City hospitals Sunderland AE Department Information Card Pack



- Slides: 46
City hospitals Sunderland A&E Department Information Card Pack Produced by Dr Sarah Frewin Correspondence to s. e. frewin@doctors. org. uk Review date: January 2012

Nexus C-spine rules Glasgow pancreatitis score Alvarado score Rectal bleeding differentials Upper GI bleed differentials Abdominal pain differentials Jaundice differentials Rockall score (GI bleed) ABCD 2 (TIA) Severe sepsis criteria Sepsis screening tool Severe sepsis 1 st hour pathway Soft tissue antibiotic policy Curb 65 (pneumonia) LRTI antibiotic policy Meningitis antibiotic policy UTI antibiotic policy Wells criteria (PE) Wells criteria (DVT) MRC dyspnoea scale ASA grading (anaesthetics) BTS asthma exacerbation grades NICE COPD guidance NICE head CT guidance (amendment) NICE head CT guidance Chest pain differentials Breathlessness / hypoxia differentials Bradyarrhythmia differentials Tachyarrhythmia differentials Reversible causes of cardiac arrest ECG interpretation New York heart failure classification Grading of murmurs Headache differentials Dizziness differentials AMTS Timed get up and go test Stroke mimics falls /collapse differentials Pain assessment Confusion differentials Hypotension differentials Stages of hypovolemic shock CO poisoning
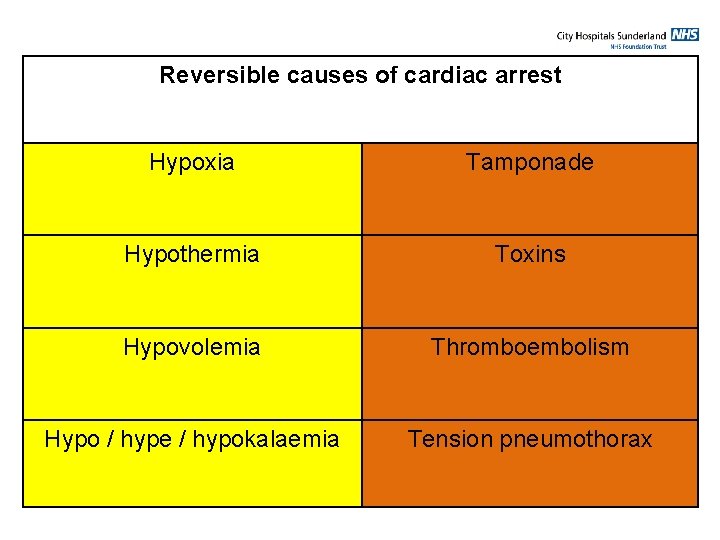
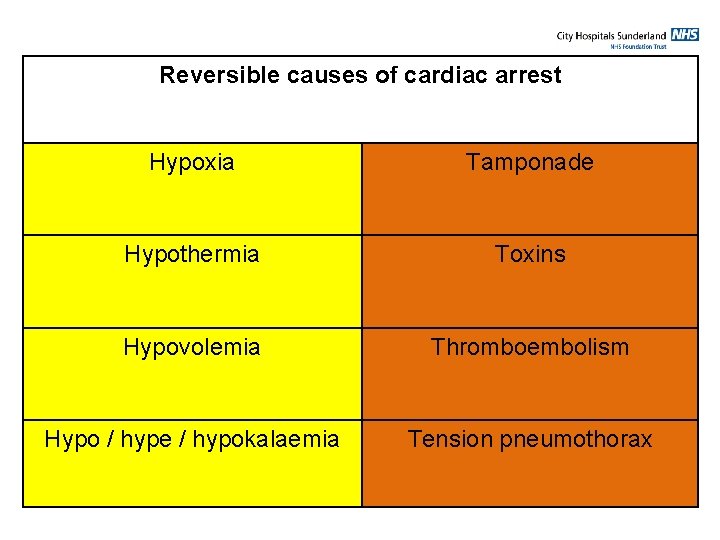
Reversible causes of cardiac arrest Hypoxia Tamponade Hypothermia Toxins Hypovolemia Thromboembolism Hypo / hype / hypokalaemia Tension pneumothorax
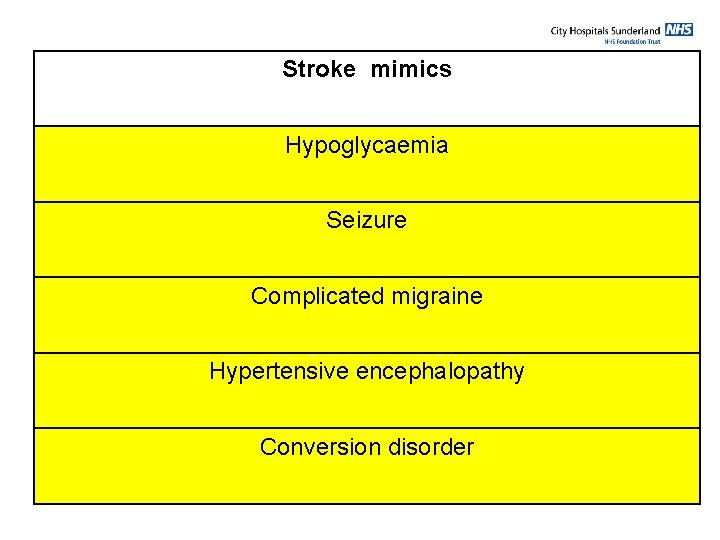
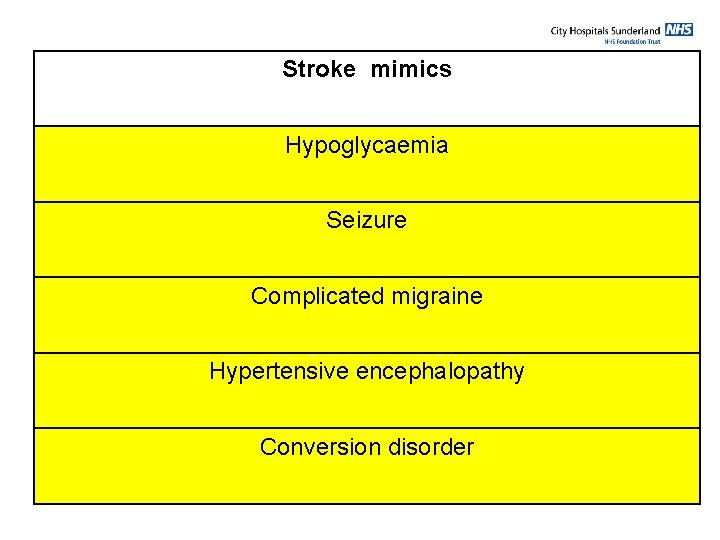
Stroke mimics Hypoglycaemia Seizure Complicated migraine Hypertensive encephalopathy Conversion disorder
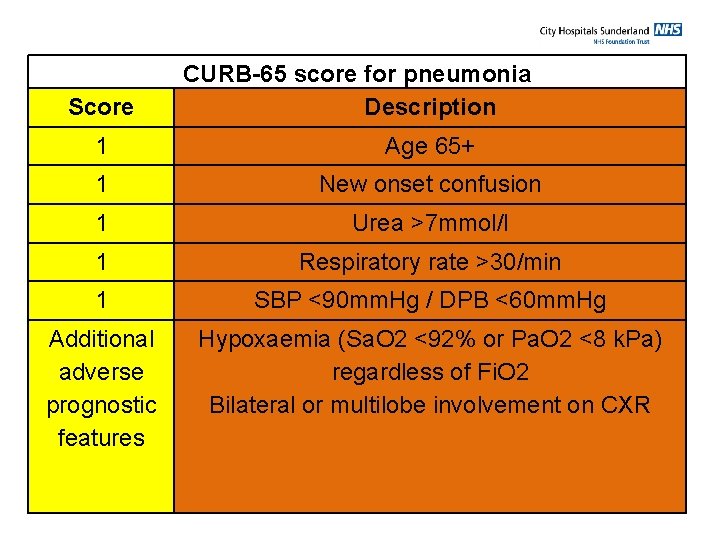
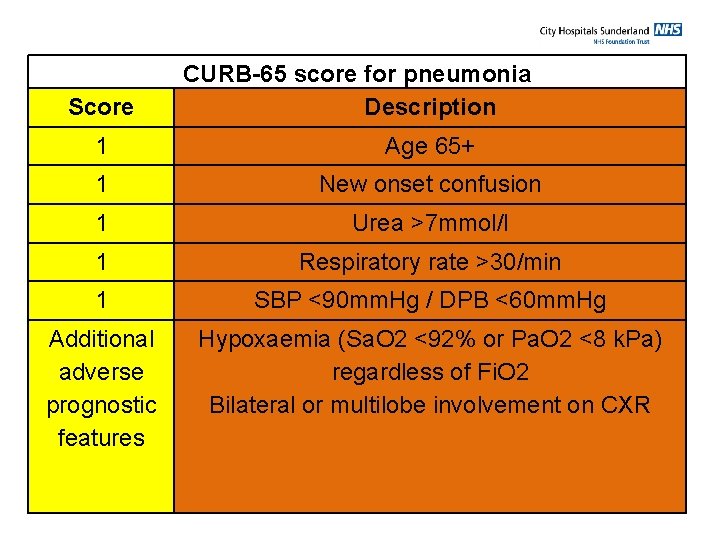
Score CURB-65 score for pneumonia Description 1 Age 65+ 1 New onset confusion 1 Urea >7 mmol/l 1 Respiratory rate >30/min 1 SBP <90 mm. Hg / DPB <60 mm. Hg Additional adverse prognostic features Hypoxaemia (Sa. O 2 <92% or Pa. O 2 <8 k. Pa) regardless of Fi. O 2 Bilateral or multilobe involvement on CXR
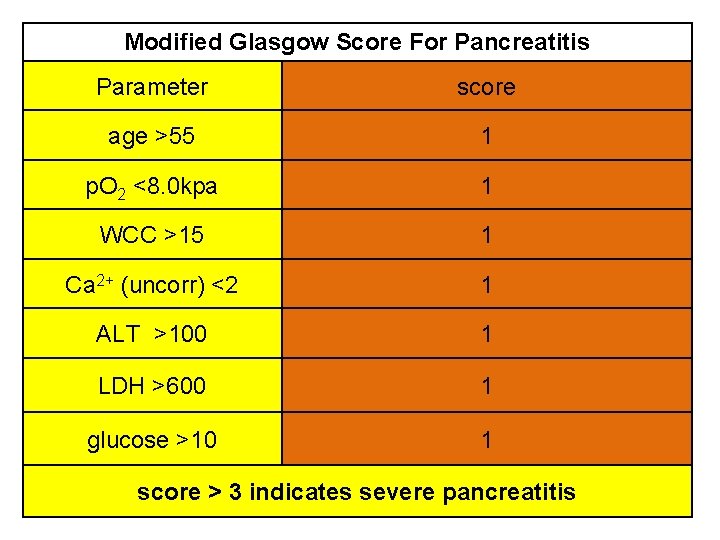
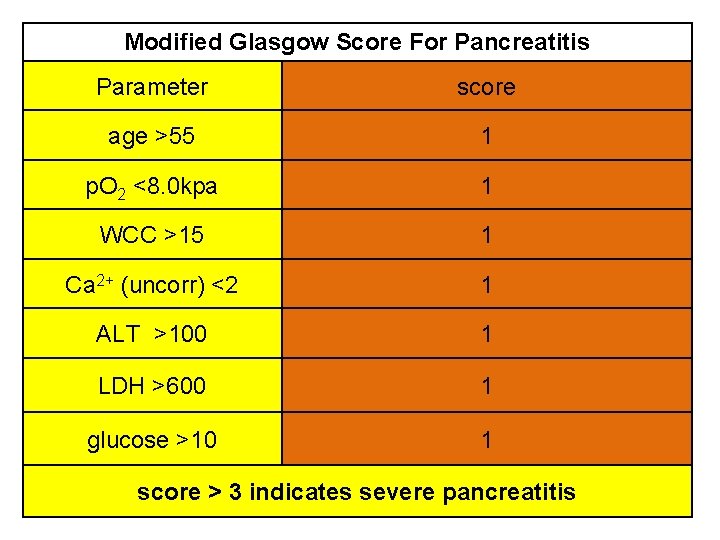
Modified Glasgow Score For Pancreatitis Parameter score age >55 1 p. O 2 <8. 0 kpa 1 WCC >15 1 Ca 2+ (uncorr) <2 1 ALT >100 1 LDH >600 1 glucose >10 1 score > 3 indicates severe pancreatitis
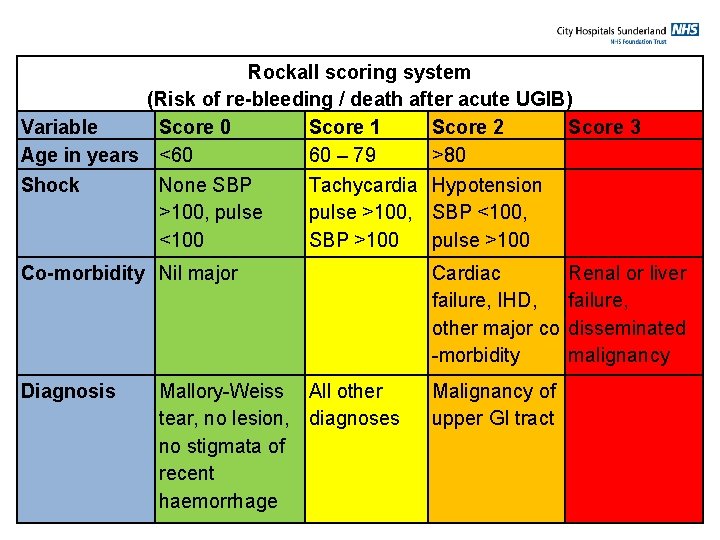
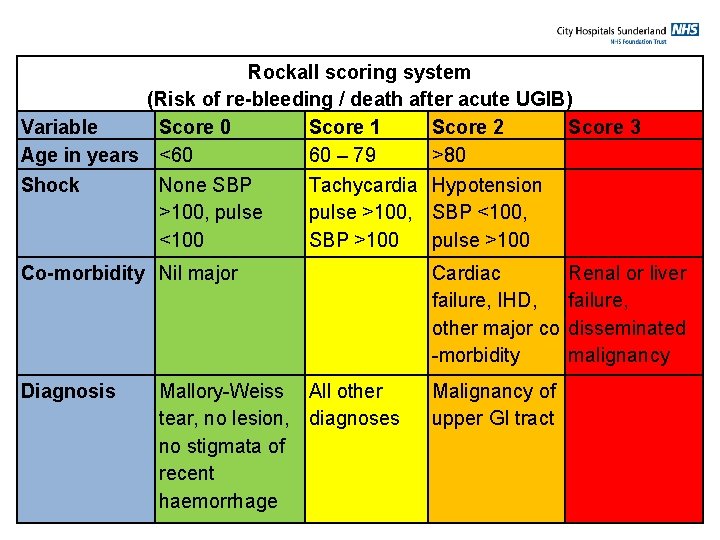
Rockall scoring system (Risk of re-bleeding / death after acute UGIB) Variable Score 0 Score 1 Score 2 Score 3 Age in years <60 60 – 79 >80 Shock None SBP Tachycardia Hypotension >100, pulse >100, SBP <100, <100 SBP >100 pulse >100 Co-morbidity Nil major Cardiac failure, IHD, other major co -morbidity Diagnosis Malignancy of upper GI tract Mallory-Weiss All other tear, no lesion, diagnoses no stigmata of recent haemorrhage Renal or liver failure, disseminated malignancy


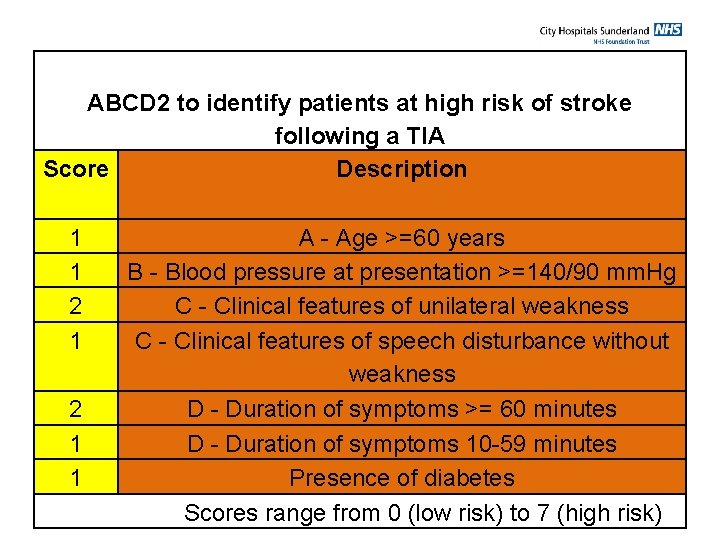
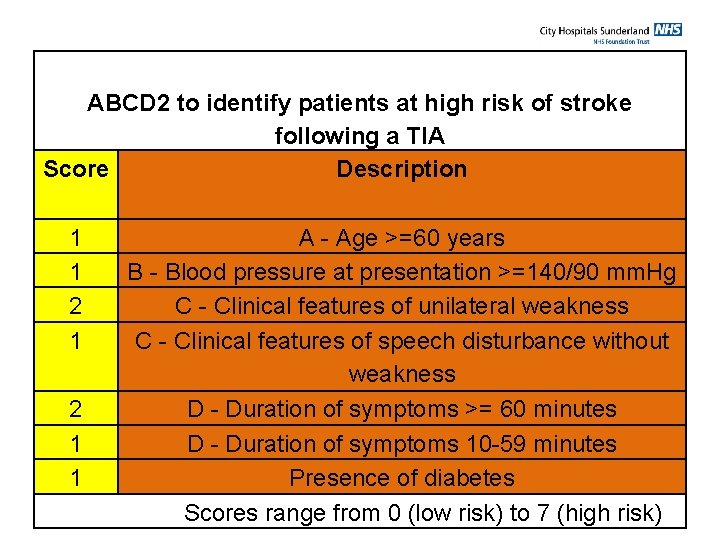
ABCD 2 to identify patients at high risk of stroke following a TIA Score Description 1 1 2 1 1 A - Age >=60 years B - Blood pressure at presentation >=140/90 mm. Hg C - Clinical features of unilateral weakness C - Clinical features of speech disturbance without weakness D - Duration of symptoms >= 60 minutes D - Duration of symptoms 10 -59 minutes Presence of diabetes Scores range from 0 (low risk) to 7 (high risk)
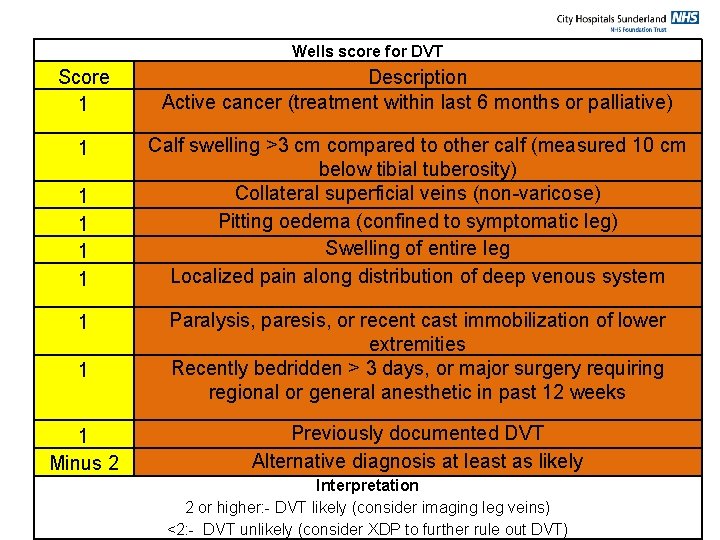
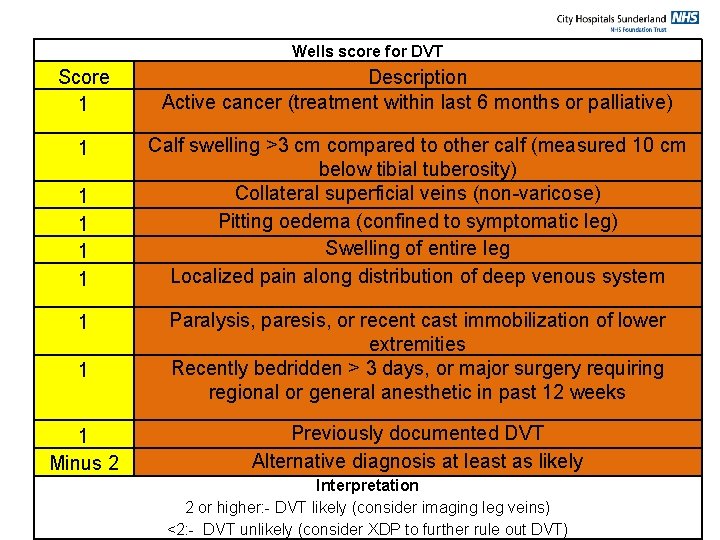
Wells score for DVT Score 1 Description Active cancer (treatment within last 6 months or palliative) 1 Calf swelling >3 cm compared to other calf (measured 10 cm below tibial tuberosity) Collateral superficial veins (non-varicose) Pitting oedema (confined to symptomatic leg) Swelling of entire leg Localized pain along distribution of deep venous system 1 1 1 1 Minus 2 Paralysis, paresis, or recent cast immobilization of lower extremities Recently bedridden > 3 days, or major surgery requiring regional or general anesthetic in past 12 weeks Previously documented DVT Alternative diagnosis at least as likely Interpretation 2 or higher: - DVT likely (consider imaging leg veins) <2: - DVT unlikely (consider XDP to further rule out DVT)
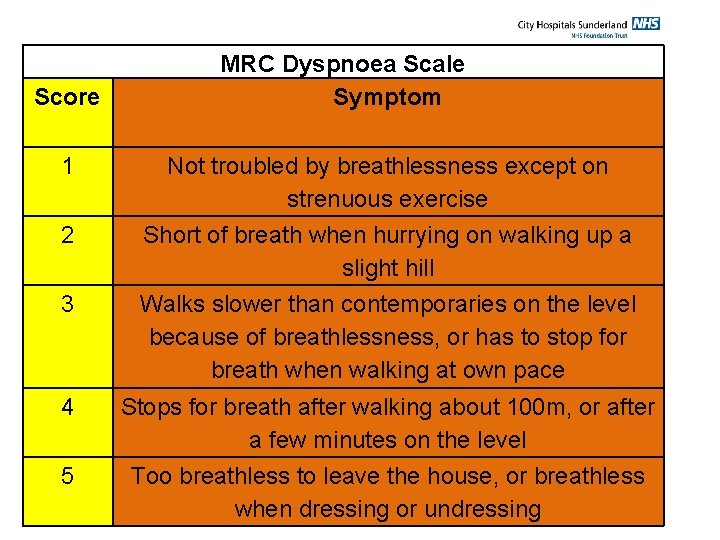
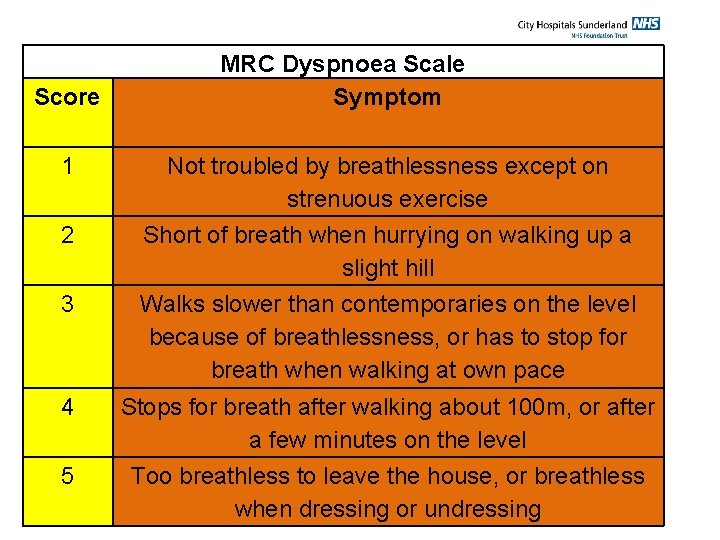
Score 1 2 3 4 5 MRC Dyspnoea Scale Symptom Not troubled by breathlessness except on strenuous exercise Short of breath when hurrying on walking up a slight hill Walks slower than contemporaries on the level because of breathlessness, or has to stop for breath when walking at own pace Stops for breath after walking about 100 m, or after a few minutes on the level Too breathless to leave the house, or breathless when dressing or undressing
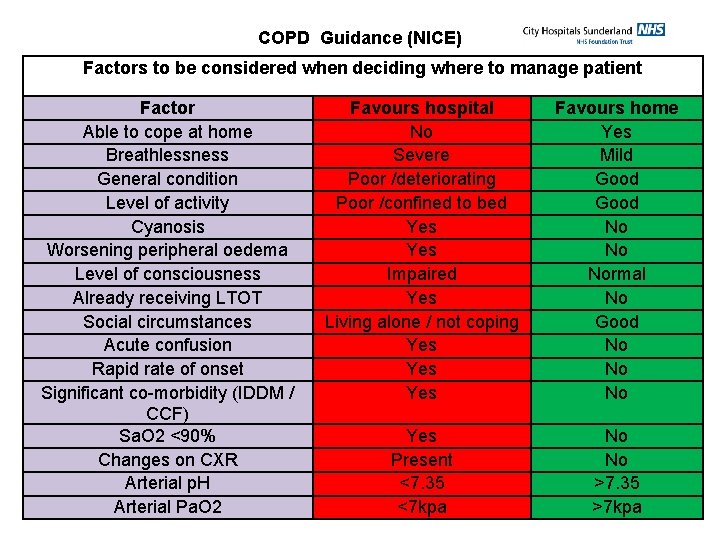
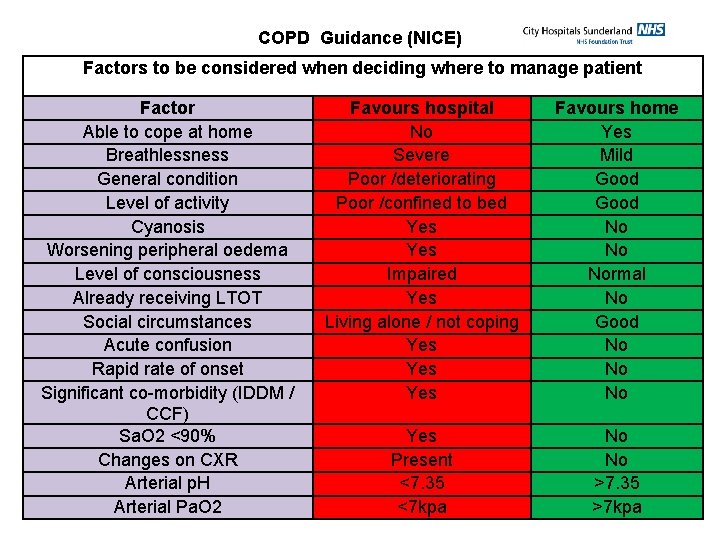
COPD Guidance (NICE) Factors to be considered when deciding where to manage patient Factor Able to cope at home Breathlessness General condition Level of activity Cyanosis Worsening peripheral oedema Level of consciousness Already receiving LTOT Social circumstances Acute confusion Rapid rate of onset Significant co-morbidity (IDDM / CCF) Sa. O 2 <90% Changes on CXR Arterial p. H Arterial Pa. O 2 Favours hospital No Severe Poor /deteriorating Poor /confined to bed Yes Impaired Yes Living alone / not coping Yes Yes Favours home Yes Mild Good No No Normal No Good No No No Yes Present <7. 35 <7 kpa No No >7. 35 >7 kpa
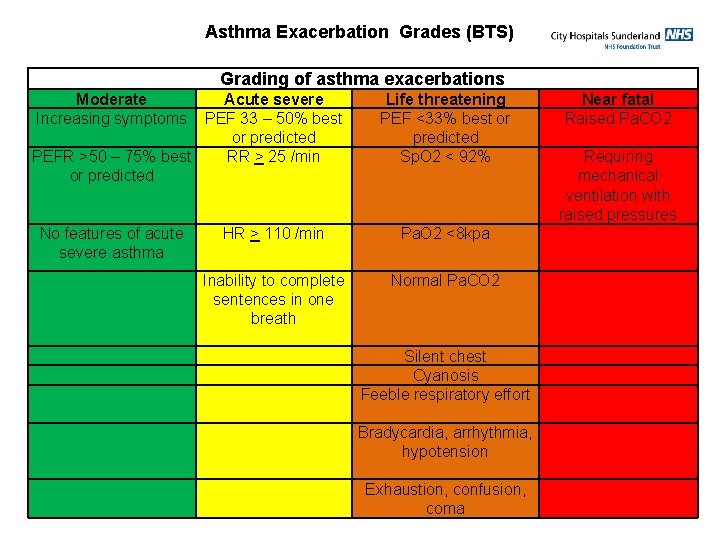
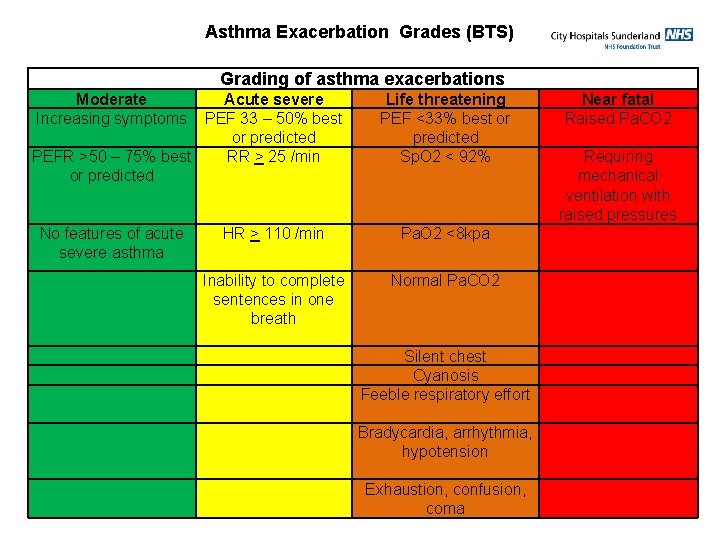
Asthma Exacerbation Grades (BTS) Grading of asthma exacerbations Moderate Increasing symptoms Acute severe PEF 33 – 50% best or predicted PEFR >50 – 75% best RR > 25 /min or predicted No features of acute severe asthma Life threatening PEF <33% best or predicted Sp. O 2 < 92% HR > 110 /min Pa. O 2 <8 kpa Inability to complete sentences in one breath Normal Pa. CO 2 Silent chest Cyanosis Feeble respiratory effort Bradycardia, arrhythmia, hypotension Exhaustion, confusion, coma Near fatal Raised Pa. CO 2 Requiring mechanical ventilation with raised pressures
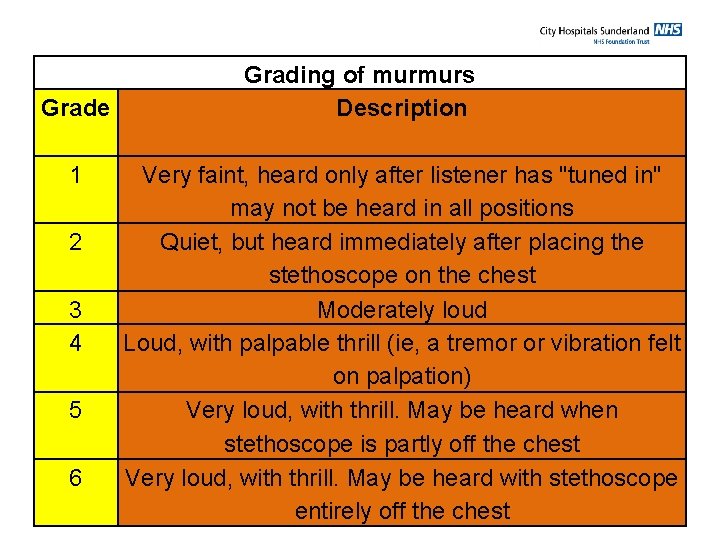
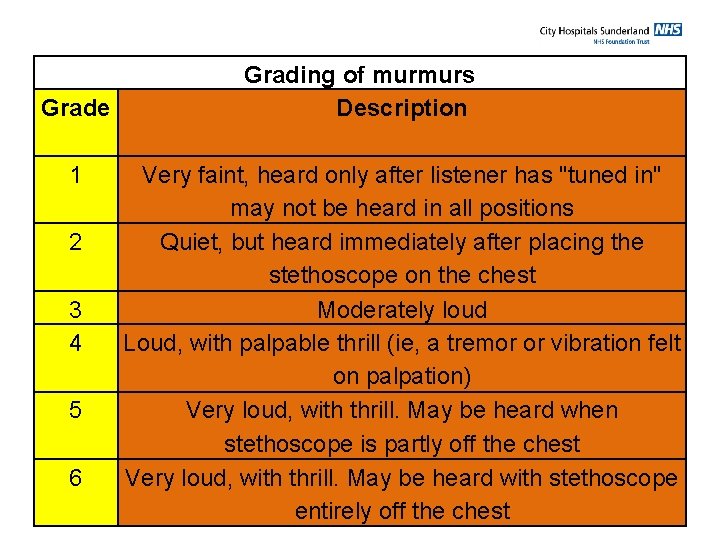
Grade 1 2 3 4 5 6 Grading of murmurs Description Very faint, heard only after listener has "tuned in" may not be heard in all positions Quiet, but heard immediately after placing the stethoscope on the chest Moderately loud Loud, with palpable thrill (ie, a tremor or vibration felt on palpation) Very loud, with thrill. May be heard when stethoscope is partly off the chest Very loud, with thrill. May be heard with stethoscope entirely off the chest
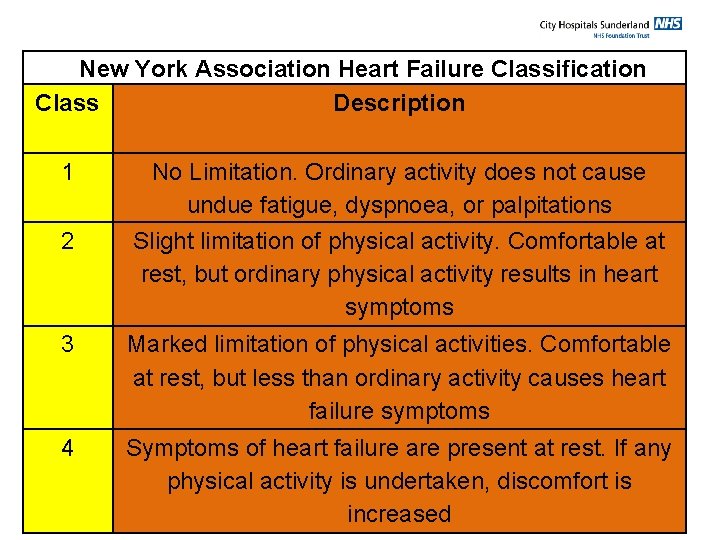
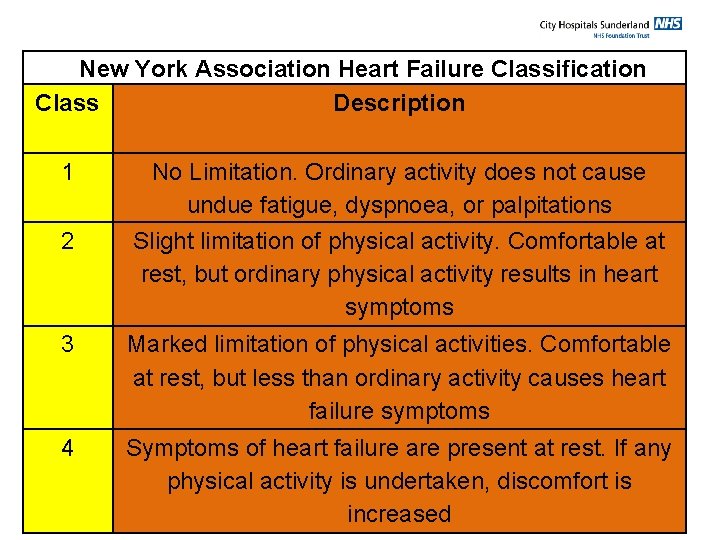
New York Association Heart Failure Classification Class Description 1 No Limitation. Ordinary activity does not cause undue fatigue, dyspnoea, or palpitations 2 Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in heart symptoms 3 Marked limitation of physical activities. Comfortable at rest, but less than ordinary activity causes heart failure symptoms 4 Symptoms of heart failure are present at rest. If any physical activity is undertaken, discomfort is increased
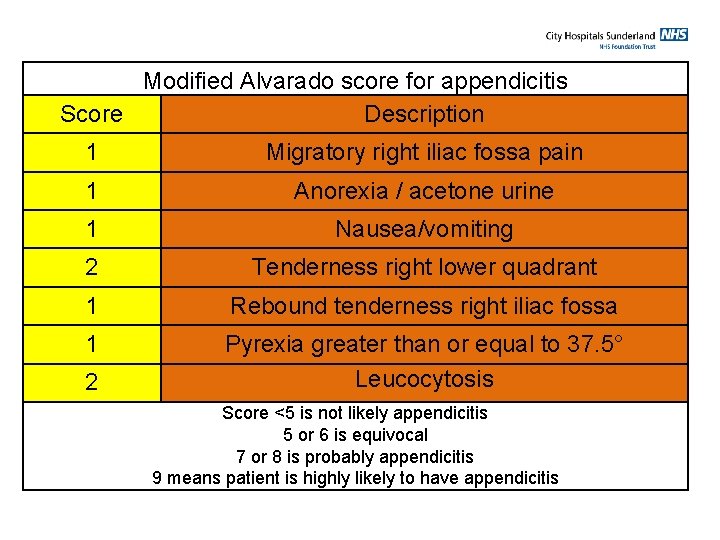
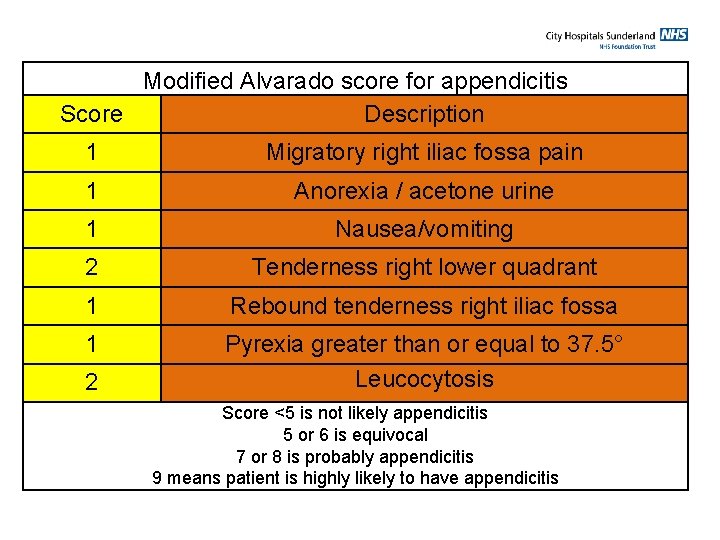
Modified Alvarado score for appendicitis Score Description 1 Migratory right iliac fossa pain 1 Anorexia / acetone urine 1 Nausea/vomiting 2 Tenderness right lower quadrant 1 Rebound tenderness right iliac fossa 1 Pyrexia greater than or equal to 37. 5° Leucocytosis 2 Score <5 is not likely appendicitis 5 or 6 is equivocal 7 or 8 is probably appendicitis 9 means patient is highly likely to have appendicitis
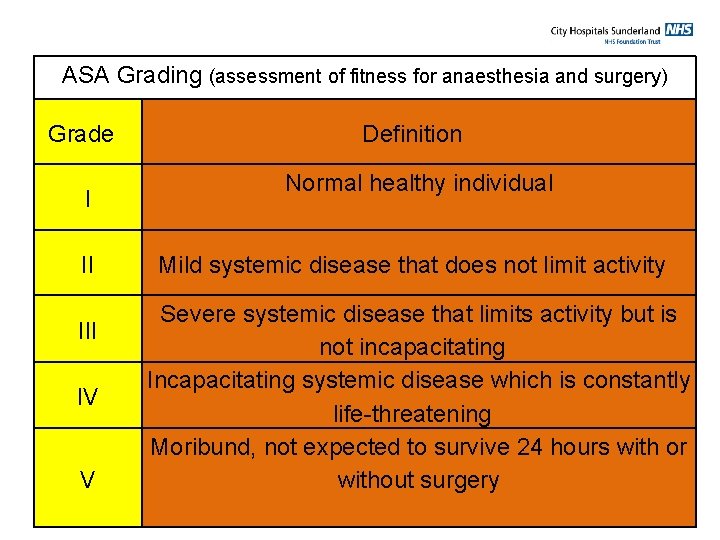
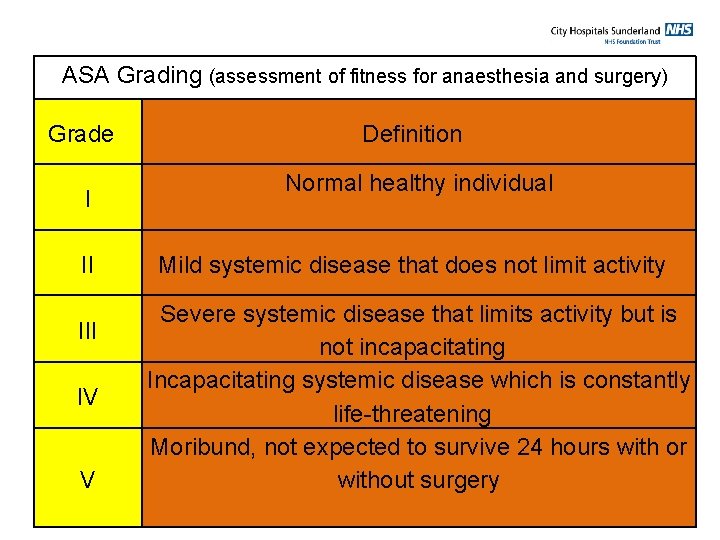
ASA Grading (assessment of fitness for anaesthesia and surgery) Grade Definition I Normal healthy individual II Mild systemic disease that does not limit activity III IV V Severe systemic disease that limits activity but is not incapacitating Incapacitating systemic disease which is constantly life-threatening Moribund, not expected to survive 24 hours with or without surgery
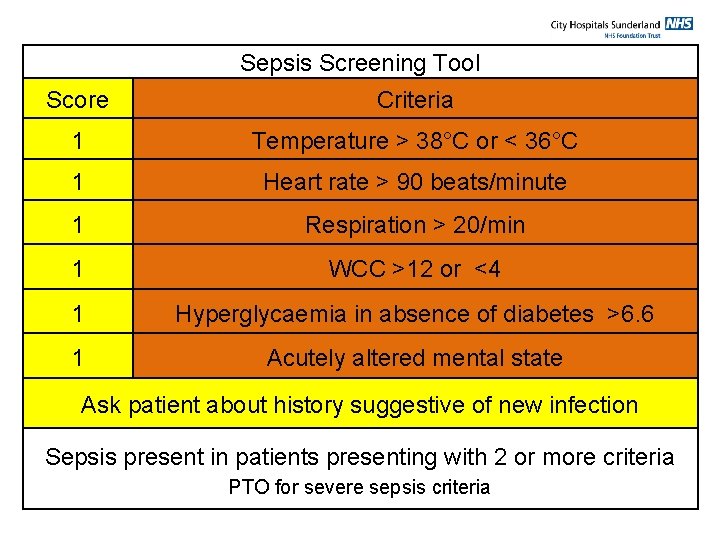
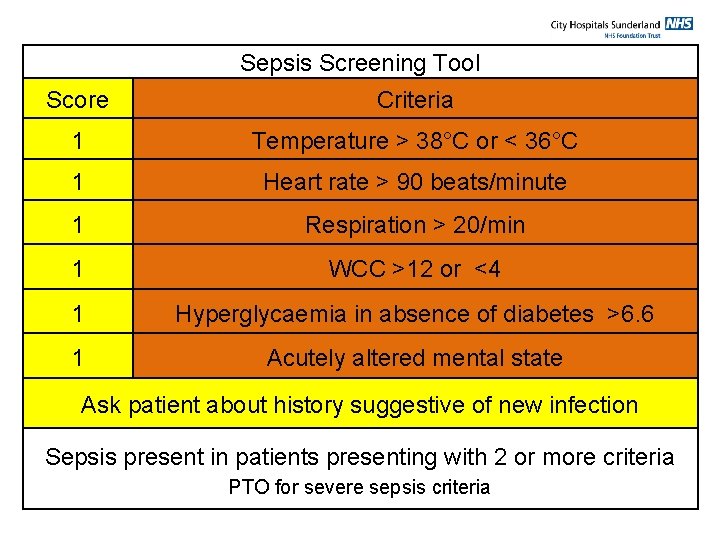
Sepsis Screening Tool Score Criteria 1 Temperature > 38°C or < 36°C 1 Heart rate > 90 beats/minute 1 Respiration > 20/min 1 WCC >12 or <4 1 Hyperglycaemia in absence of diabetes >6. 6 1 Acutely altered mental state Ask patient about history suggestive of new infection Sepsis present in patients presenting with 2 or more criteria PTO for severe sepsis criteria
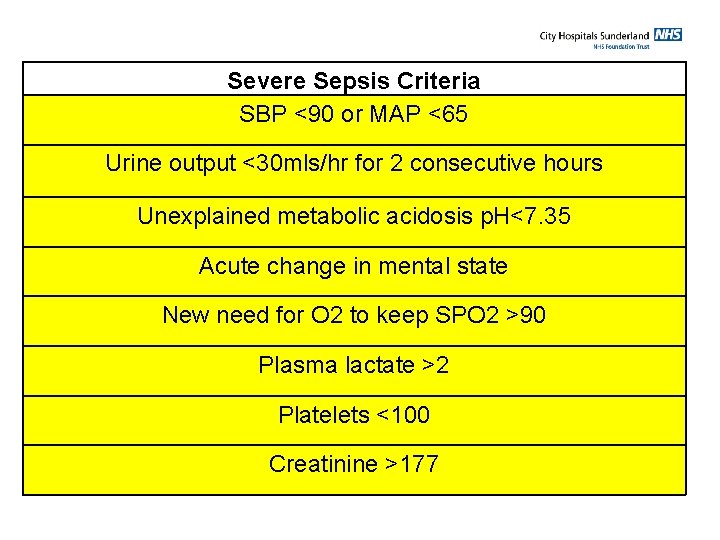
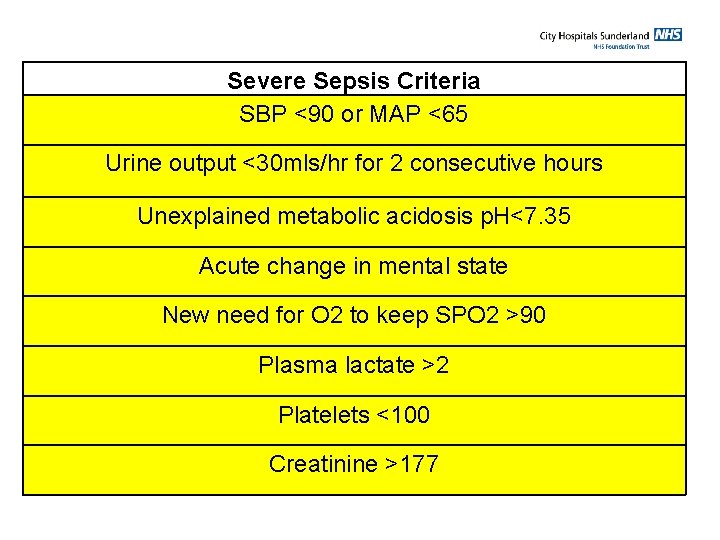
Severe Sepsis Criteria SBP <90 or MAP <65 Urine output <30 mls/hr for 2 consecutive hours Unexplained metabolic acidosis p. H<7. 35 Acute change in mental state New need for O 2 to keep SPO 2 >90 Plasma lactate >2 Platelets <100 Creatinine >177
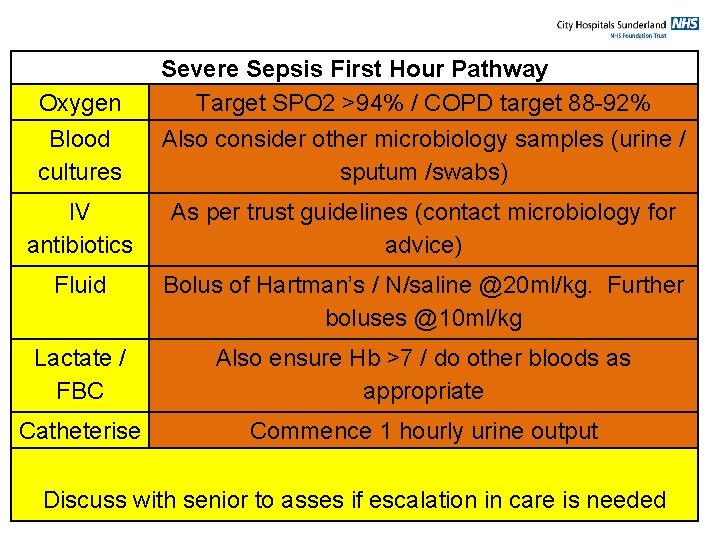
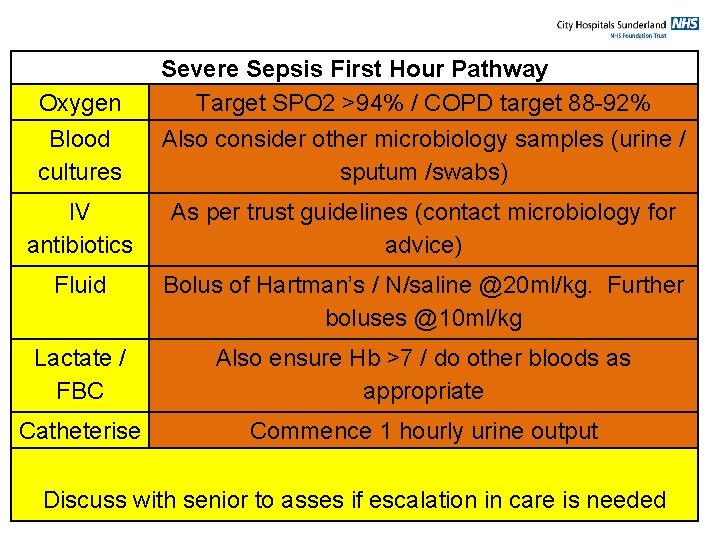
Oxygen Severe Sepsis First Hour Pathway Target SPO 2 >94% / COPD target 88 -92% Blood cultures Also consider other microbiology samples (urine / sputum /swabs) IV antibiotics As per trust guidelines (contact microbiology for advice) Fluid Bolus of Hartman’s / N/saline @20 ml/kg. Further boluses @10 ml/kg Lactate / FBC Also ensure Hb >7 / do other bloods as appropriate Catheterise Commence 1 hourly urine output Discuss with senior to asses if escalation in care is needed
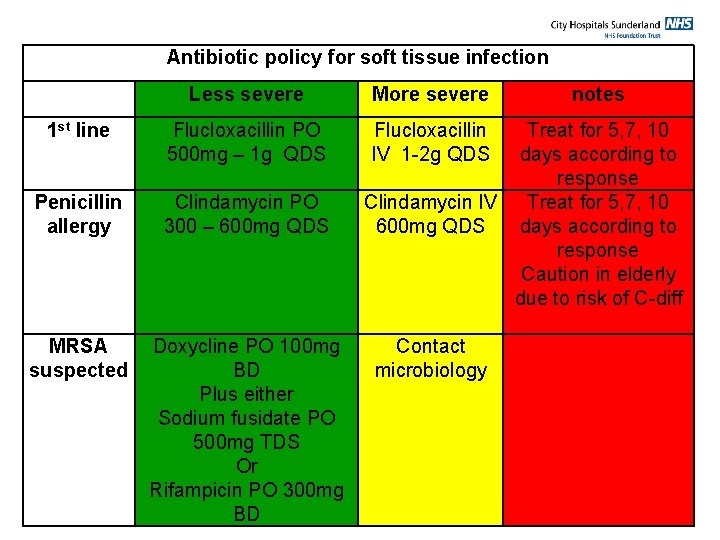
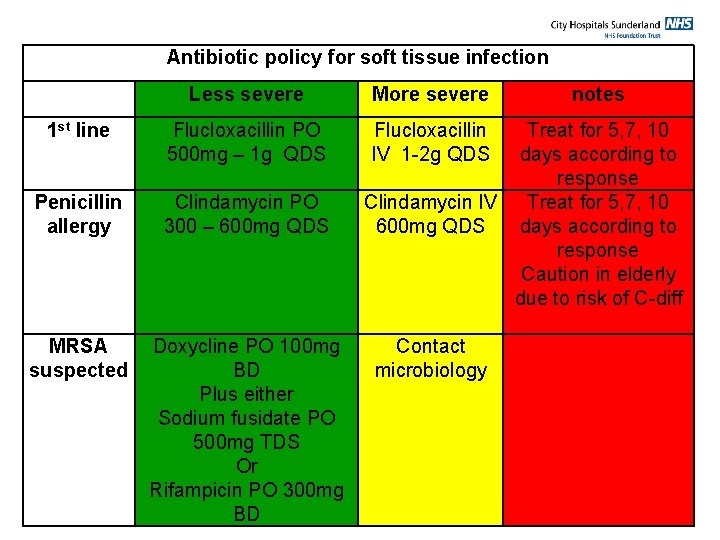
Antibiotic policy for soft tissue infection Less severe More severe 1 st line Flucloxacillin PO 500 mg – 1 g QDS Flucloxacillin IV 1 -2 g QDS Penicillin allergy Clindamycin PO 300 – 600 mg QDS MRSA suspected Doxycline PO 100 mg BD Plus either Sodium fusidate PO 500 mg TDS Or Rifampicin PO 300 mg BD notes Treat for 5, 7, 10 days according to response Clindamycin IV Treat for 5, 7, 10 600 mg QDS days according to response Caution in elderly due to risk of C-diff Contact microbiology
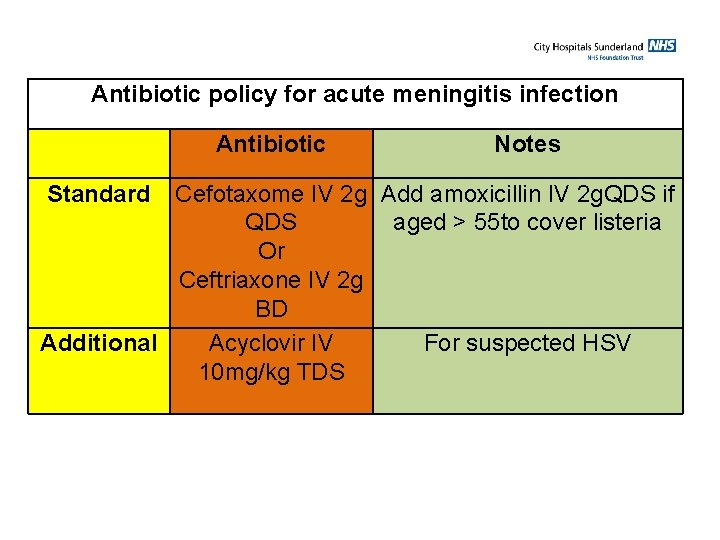
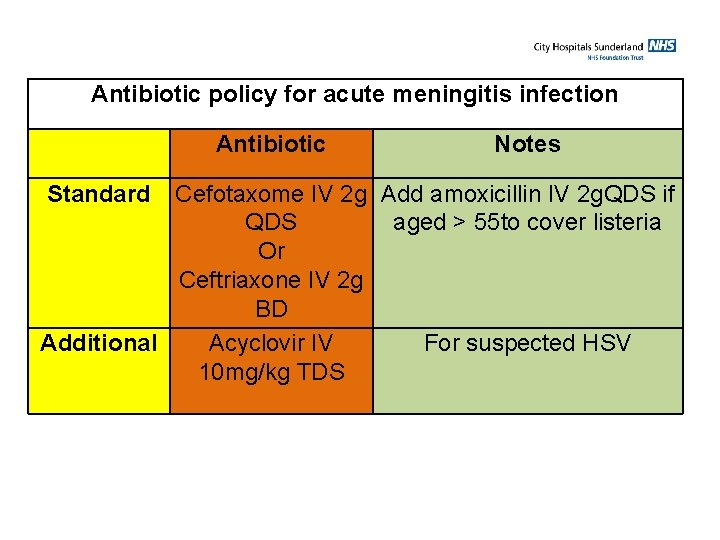
Antibiotic policy for acute meningitis infection Antibiotic Standard Notes Cefotaxome IV 2 g Add amoxicillin IV 2 g. QDS if QDS aged > 55 to cover listeria Or Ceftriaxone IV 2 g BD Additional Acyclovir IV For suspected HSV 10 mg/kg TDS
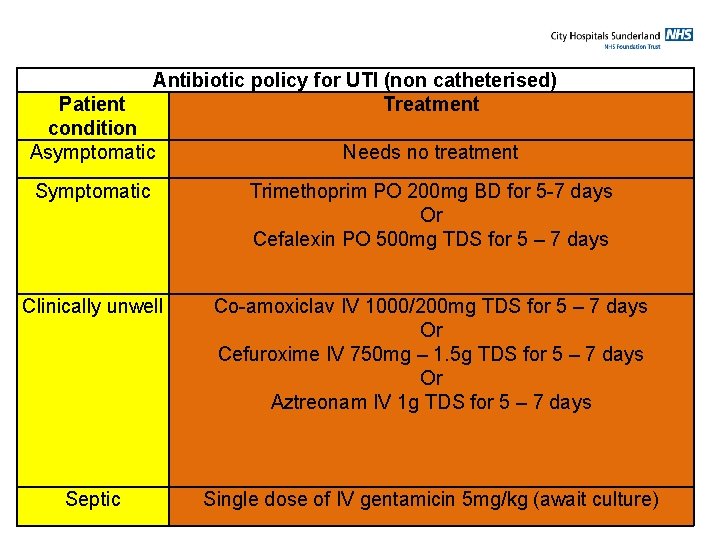
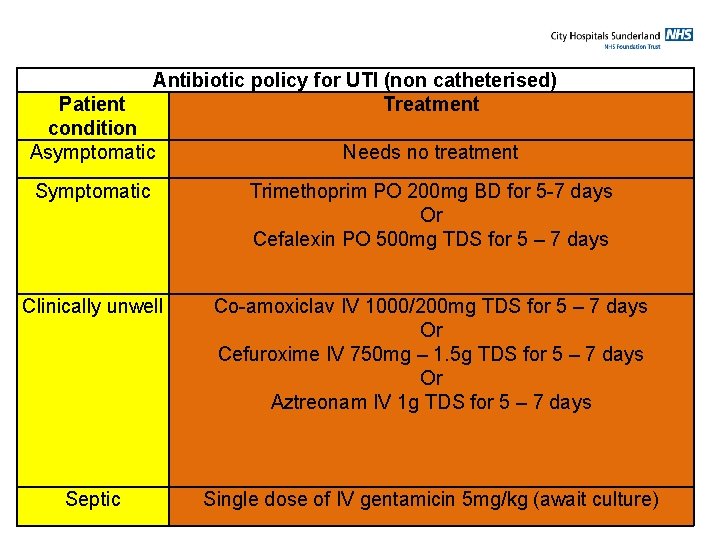
Antibiotic policy for UTI (non catheterised) Treatment Patient condition Asymptomatic Needs no treatment Symptomatic Trimethoprim PO 200 mg BD for 5 -7 days Or Cefalexin PO 500 mg TDS for 5 – 7 days Clinically unwell Co-amoxiclav IV 1000/200 mg TDS for 5 – 7 days Or Cefuroxime IV 750 mg – 1. 5 g TDS for 5 – 7 days Or Aztreonam IV 1 g TDS for 5 – 7 days Septic Single dose of IV gentamicin 5 mg/kg (await culture)
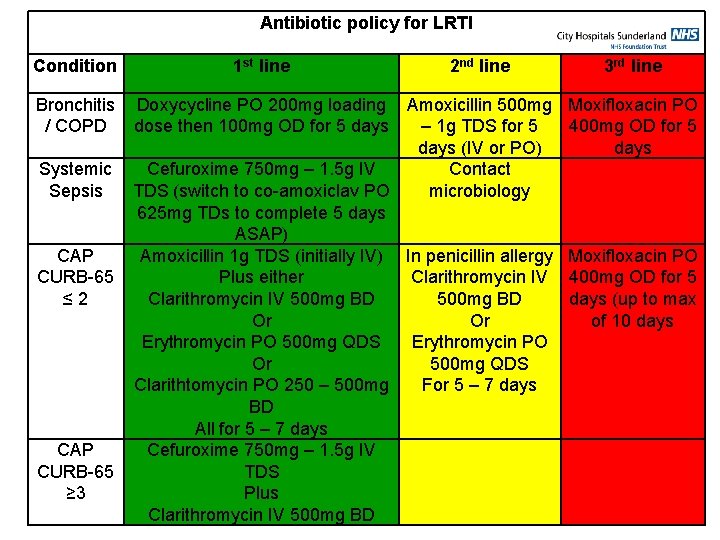
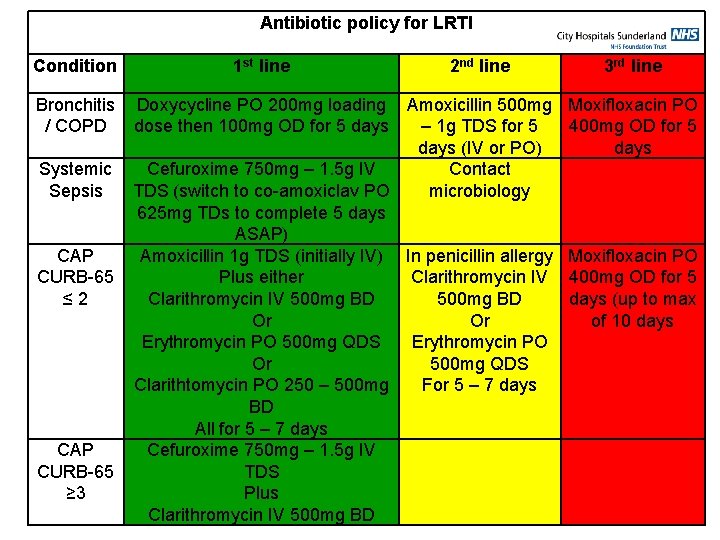
Antibiotic policy for LRTI Condition 1 st line 2 nd line 3 rd line Bronchitis Doxycycline PO 200 mg loading Amoxicillin 500 mg Moxifloxacin PO / COPD dose then 100 mg OD for 5 days – 1 g TDS for 5 400 mg OD for 5 days (IV or PO) days Systemic Cefuroxime 750 mg – 1. 5 g IV Contact Sepsis TDS (switch to co-amoxiclav PO microbiology 625 mg TDs to complete 5 days ASAP) CAP Amoxicillin 1 g TDS (initially IV) In penicillin allergy Moxifloxacin PO CURB-65 Plus either Clarithromycin IV 400 mg OD for 5 ≤ 2 Clarithromycin IV 500 mg BD days (up to max Or Or of 10 days Erythromycin PO 500 mg QDS Erythromycin PO Or 500 mg QDS Clarithtomycin PO 250 – 500 mg For 5 – 7 days BD All for 5 – 7 days CAP Cefuroxime 750 mg – 1. 5 g IV CURB-65 TDS ≥ 3 Plus Clarithromycin IV 500 mg BD
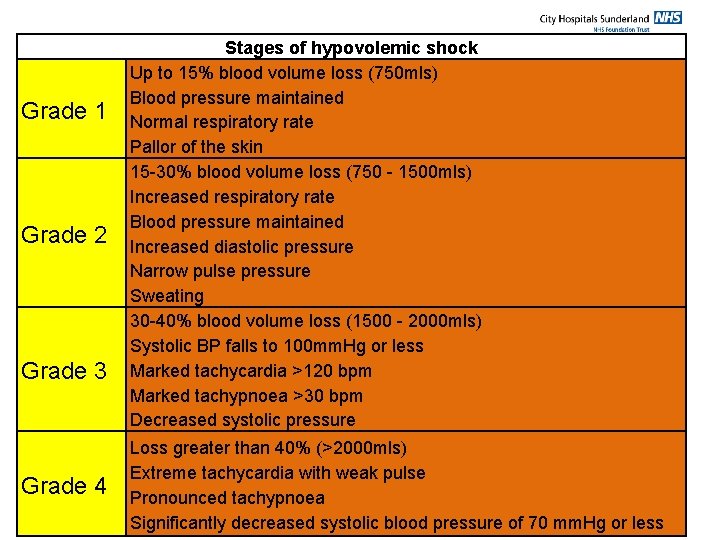
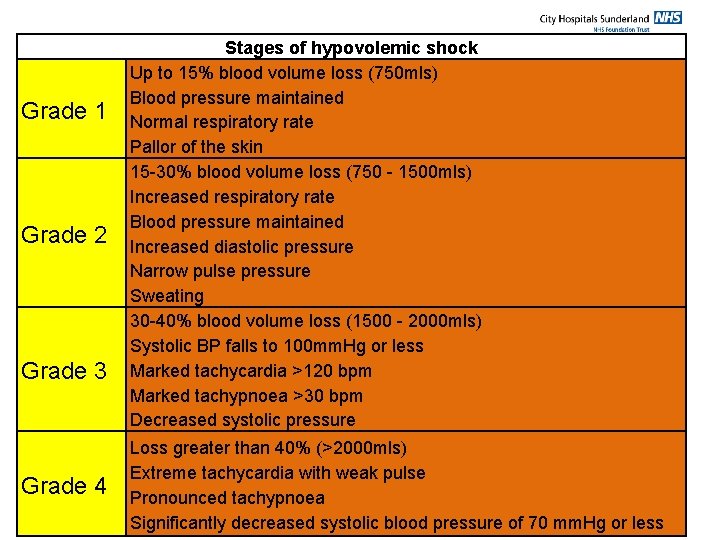
Grade 1 Grade 2 Grade 3 Grade 4 Stages of hypovolemic shock Up to 15% blood volume loss (750 mls) Blood pressure maintained Normal respiratory rate Pallor of the skin 15 -30% blood volume loss (750 - 1500 mls) Increased respiratory rate Blood pressure maintained Increased diastolic pressure Narrow pulse pressure Sweating 30 -40% blood volume loss (1500 - 2000 mls) Systolic BP falls to 100 mm. Hg or less Marked tachycardia >120 bpm Marked tachypnoea >30 bpm Decreased systolic pressure Loss greater than 40% (>2000 mls) Extreme tachycardia with weak pulse Pronounced tachypnoea Significantly decreased systolic blood pressure of 70 mm. Hg or less
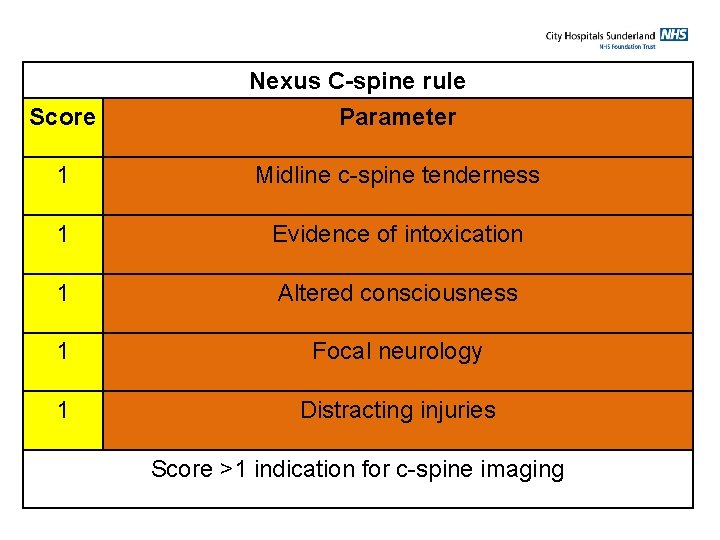
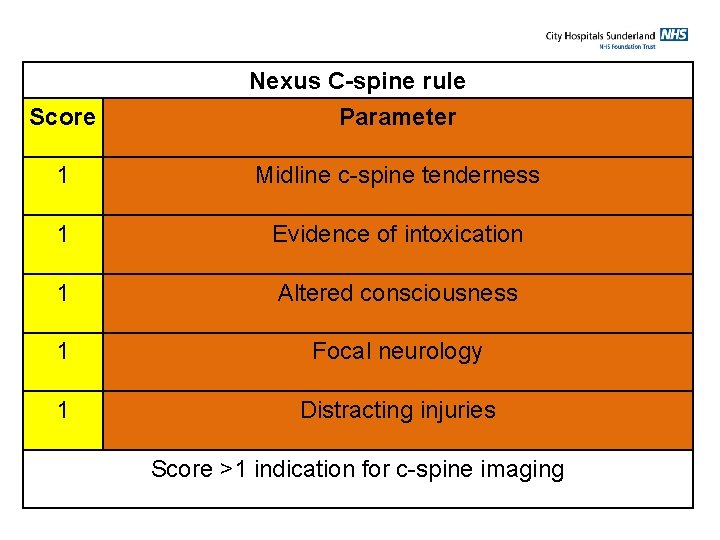
Nexus C-spine rule Score Parameter 1 Midline c-spine tenderness 1 Evidence of intoxication 1 Altered consciousness 1 Focal neurology 1 Distracting injuries Score >1 indication for c-spine imaging
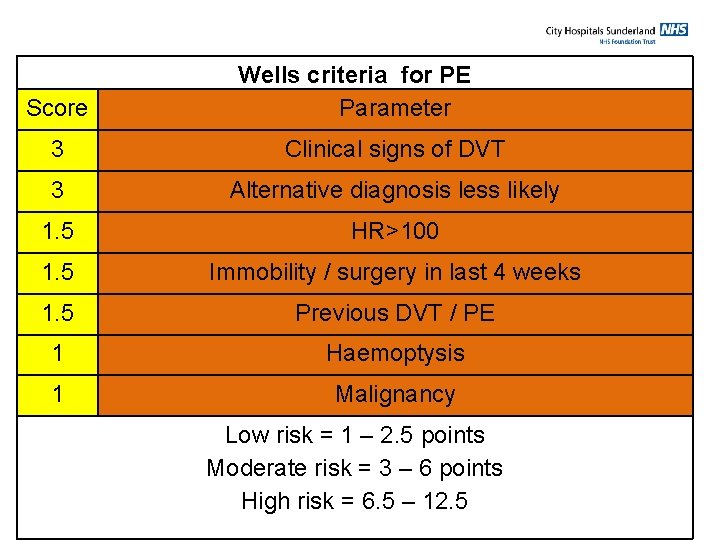
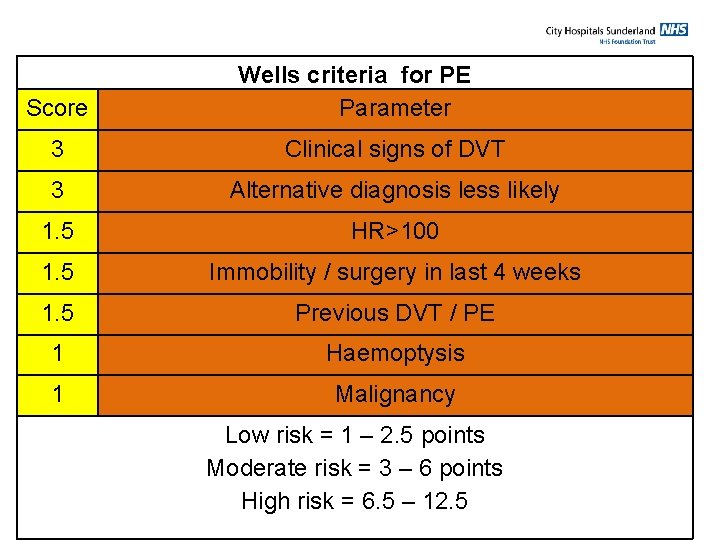
Score Wells criteria for PE Parameter 3 Clinical signs of DVT 3 Alternative diagnosis less likely 1. 5 HR>100 1. 5 Immobility / surgery in last 4 weeks 1. 5 Previous DVT / PE 1 Haemoptysis 1 Malignancy Low risk = 1 – 2. 5 points Moderate risk = 3 – 6 points High risk = 6. 5 – 12. 5
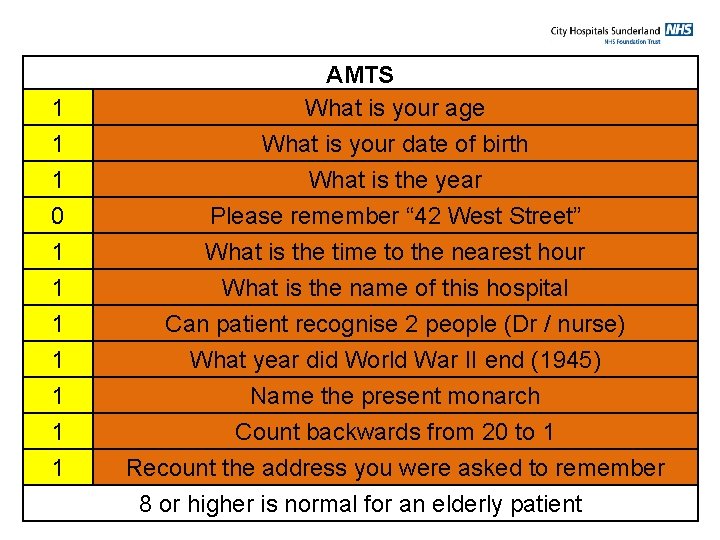
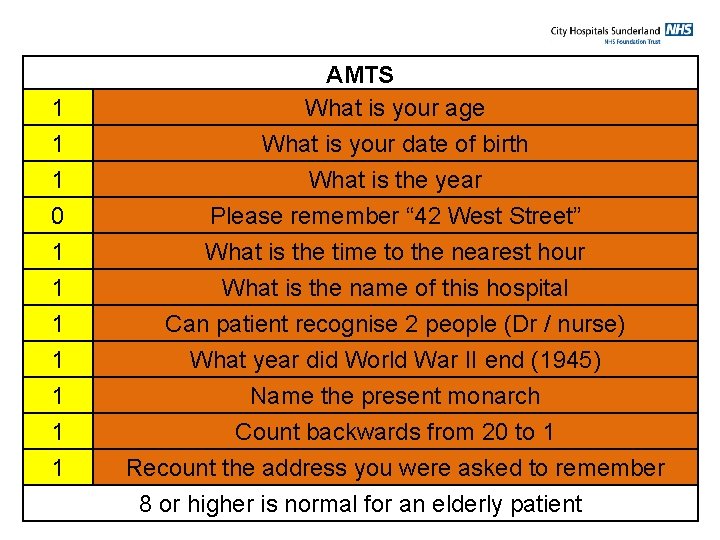
1 1 1 0 1 1 1 1 AMTS What is your age What is your date of birth What is the year Please remember “ 42 West Street” What is the time to the nearest hour What is the name of this hospital Can patient recognise 2 people (Dr / nurse) What year did World War II end (1945) Name the present monarch Count backwards from 20 to 1 Recount the address you were asked to remember 8 or higher is normal for an elderly patient
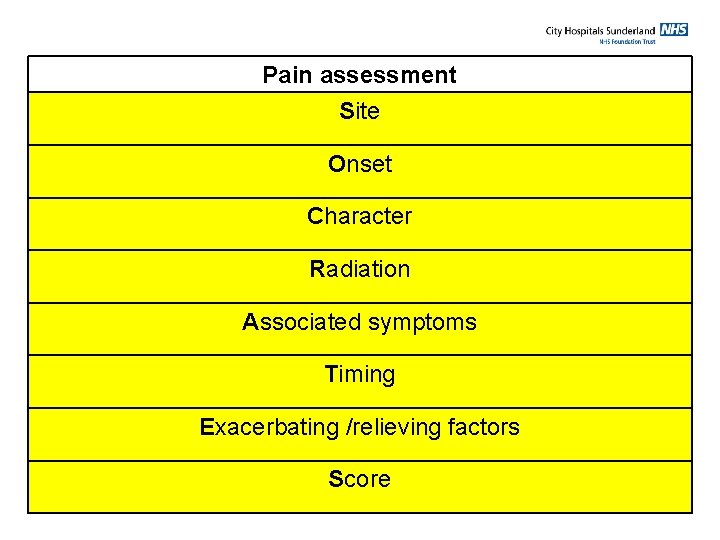
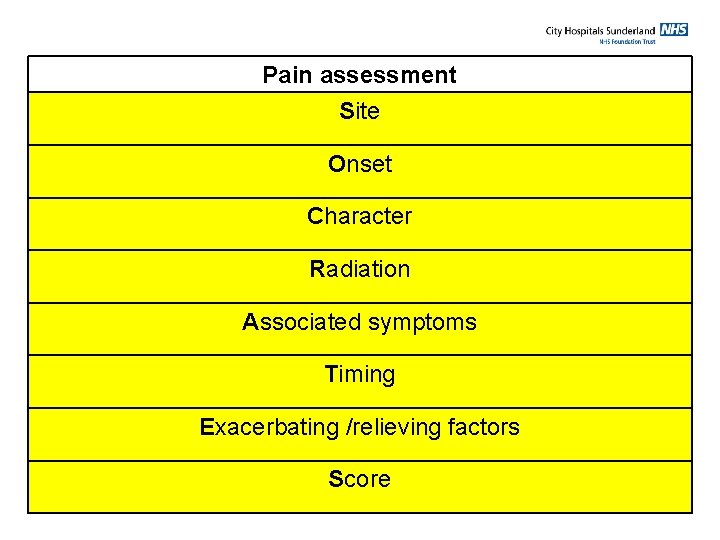
Pain assessment Site Onset Character Radiation Associated symptoms Timing Exacerbating /relieving factors Score
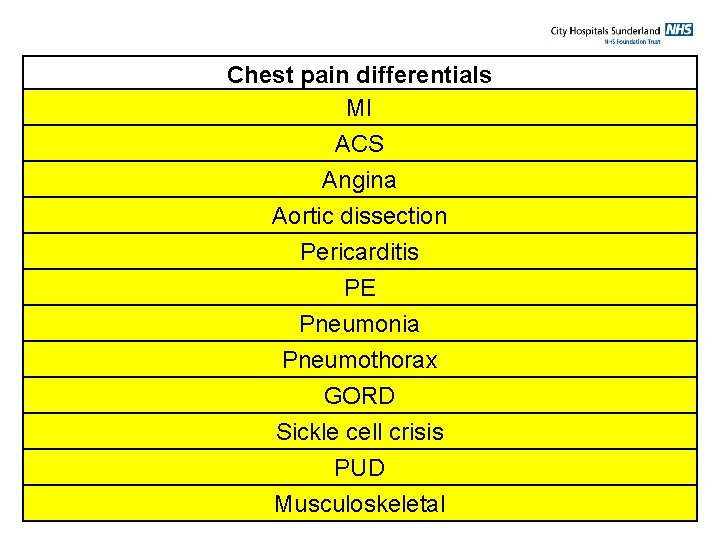
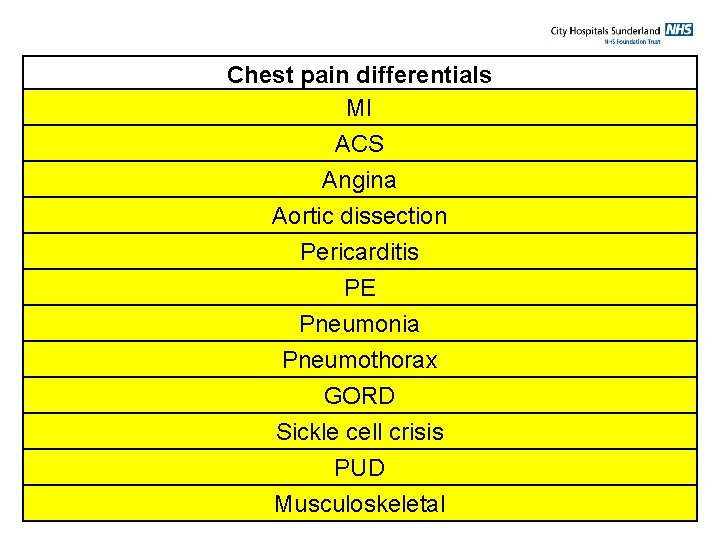
Chest pain differentials MI ACS Angina Aortic dissection Pericarditis PE Pneumonia Pneumothorax GORD Sickle cell crisis PUD Musculoskeletal
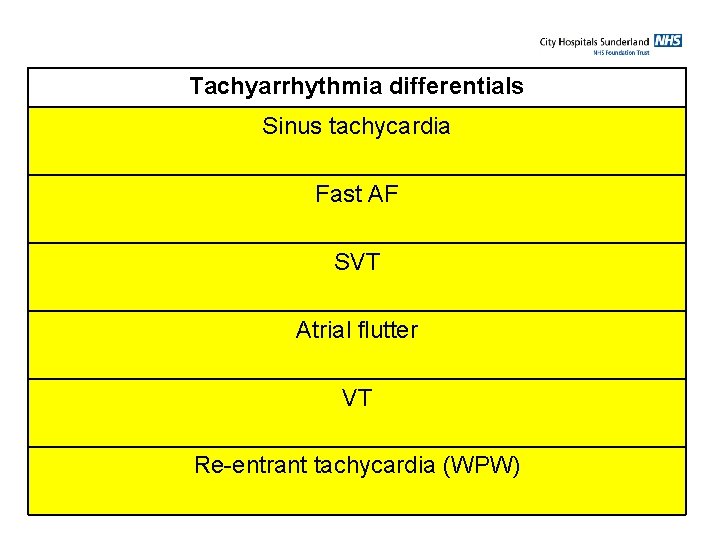
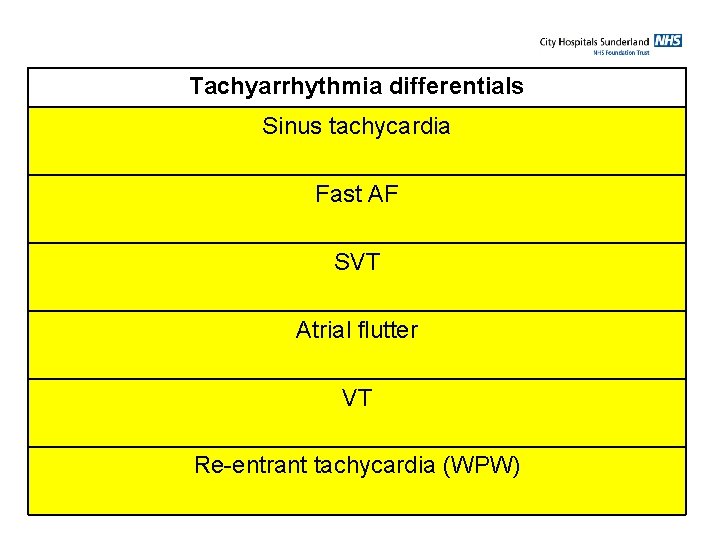
Tachyarrhythmia differentials Sinus tachycardia Fast AF SVT Atrial flutter VT Re-entrant tachycardia (WPW)
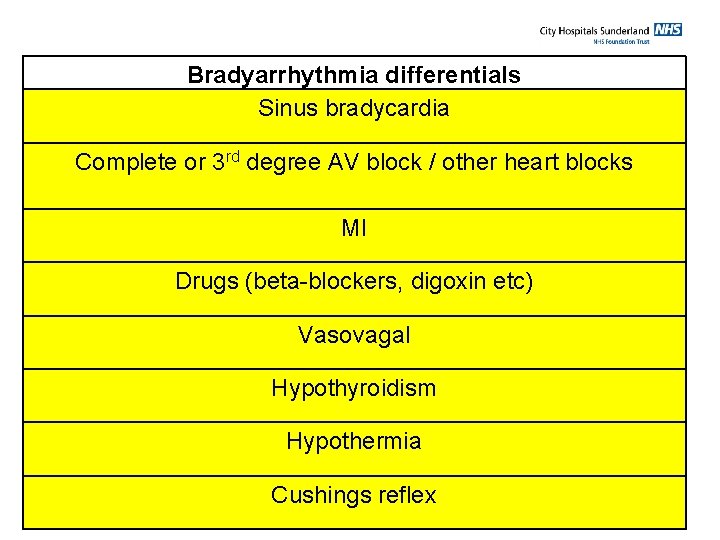
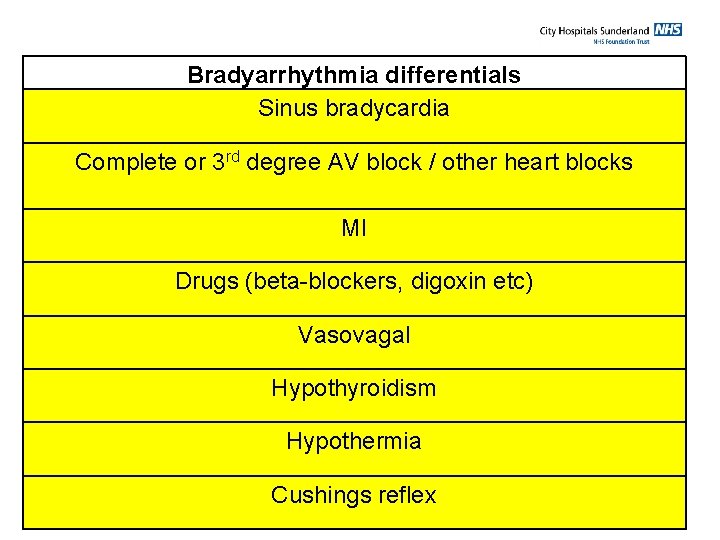
Bradyarrhythmia differentials Sinus bradycardia Complete or 3 rd degree AV block / other heart blocks MI Drugs (beta-blockers, digoxin etc) Vasovagal Hypothyroidism Hypothermia Cushings reflex
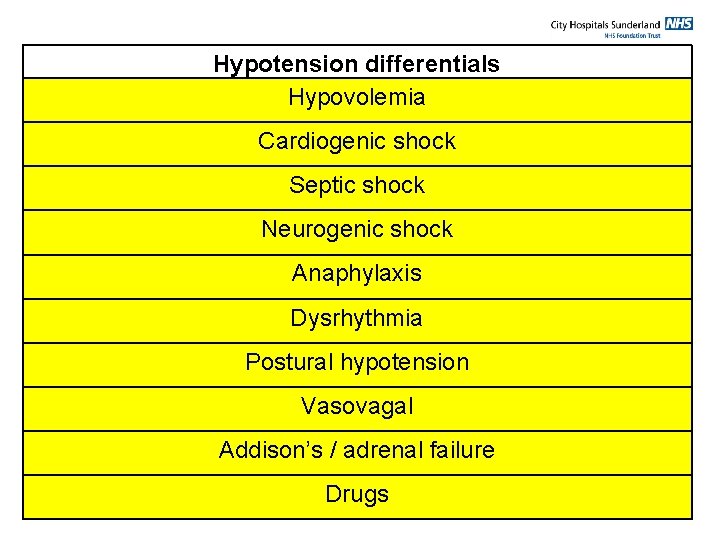
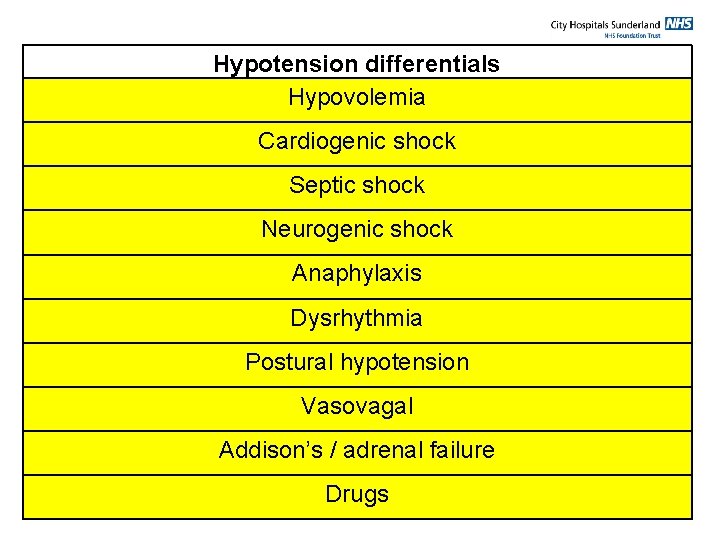
Hypotension differentials Hypovolemia Cardiogenic shock Septic shock Neurogenic shock Anaphylaxis Dysrhythmia Postural hypotension Vasovagal Addison’s / adrenal failure Drugs
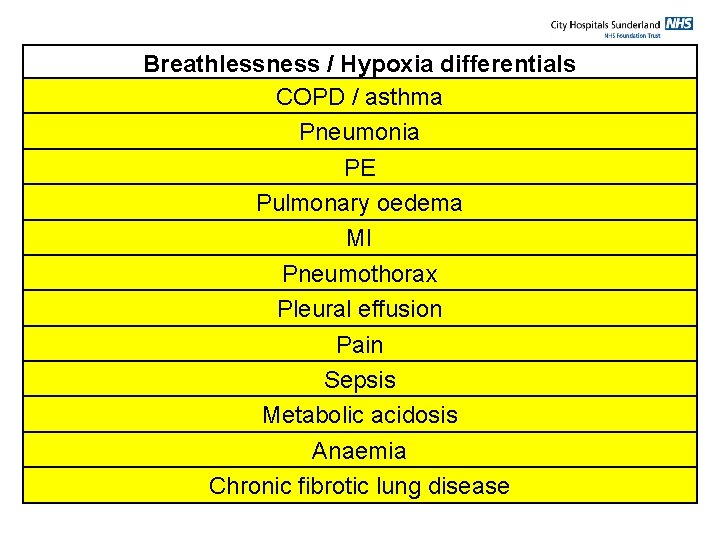
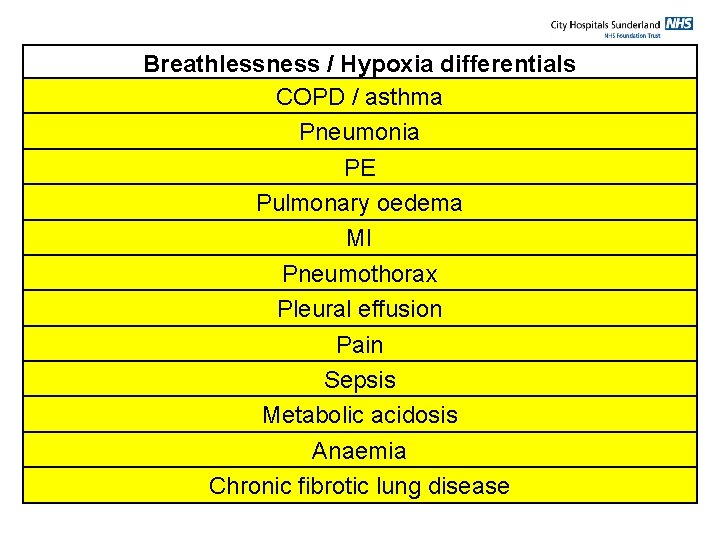
Breathlessness / Hypoxia differentials COPD / asthma Pneumonia PE Pulmonary oedema MI Pneumothorax Pleural effusion Pain Sepsis Metabolic acidosis Anaemia Chronic fibrotic lung disease
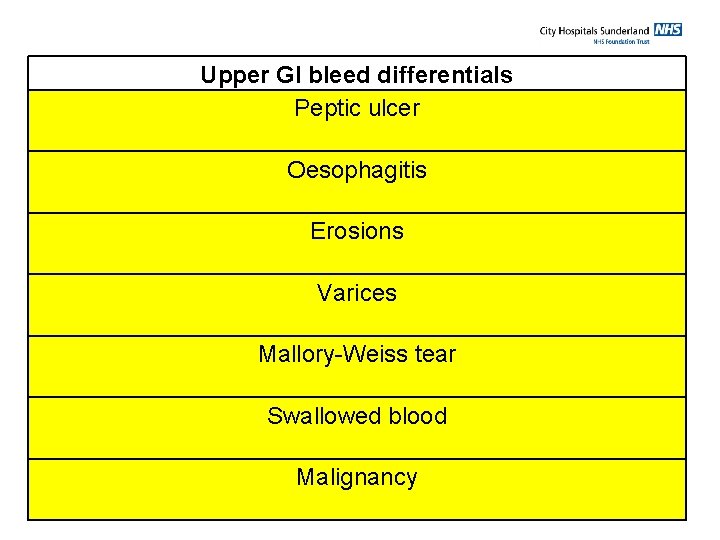
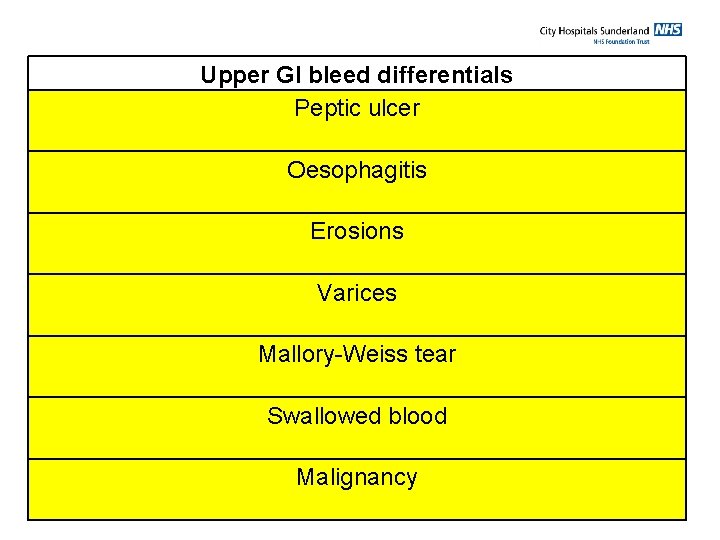
Upper GI bleed differentials Peptic ulcer Oesophagitis Erosions Varices Mallory-Weiss tear Swallowed blood Malignancy
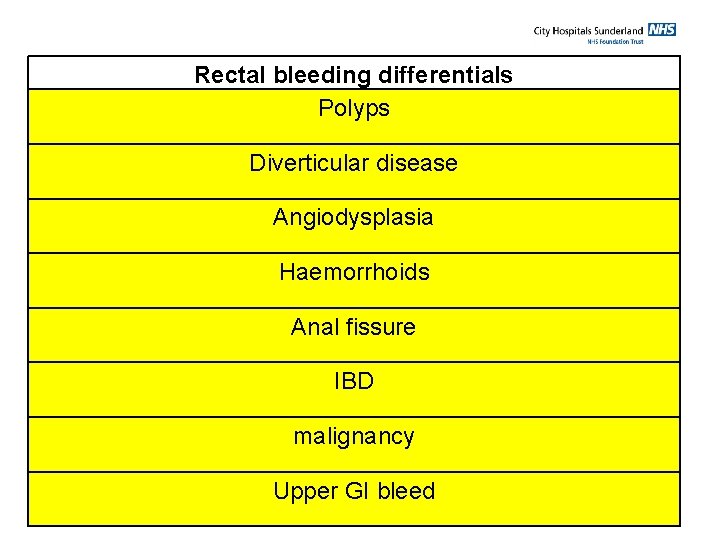
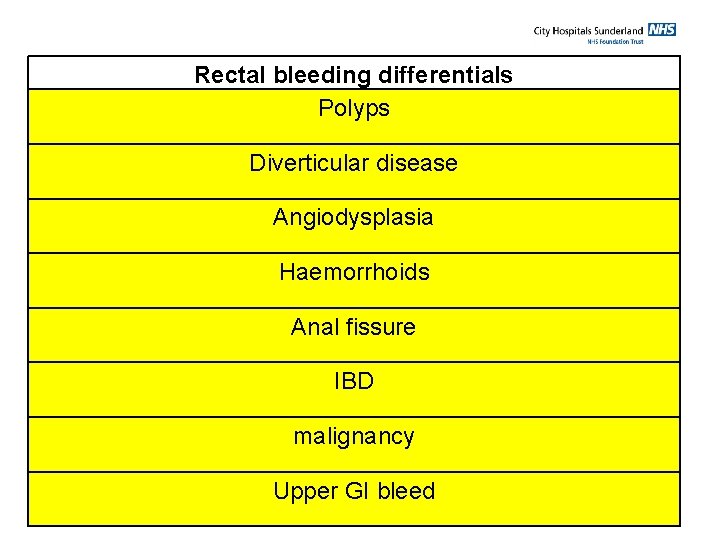
Rectal bleeding differentials Polyps Diverticular disease Angiodysplasia Haemorrhoids Anal fissure IBD malignancy Upper GI bleed
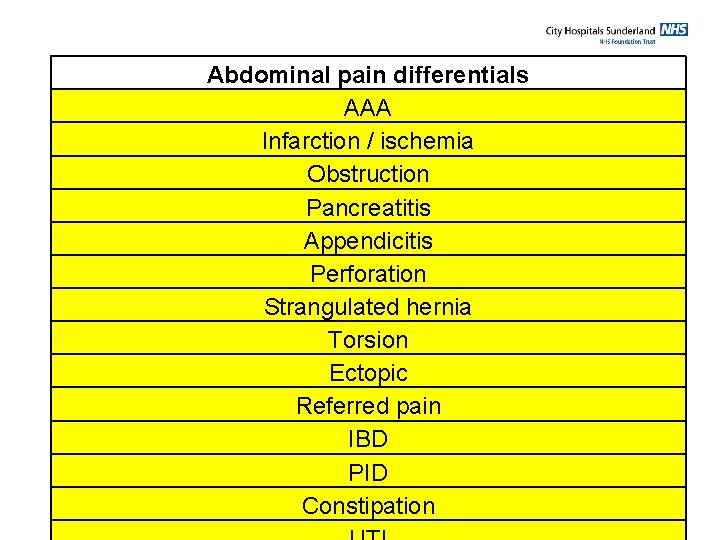
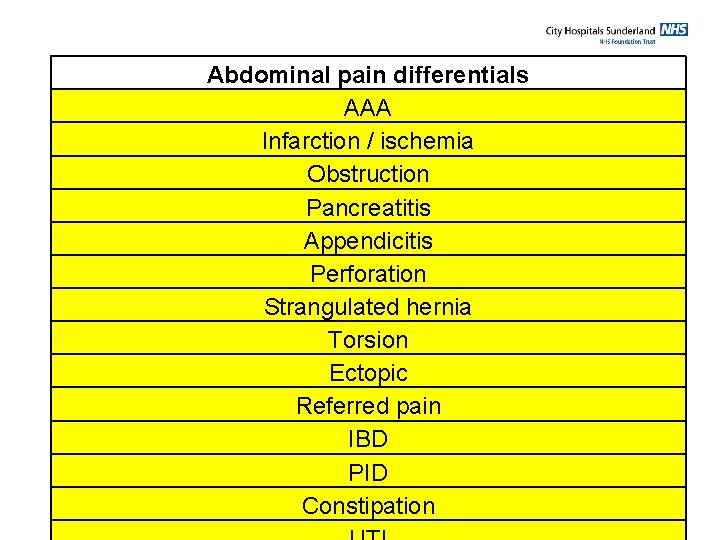
Abdominal pain differentials AAA Infarction / ischemia Obstruction Pancreatitis Appendicitis Perforation Strangulated hernia Torsion Ectopic Referred pain IBD PID Constipation
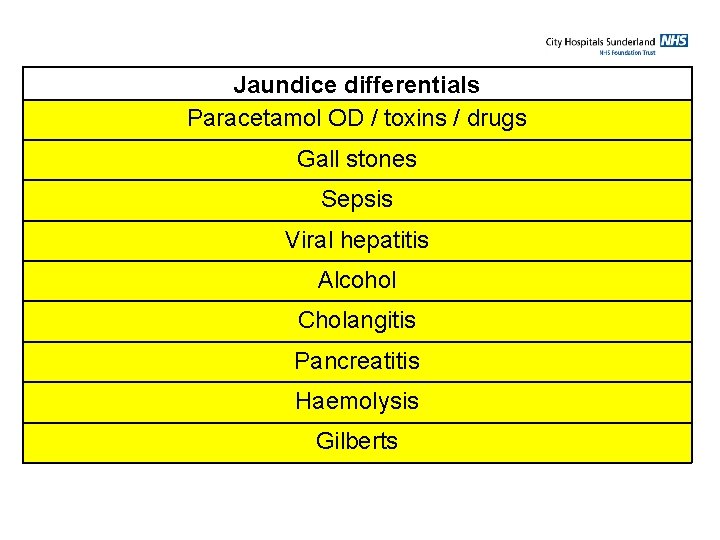
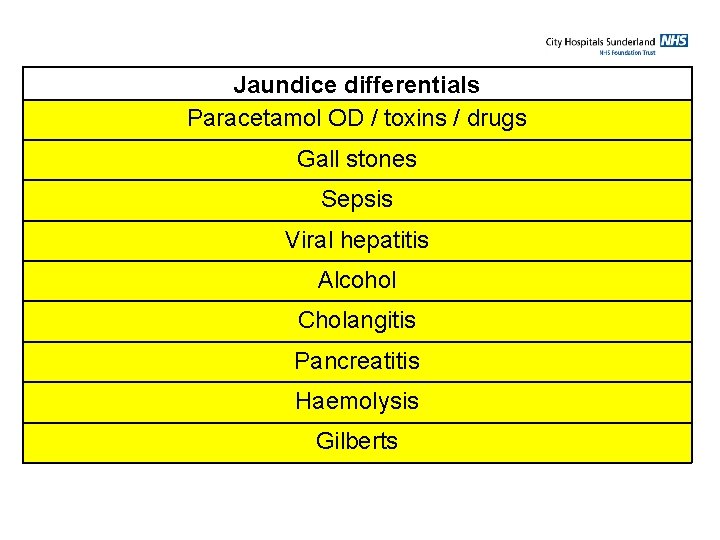
Jaundice differentials Paracetamol OD / toxins / drugs Gall stones Sepsis Viral hepatitis Alcohol Cholangitis Pancreatitis Haemolysis Gilberts
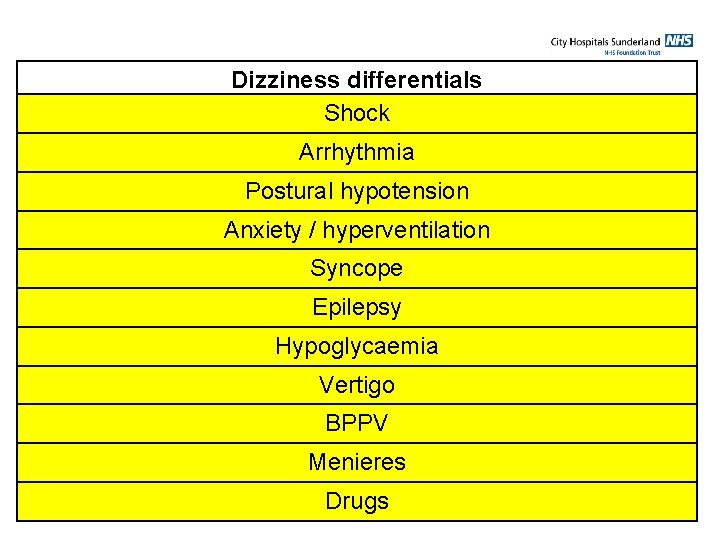
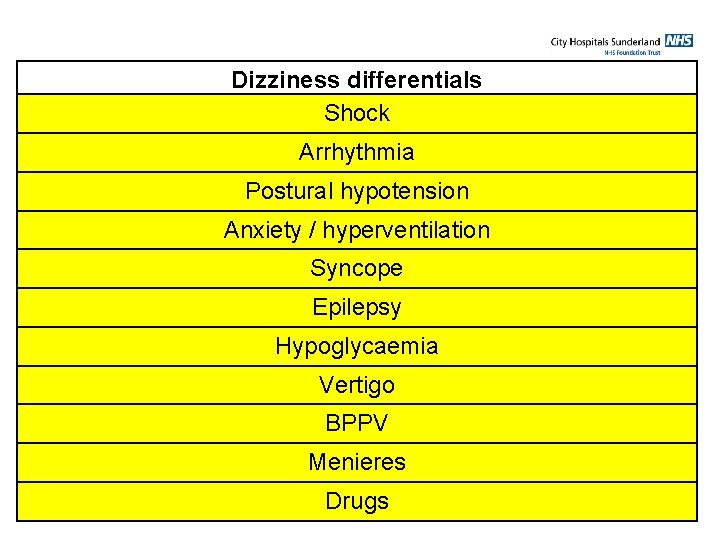
Dizziness differentials Shock Arrhythmia Postural hypotension Anxiety / hyperventilation Syncope Epilepsy Hypoglycaemia Vertigo BPPV Menieres Drugs
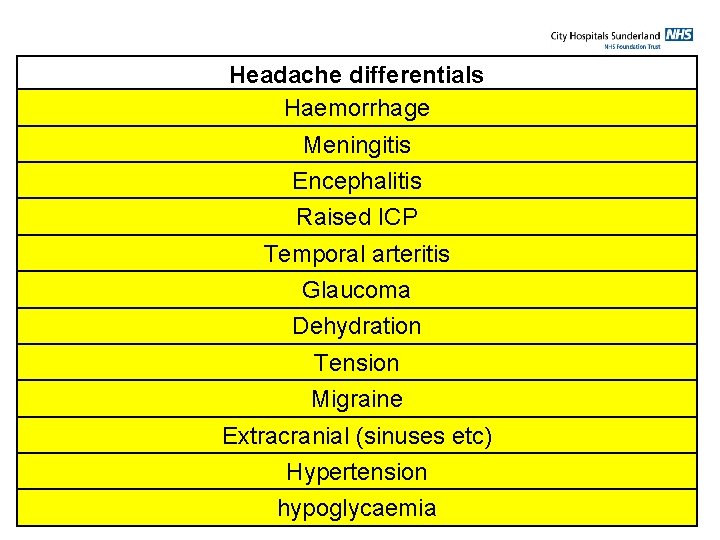
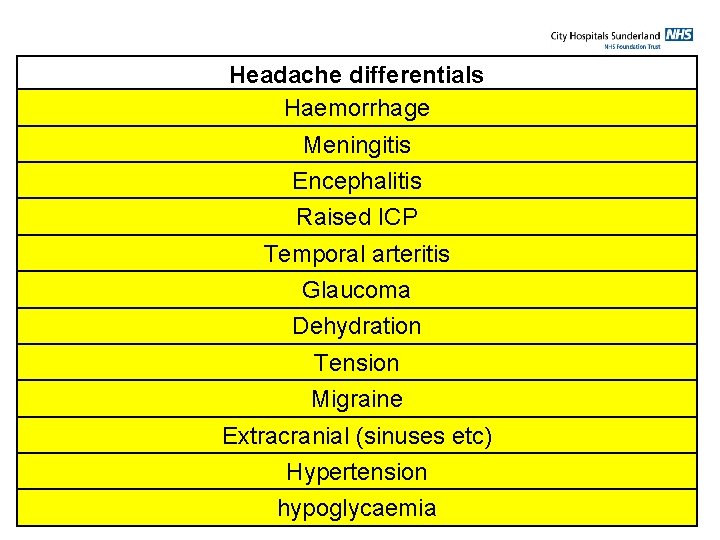
Headache differentials Haemorrhage Meningitis Encephalitis Raised ICP Temporal arteritis Glaucoma Dehydration Tension Migraine Extracranial (sinuses etc) Hypertension hypoglycaemia
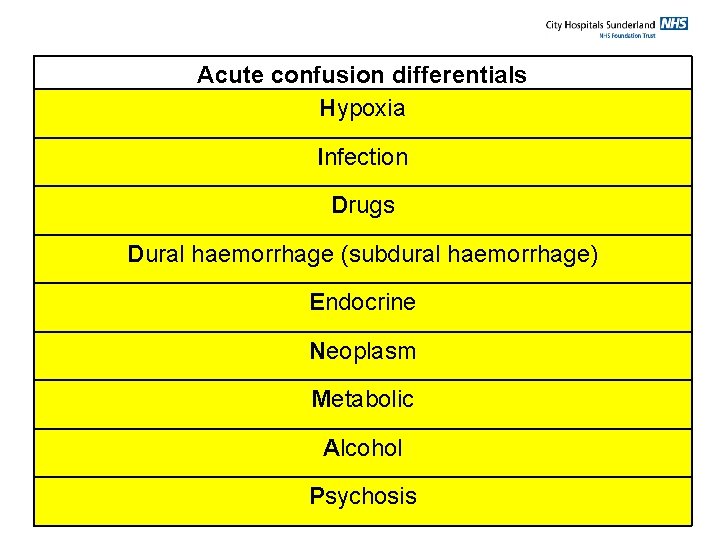
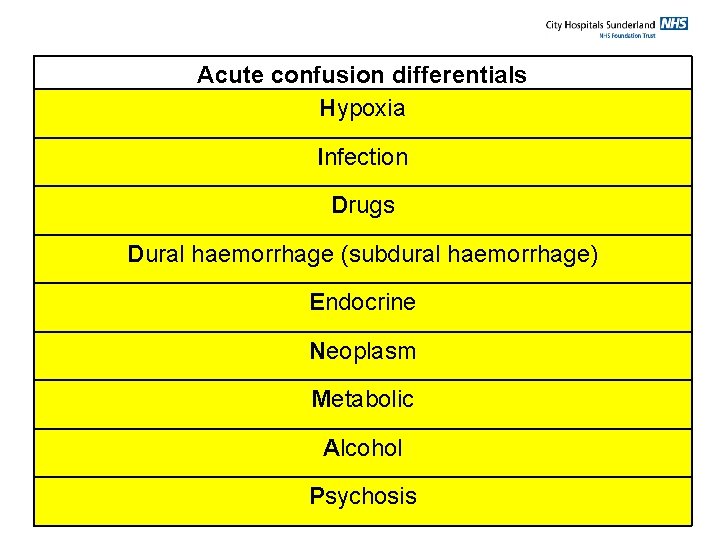
Acute confusion differentials Hypoxia Infection Drugs Dural haemorrhage (subdural haemorrhage) Endocrine Neoplasm Metabolic Alcohol Psychosis
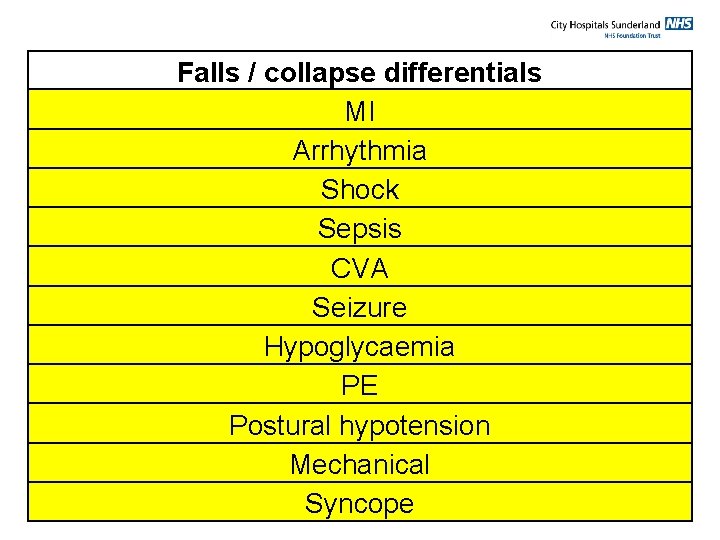
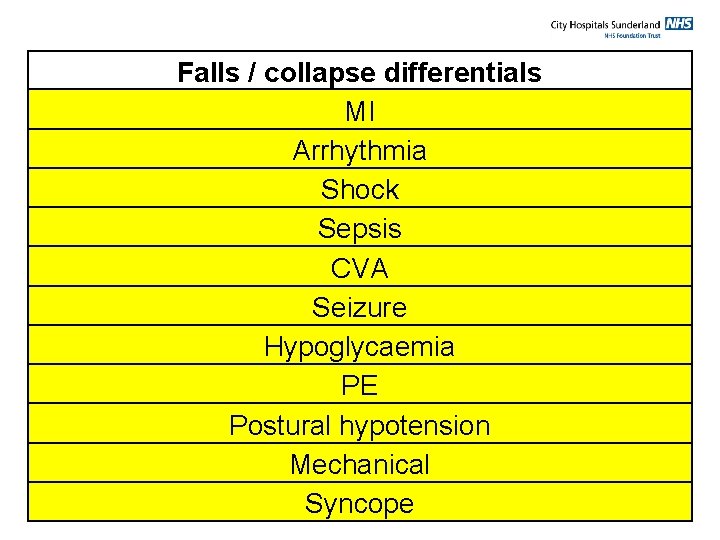
Falls / collapse differentials MI Arrhythmia Shock Sepsis CVA Seizure Hypoglycaemia PE Postural hypotension Mechanical Syncope
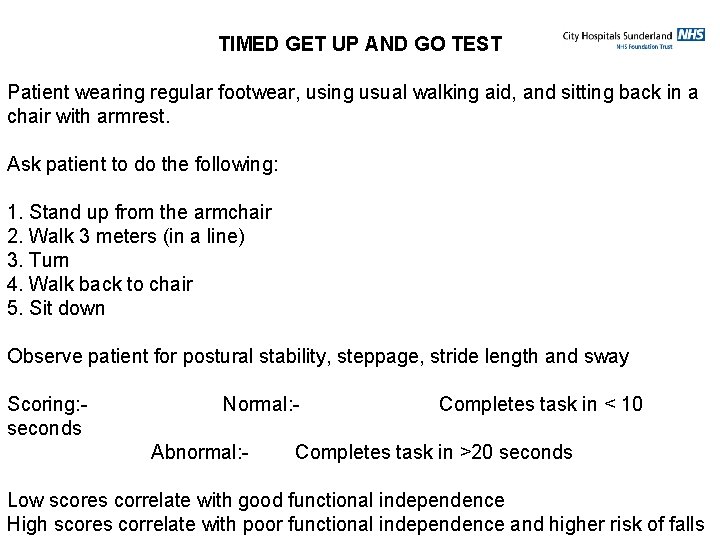
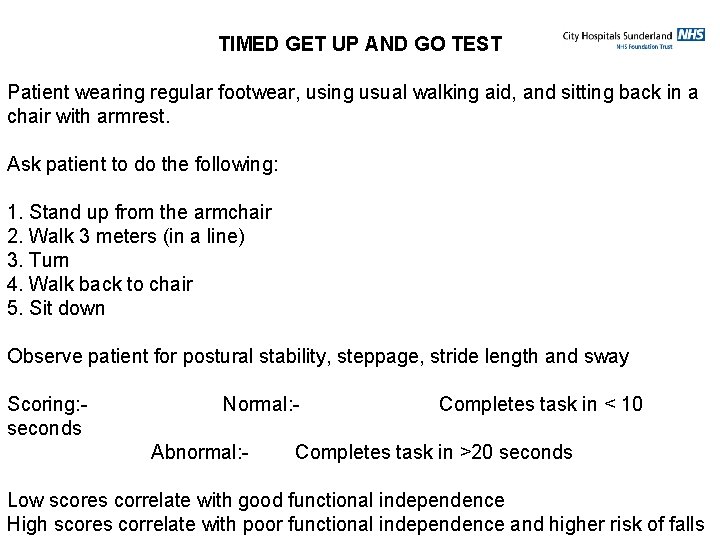
TIMED GET UP AND GO TEST Patient wearing regular footwear, using usual walking aid, and sitting back in a chair with armrest. Ask patient to do the following: 1. Stand up from the armchair 2. Walk 3 meters (in a line) 3. Turn 4. Walk back to chair 5. Sit down Observe patient for postural stability, steppage, stride length and sway Scoring: seconds Normal: Abnormal: - Completes task in < 10 Completes task in >20 seconds Low scores correlate with good functional independence High scores correlate with poor functional independence and higher risk of falls
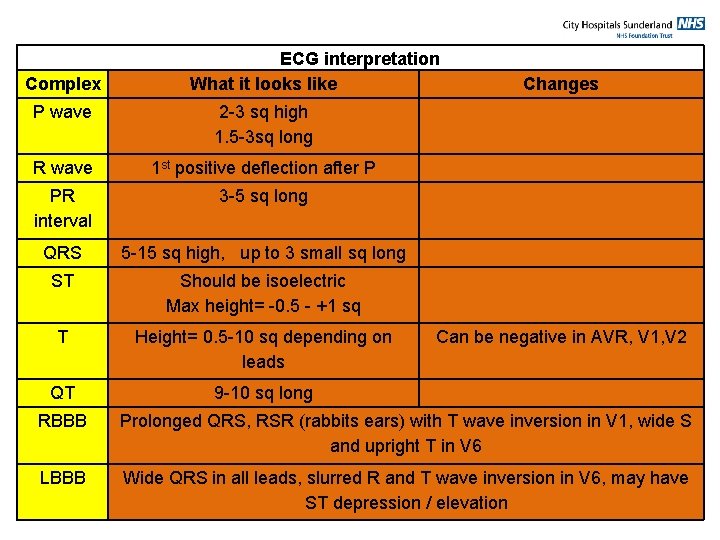
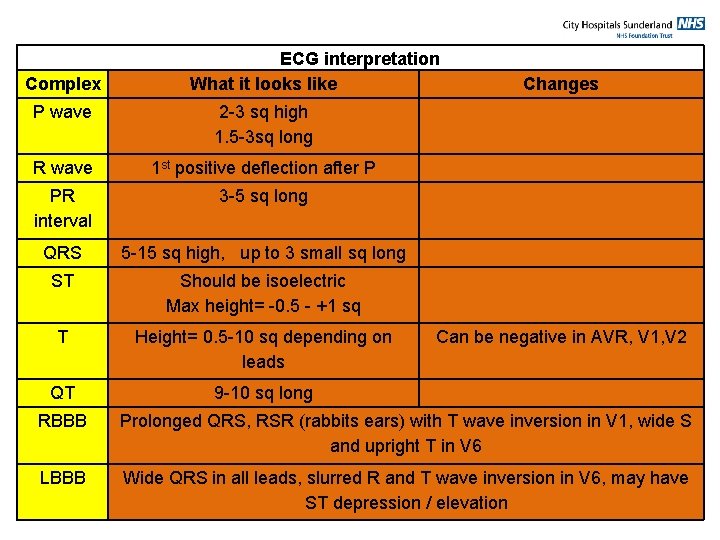
Complex ECG interpretation What it looks like P wave 2 -3 sq high 1. 5 -3 sq long R wave 1 st positive deflection after P PR interval 3 -5 sq long QRS 5 -15 sq high, up to 3 small sq long ST Should be isoelectric Max height= -0. 5 - +1 sq T Height= 0. 5 -10 sq depending on leads QT 9 -10 sq long Changes Can be negative in AVR, V 1, V 2 RBBB Prolonged QRS, RSR (rabbits ears) with T wave inversion in V 1, wide S and upright T in V 6 LBBB Wide QRS in all leads, slurred R and T wave inversion in V 6, may have ST depression / elevation
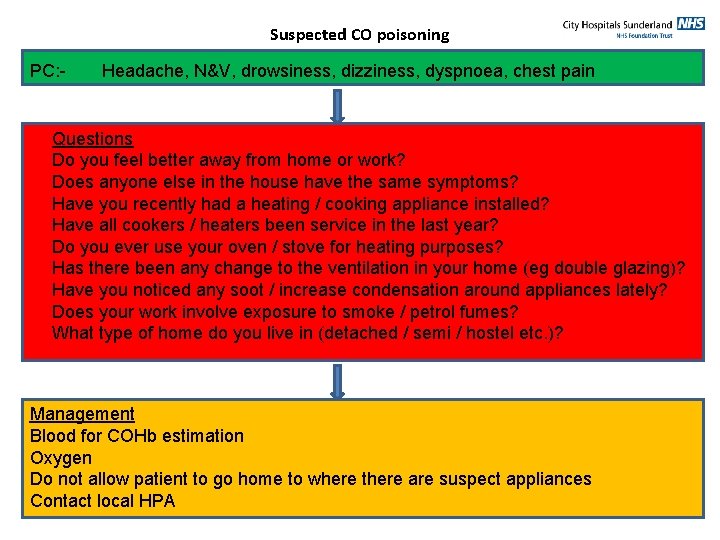
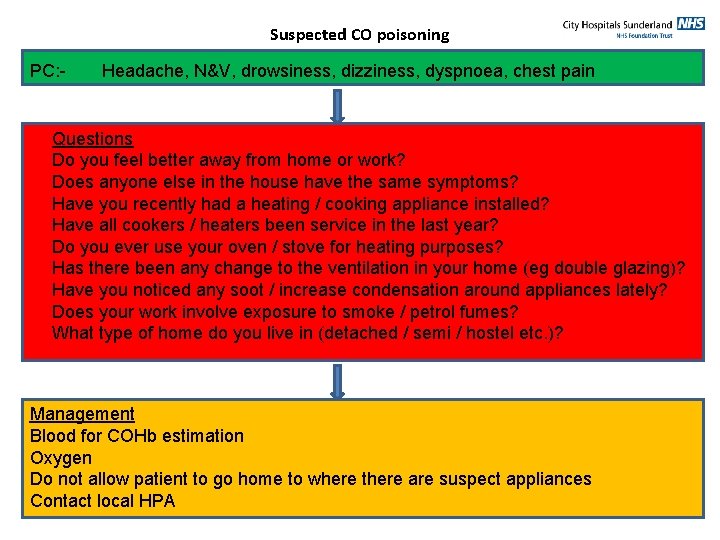
Suspected CO poisoning PC: - Headache, N&V, drowsiness, dizziness, dyspnoea, chest pain Questions Do you feel better away from home or work? Does anyone else in the house have the same symptoms? Have you recently had a heating / cooking appliance installed? Have all cookers / heaters been service in the last year? Do you ever use your oven / stove for heating purposes? Has there been any change to the ventilation in your home (eg double glazing)? Have you noticed any soot / increase condensation around appliances lately? Does your work involve exposure to smoke / petrol fumes? What type of home do you live in (detached / semi / hostel etc. )? Management Blood for COHb estimation Oxygen Do not allow patient to go home to where there are suspect appliances Contact local HPA
 Louisiana health standards
Louisiana health standards Pack it out pack it in
Pack it out pack it in Ospap exam
Ospap exam Mfl sunderland
Mfl sunderland Mfl sunderland
Mfl sunderland Alcohol delivery sunderland
Alcohol delivery sunderland Sunderland sunspace
Sunderland sunspace Sunderland mfl
Sunderland mfl Home hunt gentoo sunderland
Home hunt gentoo sunderland Sunderland mfl
Sunderland mfl Classificazione di sunderland
Classificazione di sunderland Cyps sunderland
Cyps sunderland Sunderland colors
Sunderland colors Product information file
Product information file Local information pack iras
Local information pack iras Difference between voluntary and mandatory
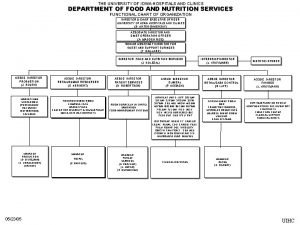
Difference between voluntary and mandatory University of iowa hospital and clinics departments
University of iowa hospital and clinics departments Qah
Qah Jci standards
Jci standards Afmsd mumbai
Afmsd mumbai Application of computer in hospital management
Application of computer in hospital management Dnv vs jcaho
Dnv vs jcaho Bcp for hospitals
Bcp for hospitals Anchorage va medical center
Anchorage va medical center Uhcw occupational health telephone number
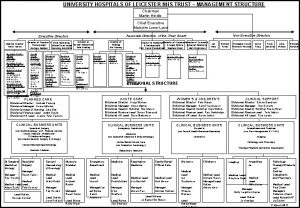
Uhcw occupational health telephone number Worcestershire acute hospitals nhs trust
Worcestershire acute hospitals nhs trust Write your strength and weakness
Write your strength and weakness Lean hospitals
Lean hospitals Lean hospitals mark graban
Lean hospitals mark graban Www.fhpl.net login employee/ecard
Www.fhpl.net login employee/ecard Erp for hospitals
Erp for hospitals Medisep hospitals in kerala
Medisep hospitals in kerala Dr sue carr
Dr sue carr Bed management in hospitals
Bed management in hospitals Clinical data repository
Clinical data repository Portsmouth hospitals nhs trust jobs
Portsmouth hospitals nhs trust jobs National accreditation board for hospitals
National accreditation board for hospitals Lokmanya orthopedic hospital pune
Lokmanya orthopedic hospital pune Inventory cycle time
Inventory cycle time Western sussex hospitals nhs foundation trust board
Western sussex hospitals nhs foundation trust board Pinpointing the enemy
Pinpointing the enemy 3-1 checking accounts worksheet answers
3-1 checking accounts worksheet answers Disadvantages of debit card
Disadvantages of debit card Ekurhuleni energy department
Ekurhuleni energy department San luis obispo planning department
San luis obispo planning department City of palm coast water department
City of palm coast water department Gabrielle langston
Gabrielle langston