KQu IPUKRR Regional Day North West 12 00











- Slides: 35

KQu. IP/UKRR Regional Day North West 12: 00 - 12: 30 § Home Therapies Data presentation – Dr Retha Steenkamp § The Manchester Experience of a Navigator Nurse on Recruitment and Training for Home Haemodialysis – John Woods, Specialist Nurse § KQu. IP & Home Therapies - Richard Fluck – Home Therapies lead
Home Therapies Data North West Regional Day Retha Steenkamp Head of Operations UKRR
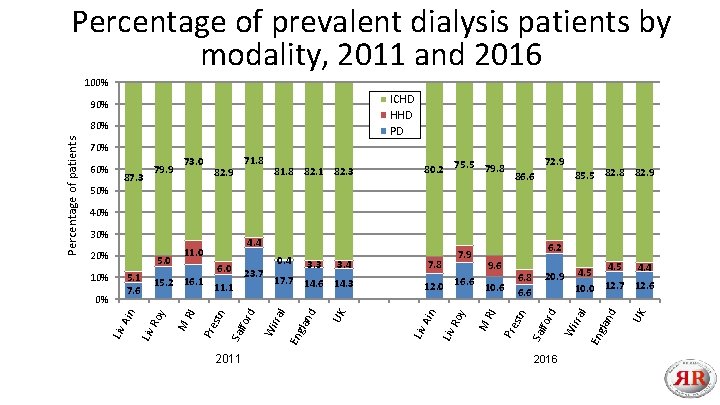
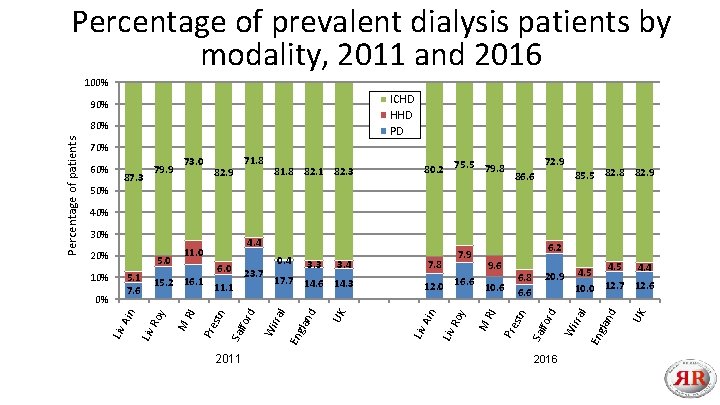
Percentage of prevalent dialysis patients by modality, 2011 and 2016 100% ICHD HHD PD 90% 70% 60% 87. 3 79. 9 73. 0 71. 8 82. 9 81. 8 82. 1 82. 3 80. 2 75. 5 79. 8 72. 9 86. 6 85. 5 82. 8 82. 9 50% 40% 6. 2 2016 En gl UK an d 4. 5 4. 4 4. 5 10. 0 12. 7 12. 6 l 20. 9 Wi rra stn Pre RI Ro y Liv Ain 12. 0 16. 6 10. 6 6. 8 6. 6 for d 9. 6 Sal 7. 9 7. 8 Liv an UK l En gl for 2011 d 3. 4 17. 7 14. 6 14. 3 Sal stn Pre RI M Liv Ain 0% 3. 3 23. 7 6. 0 15. 2 16. 1 11. 1 Ro y 5. 1 7. 6 10% 0. 4 Wi rra 5. 0 4. 4 11. 0 d 20% M 30% Liv Percentage of patients 80%
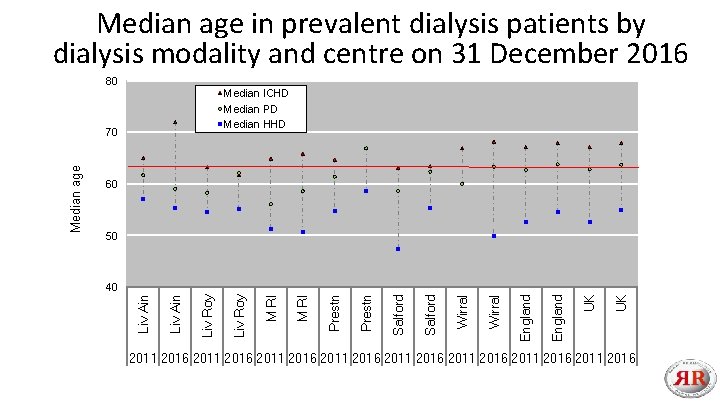
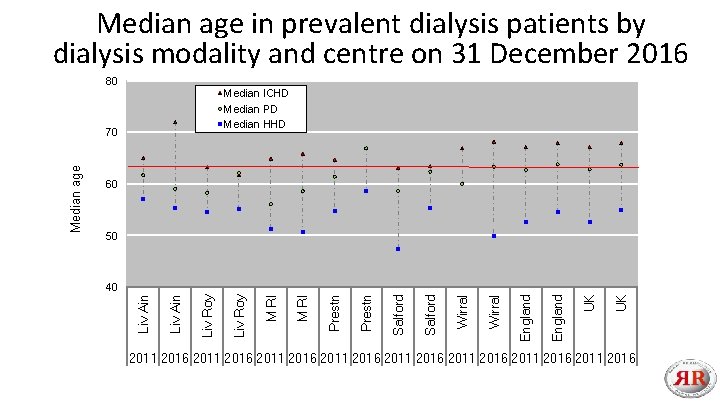
Median age in prevalent dialysis patients by dialysis modality and centre on 31 December 2016 80 Median ICHD Median PD Median HHD 60 50 UK UK England Wirral Salford Prestn M RI Liv Roy Liv Ain 40 Liv Ain Median age 70 2011 2016 2011 2016

Percentage of prevalent dialysis patients by modality, age and gender on 31 December 2016 120% Percentage of patients 100% ICHD HHD PD 80% 60% 40% 20% 0% 29 20 39 30 49 40 59 50 Male 9 -6 60 9 -7 70 + 80 9 -2 20 Age group 9 -3 30 9 -4 40 9 -5 50 69 60 Female 79 70 + 80
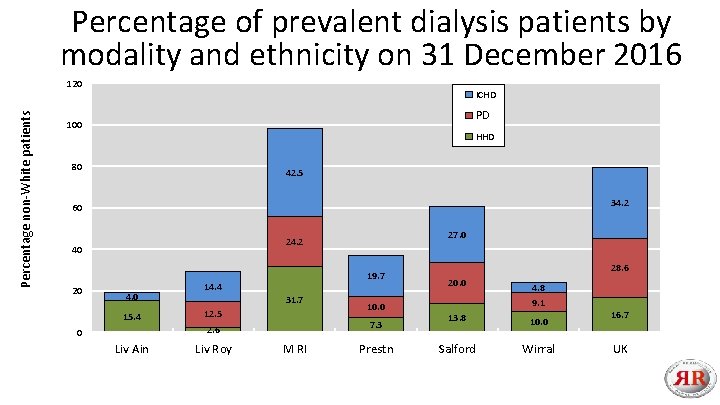
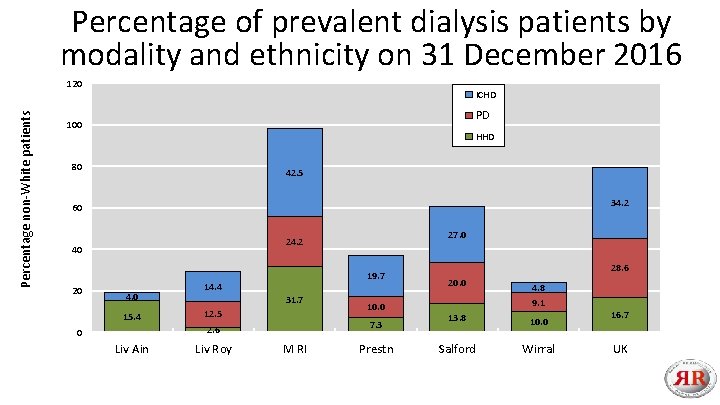
Percentage of prevalent dialysis patients by modality and ethnicity on 31 December 2016 Percentage non-White patients 120 ICHD PD 100 HHD 80 42. 5 34. 2 60 40 20 27. 0 24. 2 4. 0 15. 4 19. 7 14. 4 31. 7 12. 5 7. 3 2. 6 0 Liv Ain Liv Roy 10. 0 M RI Prestn 28. 6 20. 0 4. 8 9. 1 13. 8 10. 0 Salford Wirral 16. 7 UK
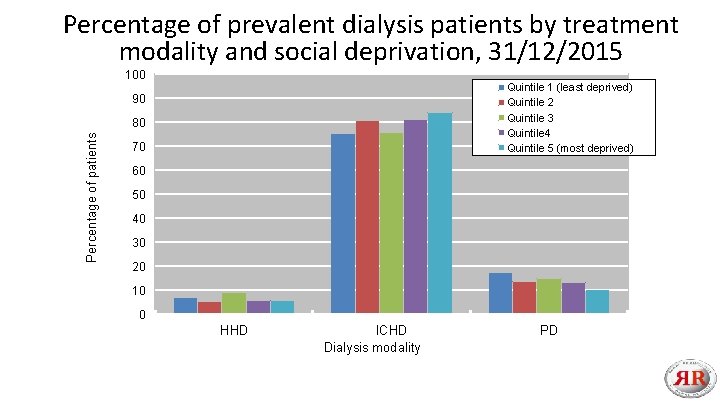
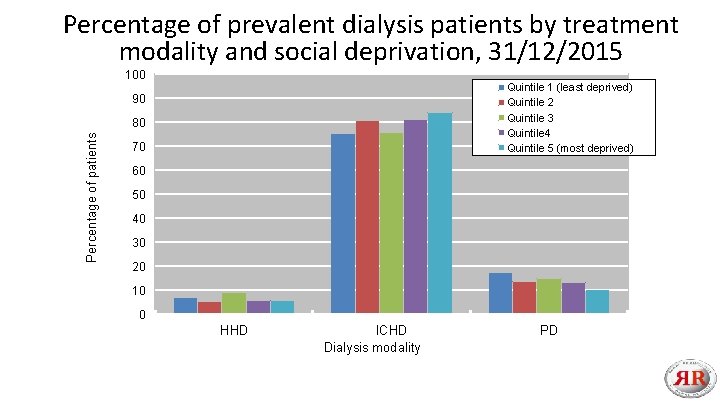
Percentage of prevalent dialysis patients by treatment modality and social deprivation, 31/12/2015 100 Quintile 1 (least deprived) Quintile 2 Quintile 3 Quintile 4 Quintile 5 (most deprived) 90 Percentage of patients 80 70 60 50 40 30 20 10 0 HHD ICHD Dialysis modality PD
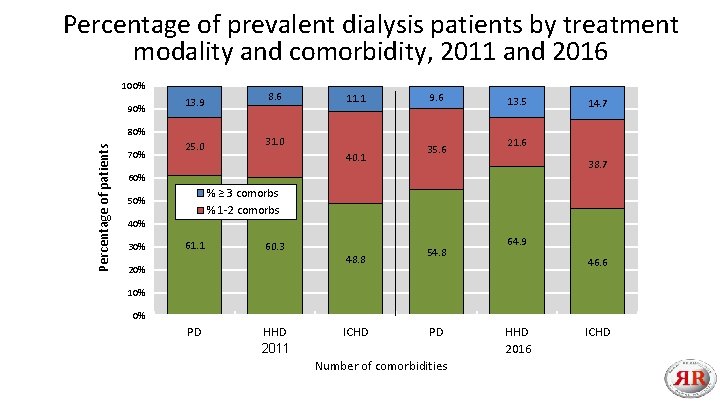
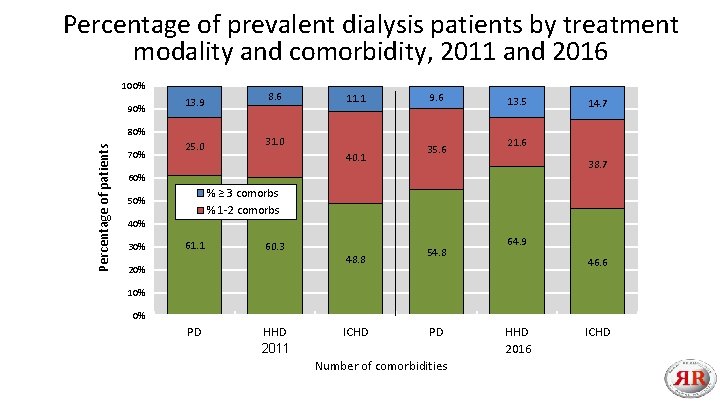
Percentage of prevalent dialysis patients by treatment modality and comorbidity, 2011 and 2016 100% 90% 13. 9 Percentage of patients 80% 70% 25. 0 8. 6 11. 1 31. 0 40. 1 9. 6 35. 6 13. 5 14. 7 21. 6 38. 7 60% % ≥ 3 comorbs % 1 -2 comorbs 50% 40% 30% 61. 1 60. 3 20% 48. 8 54. 8 64. 9 46. 6 10% 0% PD HHD 2011 ICHD PD Number of comorbidities HHD 2016 ICHD

Acknowledgements Thank you to all renal units that submit data to the UKRR Thank you also to all the people at the UKRR who work in the background to make all this possible.
“The Manchester Experience of a Navigator Nurse on Recruitment and Training for Home Haemodialysis” John Woods, Specialist Nurse in Dialysis Sandip Mitra, Consultant Nephrologist

“Conclusion: Dialysis nurses have prevailing views about modality selection that are strongly determined by their area of experience and expertise”

Manchester TRe. NDs model of Haemodialysis Care Satellite Fully assisted Satellite Shared – care level 1 care and above The Central Hub Dialysis unit Complex and unstable patients Satellite Self/shared – care level 4 Home
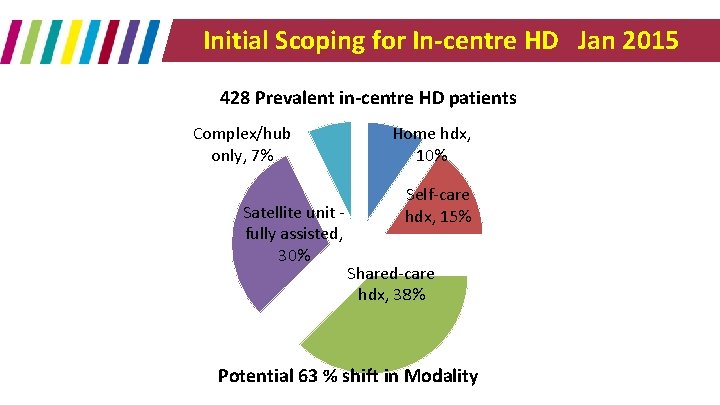
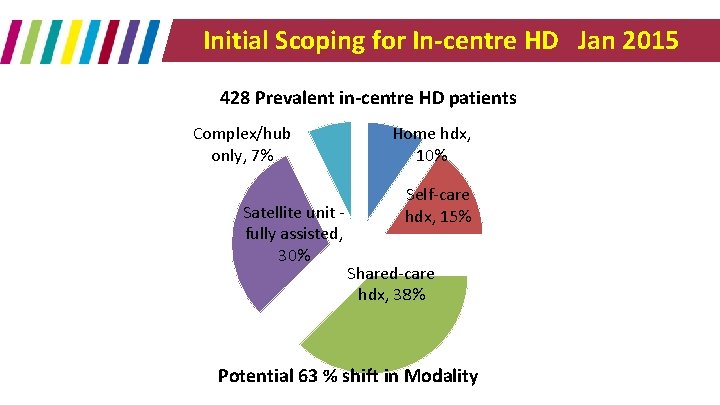
Initial Scoping for In-centre HD Jan 2015 428 Prevalent in-centre HD patients Complex/hub only, 7% Satellite unit fully assisted, 30% Home hdx, 10% Self-care hdx, 15% Shared-care hdx, 38% Potential 63 % shift in Modality

My Project Aim (Oct 2015 - Sept 2016) • Identify and demonstrate the potential and eligibility of patients who could transfer from existing fully assisted HD care to collaborative/shared/independent care within the HD centres. • Increase patients opting for Home or Shared care across the service • Develop a Proof of Concept of future HD care design at CMFT
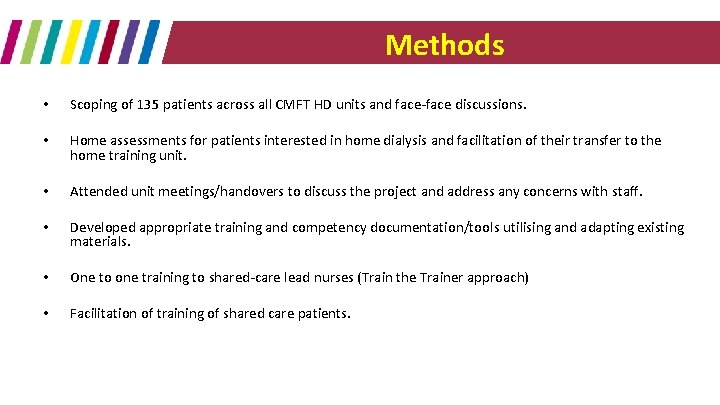
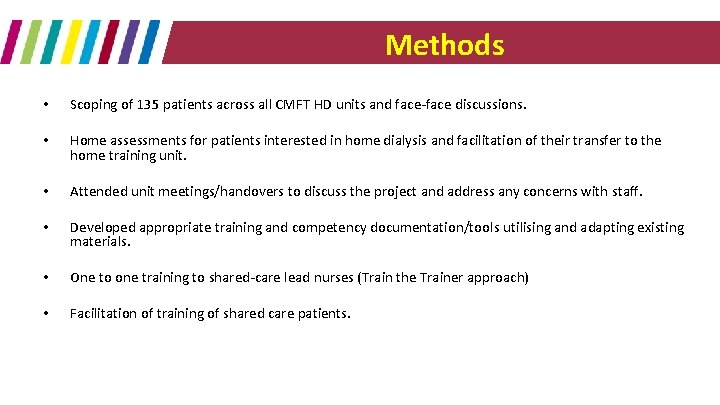
Methods • Scoping of 135 patients across all CMFT HD units and face-face discussions. • Home assessments for patients interested in home dialysis and facilitation of their transfer to the home training unit. • Attended unit meetings/handovers to discuss the project and address any concerns with staff. • Developed appropriate training and competency documentation/tools utilising and adapting existing materials. • One to one training to shared-care lead nurses (Train the Trainer approach) • Facilitation of training of shared care patients.
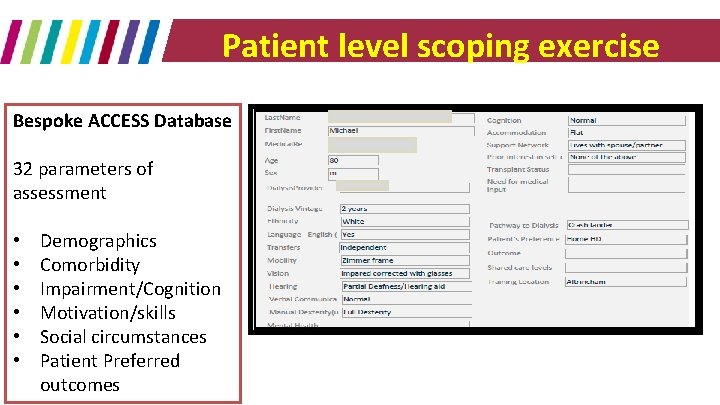
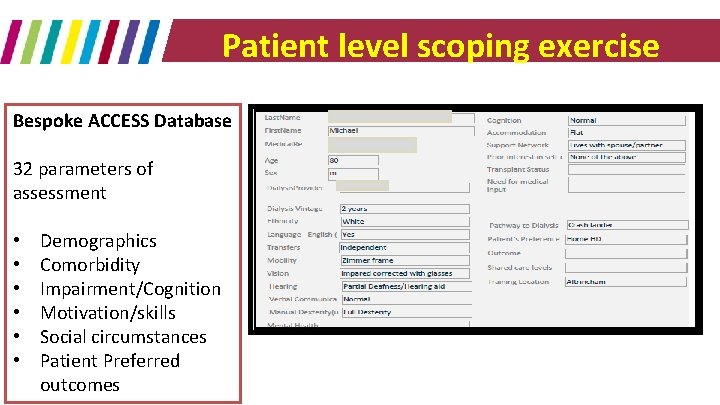
Patient level scoping exercise Bespoke ACCESS Database 32 parameters of assessment • • • Demographics Comorbidity Impairment/Cognition Motivation/skills Social circumstances Patient Preferred outcomes
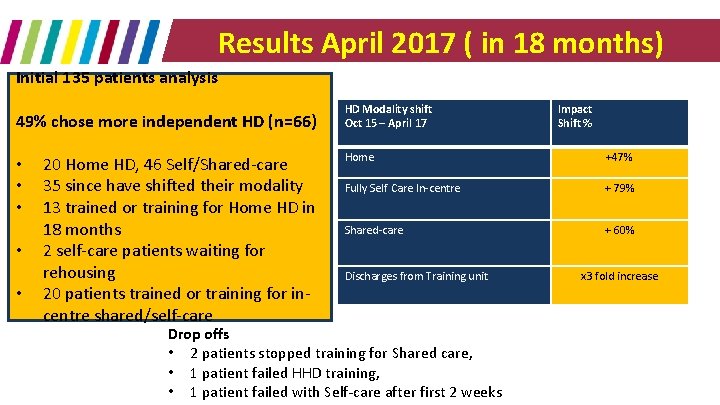
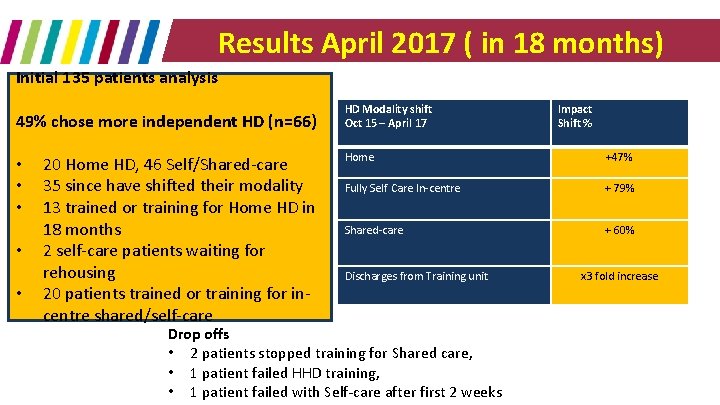
Results April 2017 ( in 18 months) Initial 135 patients analysis 49% chose more independent HD (n=66) • • • 20 Home HD, 46 Self/Shared-care 35 since have shifted their modality 13 trained or training for Home HD in 18 months 2 self-care patients waiting for rehousing 20 patients trained or training for incentre shared/self-care HD Modality shift Oct 15 – April 17 Impact Shift % Home +47% Fully Self Care In-centre + 79% Shared-care + 60% Discharges from Training unit Drop offs • 2 patients stopped training for Shared care, • 1 patient failed HHD training, • 1 patient failed with Self-care after first 2 weeks x 3 fold increase
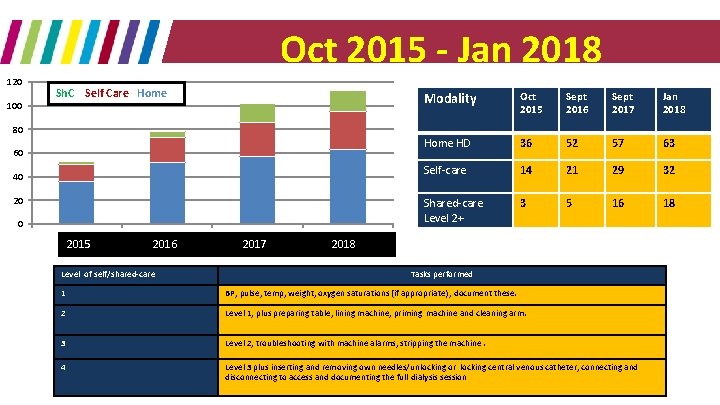
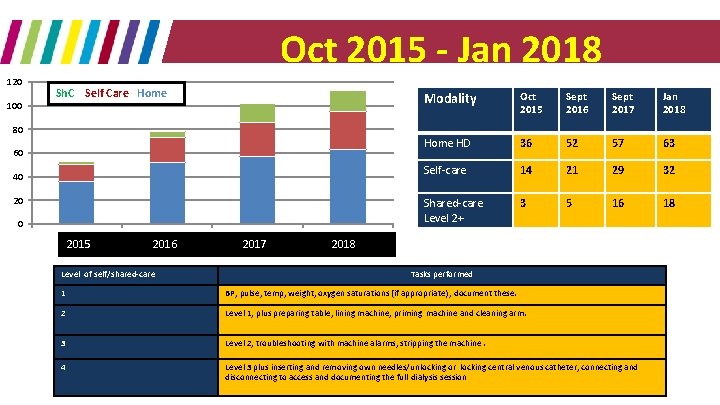
Oct 2015 - Jan 2018 120 100 Sh. C Self Care Home Modality Oct 2015 Sept 2016 Sept 2017 Jan 2018 Home HD 36 52 57 63 Self-care 14 21 29 32 Shared-care Level 2+ 3 5 16 18 80 60 40 20 0 1 2015 2 2016 Level of self/shared-care 3 2017 4 2018 Tasks performed 1 BP, pulse, temp, weight, oxygen saturations (if appropriate) , document these. 2 Level 1, plus preparing table, lining machine, priming machine and cleaning arm. 3 Level 2, troubleshooting with machine alarms, stripping the machine. 4 Level 3 plus inserting and removing own needles/unlocking or locking central venous catheter, connecting and disconnecting to access and documenting the full dialysis session

Barriers and Biases – Main themes • Lack of confidence (in their own ability to train or with regards to their health status) • Change not necessary: Happy where they are and with the present care provided • Concerns for safety • Needling fears • Logistics/Convenience: Travelling to the training unit. No late shift available for training • Home circumstances: No room, Social and personal/relationship issues • Misconceptions (Patients and staff) – Spare room required at home – Lone dx not allowed – AVF required – Can’t have home dx if got other health problems/co-morbidities
Summarising My Role • Developed a bespoke database to characterise patient phenotype & preferences • One to one patient contact across the network • Provide education around home dialysis • Troubleshooting barriers at a patient level (Myths and Facts) • Guide patients through the Decision making process [Transition to Training and discharge] • Support to unit nursing teams for shared-care and the Share. HD initiative • Handover to the home teams customised to individual preferences • Reporting of data to Senior management
ICHD. . to Sh. C HD. . to HHD “I was on regular hospital dialysis for 2 ½ years. I then did shared-care on my unit. This gave me confidence to change to home dialysis. I can now fit the dialysis around my life. I feel better and healthier on home dialysis”
A Take home message
Home dialysis Breakout session
What do we want to think about? • Consider the challenge • Diagnostics • Do we know why we are where we are? • What should we measure? • Can we identify aspects of practice to generate change? • What do well? • Where can we learn from? • How do we do it?
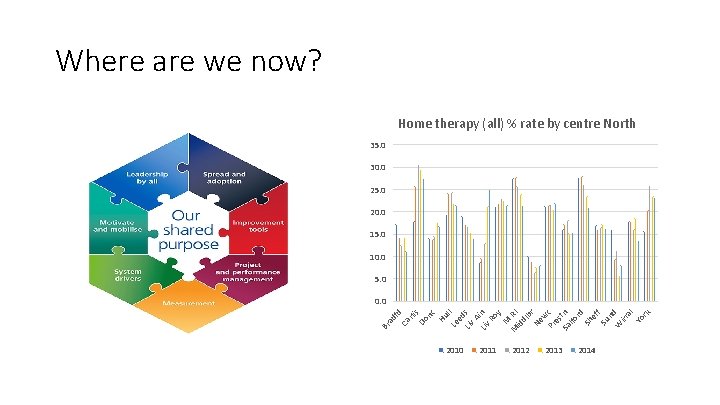
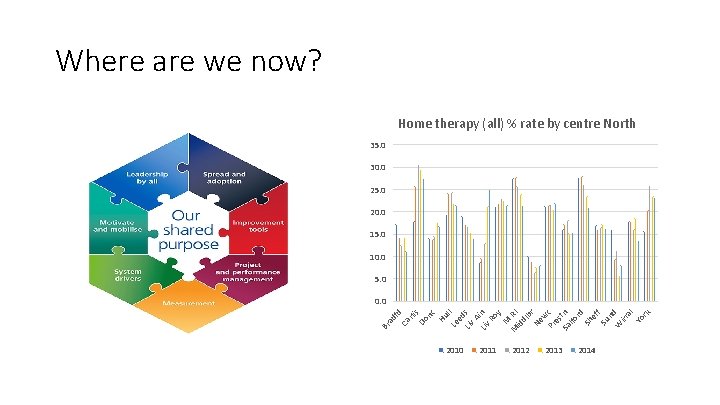
Where are we now? Home therapy (all) % rate by centre North 35. 0 30. 0 25. 0 20. 0 15. 0 10. 0 5. 0 Ca Br ad fd rli s Do nc Hu l Le l ed Liv s A Liv in Ro y M M RI id dl br Ne w Pr c es Sa tn lfo rd Sh ef f Su nd W irr al Yo rk 0. 0 2011 2012 2013 2014
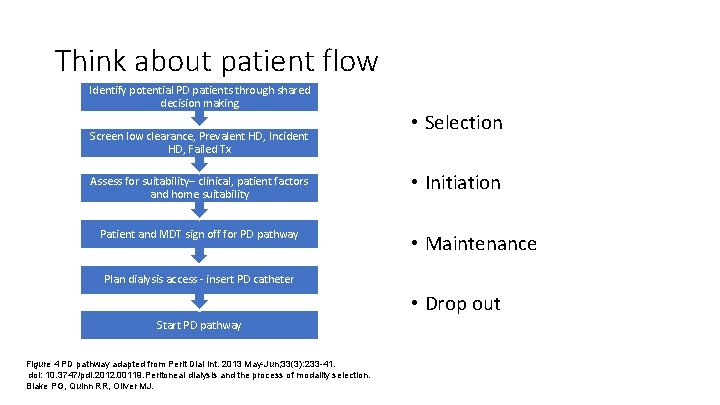
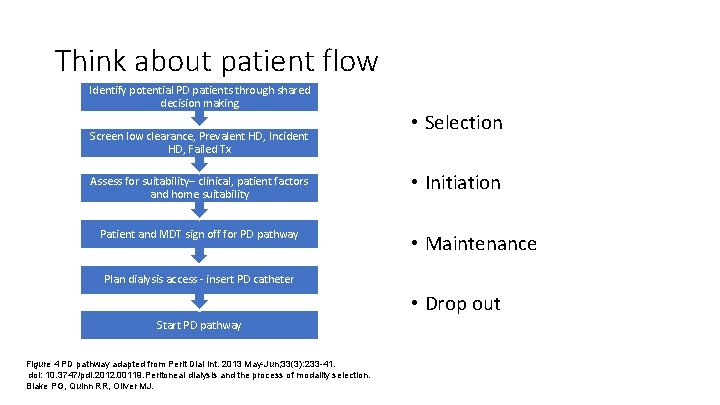
Think about patient flow Identify potential PD patients through shared decision making Screen low clearance, Prevalent HD, Incident HD, Failed Tx Assess for suitability– clinical, patient factors and home suitability Patient and MDT sign off for PD pathway • Selection • Initiation • Maintenance Plan dialysis access - insert PD catheter • Drop out Start PD pathway Figure 4 PD pathway adapted from Perit Dial Int. 2013 May-Jun; 33(3): 233 -41. doi: 10. 3747/pdi. 2012. 00119. Peritoneal dialysis and the process of modality selection. Blake PG, Quinn RR, Oliver MJ.

Project structure • ‘Co production’ – patients involved at the start and at every level • A regional team to coordinate the work, representative of the region • Each centre to form a project team • Support from KQu. IP • Project management, expertise, measurement
The project cycle • Research and discovery • Consider barriers and evidence • Consider solutions and ideas • Long list • Short list • Test ideas • Test, evaluate, share • Review and report then repeat process
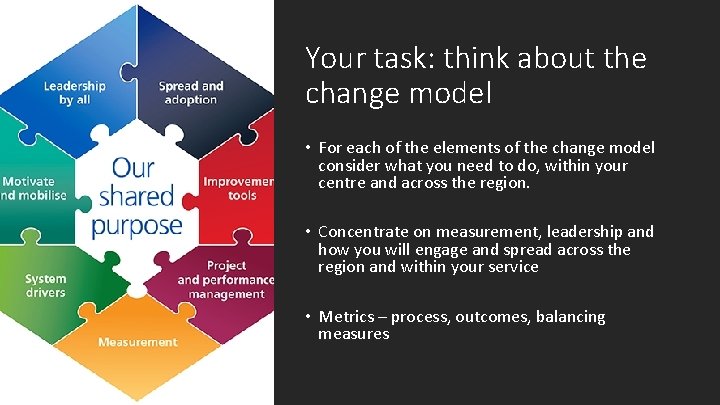
Your task: think about the change model • For each of the elements of the change model consider what you need to do, within your centre and across the region. • Concentrate on measurement, leadership and how you will engage and spread across the region and within your service • Metrics – process, outcomes, balancing measures

KQu. IP/UKRR Regional Day North West 12: 30 – 13. 20 § Group Work – Review of Home Therapies data locally

KQu. IP/UKRR Regional Day North West Group Work Questions for Consideration: § What is the data telling us, what works well and what are the important issue’s to address? § Do we need any more data? What are the barriers? § Have we any examples of interventions that worked and where is the evidence? § What are the next steps?

KQu. IP/UKRR Regional Day North West 13: 20 – 13: 50 § Feedback from each group
KQu. IP/UKRR Regional Day North West 13: 50 – 14: 20 Lunch and refreshments
 Day 1 day 2 day 3 day 4
Day 1 day 2 day 3 day 4 East south east wind direction
East south east wind direction West north west wind direction
West north west wind direction Day 1 day 2 day 817
Day 1 day 2 day 817 West midlands regional genetics laboratory
West midlands regional genetics laboratory North central texas regional certification agency
North central texas regional certification agency North american regional reanalysis
North american regional reanalysis Noord oost west zuid
Noord oost west zuid East is east and west is west
East is east and west is west Old west vs new west
Old west vs new west North, south east west leadership styles
North, south east west leadership styles North west rebellion timeline
North west rebellion timeline Dhis north west
Dhis north west North west end of life care model
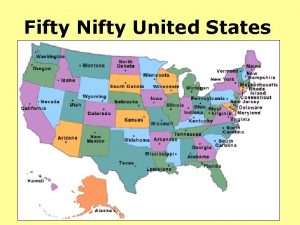
North west end of life care model 50 nifty united states
50 nifty united states North south east west in our calm objective opinion
North south east west in our calm objective opinion North east south west
North east south west North south east west leadership styles
North south east west leadership styles Swana
Swana The diagram shows two vectors that point west and north.
The diagram shows two vectors that point west and north. Jane mamelok gmc
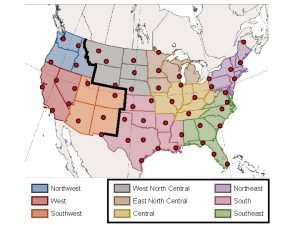
Jane mamelok gmc Map key
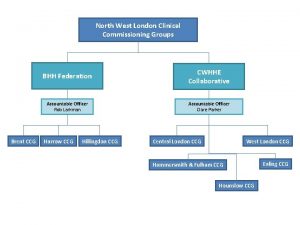
Map key North west london ccg
North west london ccg Cps north west
Cps north west West north east
West north east Department of public works and roads rustenburg
Department of public works and roads rustenburg Walsall rfc
Walsall rfc World map with latitude and longitude pdf
World map with latitude and longitude pdf North west recovery communities
North west recovery communities Western kenya union conference of sda
Western kenya union conference of sda Lines that run north and south
Lines that run north and south North west surrey ccg
North west surrey ccg The diagram shows
The diagram shows The north pole ____ a latitude of 90 degrees north
The north pole ____ a latitude of 90 degrees north True north vs magnetic north
True north vs magnetic north Cumbria and north east ics
Cumbria and north east ics