Diagnosis of Acute Appendicitis Jim Holliman M D



- Slides: 36
Diagnosis of Acute Appendicitis Jim Holliman, M. D. , F. A. C. E. P. Professor of Military and Emergency Medicine Uniformed Services University of the Health Sciences Clinical Professor of Emergency Medicine George Washington University Bethesda, Maryland, USA
Objectives ŸTo review the pathophysiology and clinical presentation of acute appendicitis ŸTo understand which patient groups are at high risk of misdiagnosis ŸTo discuss the use of laboratory and imaging studies in the diagnosis of acute appendicitis
Appendicitis Incidence & Complications Ÿ 6 % lifetime incidence Ÿ 69 % are ages 10 to 30 ŸUp to 30 % misdiagnosed initially Ÿ 20 to 30 % ruptured at surgery ŸMortality : 0. 1 to 0. 2 % unruptured, 3 to 5 % ruptured ŸSignificant morbidity
Anatomic Aspects ŸBlind pouch off of cecum ŸContains lymphoid tissue which peaks in adolescence, atrophies with age ŸFunction still unclear ŸAppendix can be anywhere within peritoneal cavity ŸOne study showed 65 % retrocecal, 31 % pelvic ŸReview of 70, 000 cases showed 4 % in RUQ, 0. 06 % LUQ, 0. 04 % LLQ

Pathophysiology of Appendicitis ŸLymphoid hyperplasia leads to luminal obstruction ŸOften follows viral illness ŸEpithelial cells secrete mucus ŸAppendix distends, bacteria multiply ŸVisceral pain begins an average of 17 hours after obstruction ŸIncreased pressure compromises blood supply ŸSomatic pain develops ŸAverage time to perforation = 34 hrs.
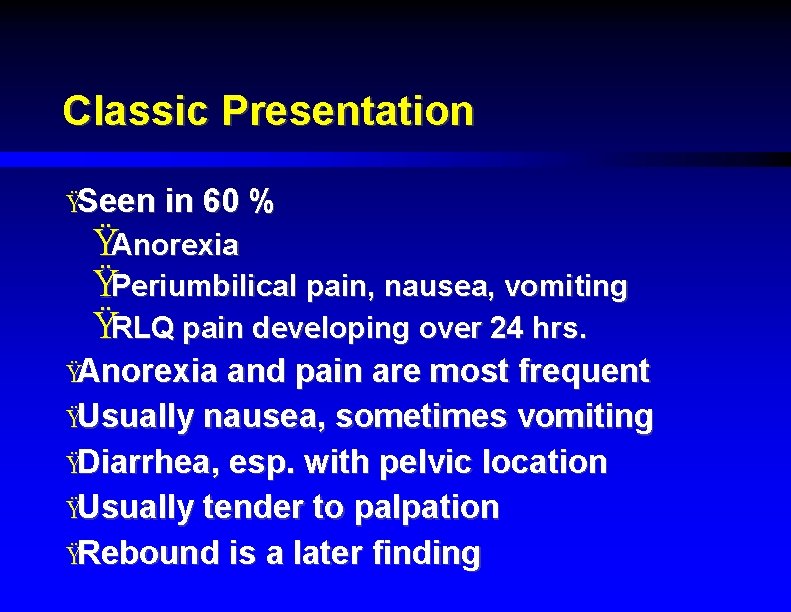
Classic Presentation ŸSeen in 60 % ŸAnorexia ŸPeriumbilical pain, nausea, vomiting ŸRLQ pain developing over 24 hrs. ŸAnorexia and pain are most frequent ŸUsually nausea, sometimes vomiting ŸDiarrhea, esp. with pelvic location ŸUsually tender to palpation ŸRebound is a later finding

Physical Exam ŸTenderness at Mc. Burney's point ŸCutaneous hyperesthesia in T 10 to 12 dermatomes ŸRovsing's sign ŸPsoas sign ŸObturator sign
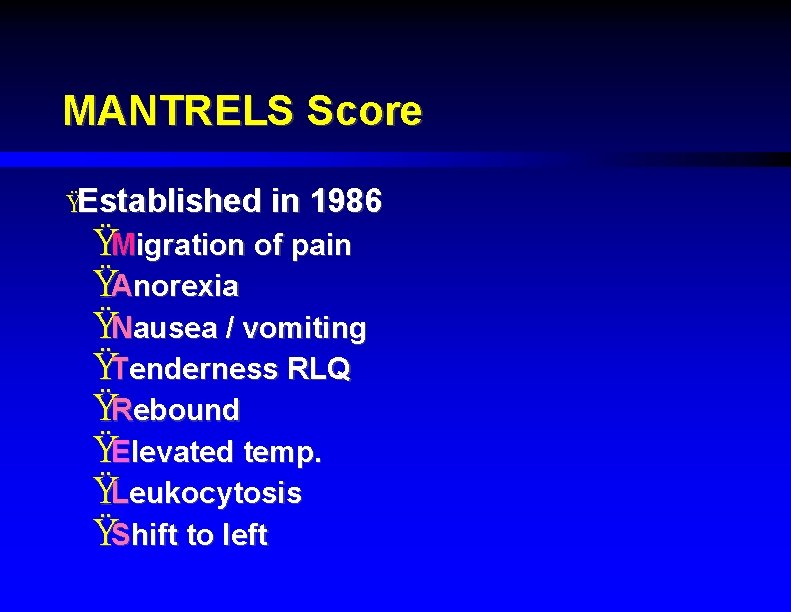
MANTRELS Score ŸEstablished in 1986 ŸMigration of pain ŸAnorexia ŸNausea / vomiting ŸTenderness RLQ ŸRebound ŸElevated temp. ŸLeukocytosis ŸShift to left
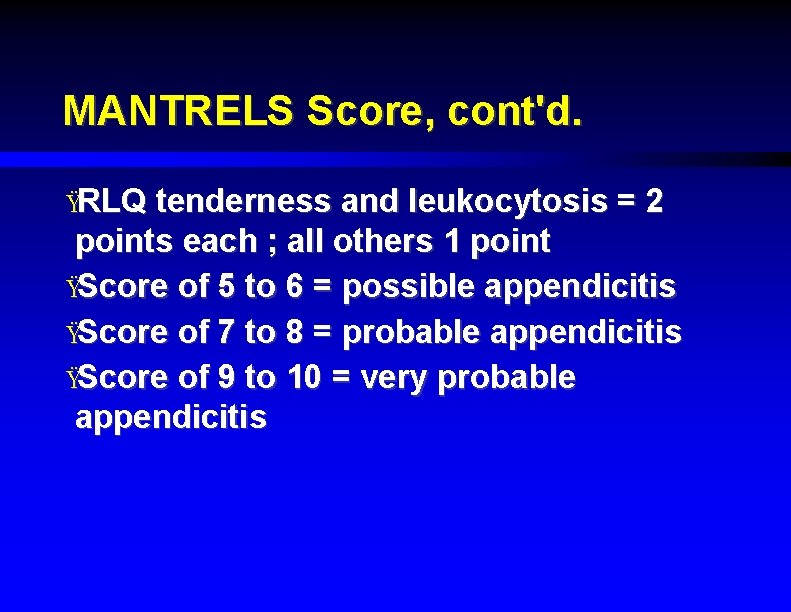
MANTRELS Score, cont'd. ŸRLQ tenderness and leukocytosis = 2 points each ; all others 1 point ŸScore of 5 to 6 = possible appendicitis ŸScore of 7 to 8 = probable appendicitis ŸScore of 9 to 10 = very probable appendicitis
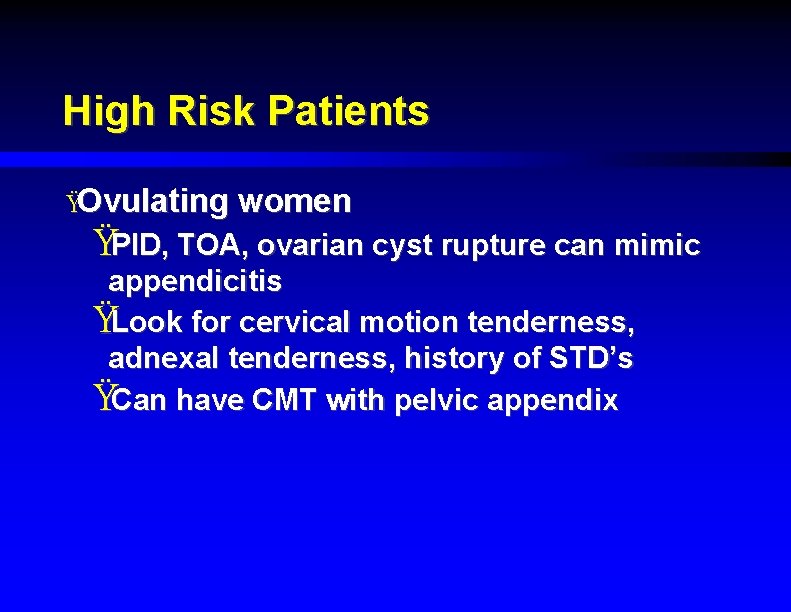
High Risk Patients ŸOvulating women ŸPID, TOA, ovarian cyst rupture can mimic appendicitis ŸLook for cervical motion tenderness, adnexal tenderness, history of STD’s ŸCan have CMT with pelvic appendix
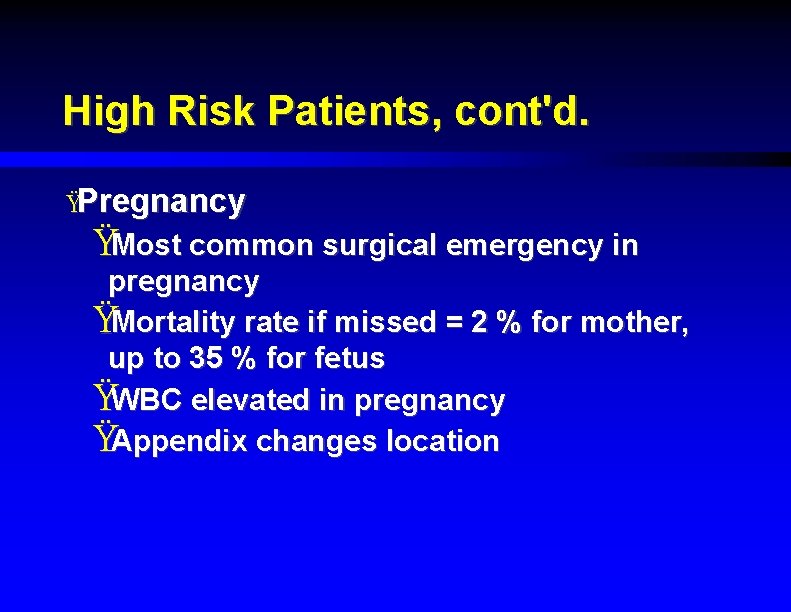
High Risk Patients, cont'd. ŸPregnancy ŸMost common surgical emergency in pregnancy ŸMortality rate if missed = 2 % for mother, up to 35 % for fetus ŸWBC elevated in pregnancy ŸAppendix changes location
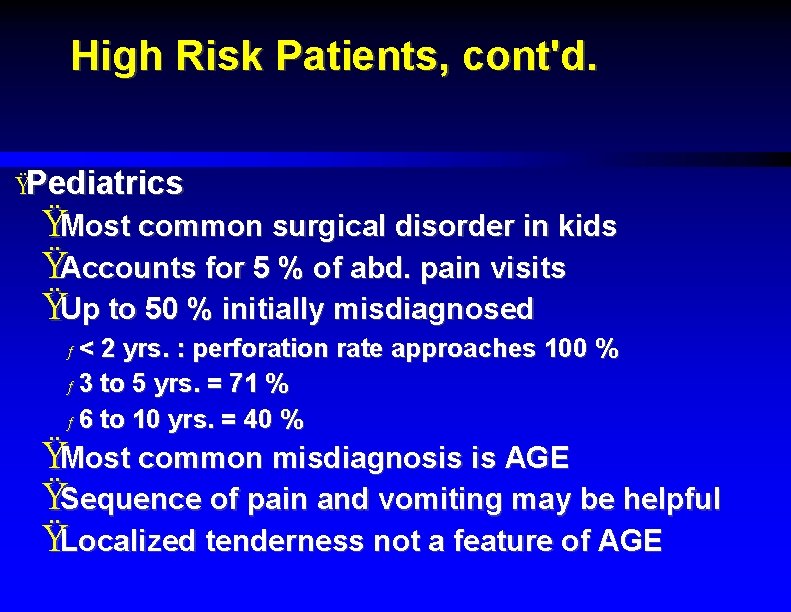
High Risk Patients, cont'd. ŸPediatrics ŸMost common surgical disorder in kids ŸAccounts for 5 % of abd. pain visits ŸUp to 50 % initially misdiagnosed ƒ< 2 yrs. : perforation rate approaches 100 % ƒ 3 to 5 yrs. = 71 % ƒ 6 to 10 yrs. = 40 % ŸMost common misdiagnosis is AGE ŸSequence of pain and vomiting may be helpful ŸLocalized tenderness not a feature of AGE
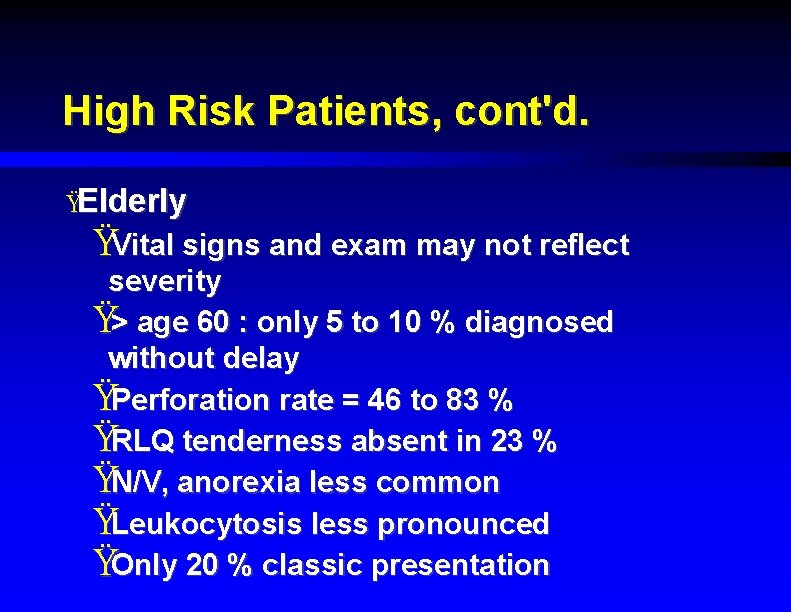
High Risk Patients, cont'd. ŸElderly ŸVital signs and exam may not reflect severity Ÿ> age 60 : only 5 to 10 % diagnosed without delay ŸPerforation rate = 46 to 83 % ŸRLQ tenderness absent in 23 % ŸN/V, anorexia less common ŸLeukocytosis less pronounced ŸOnly 20 % classic presentation
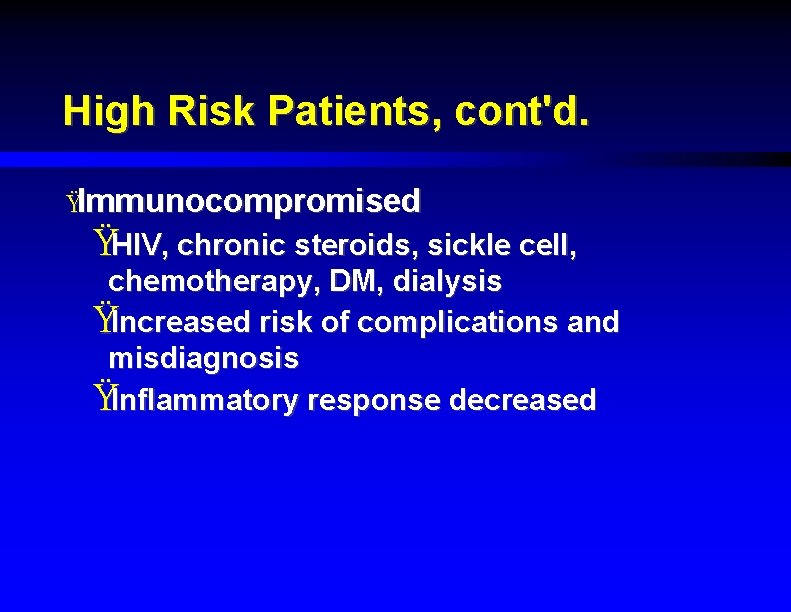
High Risk Patients, cont'd. ŸImmunocompromised ŸHIV, chronic steroids, sickle cell, chemotherapy, DM, dialysis ŸIncreased risk of complications and misdiagnosis ŸInflammatory response decreased
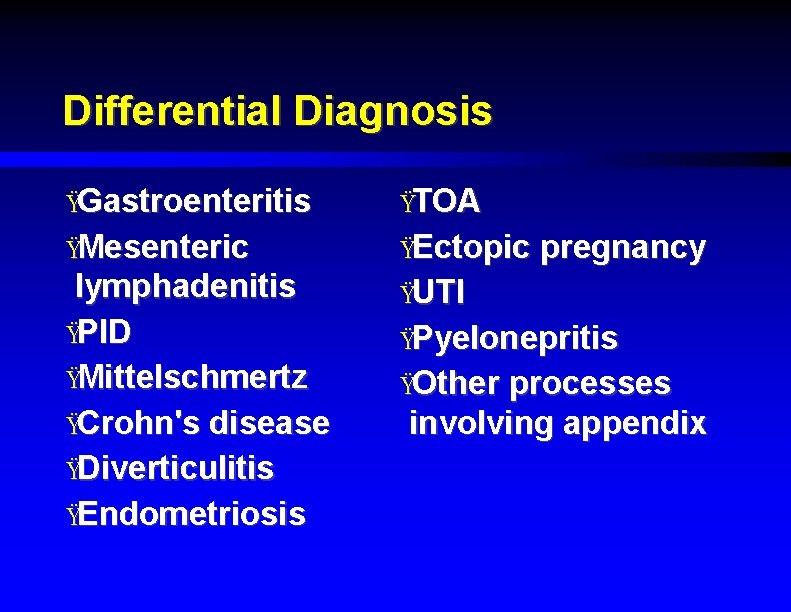
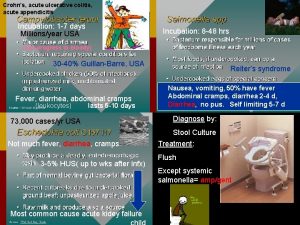
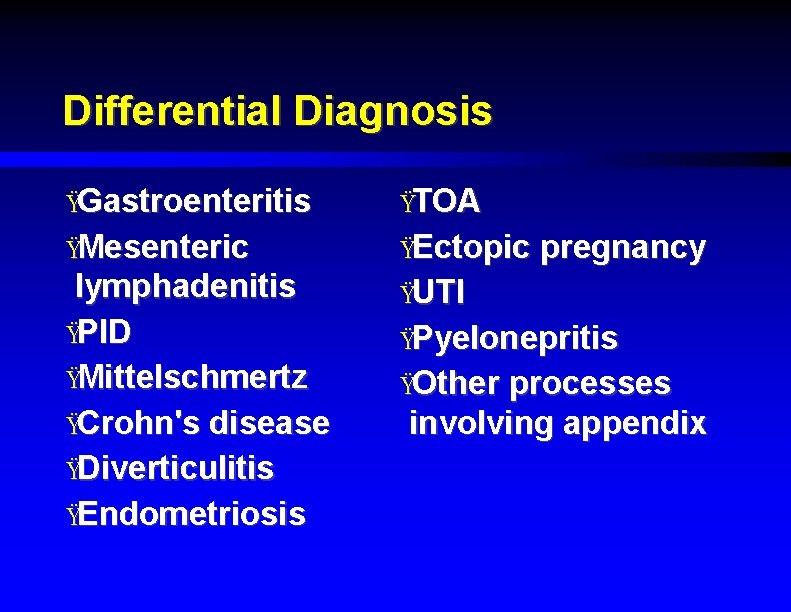
Differential Diagnosis ŸGastroenteritis ŸTOA ŸMesenteric ŸEctopic lymphadenitis ŸPID ŸMittelschmertz ŸCrohn's disease ŸDiverticulitis ŸEndometriosis ŸUTI pregnancy ŸPyelonepritis ŸOther processes involving appendix
" No single evaluation can substitute for the diagnostic accuracy of the experienced physician. "
Laboratory Studies ŸCBC Ÿ 75 to 85 % have elevated WBC, but it is nonspecific ŸWBC normal in 80 % in the first 24 hrs. ŸCan see elevated ANC in up to 89 % ŸWBC usually 12 to 18, 000 in appendicitis ŸChemistry panel ŸMay help with diagnosis of dehydration
Laboratory Studies, cont'd. ŸUrinalysis ŸSpecific gravity, ketones ŸCan see WBC’s, RBC’s, bacteria if inflamed appendix close to ureter Ÿ> 30 WBC’s = probable UTI ŸHCG ŸEssential in women of child-bearing age ŸCRP ŸAcute phase reactant
Imaging Studies ŸPlain films ŸLow sensitivity and specificity ŸAppendicolith specific, but seen in only 2 % ŸMay see local air-fluid levels, psoas obliteration, soft tissue mass, gas in appendix : all nonspecific
Imaging Studies, cont'd. ŸUltrasound Ÿ 75 to 90 % sensitive, 86 to 100 % specific ŸNoninvasive, low cost, but operatordependent ŸGood for diagnosing GYN disorders Ÿ 3 criteria for diagnosis ƒ Tender, noncompressible appendix ƒ No peristalsis of appendix ƒ Overall diameter > 6 mm
Imaging Studies, cont'd. ŸUltrasound (US) ŸAppendix may not be seen, due to obesity, guarding, bowel gas, perforation, retrocecal location Ÿ 2. 4 to 56 % of normal appendixes seen ŸOne study of 736 pediatric patients showed 36. 6 % without preop US had negative appendectomy vs. 9. 8 % who had US
Imaging Studies, cont'd. ŸUltrasound ŸStudy from Australia showed total WBC and neutrophil count were more accurate than US. They recommended pts. with unequivocal presentation go to OR. If equivocal, obtain CBC. If WBC > 15, 000, go to OR. If < 11, 000, obtain CT (US only in pregnancy).
Imaging Studies, cont'd. ŸCT ŸEarly studies showed low yield, but helical CT much more accurate ŸSensitivity 97 to 100 %, specificity 95 % (similar no matter what type or whether contrast is used) ŸOften shows alternative diagnosis ŸMore expensive, radiation exposure
Imaging Studies, cont'd. ŸCT ŸCriteria for appendicitis : ƒ Diameter > 6 mm ƒ Failure to completely fill with contrast or air ƒ Appendicolith ƒ Wall thickening or enhancement ŸOther contributory signs include fat stranding, fluid, inflammatory mass, adenopathy
Imaging Studies, cont'd. ŸCT ŸOne study showed negative laparotomy rates of 4 % in men, 8 % in ovulating women with CT (typical is 20 % and 45 % respectively), but no change in perforation rate ŸAnother study showed increase in CT use led to earlier diagnosis, less severe pathologic findings, and decreased length of stay
Imaging Studies, cont'd. ŸCT ŸStudy from Dept. of Surgery, Stamford, Connecticut : use of CT markedly increased from 1994 to 2000, without change in rate of negative appendectomy. They concluded use of CT by nonsurgeons leads to increased E. D. LOS without improving accuracy. They recommend mandatory surgical consult if CT considered.
Do We Need Imaging Studies? ŸLiterature conflicting ŸPediatric Imaging -Evidence-Based Guidelines ŸImaging most useful in clinically equivocal cases ŸCosts of imaging minor compared to cost of unnecessary surgery or delayed diagnosis ŸUS and CT both specific enough to rule in appendicitis, but only CT sensitive enough to rule it out

Do We Need Imaging Studies? ŸStudy from Austria Ÿ 350 patients divided into low, intermediate, and high probability ŸAll had US Ÿ 10 % of low prob. , 24 % of intermediate prob. , and 65 % of high prob. had appendicitis ŸSpecificity and sensitivity of US = 98 % ŸConcluded imaging should be done even in high probability patients
Do We Need Imaging Studies? ŸNEJM : Suspected Appendicitis Jan. 2003 ŸPatients with classic presentation should go to O. R. Diagnostic accuracy approaches 95 % ŸIf equivocal or suspect perforation : CT ŸUS reserved for pregnant women or high suspicion of GYN disease ŸIf study indeterminate, observe with repeated exams or laparoscopy
Analgesia ŸSir Zachary Cope's 1921 textbook of surgery said no way ŸProspective studies (both EM and Surgery literature) now show appropriate use of IV narcotics does not decrease diagnostic accuracy, and may improve exam
Analgesia, cont'd. ŸJournal of American College of Surgeons : Jan. 2003 ŸProspective, randomized, double blind study ŸAdults with abd. pain got up to 15 mg morphine vs. placebo ŸIncreased pain relief, with no change in diagnostic accuracy ŸNot all surgeons read their own literature, so give them a chance to come in a reasonable time frame or give the meds
Risk Management ŸMisdiagnosis of appendicitis = 5 th leading cause of successful litigation against EPs Ÿ 7 features of misdiagnosed cases : ŸNo nausea / vomiting ŸLack of distress ŸNo rebound ŸNo guarding ŸNo rectal exam (controversial) ŸNarcotic pain meds given ŸDiagnosis of acute gastroenteritis
Risk Management, cont'd. ŸWhen discharging, stress unclear diagnosis, what to watch for ŸFollow up in 12 hours (PMD or E. D. ) ŸCan always observe if unsure Ÿ"When in doubt, don't send them out. "
Summary ŸAppendicitis is a common surgical emergency with a varied clinical presentation ŸSeveral patient groups are at high risk of misdiagnosis ŸLab and imaging studies are helpful, but no single study is a substitute for good clinical judgement
 Jim holliman
Jim holliman Clupeotoxin
Clupeotoxin Crohn’s disease
Crohn’s disease O que é isso
O que é isso Acute suppurative appendicitis
Acute suppurative appendicitis 4 stages of appendicitis
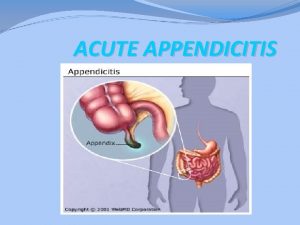
4 stages of appendicitis Acute appendicitis
Acute appendicitis Nanda nursing diagnosis for appendicitis
Nanda nursing diagnosis for appendicitis Acute pancreatitis diagnosis criteria
Acute pancreatitis diagnosis criteria Acute productive cough differential diagnosis
Acute productive cough differential diagnosis Post traumatic stress disorder
Post traumatic stress disorder Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Types of nursing diagnoses
Types of nursing diagnoses Steps of nursing process
Steps of nursing process Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Appendix definition
Appendix definition Interspinalis sík
Interspinalis sík How do you confirm appendicitis
How do you confirm appendicitis Fecolit
Fecolit Avogadro's score for appendicitis
Avogadro's score for appendicitis Anatomy and physiology of appendicitis
Anatomy and physiology of appendicitis Appendicitis maneuvers
Appendicitis maneuvers Ceftriaxone and metronidazole for appendicitis
Ceftriaxone and metronidazole for appendicitis Ziehl neelsen
Ziehl neelsen 4 stages of appendicitis
4 stages of appendicitis Referred pain from appendicitis
Referred pain from appendicitis Abdomen quadrants organs
Abdomen quadrants organs Appendicitis anamnese
Appendicitis anamnese Classification of appendicitis
Classification of appendicitis What is the pathophysiology of appendicitis?
What is the pathophysiology of appendicitis? Appendicular infiltrate
Appendicular infiltrate Mantrels score
Mantrels score Ranson criteria for acute pancreatitis
Ranson criteria for acute pancreatitis Accs em
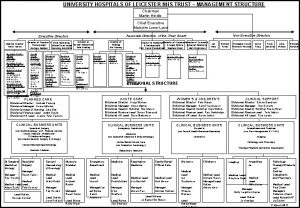
Accs em Uhl management structure
Uhl management structure Vertical angles
Vertical angles