Complications of the third stage Postpartum haemorrhage Primary



- Slides: 26
Complications of the third stage Postpartum haemorrhage
Primary postpartum haemorrhage: bleeding from the genital tract in excess of 500 ml at any time following the baby's birth up to 24 hours postpartum a mild PPH : A loss of 500– 999 ml in a healthy woman
severe hemorrhage : is deemed to be a loss of greater than 1000 ml
(PPH) is one of the most alarming and serious emergencies a midwife may face and can occur following both traumatic and straightforward births. a stressful experience for the woman and any support persons present undermine her confidence, influence her afitude to future childbearing delay her recovery. A significant causes of direct maternal death due to PPH, often in the absence of a trained health professional.
-The midwife is often the first, and may be the only, professional person present when a hemorrhage occurs -, so her prompt, competent action will be crucial l in controlling blood loss and reducing the risk of maternal morbidity or even death.
• Primary postpartum hemorrhage • Fluid loss is extremely di�cult to measure Because blood and fluid has soaked into the bed linen and spilled onto the floor. • measurable solidified clots represent only about half the total fluid loss. • small blood loss , may • adversely a� ects the mother's condition constitutes a PPH. depend upon the woman's general wellbeing
Causes • atonic uterus • retained placenta • trauma • blood coagulation disorder.
• *Atonic uterus • a failure of the myometrium at the placental site to contract and retract and to compress torn blood vessels and control blood loss by a living ligature action.
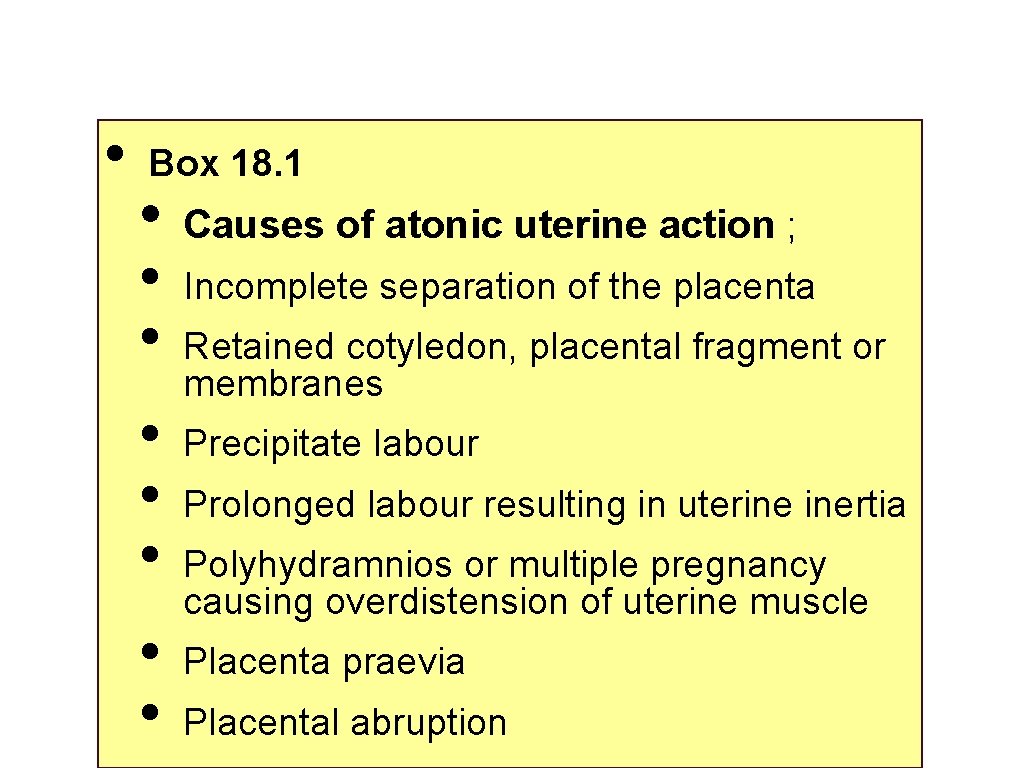
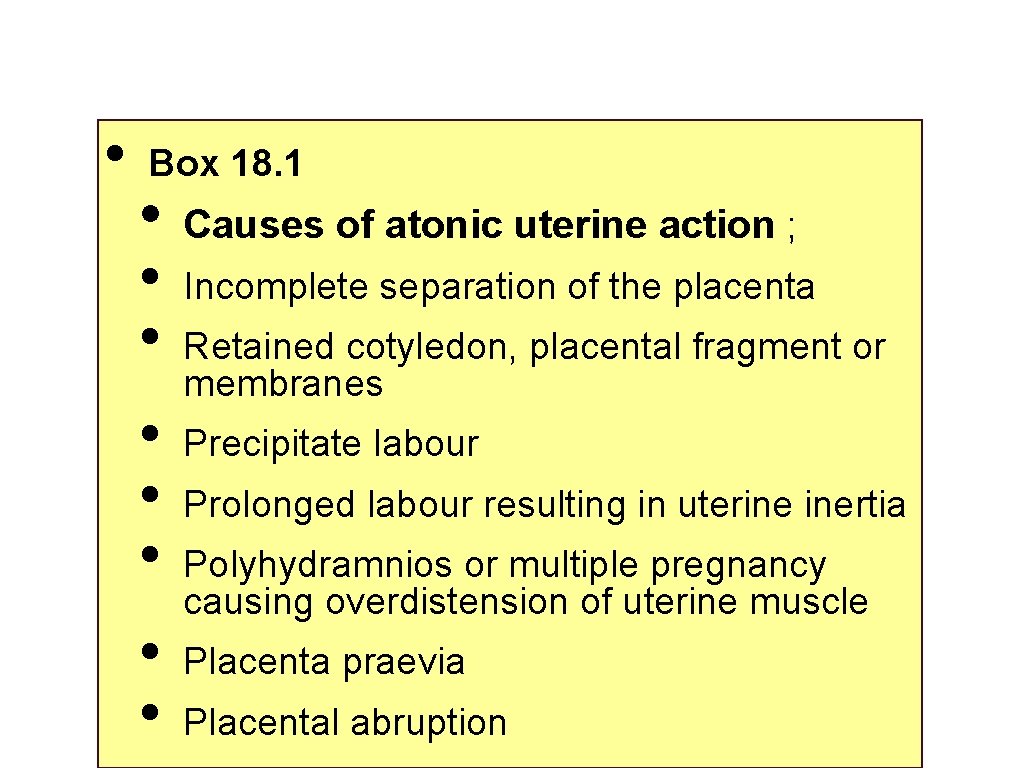
• Box 18. 1 • • Causes of atonic uterine action ; Incomplete separation of the placenta Retained cotyledon, placental fragment or membranes Precipitate labour Prolonged labour resulting in uterine inertia Polyhydramnios or multiple pregnancy causing overdistension of uterine muscle Placenta praevia Placental abruption
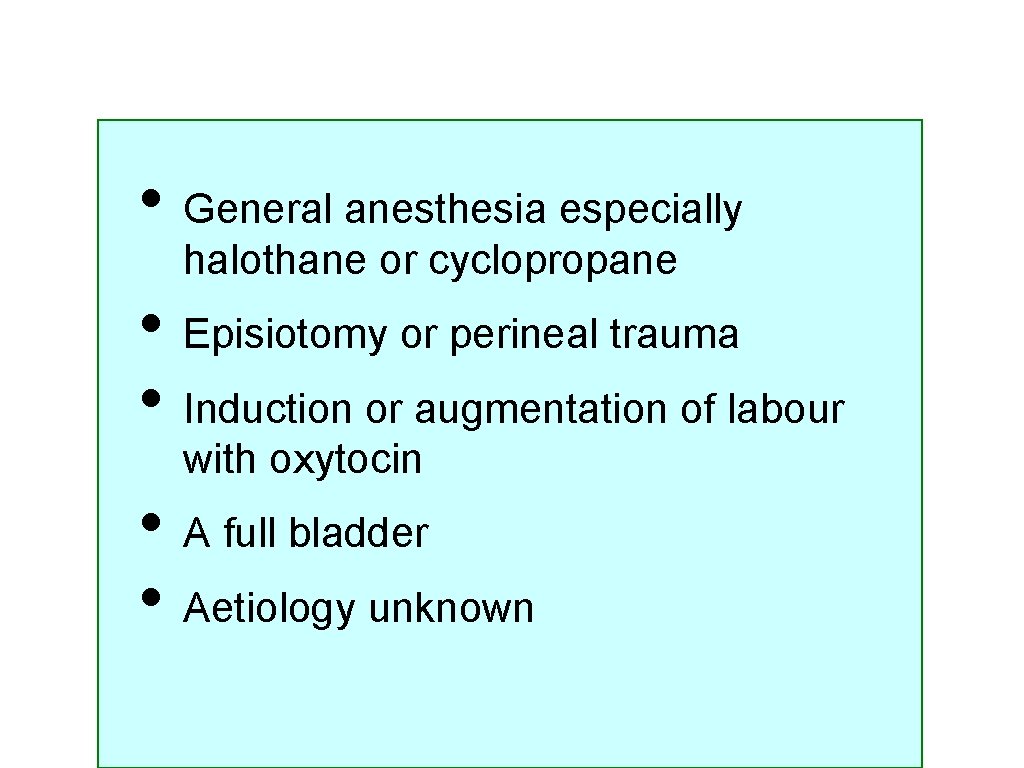
• General anesthesia especially halothane or cyclopropane • Episiotomy or perineal trauma • Induction or augmentation of labour with oxytocin • A full bladder • Aetiology unknown
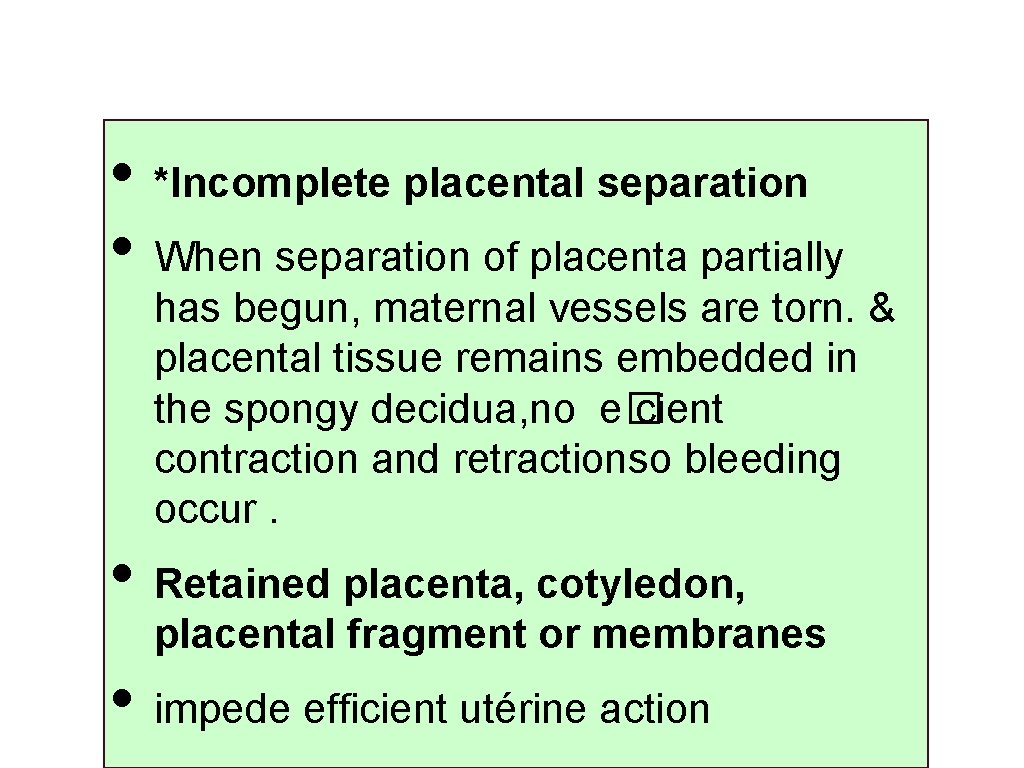
• *Incomplete placental separation • When separation of placenta partially has begun, maternal vessels are torn. & placental tissue remains embedded in the spongy decidua, no e� cient contraction and retractionso bleeding occur. • Retained placenta, cotyledon, placental fragment or membranes • impede efficient utérine action
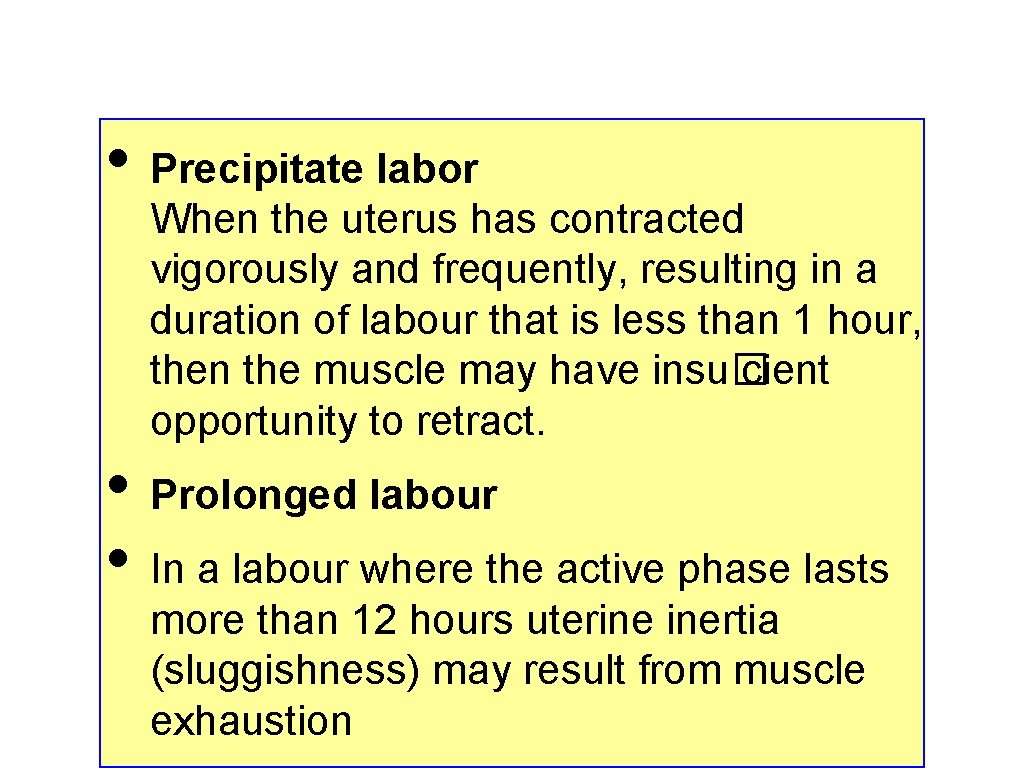
• Precipitate labor When the uterus has contracted vigorously and frequently, resulting in a duration of labour that is less than 1 hour, then the muscle may have insu� cient opportunity to retract. • Prolonged labour • In a labour where the active phase lasts more than 12 hours uterine inertia (sluggishness) may result from muscle exhaustion
• • • Polyhydramnios, macrosomia or multiple pregnancy The myometrium becomes excessively stretched and therefore less e� cient ). Placenta praevia The placental site is partly or wholly in the lower segment where thinner muscle layer contains few oblique fibres: this results in poor control of bleeding. Placental abruption Blood may have seeped between the muscle fibres, interfering with e� ective action. At its most severe this results in a Couvelaire uterus

• • Induction or augmentation of labor with oxytocin -some case , the use of oxytocin during labour may result in hyperstimulation of the uterus and cause a precipitate, expulsive birth of the baby - the uterus may still be responding in a stimulated, but ine� ective manner in terms of contracting the empty uterus. -In the case of induction or augmentation of labor, that continues over a prolonged period without establishing e� cient uterine contractions, :
• The result will be : • @physical and emotional fatigue of the mother • @ uterine fatigue or inertia may occur. • @ inertia inhibits the uterine muscle from providing strong, sustained contraction and retraction of the empty uterus that aids in the prevention of a postpartum haemorrhage
• Episiotomy, and need for perineal sutures • -Blood loss from perineal trauma, in addition to even a normal blood loss from the uterus, can together equal a mild PPH , an episiotomy can cause up to 30% of postpartum blood loss. • General anaesthesia • Anaesthetic agents may cause uterine relaxation, especially inhalational agents, for example halothane.
• Mismanagement of the third stage of labour • -‘Fundus fiddling’ or manipulation of the uterus may precipitate arrhythmic contractions so that the placenta only partially separates and retraction is lost. • A full bladder • -If the bladder is full, in the abdomen on completion of the second stage may interfere with uterine action. • Etiology unknown
• • Box 18. 2 Pr e dispo sing f a ct o r s t ha t m ig ht incr e a se t he r isks o f po st pa r t um ha e m o r r ha g e • • Previous history of postpartum haemorrhage or retained placenta Presence of fibroids Maternal anaemia Ketoacidosis Multiple pregnancy HIV/AIDS Caesarean section

• • • Previous history of PPH or retained placenta -a risk of recurrence in subsequent pregnancies, depending on the cause of the PPH in the previous birth. A detailed obstetric history taken at the first antenatal visit will ensure that optimum care can be given. Fibroids (fibromyomata) These are normally benign tumors consisting of muscle and fibrous tissue, which may impede efficient uterine action.
• • Anemia Women who enter labor with reduced hemoglobin concentration (below 10 g/dl) may feel a greater e� ect of any subsequent blood loss, however small. Moderate to severe anemia (<9 g/dl) is associated with an increase in third stage blood loss and risk of postpartum hemorrhage HIV/AIDS Women who have HIV/AIDS are often in a state of severe immunosuppressant, which lowers the platelet count to such a degree so minor blood loss may cause severe morbidity or death.
• • Ketosis The influence of ketosis upon uterine action is still unclear. ketonuria at some time during labour, if labor progressed well or not , this did not appear to jeopardize either the fetal or maternal condition. -a significant relationship between ketosis: 1 - the need for oxytocin augmentation 2 - instrumental delivery 3 - PPH
• Time for occurrence of ketoacidosis when labor lasted more than 12 hours. • Correction of ketosis by ; • ensuring women have an adequate intake of fluids and light solid nourishment as tolerated throughout labor. • There is no evidence to suggest restriction of food or fluids is necessary during the normal course of labour
• Caesarean section • a lack of routine observation of vital signs in the postoperative period, or failure on the part of sta�to notice that bleeding was occurring, were key failures in care. • Postoperative observations need to be recorded regularly, using a modified early obstetric warning score (MEOWS) chart, and abnormal findings acted upon

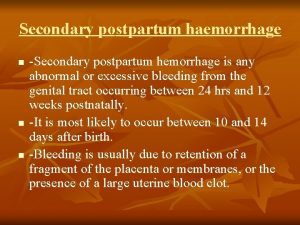
 Secondary postpartum haemorrhage
Secondary postpartum haemorrhage 4t postpartum hemorrhage
4t postpartum hemorrhage Atls classes of hemorrhagic shock
Atls classes of hemorrhagic shock Cyphalic
Cyphalic Spinelli operation
Spinelli operation Cns ischemic response
Cns ischemic response Forward and backward caries definition
Forward and backward caries definition Mount and hume classification
Mount and hume classification B lynch
B lynch Homan's sign
Homan's sign Postpartum hemorrhage treatment algorithm
Postpartum hemorrhage treatment algorithm Rubin's phases of postpartum
Rubin's phases of postpartum Vastus lateralis site for babies
Vastus lateralis site for babies Thyroiditis postpartum
Thyroiditis postpartum Lochia alba
Lochia alba Postpartum bleeding stages
Postpartum bleeding stages Lochia smell
Lochia smell Postpartum infection
Postpartum infection Postpartum stomach pain
Postpartum stomach pain Oxytoxics
Oxytoxics Postpartum prefix and suffix
Postpartum prefix and suffix Chapter 20 postpartum adaptations
Chapter 20 postpartum adaptations Postpartum hemorrhage
Postpartum hemorrhage Thyroid
Thyroid Skin manifestations of hypothyroidism
Skin manifestations of hypothyroidism Postnatal nursing diagnosis slideshare
Postnatal nursing diagnosis slideshare Postpartum infections
Postpartum infections