Dialysis Ashley K Ashley L Hennries L Leanne

- Slides: 34
Dialysis Ashley K. , Ashley L. , Hennries L. , Leanne C. , & Tina P.
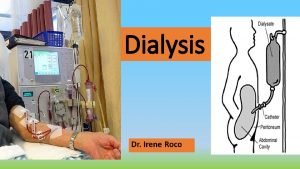
What is Dialysis? ● The movement of fluid and molecules across a semipermeable membrane from one compartment to another ● Begins when uremia can no longer be treated with conservative medical management ○ Generally begins when GFR is < 15 m. L/min/1. 73 m² ○ Physician will determine when patient will start dialysis based on clinical status ○ Uremic complications that indicate immediate dialysis: encephalopathy, neuropathies, uncontrolled hyperkalemia, pericarditis, and accelerated hypertension ● Used to correct fluid and electrolyte imbalances, to remove waste products in kidney failure, and also to treat drug overdoses
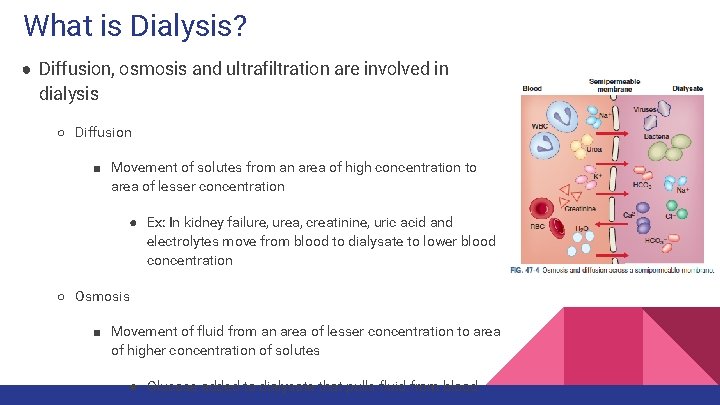
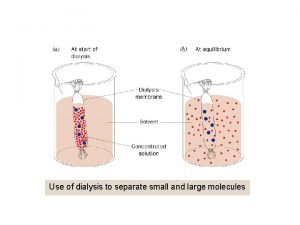
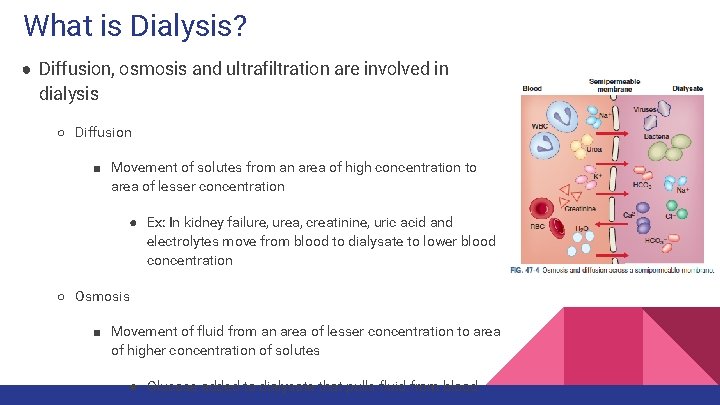
What is Dialysis? ● Diffusion, osmosis and ultrafiltration are involved in dialysis ○ Diffusion ■ Movement of solutes from an area of high concentration to area of lesser concentration ● Ex: In kidney failure, urea, creatinine, uric acid and electrolytes move from blood to dialysate to lower blood concentration ○ Osmosis ■ Movement of fluid from an area of lesser concentration to area of higher concentration of solutes ● Glucose added to dialysate that pulls fluid from blood
What is Dialysis? ● Two methods of dialysis ○ Peritoneal dialysis ■ Peritoneal membrane acts as the semipermeable membrane ○ Hemodialysis ■ An artificial membrane is used and is in contact with patient’s blood ● Usually made of cellulose-based or synthetic materials
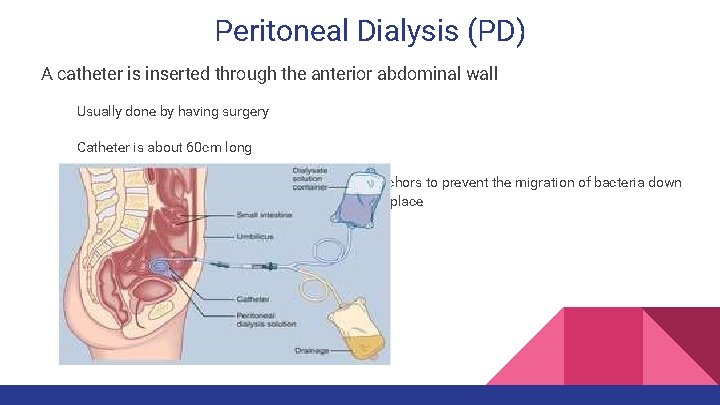
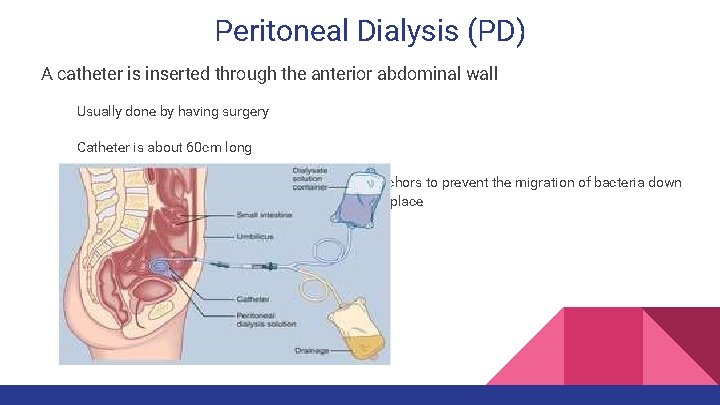
Peritoneal Dialysis (PD) A catheter is inserted through the anterior abdominal wall Usually done by having surgery Catheter is about 60 cm long Contains one or two Dacron cuffs, which act as anchors to prevent the migration of bacteria down the shaft of the skin and to keep the catheter in place
Peritoneal Dialysis Cycles Three phases make up what is considered an “exchange” This occurs when waste products enter the peritoneal cavity and cycle through the dialysis solution For adults normally they go through about 4 exchanges per a night or day Inflow Phase: Prescribed amount of Dialysate solution is infused Adults: 2 -3 L Children: 30 -50 m. L/kg Once the solution is infused the tube is clamped to prevent air from entering the tubing Dwell Phase: Diffusion and osmosis occurs between the patient’s blood and peritoneal cavity
Peritoneal Dialysis Systems Automated Peritoneal Dialysis/Continuous Cycling Peritoneal Dialysis (CCPD) This can be done while the patient sleeps, which gives the patient more freedom during the day Has an automated cycler that controls the inflow, dwelling, and drainage Takes about 1 -2 hours per an exchange Continuous Ambulatory Peritoneal Dialysis (CAPD) Is done during the day and done manually The bag can be disconnected once the fluid is administered
Complications of Peritoneal Dialysis in Adults Exit site infection Most commonly from Staphylococcus Aureus or Staphylococcus Epidermidis Manifestations: Redness at the site Tenderness Drainage Treated with antibiotics If not treated immediately, can progress into abscess formation & may cause

Complications of PD in Adults cont. Peritonitis Inflammation of the peritoneum From contamination or exit site infection Often occurs from improper technique (use sterile technique when handling catheter or tubing) Manifestations Abdominal pain and cloudy peritoneal effluent GI→ diarrhea, vomiting, abdominal distention and hyperactive bowel sounds Culture, Gram Stain and WBC differential of peritoneal effluent used for diagnosis
Complications of PD in Adults cont. Hernias From increased intraabdominal pressure secondary to dialysate infusion After repair of hernia, PD can resume after several days Use small dialysate volumes and keep patient supine Lower Back Problems From increased pressure intraabdominal pressure Orthopedic binders and regular exercise program to strengthen back muscles can help Bleeding After placement, it is not uncommon for the effluent drainage to be pink or slightly
Complications of PD in Adults cont. Pulmonary Complications Atelectasis, pneumonia and bronchitis From upward displacement of diaphragm Frequent repositioning, elevated HOB & deep breathing exercises can help Protein Loss Lost in dialysate fluid Usually around 0. 5 g/L but can be as high as 10 -20 g/L Can result in malnutrition and indicate termination of PD
Complications in Children Peritonitis a major complication Treatment with antibiotics and some may require a new catheter Tunneled infections Swellings, warmth, and tenderness along the catheter tract Treatment with antibiotics or catheter replacement Peritoneal leaks Ventral hernias
Nursing Management ● Learning how to self manage PD can typically be done in a 3 -7 day training program ● Take VS before and after dialysis ● Showering is preferred over bathing because it decreases chance of infection ● Monitor for signs of infection ● Can wash site with soap and water ● Daily dressing changes may be required depending on the order or some patients might not even have a dressing covering the site
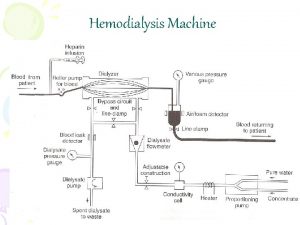
Hemodialysis (HD) Process of cleansing patient’s blood using an artificial kidney Dialyzer) ( In order to perform hemodialysis, a large blood vessel and rapid blood flow is needed. Obtaining vascular access is one of the most difficult problem associated with HD. Different types of vascular access: Arteriovenous Fistulas (AVFs) Arteriovenous Grafts (AVGs) Temporary Vascular Access
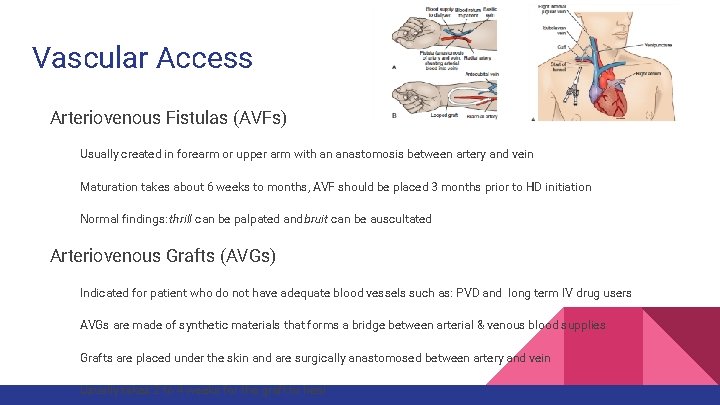
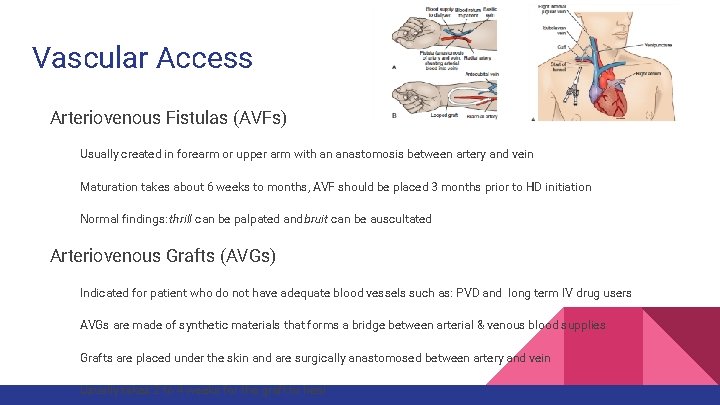
Vascular Access Arteriovenous Fistulas (AVFs) Usually created in forearm or upper arm with an anastomosis between artery and vein Maturation takes about 6 weeks to months, AVF should be placed 3 months prior to HD initiation Normal findings: thrill can be palpated and bruit can be auscultated Arteriovenous Grafts (AVGs) Indicated for patient who do not have adequate blood vessels such as: PVD and long term IV drug users AVGs are made of synthetic materials that forms a bridge between arterial & venous blood supplies Grafts are placed under the skin and are surgically anastomosed between artery and vein Usually takes 2 to 4 weeks for the graft to heal
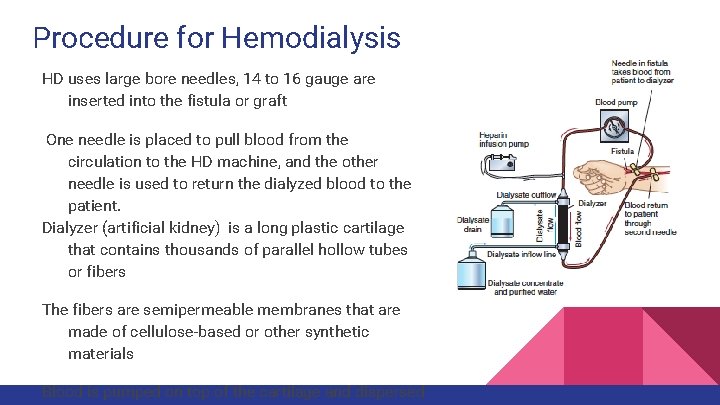
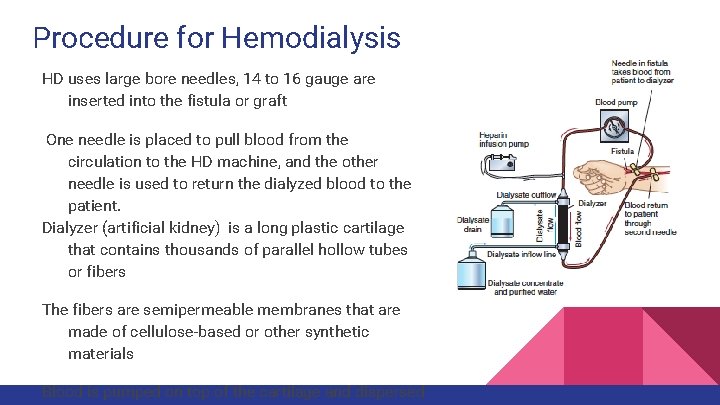
Procedure for Hemodialysis HD uses large bore needles, 14 to 16 gauge are inserted into the fistula or graft One needle is placed to pull blood from the circulation to the HD machine, and the other needle is used to return the dialyzed blood to the patient. Dialyzer (artificial kidney) is a long plastic cartilage that contains thousands of parallel hollow tubes or fibers The fibers are semipermeable membranes that are made of cellulose-based or other synthetic materials Blood is pumped on top of the cartilage and dispersed
Procedure cont. . Dialysis fluid (dialysate) is pumped into the bottom of the cartilage and bathes the outside of the fibers Ultrafiltration, diffusion and occurs across the semipermeable membrane The dialyzer is then flushed with normal saline to bring the blood back to the patient Usually done in dialysis center for 3 to 4 hours, 3 days per week Other schedules for HD are short daily HD and long nocturnal HD Hemodialysis can be done at homehttps: //www. youtube. com/watch? v=sh. FSW 8 VE 3 Gs home currently only 2% of HD patient dialyze at
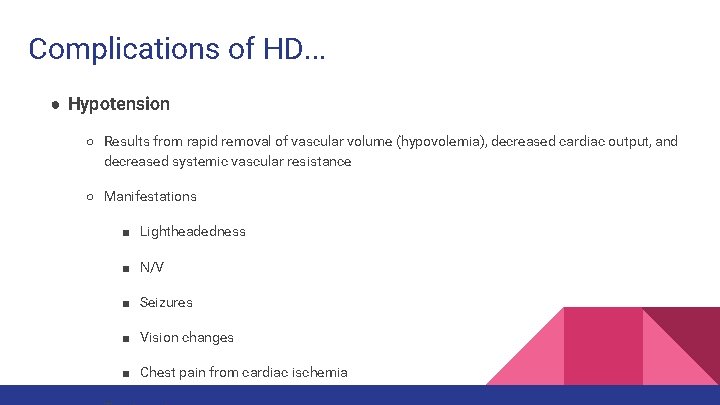
Complications of HD. . . ● Hypotension ○ Results from rapid removal of vascular volume (hypovolemia), decreased cardiac output, and decreased systemic vascular resistance ○ Manifestations ■ Lightheadedness ■ N/V ■ Seizures ■ Vision changes ■ Chest pain from cardiac ischemia
Complications of HD. . . ● Muscle cramps ○ Factors: hypotension, hypovolemia, high ultrafiltration rate, and low-sodium dialysis solution ○ Most frequently seen in the 1 st month after initiation ○ Treatment ■ Reduce ultrafiltration rate ■ Administer fluids (NS, glucose, mannitol) ■ Hypertonic glucose preferred ● Loss of blood ○ Results from blood not being completely rinsed from dialyzer, accidental separation of blood tubing, dialysis membrane rupture or bleeding after removal of needles
Complications of HD. . . ● Hepatitis ○ Hepatitis B outbreaks occur less frequently now due to screening, lower transfusion requirements and vaccinations ■ Still occur due to transmission via break in infection control practices ■ CDC recommends all patients and personnel in dialysis unit to receive hep B vaccine ○ Hepatitis C is found in majority of cases in dialysis patients ■ Approx. 8 -10% of patients undergoing dialysis in US test positive for anti-HCV (indicates previous infection) ■ Must implement infection control precautions
Nursing Management in HD Assessments prior to HD: patient’s fluid status (weight, BP, peripheral edema, lungs and heart sounds) condition of vascular access temperature general skin condition During procedure, take vital signs at least every 30 -60 minutes To prevent infection and clotting of the arteriovenous access, the following actions are contraindicated:
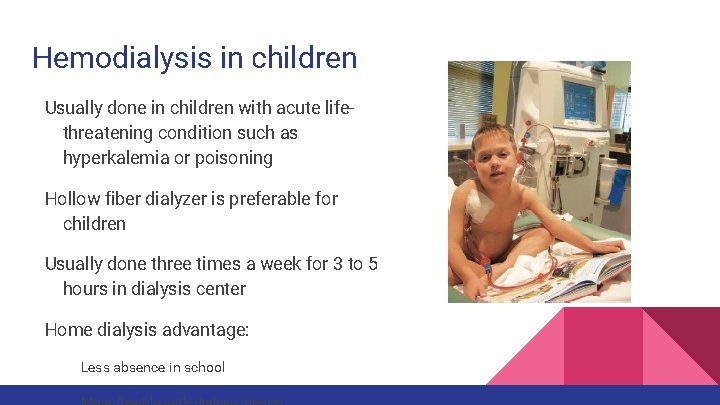
Hemodialysis in children Usually done in children with acute lifethreatening condition such as hyperkalemia or poisoning Hollow fiber dialyzer is preferable for children Usually done three times a week for 3 to 5 hours in dialysis center Home dialysis advantage: Less absence in school
Nursing Consideration Initiation of HD therapy can be traumatic experience for children Education about adequate protein intake to maximize growth Dietary restriction in chronic HD Potassium Phosphorus Fluid and sodium
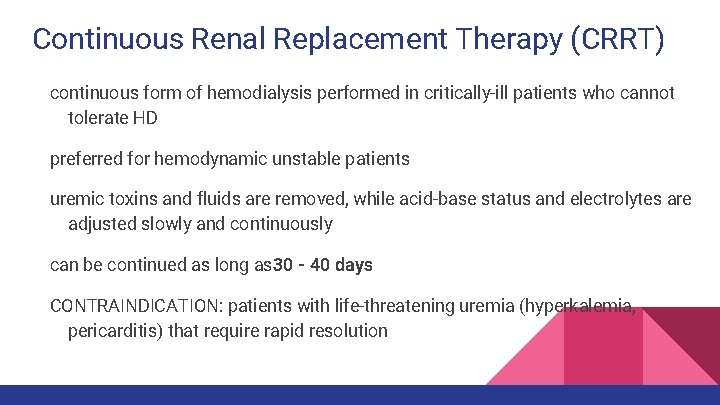
Continuous Renal Replacement Therapy (CRRT) continuous form of hemodialysis performed in critically-ill patients who cannot tolerate HD preferred for hemodynamic unstable patients uremic toxins and fluids are removed, while acid-base status and electrolytes are adjusted slowly and continuously can be continued as long as 30 - 40 days CONTRAINDICATION: patients with life-threatening uremia (hyperkalemia, pericarditis) that require rapid resolution
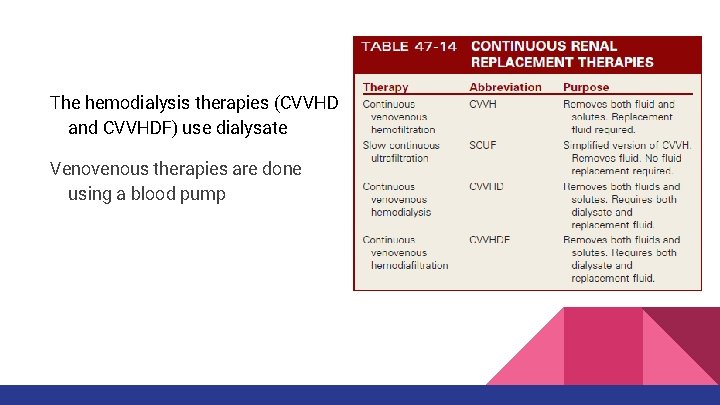
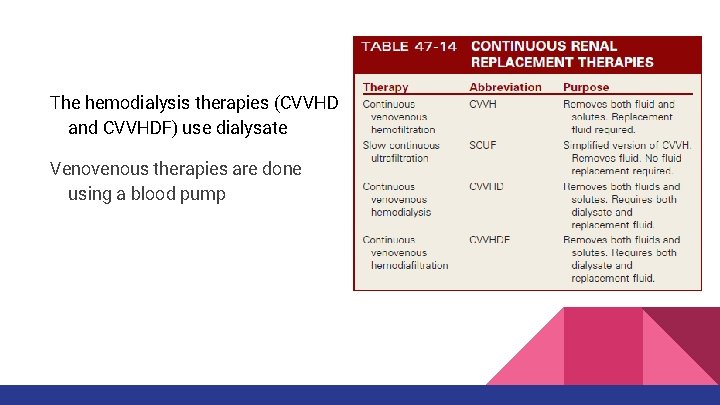
The hemodialysis therapies (CVVHD and CVVHDF) use dialysate Venovenous therapies are done using a blood pump
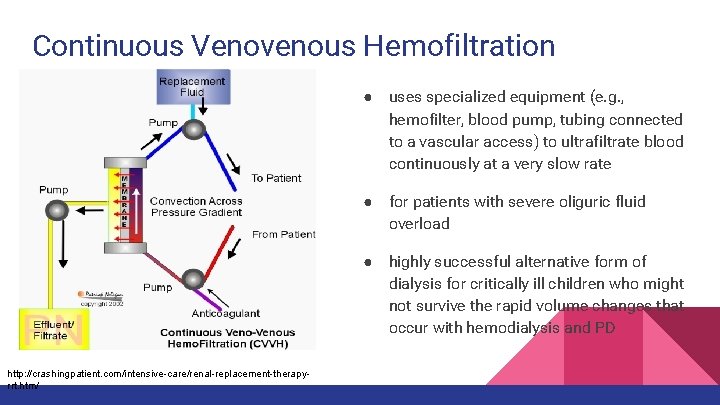
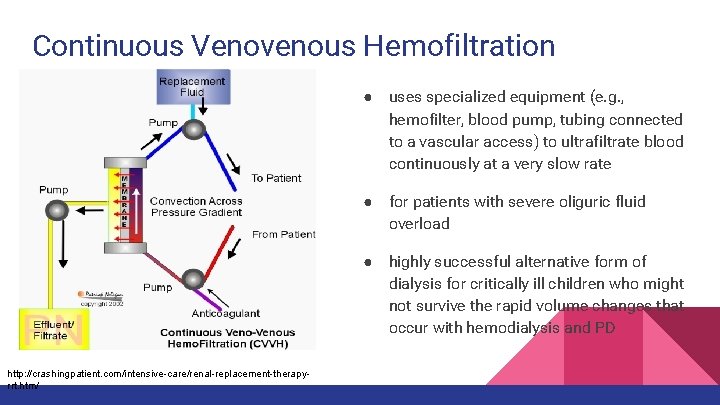
Continuous Venovenous Hemofiltration ● uses specialized equipment (e. g. , hemofilter, blood pump, tubing connected to a vascular access) to ultrafiltrate blood continuously at a very slow rate ● for patients with severe oliguric fluid overload ● highly successful alternative form of dialysis for critically ill children who might not survive the rapid volume changes that occur with hemodialysis and PD http: //crashingpatient. com/intensive-care/renal-replacement-therapyrrt. htm/
Nursing Considerations Collaborate with other health care providers Monitor closely hemodynamic state (esp. in critically ill children) Anticoagulation (ex. heparin) Change hemofilter every 24 -48 hours Obtain weight Monitor lab values Hourly I/Os
Self Assessment Which of the following are complications of peritoneal dialysis? (Select all that apply) A. Hepatitis B. Exit site infection C. Hypotension D. Lower back problems E. Protein loss
Self Assessment Which one of the following continuous renal replacement therapies removes both fluid and solutes and requires only fluid replacement? A. Continuous venous hemodiafiltration (CVVHDF) B. Slow continuous ultrafiltration (SCUF) C. Continuous venous hemofiltration (CVVH) D. Continuous venous hemodialysis (CVVHD)
Self Assessment True or False: In cases of chronic hemodialysis (HD), dietary restrictions may be placed on the following: potassium, phosphorus, fluids and sodium.
Self Assessment Which of the following allows the patient to do dialysis while asleep? A. Automated peritoneal dialysis B. Continuous ambulatory peritoneal dialysis
Self Assessment Fill in the blanks: When an arteriovenous fistula (AVF) is created, normally a _____ can be felt by palpating the area and a _____ can be heard with a stethoscope.
References Hockenberry, M. J. , & Wilson, D. (2015). Wong's Nursing Care of Infants and Children. St. Louis, MO: Mosby/Elsevier. Lewis, S. , Dirksen, S. , Heitkemper, M. , & Bucher, L. (2014). In Medical-surgical nursing: Assessment and management of clinical problems (9 th ed. ). St. Louis, Missouri: Elsevier.
 Leanne trimble
Leanne trimble Leanne brannigan
Leanne brannigan Neil thisse is a loyalist answers
Neil thisse is a loyalist answers Victorian curriculum economics
Victorian curriculum economics Leanne cameron
Leanne cameron Hearst museum
Hearst museum What is ultrafiltration in dialysis
What is ultrafiltration in dialysis Sled dialysis
Sled dialysis Dialysis milk
Dialysis milk Peritoneal dialysis contraindications
Peritoneal dialysis contraindications Dialysis port
Dialysis port Purpose of dialysis
Purpose of dialysis Dialysis can separate
Dialysis can separate Low potassium diet nemo
Low potassium diet nemo Dialysis membrane
Dialysis membrane Sister src
Sister src Causes of low drain volume peritoneal dialysis
Causes of low drain volume peritoneal dialysis Ktv meaning in dialysis
Ktv meaning in dialysis Aeiou dialysis
Aeiou dialysis Conclusion of dialysis
Conclusion of dialysis Diet chart for diabetic
Diet chart for diabetic Dialysis tubing experiment
Dialysis tubing experiment Dialysis
Dialysis Husein
Husein Peritoneal membrane
Peritoneal membrane Dialysis machine parts and functions
Dialysis machine parts and functions Ademex
Ademex Pylelolithotomy
Pylelolithotomy Color 26062003
Color 26062003 Active transportation
Active transportation Phimosis
Phimosis Dialysis
Dialysis Sled dialysis principle
Sled dialysis principle Hemodialysis machine parts and function
Hemodialysis machine parts and function Dialysis
Dialysis