DIPHTHERIA Dr Navya N Department of Community Medicine
- Slides: 27
DIPHTHERIA Dr Navya N Department of Community Medicine Yenepoya Medical College
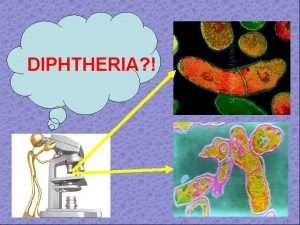
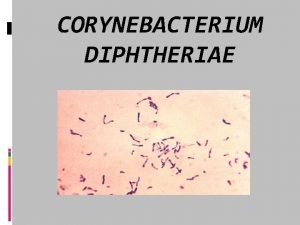
INTRODUCTION – Acute infectious disease-toxigenic strains- Corynebacterium diphtheriae. – Three major clinical types : anterior nasal, faucial and laryngeal – Bacilli multiply locally- throat- powerful exotoxin
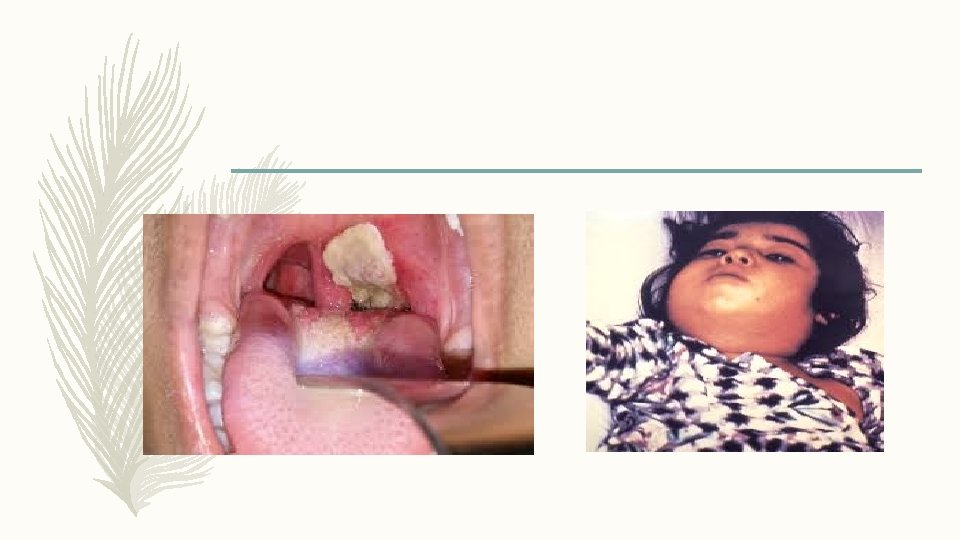
INTRODUCTION (a) Formation- greyish or yellowish membrane("false membrane")- tonsils, pharynx or larynx (or at the site of implantation)- well-defined edges and membrane cannot be wiped away; (b) Marked congestion, oedema or local tissue destruction; (c) Enlargement of the regional lymph nodes; and (d) Signs and symptoms of toxaemia. – Fatality rate- average- 10 % - untreated cases, and 5 % - treated case
PROBLEM STATEMENT WORLD : rare disease –developed countries- routine children vaccination – Improved socio-economic conditions- changing - epidemiology of diphtheria. – Changes- lifestyle - less opportunity to maintain natural immunity- skin infection – Example- waning immunity- outbreak- Russian Federation, Ukraine- 1990 and Thailand Laos in 1996 - highlight- need for booster vaccinations. – Epidemics- largely- decreasing immunization coverage- infants and children, – Developing countries- endemic- lack of adequate widespread immunization – 2012 – 4, 490 cases – globally INDIA: endemic – 2013 – 4090 cases, 64 deaths , case fatality rate – 2. 61
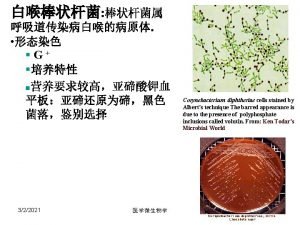
EPIDEMIOLOGICAL DETERMINANTS- Agent Factors – Causative agent : corneybacterium diphtheriae organism. – No invasive power, but produces a powerful exotoxin. – Four types of diphtheria bacilli : gravis, mitis. Belfanti and intermedius- pathogenic to man. – Gravis infections- more severe than mitis. – Not strains- toxigenic. – Non-toxigenic strain- become toxigenic – exposed- particular bacteriophage - carrying the gene- toxin production – Toxin- heart- myocarditis/ nerves- paralysis. – Diphtheria bacilli- sensitive to penicillin and readily killed-heat and chemical agents – Survive for short periods - dust and fomites.
EPIDEMIOLOGICAL DETERMINANTS- Agent Factors – SOURCE OF INFECTION : case or carrier- 0. 1 to 5 per cent 1. CASE- subclinical to frank clinical cases. Mild or silent infection- more important role than frank cases in spreading the infection. 2. CARRIER : ratio- 95 carriers for 5 clinical cases- temporary/ chronic; nasal/ throat – Nasal carriers-particularly dangerous-frequent shedding –organismenvironment, – Temporary- last for about a month; chronic carrier- year or so unless- treated. – lmmunization does not prevent- carrier state.
EPIDEMIOLOGICAL DETERMINANTS- Agent Factors – INFECTIVE MATERIAL : Nasopharyngeal secretions, discharges -skin lesions, contaminated fomites and possibly infected dust. – PERIOD OF INFECTIVITY : Unless treated- 14 to 28 days from- onset- disease. – carriers may remain infective- longer periods. – case or carrier- non-communicable- at least 2 cultures properly obtained from nose and throat- 2 hours apart- negative- diphtheria bacilli
EPIDEMIOLOGICAL DETERMINANTS- Host Factors – AGE : children aged 1 - 5. widespread immunization- shift in age incidencepreschool to schoolage. – SEX : Both sexes are affected, – IMMUNITY : Infants born- immune mothers- relatively immune- first few weeks or months of life. – Developing countries – immunity- inapparent infection. – A herd immunity- over 70% necessary- prevent epidemic – Diphtheria- action- toxin rather than invasion; resistance- availability- specific neutralizing antitoxin - bloodstream and tissues.
EPIDEMIOLOGICAL DETERMINANTSEnvironmental Factors – Occur - all seasons – Winter - months favour its spread MODES OF TRANSMISSION : – Droplet infection. – infected cutaneous lesions. – Transmission by objects (e. g. , cups, thermometers, toys, pencils), contaminated by - nasopharyngeal secretions- possible, but for only short periods.
EPIDEMIOLOGICAL DETERMINANTS- Portal of Entry and Incubation Period a) RESPIRATORY ROUTE- Common. b) NON-RESPIRATORY ROUTES : skin where cuts, wounds and ulcers - not properly attended- may get infected- diphtheria bacilli, – Umbilicus in the newborn. – Occasionally- site of implantation -eye, genitalia or middle ear. – Developed countries – respiratory route- more common INCUBATION PERIOD : - 2 -6 days – occasionally longer
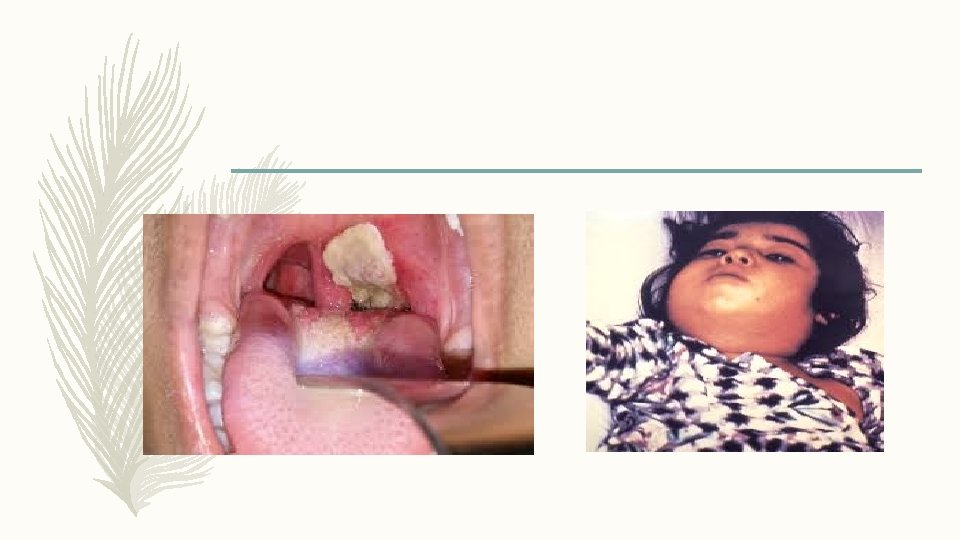
CLINICAL FEATURES – Respiratory tract forms - Pharyngotonsillar, laryngotracheal, nasal, and combinations – Pharyngotonsillar diphtheria- sore throat, difficulty in swallowing, low grade fever – Examination- throat- mild erythema, localized exudate, or a pseudo-membrane. – Membrane- localized/ patch- posterior pharynx or tonsil, may cover entire tonsil, or, cover the soft and hard palates and posterior portion of the pharynx. – Early stage- pseudo-membrane-whitish and may wipe off easily. – Membrane- extend to become thick, blue-white or grey-black, and adherentmucosal erythema- surrounds – membrane – "bullnecked" appearance- severe disease- marked oedema- submandibular area and anterior portion of the neck, along with lymphadenopathy
CLINICAL FEATURES – Laryngotracheal diphtheria- preceded by- pharyngotonsillar disease – Fever, hoarseness and croupy cough at presentation – If infection extends- bronchial tree- most severe form – Initially- clinically indistinguishable- viral croup or epiglottitis. – Prostration and dyspnea- obstruction due to membrane. – Suffocation if not promptly relieved - intubation or tracheostomy
CLINICAL FEATURES – Diphtheria bacilli within- membrane- produce toxin actively. – Toxin – absorbed- distant toxic damage: – parenchymatous degeneration, fatty infiltration and necrosis- heart muscle, liver, kidneys, adrenals, gross hemorrhage – Irregularities- cardiac rhythm- damage- heart. – Difficulties- vision, speech, swallowing. or movement- arms or legs. – Nerve damage- paralysis- soft palate, eye muscles, or extremities – Patients- survive- complications recover completely.
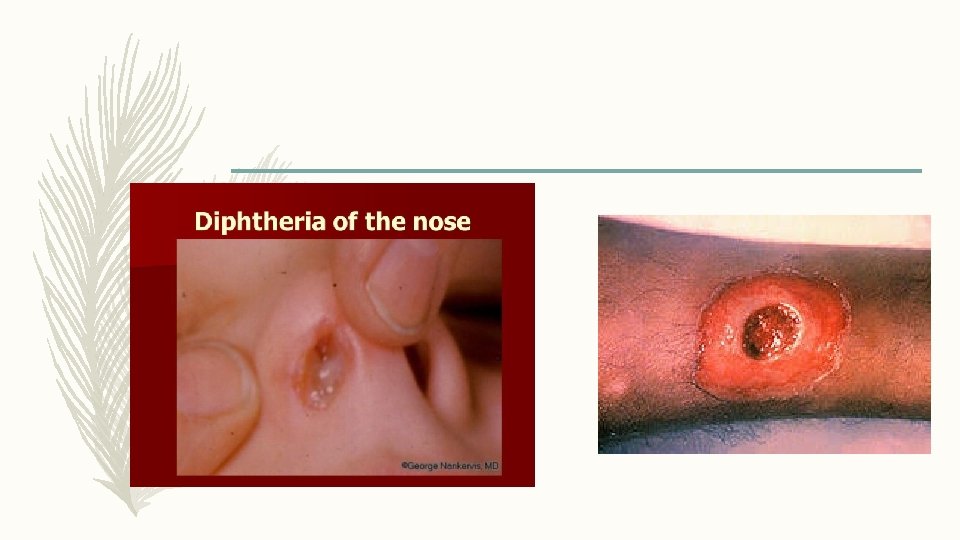
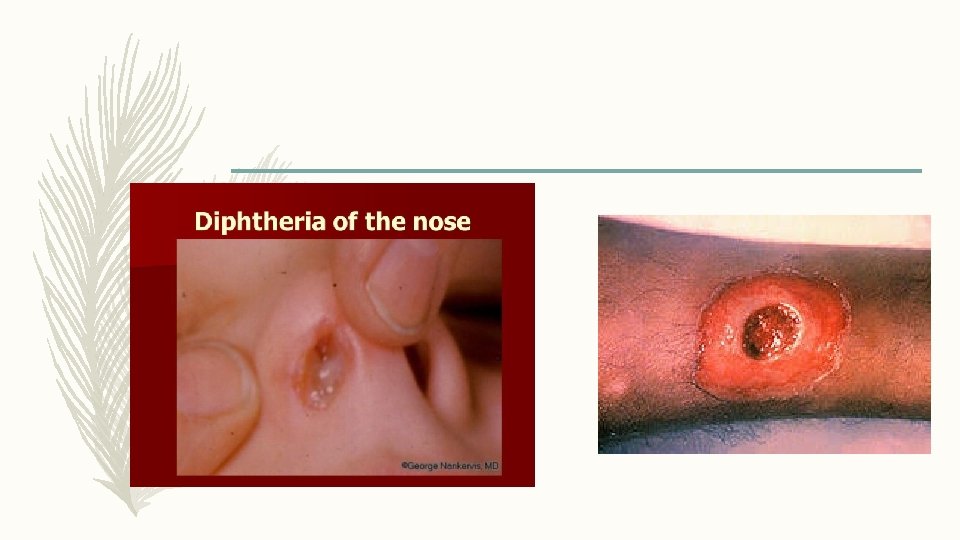
CLINICAL FEATURES – Nasal diphtheria – mildest form of respiratory diphtheria- localized- septum/ turbinates – Occasionally- membrane- extend into - pharynx – Non-respiratory mucosal surface- conjunctivae and genitals may also- sites of infection. – Cutaneous diphtheria- common- tropical areas- appears- secondary infectionprevious skin abrasion/ infection. – Presenting lesion- an ulcer- surrounded by erythema and covered with a membrane. – Patients- seek treatment- chronicity of skin lesion.
CONTROL OF DIPHTHERIA – CASES AND CARRIERS (a) Early detection : Active search- cases and carriers- start immediately- family and school contacts. – Carriers- detected only- culture method. – Swabs- taken- both nose and throat and examined- culture methods (b) Isolation : All cases, suspected cases and carriers- promptly isolated – preferably- hospital- at least 14 days or until proved free of infection. – At least 2 consecutive nose and throat swabs- 24 hours apart-negative before terminating isolation.
CONTROL OF DIPHTHERIA – CASES AND CARRIERS (c) Treatment : (i) CASES : diphtheria- suspected- antitoxins- given without delay- IM/ IV – Dose- 20, 000 to 100, 000 units or more- upon- severity- case , after- preliminary test dose- 0. 2 ml subcutaneously – Mild early pharyngeal or laryngeal disease- 20, 000 -40, 000 units; – Moderate nasopharyngeal disease- 40, 000 -60, 000 units – Severe, extensive or late (3 days or more) disease, 80, 000 -100, 000 units – Every case- Antitoxin + penicillin or erythromycin- 5 to 6 days – (ii) CARRIERS : 10 day course- oral erythromycin- most effective drug – treatment of carriers.
CONTROL OF DIPHTHERIA – CONTACTS: special attention- throat swabbed- immunity status determined. (a) where primary immunization or booster dose- received within - previous 2 years, no further action- needed (b) where primary course or booster dose- diphtheria toxoid- received more than 2 years before, only- booster dose- diphtheria toxoid (c) non-immunized close contact- prophylactic penicillin or erythromycin. – 1000 -2000 units- diphtheria antitoxin and actively immunized against diphtheria. – Contacts- medical surveillance and examined daily - atleast a week after exposure – Bacteriological surveillance- close contacts- several weeks- repeated swabbingapproximately weekly intervals
CONTROL OF DIPHTHERIA – COMMUNITY – Only effective control- active immunization- diphtheria toxoid- all infants as early in life as possible, as scheduled. – Subsequent booster doses every 10 years thereafter – Aim- immunize before- infant loses- maternally derived immunity – Vaccine- toxoid- not directed against organisms- does not prevent- carrier state – Nonimmune individuals- not protected- high level - population immunity – Immunization rate- maintained at a high level
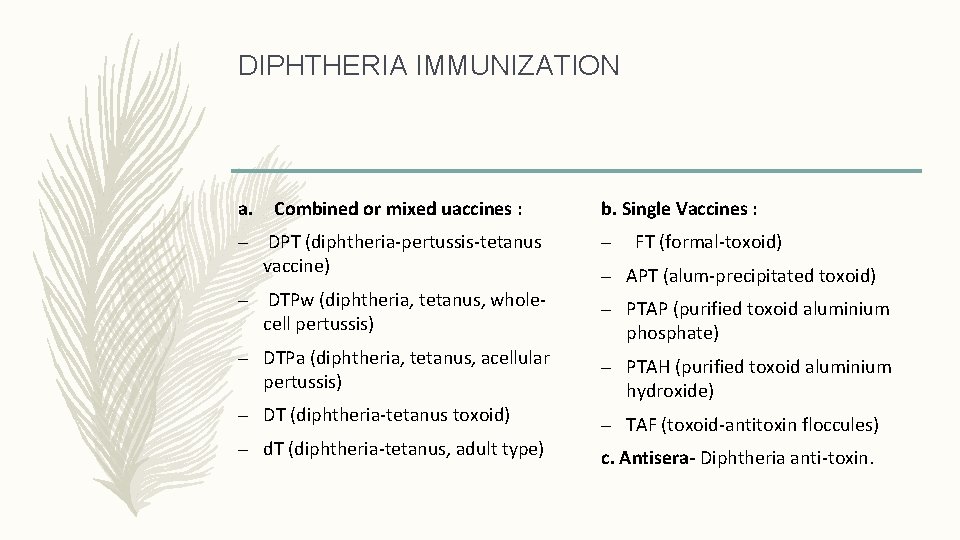
DIPHTHERIA IMMUNIZATION a. Combined or mixed uaccines : b. Single Vaccines : – DPT (diphtheria-pertussis-tetanus vaccine) – – DTPw (diphtheria, tetanus, wholecell pertussis) – PTAP (purified toxoid aluminium phosphate) – DTPa (diphtheria, tetanus, acellular pertussis) – DT (diphtheria-tetanus toxoid) – d. T (diphtheria-tetanus, adult type) FT (formal-toxoid) – APT (alum-precipitated toxoid) – PTAH (purified toxoid aluminium hydroxide) – TAF (toxoid-antitoxin floccules) c. Antisera- Diphtheria anti-toxin.
COMBINED VACCINES – Immunizing infants- preparation of choice- DPT. – infant can be immunized simultaneously against three diseases- great gain administratively. – Pertussis component- enhances- potency- diphtheria toxoid. – Two types- DPT vaccine - plain and adsorbed. – WHO recommends- only adjuvant DPT preparations- utilized- immunization programmes
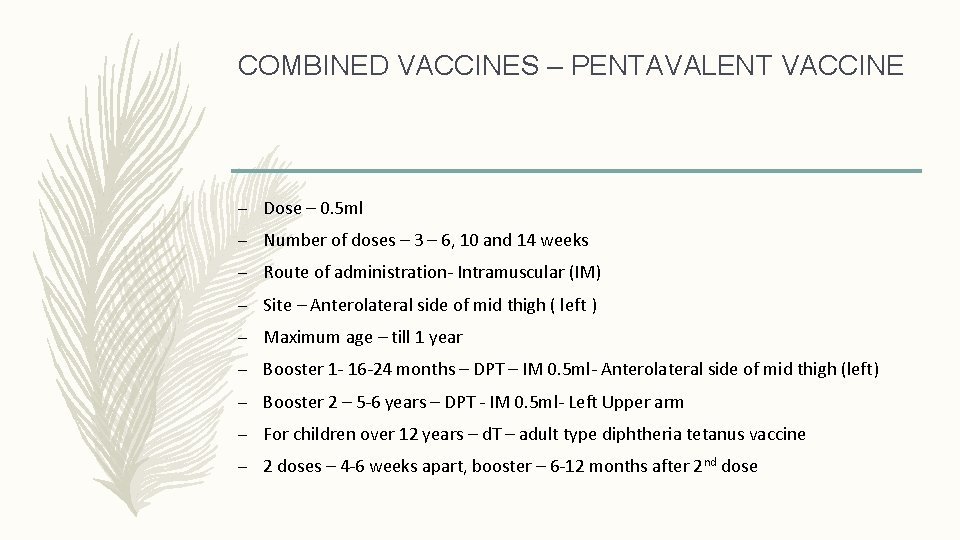
COMBINED VACCINES – PENTAVALENT VACCINE – Dose – 0. 5 ml – Number of doses – 3 – 6, 10 and 14 weeks – Route of administration- Intramuscular (IM) – Site – Anterolateral side of mid thigh ( left ) – Maximum age – till 1 year – Booster 1 - 16 -24 months – DPT – IM 0. 5 ml- Anterolateral side of mid thigh (left) – Booster 2 – 5 -6 years – DPT - IM 0. 5 ml- Left Upper arm – For children over 12 years – d. T – adult type diphtheria tetanus vaccine – 2 doses – 4 -6 weeks apart, booster – 6 -12 months after 2 nd dose
COMBINED VACCINES REACTIONS AND CONTRAINDICATIONS – Fever and mild local reactions – common – Severe complications- Pertussis component - neurological- encephalitis/ encephalopathy ) - prolonged convulsions - infantile spasms - Reye’s Syndrome CONTRAINDICATIONS : – Previous – severe reaction – DPT not repeated instead DT given
SINGLE VACCINE AND ANTISERA – Single vaccines less frequently used ANTISERA : – Diphtheria antitoxin – horse serum – mainstay of passive prophylaxis – Protection against diphtheria toxin – quantitative phenomenon
SUMMARY – Acute infectious disease-toxigenic strains- Corynebacterium diphtheriae. – Three major clinical types : anterior nasal, faucial and laryngeal – Mode of spread – respiratory and non respiratory – Bacilli multiply locally- throat- powerful exotoxin – Formation of greyish membrane ( false membrane ) – Bull necked appearance – Pentavalent vaccine
 Navya venkateshaiah
Navya venkateshaiah Diphtheria cdc
Diphtheria cdc Katrina kretsinger
Katrina kretsinger Diphtheria
Diphtheria Diphtheria stain
Diphtheria stain Diphtheria
Diphtheria Mcgill medicine supporting documents
Mcgill medicine supporting documents Department of medicine solna
Department of medicine solna Seqs community medicine
Seqs community medicine Introduction to community medicine
Introduction to community medicine Minus type desk
Minus type desk Lead time in community medicine
Lead time in community medicine Elements of primary health care
Elements of primary health care Cohort study community medicine
Cohort study community medicine Types of family in community medicine
Types of family in community medicine Introduction to community medicine
Introduction to community medicine Duke medicine grand rounds
Duke medicine grand rounds Lead time in community medicine
Lead time in community medicine New york city department of youth and community development
New york city department of youth and community development Georgia department of community health
Georgia department of community health Prepare to scale up in social mobilization
Prepare to scale up in social mobilization Innovation 2023
Innovation 2023 Margaret wiedmann
Margaret wiedmann Family apgar
Family apgar Calculating drops per minute
Calculating drops per minute Ethical issues in precision medicine
Ethical issues in precision medicine Navy medicine professional development center
Navy medicine professional development center Upjs medicine timetable
Upjs medicine timetable