Comprehensive Chromosome Screening in IVF Enhancing Outcomes While

- Slides: 57
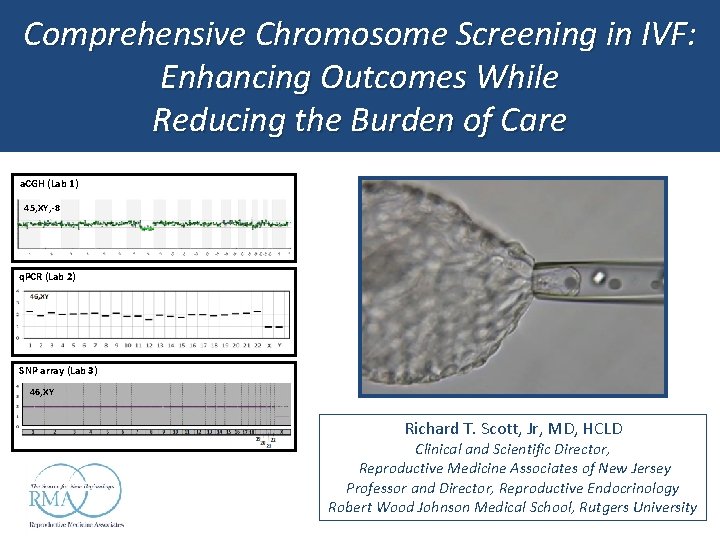
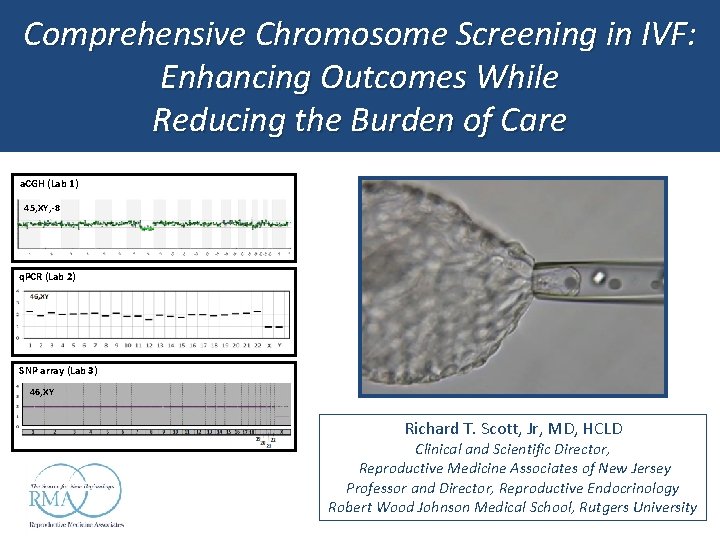
Comprehensive Chromosome Screening in IVF: Enhancing Outcomes While Reducing the Burden of Care a. CGH (Lab 1) 45, XY, -8 q. PCR (Lab 2) SNP array (Lab 3) 46, XY Richard T. Scott, Jr, MD, HCLD Clinical and Scientific Director, Reproductive Medicine Associates of New Jersey Professor and Director, Reproductive Endocrinology Robert Wood Johnson Medical School, Rutgers University
Disclosures • Board Member – FEC • No compensation of any kind • No financial interest in any test or diagnostic platform
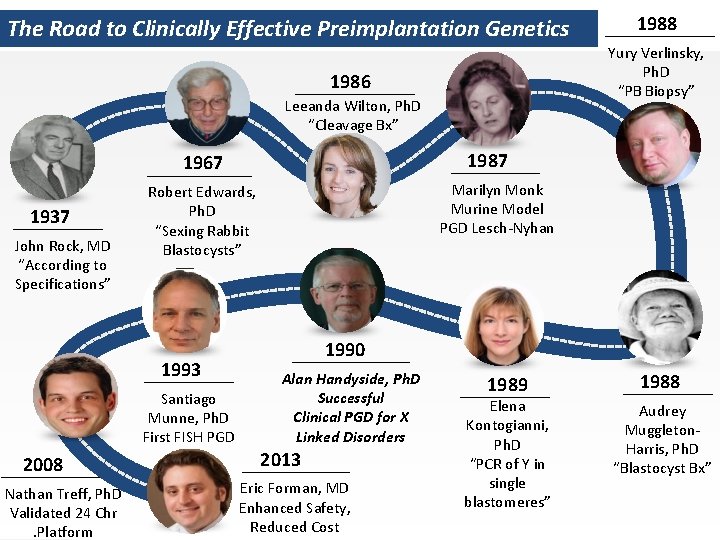
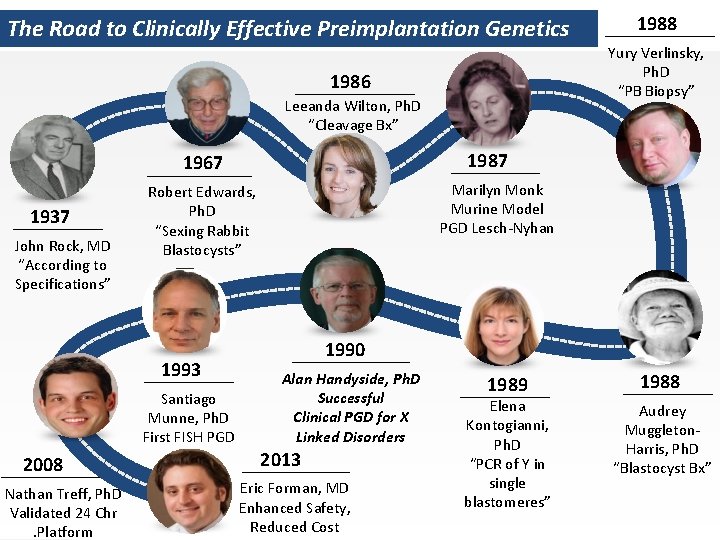
The Road to Clinically Effective Preimplantation Genetics Yury Verlinsky, Ph. D “PB Biopsy” 1986 Leeanda Wilton, Ph. D “Cleavage Bx” 1987 1967 1937 John Rock, MD “According to Specifications” Santiago Munne, Ph. D First FISH PGD 2008 Nathan Treff, Ph. D Validated 24 Chr. Platform Marilyn Monk Murine Model PGD Lesch-Nyhan Robert Edwards, Ph. D “Sexing Rabbit Blastocysts” 1993 1988 1990 Alan Handyside, Ph. D Successful Clinical PGD for X Linked Disorders 2013 Eric Forman, MD Enhanced Safety, Reduced Cost 1989 Elena Kontogianni, Ph. D “PCR of Y in single blastomeres” 1988 Audrey Muggleton. Harris, Ph. D “Blastocyst Bx”
What do people think about when you say IVF…
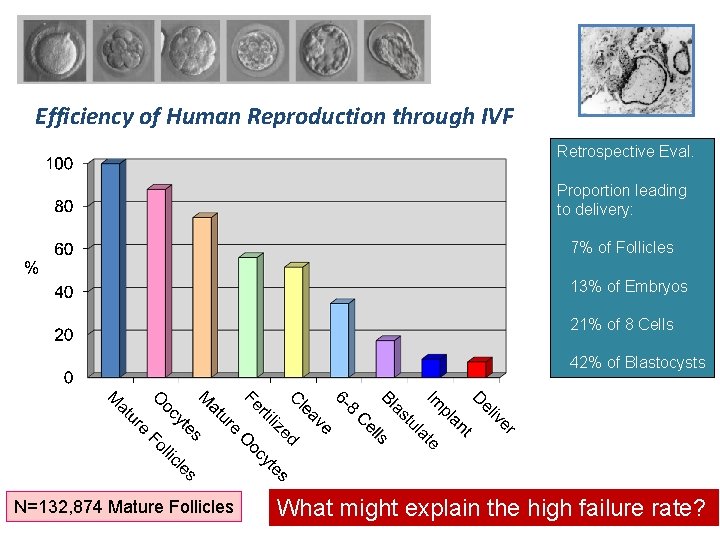
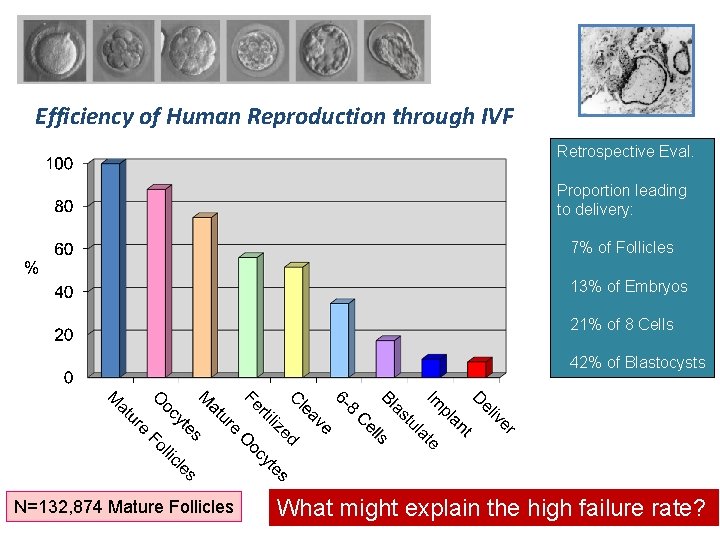
Efficiency of Human Reproduction through IVF Retrospective Eval. Proportion leading to delivery: 7% of Follicles 13% of Embryos 21% of 8 Cells 42% of Blastocysts N=132, 874 Mature Follicles What might explain the high failure rate?
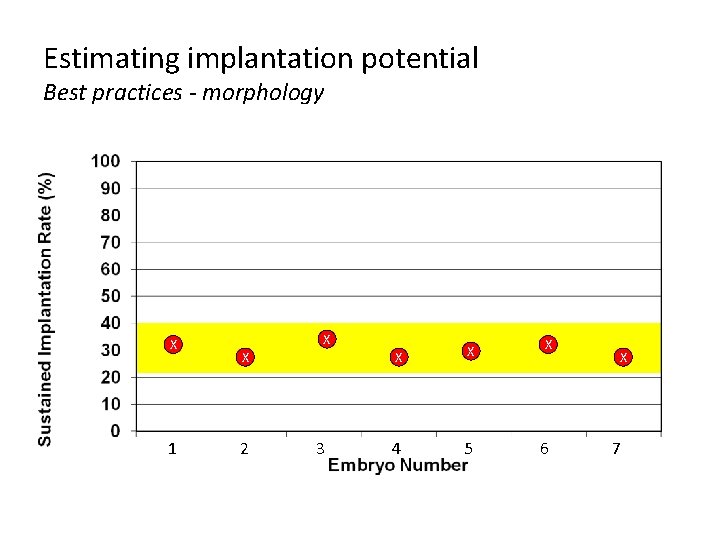
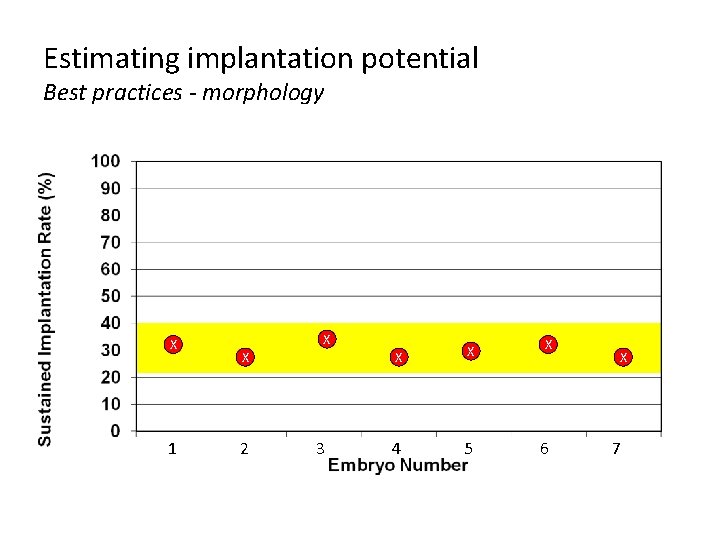
Estimating implantation potential Best practices - morphology X 1 X X 2 3 X X X 4 5 6 X 7
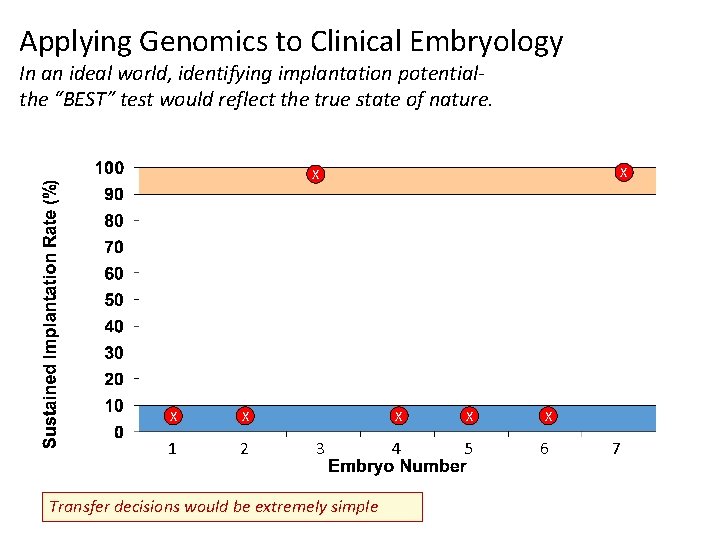
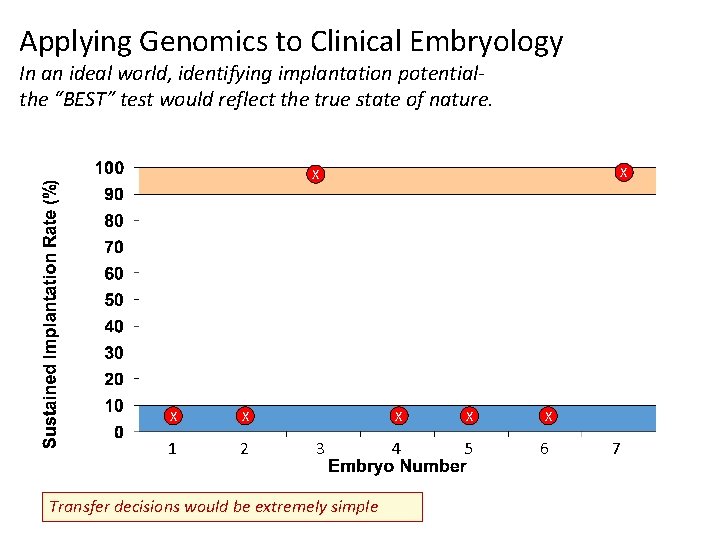
Applying Genomics to Clinical Embryology In an ideal world, identifying implantation potentialthe “BEST” test would reflect the true state of nature. X X 1 2 3 Transfer decisions would be extremely simple X X X 4 5 6 7
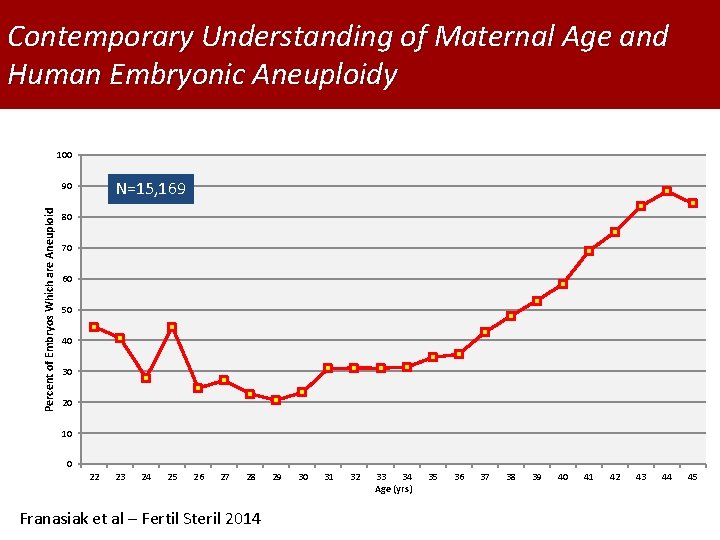
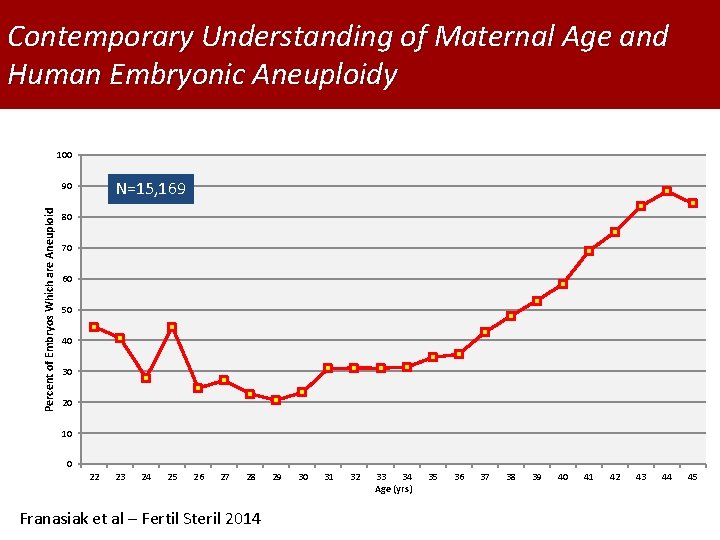
Contemporary Understanding of Maternal Age and Human Embryonic Aneuploidy 100 N=15, 169 Percent of Embryos Which are Aneuploid 90 80 70 60 50 40 30 20 10 0 22 23 24 25 26 27 28 Franasiak et al – Fertil Steril 2014 29 30 31 32 33 34 Age (yrs) 35 36 37 38 39 40 41 42 43 44 45
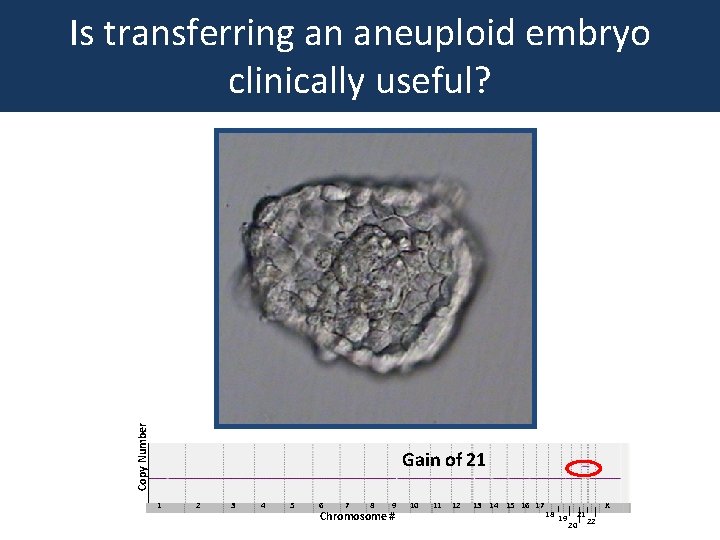
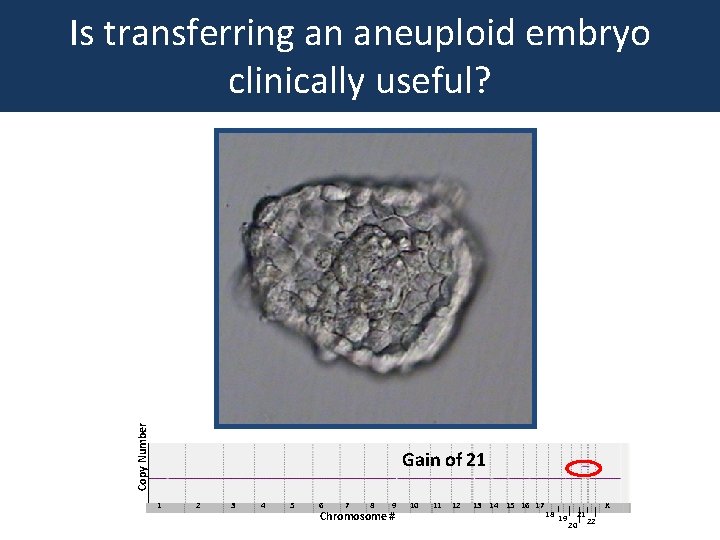
Copy Number Is transferring an aneuploid embryo clinically useful? Gain of 21 1 2 3 4 5 6 7 8 9 Chromosome # 10 11 12 13 14 15 16 17 18 19 21 20 22 X
What are the “Burdens” of CCS Thus the real questions are: 1. Safely attaining embryonic DNA 2. Predictive values of the techniques 3. Proportion of euploid embryos that will fail 4. Cost effectiveness
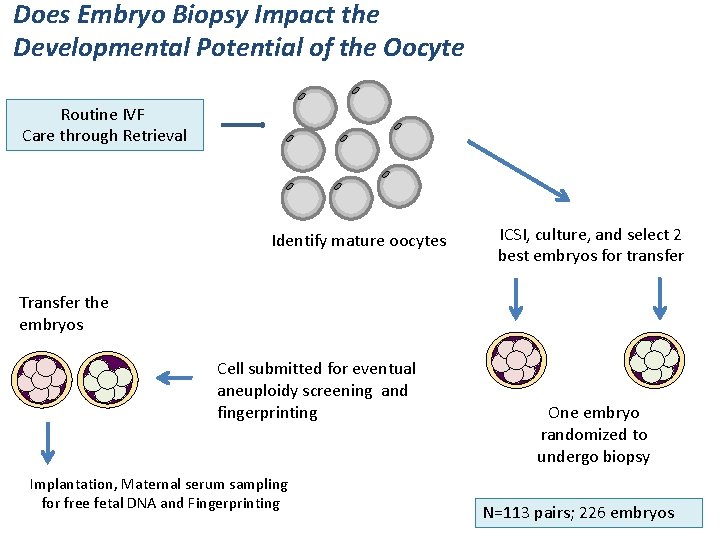
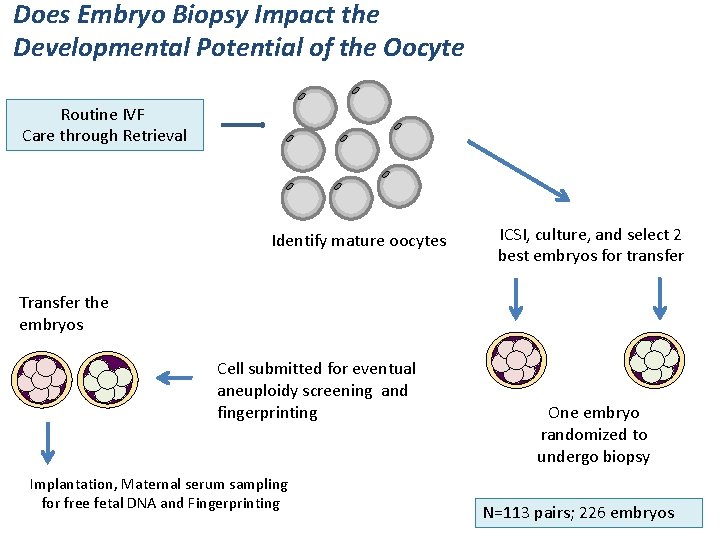
Does Embryo Biopsy Impact the Developmental Potential of the Oocyte Routine IVF Care through Retrieval Identify mature oocytes ICSI, culture, and select 2 best embryos for transfer Transfer the embryos Cell submitted for eventual aneuploidy screening and fingerprinting Implantation, Maternal serum sampling for free fetal DNA and Fingerprinting One embryo randomized to undergo biopsy N=113 pairs; 226 embryos
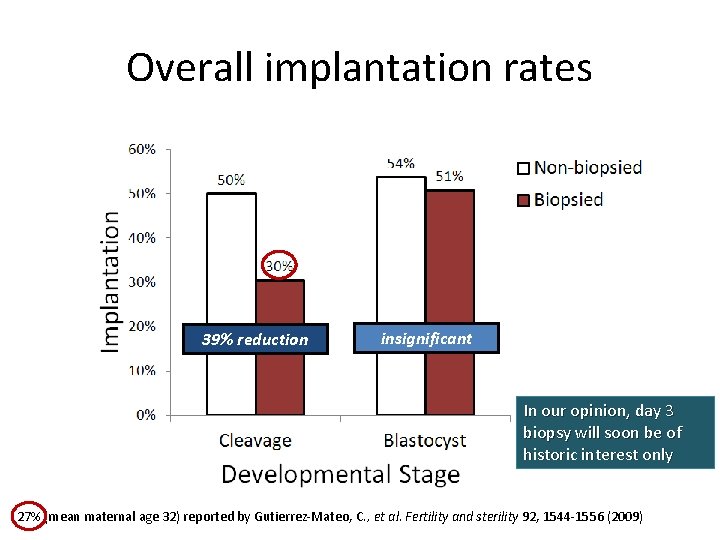
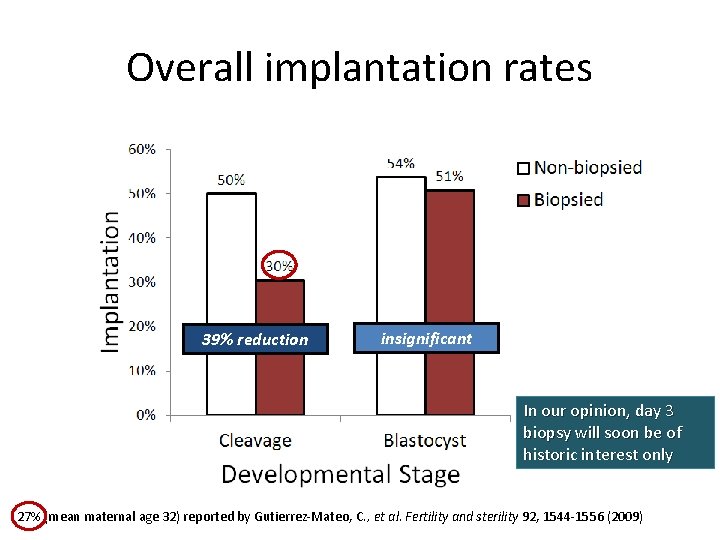
Overall implantation rates 39% reduction insignificant In our opinion, day 3 biopsy will soon be of historic interest only 27% (mean maternal age 32) reported by Gutierrez-Mateo, C. , et al. Fertility and sterility 92, 1544 -1556 (2009)
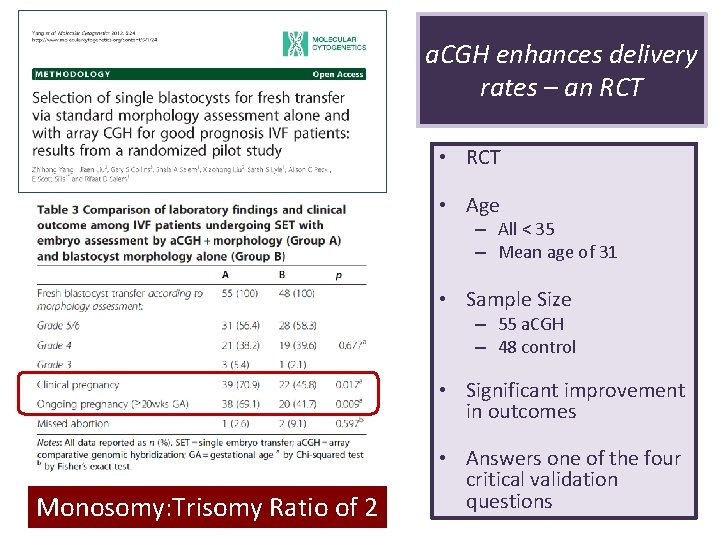
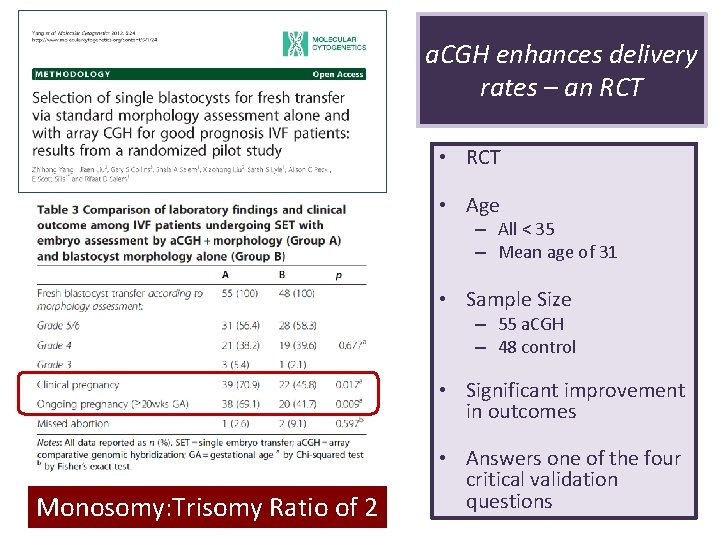
a. CGH enhances delivery rates – an RCT • Age – All < 35 – Mean age of 31 • Sample Size – 55 a. CGH – 48 control • Significant improvement in outcomes Monosomy: Trisomy Ratio of 2 • Answers one of the four critical validation questions
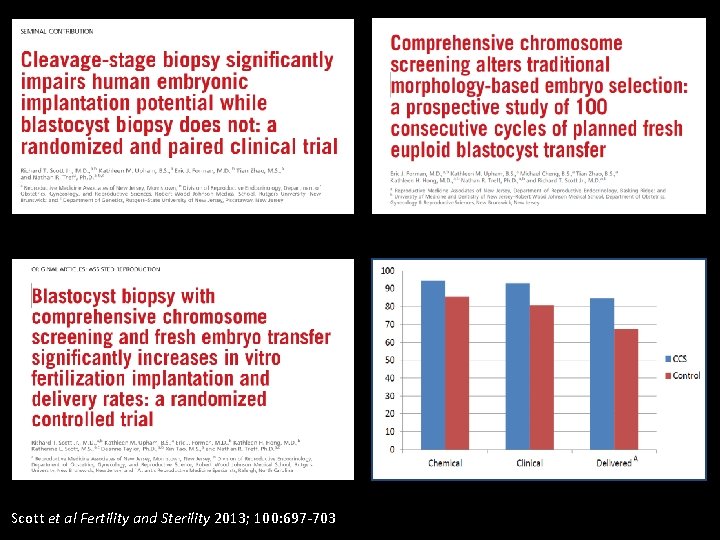
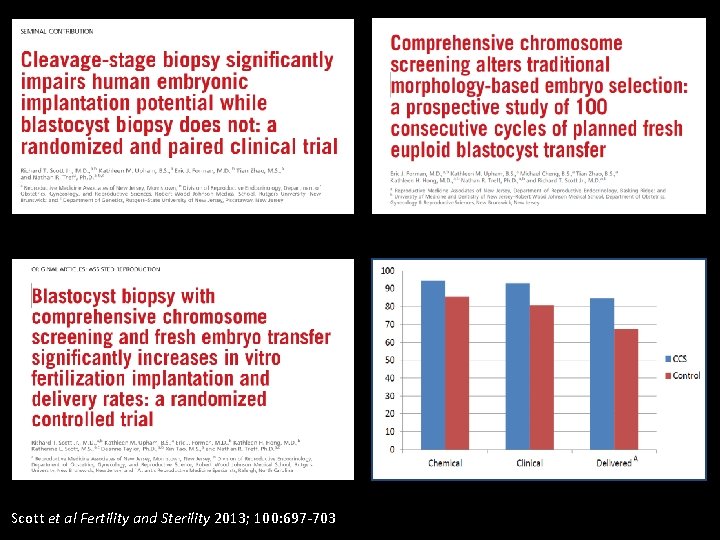
Scott et al Fertility and Sterility 2013; 100: 697 -703
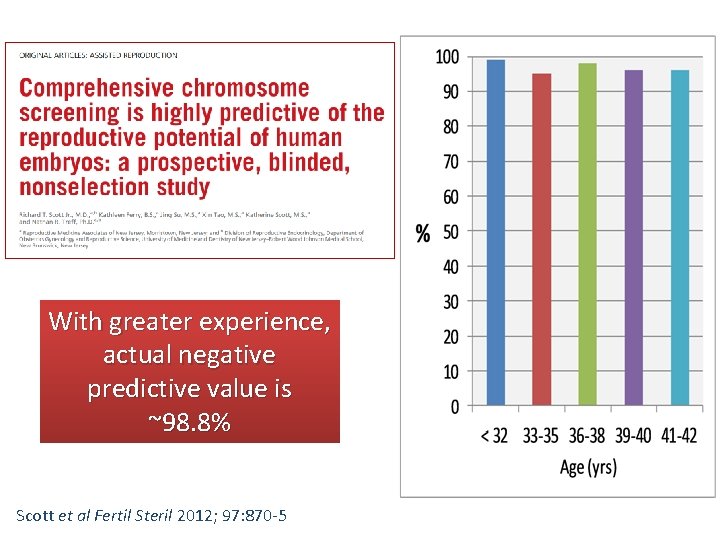
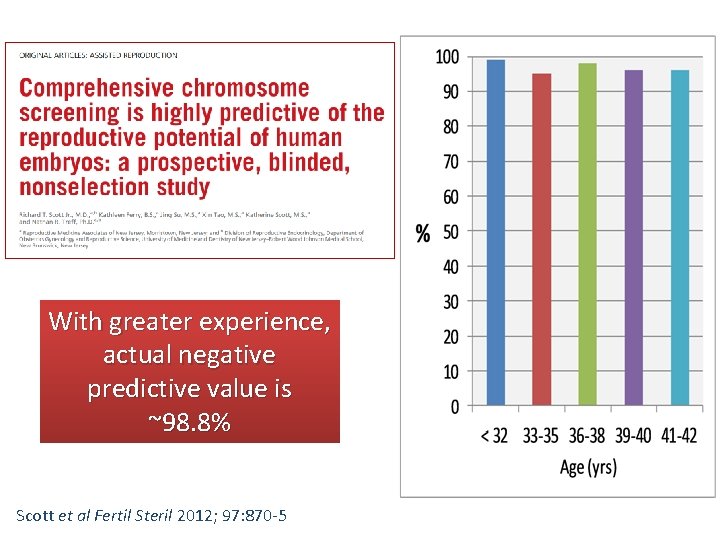
With greater experience, actual negative predictive value is ~98. 8% Scott et al Fertil Steril 2012; 97: 870 -5
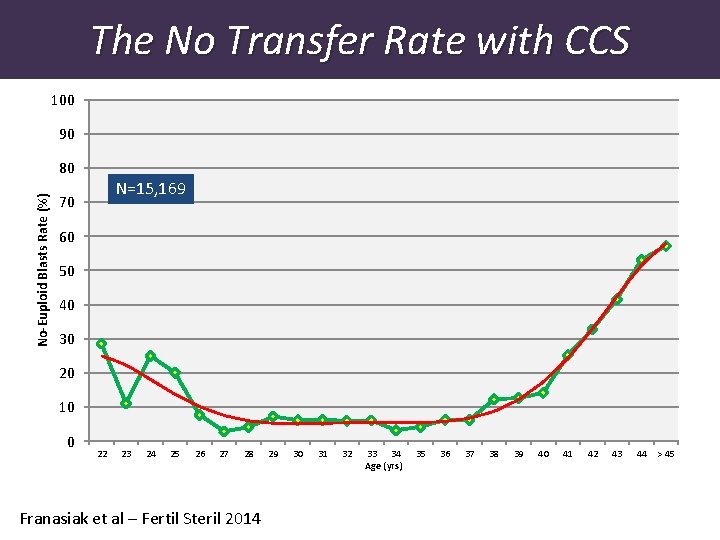
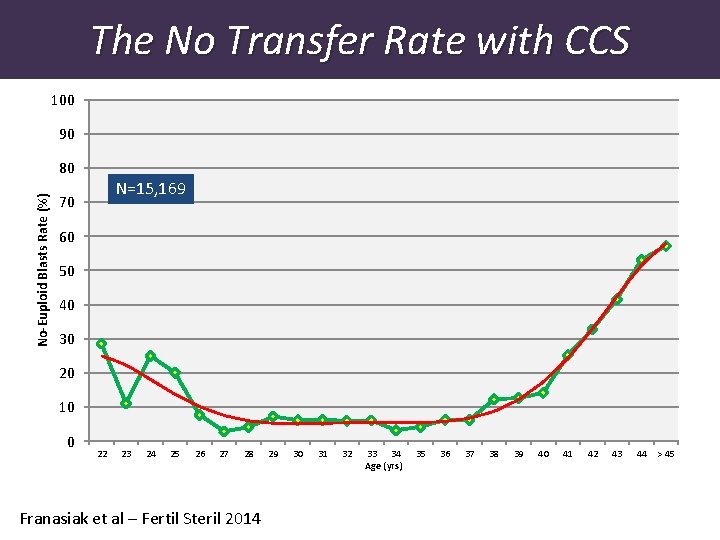
The No Transfer Rate with CCS 100 90 No-Euploid Blasts Rate (%) 80 N=15, 169 70 60 50 40 30 20 10 0 22 23 24 25 26 27 28 Franasiak et al – Fertil Steril 2014 29 30 31 32 33 34 Age (yrs) 35 36 37 38 39 40 41 42 43 44 > 45
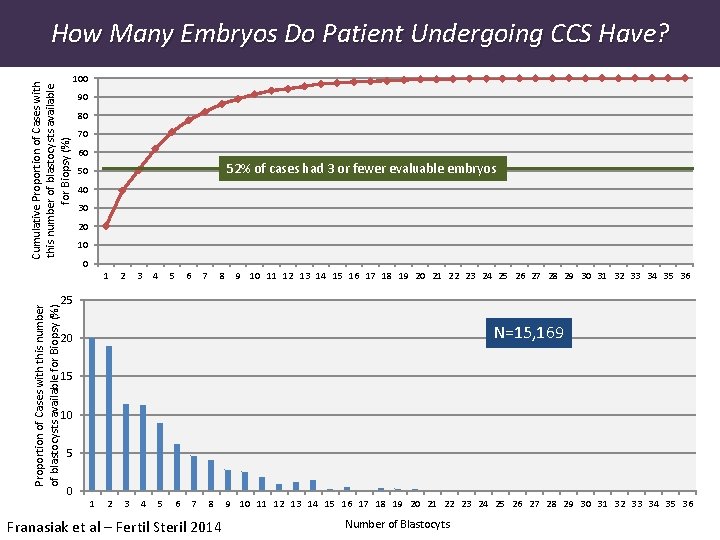
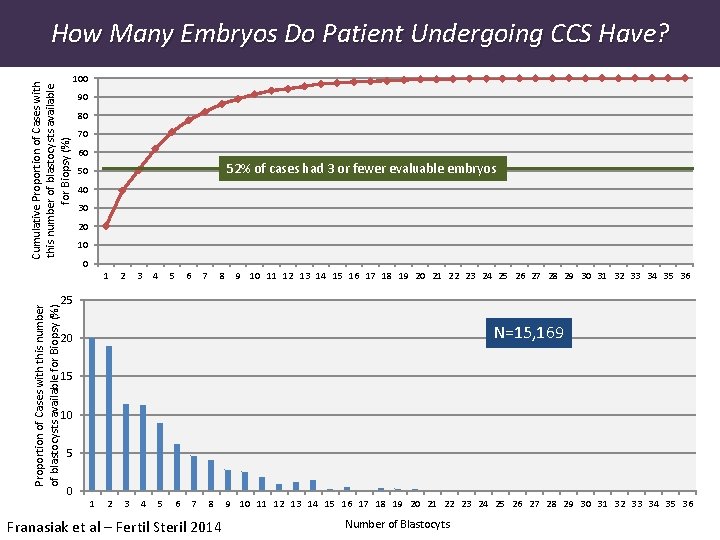
Proportion of Cases with this number of blastocysts available for Biopsy (%) Cumulative Proportion of Cases with this number of blastocysts available for Biopsy (%) How Many Embryos Do Patient Undergoing CCS Have? 100 90 80 70 60 52% of cases had 3 or fewer evaluable embryos 50 40 30 20 10 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 25 N=15, 169 20 15 10 5 0 1 2 3 4 5 6 7 8 Franasiak et al – Fertil Steril 2014 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 Number of Blastocyts
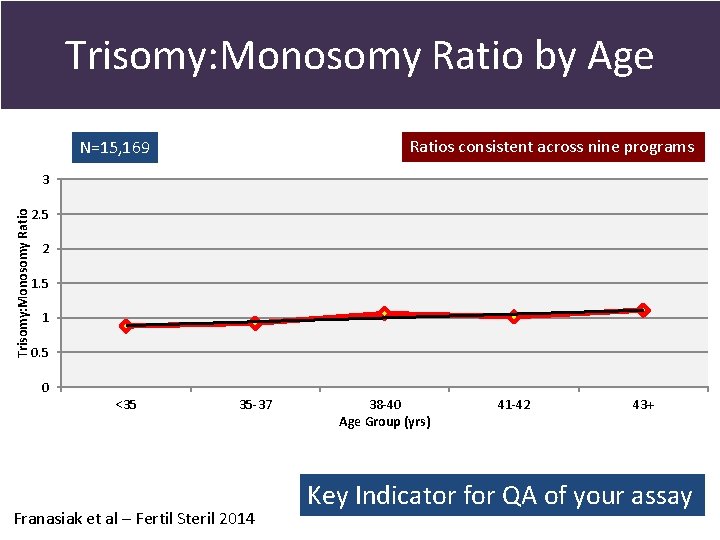
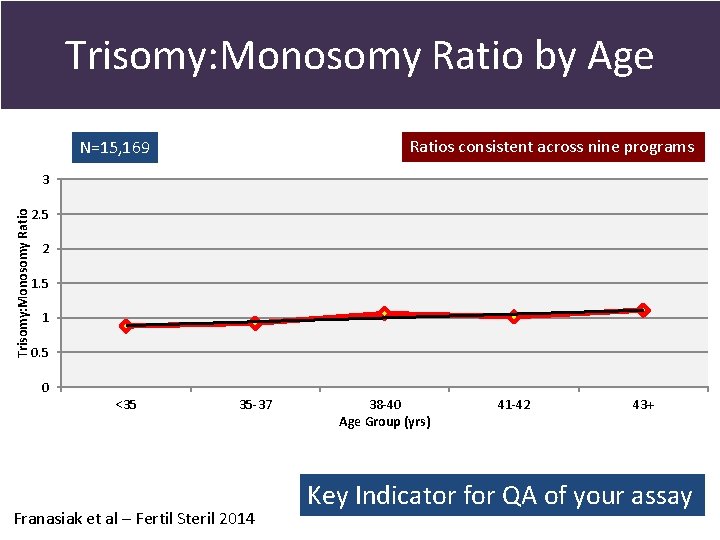
Trisomy: Monosomy Ratio by Age Ratios consistent across nine programs N=15, 169 Trisomy: Monosomy Ratio 3 2. 5 2 1. 5 1 0. 5 0 <35 35 -37 Franasiak et al – Fertil Steril 2014 38 -40 Age Group (yrs) 41 -42 43+ Key Indicator for QA of your assay
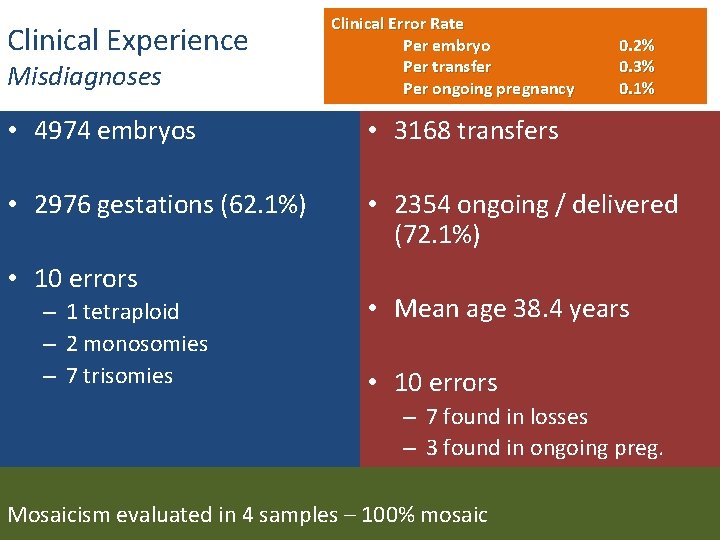
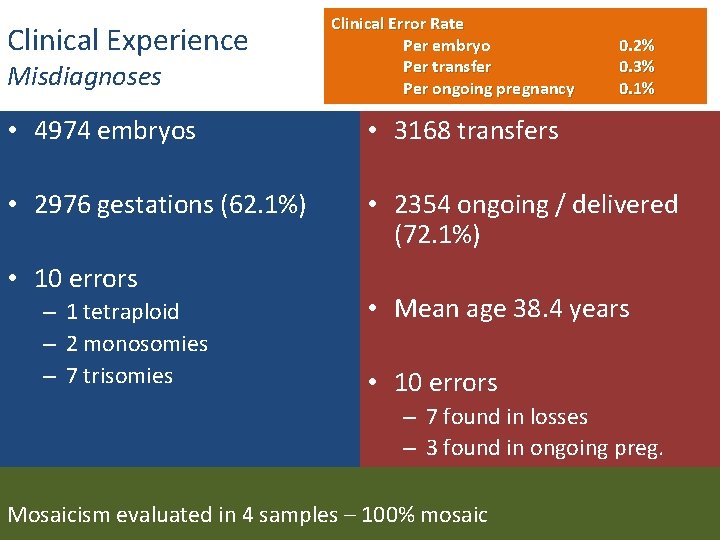
Clinical Experience Misdiagnoses Clinical Error Rate Per embryo Per transfer Per ongoing pregnancy 0. 2% 0. 3% 0. 1% • 4974 embryos • 3168 transfers • 2976 gestations (62. 1%) • 2354 ongoing / delivered (72. 1%) • 10 errors – 1 tetraploid – 2 monosomies – 7 trisomies • Mean age 38. 4 years • 10 errors – 7 found in losses – 3 found in ongoing preg. Mosaicism evaluated in 4 samples – 100% mosaic
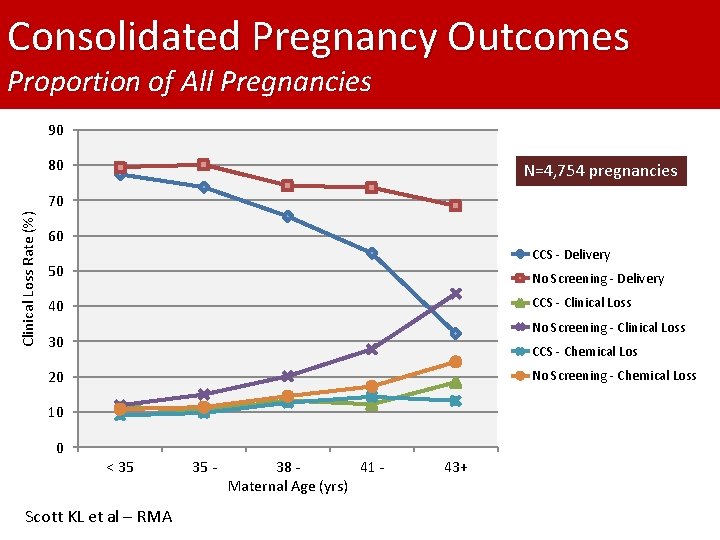
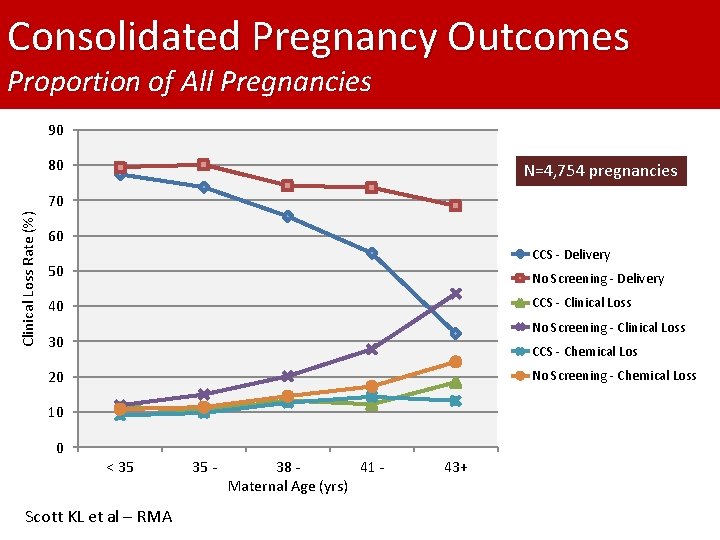
Consolidated Pregnancy Outcomes Proportion of All Pregnancies 90 80 N=4, 754 pregnancies Clinical Loss Rate (%) 70 60 CCS - Delivery 50 No Screening - Delivery CCS - Clinical Loss 40 No Screening - Clinical Loss 30 CCS - Chemical Los 20 No Screening - Chemical Loss 10 0 < 35 Scott KL et al – RMA 35 - 38 41 Maternal Age (yrs) 43+
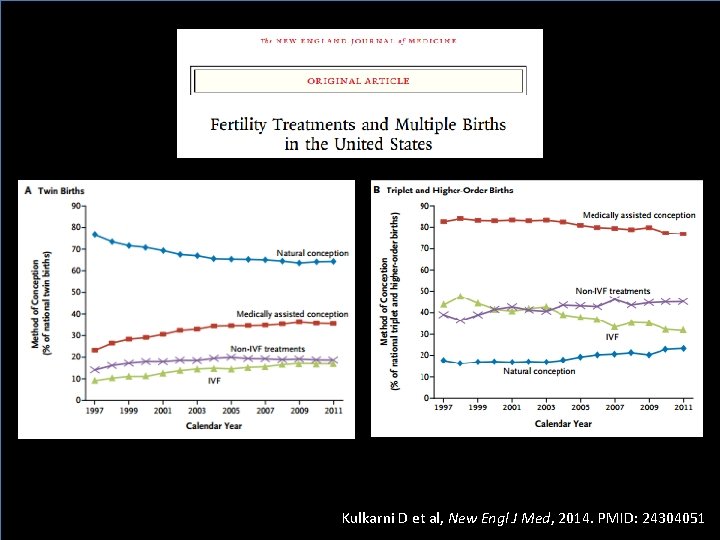
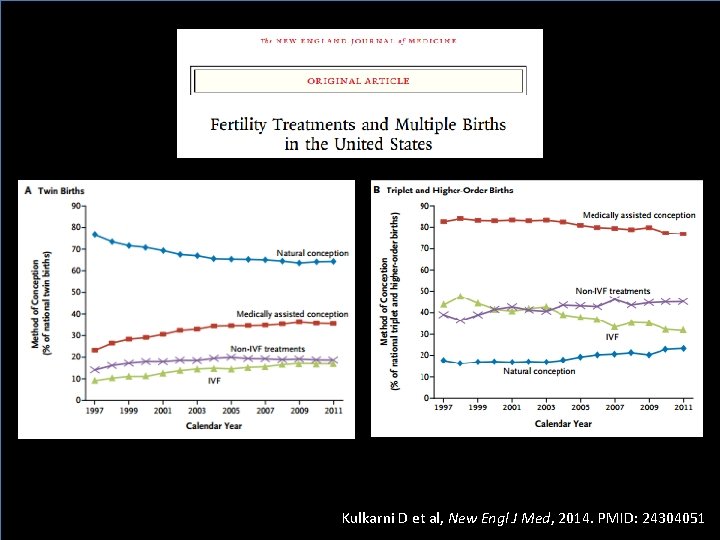
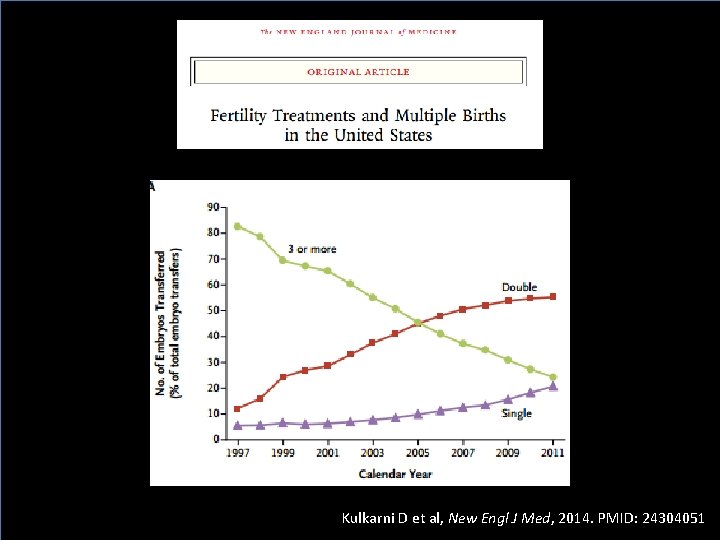
Kulkarni D et al, New Engl J Med, 2014. PMID: 24304051
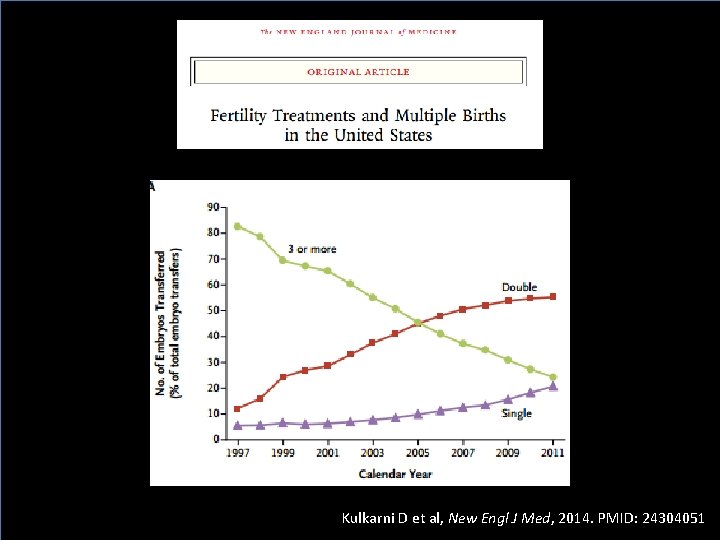
Kulkarni D et al, New Engl J Med, 2014. PMID: 24304051
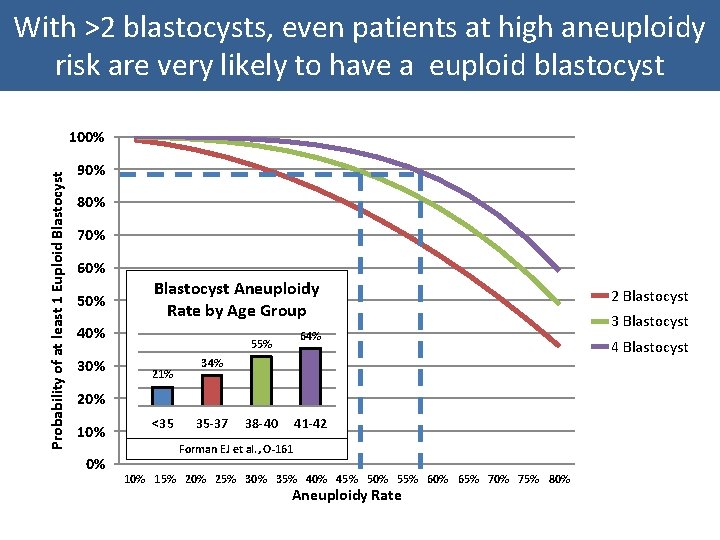
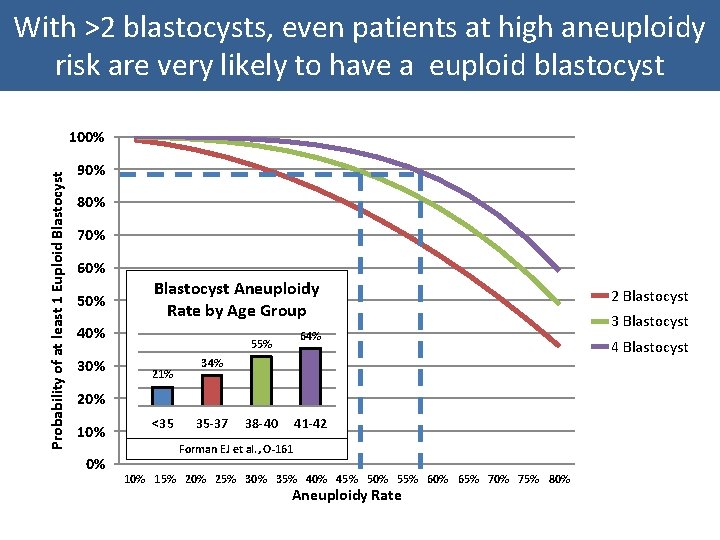
With >2 blastocysts, even patients at high aneuploidy risk are very likely to have a euploid blastocyst Probability of at least 1 Euploid Blastocyst 100% 90% 80% 70% 60% 50% Blastocyst Aneuploidy Rate by Age Group 40% 64% 30% 55% 21% 34% 20% 10% 0% <35 35 -37 38 -40 41 -42 Forman EJ et al. , O-161 10% 15% 20% 25% 30% 35% 40% 45% 50% 55% 60% 65% 70% 75% 80% Aneuploidy Rate 2 Blastocyst 3 Blastocyst 4 Blastocyst
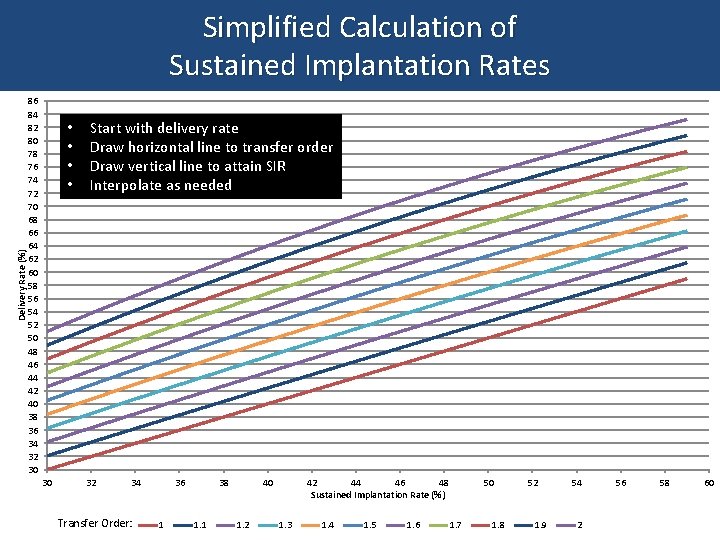
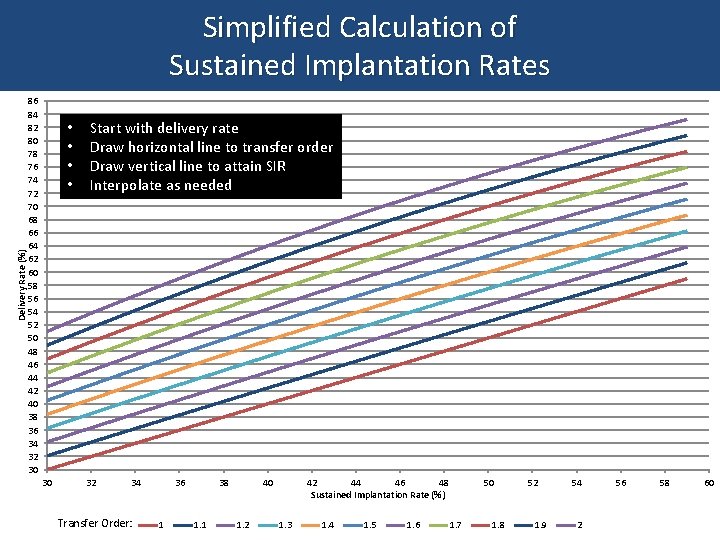
Delivery Rate (%) Simplified Calculation of Sustained Implantation Rates 86 84 82 80 78 76 74 72 70 68 66 64 62 60 58 56 54 52 50 48 46 44 42 40 38 36 34 32 30 • • 30 Start with delivery rate Draw horizontal line to transfer order Draw vertical line to attain SIR Interpolate as needed 32 34 Transfer Order: 36 1 38 1. 1 40 1. 2 42 44 46 48 Sustained Implantation Rate (%) 1. 3 1. 4 1. 5 1. 6 50 1. 7 1. 8 52 1. 9 54 2 56 58 60
Singleton Term Delivery: The Ideal IVF Outcome • IVF twin pregnancies are at an increased risk of: – Preeclampsia (2 -fold risk increase)1 – Extreme prematurity (7. 4 -fold increase delivery <32 wks) 2 – NICU admission (3. 8 -fold increased risk)2 – Perinatal Death (2 -fold increase)2 • Two IVF singleton deliveries have better obstetrical outcomes than one IVF twin delivery 3 1. 2. 3. ASRM Practice Committee, Fertil Steril, 2012. PMID: 22192352 Pinborg A, et al. , Acta Obstet Gynecol Scand, 2004. PMID: 15488125 Sazonova A , et al. , Fertil Steril, 2013. PMID: 23219009
The Perception that Patients Love Multiples if They are Born Healthy is not Well Validated Provided by a patient…
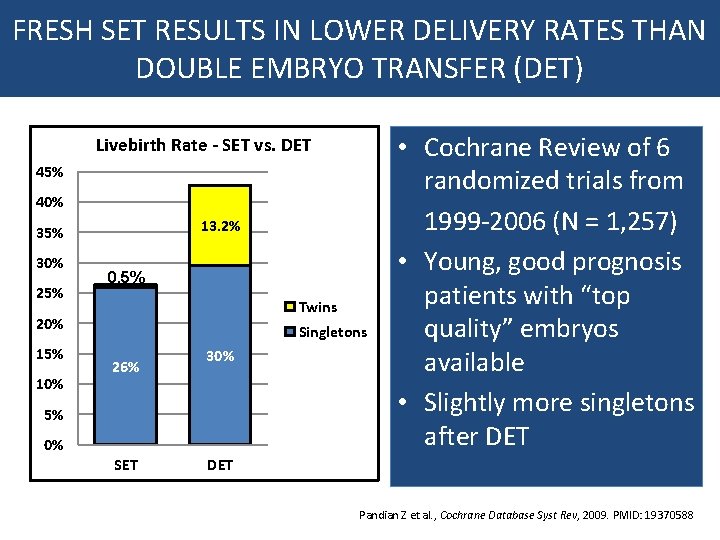
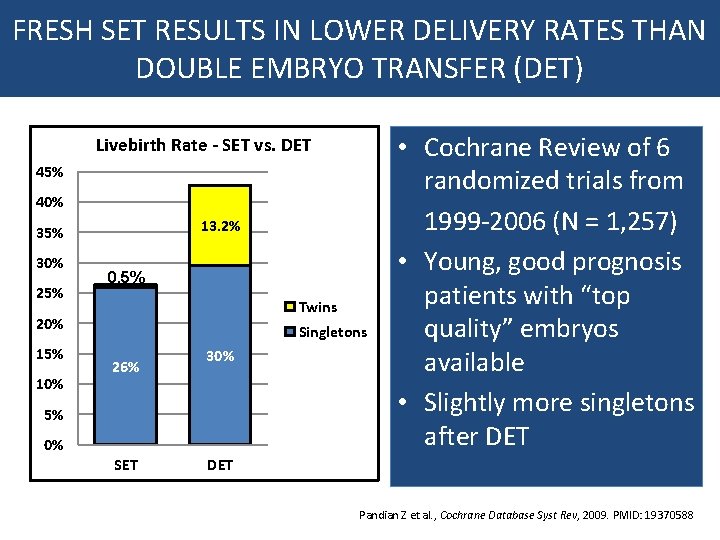
FRESH SET RESULTS IN LOWER DELIVERY RATES THAN DOUBLE EMBRYO TRANSFER (DET) Livebirth Rate - SET vs. DET 45% 40% 13. 2% 35% 30% 25% 0. 5% Twins 20% 15% 10% Singletons 26% 30% 5% 0% SET • Cochrane Review of 6 randomized trials from 1999 -2006 (N = 1, 257) • Young, good prognosis patients with “top quality” embryos available • Slightly more singletons after DET Pandian Z et al. , Cochrane Database Syst Rev, 2009. PMID: 19370588
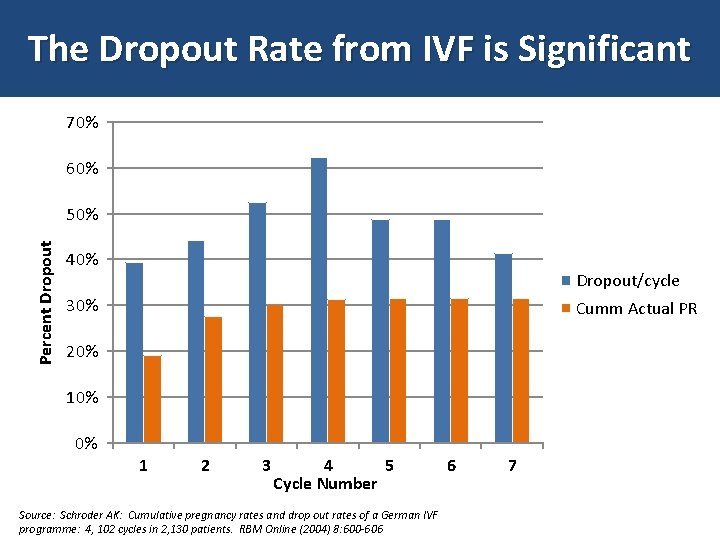
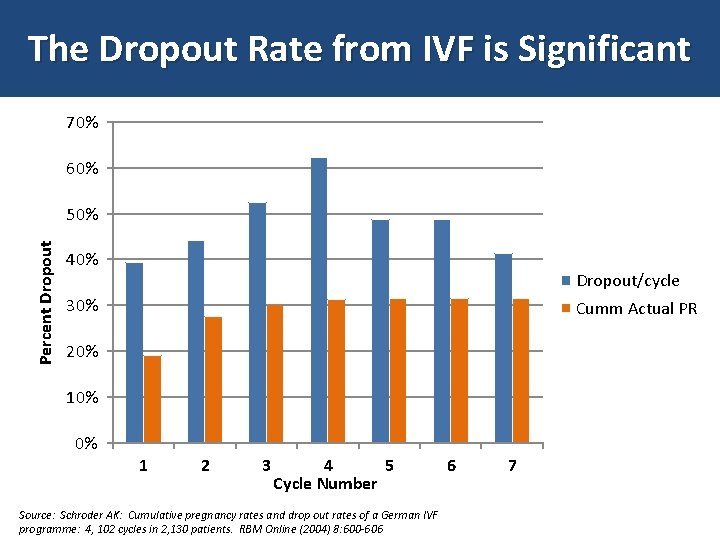
The Dropout Rate from IVF is Significant 70% 60% Percent Dropout 50% 40% Dropout/cycle 30% Cumm Actual PR 20% 10% 0% 1 2 3 4 5 Cycle Number Source: Schroder AK: Cumulative pregnancy rates and drop out rates of a German IVF programme: 4, 102 cycles in 2, 130 patients. RBM Online (2004) 8: 600 -606 6 7
1 Can ≥ 2?
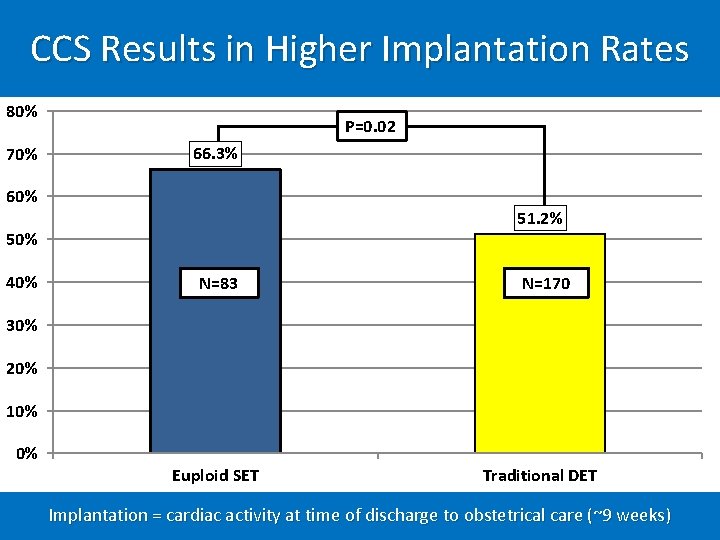
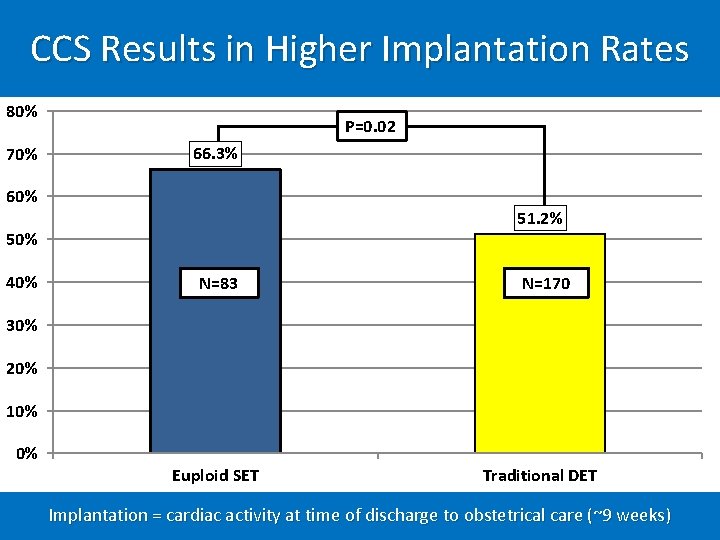
CCS Results in Higher Implantation Rates 80% 70% P=0. 02 66. 3% 60% 51. 2% 50% 40% N=83 N=170 30% 20% 10% 0% Euploid SET Traditional DET Implantation = cardiac activity at time of discharge to obstetrical care (~9 weeks)
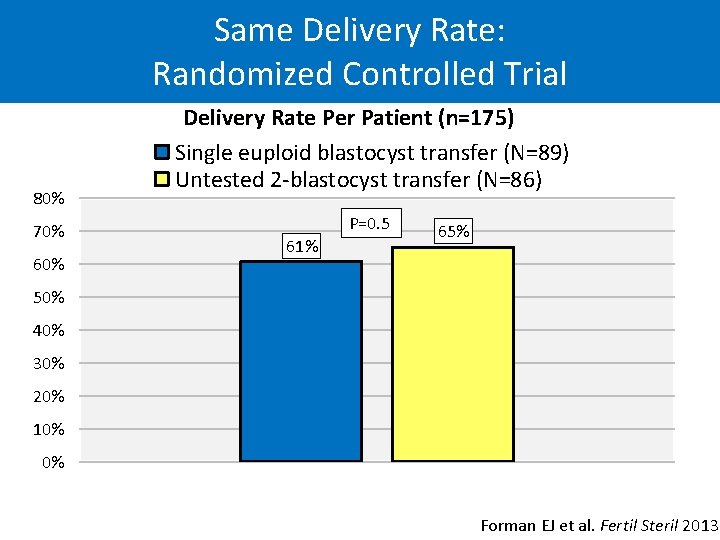
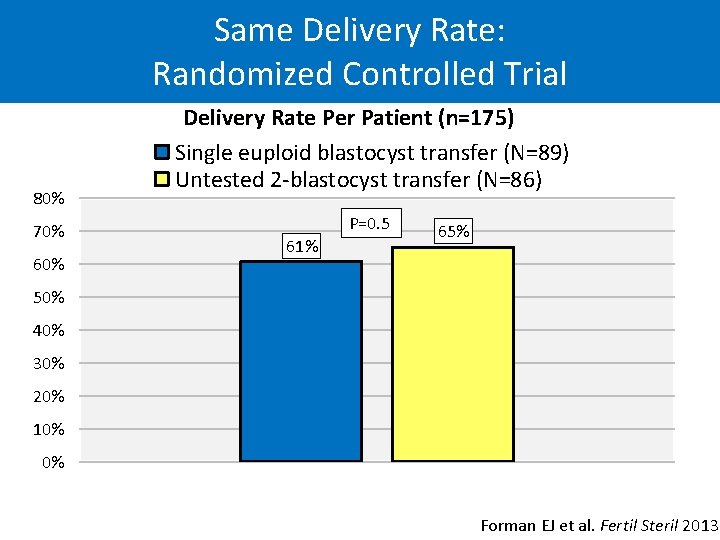
Same Delivery Rate: Randomized Controlled Trial 80% 70% 60% Delivery Rate Per Patient (n=175) Single euploid blastocyst transfer (N=89) Untested 2 -blastocyst transfer (N=86) P=0. 5 61% 65% 50% 40% 30% 20% 10% 0% Forman EJ et al. Fertil Steril 2013
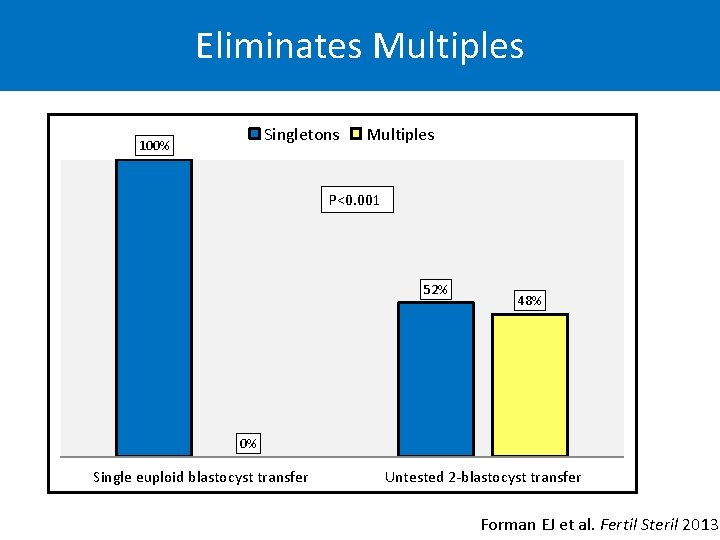
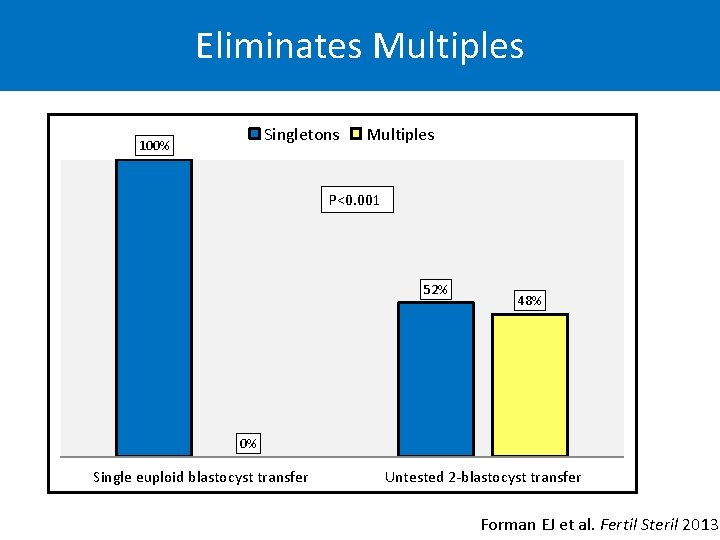
Eliminates Multiples Singletons 100% Multiples P<0. 001 52% 48% 0% Single euploid blastocyst transfer Untested 2 -blastocyst transfer Forman EJ et al. Fertil Steril 2013
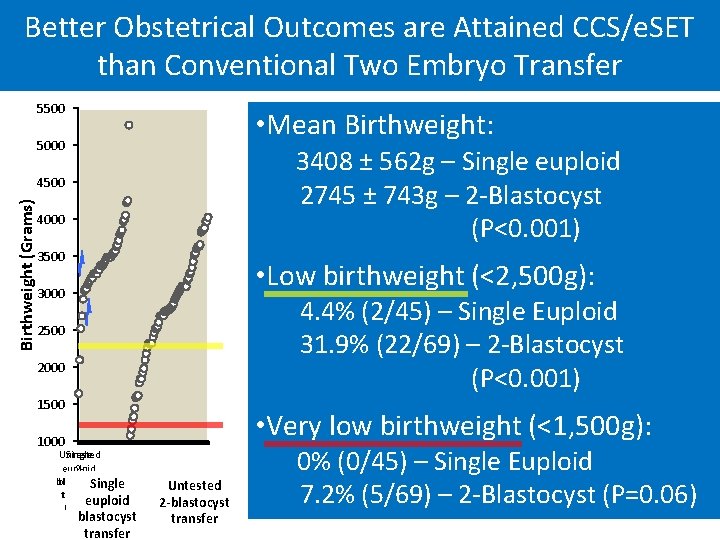
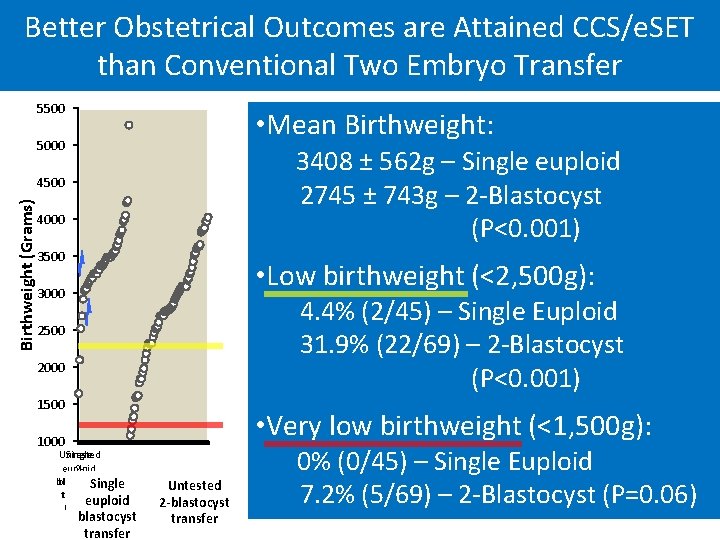
Better Obstetrical Outcomes are Attained CCS/e. SET than Conventional Two Embryo Transfer 5500 • Mean Birthweight: 5000 3408 ± 562 g – Single euploid 2745 ± 743 g – 2 -Blastocyst (P<0. 001) Birthweight (Grams) 4500 4000 3500 • Low birthweight (<2, 500 g): 3000 4. 4% (2/45) – Single Euploid 31. 9% (22/69) – 2 -Blastocyst (P<0. 001) 2500 2000 1500 • Very low birthweight (<1, 500 g): 1000 Untested Single euploid 2 blastocyst Single transfer euploid Grams blastocyst transfer Untested 2 -blastocyst transfer 0% (0/45) – Single Euploid 7. 2% (5/69) – 2 -Blastocyst (P=0. 06)
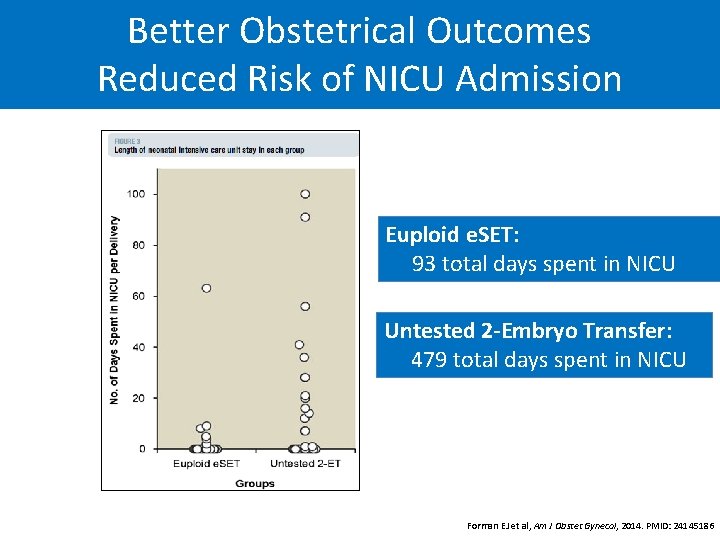
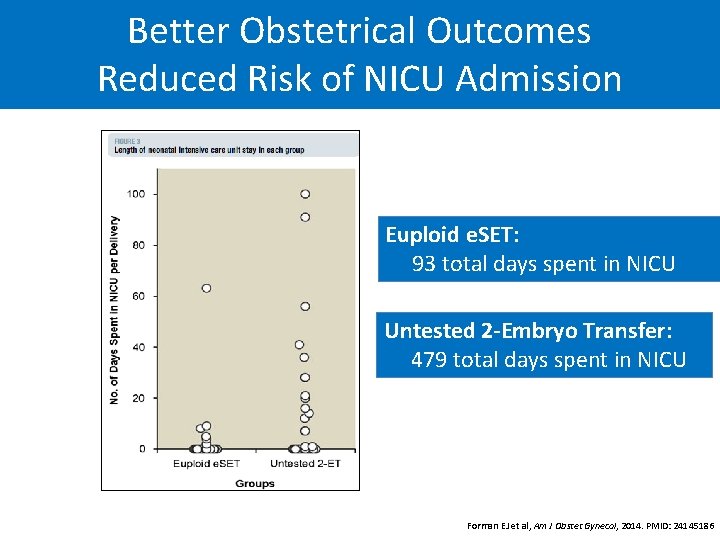
Better Obstetrical Outcomes Reduced Risk of NICU Admission Euploid e. SET: 93 total days spent in NICU Untested 2 -Embryo Transfer: 479 total days spent in NICU Forman EJ et al, Am J Obstet Gynecol, 2014. PMID: 24145186
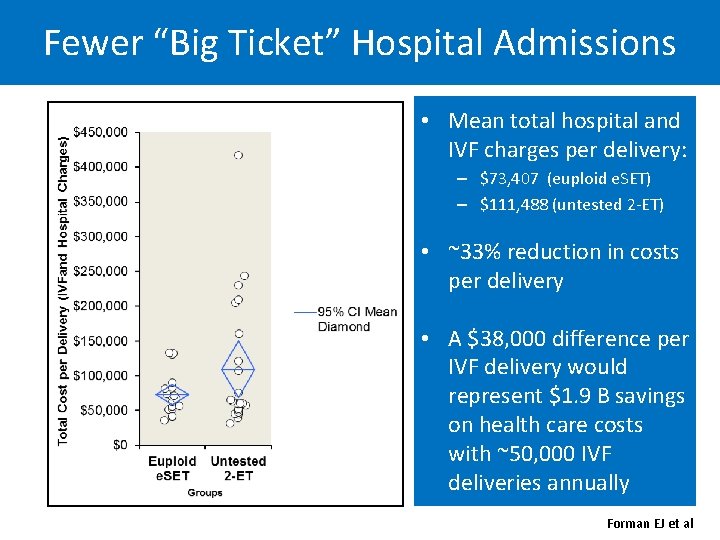
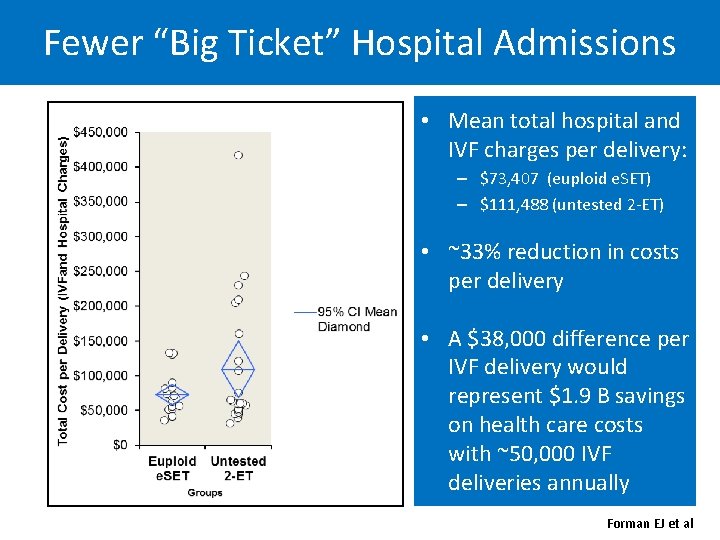
Fewer “Big Ticket” Hospital Admissions • Mean total hospital and IVF charges per delivery: – $73, 407 (euploid e. SET) – $111, 488 (untested 2 -ET) • ~33% reduction in costs per delivery • A $38, 000 difference per IVF delivery would represent $1. 9 B savings on health care costs with ~50, 000 IVF deliveries annually Forman EJ et al
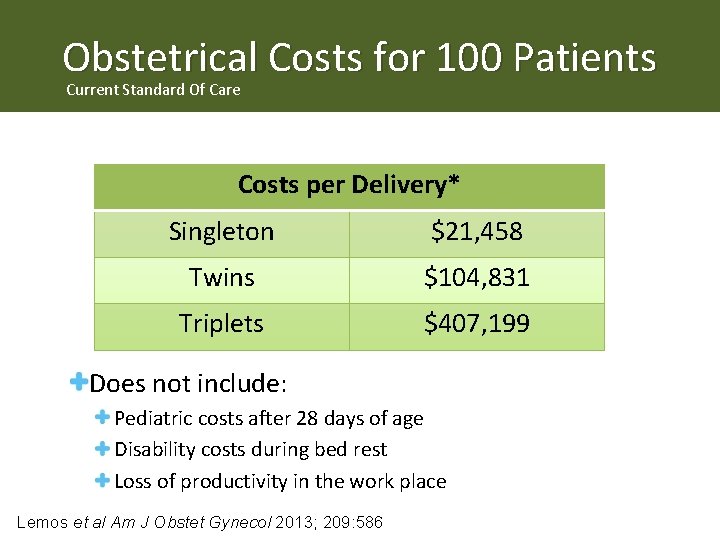
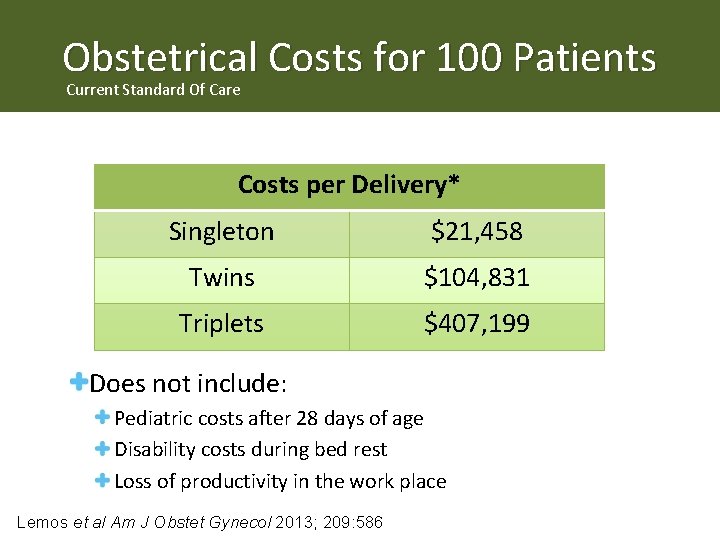
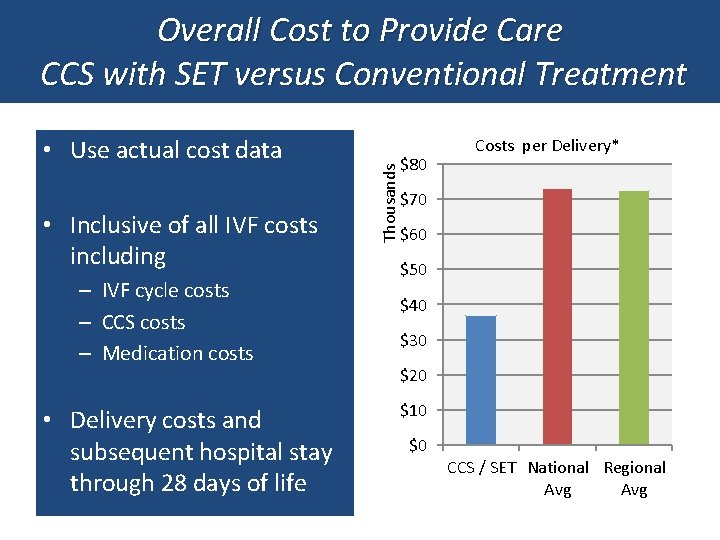
Obstetrical Costs for 100 Patients Current Standard Of Care Costs per Delivery* Singleton $21, 458 Twins $104, 831 Triplets $407, 199 Does not include: Pediatric costs after 28 days of age Disability costs during bed rest Loss of productivity in the work place Lemos et al Am J Obstet Gynecol 2013; 209: 586
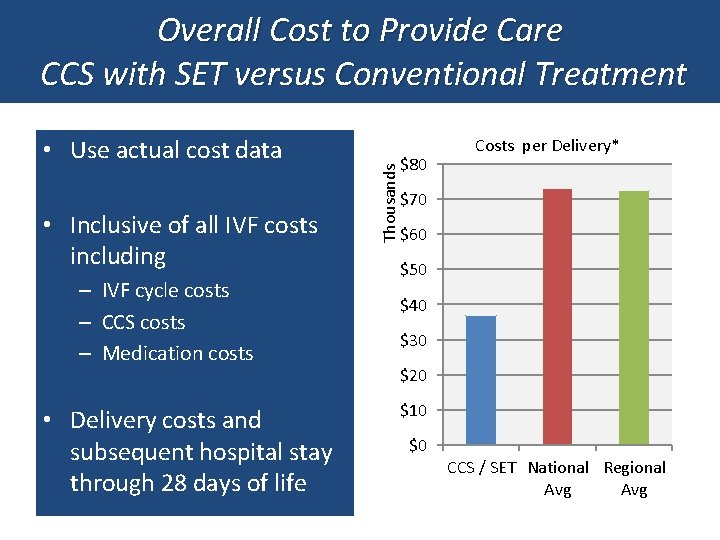
• Use actual cost data • Inclusive of all IVF costs including – IVF cycle costs – CCS costs – Medication costs • Delivery costs and subsequent hospital stay through 28 days of life Thousands Overall Cost to Provide Care CCS with SET versus Conventional Treatment $80 Costs per Delivery* $70 $60 $50 $40 $30 $20 $10 $0 CCS / SET National Regional Avg
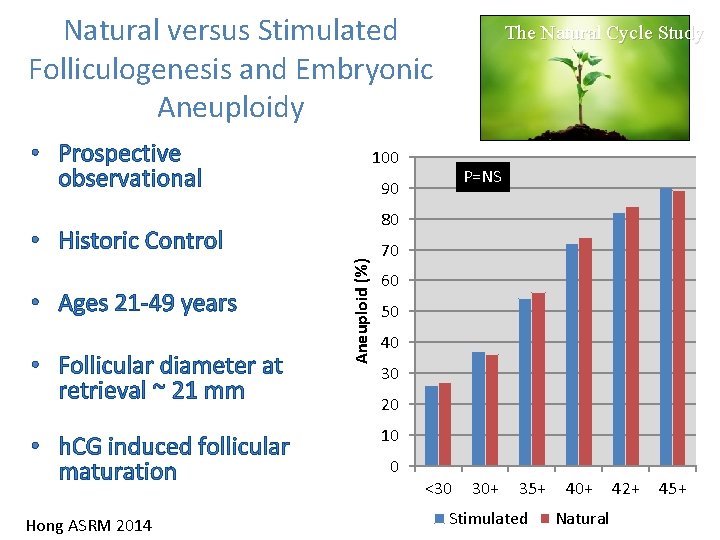
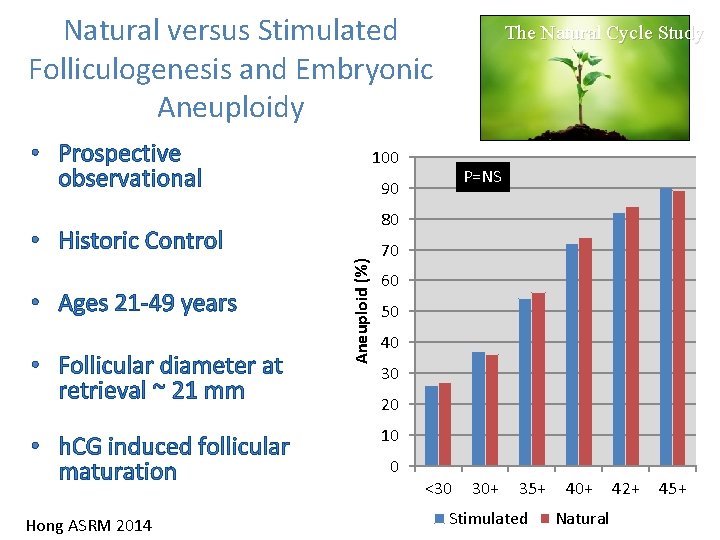
Natural versus Stimulated Folliculogenesis and Embryonic Aneuploidy • Prospective observational 100 80 • h. CG induced follicular maturation Hong ASRM 2014 Aneuploid (%) • Follicular diameter at retrieval ~ 21 mm P=NS 90 • Historic Control • Ages 21 -49 years The Natural Cycle Study 70 60 50 40 30 20 10 0 <30 30+ 35+ Stimulated 40+ Natural 42+ 45+
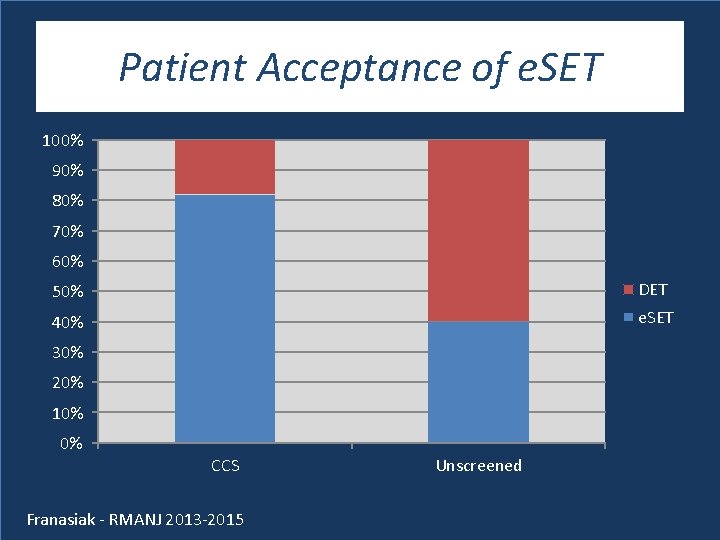
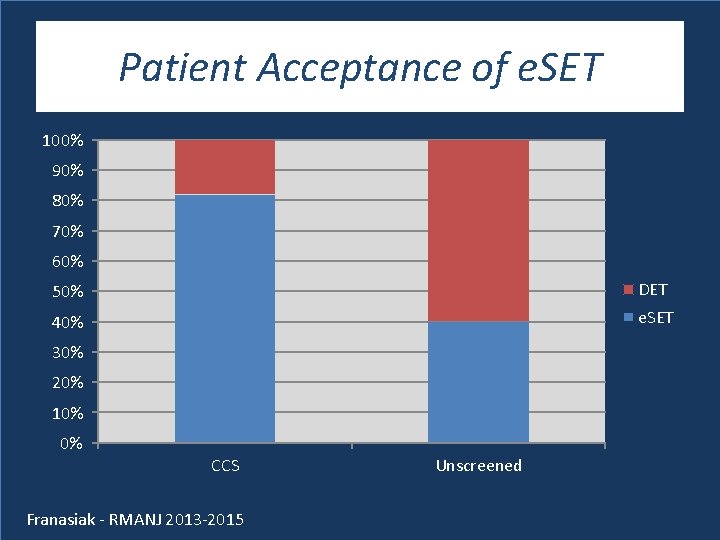
Patient Acceptance of e. SET 100% 90% 80% 70% 60% 50% DET 40% e. SET 30% 20% 10% 0% CCS Franasiak - RMANJ 2013 -2015 Unscreened

Follow Up on Prospective Trials
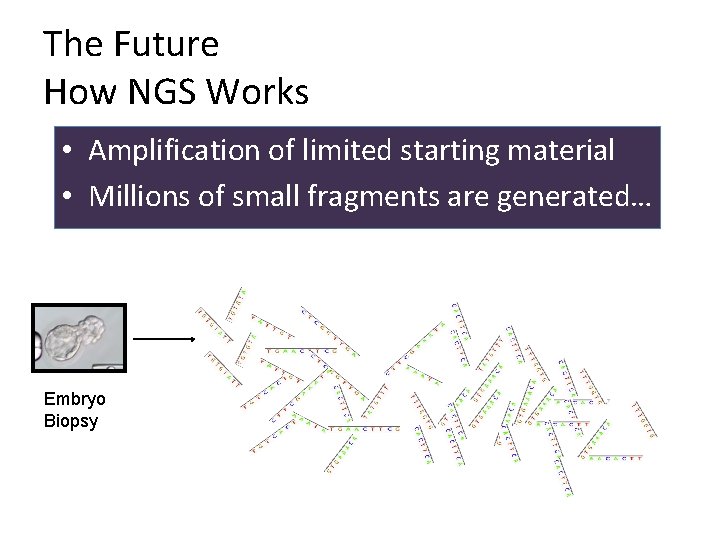
The Future How NGS Works • Amplification of limited starting material • Millions of small fragments are generated… Embryo Biopsy
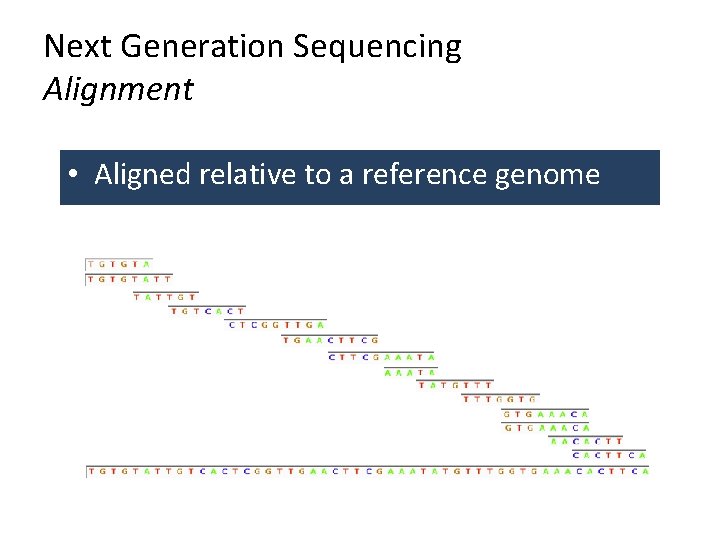
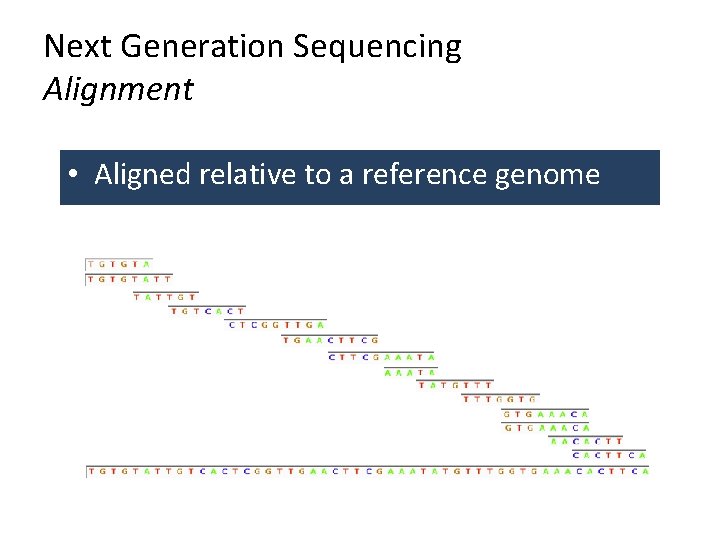
Next Generation Sequencing Alignment • Aligned relative to a reference genome
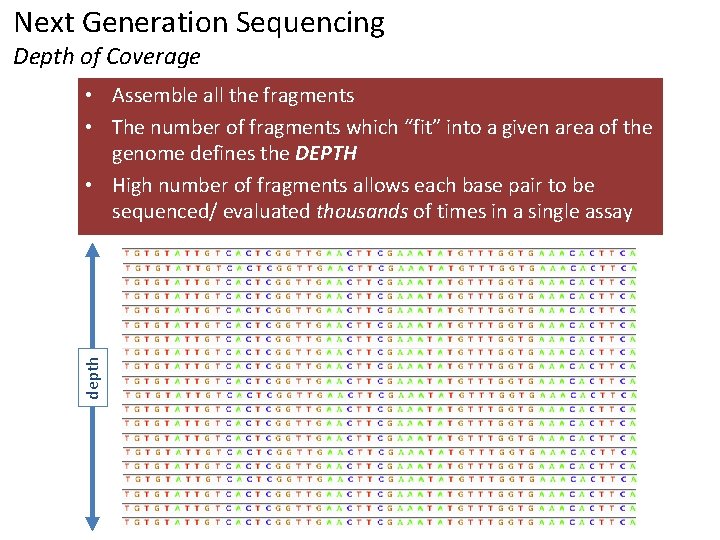
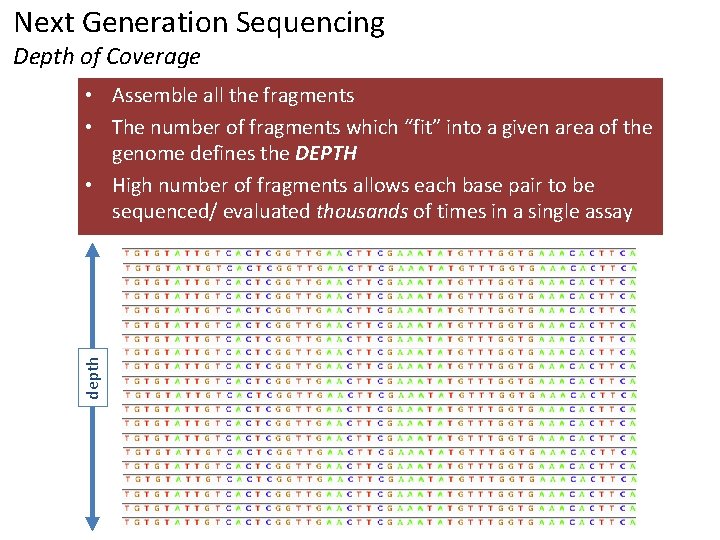
Next Generation Sequencing Depth of Coverage depth • Assemble all the fragments • The number of fragments which “fit” into a given area of the genome defines the DEPTH • High number of fragments allows each base pair to be sequenced/ evaluated thousands of times in a single assay
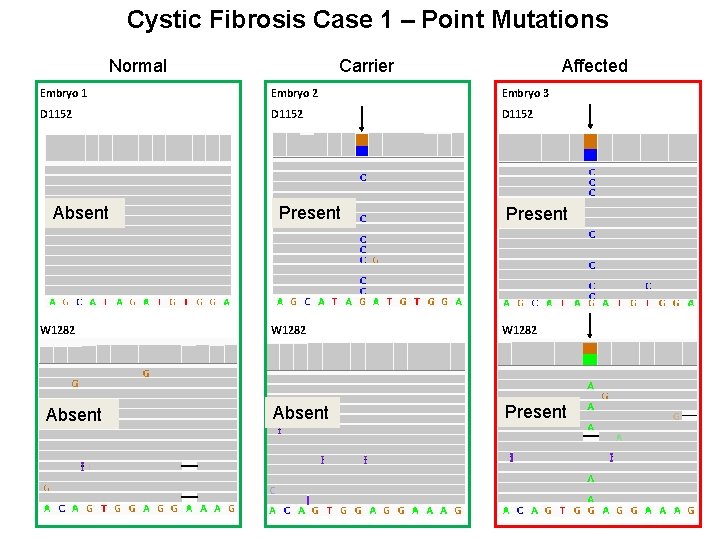
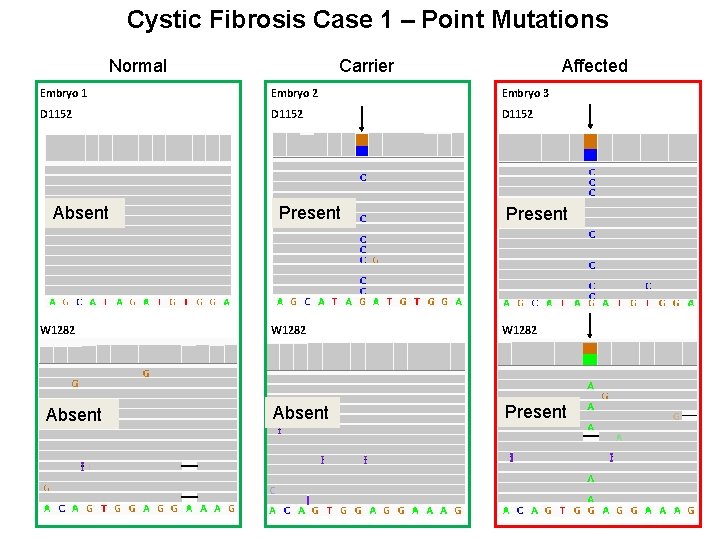
Cystic Fibrosis Case 1 – Point Mutations Normal Carrier Affected Embryo 1 Embryo 2 Embryo 3 D 1152 Absent W 1282 Absent Present
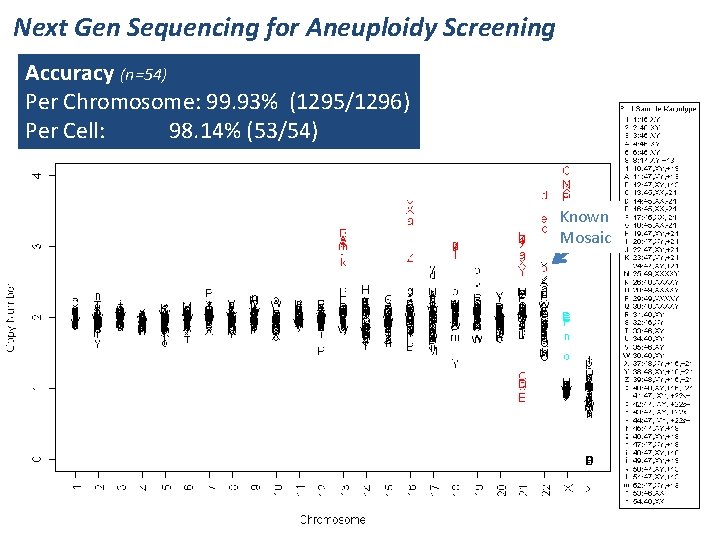
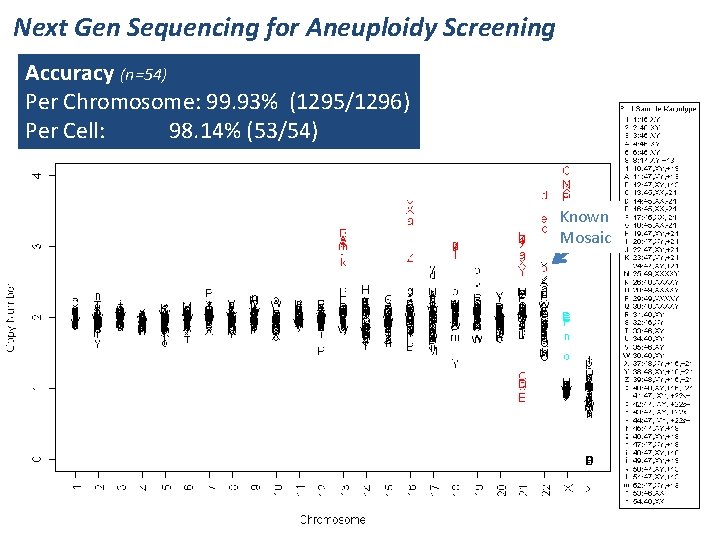
Next Gen Sequencing for Aneuploidy Screening Accuracy (n=54) Per Chromosome: 99. 93% (1295/1296) Per Cell: 98. 14% (53/54) Known Mosaic Universal Primer with new UP reference (SNPs replaced with Ns), on 54 samples. Some small improvements. Coverage per sample is on next page. Known aneuploidies in red; known XX in cyan.
Time Lapse Observations in the Embryology Laboratory And others…. .
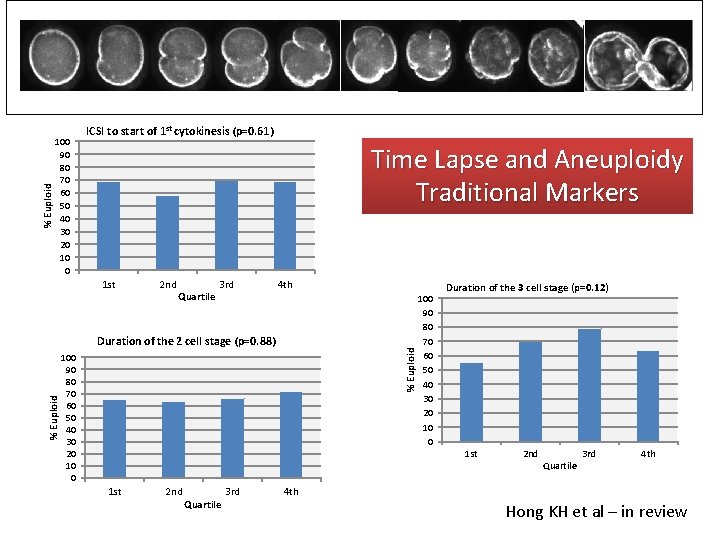
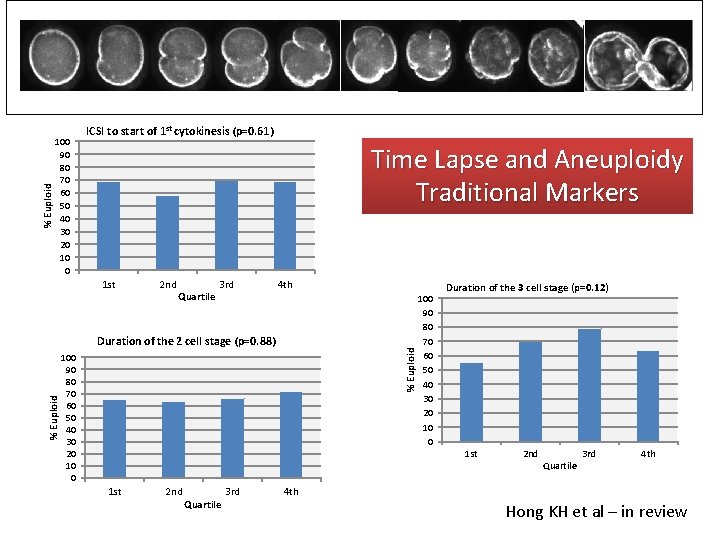
% Euploid 100 90 80 70 60 50 40 30 20 10 0 ICSI to start of 1 st cytokinesis (p=0. 61) Time Lapse and Aneuploidy Traditional Markers 1 st 2 nd Quartile 3 rd 4 th % Euploid Duration of the 2 cell stage (p=0. 88) 100 90 80 70 60 50 40 30 20 10 0 Duration of the 3 cell stage (p=0. 12) 1 st 2 nd Quartile 3 rd 4 th Hong KH et al – in review
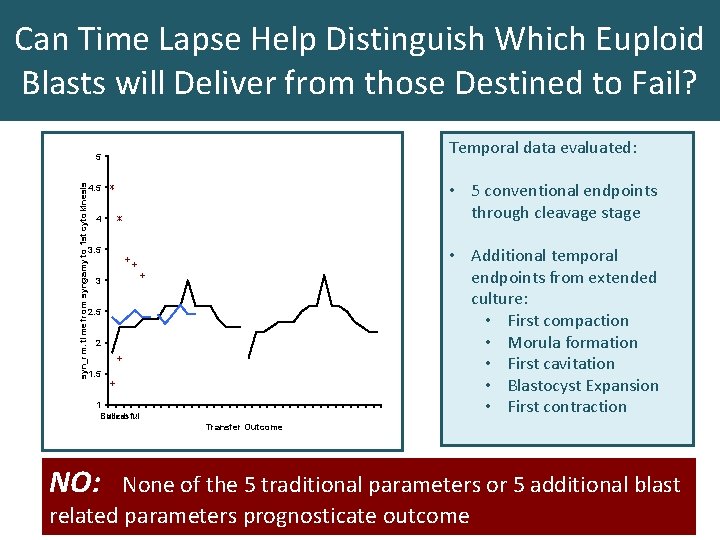
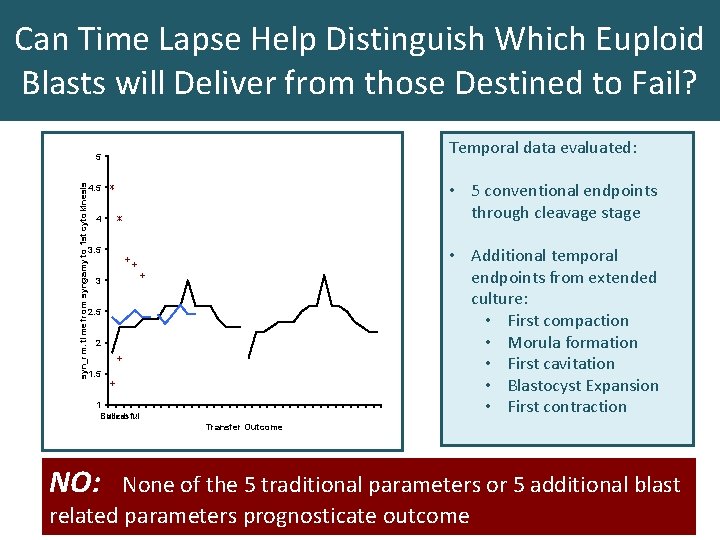
Can Time Lapse Help Distinguish Which Euploid Blasts will Deliver from those Destined to Fail? Temporal data evaluated: syn_rm: time from syngamy to 1 st cytokinesis 5 • 5 conventional endpoints through cleavage stage 4. 5 4 • Additional temporal endpoints from extended culture: • First compaction • Morula formation • First cavitation • Blastocyst Expansion • First contraction 3. 5 3 2. 5 2 1. 5 1 Failed Succesful Transfer Outcome NO: None of the 5 traditional parameters or 5 additional blast related parameters prognosticate outcome
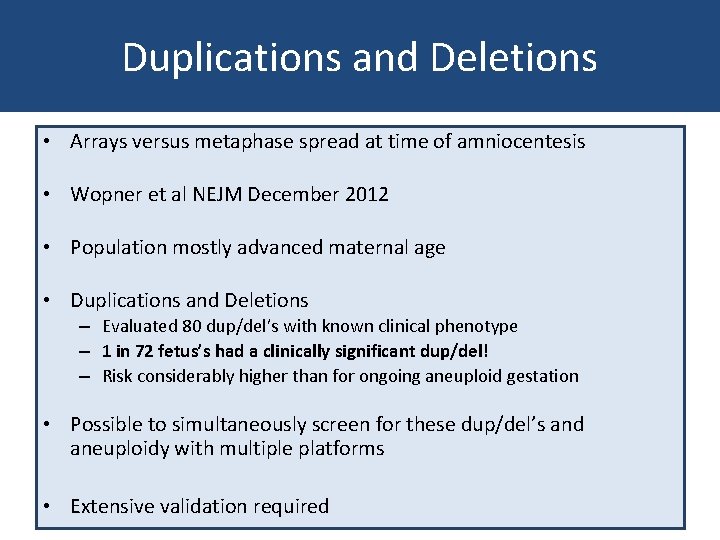
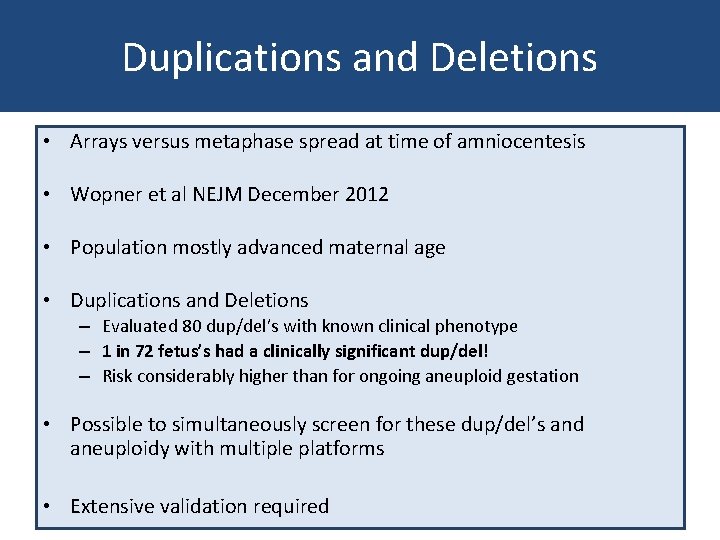
Duplications and Deletions • Arrays versus metaphase spread at time of amniocentesis • Wopner et al NEJM December 2012 • Population mostly advanced maternal age • Duplications and Deletions – Evaluated 80 dup/del’s with known clinical phenotype – 1 in 72 fetus’s had a clinically significant dup/del! – Risk considerably higher than for ongoing aneuploid gestation • Possible to simultaneously screen for these dup/del’s and aneuploidy with multiple platforms • Extensive validation required
Some Disagree with PGS • • All embryo selection techniques are detrimental Inappropriate to use “Implantation Rates” as an endpoint “it can be questioned whether all patients will ever be able to understand all of the complexities concerning PGS” “cost-effectiveness is being forgotten” “In our view evaluating the (cost-)effectiveness of medical treatments is by far the greatest challenge in current day medicine, especially in an era where health care costs continue to increase to the extent where they are the number one item of expense for many governments across the globe” “evidence is now accumulating that all embryos in an IVF cycle can be cryopreserved and transferred in subsequent cycles without impairing, and maybe even improving, the cumulative pregnancy rate of that IVF cycle” Embryo selection should therefore not be used to select out embryos, but only to determine the order in which the embryos will be transferred, as the time to pregnancy can be improved by embryo selection, if embryos with the highest implantation potential are transferred first. Culturing to the blastocyst may be harmful
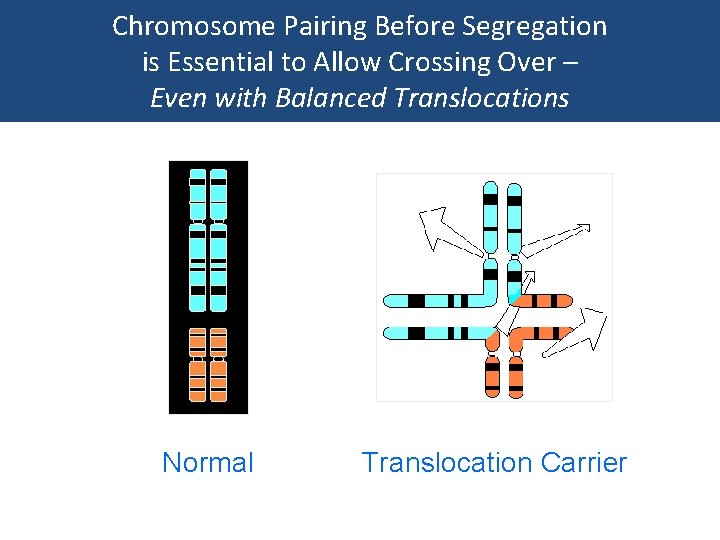
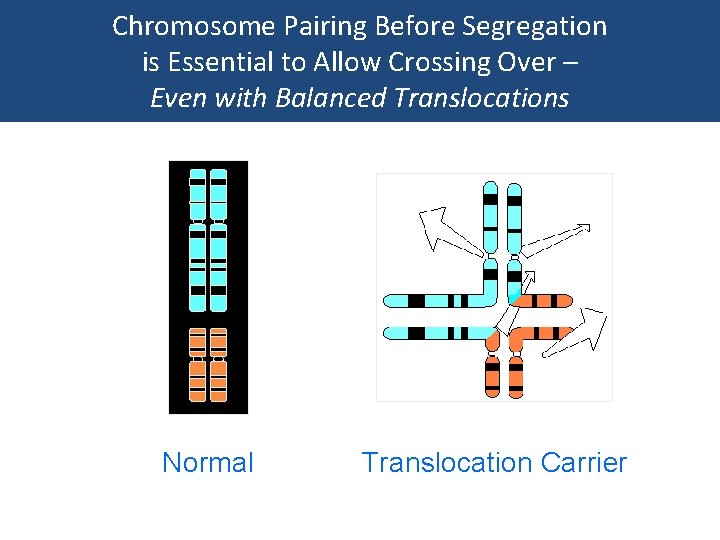
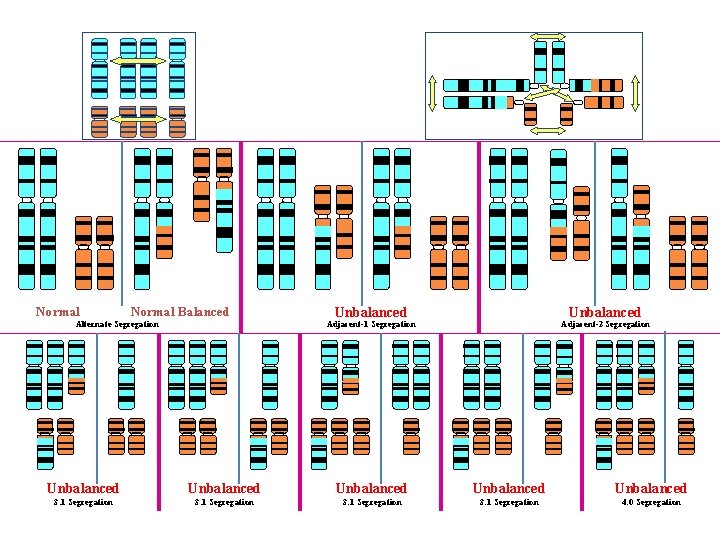
Chromosome Pairing Before Segregation is Essential to Allow Crossing Over – Even with Balanced Translocations Normal Translocation Carrier
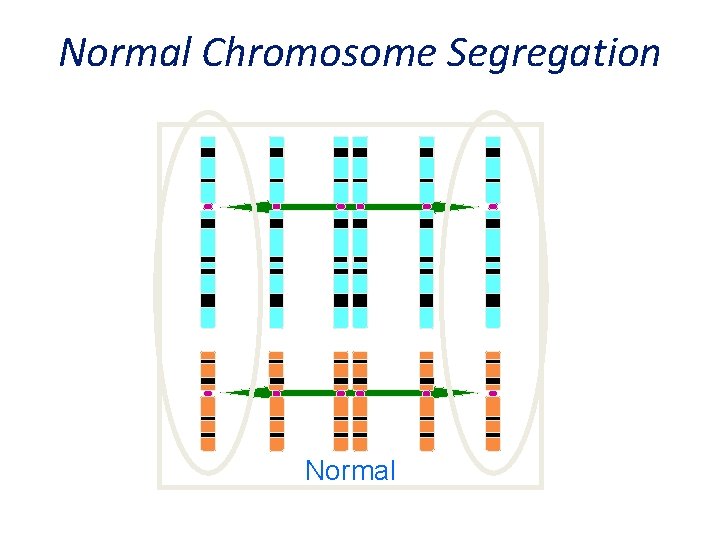
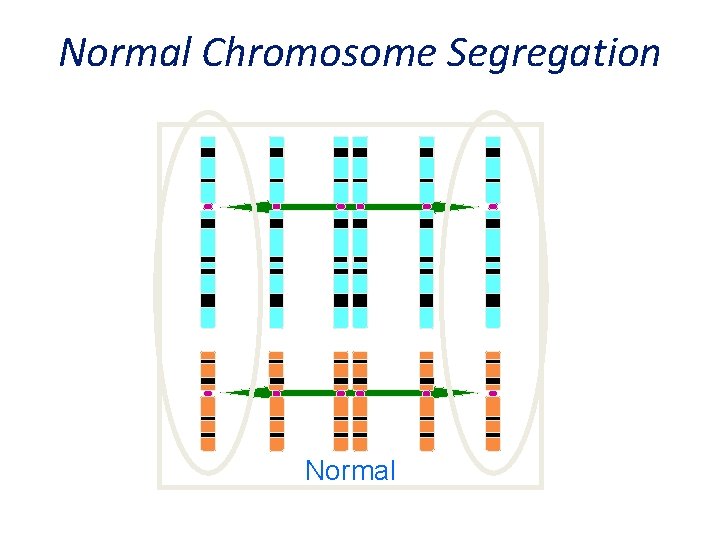
Normal Chromosome Segregation Normal
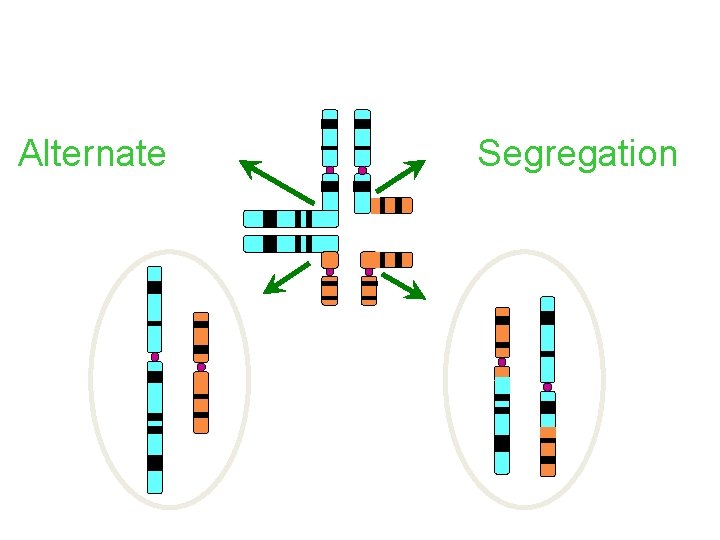
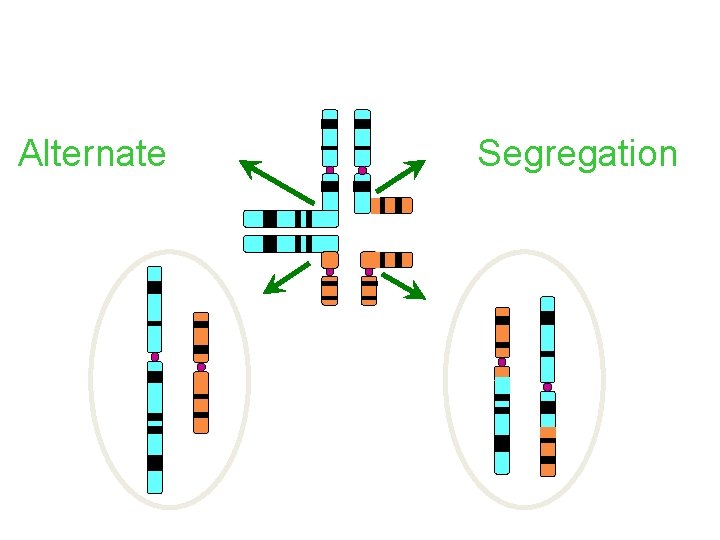
Translocations - Chromosome Segregation Alternate Segregation
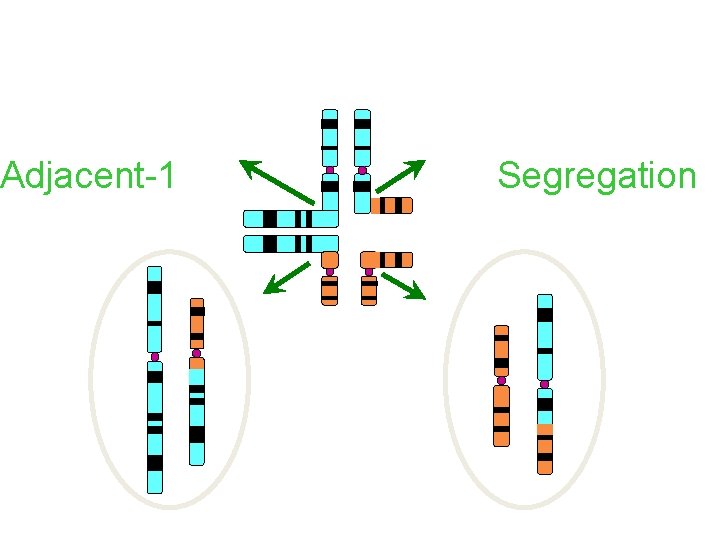
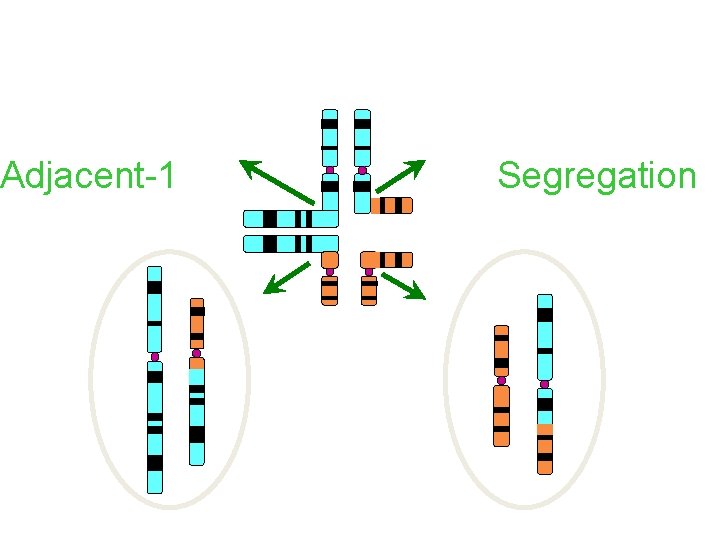
Translocations - Chromosome Segregation Adjacent-1 Segregation
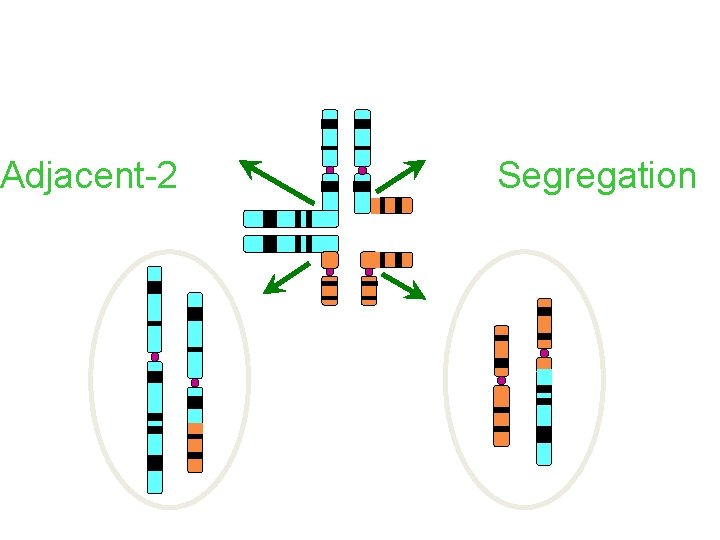
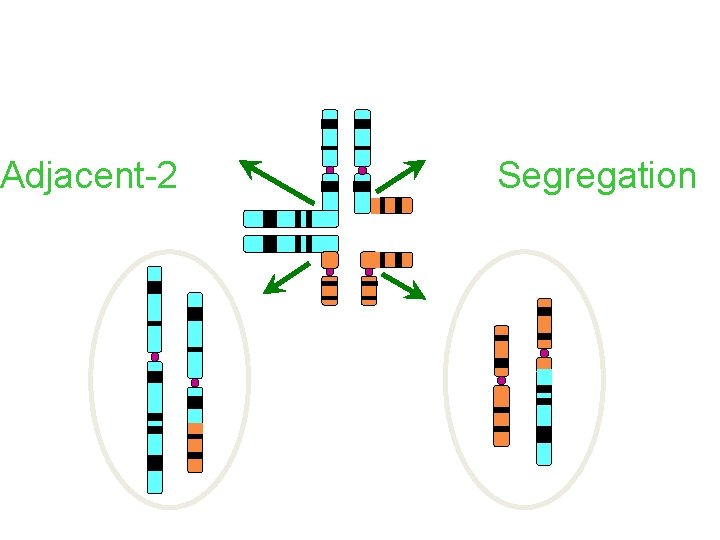
Translocations - Chromosome Segregation Adjacent-2 Segregation
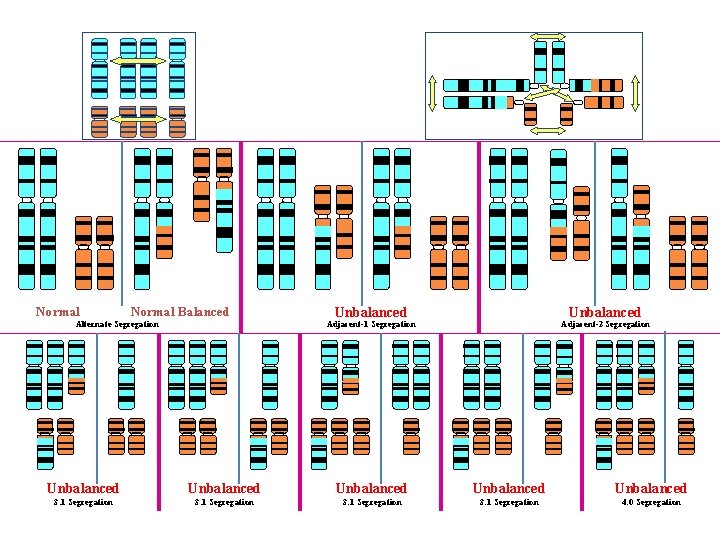
Normal Balanced Alternate Segregation Unbalanced Adjacent-1 Segregation Adjacent-2 Segregation Unbalanced Unbalanced 3: 1 Segregation 4: 0 Segregation
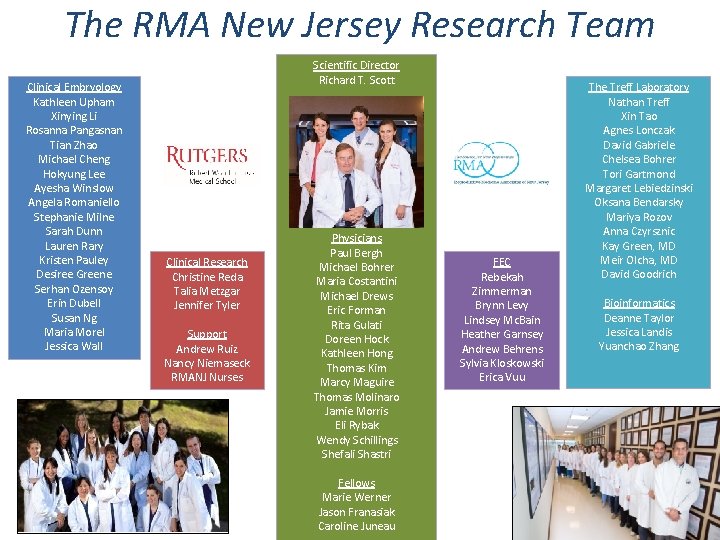
The RMA New Jersey Research Team Clinical Embryology Kathleen Upham Xinying Li Rosanna Pangasnan Tian Zhao Michael Cheng Hokyung Lee Ayesha Winslow Angela Romaniello Stephanie Milne Sarah Dunn Lauren Rary Kristen Pauley Desiree Greene Serhan Ozensoy Erin Dubell Susan Ng Maria Morel Jessica Wall Scientific Director Richard T. Scott Clinical Research Christine Reda Talia Metzgar Jennifer Tyler Support Andrew Ruiz Nancy Niemaseck RMANJ Nurses Physicians Paul Bergh Michael Bohrer Maria Costantini Michael Drews Eric Forman Rita Gulati Doreen Hock Kathleen Hong Thomas Kim Marcy Maguire Thomas Molinaro Jamie Morris Eli Rybak Wendy Schillings Shefali Shastri Fellows Marie Werner Jason Franasiak Caroline Juneau FEC Rebekah Zimmerman Brynn Levy Lindsey Mc. Bain Heather Garnsey Andrew Behrens Sylvia Kloskowski Erica Vuu The Treff Laboratory Nathan Treff Xin Tao Agnes Lonczak David Gabriele Chelsea Bohrer Tori Gartmond Margaret Lebiedzinski Oksana Bendarsky Mariya Rozov Anna Czyrsznic Kay Green, MD Meir Olcha, MD David Goodrich Bioinformatics Deanne Taylor Jessica Landis Yuanchao Zhang