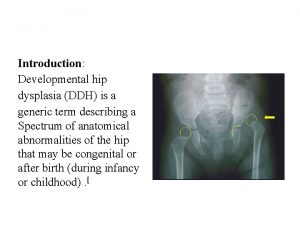
Developmental dysplasia of the hip DDH Developmental dysplasia

- Slides: 28
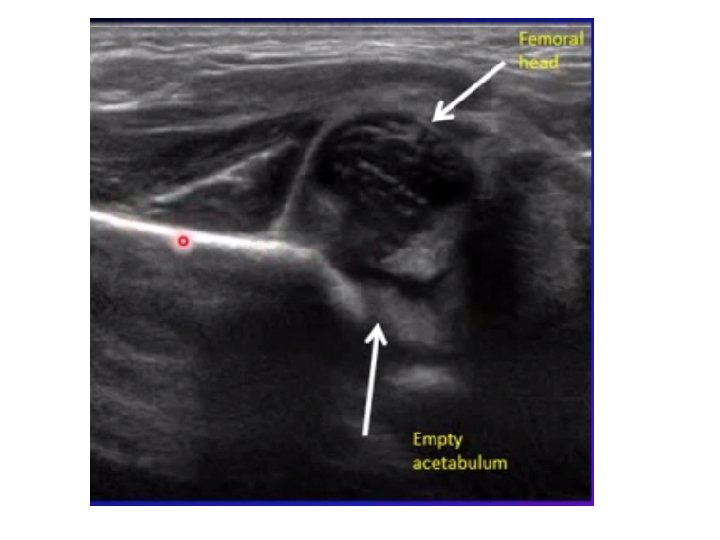
Developmental dysplasia of the hip (DDH) • Developmental dysplasia (abnormal development) of the hip refers to a variety of conditions where the femoral head and the acetabulum are improperly aligned. Previously known as congenital dislocation. Occur as a result of abnormal development of the hips during fetal development, more in female than male. • These conditions include dislocation (displacement of the bone from its normal position in a joint), subluxation (partial dislocation), and acetabular dysplasia.
• Etiology: • 1) Hormonal: around the time of delivery, hormones in the mother cause ligaments around her birth passage (pelvis) to relax, to make it easier for the baby to pass through her pelvis during birth. These hormones may pass through the placenta to the baby and cause the ligaments around the baby's joints to relax, making the baby's hip joint less stable. • 2) Mechanical factors such as breech positioning or the presence of oligohydramnios • 3) Genetic factors (the problem is more common in some families).
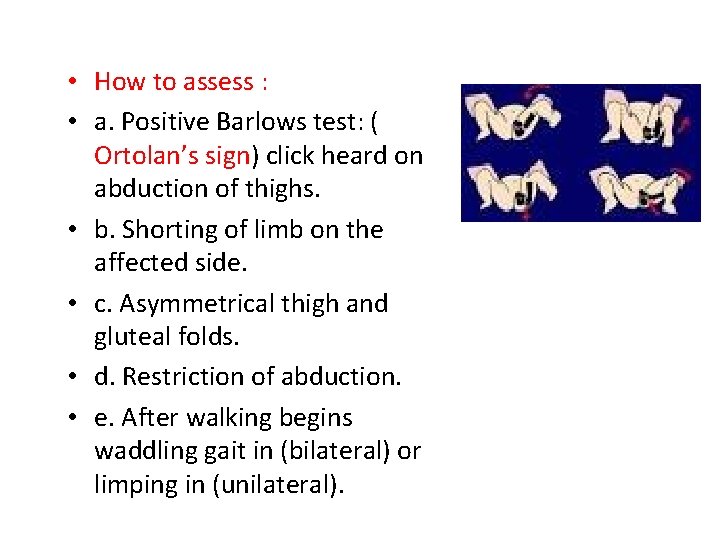
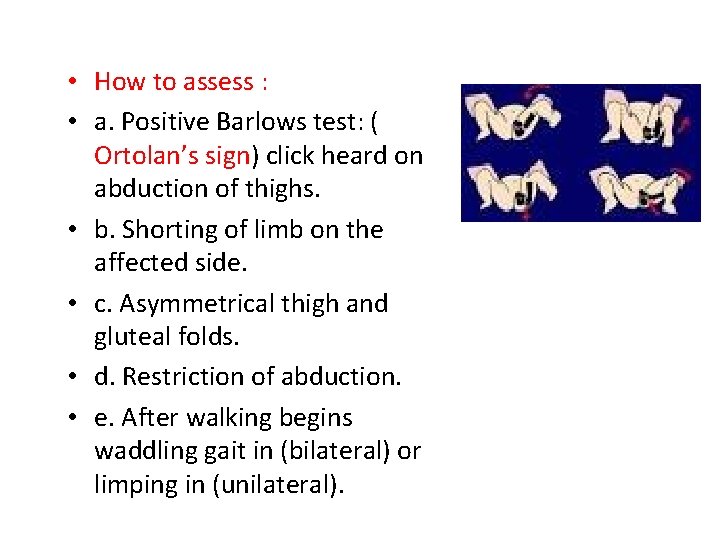
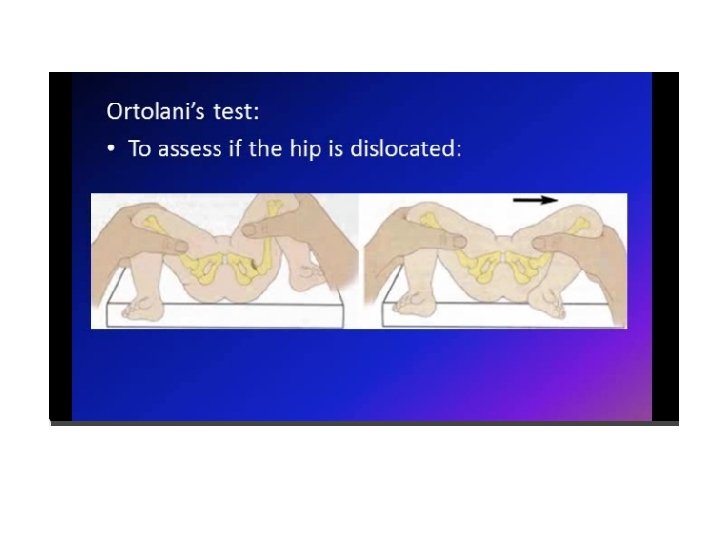
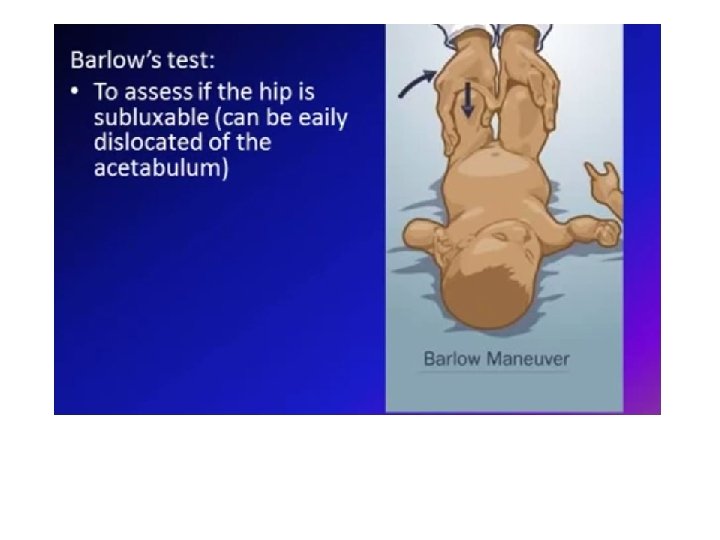
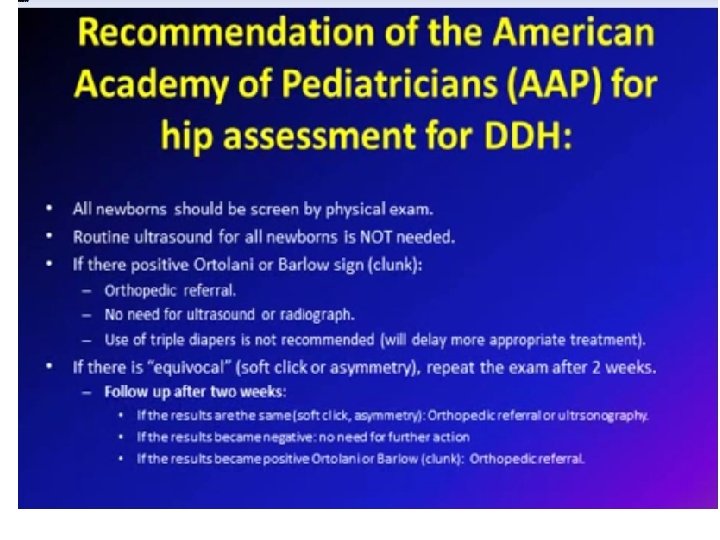
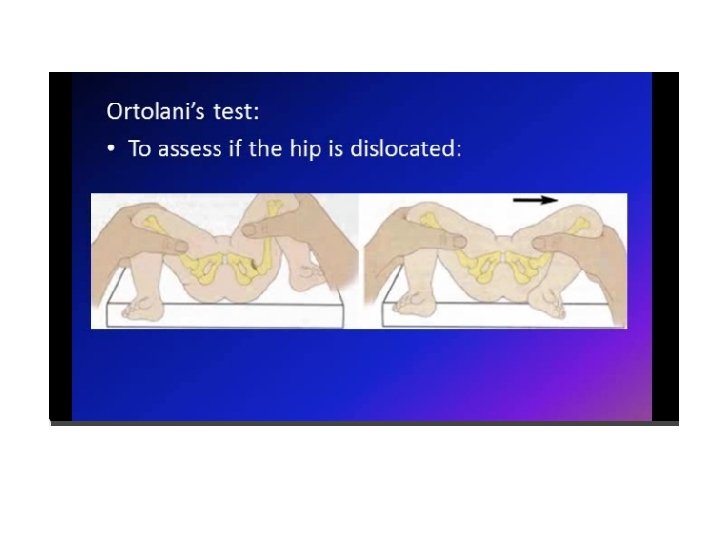
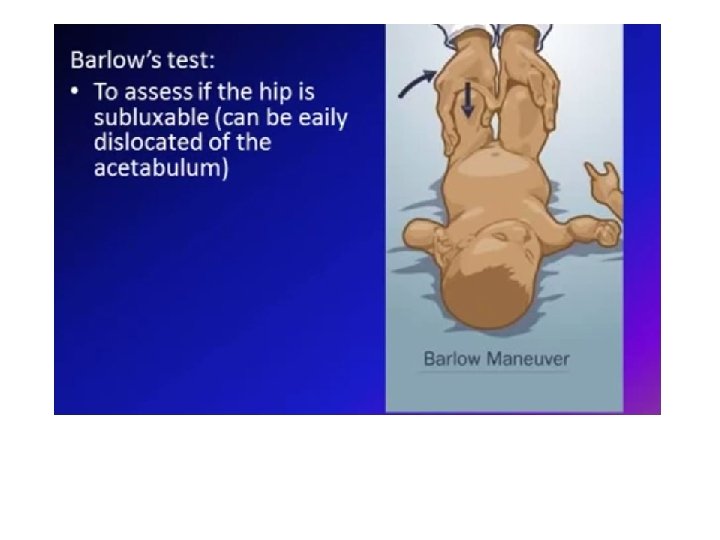
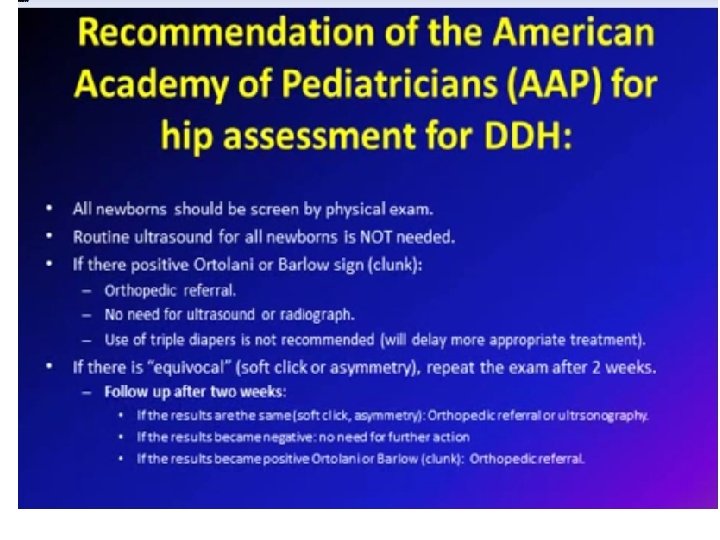
• How to assess : • a. Positive Barlows test: ( Ortolan’s sign) click heard on abduction of thighs. • b. Shorting of limb on the affected side. • c. Asymmetrical thigh and gluteal folds. • d. Restriction of abduction. • e. After walking begins waddling gait in (bilateral) or limping in (unilateral).

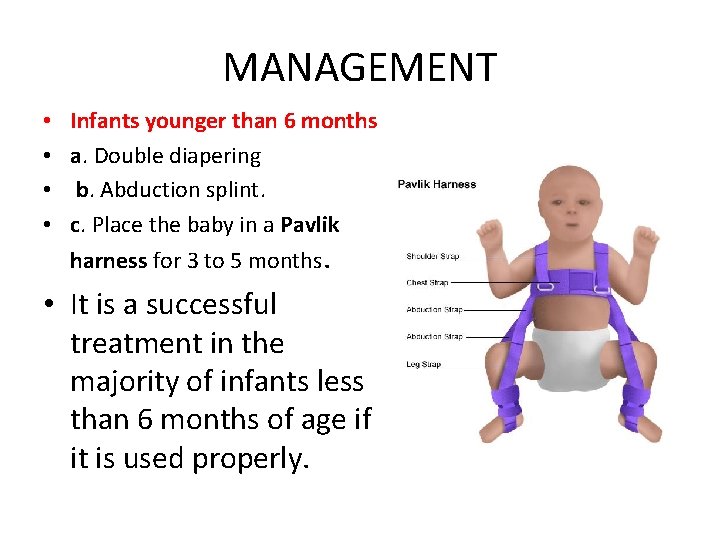
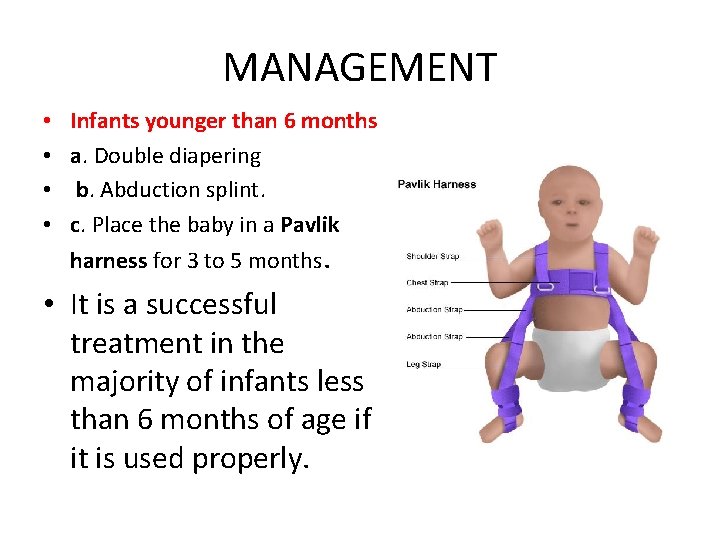
MANAGEMENT • • Infants younger than 6 months a. Double diapering b. Abduction splint. c. Place the baby in a Pavlik harness for 3 to 5 months. • It is a successful treatment in the majority of infants less than 6 months of age if it is used properly.
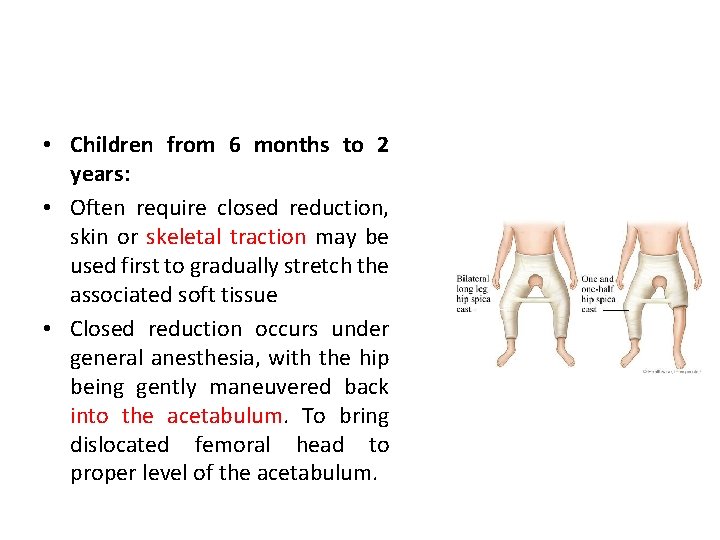
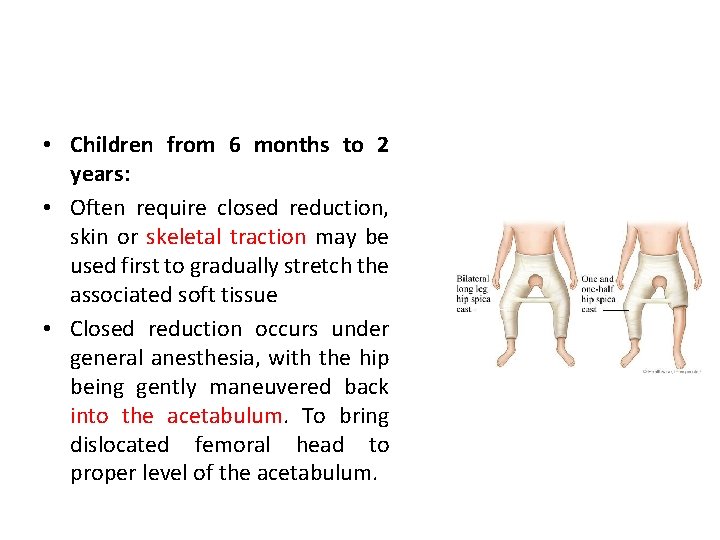
• Children from 6 months to 2 years: • Often require closed reduction, skin or skeletal traction may be used first to gradually stretch the associated soft tissue • Closed reduction occurs under general anesthesia, with the hip being gently maneuvered back into the acetabulum. To bring dislocated femoral head to proper level of the acetabulum.
• A spica cast worn for 12 weeks maintains reduction of the hip. The hip spica cast immobilizes the legs and knees and holds the hips in proper alignment. • After the cast is removed, the child must wear an abduction brace full-time (except for baths) for 2 months. Then the brace is worn at night and during naps until development of the acetabulum is normal.
• Children over 2 years • Surgical reduction followed by a period of casting of age or those who have failed to respond to • prior treatment.
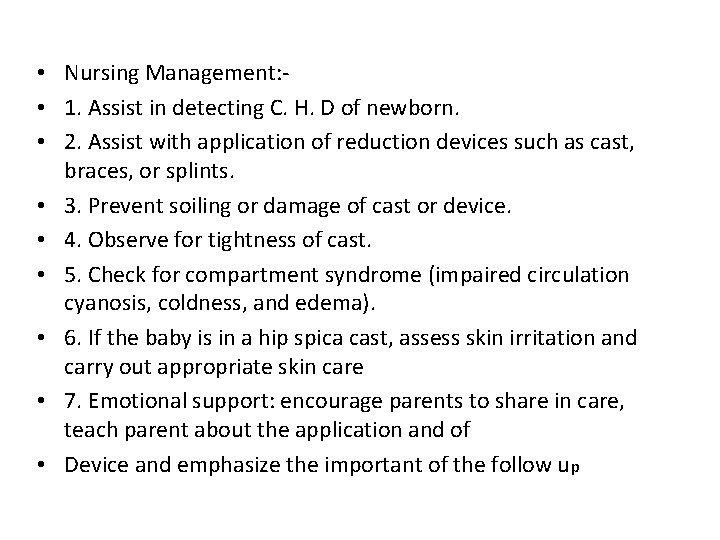
• Nursing Management: • 1. Assist in detecting C. H. D of newborn. • 2. Assist with application of reduction devices such as cast, braces, or splints. • 3. Prevent soiling or damage of cast or device. • 4. Observe for tightness of cast. • 5. Check for compartment syndrome (impaired circulation cyanosis, coldness, and edema). • 6. If the baby is in a hip spica cast, assess skin irritation and carry out appropriate skin care • 7. Emotional support: encourage parents to share in care, teach parent about the application and of • Device and emphasize the important of the follow up
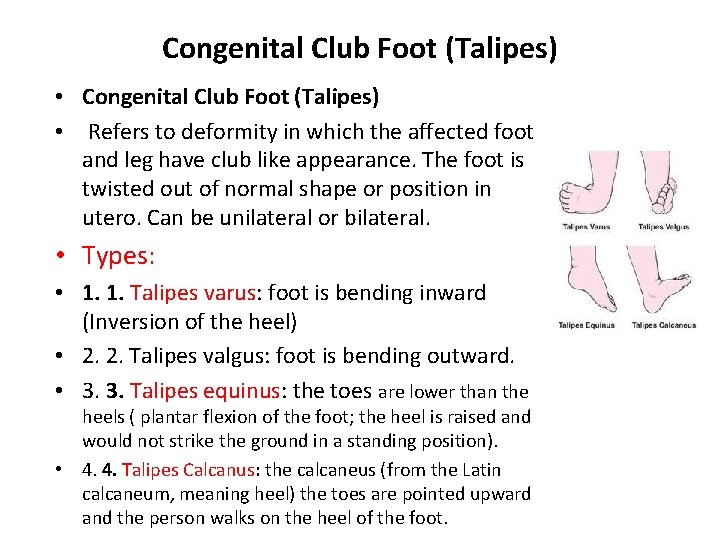
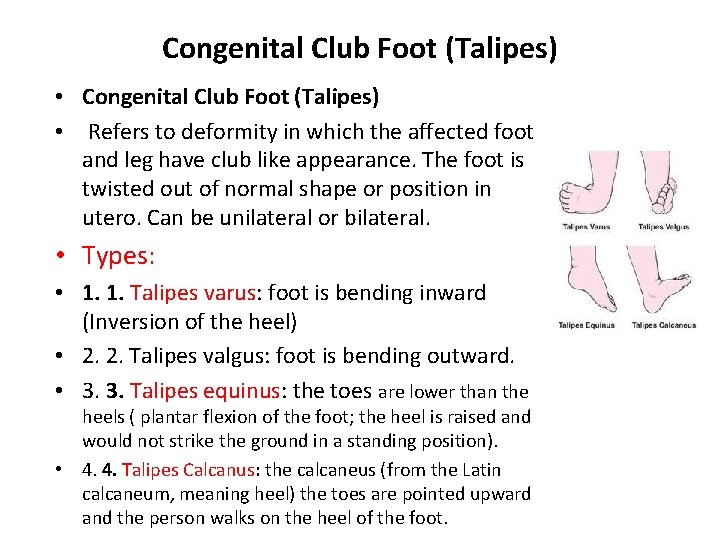
Congenital Club Foot (Talipes) • Refers to deformity in which the affected foot and leg have club like appearance. The foot is twisted out of normal shape or position in utero. Can be unilateral or bilateral. • Types: • 1. 1. Talipes varus: foot is bending inward (Inversion of the heel) • 2. 2. Talipes valgus: foot is bending outward. • 3. 3. Talipes equinus: the toes are lower than the heels ( plantar flexion of the foot; the heel is raised and would not strike the ground in a standing position). • 4. 4. Talipes Calcanus: the calcaneus (from the Latin calcaneum, meaning heel) the toes are pointed upward and the person walks on the heel of the foot.
• Causes: • 1. Familial: Occur more in families who have affected child. • 2. Congenital that occurs in utero due to adverse effects of medication, infection, or genetic trait resulting in contracture of soft tissue and abnormal development of a joint and muscles.
• Medical Management: • 1. Passive stretching exercises: manipulate the foot into the abnormal position, 3 - 4 times for 10 - 15 minutes each. • 2. Casting. L: application from toes to the knee (for 3 - 6 wks) • 3. Special shoes or splint (Denis Browne splint) to maintain correction of the foot.
• Deformities of the spine • Refers to deformities of the spine which affect the surrounding skeletal and soft tissue structures. Its assumes one of the three types: • 1. Scoliosis: rotary lateral curvature of the spine. • 2. Kyphosis: abnormally increased convex angle in the curvature of the thoracic spine. • 3. Lordosis: abnormally increased concave angle in the lumbar spine. • Scoliosis, the most common spinal deformity in children, involves lateral curvature greater than 20 degrees, spinal rotation, rib asymmetry, and thoracic hypokyphosis
• Clinical manifestations include • Not painful visible curve of the spine, posterior rib hump when bending forward, asymmetrical rib cage, and uneven shoulder. • Caregivers may notice that the child’s clothes do not fit properly, unequal leg length and the child seems to lean to one side.
• Treatments • Up to 20 -degree curvature: Exercise to enhance muscle tone and posture. • Between 20 and 40 degree curvature: Apply a brace to maintain curvature. Bracing is intended to prevent progression of the curve but does not correct the current curve. • Greater than 40 degree curvature: Spinal fusion surgery. • Nursing Interventions: If spinal fusion surgery is performed • Reposition the child every 2 hours to inhibit development of pressure sores and to adequately inflate lungs and monitor vital signs following surgery. • Assess for Homan sign for signs of an embolism and apply anti-embolism stockings while the patient is on bed rest. Remove the anti-embolism stocking for 1 hour three times a day. • Assess the patient’s pain level.
• Juvenile rheumatoid arthritis (JRA) • �It is an autoimmune disease that causes chronic inflammation of connective tissue and joints resulting in swelling, pain, and limited motion. There are two peak ages of onset between 1 and 3 years and between 8 and 10 years of age. • �The synovial membrane becomes inflamed, called synovitis, resulting in increased fluid, lymphocytes, and plasma in the joint, which causes the joint to swell. The joint can erode and deform over time resulting in bone loss, osteoporosis, subluxation, and ankylosis. • �There are three types of JRA: • 1. Oligoarticular: This affects fewer than five joints and might exhibit inflammation of the iris without joint symptoms. • 2. Polyarticular: This affects the small joints of the hands and weight bearing joints. • 3. Systemic: This affects the entire body resulting in high fever that suddenly drops to normal. A rash may appear and then suddenly disappear.
• Signs and Symptoms • • 1. Irritability, high fever and rash 2. Poor appetite and mild growth delay 3. Changes in gait and poor weight gain 4. Flex position at rest • Test Results • �Increased erythrocyte sedimentation rate (ESR). • �Positive rheumatoid factor (RF) in serum. • �Positive immunoglobulin (Ig) G and Ig. M present in serum.
• Treatments • Administer nonsteroidal antiinflammatory drugs (NSAIDs) and slow-acting anti-rheumatic drugs (SAARDS) such as methotrexate to suppress the autoimmune response. • Administeroids if other treatments fail. Steroids reduce inflammation but have adverse side effects with long-term use. • Physical therapy to ensure safety ambulation.
THANKS A LOT
 Barlow ortolani test
Barlow ortolani test Hip and elbow dysplasia
Hip and elbow dysplasia Ppt
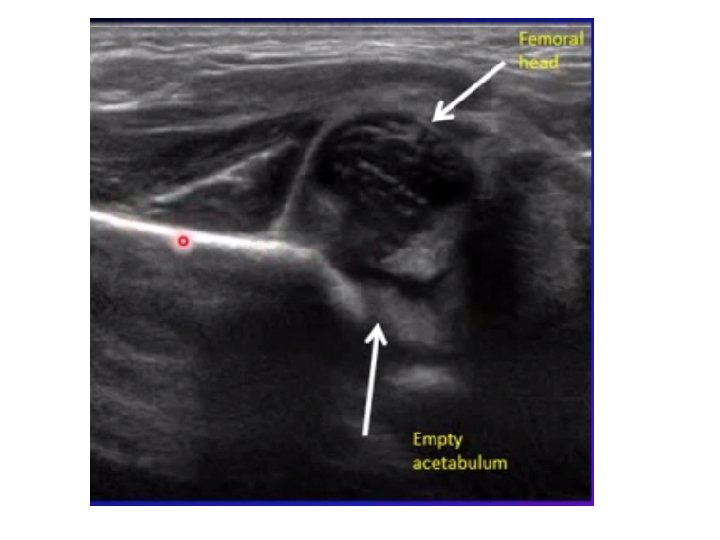
Ppt Infant hip
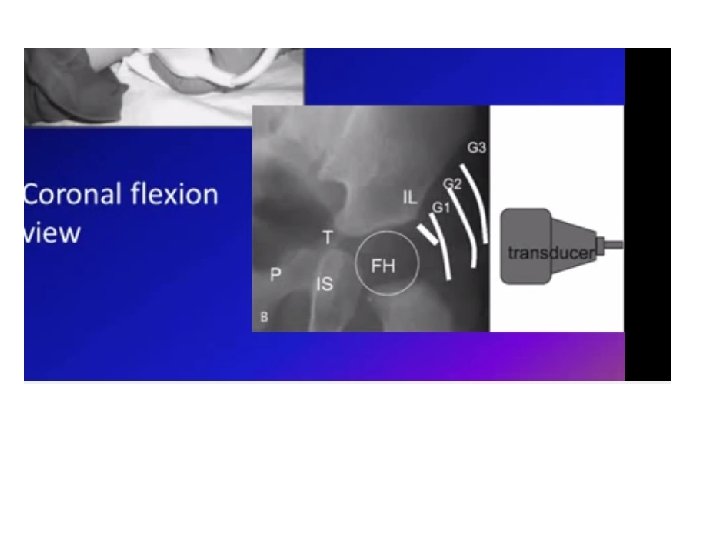
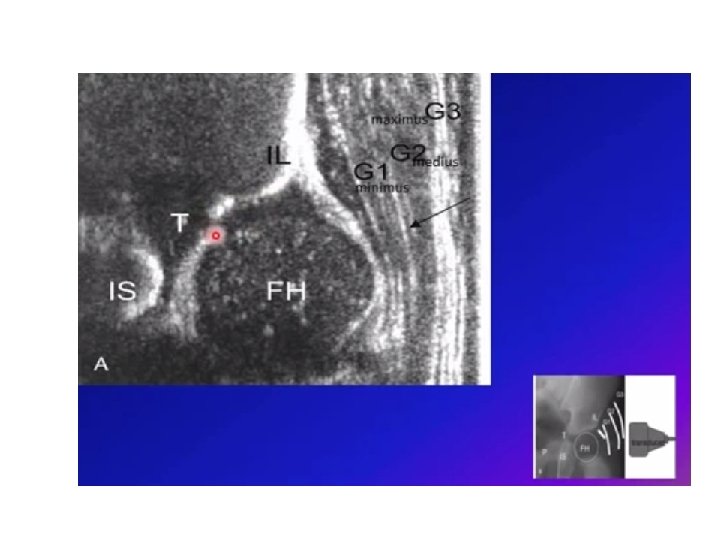
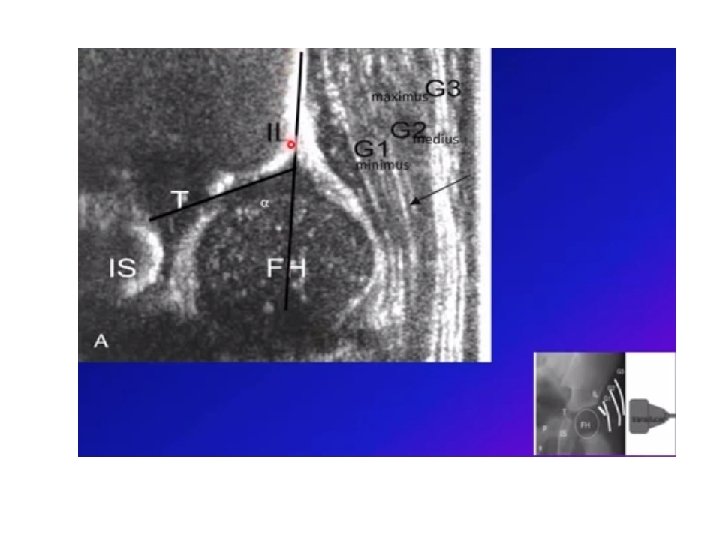
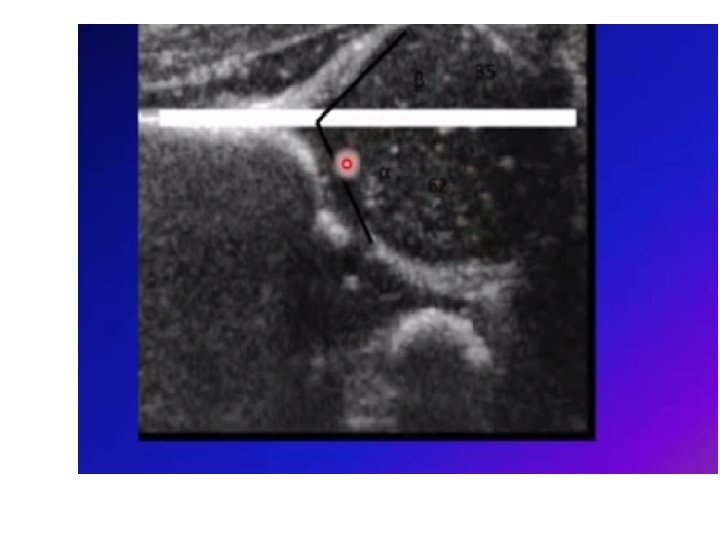
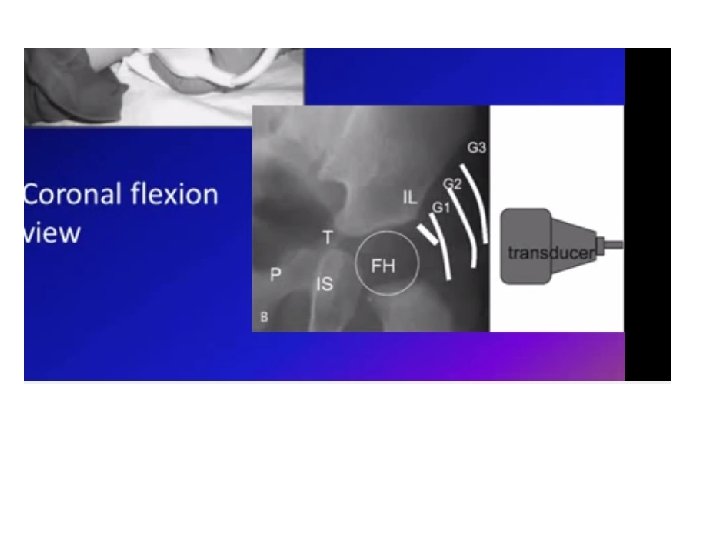
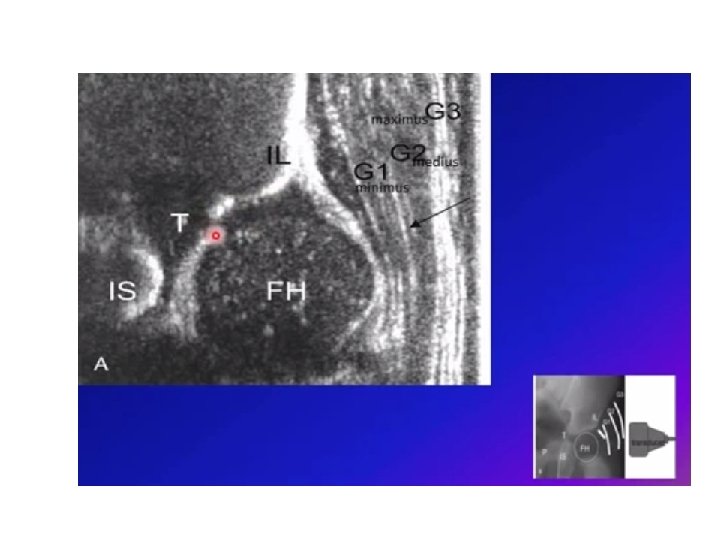
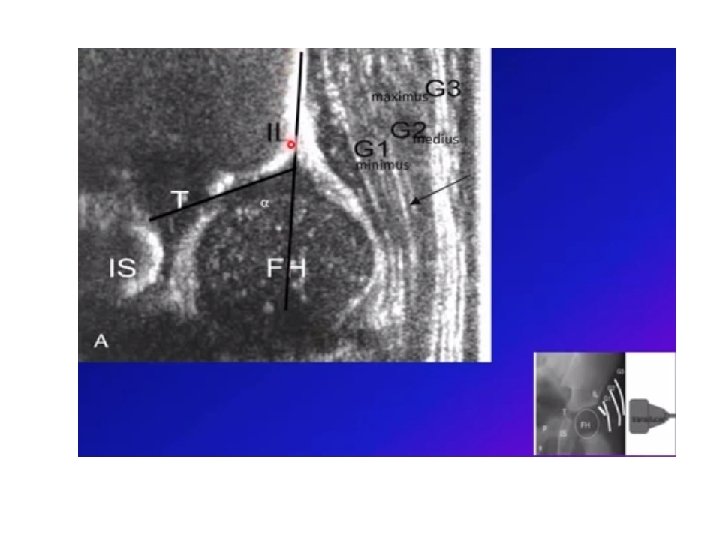
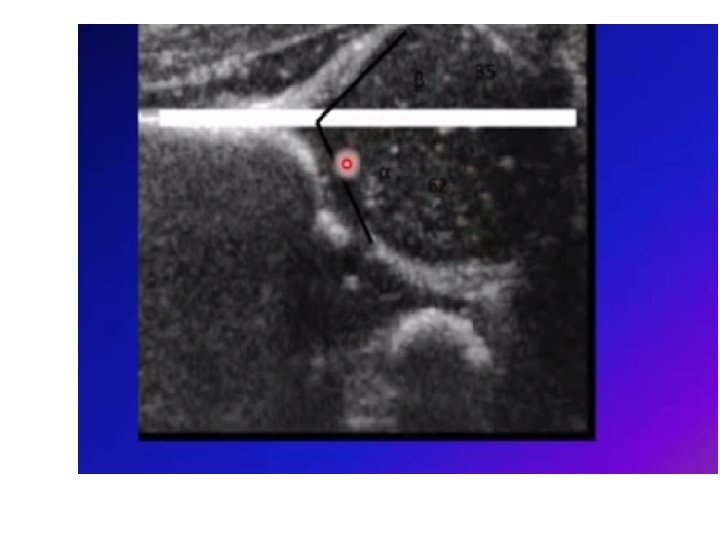
Infant hip Hip dysplasia alpha angle
Hip dysplasia alpha angle Hip hop hip to the hippity
Hip hop hip to the hippity Hip to the hop to the hippity hop
Hip to the hop to the hippity hop Von rosen splint
Von rosen splint Alpha and beta angle in ddh
Alpha and beta angle in ddh Ddh
Ddh Hip spica cast
Hip spica cast Periapical granuloma vs abscess
Periapical granuloma vs abscess Renal dysplasia
Renal dysplasia Supernumeray
Supernumeray Epidermal dysplasia verruciformis
Epidermal dysplasia verruciformis Epithelial dysplasia
Epithelial dysplasia Osmf differential diagnosis
Osmf differential diagnosis Osteofytes
Osteofytes Dog kidney
Dog kidney Prof dr emine şen
Prof dr emine şen Epithelial dysplasia
Epithelial dysplasia Ununited anconeal process
Ununited anconeal process Diastrophic dysplasia
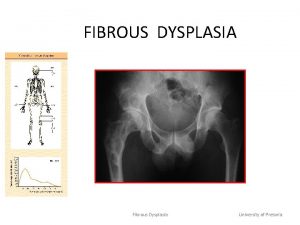
Diastrophic dysplasia Ground glass appearance fibrous dysplasia
Ground glass appearance fibrous dysplasia Thalassemia autosomal recessive
Thalassemia autosomal recessive Thẻ vin
Thẻ vin Thể thơ truyền thống
Thể thơ truyền thống Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu