Continuous Capnography The Wave of the Future Amy

- Slides: 71
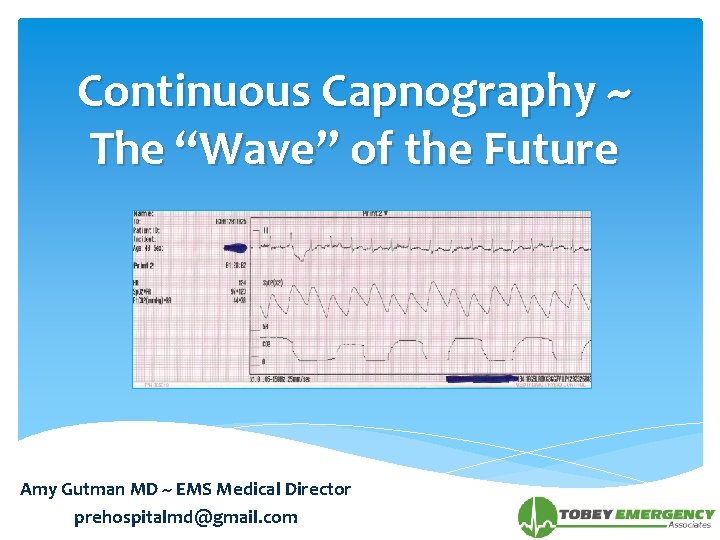
Continuous Capnography ~ The “Wave” of the Future Amy Gutman MD ~ EMS Medical Director prehospitalmd@gmail. com
Objectives What is the capnogram? Review capnogram appearance in relation to physiology with clinical implications Incorporate capnography into protocols Appreciation to Medtronics for 2010 permission to use portions of their training module in preparing this presentation
Waveform Capnography Non-invasive, continuous measurement of airway CO 2 concentration “Vital” sign of patient’s ventilatory & hemodynamic status Provides an early objective measurement & warning of changes in ventilation & cardiopulmonary status from one breath to another Important for medico-legal documentation Standard of care for prehospital & hospital patient monitoring
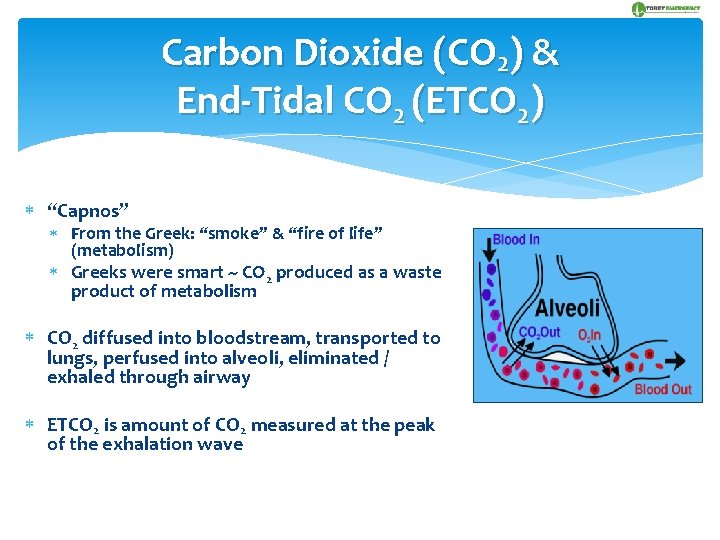
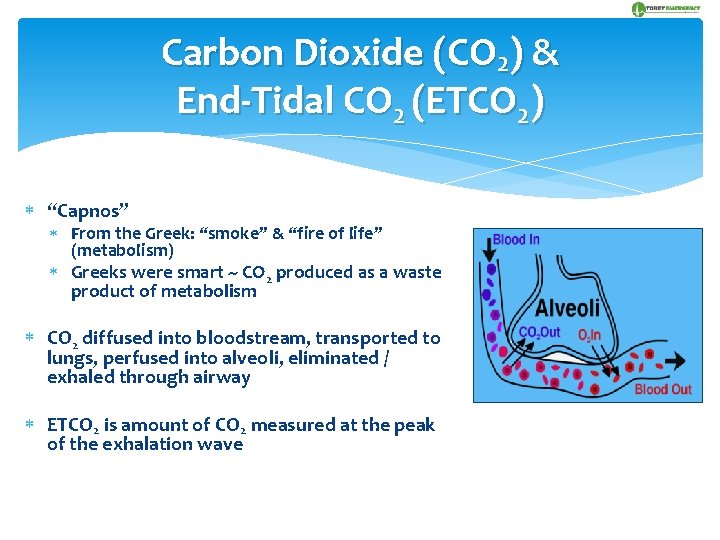
Carbon Dioxide (CO 2) & End-Tidal CO 2 (ETCO 2) “Capnos” From the Greek: “smoke” & “fire of life” (metabolism) Greeks were smart ~ CO 2 produced as a waste product of metabolism CO 2 diffused into bloodstream, transported to lungs, perfused into alveoli, eliminated / exhaled through airway ETCO 2 is amount of CO 2 measured at the peak of the exhalation wave
AHA 2010 Guidelines Summary Continuous waveform capnography recommended for intubated patients throughout arrest / peri-arrest period Confirm ETT Placement (Class I, LOE A) Continuous monitoring of patient, airway, equipment Monitor CPR quality (Class IIb, LOE C) <10 mm. Hg not associated with successful resuscitation or effective compressions Push Hard, Push Fast Change rescuer every 2 minutes Detect ROSC (Class IIa, LOE B)
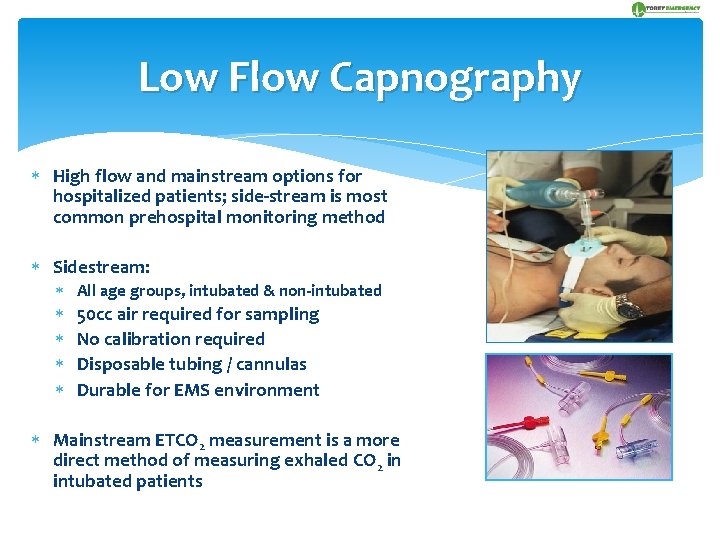
Low Flow Capnography High flow and mainstream options for hospitalized patients; side-stream is most common prehospital monitoring method Sidestream: All age groups, intubated & non-intubated 50 cc air required for sampling No calibration required Disposable tubing / cannulas Durable for EMS environment Mainstream ETCO 2 measurement is a more direct method of measuring exhaled CO 2 in intubated patients
Documentation Printed confirmation of procedural skills & patient responses to treatment No further “blame games”, i. e. “The tube was in place until you dislodged it” Prints out both waveform & patient trends State requirement to attach the waveform summary to your PCR (similar to an EKG)
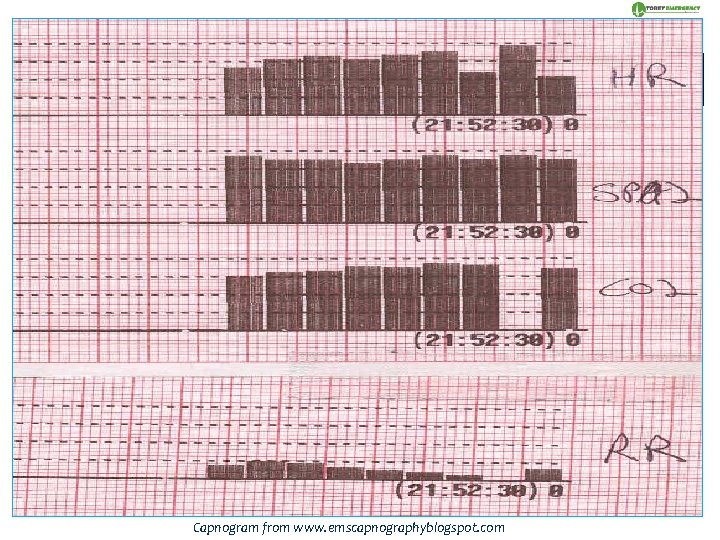
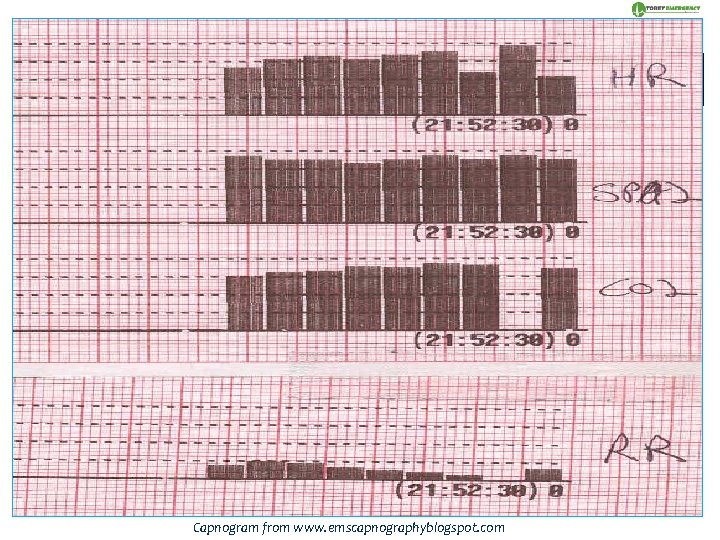
OXYGENTATION O 2 bloodstream to cells Non-invasive measurement by pulse oximetry (Sp. O 2) of %O 2 in RBCs Changes in ventilation take minutes to be detected Affected by motion artifact, poor perfusion & some dysrhythmias VENTILATION Exhaling of CO 2 metabolism byproduct via respiratory tract Measured by ETCO 2 as a partial pressure (mm. Hg) or volume (% vol) of CO 2 in airway at end of exhalation Breath-to-breath measurement provides info within seconds Not affected by motion artifact, poor perfusion or dysrhythmias Capnogram from www. emscapnographyblogspot. com
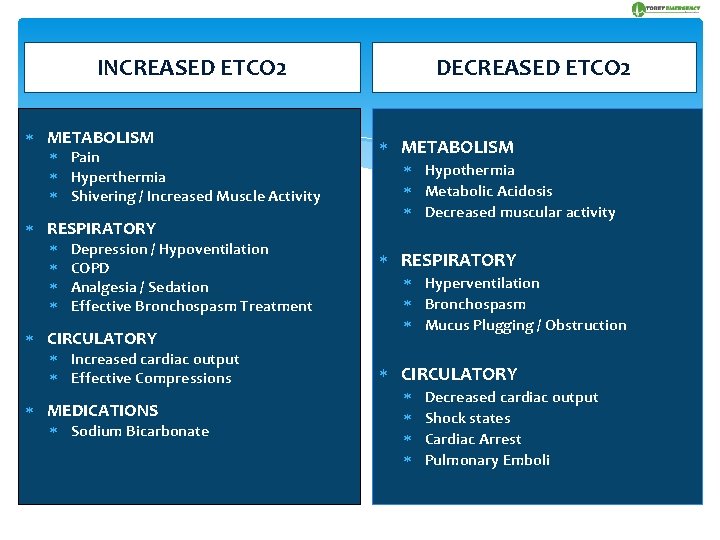
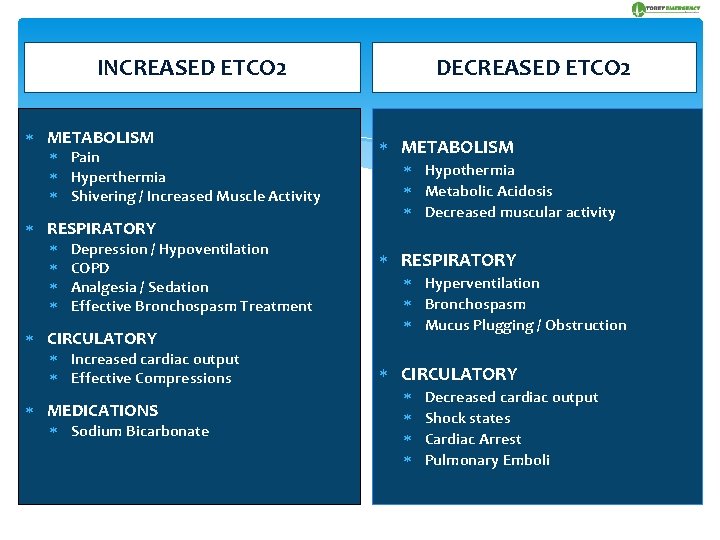
INCREASED ETCO 2 METABOLISM Pain Hyperthermia Shivering / Increased Muscle Activity RESPIRATORY Depression / Hypoventilation COPD Analgesia / Sedation Effective Bronchospasm Treatment CIRCULATORY Increased cardiac output Effective Compressions MEDICATIONS Sodium Bicarbonate DECREASED ETCO 2 METABOLISM Hypothermia Metabolic Acidosis Decreased muscular activity RESPIRATORY Hyperventilation Bronchospasm Mucus Plugging / Obstruction CIRCULATORY Decreased cardiac output Shock states Cardiac Arrest Pulmonary Emboli
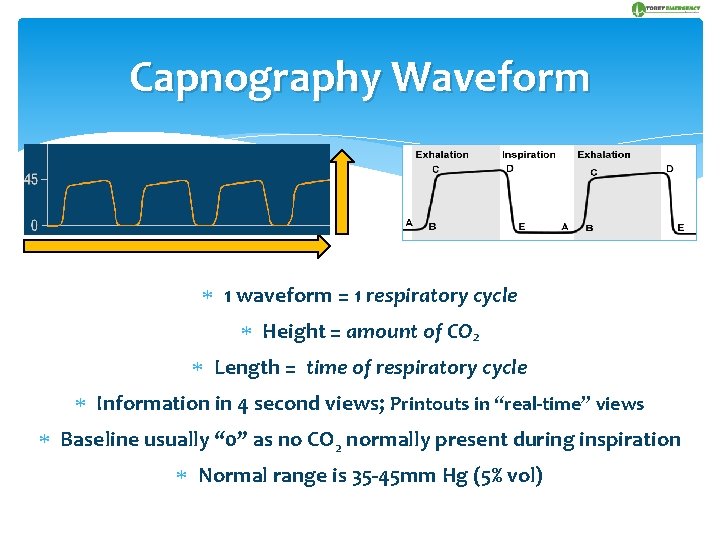
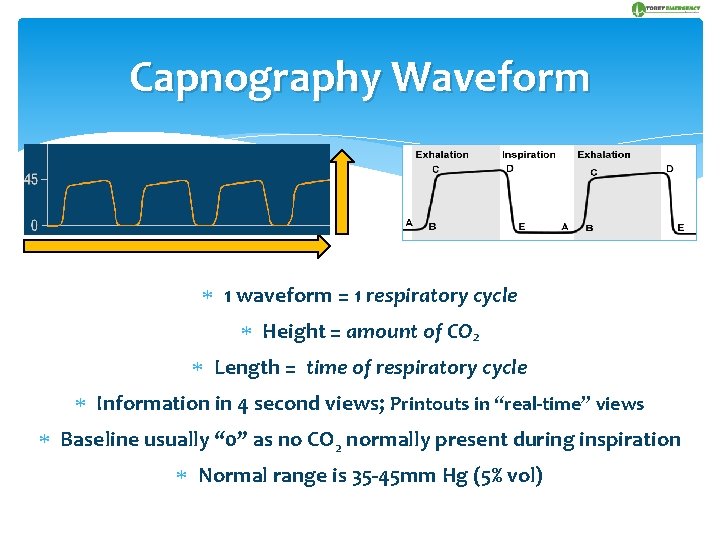
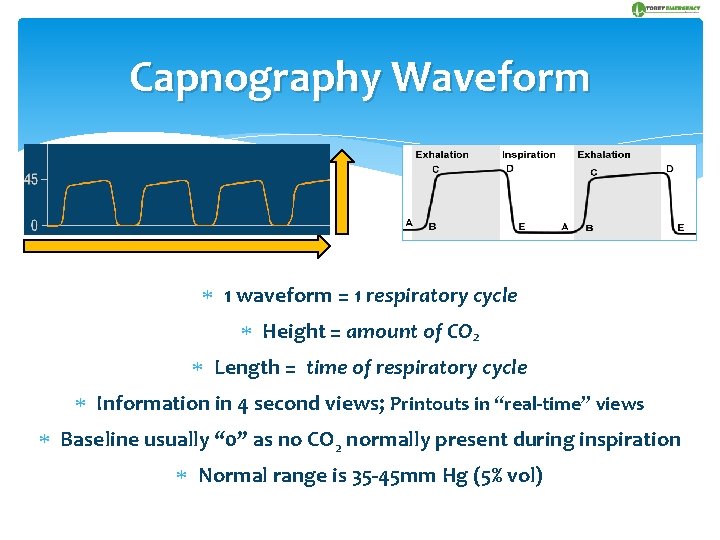
Capnography Waveform 1 waveform = 1 respiratory cycle Height = amount of CO 2 Length = time of respiratory cycle Information in 4 second views; Printouts in “real-time” views Baseline usually “ 0” as no CO 2 normally present during inspiration Normal range is 35 -45 mm Hg (5% vol)
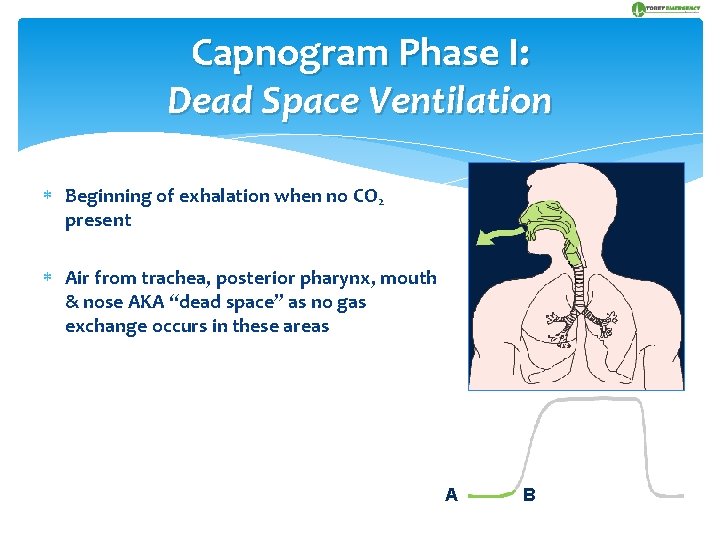
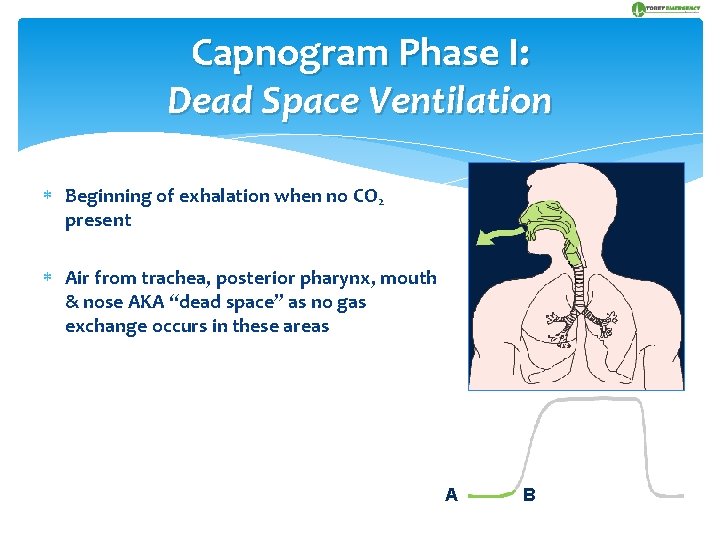
Capnogram Phase I: Dead Space Ventilation Beginning of exhalation when no CO 2 present Air from trachea, posterior pharynx, mouth & nose AKA “dead space” as no gas exchange occurs in these areas A B
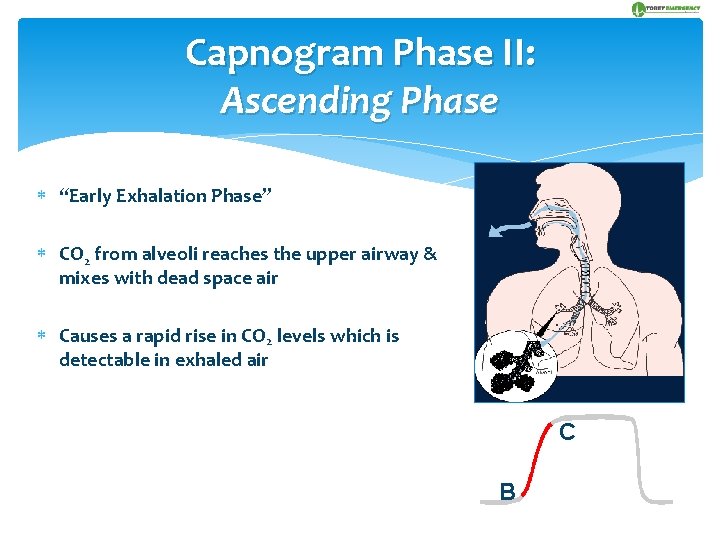
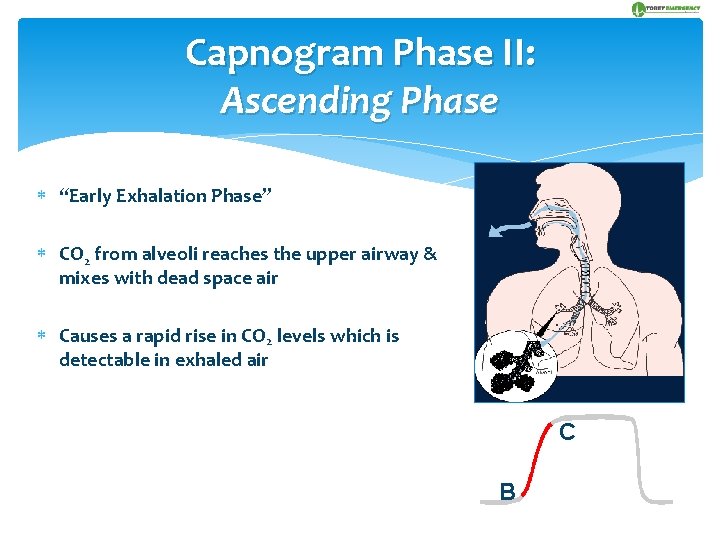
Capnogram Phase II: Ascending Phase “Early Exhalation Phase” CO 2 from alveoli reaches the upper airway & mixes with dead space air Causes a rapid rise in CO 2 levels which is detectable in exhaled air C B
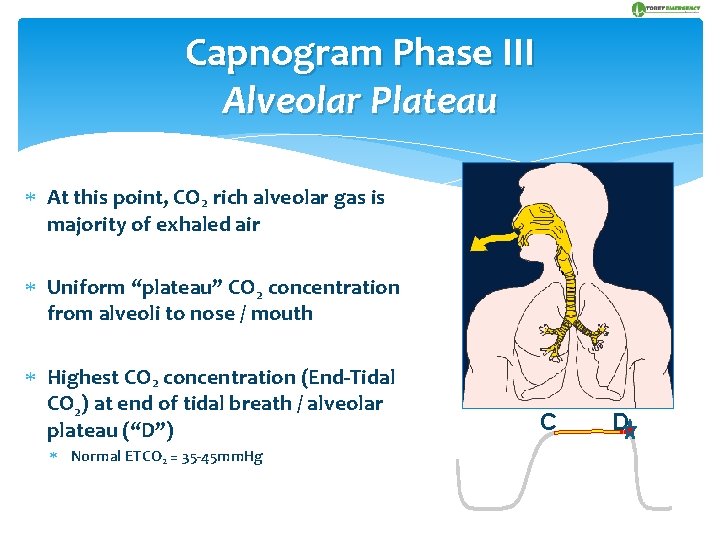
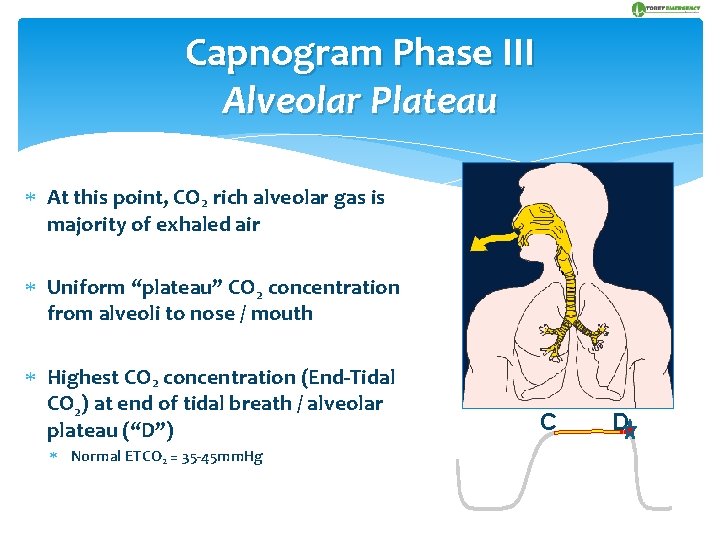
Capnogram Phase III Alveolar Plateau At this point, CO 2 rich alveolar gas is majority of exhaled air Uniform “plateau” CO 2 concentration from alveoli to nose / mouth Highest CO 2 concentration (End-Tidal CO 2) at end of tidal breath / alveolar plateau (“D”) Normal ETCO 2 = 35 -45 mm. Hg C D
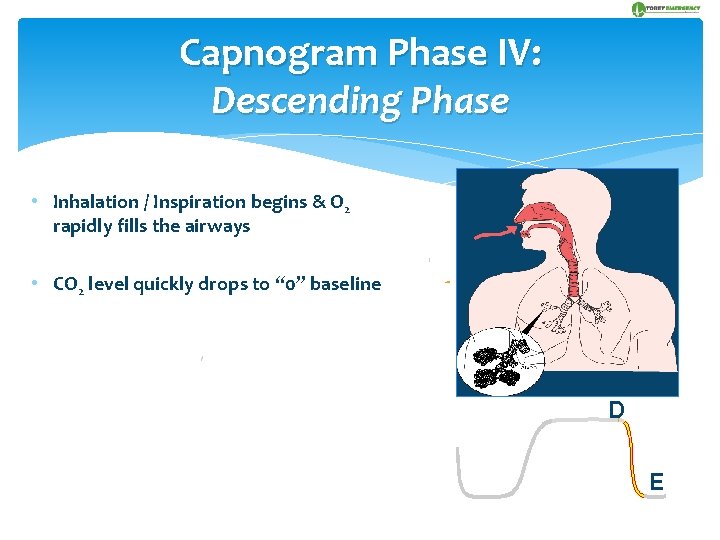
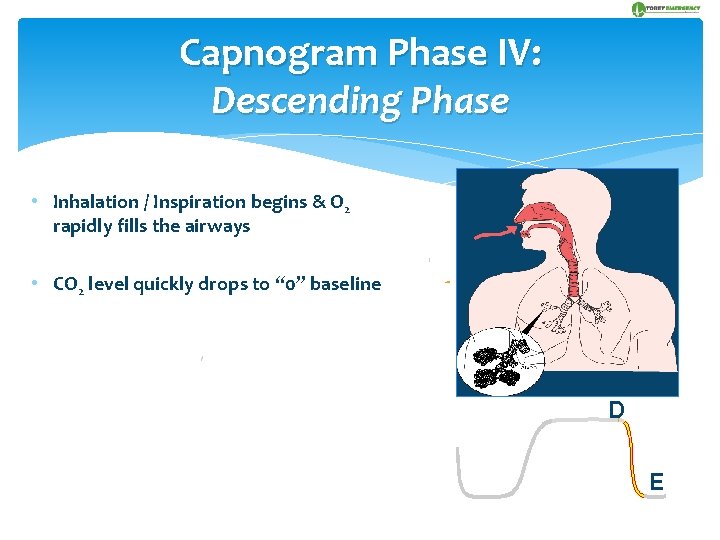
Capnogram Phase IV: Descending Phase • Inhalation / Inspiration begins & O 2 rapidly fills the airways • CO 2 level quickly drops to “ 0” baseline D E
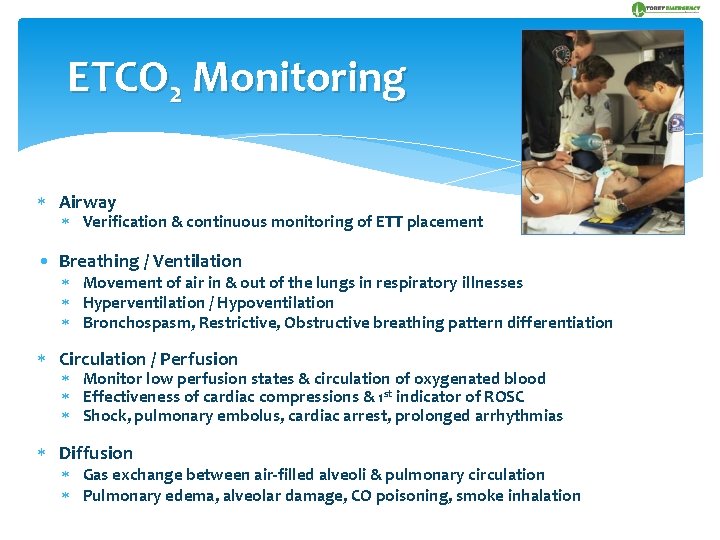
ETCO 2 Monitoring Airway Verification & continuous monitoring of ETT placement • Breathing / Ventilation Movement of air in & out of the lungs in respiratory illnesses Hyperventilation / Hypoventilation Bronchospasm, Restrictive, Obstructive breathing pattern differentiation Circulation / Perfusion Monitor low perfusion states & circulation of oxygenated blood Effectiveness of cardiac compressions & 1 st indicator of ROSC Shock, pulmonary embolus, cardiac arrest, prolonged arrhythmias Diffusion Gas exchange between air-filled alveoli & pulmonary circulation Pulmonary edema, alveolar damage, CO poisoning, smoke inhalation
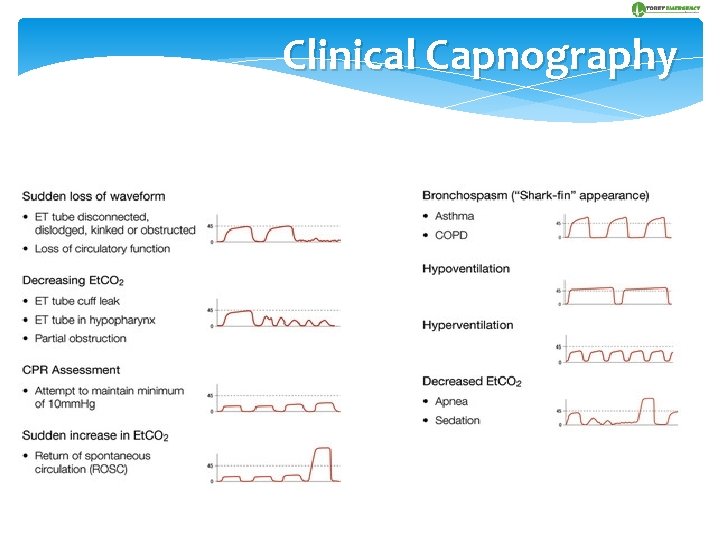
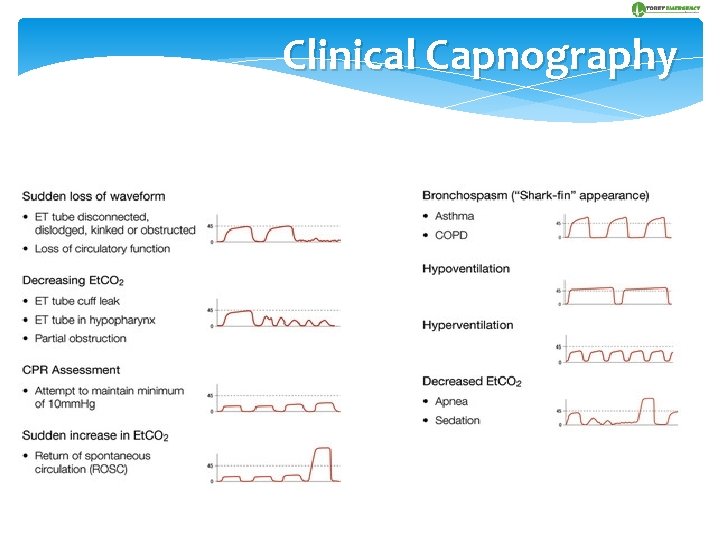
Clinical Capnography
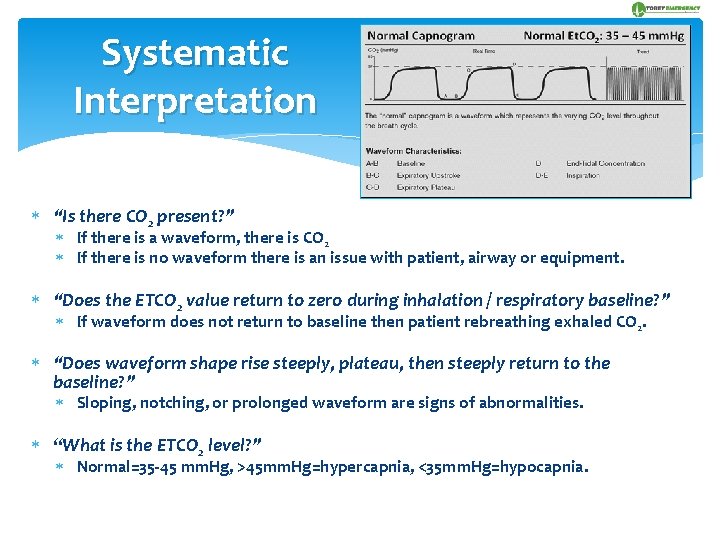
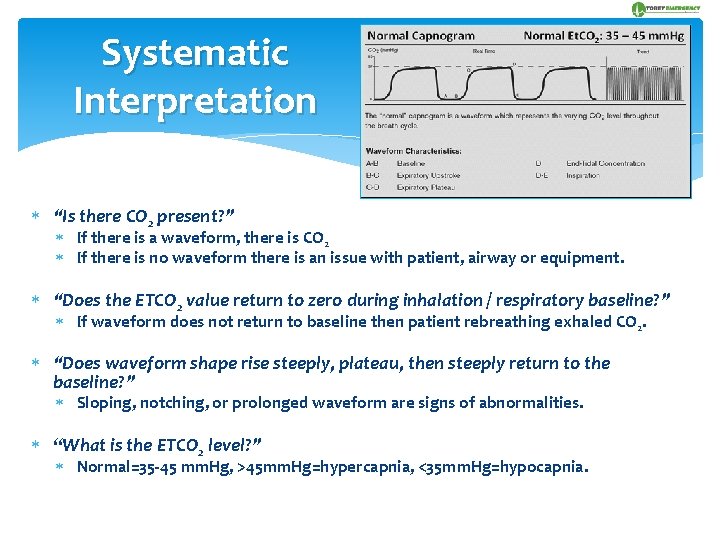
Systematic Interpretation “Is there CO 2 present? ” If there is a waveform, there is CO 2 If there is no waveform there is an issue with patient, airway or equipment. “Does the ETCO 2 value return to zero during inhalation / respiratory baseline? ” If waveform does not return to baseline then patient rebreathing exhaled CO 2. “Does waveform shape rise steeply, plateau, then steeply return to the baseline? ” Sloping, notching, or prolonged waveform are signs of abnormalities. “What is the ETCO 2 level? ” Normal=35 -45 mm. Hg, >45 mm. Hg=hypercapnia, <35 mm. Hg=hypocapnia.
Intubated Patients (Non-Arrest) Verify & continuously confirm ETT placement Immediately detect ETT position changes Optimize ventilation management
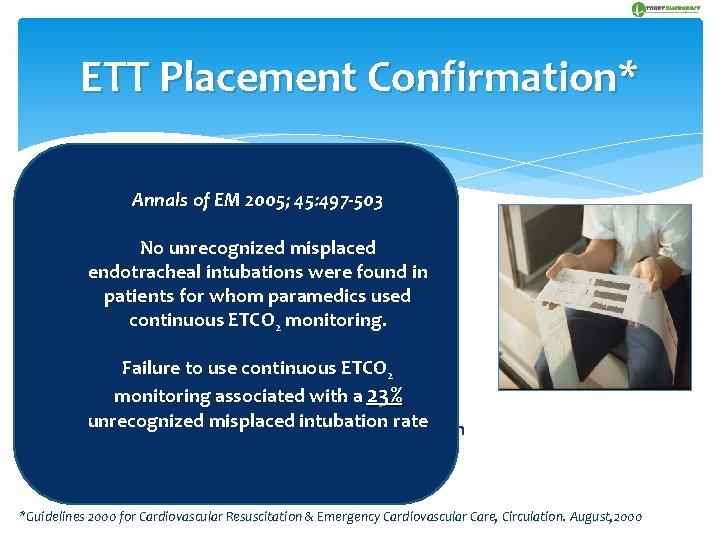
ETT Placement Confirmation* Annals 2005; 45: 497 -503 Standard of care of for. EM confirmation & monitoring of the intubated patient is waveform capnography, pulse oximetry, & physical No unrecognized misplaced confirmation (i. e. auscultation, tube found fog) in endotracheal intubations were patients for whom paramedics used Presence continuous of exhaled CO tracheal 2 indicates ETCO 2 monitoring. placement within seconds of proper placement Esophageal ETT placement may briefly detect CO 2 Failure“washed to use continuous 2 but residuals out” within 6 ETCO positivepressure ventilations monitoring associated with a 23% Gastric CO 2 from: carbonated beverages, Tums, unrecognized misplaced intubation rate gastric distention from mouth to mouth ventilation *Guidelines 2000 for Cardiovascular Resuscitation & Emergency Cardiovascular Care, Circulation. August, 2000
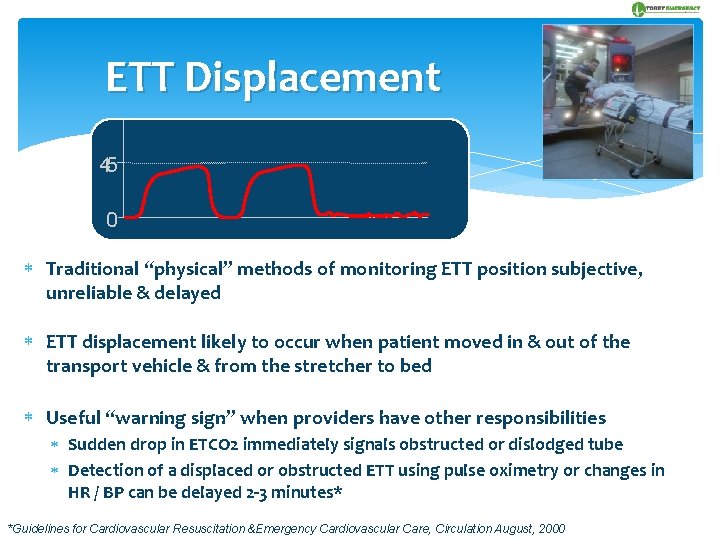
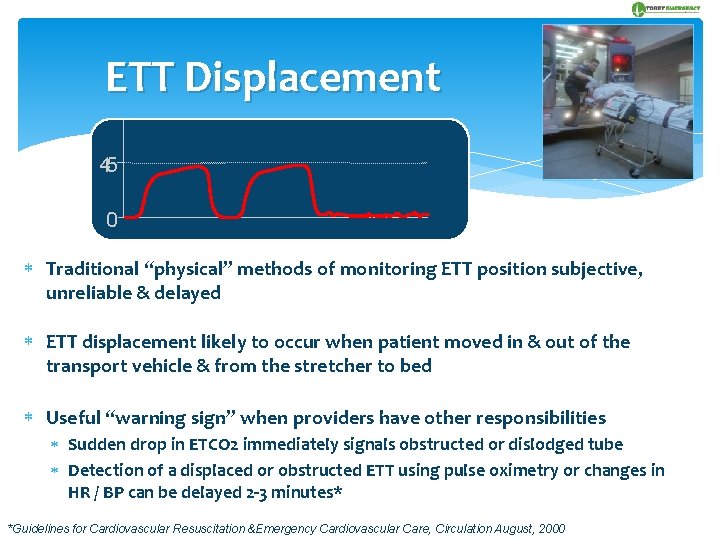
ETT Displacement 45 0 Traditional “physical” methods of monitoring ETT position subjective, unreliable & delayed ETT displacement likely to occur when patient moved in & out of the transport vehicle & from the stretcher to bed Useful “warning sign” when providers have other responsibilities Sudden drop in ETCO 2 immediately signals obstructed or dislodged tube Detection of a displaced or obstructed ETT using pulse oximetry or changes in HR / BP can be delayed 2 -3 minutes* *Guidelines for Cardiovascular Resuscitation &Emergency Cardiovascular Care, Circulation August, 2000
How Good Is ETCO 2 In the Intubated Patient ? 1999: 1 st research demonstrating efficacy of ETCO 2 in prehospital ETI: “Confirmation of Airway Placement” (Sayre, M. PEC) Silvestri S. “Improvement in Misplaced ETT Recognition within a Regional EMS System” (AEM. 2003) 108 patients intubated in the field 52 trauma, 56 medical patients 108 patients intubated in the field ETT placement at ED arrival showed 27 pts (25%) had improperly placed ETT 18 esophageal, 9 oropharyngeal No patients with quantitative capnography had misplaced ETTs 9% had improperly placed ETT No unrecognized misplaced ETT in pts with continuous ETCO 2 monitoring
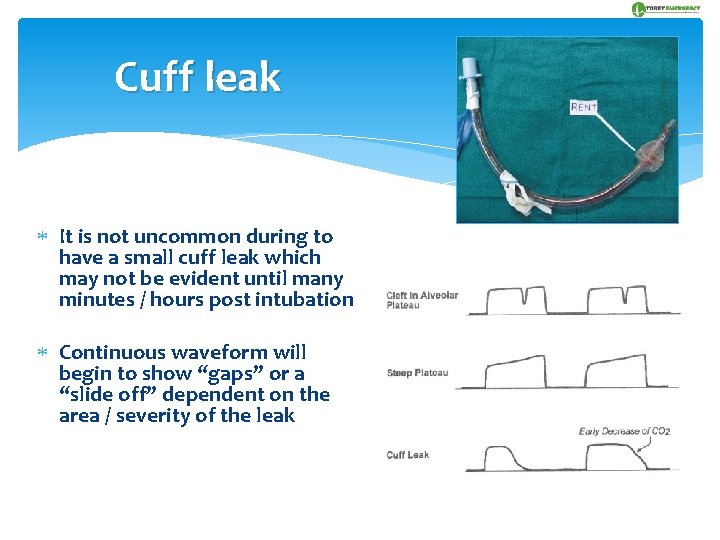
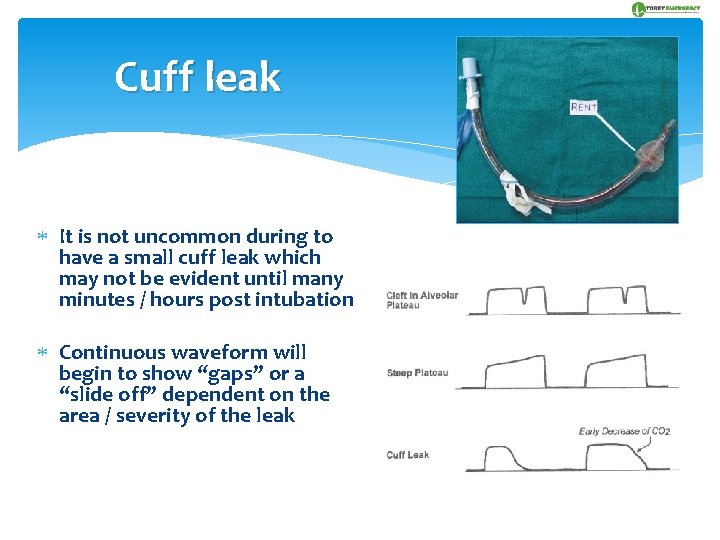
Cuff leak It is not uncommon during to have a small cuff leak which may not be evident until many minutes / hours post intubation Continuous waveform will begin to show “gaps” or a “slide off” dependent on the area / severity of the leak
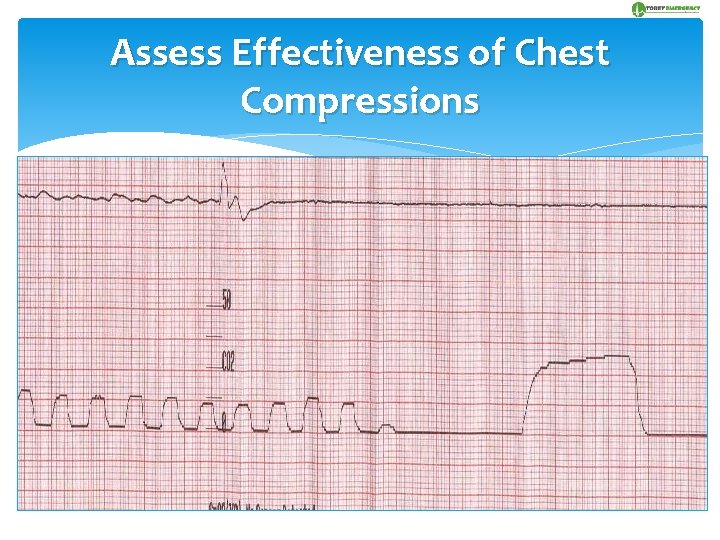
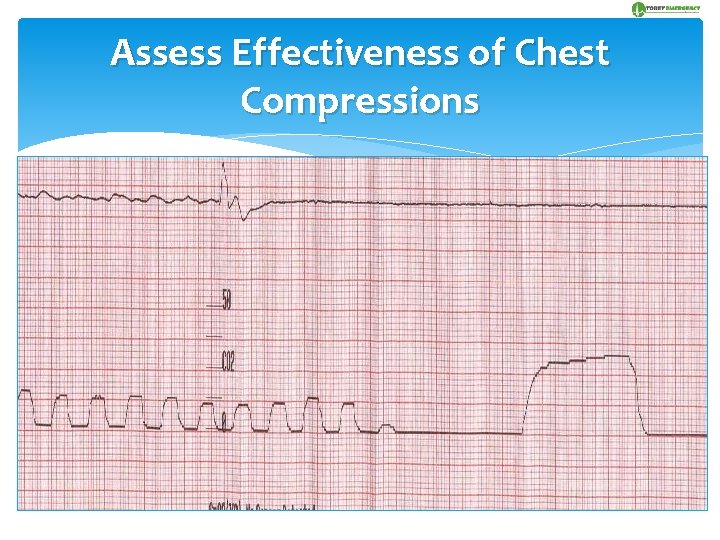
Assess Effectiveness of Chest Compressions With constant ventilation, non-invasive capnography correlates with the blood flow / circulatory status produced by compressions Good correlation between ETCO 2 & cardiac output Low cardiac output reduces blood flow to the lungs & fails to clear CO 2 from the bloodstream Properly done chest compressions provide 25 -30% of normal blood supply to the brain 5%-10% of normal blood supply to the heart Adequate chest compressions promote the elimination of metabolic wastes A spike in ETCO 2 indicates ROSC prior to any other “vital” sign
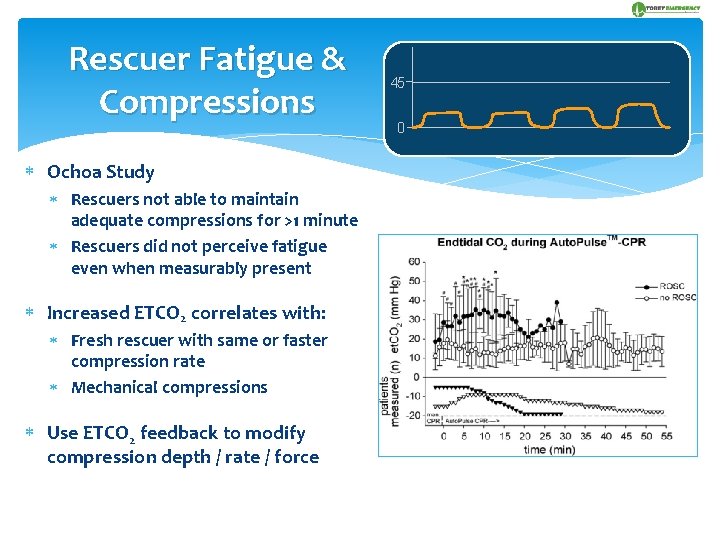
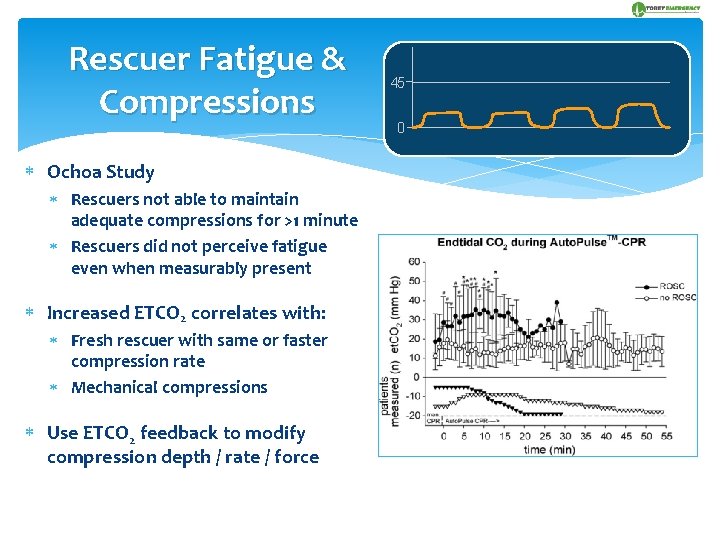
Rescuer Fatigue & Compressions Ochoa Study Rescuers not able to maintain adequate compressions for >1 minute Rescuers did not perceive fatigue even when measurably present Increased ETCO 2 correlates with: Fresh rescuer with same or faster compression rate Mechanical compressions Use ETCO 2 feedback to modify compression depth / rate / force 45 0
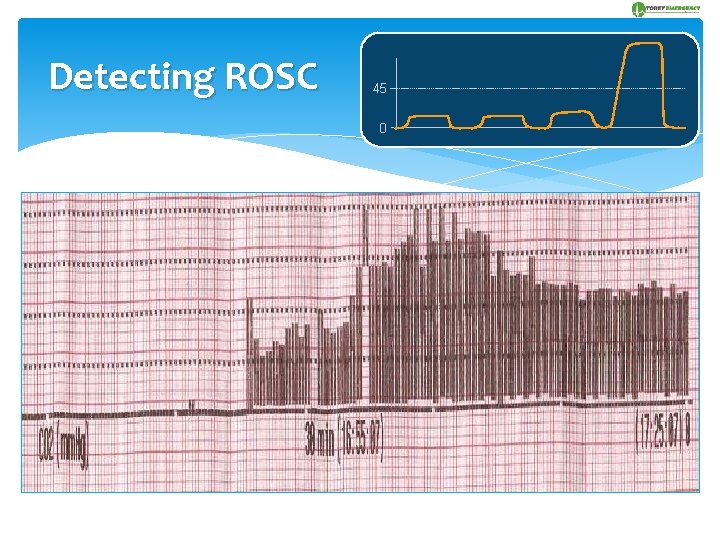
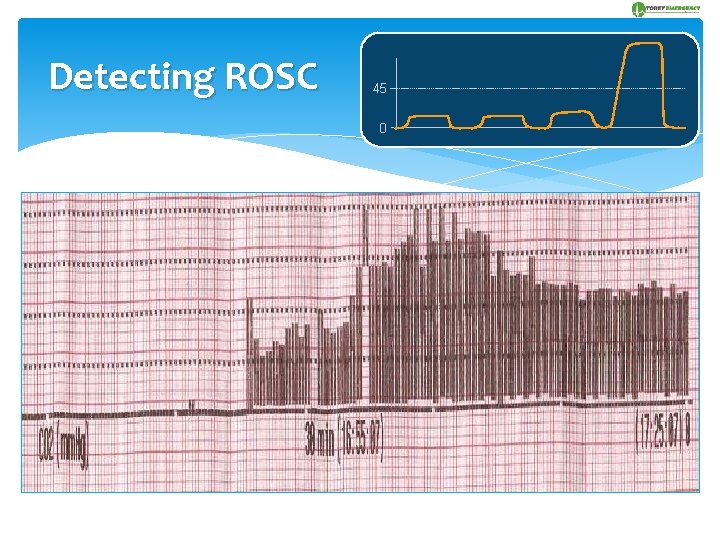
Detecting ROSC 45 0 Continuous ETCO 2 an almost immediate indicator of successful resuscitation Sudden increase in ETCO 2 is an indicator that cellular metabolism has resumed & that pulses soon to be regained (cardiac output increasing) Arrhythmia / arterial vasoconstriction makes pulses initially difficult to detect After 2 mins, briefly stop CPR & check for organized rhythm on ECG monitor Capnography predicts probability of successful outcome following resuscitation & may be used in the decision to cease resuscitation efforts ETCO 2 <10 mm. Hg throughout the duration of a code signals a poor outcome.
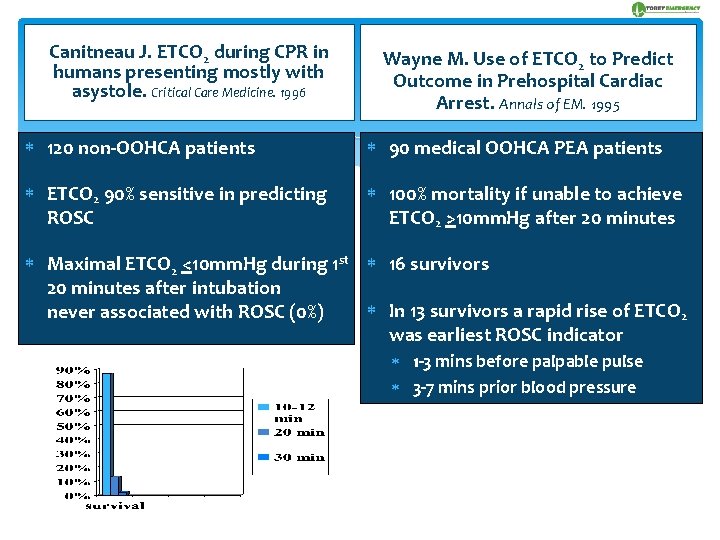
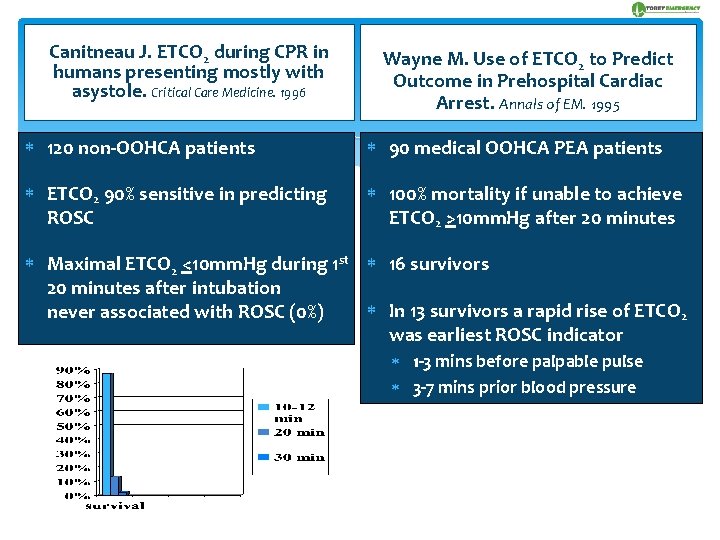
Canitneau J. ETCO 2 during CPR in humans presenting mostly with asystole. Critical Care Medicine. 1996 Wayne M. Use of ETCO 2 to Predict Outcome in Prehospital Cardiac Arrest. Annals of EM. 1995 120 non-OOHCA patients 90 medical OOHCA PEA patients ETCO 2 90% sensitive in predicting ROSC 100% mortality if unable to achieve ETCO 2 >10 mm. Hg after 20 minutes Maximal ETCO 2 <10 mm. Hg during 1 st 16 survivors 20 minutes after intubation In 13 survivors a rapid rise of ETCO 2 never associated with ROSC (0%) was earliest ROSC indicator 1 -3 mins before palpable pulse 3 -7 mins prior blood pressure
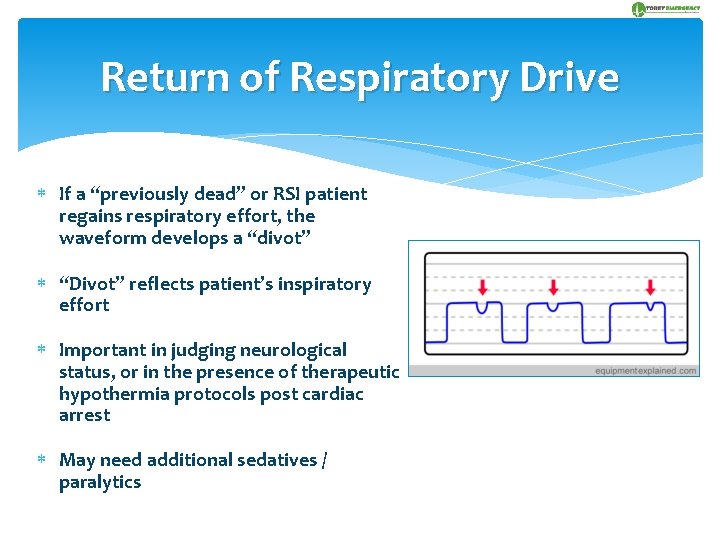
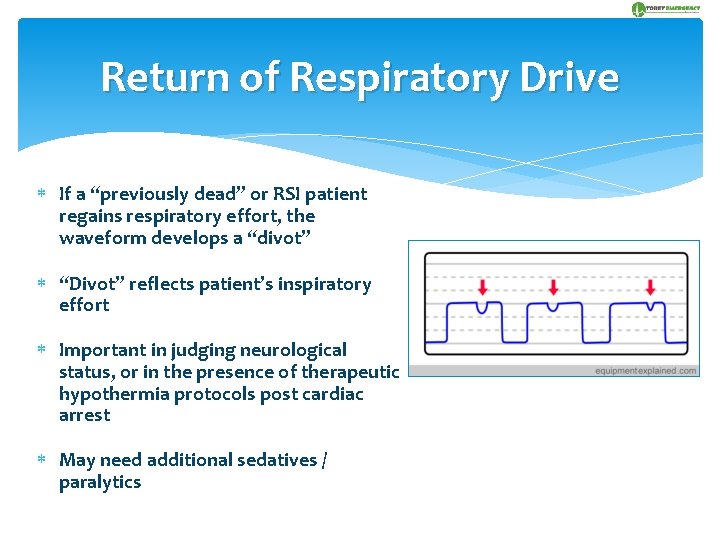
Return of Respiratory Drive If a “previously dead” or RSI patient regains respiratory effort, the waveform develops a “divot” “Divot” reflects patient’s inspiratory effort Important in judging neurological status, or in the presence of therapeutic hypothermia protocols post cardiac arrest May need additional sedatives / paralytics
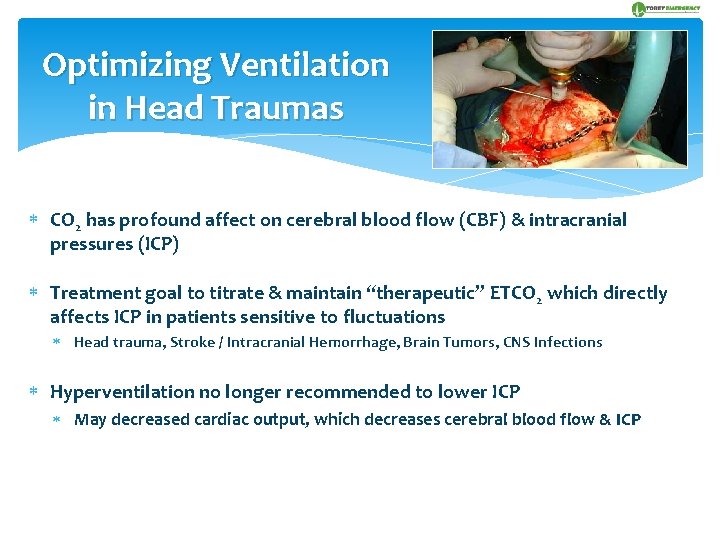
Optimizing Ventilation in Head Traumas CO 2 has profound affect on cerebral blood flow (CBF) & intracranial pressures (ICP) Treatment goal to titrate & maintain “therapeutic” ETCO 2 which directly affects ICP in patients sensitive to fluctuations Head trauma, Stroke / Intracranial Hemorrhage, Brain Tumors, CNS Infections Hyperventilation no longer recommended to lower ICP May decreased cardiac output, which decreases cerebral blood flow & ICP
Head Trauma Ventilation Goals Current critical care recommendations (Class IIa) are to ventilate head trauma patients to achieve normocarbia ETCO 2 25 -30 mm. HG causes mild cerebral vasoconstriction decreasing ICP Hypoventilation increases CO 2 levels Increases cerebral hypoxia which causes cerebral vasodilation Cerebral hypoxia increases CBF to counter cerebral hypoxia, but increased CBF increases ICP which worsens brain edema & secondary brain injury Hyperventilation decreases CO 2 levels Causes cerebral vasoconstriction decreasing ICP, but increases cerebral hypoxia
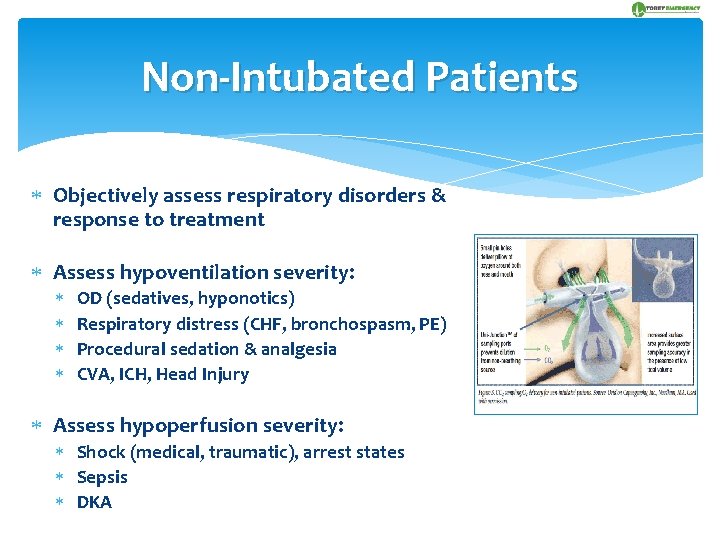
Non-Intubated Patients Objectively assess respiratory disorders & response to treatment Assess hypoventilation severity: OD (sedatives, hyponotics) Respiratory distress (CHF, bronchospasm, PE) Procedural sedation & analgesia CVA, ICH, Head Injury Assess hypoperfusion severity: Shock (medical, traumatic), arrest states Sepsis DKA
Non-Intubated Patients Identify problem Assess patient’s status & anticipate sudden changes Monitor treatments for respiratory, medical & traumatic processes Ventilation: movement of gases in & out of lungs Diffusion: gas exchange between oxygenated alveoli & pulmonary circulation Perfusion: blood circulation through arterial & venous systems
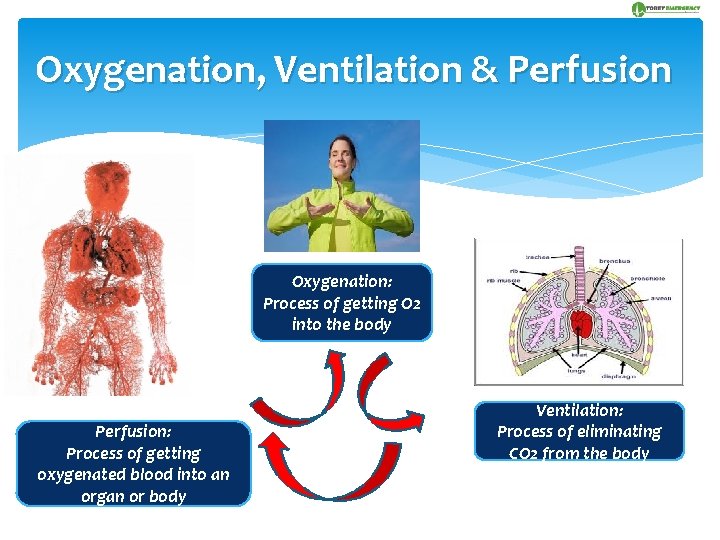
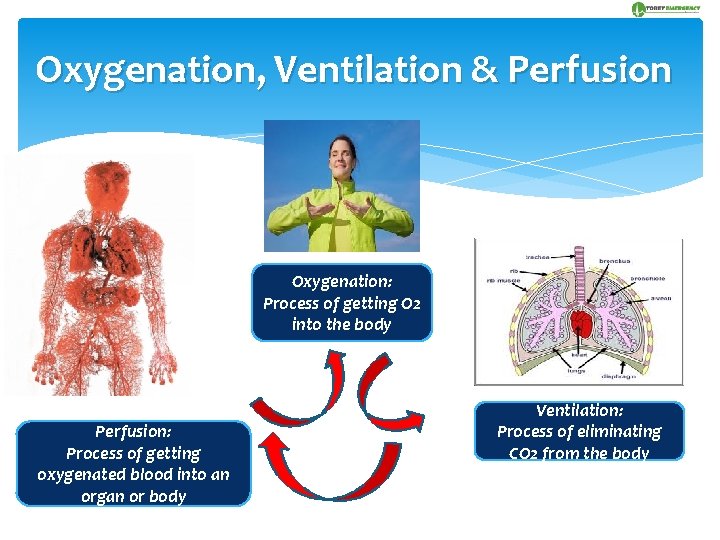
Oxygenation, Ventilation & Perfusion Oxygenation: Process of getting O 2 into the body Perfusion: Process of getting oxygenated blood into an organ or body Ventilation: Process of eliminating CO 2 from the body
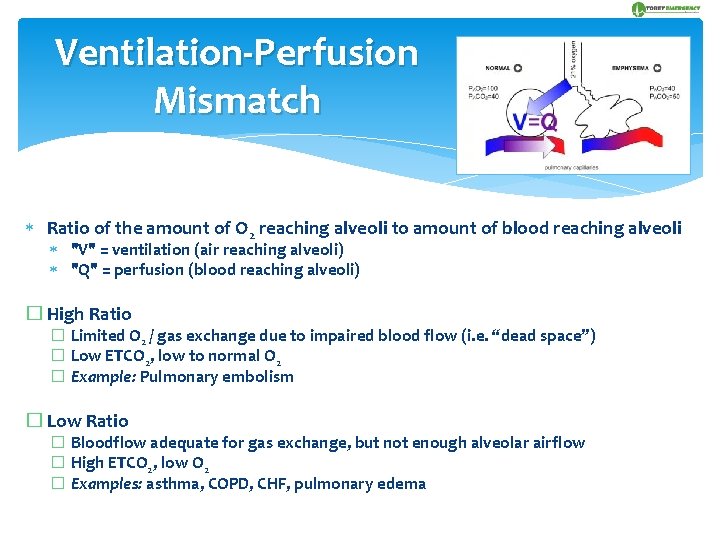
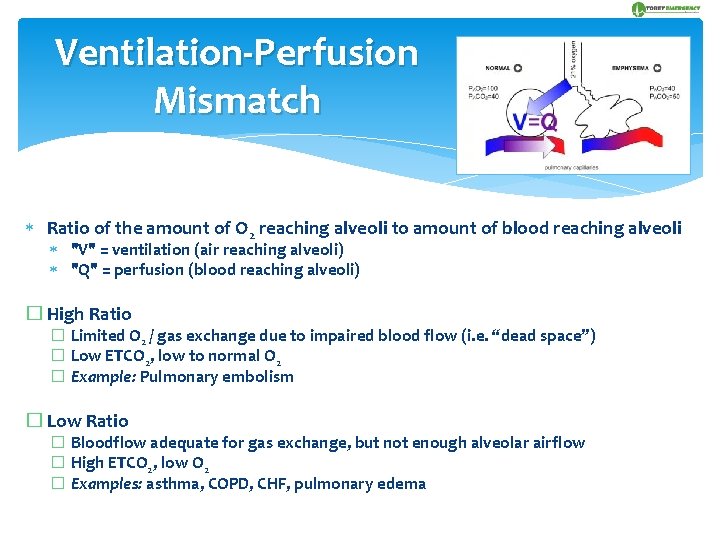
Ventilation-Perfusion Mismatch Ratio of the amount of O 2 reaching alveoli to amount of blood reaching alveoli "V" = ventilation (air reaching alveoli) "Q" = perfusion (blood reaching alveoli) � High Ratio � Limited O 2 / gas exchange due to impaired blood flow (i. e. “dead space”) � Low ETCO 2, low to normal O 2 � Example: Pulmonary embolism � Low Ratio � Bloodflow adequate for gas exchange, but not enough alveolar airflow � High ETCO 2, low O 2 � Examples: asthma, COPD, CHF, pulmonary edema
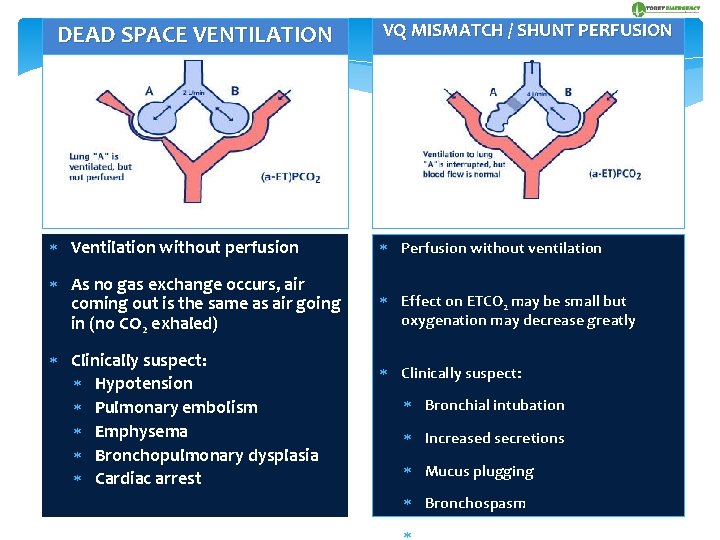
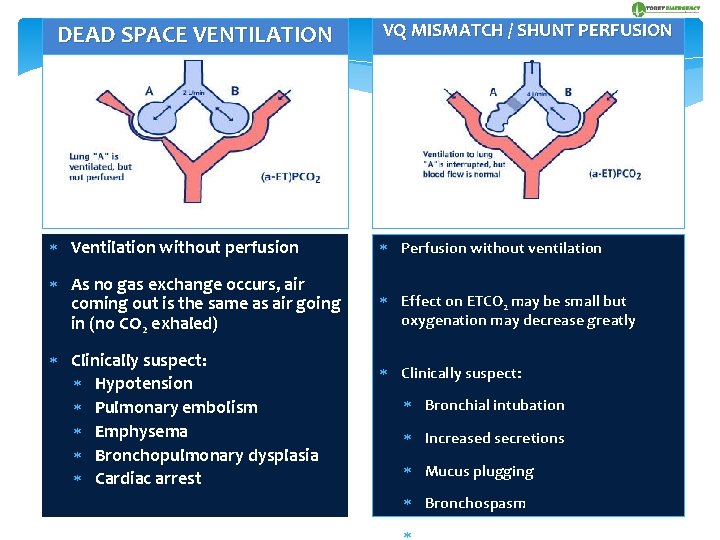
DEAD SPACE VENTILATION VQ MISMATCH / SHUNT PERFUSION Ventilation without perfusion Perfusion without ventilation As no gas exchange occurs, air coming out is the same as air going in (no CO 2 exhaled) Effect on ETCO 2 may be small but oxygenation may decrease greatly Clinically suspect: Hypotension Pulmonary embolism Emphysema Bronchopulmonary dysplasia Cardiac arrest Clinically suspect: Bronchial intubation Increased secretions Mucus plugging Bronchospasm
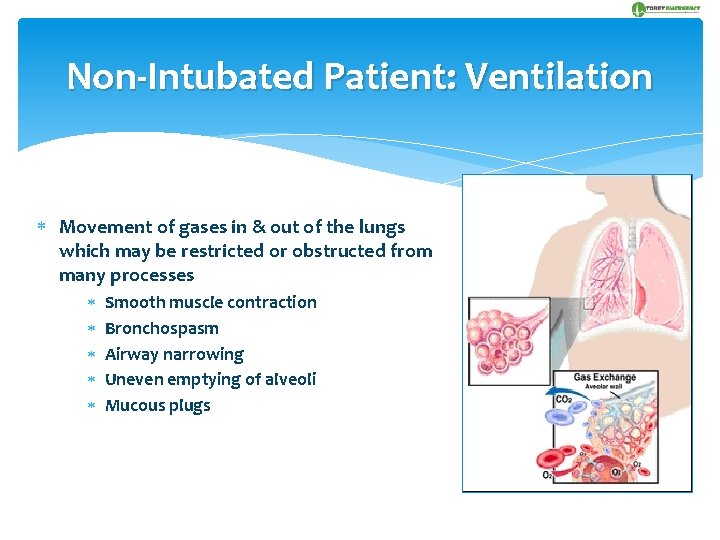
Non-Intubated Patient: Ventilation Movement of gases in & out of the lungs which may be restricted or obstructed from many processes Smooth muscle contraction Bronchospasm Airway narrowing Uneven emptying of alveoli Mucous plugs
Non-Intubated Patient: Diffusion Gas exchange between air-filled alveoli & pulmonary circulation Inflammation Retained secretions Fibrosis Decreased compliance of alveoli walls Chronic airway modeling (COPD) Reversible airway disease (asthma)
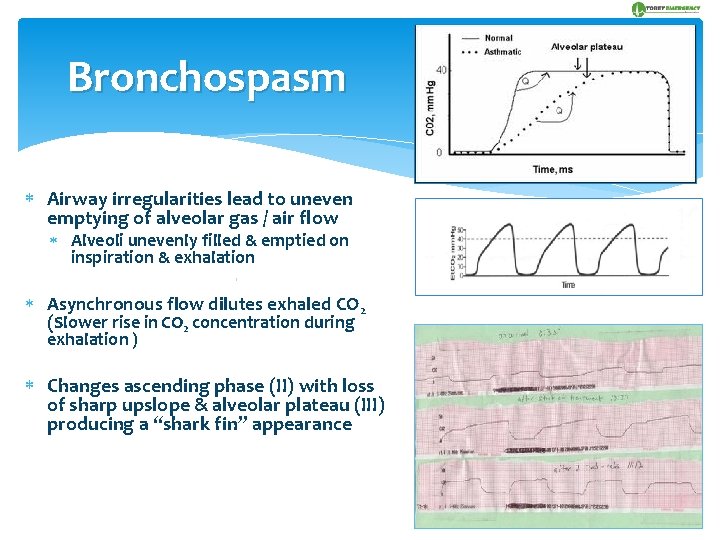
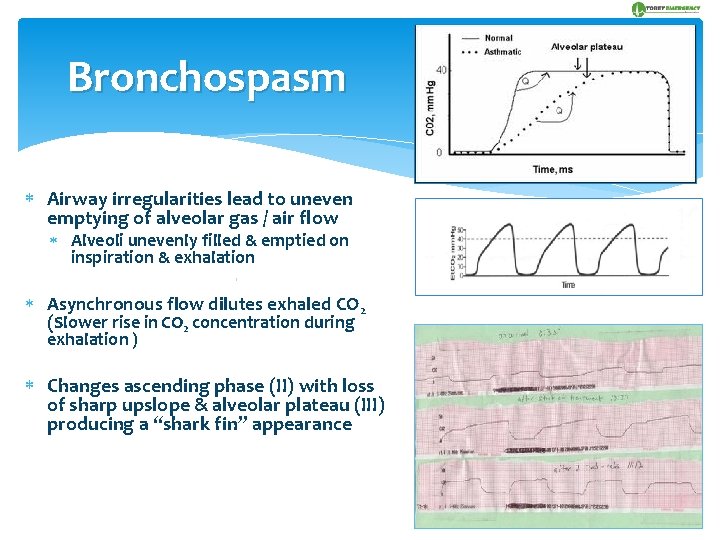
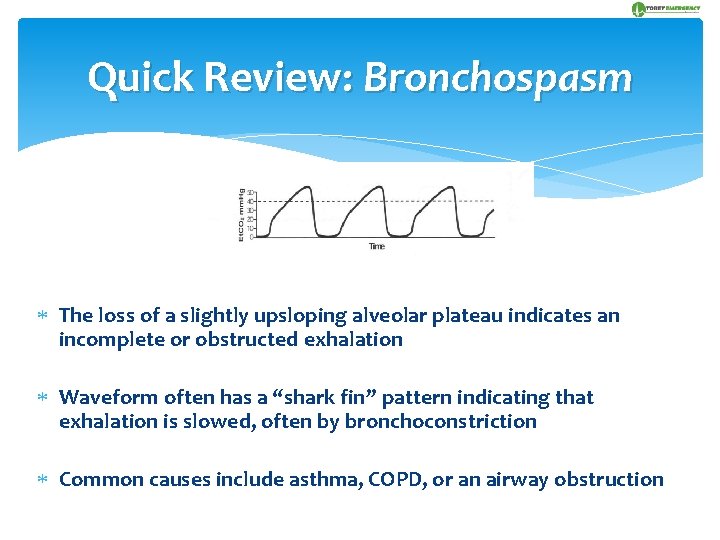
Bronchospasm Airway irregularities lead to uneven emptying of alveolar gas / air flow Alveoli unevenly filled & emptied on inspiration & exhalation Asynchronous flow dilutes exhaled CO 2 (Slower rise in CO 2 concentration during exhalation ) Changes ascending phase (II) with loss of sharp upslope & alveolar plateau (III) producing a “shark fin” appearance
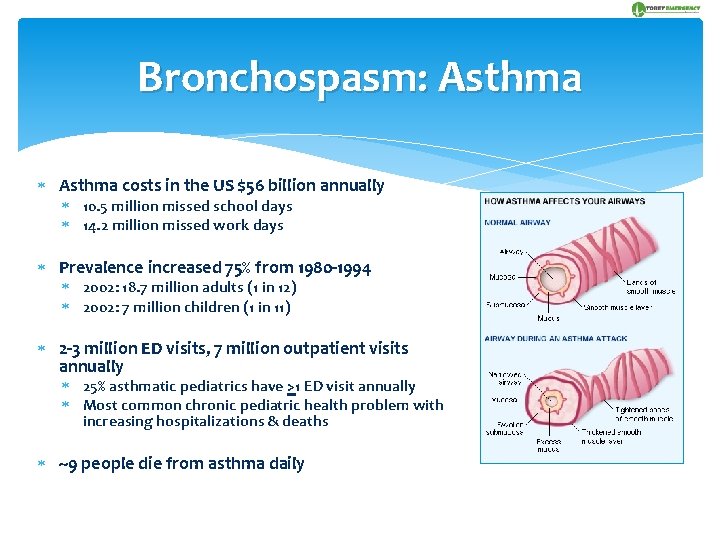
Bronchospasm: Asthma costs in the US $56 billion annually 10. 5 million missed school days 14. 2 million missed work days Prevalence increased 75% from 1980 -1994 2002: 18. 7 million adults (1 in 12) 2002: 7 million children (1 in 11) 2 -3 million ED visits, 7 million outpatient visits annually 25% asthmatic pediatrics have >1 ED visit annually Most common chronic pediatric health problem with increasing hospitalizations & deaths ~9 people die from asthma daily
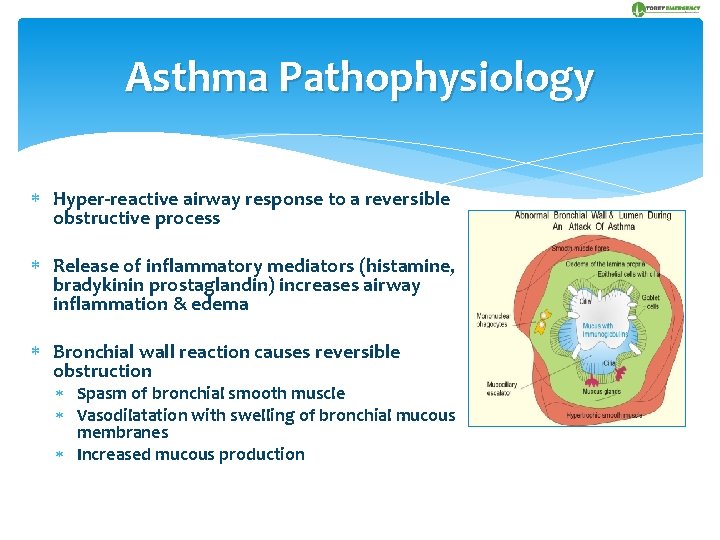
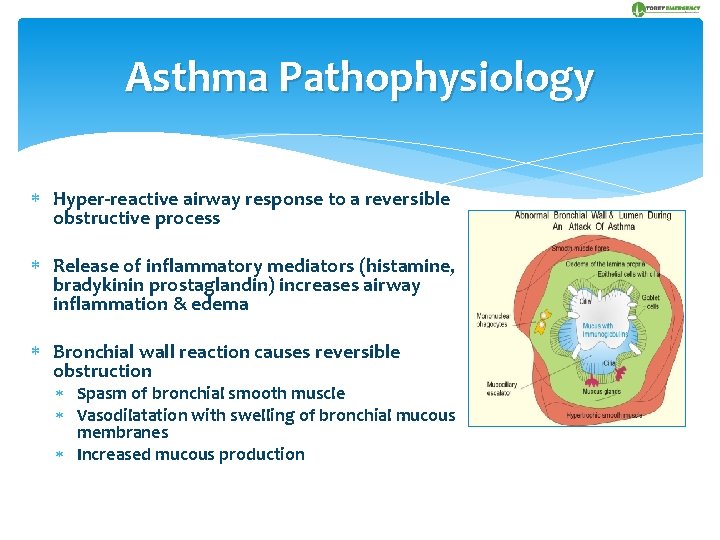
Asthma Pathophysiology Hyper-reactive airway response to a reversible obstructive process Release of inflammatory mediators (histamine, bradykinin prostaglandin) increases airway inflammation & edema Bronchial wall reaction causes reversible obstruction Spasm of bronchial smooth muscle Vasodilatation with swelling of bronchial mucous membranes Increased mucous production
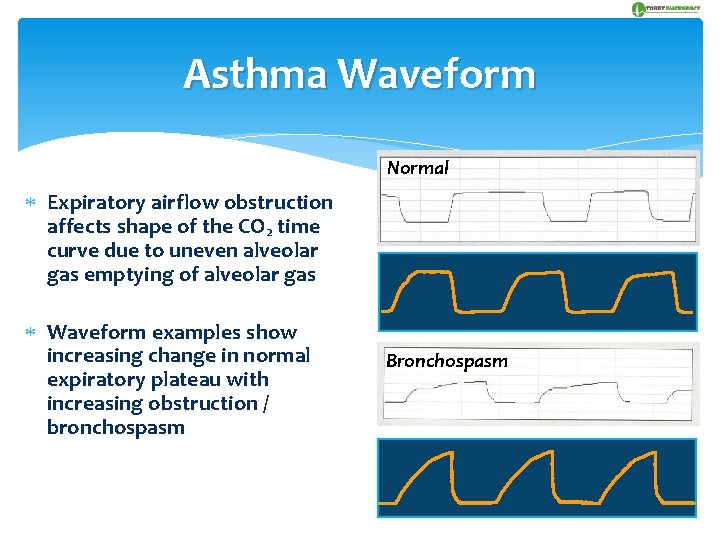
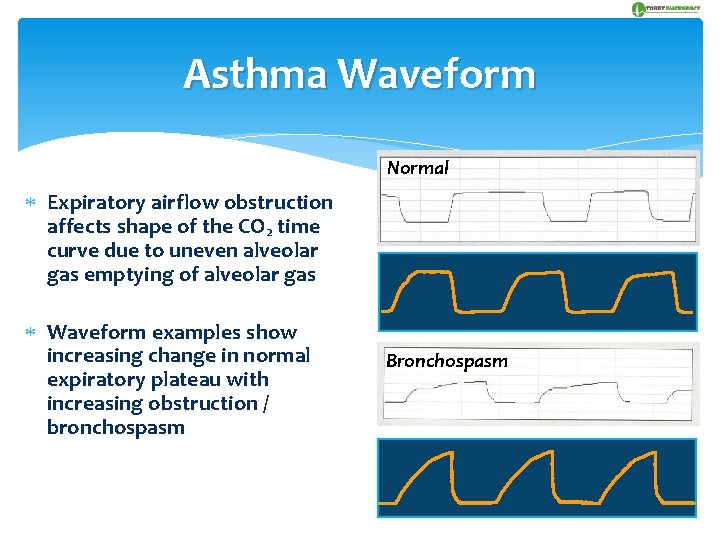
Asthma Waveform Normal Expiratory airflow obstruction affects shape of the CO 2 time curve due to uneven alveolar gas emptying of alveolar gas Waveform examples show increasing change in normal expiratory plateau with increasing obstruction / bronchospasm Bronchospasm
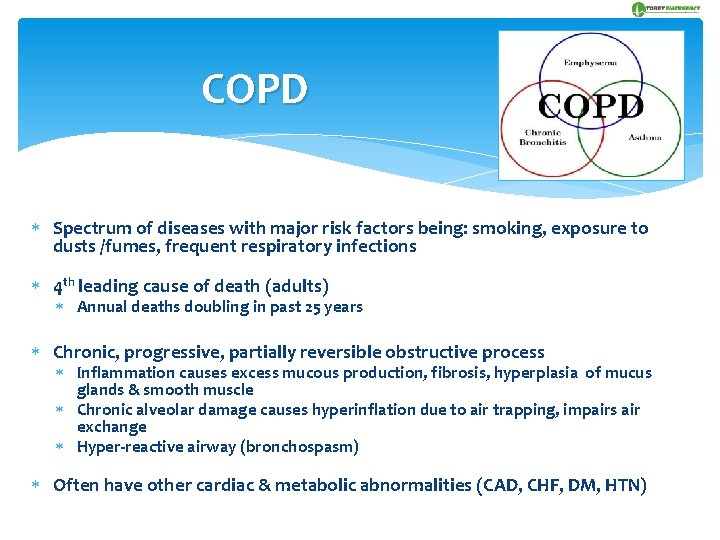
COPD Spectrum of diseases with major risk factors being: smoking, exposure to dusts /fumes, frequent respiratory infections 4 th leading cause of death (adults) Annual deaths doubling in past 25 years Chronic, progressive, partially reversible obstructive process Inflammation causes excess mucous production, fibrosis, hyperplasia of mucus glands & smooth muscle Chronic alveolar damage causes hyperinflation due to air trapping, impairs air exchange Hyper-reactive airway (bronchospasm) Often have other cardiac & metabolic abnormalities (CAD, CHF, DM, HTN)
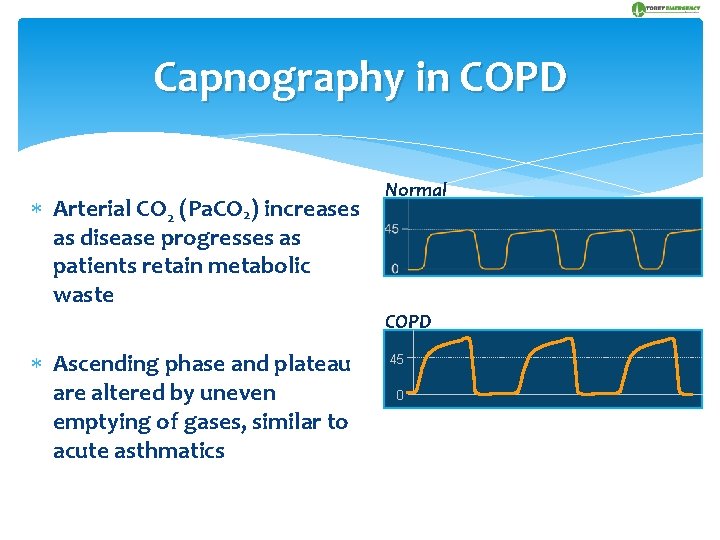
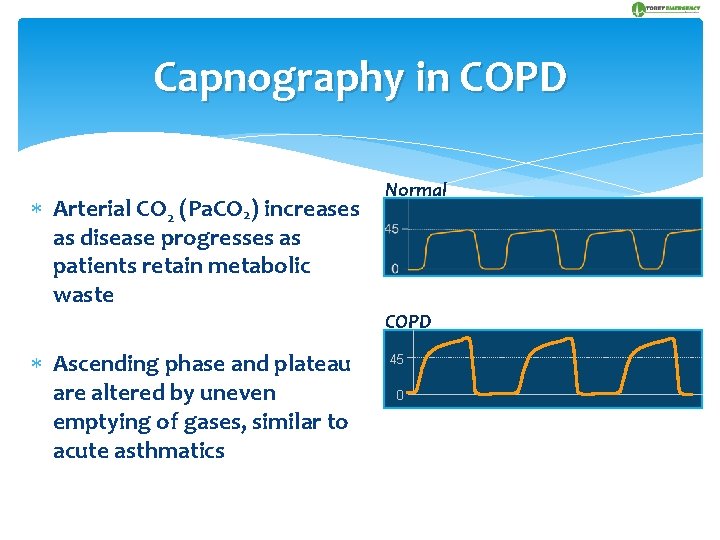
Capnography in COPD Arterial CO 2 (Pa. CO 2) increases as disease progresses as patients retain metabolic waste Normal COPD Ascending phase and plateau are altered by uneven emptying of gases, similar to acute asthmatics 45 0
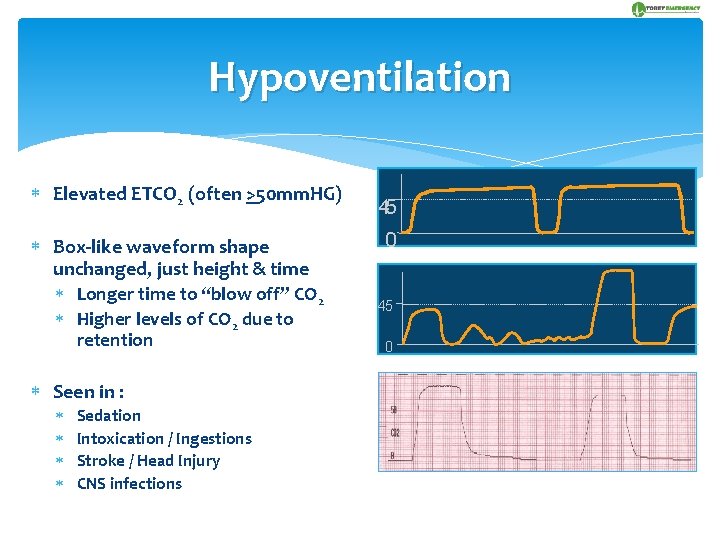
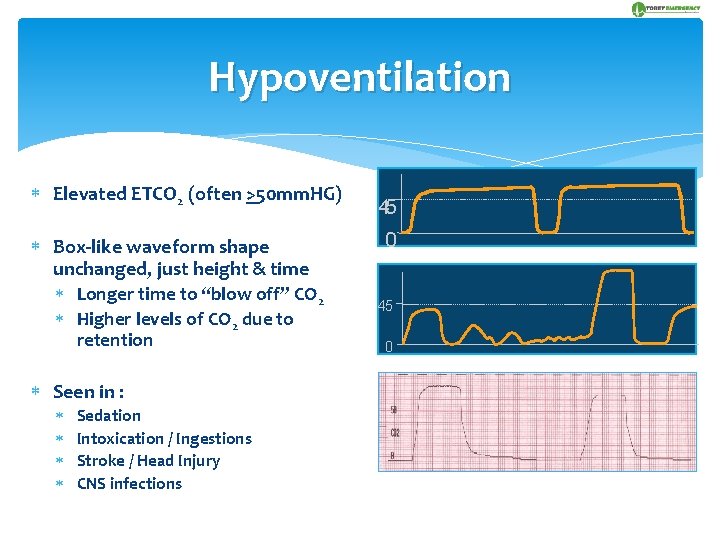
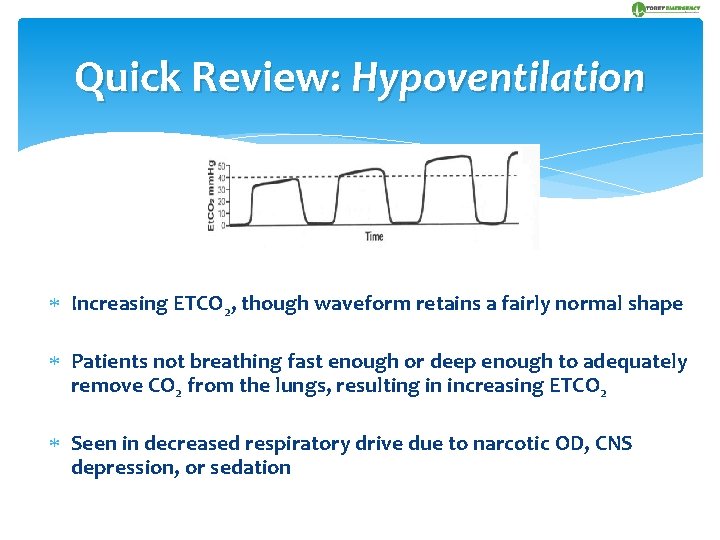
Hypoventilation Elevated ETCO 2 (often >50 mm. HG) Box-like waveform shape unchanged, just height & time Longer time to “blow off” CO 2 Higher levels of CO 2 due to retention Seen in : Sedation Intoxication / Ingestions Stroke / Head Injury CNS infections 45 0
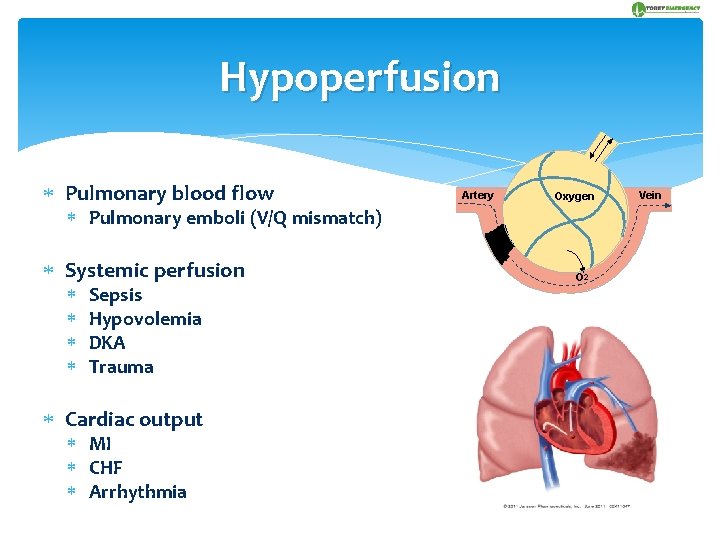
Hypoperfusion Pulmonary blood flow Artery Oxygen Pulmonary emboli (V/Q mismatch) Systemic perfusion Sepsis Hypovolemia DKA Trauma Cardiac output MI CHF Arrhythmia O 2 Vein
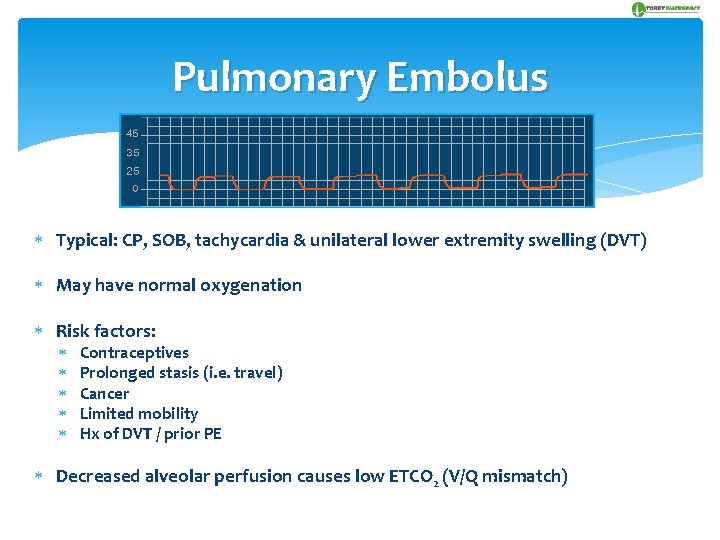
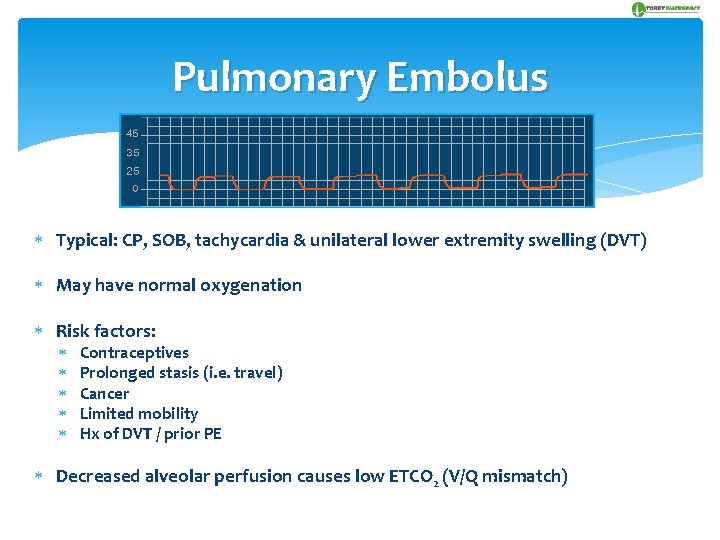
Pulmonary Embolus Typical: CP, SOB, tachycardia & unilateral lower extremity swelling (DVT) May have normal oxygenation Risk factors: Contraceptives Prolonged stasis (i. e. travel) Cancer Limited mobility Hx of DVT / prior PE Decreased alveolar perfusion causes low ETCO 2 (V/Q mismatch)
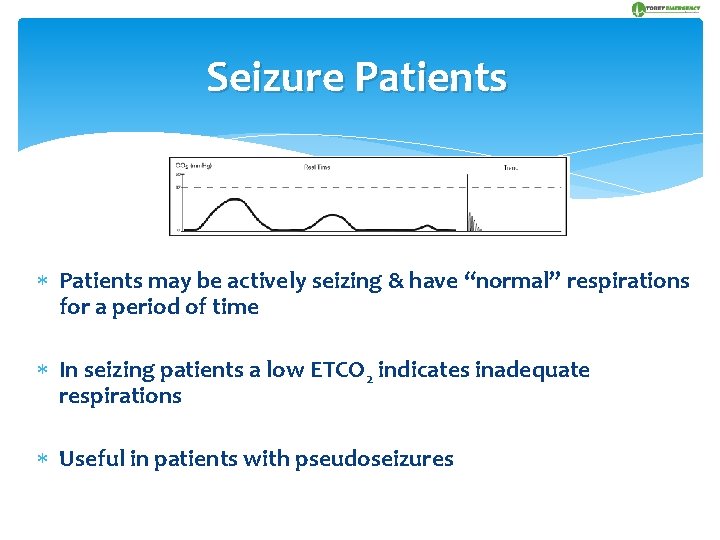
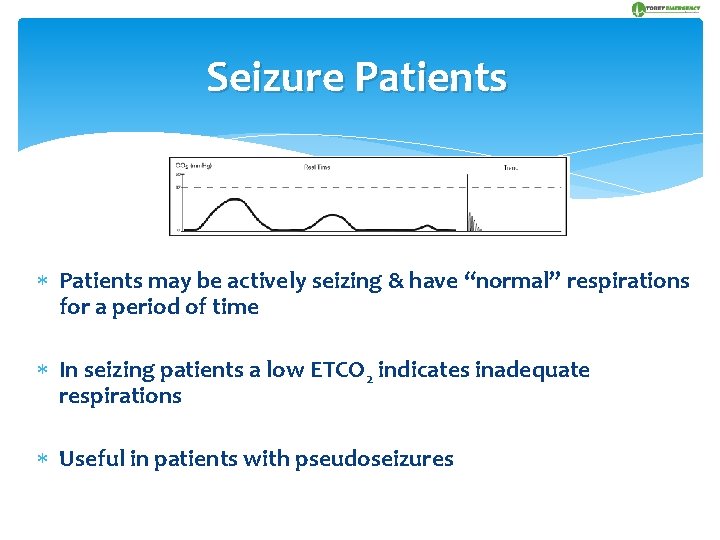
Seizure Patients may be actively seizing & have “normal” respirations for a period of time In seizing patients a low ETCO 2 indicates inadequate respirations Useful in patients with pseudoseizures
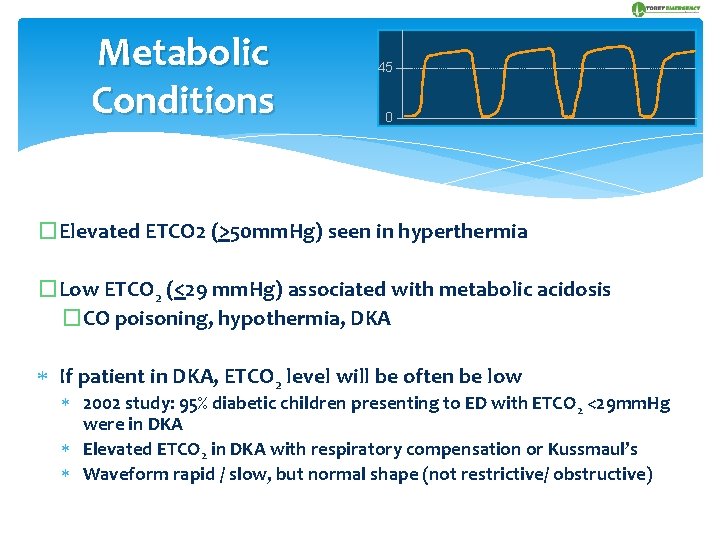
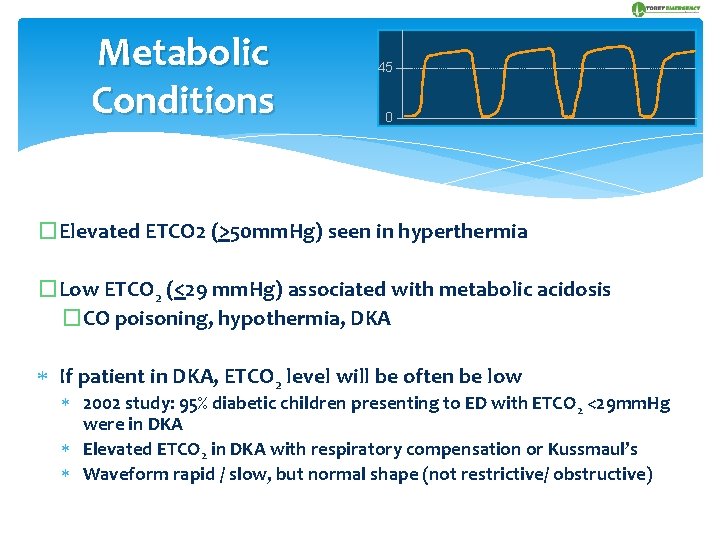
Metabolic Conditions 45 0 �Elevated ETCO 2 (>50 mm. Hg) seen in hyperthermia �Low ETCO 2 (<29 mm. Hg) associated with metabolic acidosis �CO poisoning, hypothermia, DKA If patient in DKA, ETCO 2 level will be often be low 2002 study: 95% diabetic children presenting to ED with ETCO 2 <29 mm. Hg were in DKA Elevated ETCO 2 in DKA with respiratory compensation or Kussmaul’s Waveform rapid / slow, but normal shape (not restrictive/ obstructive)
WAVEFORM REVIEW & CASE STUDIES
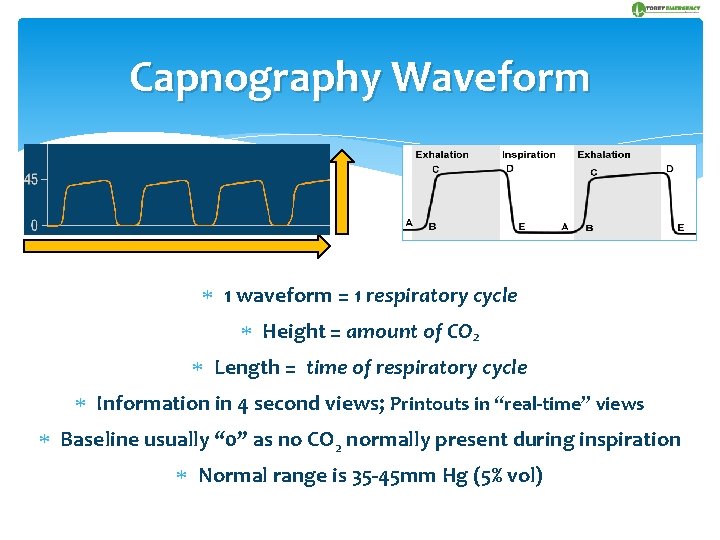
Capnography Waveform 1 waveform = 1 respiratory cycle Height = amount of CO 2 Length = time of respiratory cycle Information in 4 second views; Printouts in “real-time” views Baseline usually “ 0” as no CO 2 normally present during inspiration Normal range is 35 -45 mm Hg (5% vol)
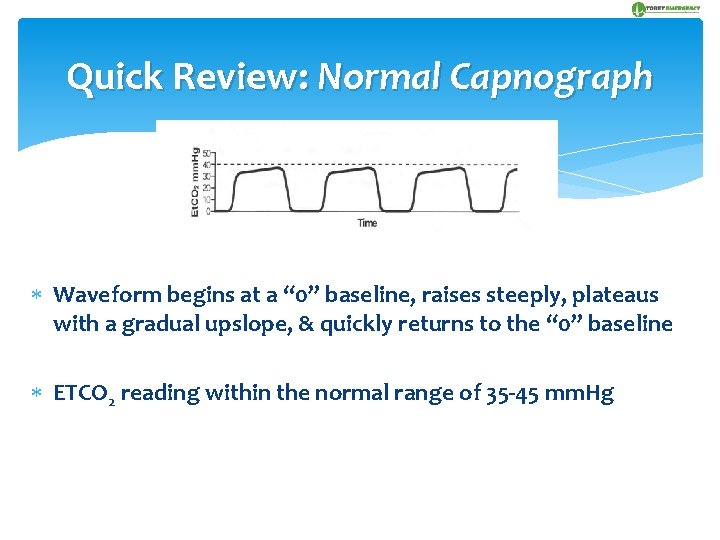
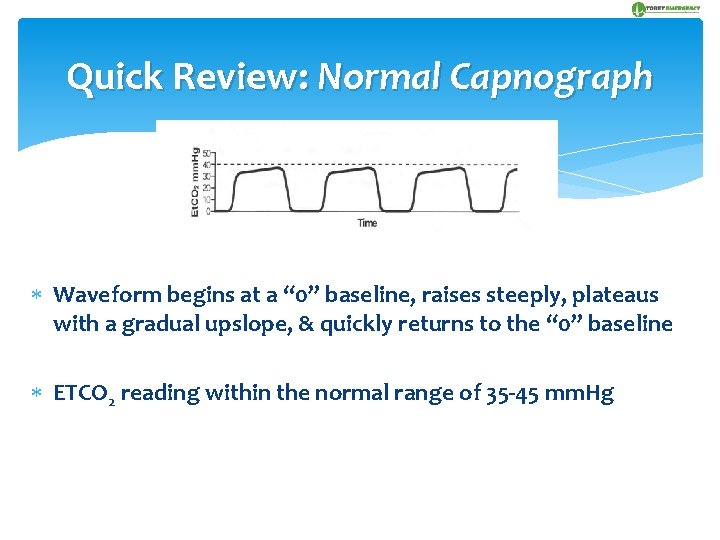
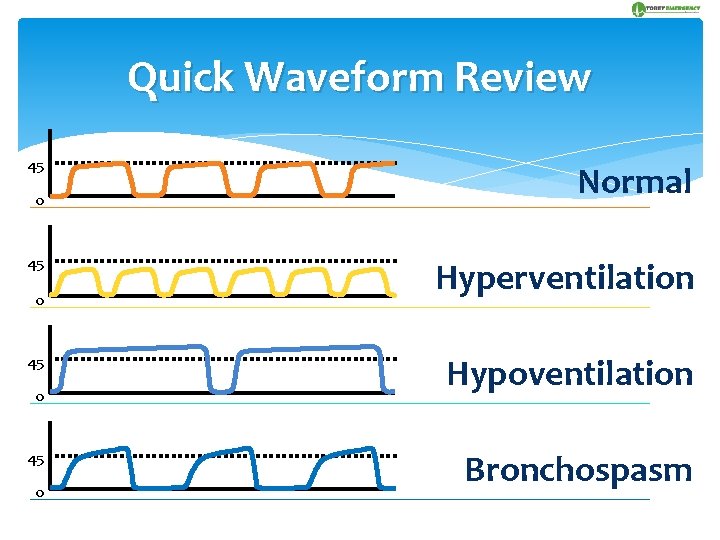
Quick Review: Normal Capnograph Waveform begins at a “ 0” baseline, raises steeply, plateaus with a gradual upslope, & quickly returns to the “ 0” baseline ETCO 2 reading within the normal range of 35 -45 mm. Hg
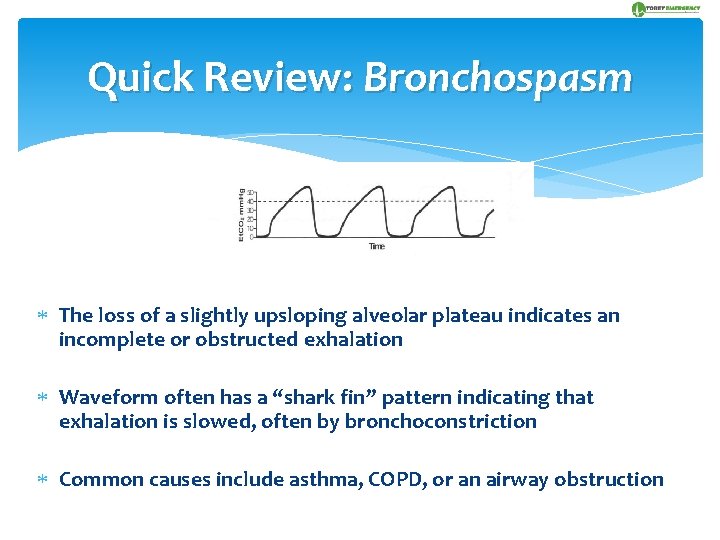
Quick Review: Bronchospasm The loss of a slightly upsloping alveolar plateau indicates an incomplete or obstructed exhalation Waveform often has a “shark fin” pattern indicating that exhalation is slowed, often by bronchoconstriction Common causes include asthma, COPD, or an airway obstruction
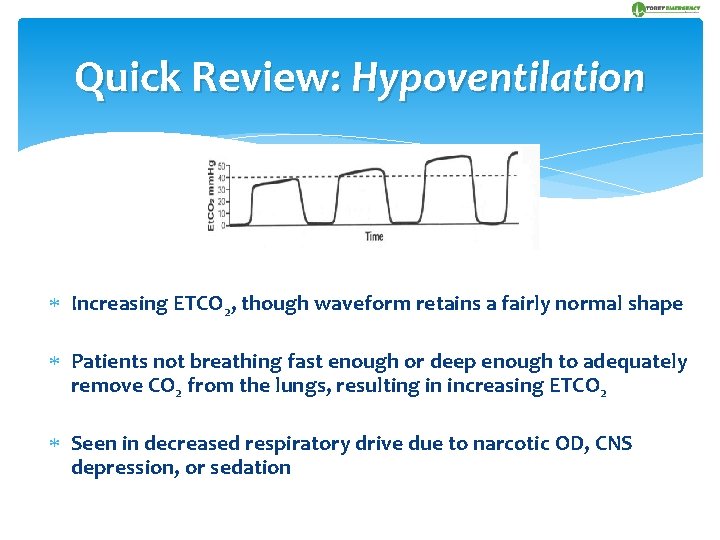
Quick Review: Hypoventilation Increasing ETCO 2, though waveform retains a fairly normal shape Patients not breathing fast enough or deep enough to adequately remove CO 2 from the lungs, resulting in increasing ETCO 2 Seen in decreased respiratory drive due to narcotic OD, CNS depression, or sedation
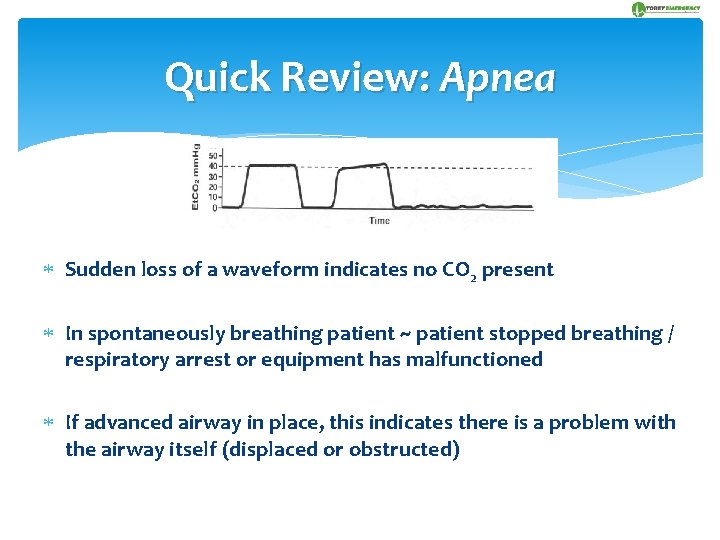
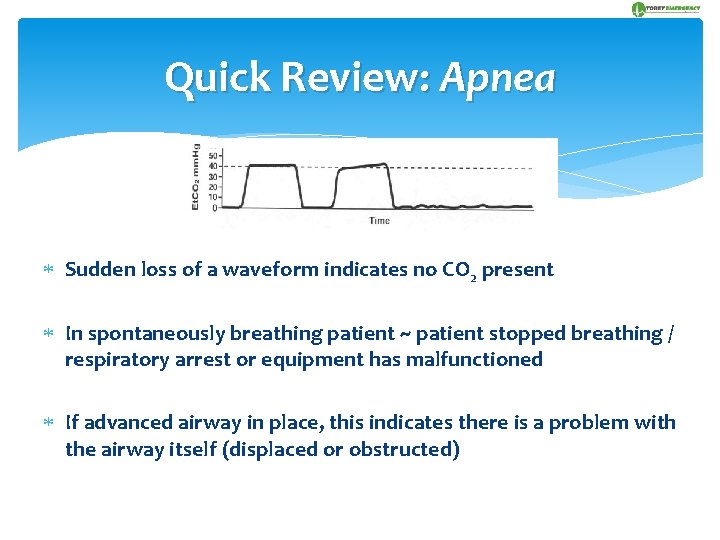
Quick Review: Apnea Sudden loss of a waveform indicates no CO 2 present In spontaneously breathing patient ~ patient stopped breathing / respiratory arrest or equipment has malfunctioned If advanced airway in place, this indicates there is a problem with the airway itself (displaced or obstructed)
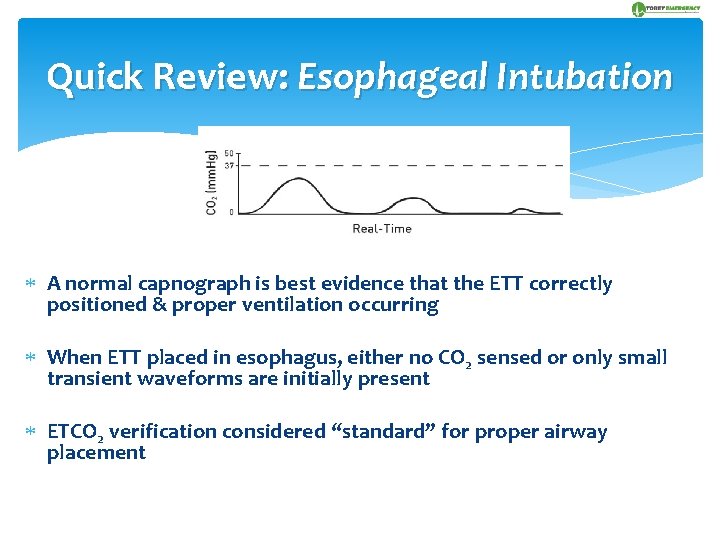
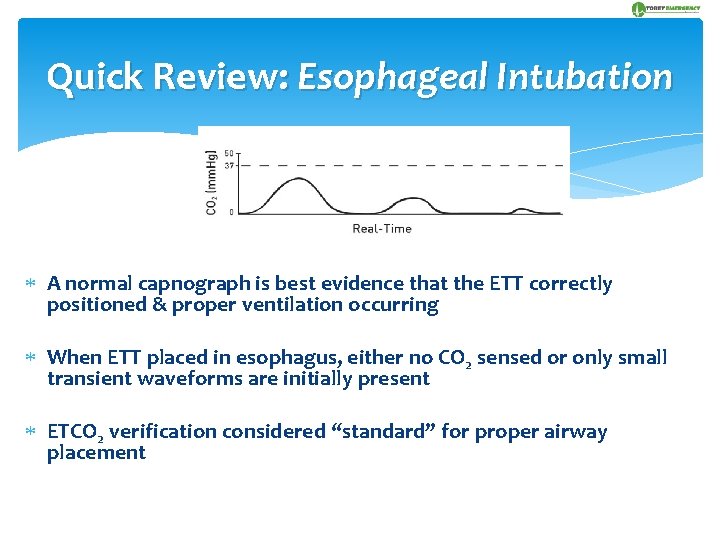
Quick Review: Esophageal Intubation A normal capnograph is best evidence that the ETT correctly positioned & proper ventilation occurring When ETT placed in esophagus, either no CO 2 sensed or only small transient waveforms are initially present ETCO 2 verification considered “standard” for proper airway placement
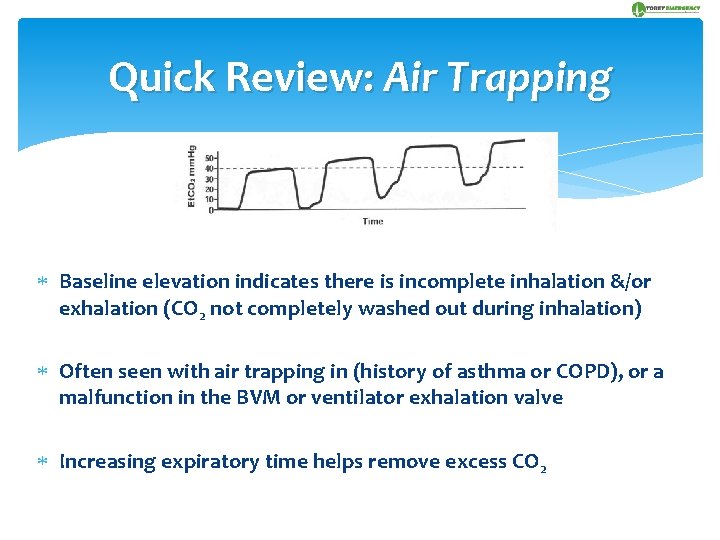
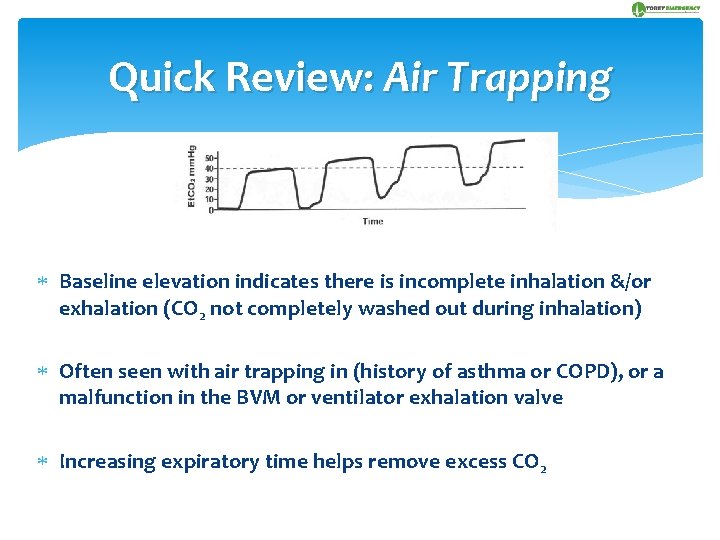
Quick Review: Air Trapping Baseline elevation indicates there is incomplete inhalation &/or exhalation (CO 2 not completely washed out during inhalation) Often seen with air trapping in (history of asthma or COPD), or a malfunction in the BVM or ventilator exhalation valve Increasing expiratory time helps remove excess CO 2
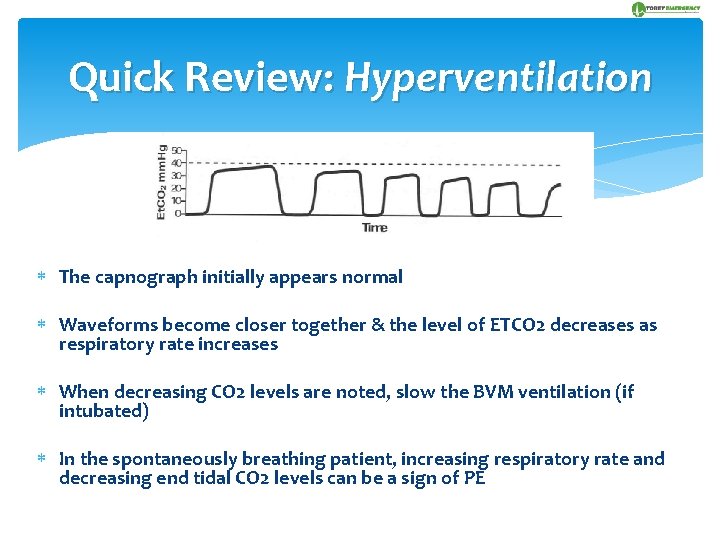
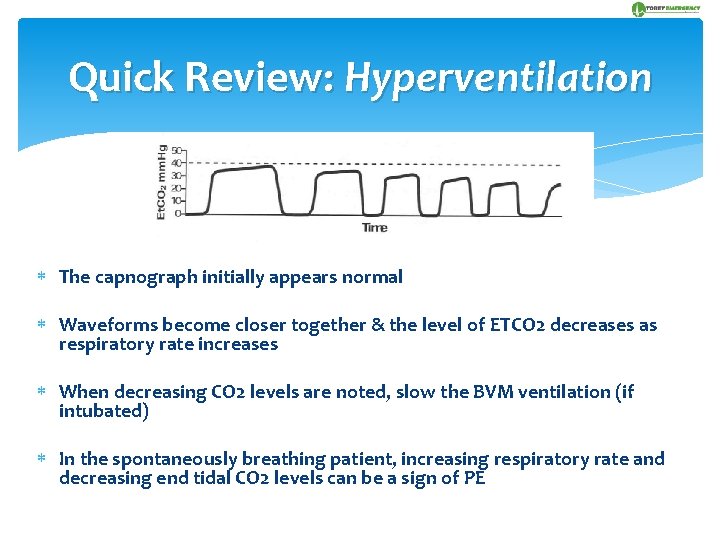
Quick Review: Hyperventilation The capnograph initially appears normal Waveforms become closer together & the level of ETCO 2 decreases as respiratory rate increases When decreasing CO 2 levels are noted, slow the BVM ventilation (if intubated) In the spontaneously breathing patient, increasing respiratory rate and decreasing end tidal CO 2 levels can be a sign of PE
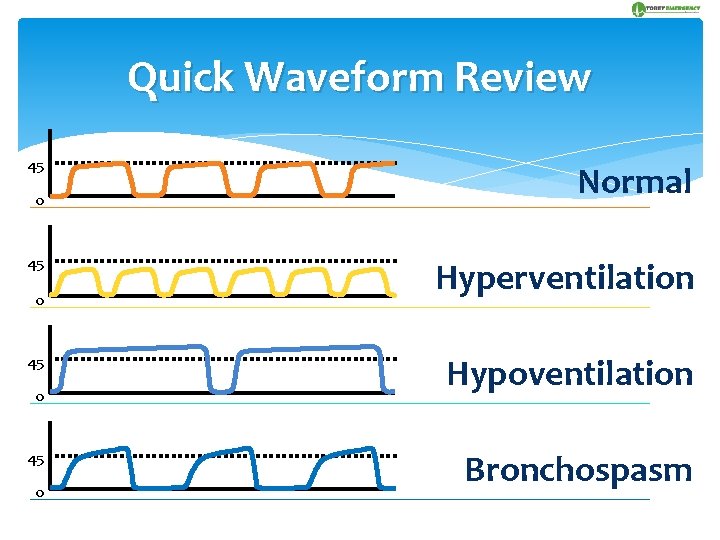
Quick Waveform Review 45 0 Normal Hyperventilation Hypoventilation Bronchospasm
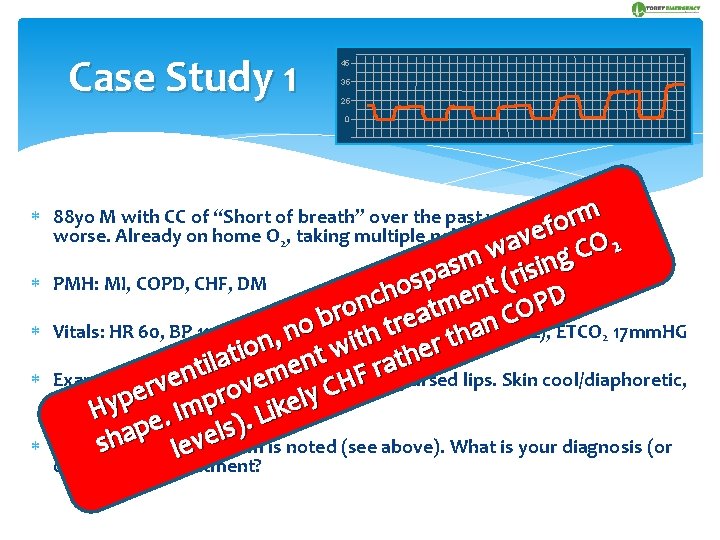
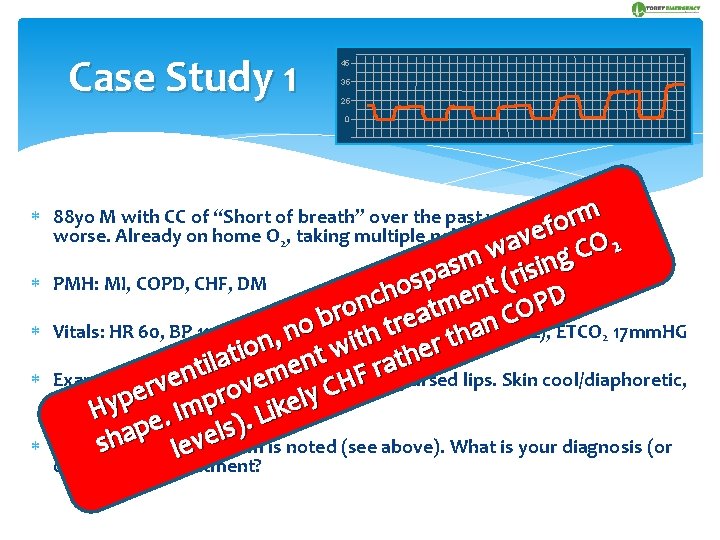
Case Study 1 45 35 25 0 88 yo M with CC of “Short of breath” over the past week, now acutely rm o f worse. Already on home O 2, taking multiple nebs ave O 2 w C g m isin s a p r ( s PMH: MI, COPD, CHF, DM t o n h c e D n P m o t O r a C(2 L), ETCO 17 mm. HG b e r n o t Vitals: HR 60, BP 110/70, RR, 36 labored/shallow, O 72% a n 2 2 h h t t i n r o w e i t t h a t n l i rhonchi apursed lips. Skin cool/diaphoretic, e trales, r n m F Exam: Wheezing, through e e H v v r C o e y pittingyedema BL r H p e. Imp ). Likel p s l a e h v s The following waveform is noted (see above). What is your diagnosis (or le diagnoses) & treatment?
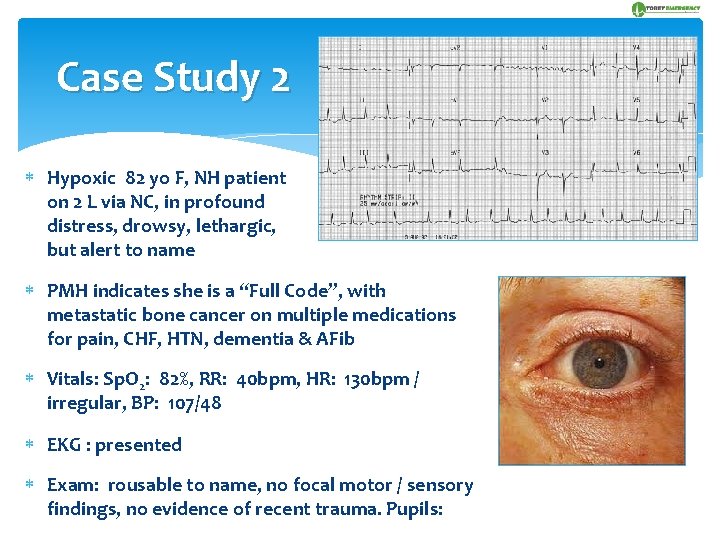
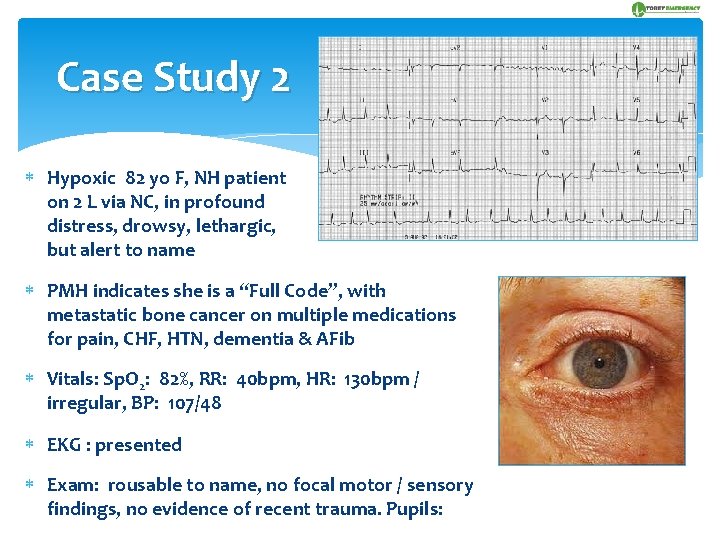
Case Study 2 Hypoxic 82 yo F, NH patient on 2 L via NC, in profound distress, drowsy, lethargic, but alert to name PMH indicates she is a “Full Code”, with metastatic bone cancer on multiple medications for pain, CHF, HTN, dementia & AFib Vitals: Sp. O 2: 82%, RR: 40 bpm, HR: 130 bpm / irregular, BP: 107/48 EKG : presented Exam: rousable to name, no focal motor / sensory findings, no evidence of recent trauma. Pupils:
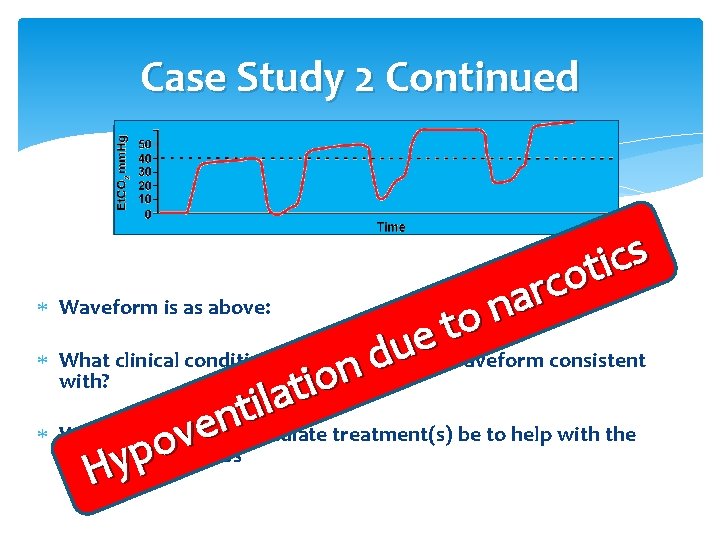
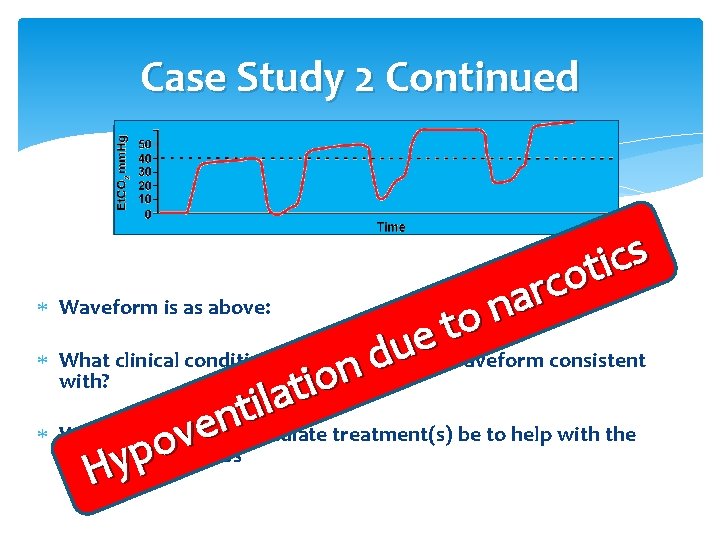
Case Study 2 Continued Waveform is as above: s c i t o c r a n to e u d n o i t a l i t n e What would your immediate treatment(s) be to help with the v o respiratory distress p y H What clinical condition(s) is exam, EKG & waveform consistent with?
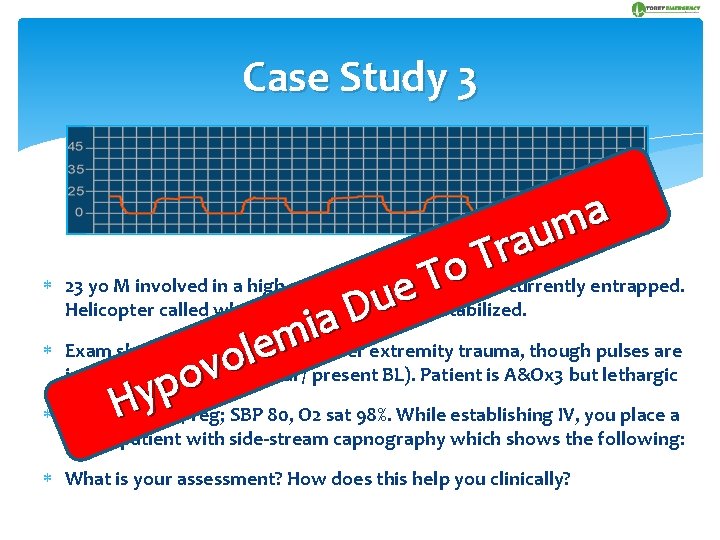
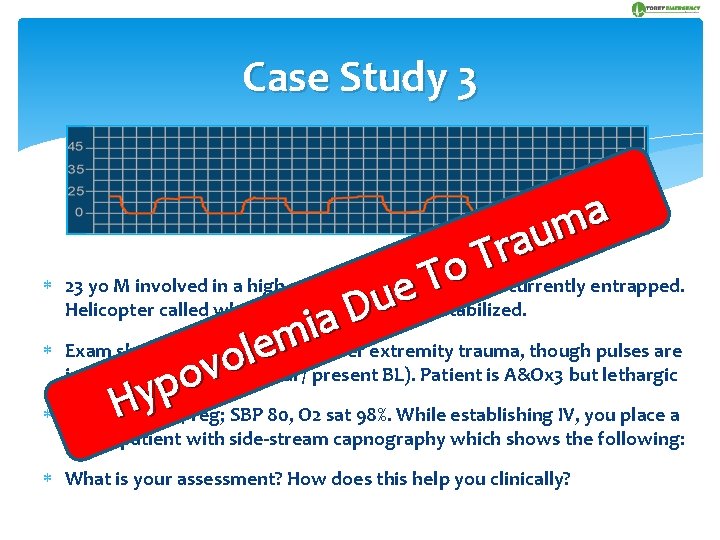
Case Study 3 a m u a r T o T 23 yo M involved in a high speed MVC in which he is currently entrapped. e u & stabilized. Helicopter called while patient extricated D a i m Exam shows obvious chest & lower extremity trauma, though pulses are e l o/ equal / present BL). Patient is A&Ox 3 but lethargic intact distally o (weak v p y Vitals: H HR 120 / reg; SBP 80, O 2 sat 98%. While establishing IV, you place a NC on patient with side-stream capnography which shows the following: What is your assessment? How does this help you clinically?
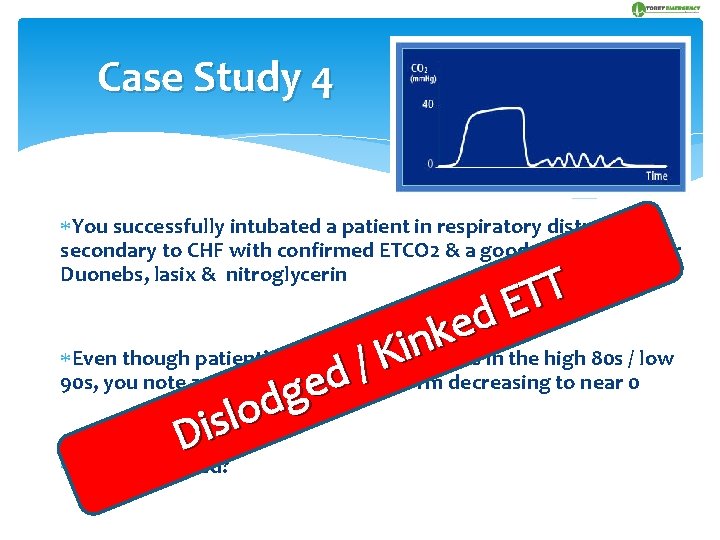
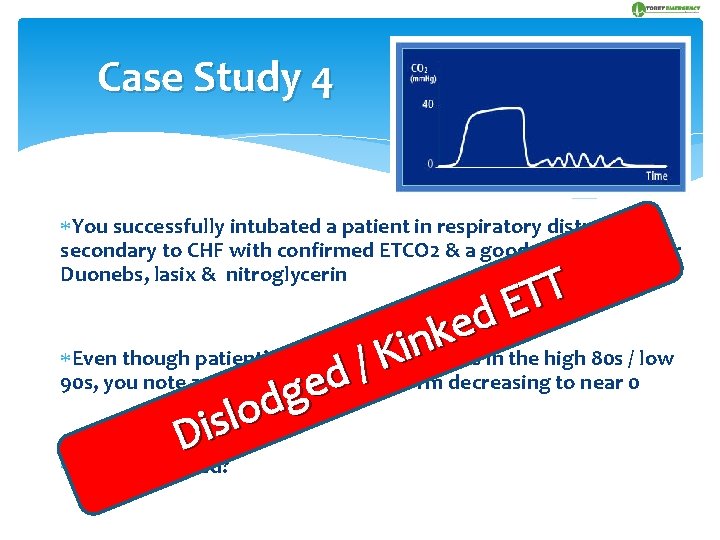
Case Study 4 You successfully intubated a patient in respiratory distress secondary to CHF with confirmed ETCO 2 & a good waveform after Duonebs, lasix & nitroglycerin T T E d e k n i Even though patient’s oxygenation remains in the high 80 s / low K / 90 s, you note a sudden losseof waveform decreasing to near 0 d g d o l s Di What happened?
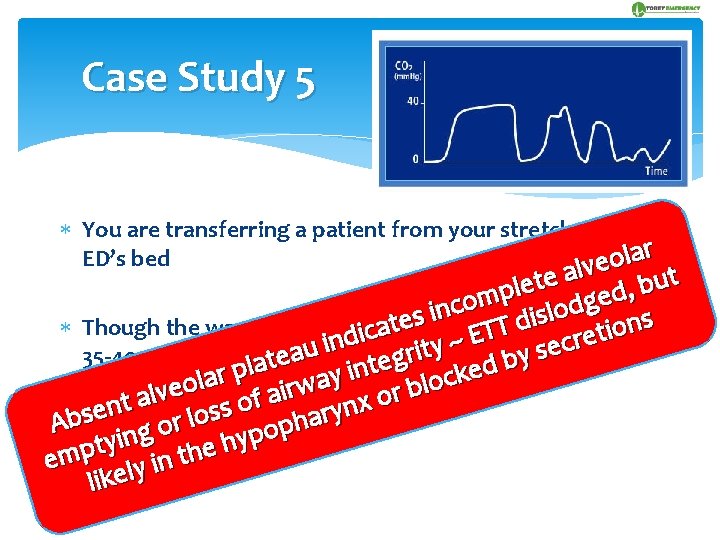
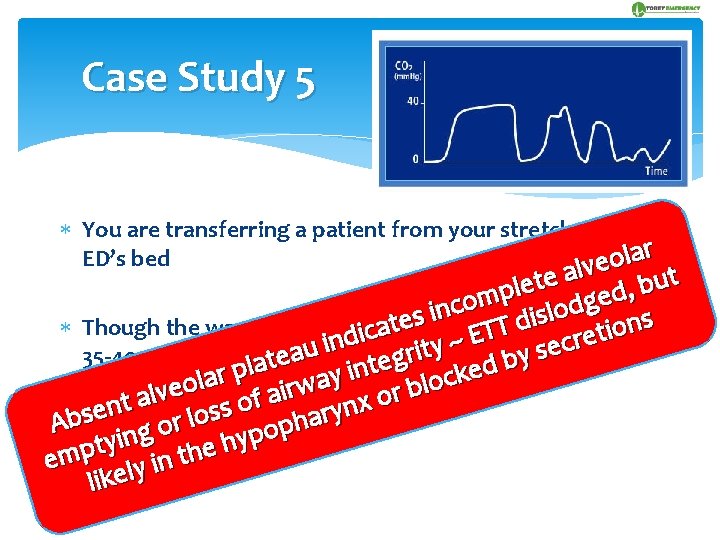
Case Study 5 You are transferring a patient from your stretcher to the r a l ED’s bed o lve l a t e u t e b l , p d e m g o c d n o i l s s i s e d t normal, n Though the waveform haddbeen with levels in the T a o i c T t i E e r ~ n c i y e u t s a ri thedfollowing 35 -40 range, after transfer, you note y e g t b e a t l n p e i k r y c a l a o waveform l o w b r i ve r l a o a f t n s o harynx e s s o l b r A p o o g p n y i happened? y h t e p What h t m e n i y l like
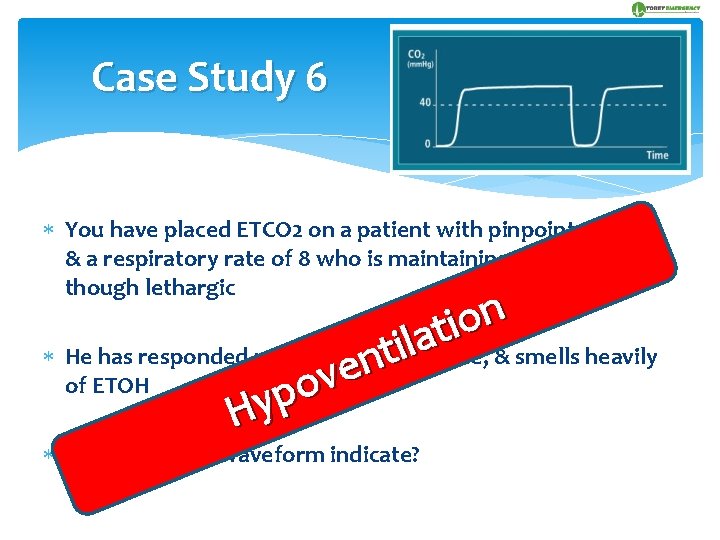
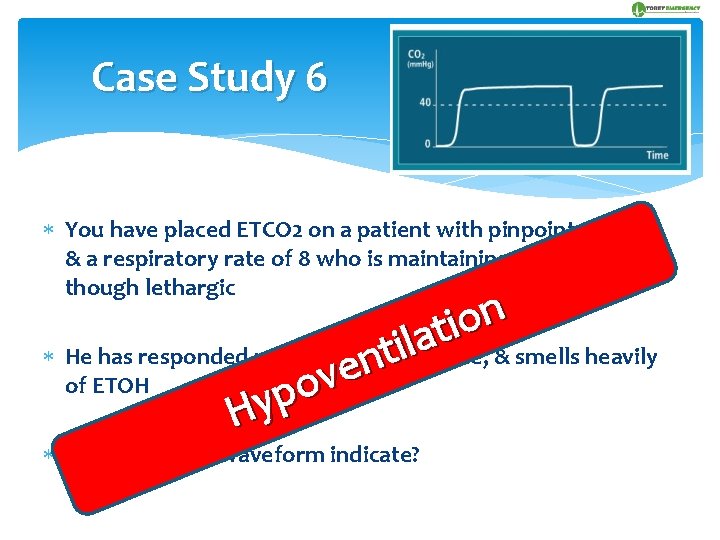
Case Study 6 You have placed ETCO 2 on a patient with pinpoint pupils, & a respiratory rate of 8 who is maintaining his airway, though lethargic n o i t a l i He has responded minimally to naloxone, & smells heavily t n e v of ETOH o p Hy What does the waveform indicate?

Case Study 7 You have been called to the house of a 16 year old girl who has just broken up with her boyfriend n o i t a l i t n eis 99%, but she does appear to v He lungs are clear, O 2 saturation r e have some respiratory distress p Hy She is hysterical & her mother states that “she is having a bad asthma attack” What diagnosis is suggested by upon the waveform?
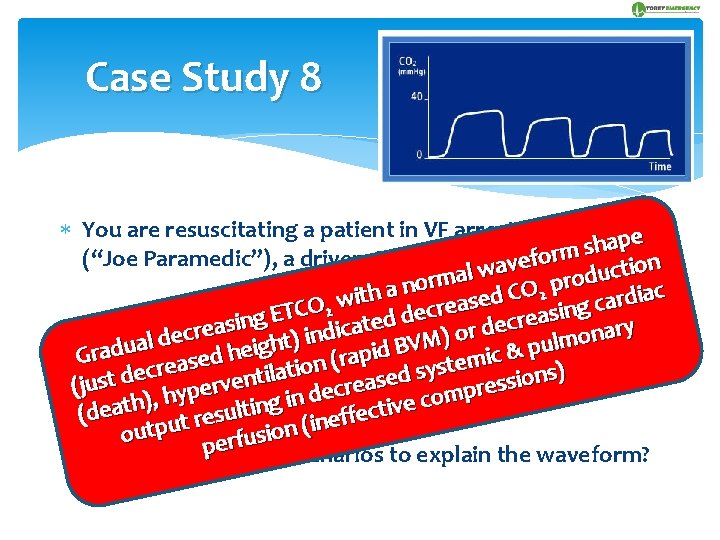
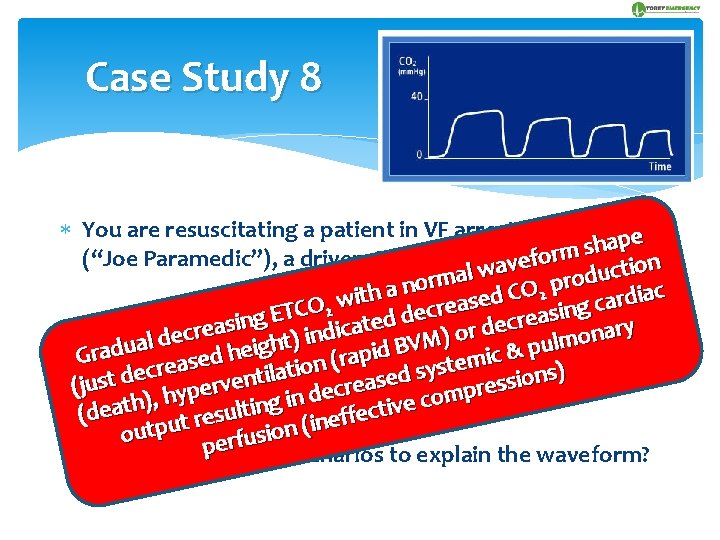
Case Study 8 You are resuscitating a patient in VF arrest with just you pe a h s m (“Joe Paramedic”), a driver, & one EMTwavefor ion t c l u a d o rm r o p n a O 2 C h iac t i d d r e w s a c a O 2 g re C n c i T e s E d a g e d r c te sin doing e a abeen The EMTdehas compressions throughout the d ry c e i r r a d c o n n ) i o ) l lm VM ht u B g p i e d i & h radua a(10 p c minutes) when you note the change in Gtransport i a d r e ( m s e n t e o s i cr sy at s) e l i d n d t e o t n i s s s e a s u v (jwaveform re re er c p p e y d m h o n , i c ) (death ut resulting (ineffective outp perfusion What are two likely scenarios to explain the waveform?
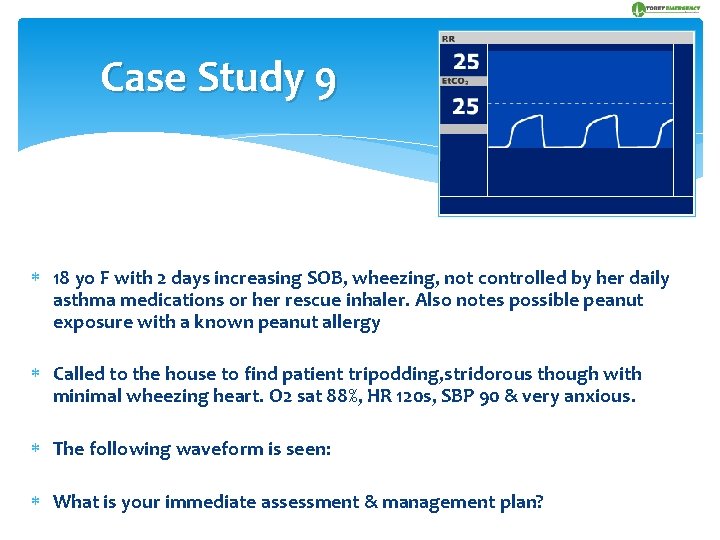
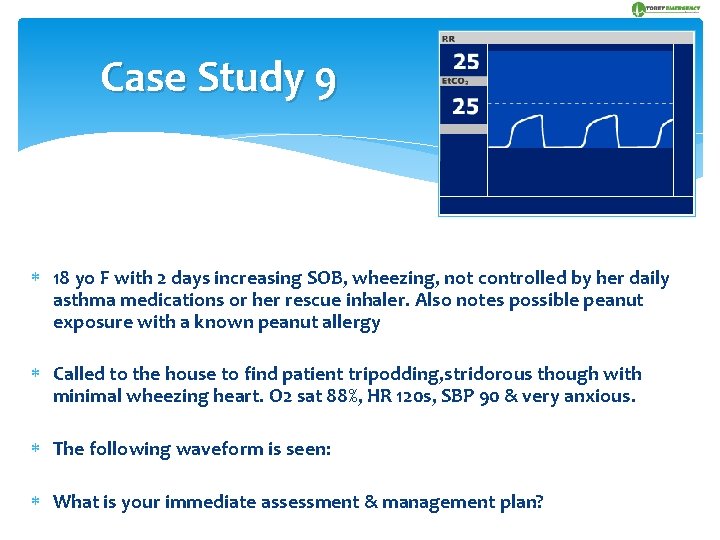
Case Study 9 18 yo F with 2 days increasing SOB, wheezing, not controlled by her daily asthma medications or her rescue inhaler. Also notes possible peanut exposure with a known peanut allergy Called to the house to find patient tripodding, stridorous though with minimal wheezing heart. O 2 sat 88%, HR 120 s, SBP 90 & very anxious. The following waveform is seen: What is your immediate assessment & management plan?
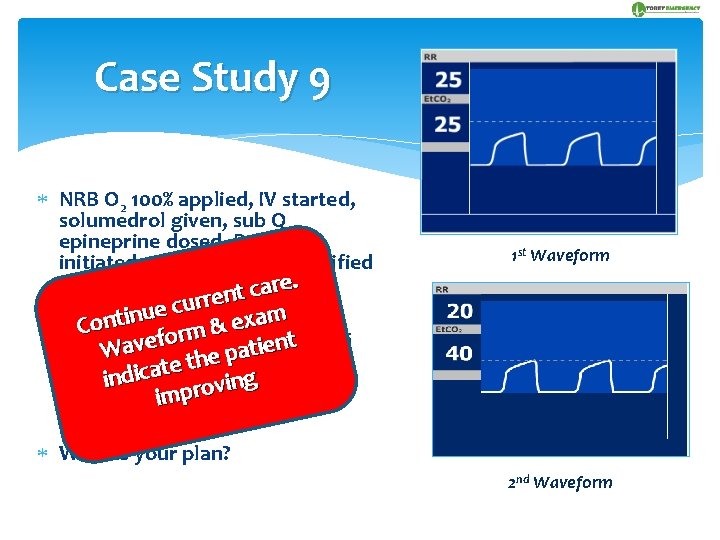
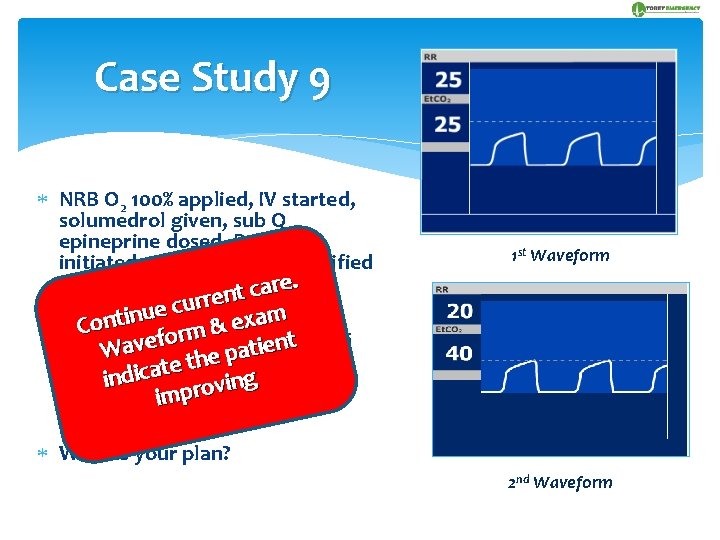
Case Study 9 NRB O 2 100% applied, IV started, solumedrol given, sub Q epineprine dosed, Duoneb initiated, medical control notified e. r a c t en r r u c ue Within 5 nminutes, the m i t xa. O 2 n e o C & m HR in nthe r 92%, saturation is 130 s o f t e v e a i t a anxious p with W patient remaining e h t ate now 110 but alert. g & the indic. SBP n i v o r imp following waveform is seen: 1 st Waveform What is your plan? 2 nd Waveform
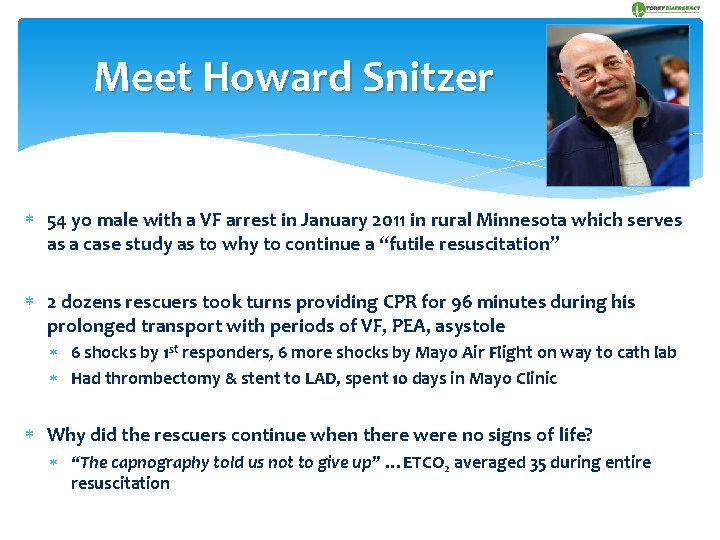
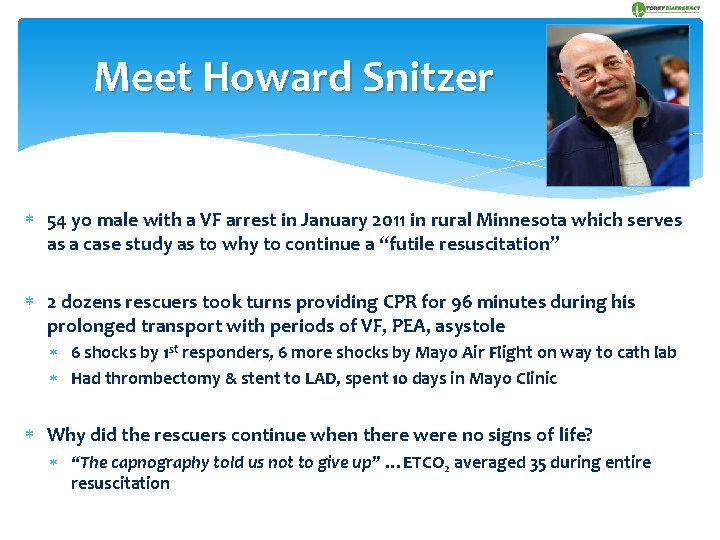
Meet Howard Snitzer 54 yo male with a VF arrest in January 2011 in rural Minnesota which serves as a case study as to why to continue a “futile resuscitation” 2 dozens rescuers took turns providing CPR for 96 minutes during his prolonged transport with periods of VF, PEA, asystole 6 shocks by 1 st responders, 6 more shocks by Mayo Air Flight on way to cath lab Had thrombectomy & stent to LAD, spent 10 days in Mayo Clinic Why did the rescuers continue when there were no signs of life? “The capnography told us not to give up” …ETCO 2 averaged 35 during entire resuscitation
References EMSWorld. com. “Waveform Capnography” 2009. Bonner County EMS “Waveform Capnography”. 2010. Medtronic “Capnography in Emergency Care”. 2008. English J, Pointer J, Jacobs M. “Capnography: The Standard of Care”. 2005 Guidelines for Cardiovascular Resuscitation and Emergency Cardiovascular Care, Circulation 102 (suppl I) 8. August 22, 2010 www. emscapnographyblogspot. com Wayne MA, Levine RL, Miller CC. “Use of End-tidal Carbon Dioxide to Predict Outcome in Prehospital Cardiac Arrest”. Annals of Emergency Medicine. 1995; 25(6): 762 -767. Levine RL. , Wayne MA. , Miller CC. “End-tidal carbon dioxide and outcome of out-of-hospital cardiac arrest. ” New England Journal of Medicine. 1997; 337(5): 301 -306. Cummins RO. Principles & Practice. American Heart Association. 2003. Weil MH. 1985. Cardiac output and ETCO 2. Critical Care Medicine 13 (11): 907 -909 Ochoa F. et al. 1998. The Effect of Rescuer Fatigue on Quality of Chest Compressions. Resuscitation April; 37: 149 -52 White RD. Out-of-Hospital Monitoring of ETCO 2 Pressure During CPR. AEM. 199423 (1): 756 -761 Levine R. L. ETCO 2 & outcome of OOHCA. NEJM. 1997. 337 (5): 301 -306. Huizenga JE. Guidelines for the Management of Severe Head Injury: Are Emergency Physicians Following Them? AEM. 2000. 9 (8): 806 -812 Asthmatic Statistics. American Academy of Allergies, Asthma and Immunology. www. aaaai. org Hall J. B. , Acute Asthma, Assessment and Management, Mc. Graw-Hill, New York. Falk J. 1988. ETCO 2 concentration during CPR. NEJM. 318 (10): 607 -611 Flanagan, J. F. , et al. 1995. Noninvasive monitoring of ETCO 2 tension via nasal cannulas in spontaneously breathing children with profound hypocarbia. Critical Care Medicine. June; 23 (6): 1140 -1142 Delbridge T, et al. 2003 Prehospital Asthma Management. PEC. 7(1) 42 -47 Capnography: The Standard of Care. JEnglish, J Pointer, M Jacobs, EMT-P. A; lameda Public Health Department. Hanley C. Perianesthesia Nurses Association of British Columbia. “Capnography in the PACU: Theory and Clinical Applications of end tidal C 02 Monitoring”. 2010. Mc. Evoy M. Capnography Could Make You a Rock Star! CTICU and Resuscitation Committee Chair Albany Medical Center. 2011.
Summary prehospitalmd@gmail. com Visual objective measure of ventilation Breath-to-breath readings for intubated & non-intubated patients Clinical information to guide patient care Objective documentation