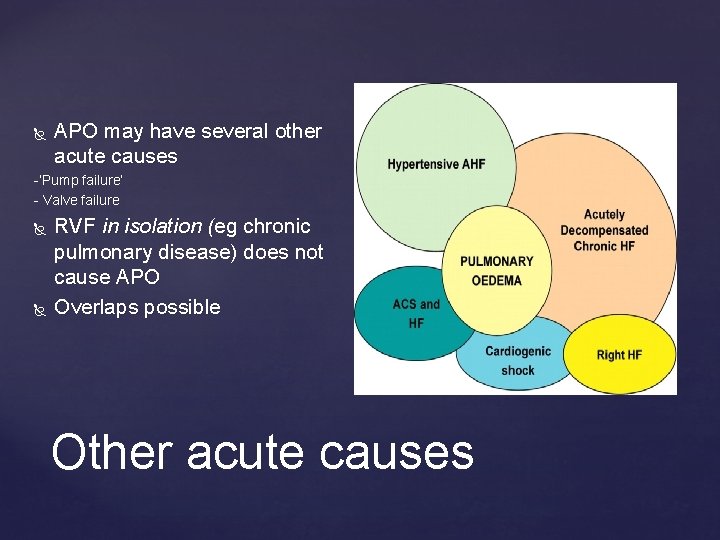
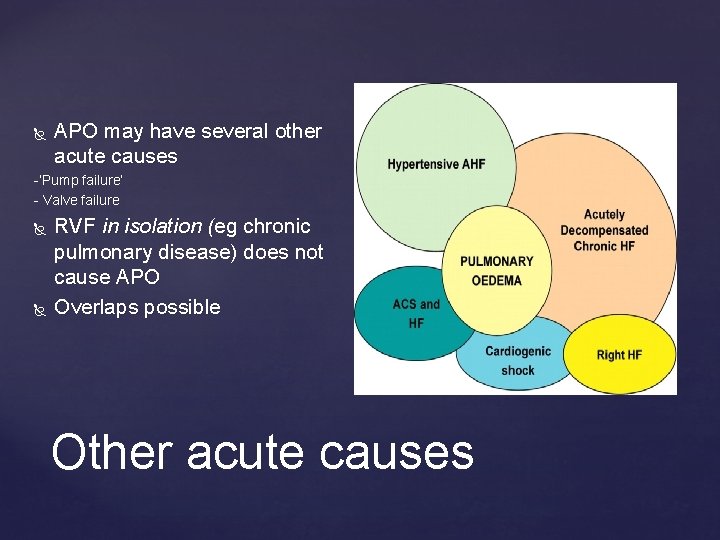
APO may have several other acute causes -’Pump failure’ - Valve failure RVF in isolation (eg ( chronic pulmonary disease) does not cause APO Overlaps possible Other acute causes
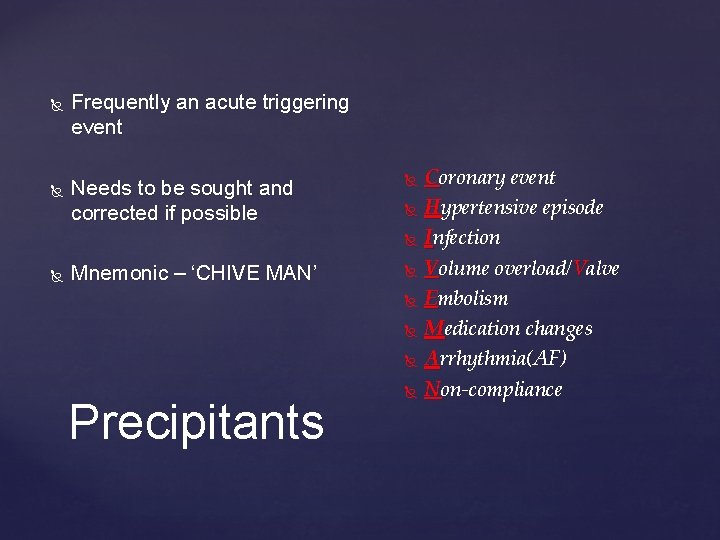
Frequently an acute triggering event Needs to be sought and corrected if possible Mnemonic – ‘CHIVE MAN’ Precipitants Coronary event Hypertensive episode Infection Volume overload/Valve Embolism Medication changes Arrhythmia(AF) Non-compliance
Principles of treatment -Reverse hypoxia -Reduce Wo. B -Decrease SVR -Improve cardiac output -Seek and remove triggering factors Management
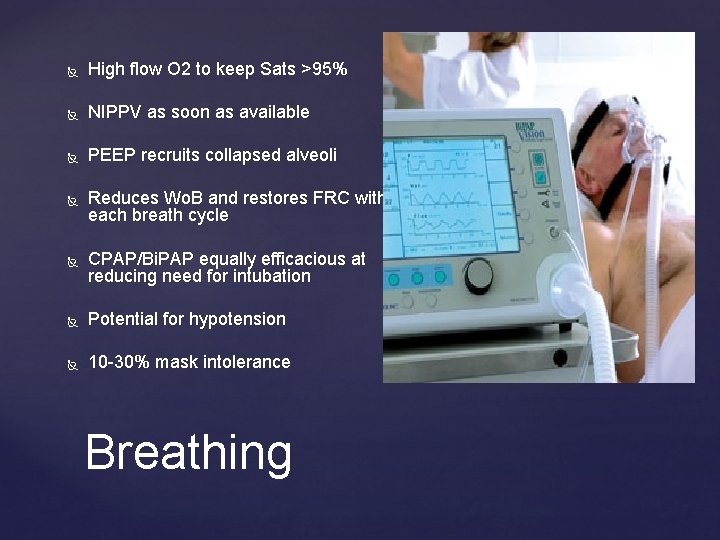
High flow O 2 to keep Sats >95% NIPPV as soon as available PEEP recruits collapsed alveoli Reduces Wo. B and restores FRC with each breath cycle CPAP/Bi. PAP equally efficacious at reducing need for intubation Potential for hypotension 10 -30% mask intolerance Breathing
Aim to reduce preload and afterload to assist failing LV PEEP reduces both by instituting intrathoracic pressure Effect can be increased by use of nitrates GTN SL or by infusion. GTN 600 mcg SL q 5 equivalent to 60 mcg/min infusion Action primarily by venodilation + preload reduction May cause hypotension. Avoid in Aortic Stenosis Circulation
Mainstay of treatment for 40 + yrs Primarily useful in volume overload APO Utility in hypertensive diastolic LVF? Postulated to have venodilating and diuretic effect Frusemide should produce diuresis in 15 -20 mins Diuretics
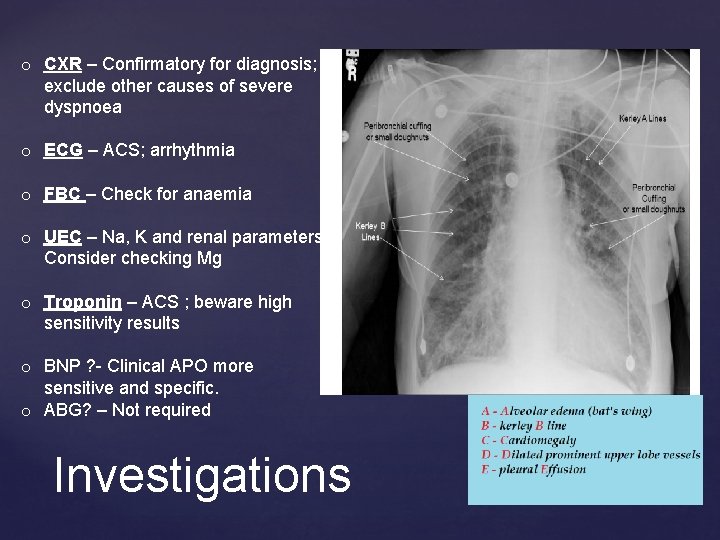
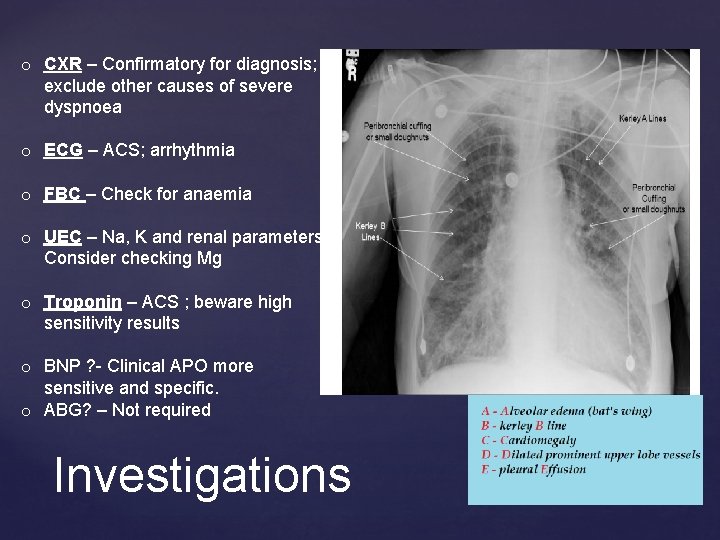
o CXR – Confirmatory for diagnosis; exclude other causes of severe dyspnoea o ECG – ACS; arrhythmia o FBC – Check for anaemia o UEC – Na, K and renal parameters. Consider checking Mg o Troponin – ACS ; beware high sensitivity results o BNP ? - Clinical APO more sensitive and specific. o ABG? – Not required Investigations
APO in the Dialysis patient APO with rapid AF APO with hypotension Challenging scenarios
Often true volume overload Prone to all other causes of LVF however!! Unable to remove salt/H 2 O Often respond well to NIPPV/nitrates Require emergent transfer to acute dialysis centre/ICU APO and the dialysis pt
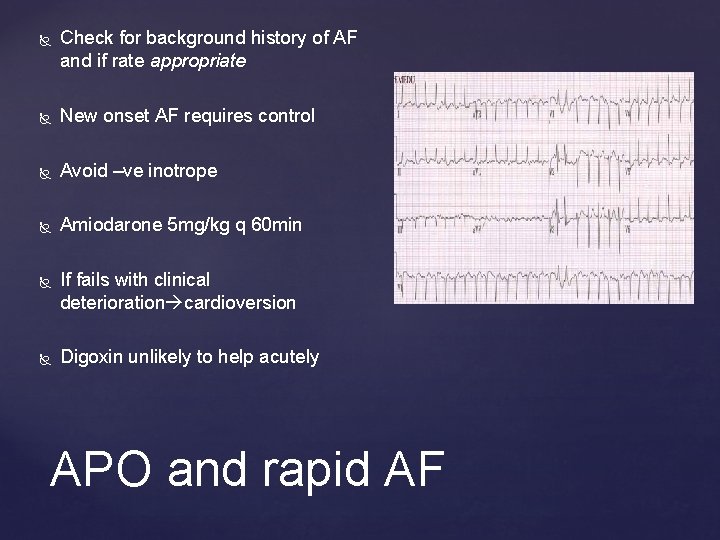
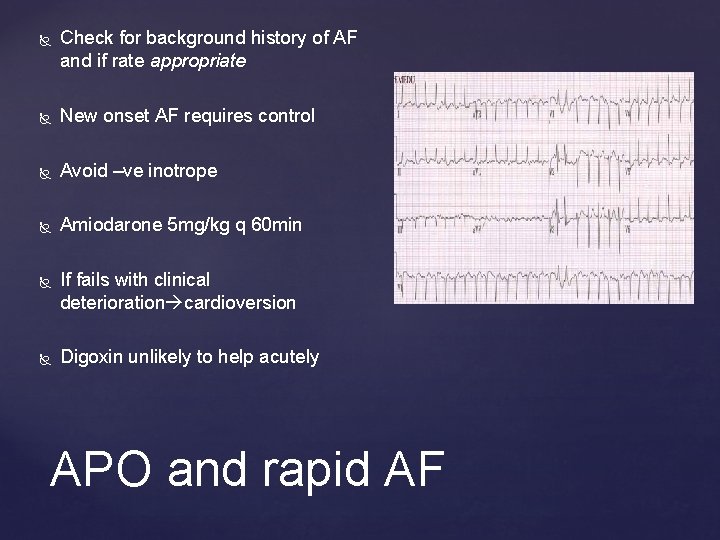
Check for background history of AF and if rate appropriate New onset AF requires control Avoid –ve inotrope Amiodarone 5 mg/kg q 60 min If fails with clinical deterioration cardioversion Digoxin unlikely to help acutely APO and rapid AF
Potentially = cardiogenic shock Check to ensure PEEP correct Assess cause and prognosis Senior intervention with Cardiology and ICU STEMI/ACS Retrieve to Cath. Centre (? Cardiothoracic) Dobutamine 2. 5 -20 mcg/kg/min OR Adrenaline. 01 -1 mcg/kg/min Consider early intubation (high risk) APO and hypotension

Questions?
APO = syndrome, not a diagnosis APO is due to LV failure which may be either due to systolic or diastolic failure NIPPV improves both oxygenation and cardiac performance Seek precipitating causes and treat Beware the hypotensive APO patient Summary

 Mrc dyspnoea scale
Mrc dyspnoea scale Mrc dyspnoea scale
Mrc dyspnoea scale Orhtopnoe
Orhtopnoe Grading of oedema
Grading of oedema Silver wiring retina
Silver wiring retina Lip oedema
Lip oedema Oedema malignum
Oedema malignum Hamlet act iii scene iii
Hamlet act iii scene iii Tapvc
Tapvc Tributaries of pulmonary vein
Tributaries of pulmonary vein Arteries
Arteries Pulmonary toilet
Pulmonary toilet Right marginal artery
Right marginal artery Priyanka breathing
Priyanka breathing Pulmonary surfactant function
Pulmonary surfactant function Pulmonary embolism cxr
Pulmonary embolism cxr Pft loops
Pft loops Hampton hump sign คือ
Hampton hump sign คือ Pulmonary embolism test
Pulmonary embolism test Med
Med Complications of empyema
Complications of empyema