Development of the Respiratory System and Diaphragm Matt
- Slides: 31
Development of the Respiratory System and Diaphragm Matt Velkey jvelkey@umich. edu 454 D Davison Reading: Langman’s Ch. 11 (pp. 155 -164) and Ch. 13 (pp. 201 -207)
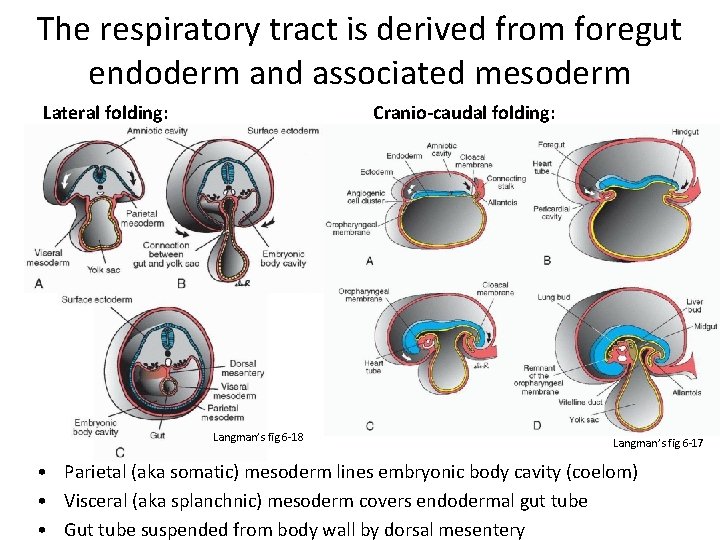
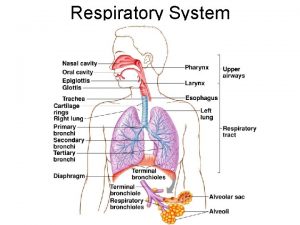
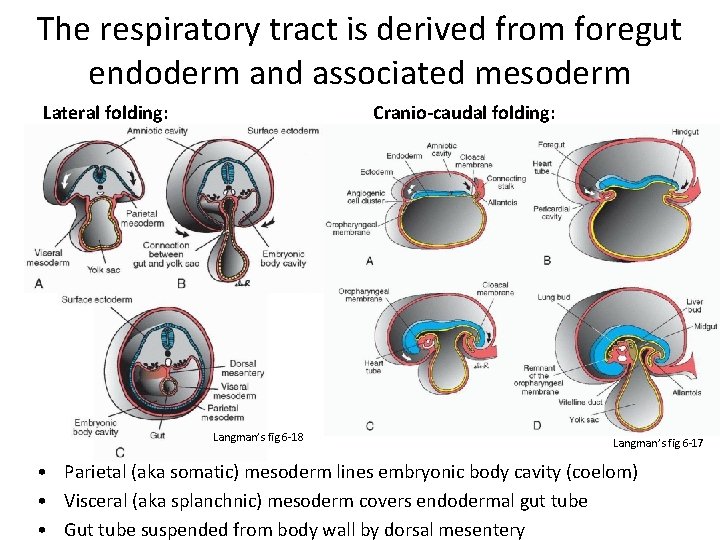
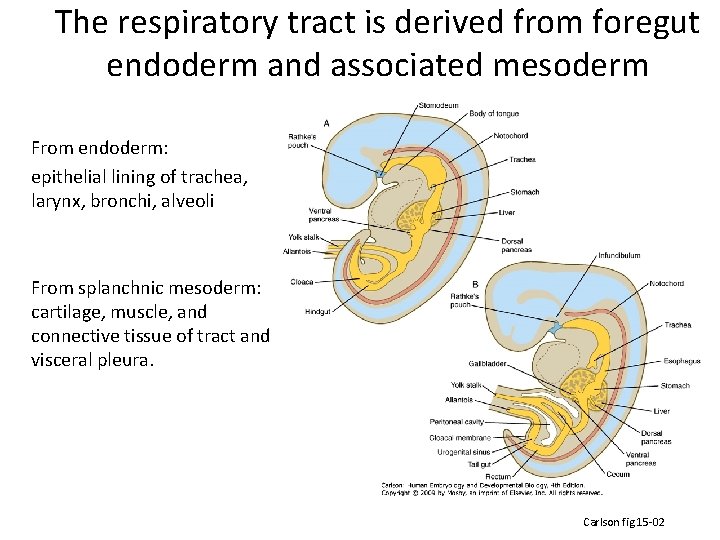
The respiratory tract is derived from foregut endoderm and associated mesoderm Lateral folding: Cranio-caudal folding: Langman’s fig 6 -18 Langman’s fig 6 -17 • Parietal (aka somatic) mesoderm lines embryonic body cavity (coelom) • Visceral (aka splanchnic) mesoderm covers endodermal gut tube • Gut tube suspended from body wall by dorsal mesentery
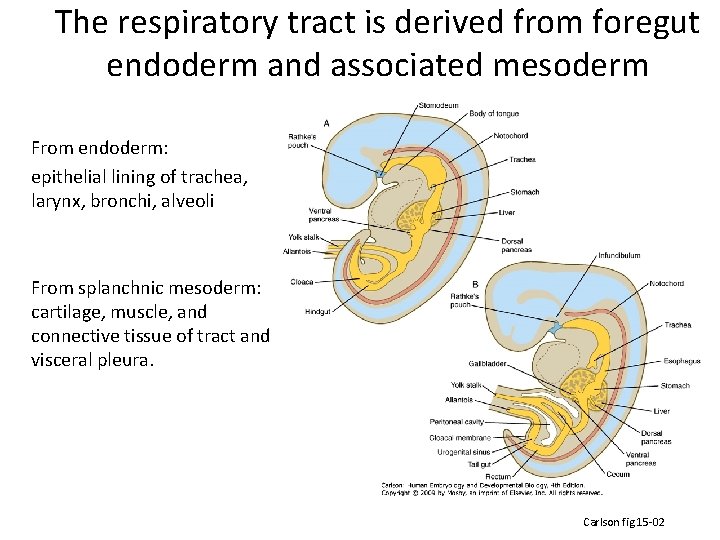
The respiratory tract is derived from foregut endoderm and associated mesoderm From endoderm: epithelial lining of trachea, larynx, bronchi, alveoli From splanchnic mesoderm: cartilage, muscle, and connective tissue of tract and visceral pleura. Carlson fig 15 -02
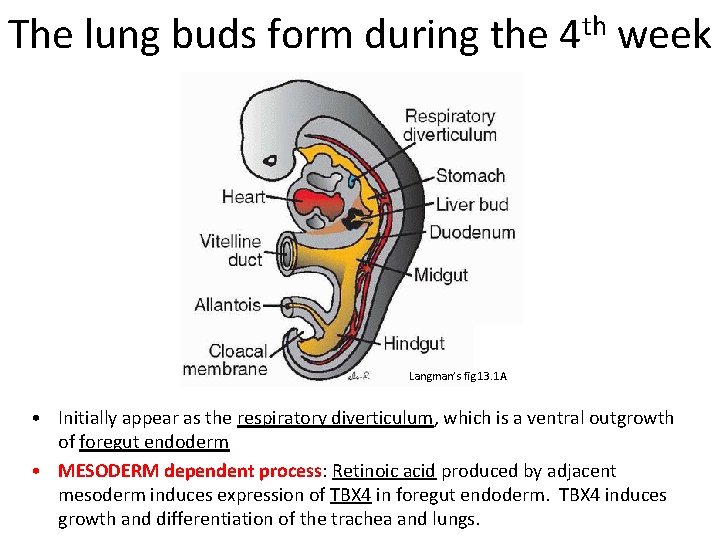
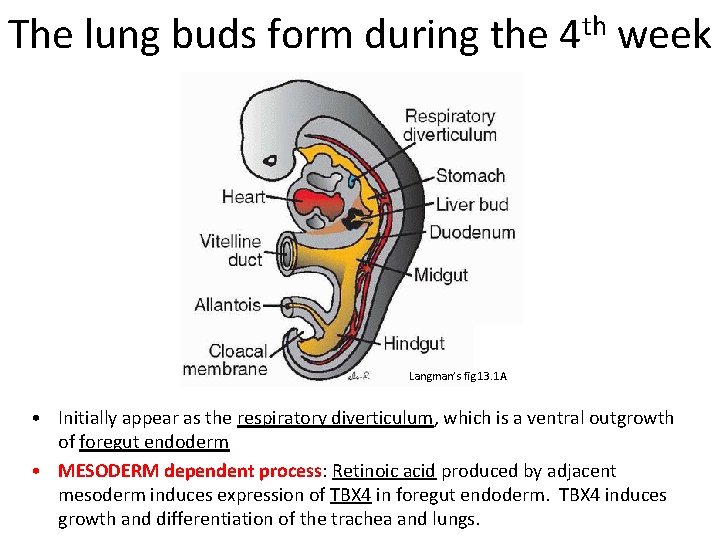
The lung buds form during the 4 th week Langman’s fig 13. 1 A • Initially appear as the respiratory diverticulum, which is a ventral outgrowth of foregut endoderm • MESODERM dependent process: Retinoic acid produced by adjacent mesoderm induces expression of TBX 4 in foregut endoderm. TBX 4 induces growth and differentiation of the trachea and lungs.
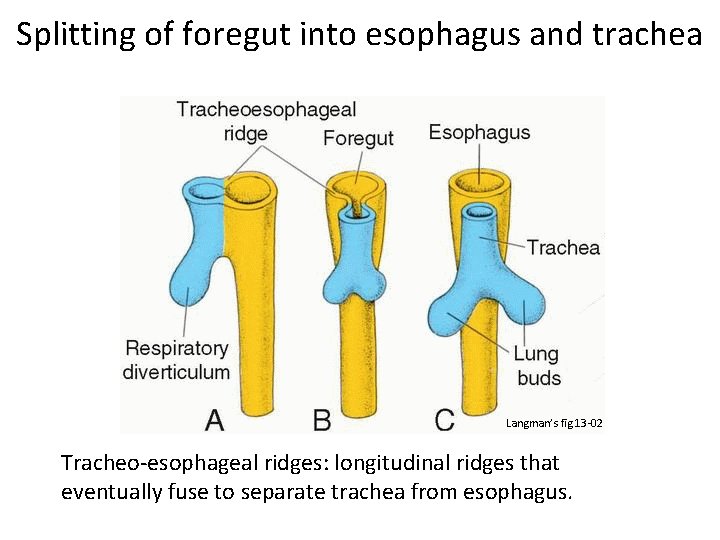
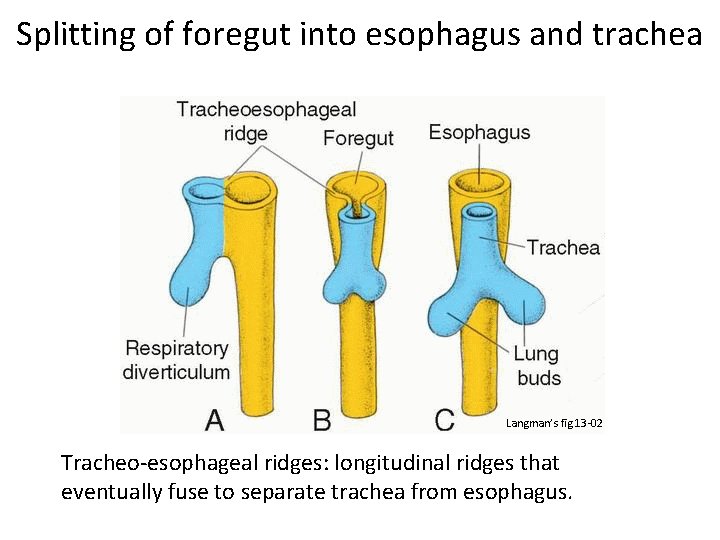
Splitting of foregut into esophagus and trachea Langman’s fig 13 -02 Tracheo-esophageal ridges: longitudinal ridges that eventually fuse to separate trachea from esophagus.
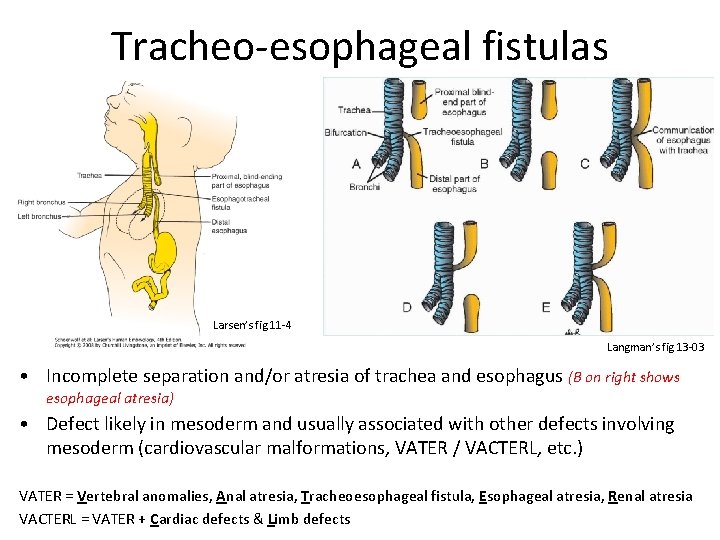
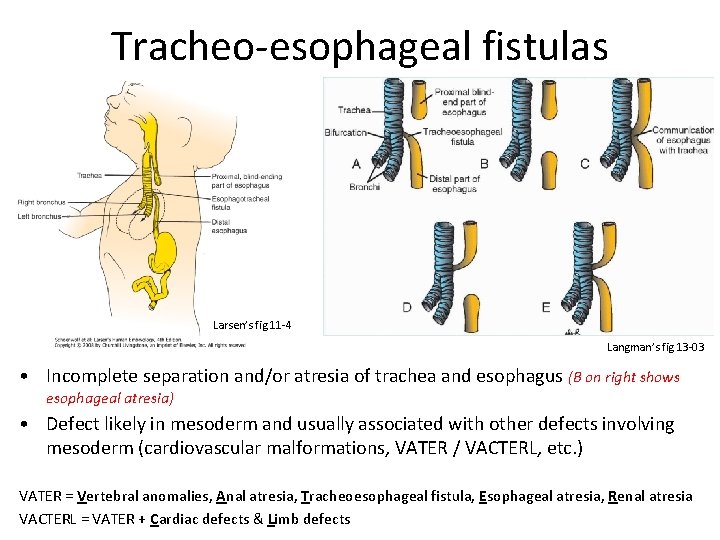
Tracheo-esophageal fistulas Larsen’s fig 11 -4 Langman’s fig 13 -03 • Incomplete separation and/or atresia of trachea and esophagus (B on right shows esophageal atresia) • Defect likely in mesoderm and usually associated with other defects involving mesoderm (cardiovascular malformations, VATER / VACTERL, etc. ) VATER = Vertebral anomalies, Anal atresia, Tracheoesophageal fistula, Esophageal atresia, Renal atresia VACTERL = VATER + Cardiac defects & Limb defects
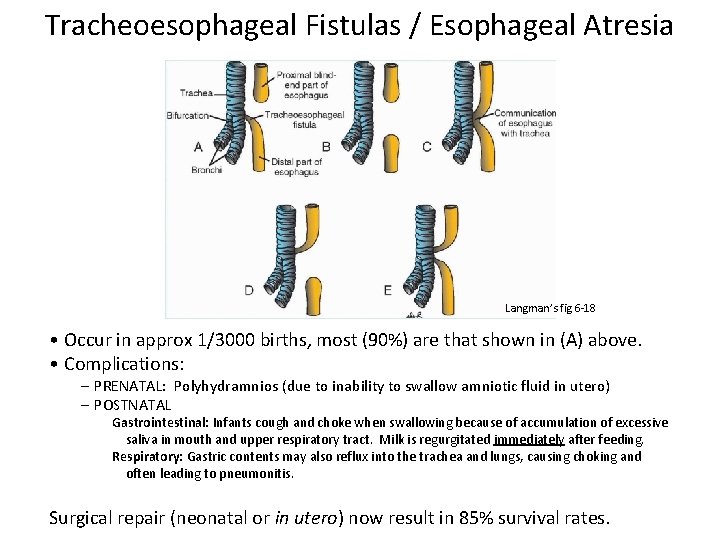
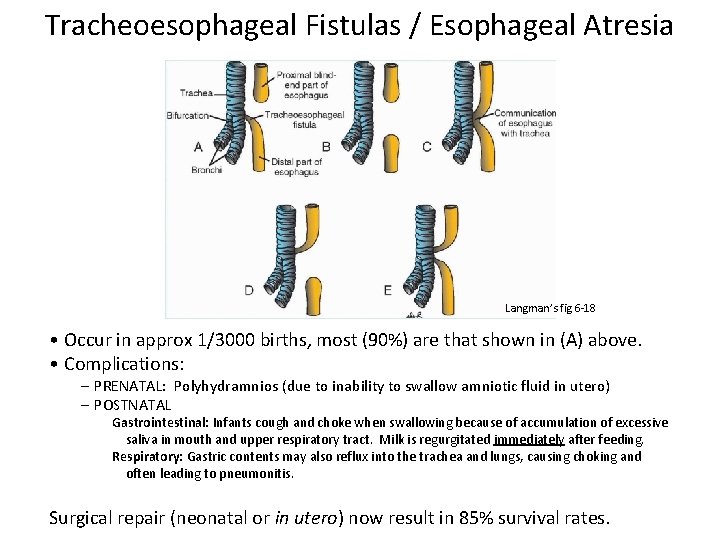
Tracheoesophageal Fistulas / Esophageal Atresia Langman’s fig 6 -18 • Occur in approx 1/3000 births, most (90%) are that shown in (A) above. • Complications: – PRENATAL: Polyhydramnios (due to inability to swallow amniotic fluid in utero) – POSTNATAL Gastrointestinal: Infants cough and choke when swallowing because of accumulation of excessive saliva in mouth and upper respiratory tract. Milk is regurgitated immediately after feeding. Respiratory: Gastric contents may also reflux into the trachea and lungs, causing choking and often leading to pneumonitis. Surgical repair (neonatal or in utero) now result in 85% survival rates.
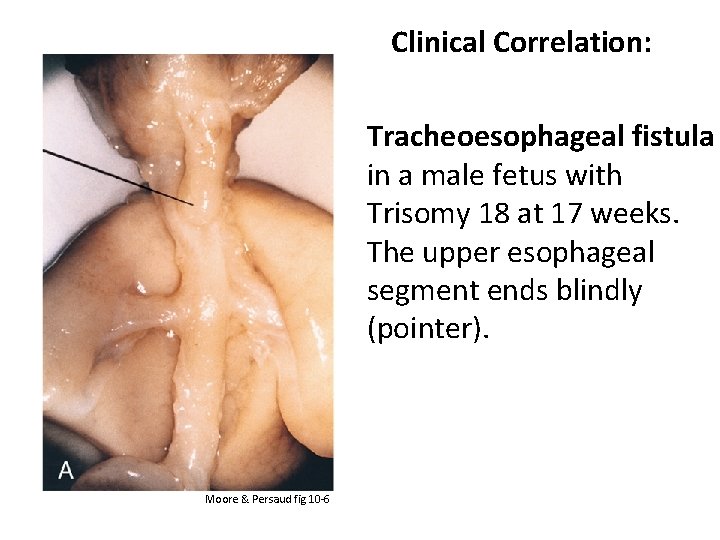
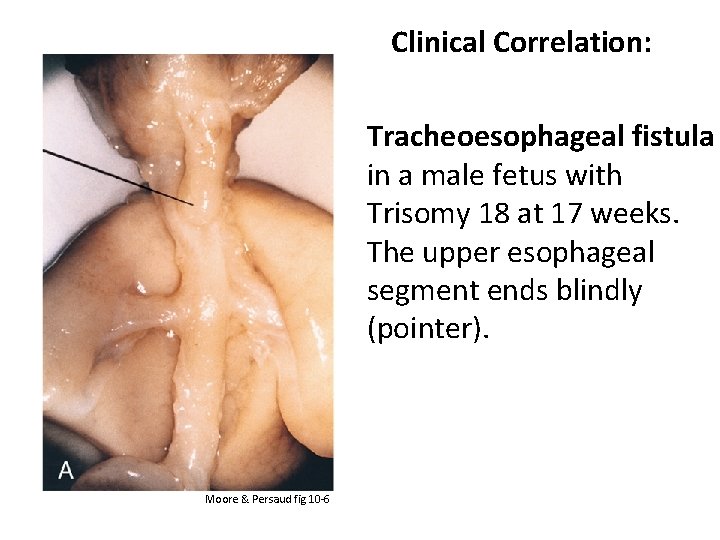
Clinical Correlation: Tracheoesophageal fistula in a male fetus with Trisomy 18 at 17 weeks. The upper esophageal segment ends blindly (pointer). Moore & Persaud fig 10 -6
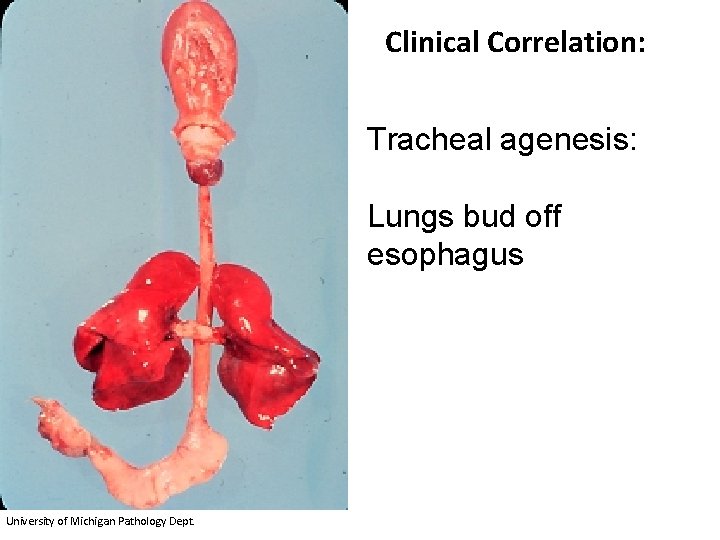
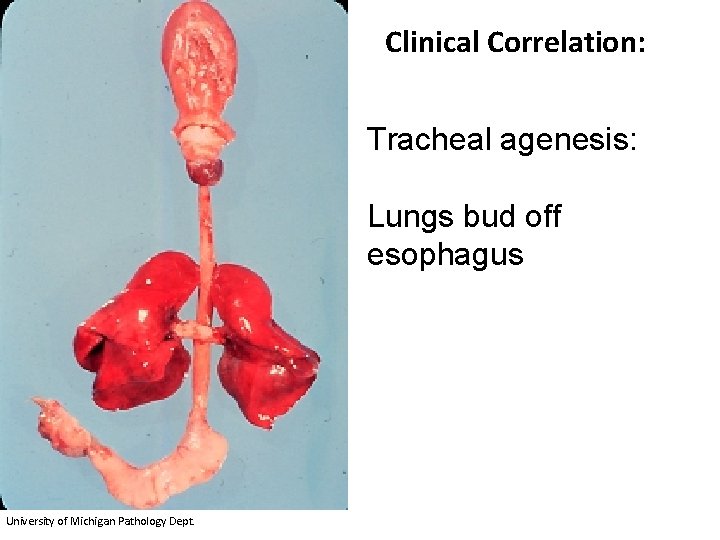
Clinical Correlation: Tracheal agenesis: Lungs bud off esophagus University of Michigan Pathology Dept.
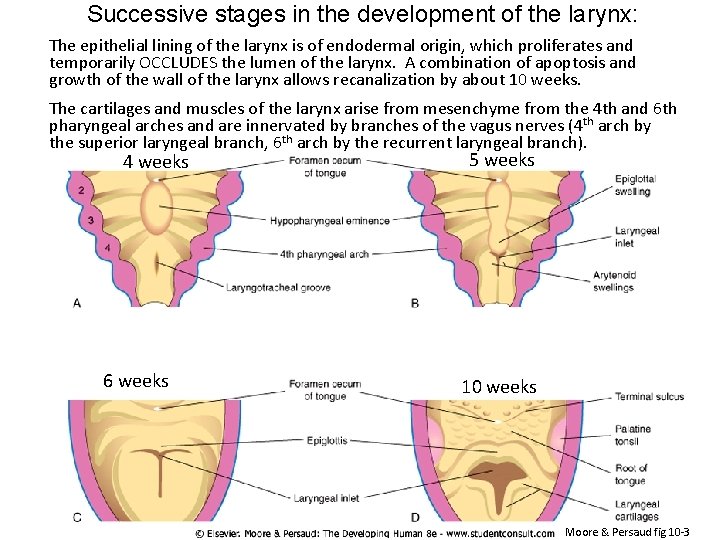
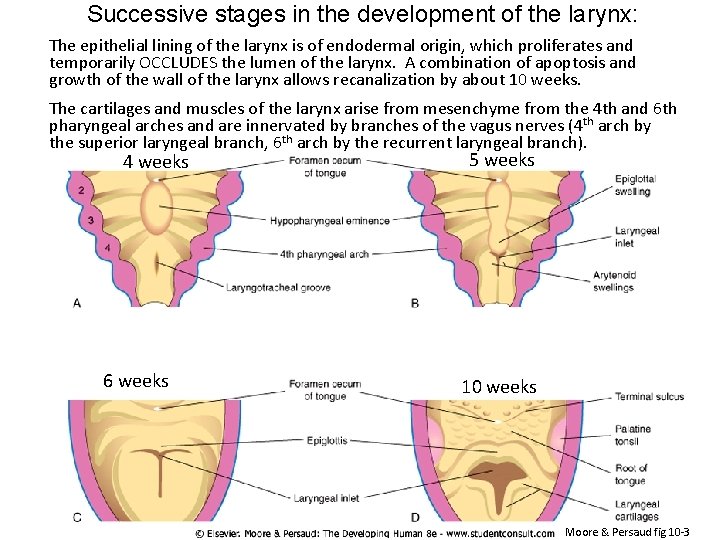
Successive stages in the development of the larynx: The epithelial lining of the larynx is of endodermal origin, which proliferates and temporarily OCCLUDES the lumen of the larynx. A combination of apoptosis and growth of the wall of the larynx allows recanalization by about 10 weeks. The cartilages and muscles of the larynx arise from mesenchyme from the 4 th and 6 th pharyngeal arches and are innervated by branches of the vagus nerves (4 th arch by the superior laryngeal branch, 6 th arch by the recurrent laryngeal branch). 4 weeks 6 weeks 5 weeks 10 weeks Moore & Persaud fig 10 -3
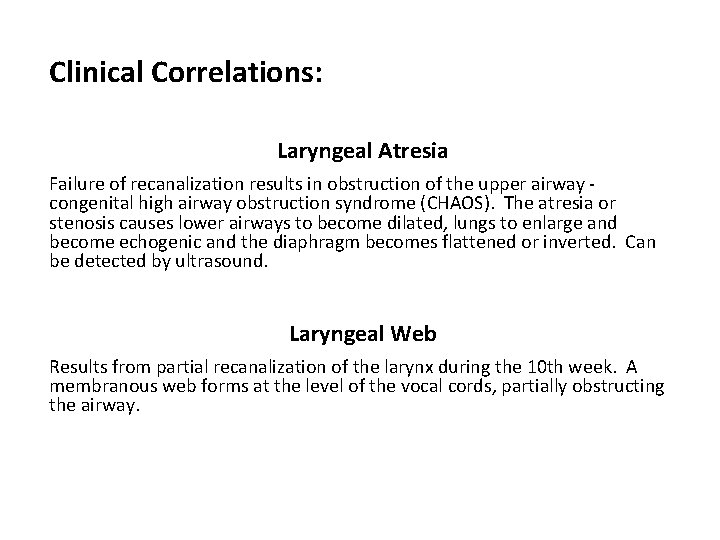
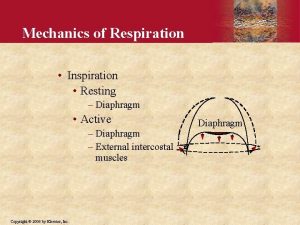
Clinical Correlations: Laryngeal Atresia Failure of recanalization results in obstruction of the upper airway congenital high airway obstruction syndrome (CHAOS). The atresia or stenosis causes lower airways to become dilated, lungs to enlarge and become echogenic and the diaphragm becomes flattened or inverted. Can be detected by ultrasound. Laryngeal Web Results from partial recanalization of the larynx during the 10 th week. A membranous web forms at the level of the vocal cords, partially obstructing the airway.
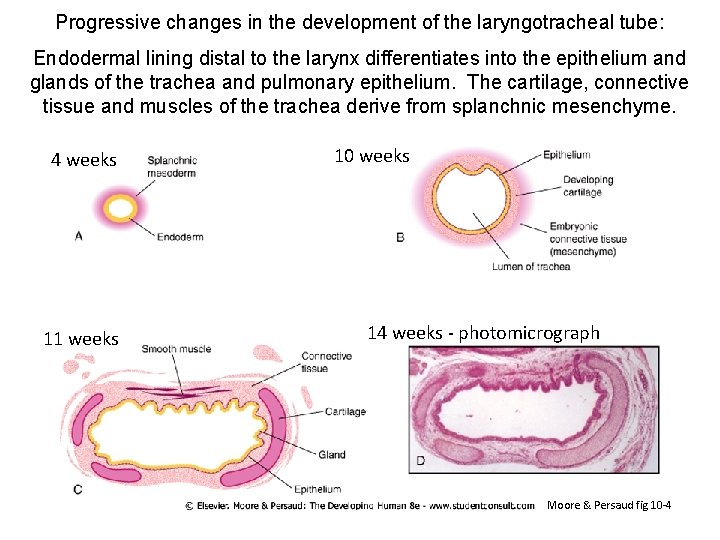
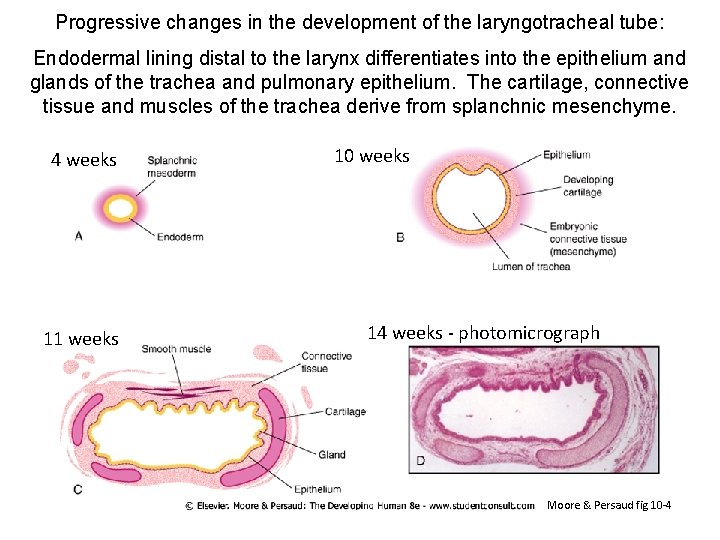
Progressive changes in the development of the laryngotracheal tube: Endodermal lining distal to the larynx differentiates into the epithelium and glands of the trachea and pulmonary epithelium. The cartilage, connective tissue and muscles of the trachea derive from splanchnic mesenchyme. 4 weeks 11 weeks 10 weeks 14 weeks - photomicrograph Moore & Persaud fig 10 -4
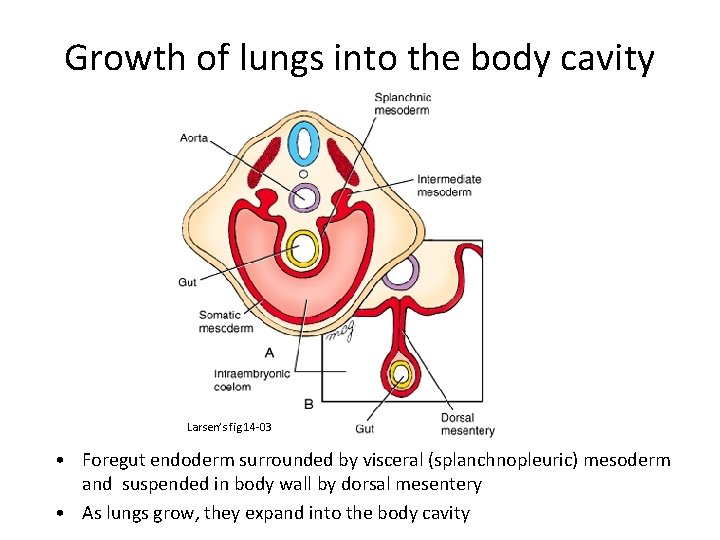
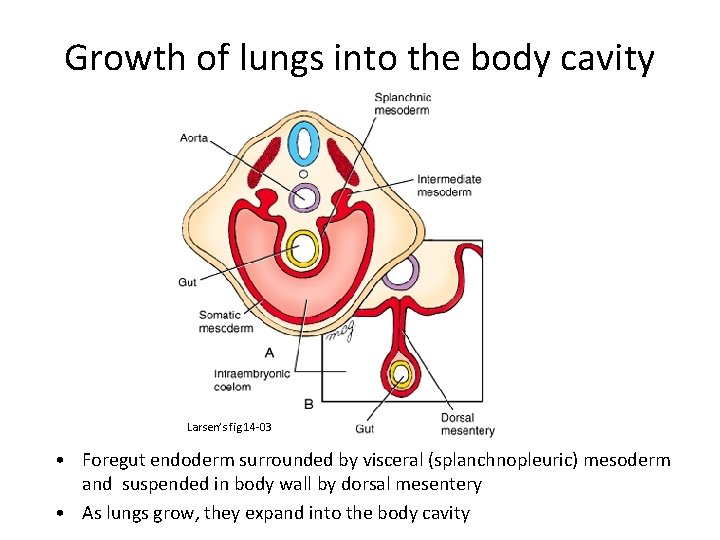
Growth of lungs into the body cavity Larsen’s fig 14 -03 • Foregut endoderm surrounded by visceral (splanchnopleuric) mesoderm and suspended in body wall by dorsal mesentery • As lungs grow, they expand into the body cavity
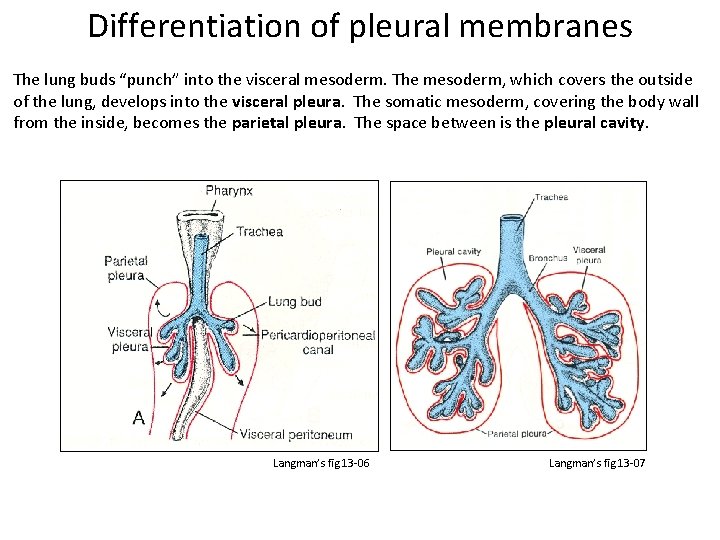
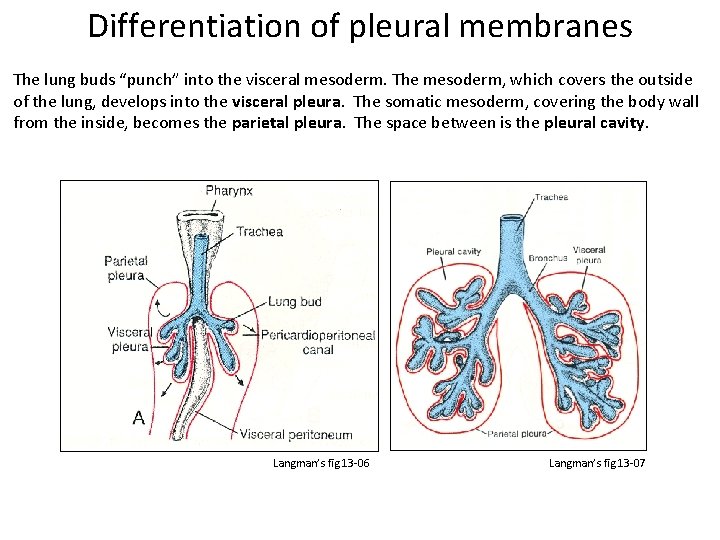
Differentiation of pleural membranes The lung buds “punch” into the visceral mesoderm. The mesoderm, which covers the outside of the lung, develops into the visceral pleura. The somatic mesoderm, covering the body wall from the inside, becomes the parietal pleura. The space between is the pleural cavity. Langman’s fig 13 -06 Langman’s fig 13 -07
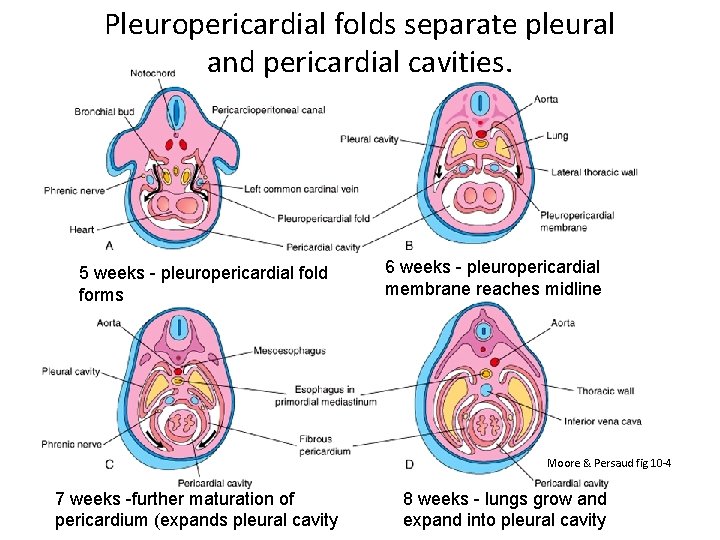
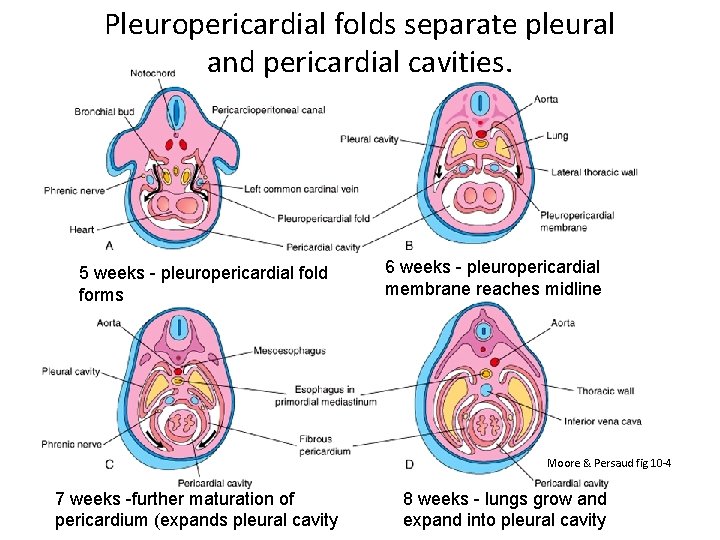
Pleuropericardial folds separate pleural and pericardial cavities. 5 weeks - pleuropericardial fold forms 6 weeks - pleuropericardial membrane reaches midline Moore & Persaud fig 10 -4 7 weeks -further maturation of pericardium (expands pleural cavity 8 weeks - lungs grow and expand into pleural cavity
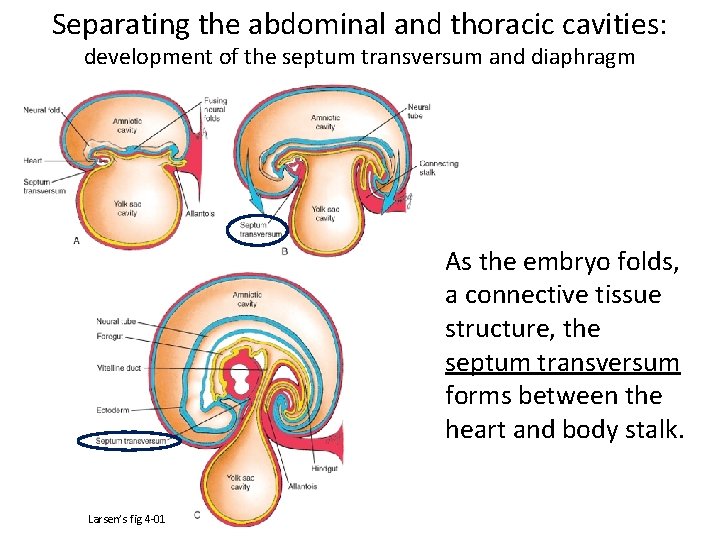
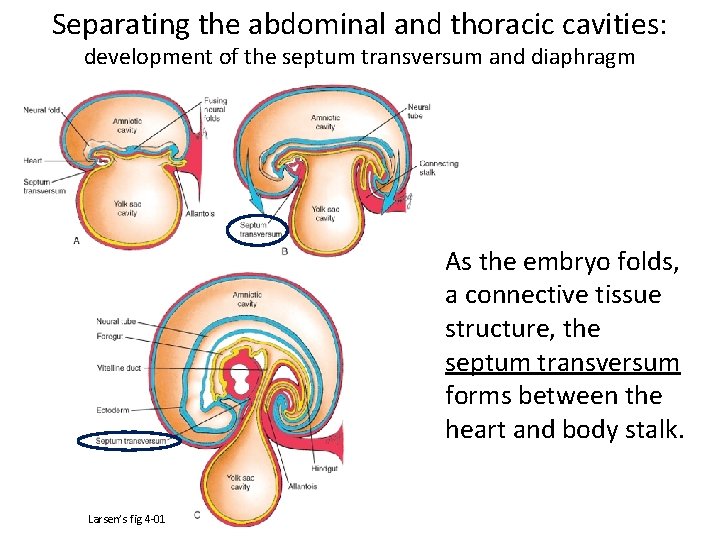
Separating the abdominal and thoracic cavities: development of the septum transversum and diaphragm As the embryo folds, a connective tissue structure, the septum transversum forms between the heart and body stalk. Larsen’s fig 4 -01
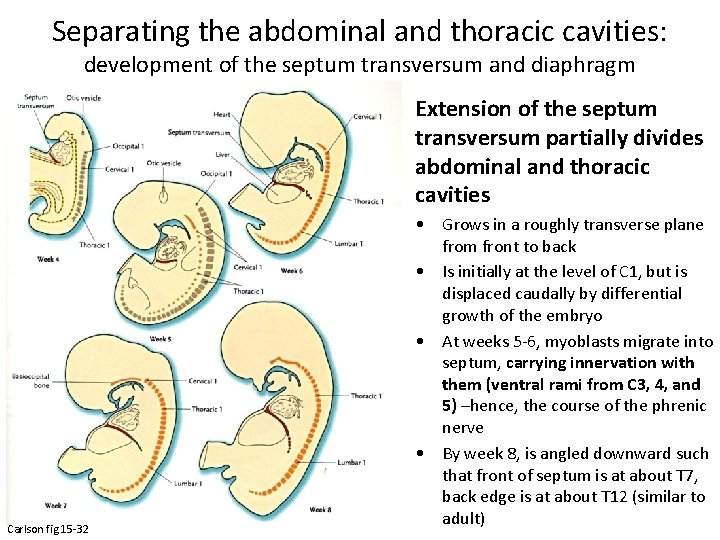
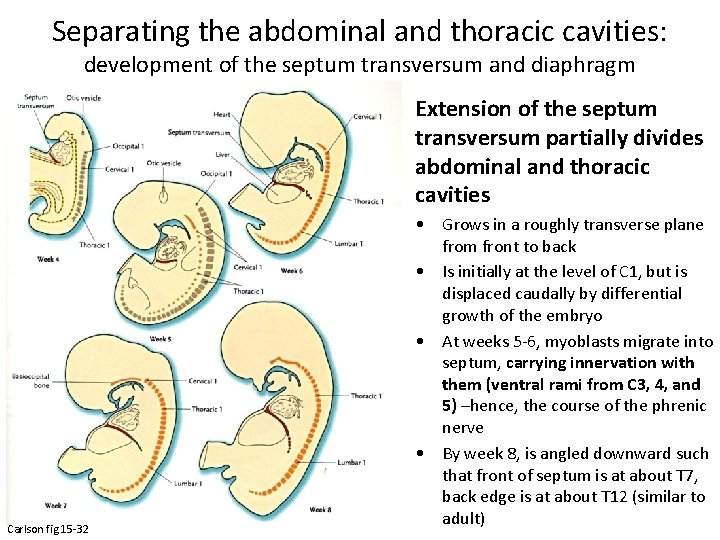
Separating the abdominal and thoracic cavities: development of the septum transversum and diaphragm Extension of the septum transversum partially divides abdominal and thoracic cavities Carlson fig 15 -32 • Grows in a roughly transverse plane from front to back • Is initially at the level of C 1, but is displaced caudally by differential growth of the embryo • At weeks 5 -6, myoblasts migrate into septum, carrying innervation with them (ventral rami from C 3, 4, and 5) –hence, the course of the phrenic nerve • By week 8, is angled downward such that front of septum is at about T 7, back edge is at about T 12 (similar to adult)
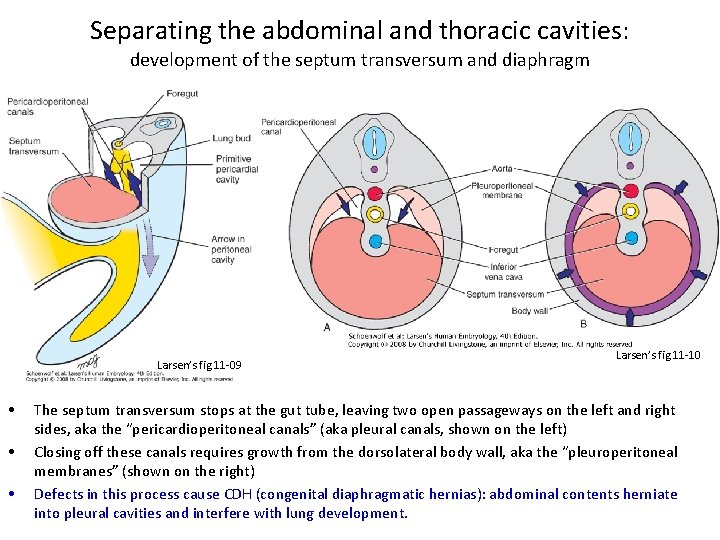
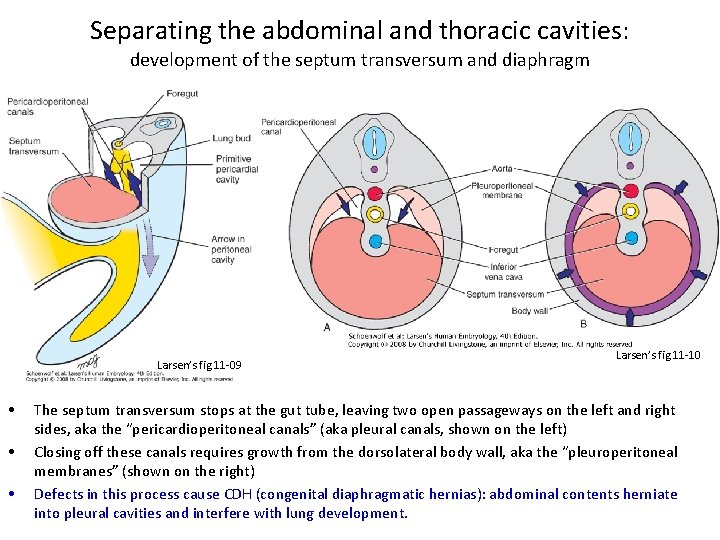
Separating the abdominal and thoracic cavities: development of the septum transversum and diaphragm Larsen’s fig 11 -09 • • • Larsen’s fig 11 -10 The septum transversum stops at the gut tube, leaving two open passageways on the left and right sides, aka the “pericardioperitoneal canals” (aka pleural canals, shown on the left) Closing off these canals requires growth from the dorsolateral body wall, aka the “pleuroperitoneal membranes” (shown on the right) Defects in this process cause CDH (congenital diaphragmatic hernias): abdominal contents herniate into pleural cavities and interfere with lung development.
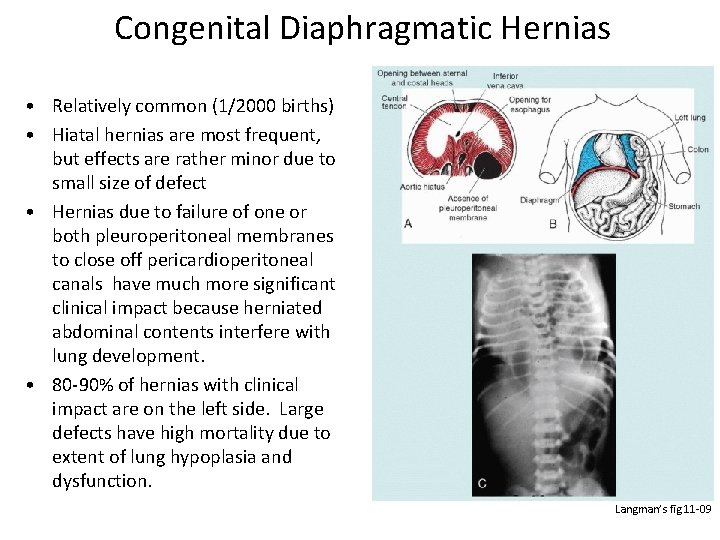
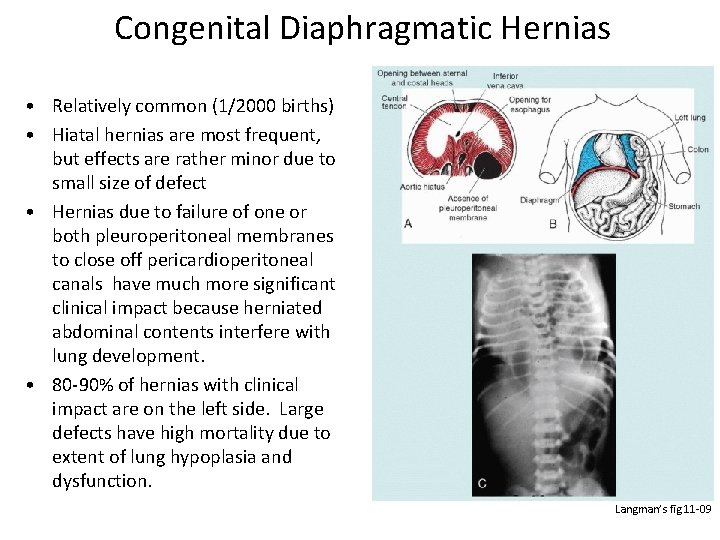
Congenital Diaphragmatic Hernias • Relatively common (1/2000 births) • Hiatal hernias are most frequent, but effects are rather minor due to small size of defect • Hernias due to failure of one or both pleuroperitoneal membranes to close off pericardioperitoneal canals have much more significant clinical impact because herniated abdominal contents interfere with lung development. • 80 -90% of hernias with clinical impact are on the left side. Large defects have high mortality due to extent of lung hypoplasia and dysfunction. Langman’s fig 11 -09
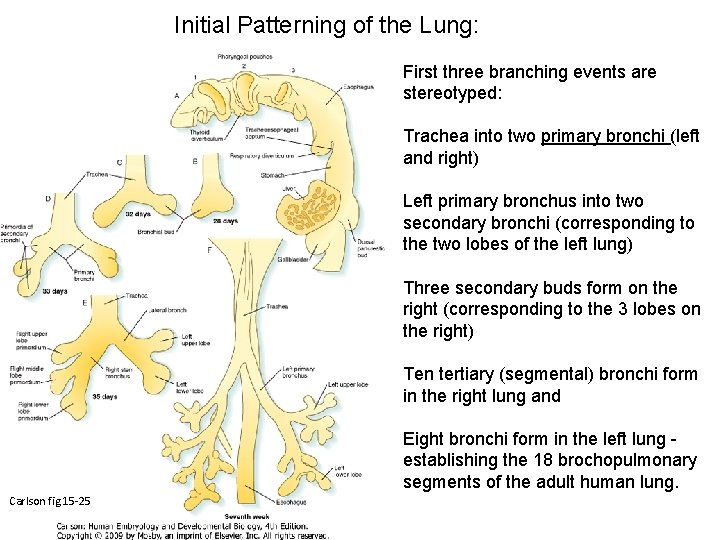
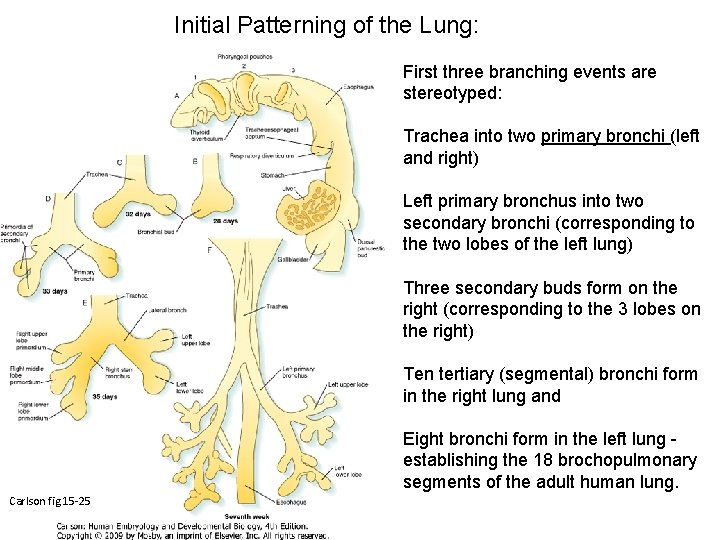
Initial Patterning of the Lung: First three branching events are stereotyped: Trachea into two primary bronchi (left and right) Left primary bronchus into two secondary bronchi (corresponding to the two lobes of the left lung) Three secondary buds form on the right (corresponding to the 3 lobes on the right) Ten tertiary (segmental) bronchi form in the right lung and Eight bronchi form in the left lung establishing the 18 brochopulmonary segments of the adult human lung. Carlson fig 15 -25 (10) Segmental bronchi (7 -8)
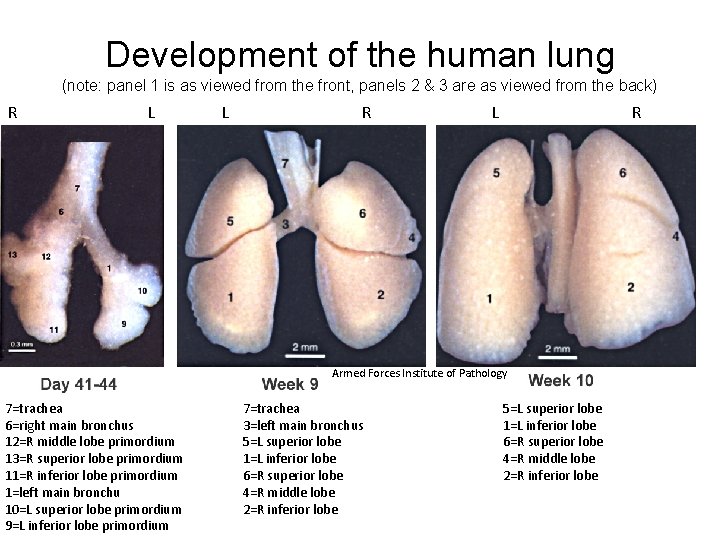
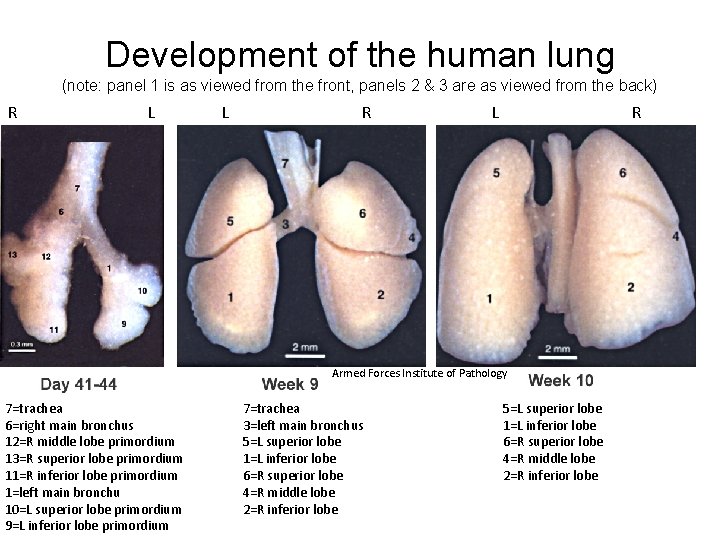
Development of the human lung (note: panel 1 is as viewed from the front, panels 2 & 3 are as viewed from the back) R L L R Armed Forces Institute of Pathology 7=trachea 6=right main bronchus 12=R middle lobe primordium 13=R superior lobe primordium 11=R inferior lobe primordium 1=left main bronchu 10=L superior lobe primordium 9=L inferior lobe primordium 7=trachea 3=left main bronchus 5=L superior lobe 1=L inferior lobe 6=R superior lobe 4=R middle lobe 2=R inferior lobe
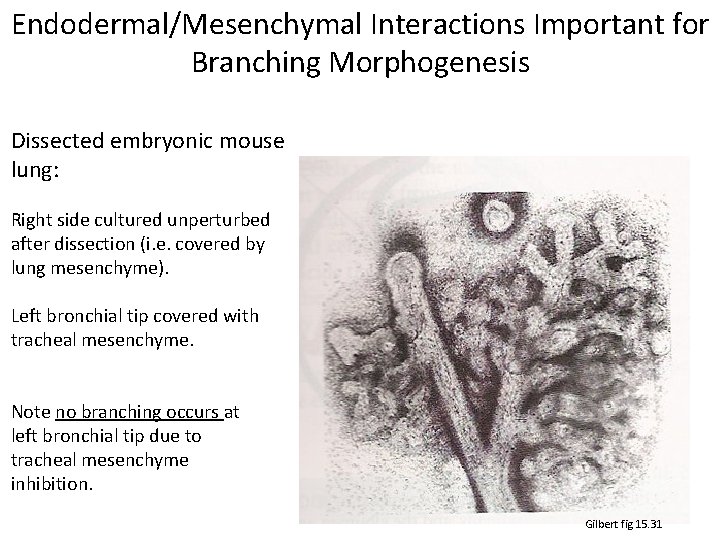
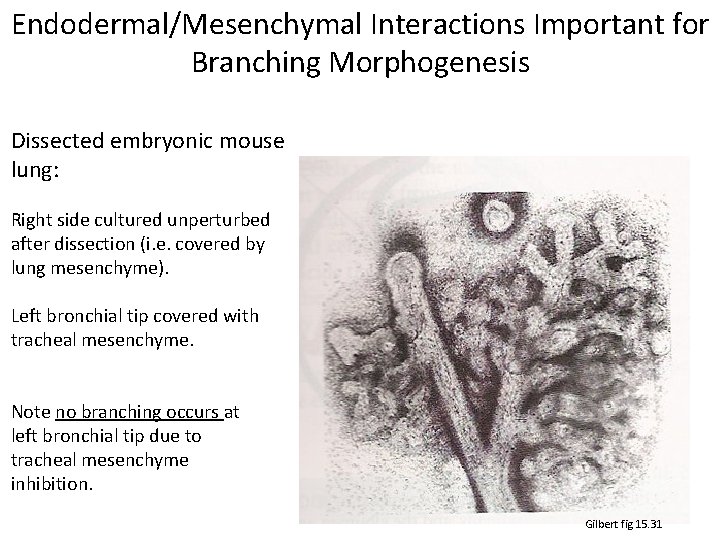
Endodermal/Mesenchymal Interactions Important for Branching Morphogenesis Dissected embryonic mouse lung: Right side cultured unperturbed after dissection (i. e. covered by lung mesenchyme). Left bronchial tip covered with tracheal mesenchyme. Note no branching occurs at left bronchial tip due to tracheal mesenchyme inhibition. Gilbert fig 15. 31
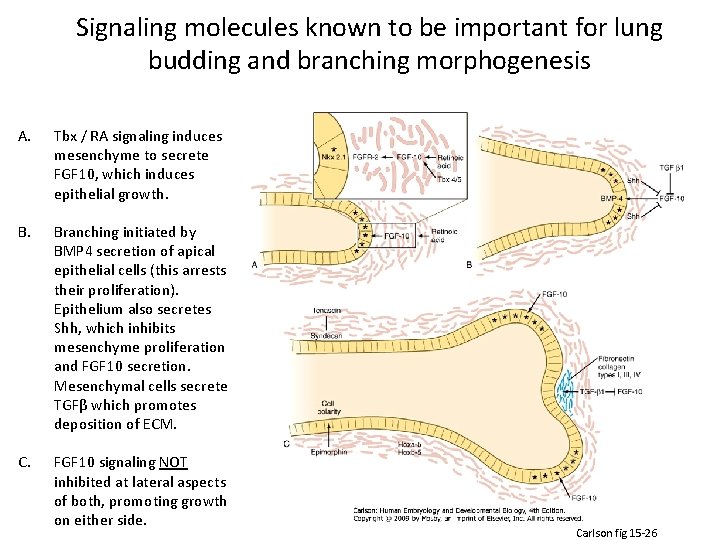
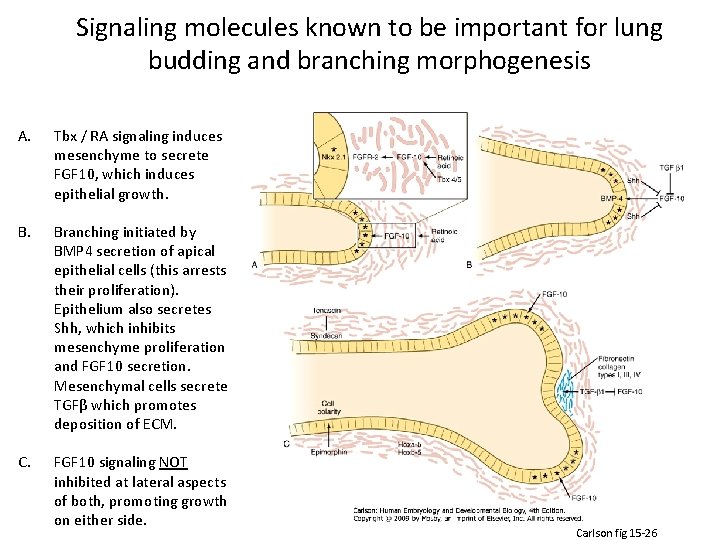
Signaling molecules known to be important for lung budding and branching morphogenesis A. Tbx / RA signaling induces mesenchyme to secrete FGF 10, which induces epithelial growth. Branching initiated by BMP 4 secretion of apical epithelial cells (this arrests their proliferation). Epithelium also secretes Shh, which inhibits mesenchyme proliferation and FGF 10 secretion. Mesenchymal cells secrete TGFβ which promotes deposition of ECM. C. FGF 10 signaling NOT inhibited at lateral aspects of both, promoting growth on either side. Carlson fig 15 -26
By the end of the sixth month, 17 generations of subdivisions have formed. Six more divisions occur during postnatal life for a total of 23 branching events in the adult human lung. Branching continues to be regulated by epithelialmesenchymal interactions (deriving from endodermal epithelial lung buds and the splanchnic mesoderm surrounding them). MAIN POINT: Branching morphogenesis in the lungs is mesoderm and retinoid-dependent (among other factors). Late disruption may have minor effects whereas early disruption may result in hypoplasia or even agenesis.
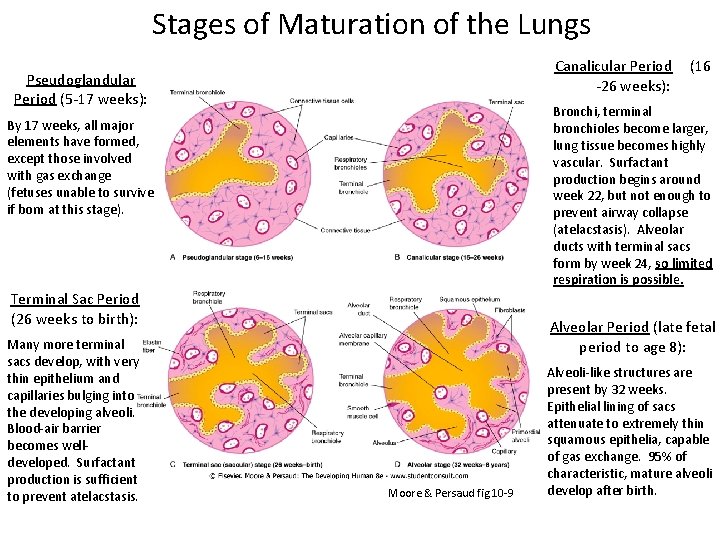
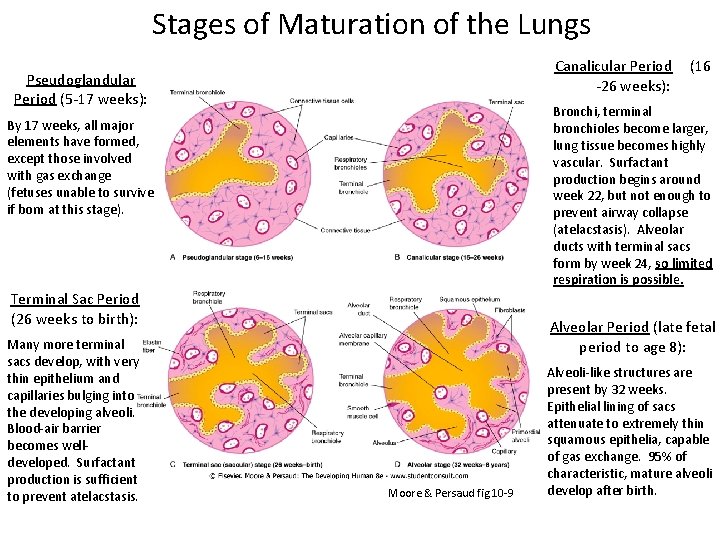
Stages of Maturation of the Lungs Canalicular Period -26 weeks): Pseudoglandular Period (5 -17 weeks): Bronchi, terminal bronchioles become larger, lung tissue becomes highly vascular. Surfactant production begins around week 22, but not enough to prevent airway collapse (atelacstasis). Alveolar ducts with terminal sacs form by week 24, so limited respiration is possible. By 17 weeks, all major elements have formed, except those involved with gas exchange (fetuses unable to survive if born at this stage). Terminal Sac Period (26 weeks to birth): Many more terminal sacs develop, with very thin epithelium and capillaries bulging into the developing alveoli. Blood-air barrier becomes welldeveloped. Surfactant production is sufficient to prevent atelacstasis. (16 Alveolar Period (late fetal period to age 8): Moore & Persaud fig 10 -9 Alveoli-like structures are present by 32 weeks. Epithelial lining of sacs attenuate to extremely thin squamous epithelia, capable of gas exchange. 95% of characteristic, mature alveoli develop after birth.
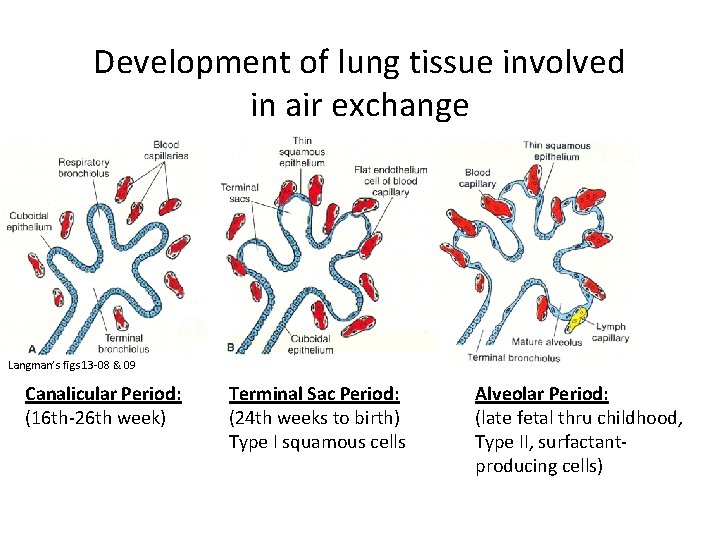
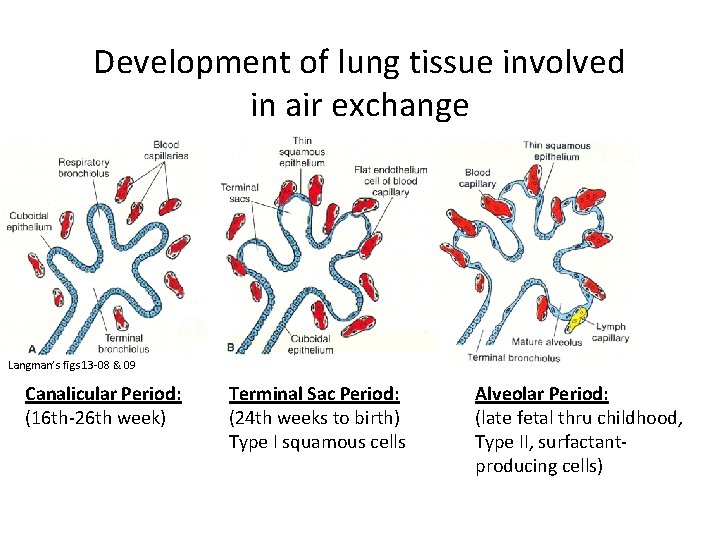
Development of lung tissue involved in air exchange Langman’s figs 13 -08 & 09 Canalicular Period: (16 th-26 th week) Terminal Sac Period: (24 th weeks to birth) Type I squamous cells Alveolar Period: (late fetal thru childhood, Type II, surfactantproducing cells)
At birth: Alveoli continue to mature after birth, become more muscular. Growth of lungs after birth due primarily to increase of respiratory bronchioles and alveoli. Only 1/6 of adult alveoli present at birth. Lungs are fluid filled; fluid squeezed out and into lymphatics and blood vessels, expelled via trachea at delivery. Surfactant remains on surface, lowers air/blood tension.
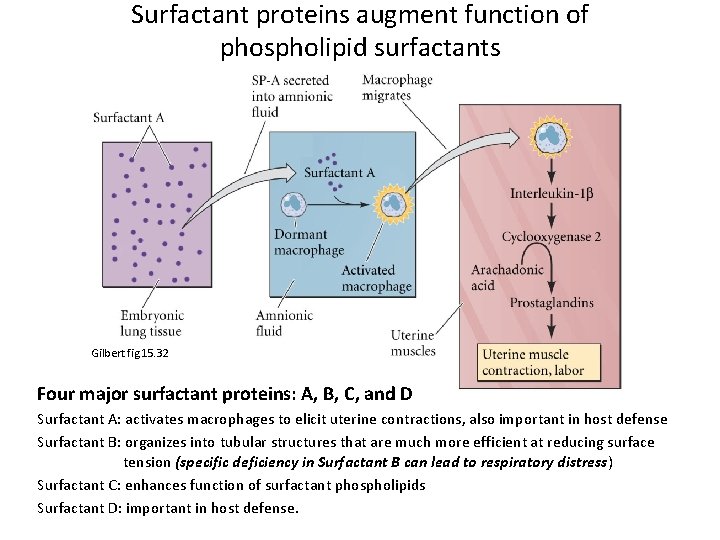
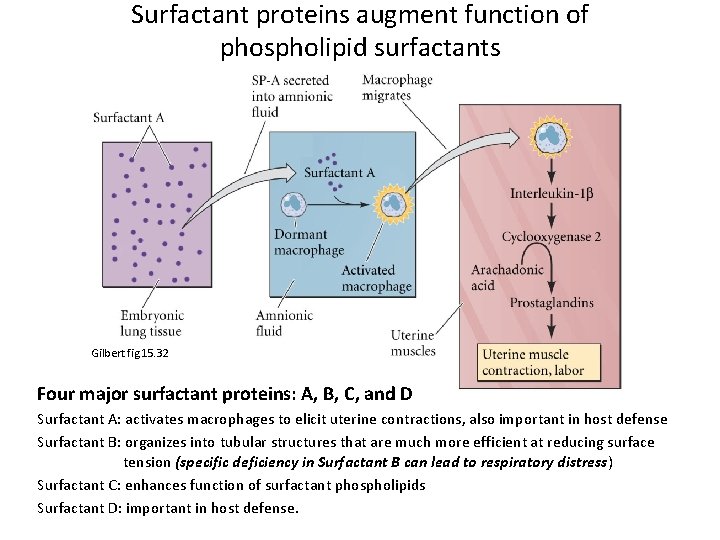
Surfactant proteins augment function of phospholipid surfactants Gilbert fig 15. 32 Four major surfactant proteins: A, B, C, and D Surfactant A: activates macrophages to elicit uterine contractions, also important in host defense Surfactant B: organizes into tubular structures that are much more efficient at reducing surface tension (specific deficiency in Surfactant B can lead to respiratory distress) Surfactant C: enhances function of surfactant phospholipids Surfactant D: important in host defense.
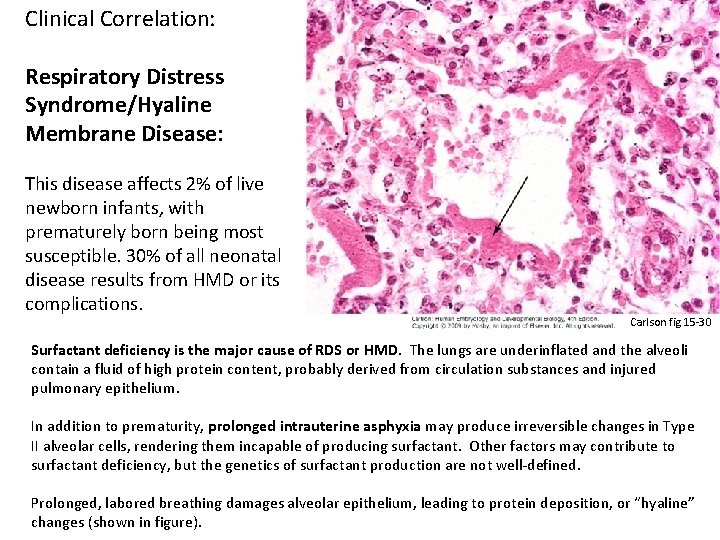
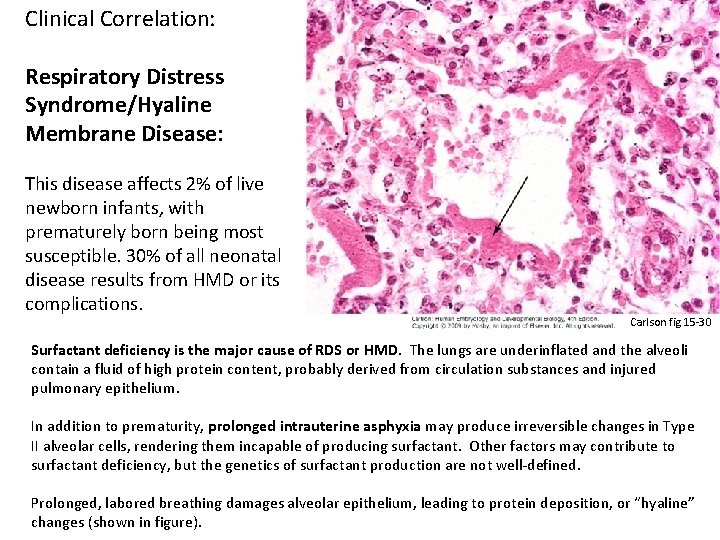
Clinical Correlation: Respiratory Distress Syndrome/Hyaline Membrane Disease: This disease affects 2% of live newborn infants, with prematurely born being most susceptible. 30% of all neonatal disease results from HMD or its complications. Carlson fig 15 -30 Surfactant deficiency is the major cause of RDS or HMD. The lungs are underinflated and the alveoli contain a fluid of high protein content, probably derived from circulation substances and injured pulmonary epithelium. In addition to prematurity, prolonged intrauterine asphyxia may produce irreversible changes in Type II alveolar cells, rendering them incapable of producing surfactant. Other factors may contribute to surfactant deficiency, but the genetics of surfactant production are not well-defined. Prolonged, labored breathing damages alveolar epithelium, leading to protein deposition, or “hyaline” changes (shown in figure).
Clinical Correlations: Congenital Lung Cysts: Cysts (filled with fluid or air) are thought to be formed by the dilation of terminal bronchi, probably due to branching irregularities in later development. If severe, cysts are visible on radiographs. Highly variable outcomes result from different cystic conditions. Agenesis of the Lungs: Can occur bilaterally or unilaterally due to early failure of the respiratory bud to develop and/or branch (e. g. insufficient mesoderm, teratogens such as RA or alcohol, or genetic mutation). Unilateral lung agenesis is compatible with life (remaining side usually hyperexpands and compensates). Lung Hypoplasia: May be due to inadequate branching morphogenesis, but often caused by congenital diaphragmatic hernias or congenital heart disease. Characterized by reduced lung volume. Extreme hypoplasia is inconsistent with life.
Figures from the following texts: Bruce M. Carlson, Human Embryology & Developmental Biology, 4 th ed. Scott Gilbert, Developmental Biology, 8 th ed. Keith Moore & Vid Persaud, The Developing Human, 8 th ed. Tom W Sadler, Langman’s Medical Embryology, 11 th ed. Gary Schoenwolf, et al. , Larsen’s Human Embryology, 4 th ed.
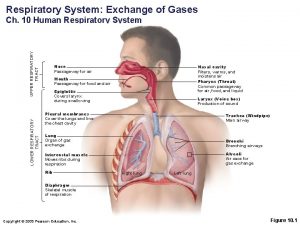
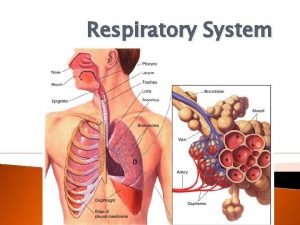
 Conducting zone respiratory
Conducting zone respiratory Digestive system respiratory system and circulatory system
Digestive system respiratory system and circulatory system Development of respiratory system
Development of respiratory system Pharynx and larynx and trachea
Pharynx and larynx and trachea Image search
Image search Splanchnic mesoderm
Splanchnic mesoderm Development of respiratory system
Development of respiratory system Circulatory system and respiratory system work together
Circulatory system and respiratory system work together Plot
Plot Diaphragm of the female reproductive system
Diaphragm of the female reproductive system Tiny air sacs at the end of the bronchioles
Tiny air sacs at the end of the bronchioles Advantages of diaphragm cell
Advantages of diaphragm cell Lethenic
Lethenic Diaphragm origin insertion
Diaphragm origin insertion Left crus of diaphragm
Left crus of diaphragm Hernia
Hernia Urinary system diagram
Urinary system diagram Sternal and costal slips of diaphragm
Sternal and costal slips of diaphragm Maxp series pumps
Maxp series pumps Upper and lower respiratory tract
Upper and lower respiratory tract Stress and respiratory system
Stress and respiratory system Circulatory and respiratory system working together
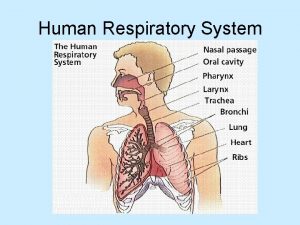
Circulatory and respiratory system working together Human respiratory system diagram
Human respiratory system diagram Middlesex radiology
Middlesex radiology Rat diaphragm
Rat diaphragm Rat dissection digestive system
Rat dissection digestive system Gegasx
Gegasx The regulator diaphragm is often made from
The regulator diaphragm is often made from Air bronchogram
Air bronchogram Educa evoluciona
Educa evoluciona Percussion lungs
Percussion lungs External anatomy of a rat
External anatomy of a rat