DISEASES OF THE NERVOUS SYSTEM PART 2 Atlantoaxial

















- Slides: 53
DISEASES OF THE NERVOUS SYSTEM PART 2
Atlantoaxial Instability • Condition where there is abnormal movement in the neck (between atlas and axis) • Causes: Congenital, developmental abnormalities, trauma, or a combination of both • The atlantoaxial joint is normally stabilized by a projection off the axis called dens (this projection fits into the atlas) • Trauma occurs after forceful flexion of the head (causing a fracture of the dens or other parts of the axis) • Congenital occurs with small amount trauma (jumping off couch or being jumped on)

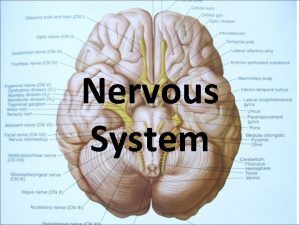
Atlantoaxial Joint Atlanto-Axial Joint
Atlantoaxial Instability Clinical signs: Toy and miniature breeds Reluctance to be patted on head Neck pain May have tetraparesis (weakness in all 4 limbs) or tetraplegia (paralysis in all 4 legs) Sudden death due to respiratory paralysis

Atlantoaxial Instability
Atlantoaxial instability Diagnosis Radiographs: lateral x-ray of neck in slight ventroflexion avoid further spinal cord damage with positioning Avoid anesthesia when taking radiographs. The decrease of muscle tone during anesthesia may result in future subluxation and spinal cord damage
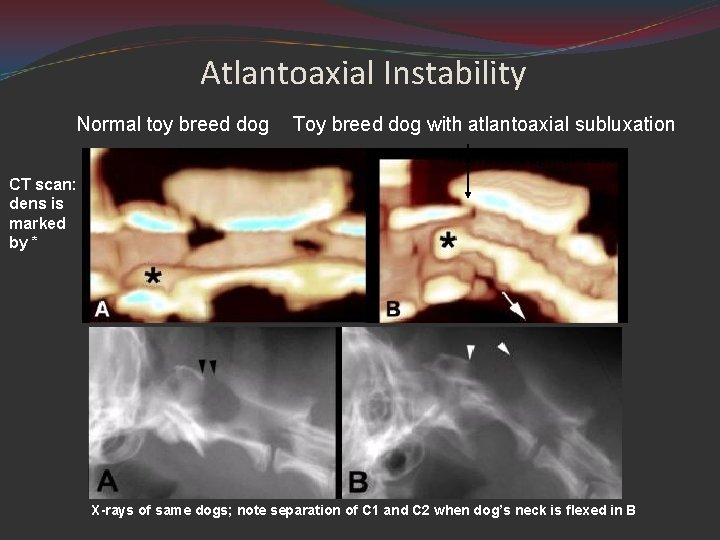
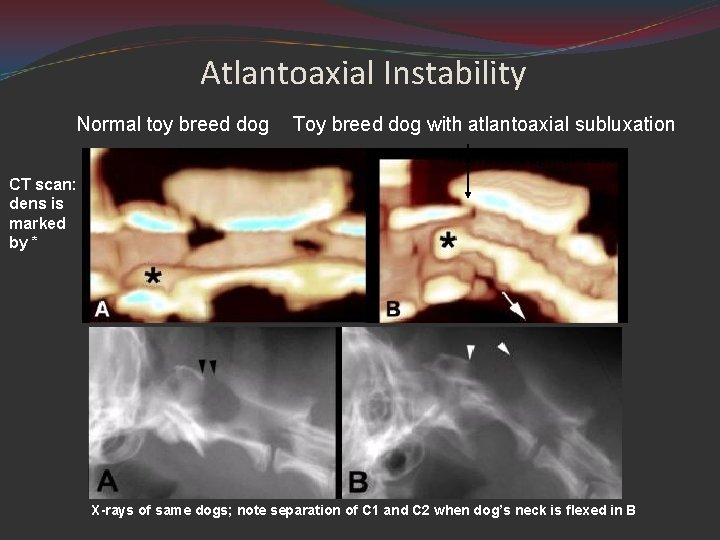
Atlantoaxial Instability Normal toy breed dog Toy breed dog with atlantoaxial subluxation Narrowed spinal canal CT scan: dens is marked by * X-rays of same dogs; note separation of C 1 and C 2 when dog’s neck is flexed in B
Atlantoaxial Instability (Subluxation) Treatment Medical splint neck in extension with cage confinement x 6 w treat like other spinal cord trauma Surgical (if unresponsive to medical Rx) stabilize/decompress attach dorsal process of axis to arch of atlas fuse atlas and axis joint with pins and bone graft hemilaminectomy to relieve spinal cord compression
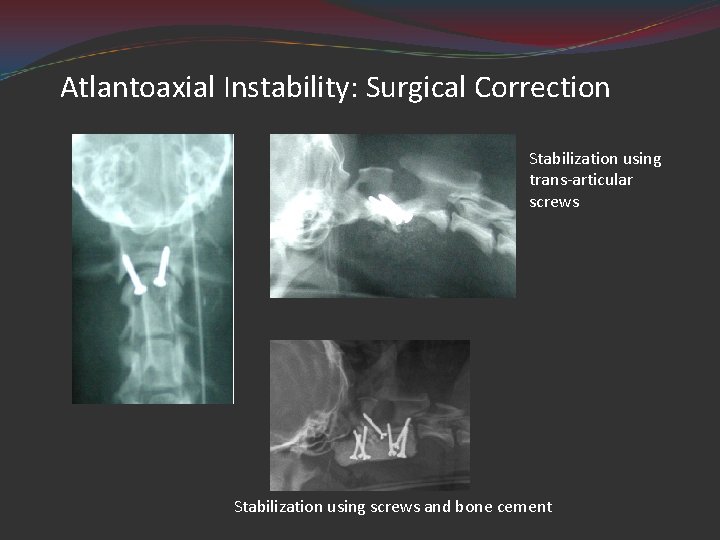
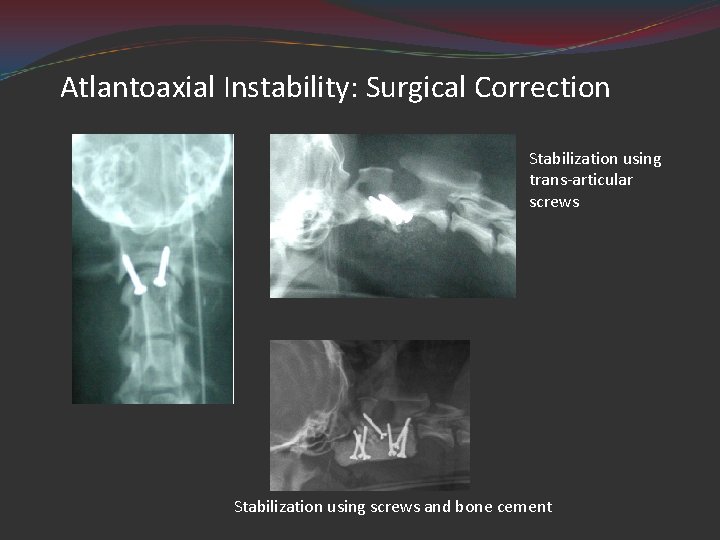
Atlantoaxial Instability: Surgical Correction Stabilization using trans-articular screws Stabilization using screws and bone cement

Atlantoaxial Instability Client info prognosis is fair to good for animals with mild signs animals should not be used for breeding; may be hereditary
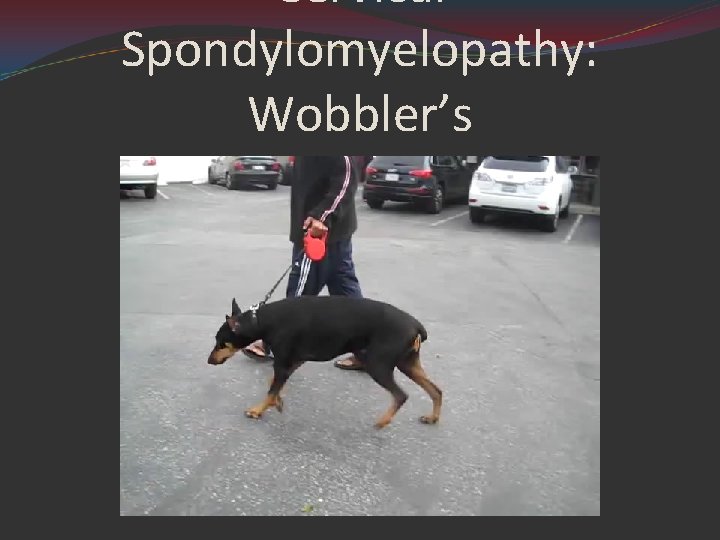
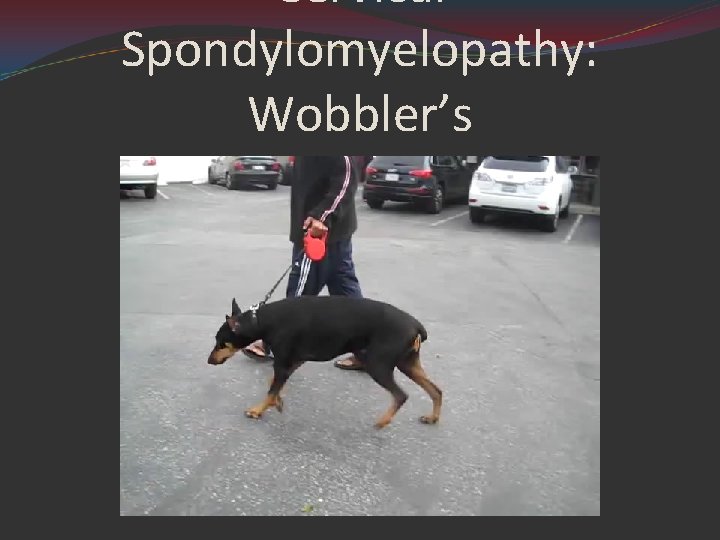
Cervical Spondylomyelopathy: Wobbler’s
Cervical Spondylomyelopathy: Wobbler’s Cervical spinal cord compression as a result of caudal vertebral malformation or misarticulation. Large breed dogs (Great Danes and Dobermans) The onset of C/S usually occur before 1 year of age in the Great Dane C/S occur after 2 years of age in the Doberman
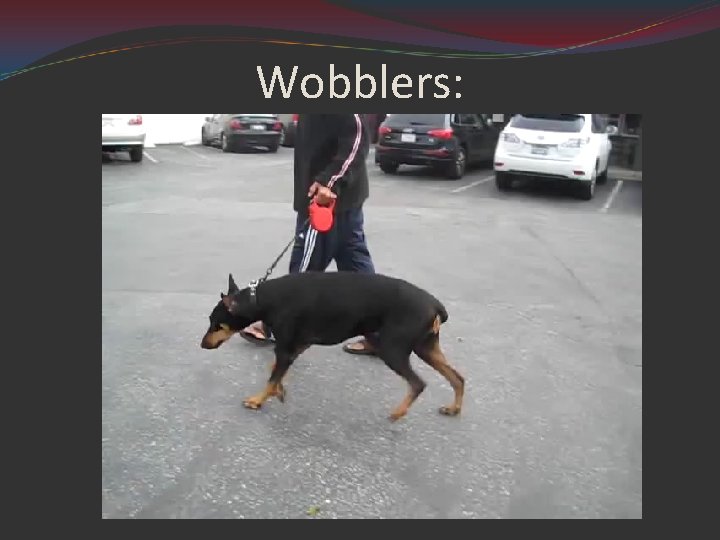
Clinical signs: Progressive hind-limb ataxia (wobbly gait) Pelvic limbs cross each other when walking Abduct widely/tend to collapse May drag toes (wears dorsal surface of nails) Impaired proprioception Signs may also be present in front limb Crouching stance with downward flexed neck Rigid flexion of neck; may have neck pain
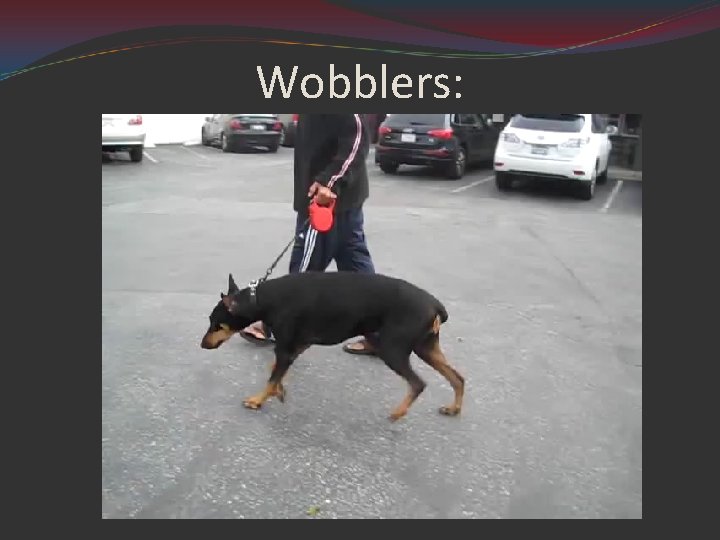
Wobblers:
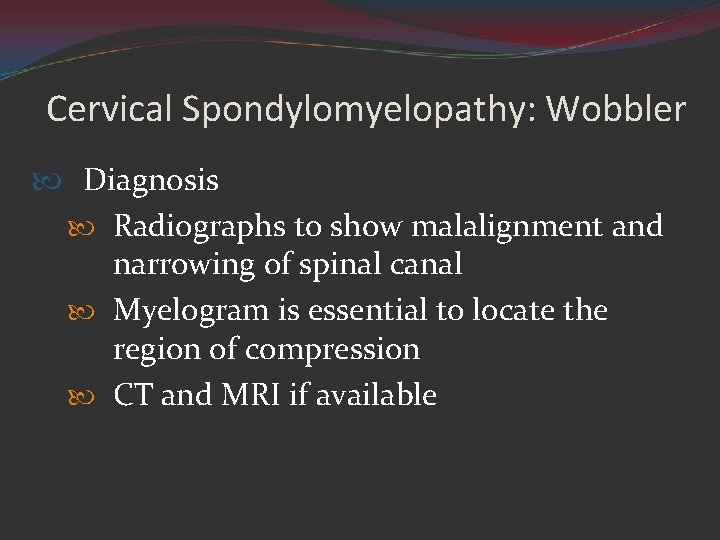
Cervical Spondylomyelopathy: Wobbler Diagnosis Radiographs to show malalignment and narrowing of spinal canal Myelogram is essential to locate the region of compression CT and MRI if available
Cervical Spondylomyelopathy: Wobblers Treatment: Medical Corticosteroids Neck brace Cage confinement Without treatment, prognosis is poor
Cervical Spondylomyelopathy: Wobbler Surgical Decompression of spinal cord by laminectomy Stabilize vertebral column screws and wire dorsally spinal fusion ventrally
Cervical Spondylomyelopathy: Wobbler Client info Prognosis is guarded Most likely a hereditary disease Multiple levels of compression less favorable prognosis than a single area of compression Surgery is risky and costly
Catch those Zzzzzzzs……. “Keep the dream alive. HIT THE SNOOZE BUTTON!”

Degenerative Myelopathy

Degenerative Myelopathy Progressive disease of the canine spinal cord Also known as: Chronic radiculomyelopathy (CDRM) Lesion consist of a diffuse degeneration of the white matter in both the ascending and descending tracts of all segments of the spinal cord Etiology: unclear May be autoimmune response to antigen in nervous system Degeneration of white matter in ascending and descending tracts
Clinical signs: Mainly in German Shep and Shep mixes (>5 yr) Progressive ataxia and paresis of hind limbs Loss of proprioception is first sign Dog “falls down” when trying to defecate Muscle wasting of back muscles along caudal thoracic and lumbosacral areas Symptoms progress until animal is unable to support weight on hind limbs

Degenerative Myelopathy

Degenerative Myelopathy Diagnosis Neurologic Exam ↓ proprioception N-↑ patellar reflexes Lack of pain Normal sphincter tone; normal panniculus (pin prick) reflex Radiographs usually normal Treatment: none - symptoms will progress to paralysis

Degenerative Myelopathy

Degenerative Myelopathy Client info Degenerative myelopathy is a progressive, incurable disease Although symptoms are similar at early stages, it is a different disease from hip dysplasia When dog cannot support weight, quality of life should be evaluated
Deafness damage to auditory pathway chronic otitis rupture of tympanic membrane damage to middle ear (ossicles) damage to auditory nerve hereditary or congenital bull terriers, Dobes, Rotts, Pointers, blueeyed white cats, Dalmations, Aust Heelers, Aust shepherds, Eng setters, Catahoula
Deafness continued: related to drug therapy aminoglycosides (gentamicin, streptomycin, kanamycin) topical polymyxin B Chloramphenicol Chlorhexidine w/ centrimide normal old age: usually due to atrophy of nerve ganglia or cochlear hair cells
Deafness Diagnosis Inability to rouse sleeping animal with loud noise (e, g, . blast from air horn) is diagnostic Treatment: No treatment is available in most cases Hearing aids are available for animals, but most will not tolerate something in ear canal
Client info Hearing loss is permanent If hereditary, do not breed Animals can be taught to hand signals rather than words Animals should not be off leash when outside Hearing aids are available for dogs but are usually not tolerated; would only be appropriate for hearing impaired

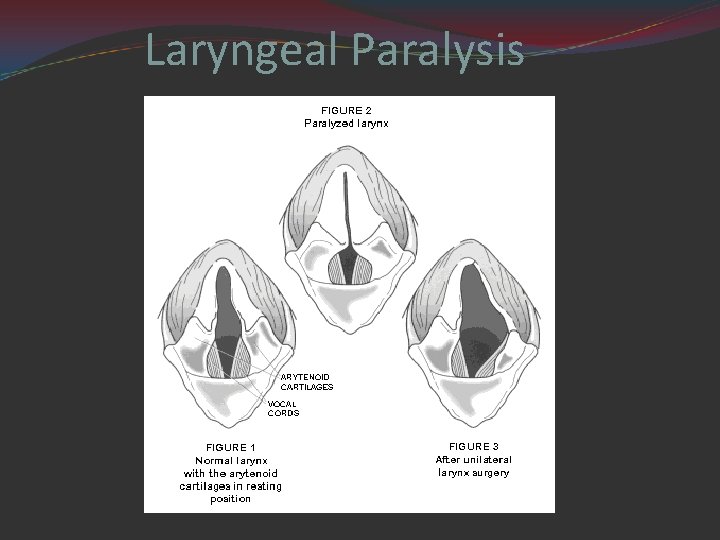
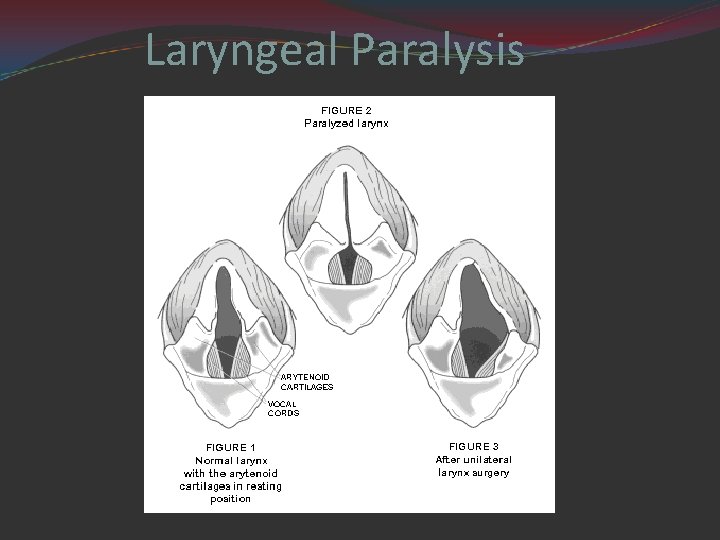
Laryngeal Paralysis Disorder in which the nerves that control the muscles and cartilage that open and close the larynx do not function properly. Air moves from the mouth or nose through the larynx into the trachea. Normally, the laryngeal cartilages(arytenoid cartilage) are pulled open when breathing. With Laryngeal paralysis, these cartilages do not open and close properly.
Laryngeal Paralysis
Three types: Hereditary: seen in Bouvier des Flandres and Siberian Huskies Seen at 4 -6 mo of age Acquired: can occur from lead poisoning, rabies, trauma, inflammation of vagus nerve 1. 5 to 13 yr of age Idiopathic: seen in middle-age to old large- and giant -breed dogs; castrated dogs and cats have a higher incidence than female and non-neutered males

Hereditary: Less common Signs of difficulty breathing usually starts at 4 -6 months old Affected puppies may have difficulty swallowing/breathing, they may gag, and bark may sound abnormal Acquired: Results from damage to the nerves and/or muscles of the larynx due to bite wound or other trauma

Idiopathic: Usually, the larynx is normal at birth, but over time, the nerves and muscles that control the laryngeal cartilages lose function The cause is unknown and the dogs affected are usually around middle aged large breeds
Laryngeal Paralysis Clinical Signs: Inspiratory stridor Resp distress Voice change Dyspnea/cyanosis/complete resp collapse
Laryngeal Paralysis Diagnosis: laryngoscopy will show laryngeal abductor dysfunction Treatment: surgical intervention including: Arytenoidectomy Removal of vocal folds Arytenoid lateralization Client info: prognosis is guarded to good; do not breed if hereditary

Arytenoid lateralization Most common type of surgery Sometimes referred to as “laryngeal tie-back” Involves putting one or more permanent sutures in place to hold the arytenoid cartilage open so that adequate air can pass through Most dogs do well (risk of bleeding during surgery, aspiration of stomach contents, or aspiration of food and water after surgery) Usually only done on one side

Laryngeal tie back https: //www. youtube. com/watch? v=6 it. Voyv N 2 q 4
Coonhound Paralysis
Coonhound Paralysis (Polyradiculoneuritis ) Thought to be an immune response to an unknown etiologic factor in raccoon saliva some dogs will get it 1 -2 wk after exposure, others exposed to same raccoon will not Signs: similar to tick paralysis and rabies Weakness begins in hind limbs with paralysis progressing rapidly to tetraplegia Alert, a febrile animal Loss of spinal reflexes (patella tap, etc) Loss of voice; labored breathing; inability to lift head May die of respiratory failure May last for 2 -3 mo (usually good Px)

Coonhound Paralysis video
Diagnosis: Clinical signs History of raccoon exposure or history of some antigenic stimulation All metabolic or infectious causes ruled out Treatment: Supportive nursing care Corticosteroids and anti-inflammatory doses have been used Support respirations, if necessary
Client info Dogs can be affected without exposure to raccoon May require long-term nursing care Some animals will regain total function, while more severely affected animals may not

Tick Paralysis
Tick Paralysis Cause: female tick (Dermacenter variablis, D. andersoni) → salivary neurotoxin Neurotoxin interfered with Ach at neuromuscular jct Not seen in cats; humans are affected Clinical signs Gradual onset of voice changes and hind-limb ataxia (motor deficit) progressing to a flaccid, ascending paralysis (1 -3 d) Sensation is intact Ticks on the dog
Diagnosis: Rule out other causes of neuromuscular disease Treatment Remove ticks (manually or with dip) Usually resolves in 1 -3 d Supportive care until dog recovers Ventilation required for resp paralysis

Tick Paralysis video https: //www. youtube. com/watch? v=w 8_k. Vli air. Q
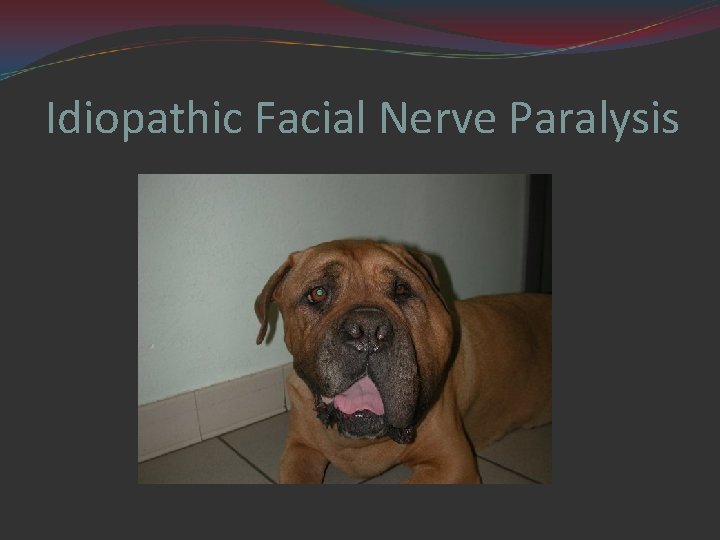
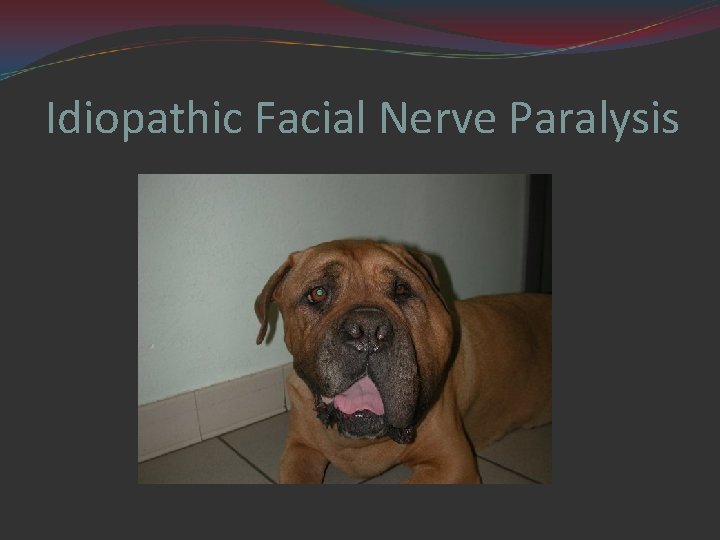
Idiopathic Facial Nerve Paralysis
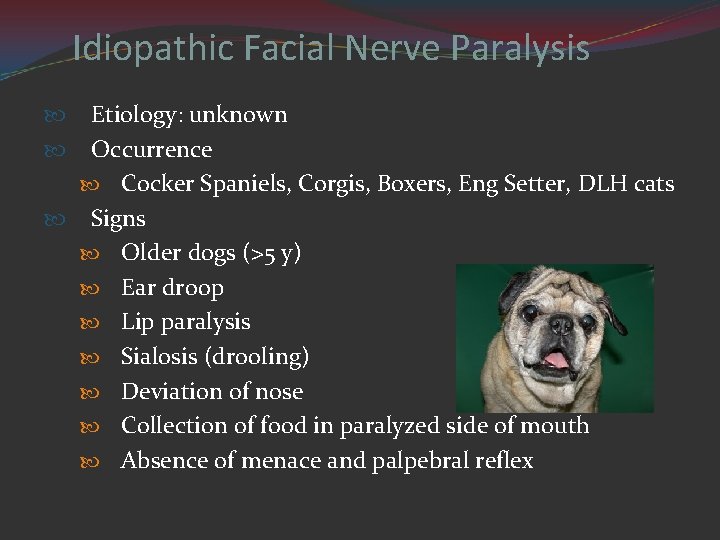
Idiopathic Facial Nerve Paralysis Etiology: unknown Occurrence Cocker Spaniels, Corgis, Boxers, Eng Setter, DLH cats Signs Older dogs (>5 y) Ear droop Lip paralysis Sialosis (drooling) Deviation of nose Collection of food in paralyzed side of mouth Absence of menace and palpebral reflex
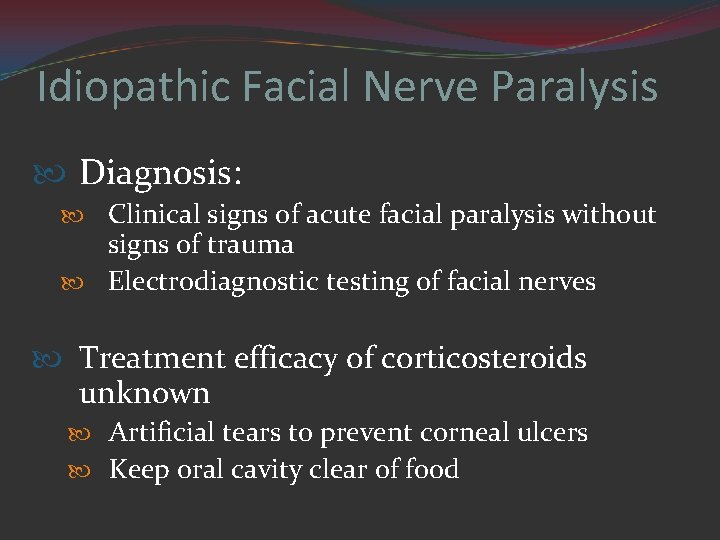
Idiopathic Facial Nerve Paralysis Diagnosis: Clinical signs of acute facial paralysis without signs of trauma Electrodiagnostic testing of facial nerves Treatment efficacy of corticosteroids unknown Artificial tears to prevent corneal ulcers Keep oral cavity clear of food
Client info Cause is unknown Complete recovery does not usually occur May develop keratoconjunctivitis sicca (dry eye) Animals may require life-long maintenance
 Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Atlantoaxial joint
Atlantoaxial joint Atlantoaxial osteoarthritis
Atlantoaxial osteoarthritis Atlantoaxial rotatory subluxation
Atlantoaxial rotatory subluxation Identify each type of neuronal pool
Identify each type of neuronal pool Fundamentals of the nervous system and nervous tissue
Fundamentals of the nervous system and nervous tissue What are neuron processes
What are neuron processes What does this graph show
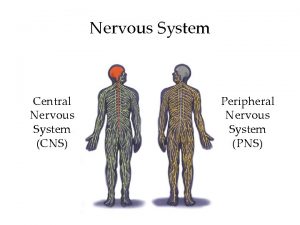
What does this graph show Diagram central nervous system
Diagram central nervous system Nervous system and digestive system
Nervous system and digestive system Endocrine system vs nervous system
Endocrine system vs nervous system Endo crine gland
Endo crine gland Adh function
Adh function Chapter 6 musculoskeletal system
Chapter 6 musculoskeletal system Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 10 lymphatic system diseases and disorders
Chapter 10 lymphatic system diseases and disorders Chapter 8 cardiovascular system
Chapter 8 cardiovascular system Capnia medical term
Capnia medical term Diseases of the musculoskeletal system
Diseases of the musculoskeletal system Female reproductive system diseases
Female reproductive system diseases Chemical messengers of the nervous system
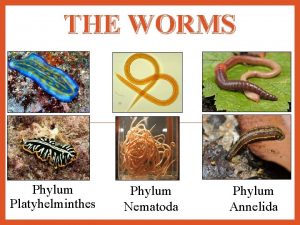
Chemical messengers of the nervous system Flat worms asexual reproduction
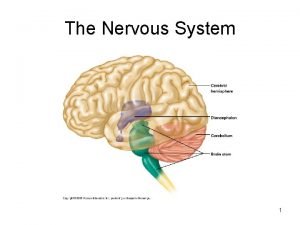
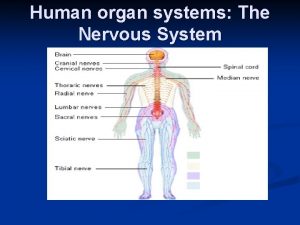
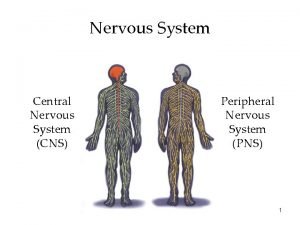
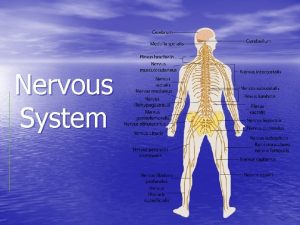
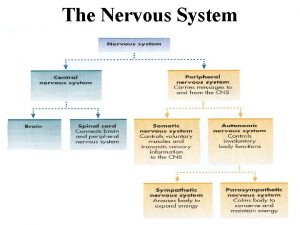
Flat worms asexual reproduction The nervous system is made up of
The nervous system is made up of Neuron anatomy
Neuron anatomy Nervous system learning objectives
Nervous system learning objectives Chapter 7 the nervous system
Chapter 7 the nervous system Stimulus in nervous system
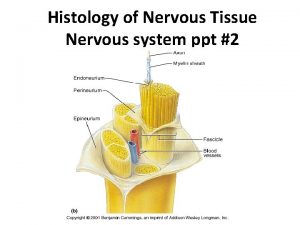
Stimulus in nervous system Neuron bundle
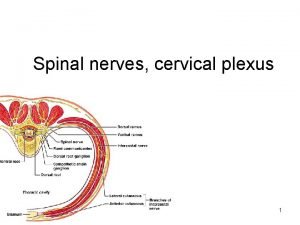
Neuron bundle Craniosacral region
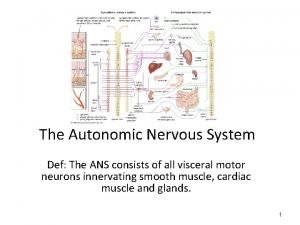
Craniosacral region Sympathetic nervous system def
Sympathetic nervous system def Peripheral nerves
Peripheral nerves Sns somatic nervous system
Sns somatic nervous system Brain scienstructable
Brain scienstructable Autonomic nervous system skeletal muscle
Autonomic nervous system skeletal muscle Roundworms nervous system
Roundworms nervous system Meristomata
Meristomata Nervous system of arthropods
Nervous system of arthropods Nervous system of arthropods
Nervous system of arthropods Division of nervous system
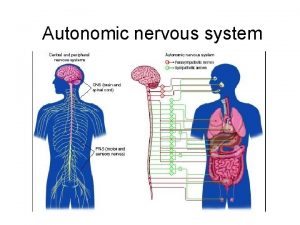
Division of nervous system Ans
Ans Nervous system of coelenterates
Nervous system of coelenterates Autonomic nervous system consists of
Autonomic nervous system consists of Module 10 the nervous and endocrine systems
Module 10 the nervous and endocrine systems Section 35-1 human body systems answer key
Section 35-1 human body systems answer key Autonomic nervous system pathway
Autonomic nervous system pathway Brain layer
Brain layer Basic unit of nervous system
Basic unit of nervous system Positive feedback loop in pregnancy
Positive feedback loop in pregnancy Ppt
Ppt Koosha golmohammadi
Koosha golmohammadi Comparison of endocrine and nervous system
Comparison of endocrine and nervous system 8 divisions of the nervous system
8 divisions of the nervous system How to take care of your nervous system
How to take care of your nervous system Effector cells nervous system
Effector cells nervous system