Complications of the Neonate Assessment Thermoregulation Nutrition Skin




- Slides: 31
Complications of the Neonate Assessment Thermoregulation Nutrition Skin care Pain Growth & Development Parental involvement
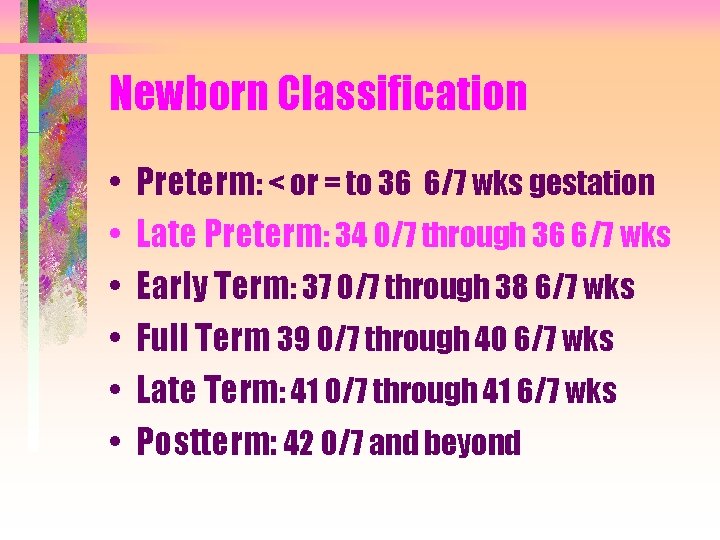
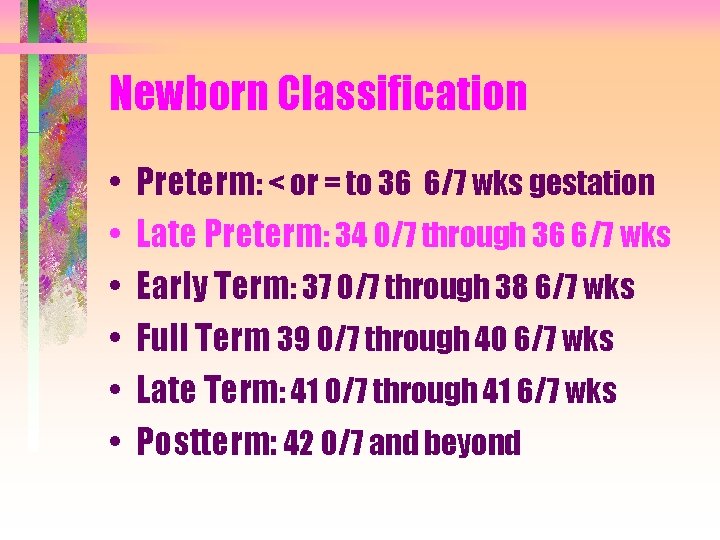
Newborn Classification • • • Preterm: < or = to 36 6/7 wks gestation Late Preterm: 34 0/7 through 36 6/7 wks Early Term: 37 0/7 through 38 6/7 wks Full Term 39 0/7 through 40 6/7 wks Late Term: 41 0/7 through 41 6/7 wks Postterm: 42 0/7 and beyond
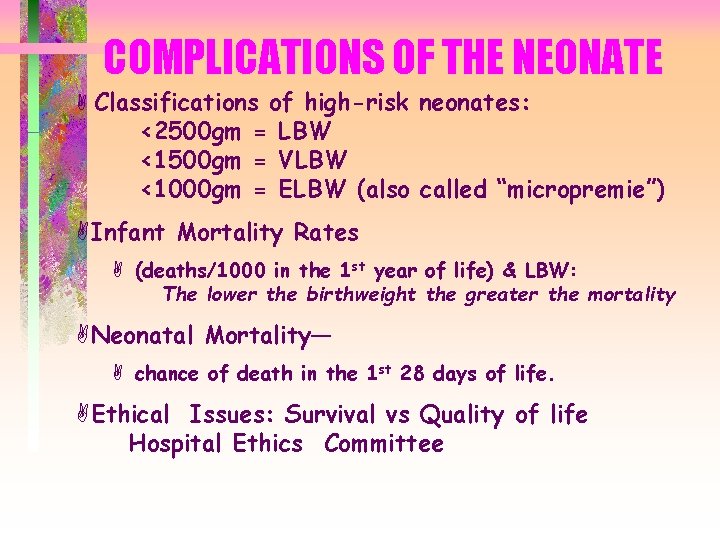
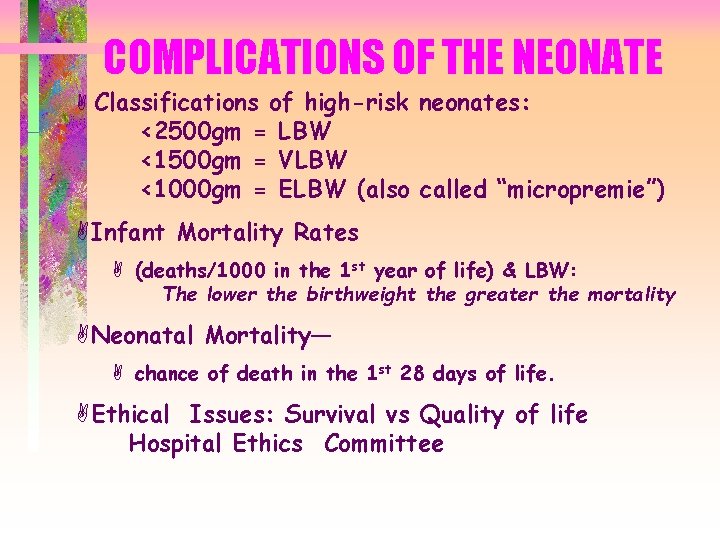
COMPLICATIONS OF THE NEONATE A Classifications of high-risk neonates: <2500 gm = LBW <1500 gm = VLBW <1000 gm = ELBW (also called “micropremie”) AInfant Mortality Rates A (deaths/1000 in the 1 st year of life) & LBW: The lower the birthweight the greater the mortality ANeonatal Mortality— A chance of death in the 1 st 28 days of life. AEthical Issues: Survival vs Quality of life Hospital Ethics Committee
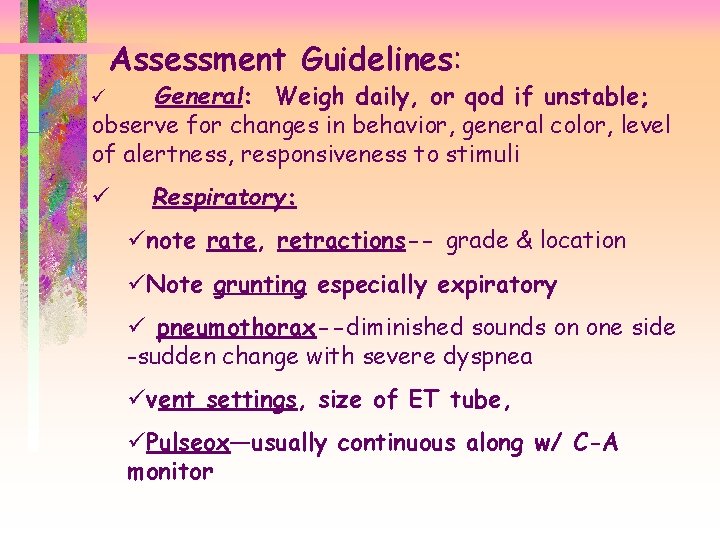
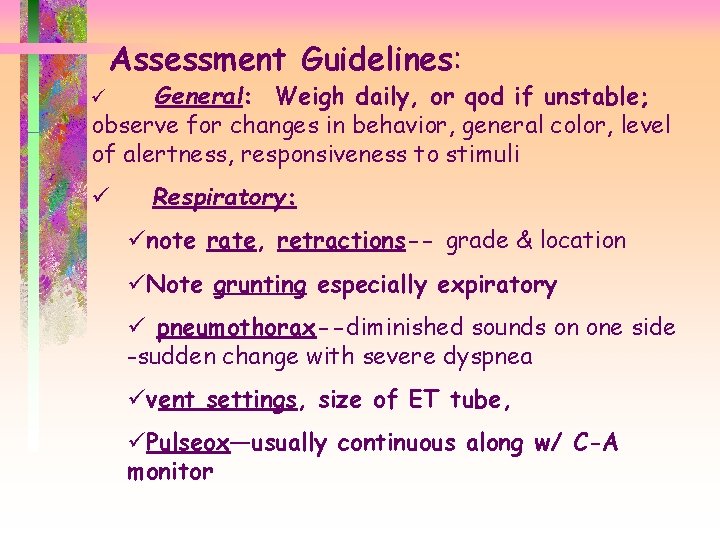
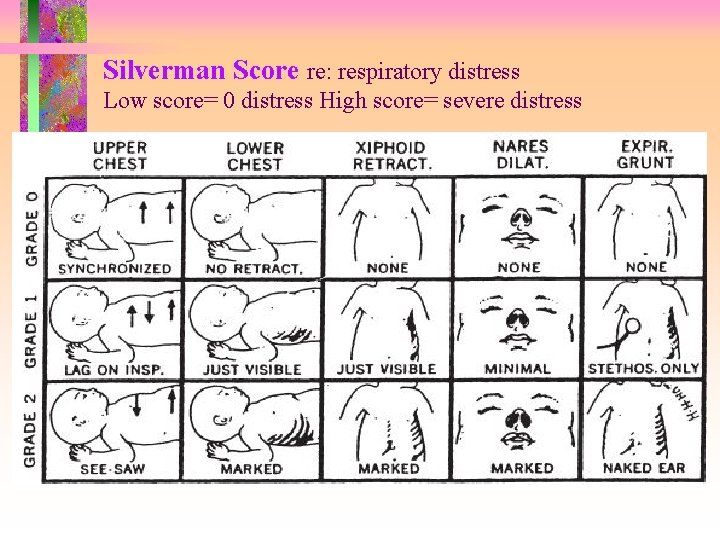
Assessment Guidelines: Guidelines General: Weigh daily, or qod if unstable; observe for changes in behavior, general color, level of alertness, responsiveness to stimuli ü ü Respiratory: ünote rate, retractions-- grade & location üNote grunting especially expiratory ü pneumothorax--diminished sounds on one side -sudden change with severe dyspnea üvent settings, size of ET tube, üPulseox—usually continuous along w/ C-A monitor
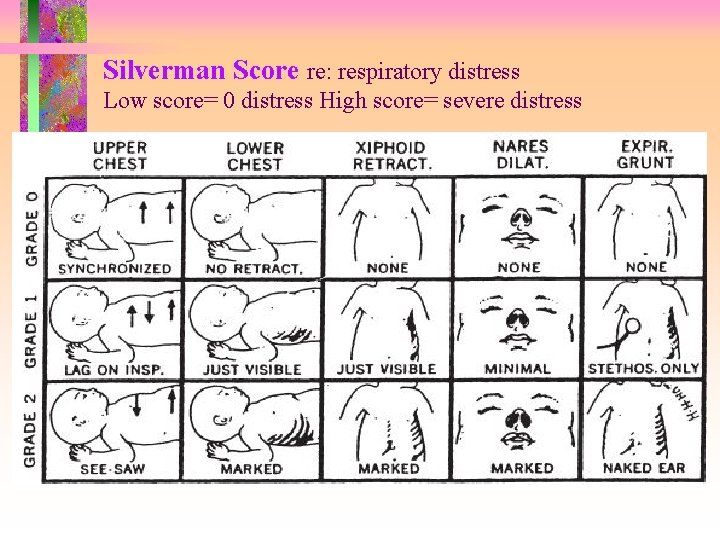
Silverman Score re: respiratory distress Low score= 0 distress High score= severe distress
Assessment Guidelines: Guidelines (continued) ü Cardiovascular: ü note murmurs--location & amplitude. ü PMI-if on wrong side may indicate diaphragmatic hernia. üAssess Peripheral pulses. üNote mottling if poor peripheral perfusion üC-A Monitors- every hour for positioning and accuracy. Change site of electrodes per protocol.
Assessment Guidelines: Guidelines ü Gastrointestinal: ü Assess Bowel Sounds ü Abd. Distention, loops of bowel seen. ü Feeding tolerance- regurge, gastric aspirate ac. Blood in stools( + hemoccult test) ü Genitourinary: 1 ml/kg/hr ü daily weight for hydration. ü Weigh diapers on gram scale for output. ü Assess for Ambiguous genitalia, preterm genitalia
Assessment Guidelines: Guidelines üNeurological: jittery-- immature CNS or hypoglycemia. Reflexes, head circumference, fontanels soft & flat üTemperature: skin temp vs air temp in isolette; weaning baby from isolette, axillary vs rectal; monitor continuously üSkin: Watch closely!!irritation from all the monitoring equipment/probes/IV’s/heel sticks; preterm “look” of skin: translucent, waxy
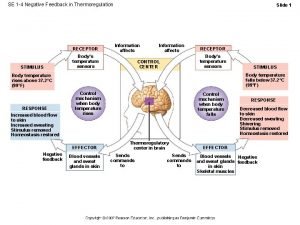
Maintaining Thermoneutrality. Essential to prevent increased stress on baby J Goal is to keep axillary temp. 36. 5 - 37. 5 C. JTypes of beds in NICU: *Radiant Warmer (Panda or Giraffe) *Double-walled isolette *Open crib
Maintaining Thermoneutrality (cont’d) J Other options: JBubblewrap Jsaran wrap JKangaroo Care-as soon as stable J Essential to watch for signs of INFECTION: Jlethargy, poor feeding JTemp or Jmost babes are on Ampicillin & Gentamycin IV prophylactically
HYDRATION ØPreterm infant is at great risk for dehydration because of large body surface area, 90% extracellular body water content, & underdeveloped kidneys ØWays to provide Hydration Parenterally: • Peripheral: hands, feet scalp, antecubital • UAC-- umbilical artery catheter • UVC -- umbilical venous catheter • PICC or PCVC -- Peripheral Intravenous Central Catheter or Percutaneous Central Venous Catheter
NUTRITION, Imbalanced: < body requirements R/T metabolic needs in the infant ðSuck reflex: appears 32 -34 weeks gestation, but cannot coordinate suck, swallow, breathe until 36 wks. ðPremies have poor muscle tone in lower esophageal sphincter so regurge a lot, which may lead to aspiration or vagal response of apnea ðPremies need calories to GROW, KEEP WARM, & to HEAL
Nutrition (cont’d) ð 110 -140 kcal/kg/day is caloric need ð TPN—used when enteral fdg is contraindicated or needs supplement ð “Minimal enteral feedings” also called priming the gut: 0. 5 cc/hr of premie formula or breastmilk per infusion pump to stimulate GI tract, even though most nutrition still given parenterally ð Breastmilk is still STRONGLY advocated with added fortifier—many NICU’s have “Exclusive Breastmilk” protocols
NUTRITION (cont’d) ØGavage feeding-(Procedure 31 -1, p. 776) ØNG interferes with nasal breathing, but OG interferes with oral intake. ØDepends on infant status & NICU protocol. ØMay be administered by gravity, or pumpintermittent or continuous ØNursing Assessments: Ø need to always aspirate and placement ac Ø non-nutritive sucking often advocated during gavage feedings to foster cognitive association of sucking with nourishment and sense of satiation.
Nutrition (cont’d) § Bottlefeeding- signs of readiness: § strong suck; § can coordinate suck, swallow, breathe; § gag reflex present; § sucking motions; § rooting & wakefulness ac and sleeping pc. § May need to do partial feeding nippled & the rest via NG/OG tube to stress on babe
Breastfeeding • Start as soon as premie – Has demonstrated coordinated suck/swallow reflex – Has consistent weight gain – Safe thermoregulation out of isolette • Contributes to maternal attachment – Pump and store for future feedings

NUTRITION –multi-disciplinary effort ØSpeech Therapists- often used to teach special exercises to foster sucking. ØNutritionists calculate daily caloric needs ØPositioning: preterm infants digest better in a PRONE position. They use less energy when prone, and have improved oxygenation.

NEONATAL SKIN CARE Preterm skin is thinner, delicate, and lacks”RETE PEGS” which anchor epidermis to dermis. Puts premies at great risk for skin tears. Limit use of adhesivie tape, bandaids. Use Stomahesive under tape. Do NOT use adhesive remover! Rather use warm water to remove sticky tape. Warm heels before heelsticks.

Skin injury r/t poor care
ACUTE PAIN IN THE PREMATURE INFANT Ô Look for symptoms of distress: * grimacing * thrashing * flaccidity * fussiness * desaturations * HR/RR increase Ô CNS is developed enough for babies to feel pain!

FOSTERING GROWTH & DEVELOPMENT ± Need to foster normal G & D by establishing some kind of daily routine for baby. ± Get nursing care done, then let baby rest. ± Infant massage may relax baby. ± Cover isolettes with blankets to create “day & night” environment ± Make recordings of parents talking, or have soft music and play in isolette if parents cannot be present
FOSTERING GROWTH & DEVELOPMENT ± Kangaroo Care- once baby is stable. Skin-to-skin contact has been proven through research to ± Sa. O 2, ± rate of weight gain, ± HR ± # of apneic episodes ± Encourage parents to put black & white mobiles around crib for visual stimulation
PARENT INFANT INTERACTION {Parents are often scared to touch the premie because of his size and apparent fragility. Fear of loss and fear of attachment are conflicting emotions all parents go through. {Parents feel overwhelmed by the amount of technical equipment being used to keep their baby alive & by the number of people it takes to coordinate his care. {The NURSE needs to serve as the parent advocate by clarifying what the doctors say on rounds, explaining the purpose behind all the diagnostic testing and equipment, and emphasizing the attributes of THEIR BABY.
PARENT INFANT INTERACTION (cont’d) { Let parents do as much of the care as is safe and they can handle. Encourage visits whenever possible. Point out personality characteristics seen in their baby! { Sibling visits are encouraged but still mostly at specific times. Siblings must have their temps taken, answer questions about exposure to communicable dzs, and wash their hands before visiting with premie.
NEONATAL LOSS • If the premature infant dies, it is important to support the family through this loss. • Photos of the baby dressed in doll clothes are routinely taken and saved on the unit if the parents are not ready to take the photos with them. • Parents are given the option of holding their baby when he is dying when all the machines have been turned off. • Nurse or chaplain may baptize baby before death.
Neonatal Loss (cont’d) • A “Memory Book” is made for the family with armbands, footprints & handprints, lock of hair, hat and booties and any other memorabilia belonging to the baby. • Referral is made to support groups for parents who have experienced such a loss.
The following are the key elements of the recommendations provided by AAP guidelines for Management of Hyperbilirubinemia. Clinicians should: • Promote and support successful breastfeeding. • Establish nursery protocols for the identification and evaluation of hyperbilirubinemia. • Measure the total serum bilirubin (TSB) or transcutaneous bilirubin (Tc. B) level on infants jaundiced in the first 24 hours.
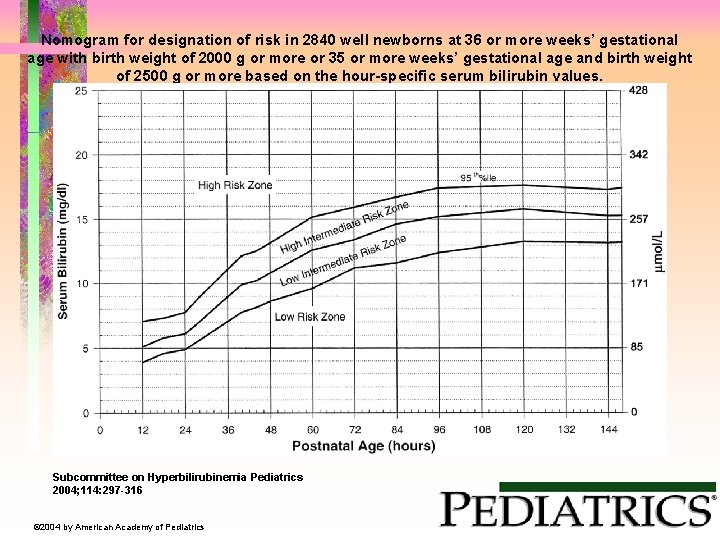
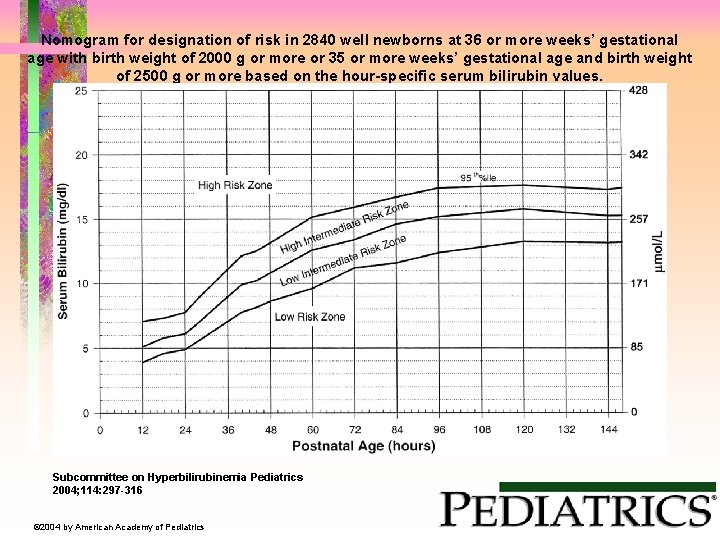
Nomogram for designation of risk in 2840 well newborns at 36 or more weeks’ gestational age with birth weight of 2000 g or more or 35 or more weeks’ gestational age and birth weight of 2500 g or more based on the hour-specific serum bilirubin values. Subcommittee on Hyperbilirubinemia Pediatrics 2004; 114: 297 -316 © 2004 by American Academy of Pediatrics
• Recognize that visual estimation of the degree of jaundice can lead to errors, particularly in darkly pigmented infants. • Interpret all bilirubin levels according to the infant’s age in hours. • Recognize that infants at less than 38 weeks’ gestation, particularly those who are breastfed, are at higher risk of developing hyperbilirubinemia and require closer surveillance and monitoring.
• Perform a systematic assessment on all infants before discharge for the risk of severe hyperbilirubinemia. • Provide parents with written and verbal information about newborn jaundice. • Provide appropriate follow-up based on the time of discharge and the risk assessment. • Treat newborns, when indicated, with phototherapy or exchange transfusion. http: //pediatrics. aappublications. org/content/114/1/297. full
That’s It!! • Be sure to review all the pathophysiology discussed in the Complications of the Neonate: DISEASES in your course calendar re: • • • RDS Hypoglycemia Hyperbilirubinemia Complications as NEC, ROP Meconium Aspiration Syndrome
 Grimace reflex
Grimace reflex Definition of high risk neonate
Definition of high risk neonate Petechiae neonate
Petechiae neonate Priformus
Priformus Countercurrent exchange thermoregulation
Countercurrent exchange thermoregulation Thermorégulation ifsi
Thermorégulation ifsi Thermoregulation
Thermoregulation Thermoregulation
Thermoregulation Thermoregulation
Thermoregulation Thermoregulation
Thermoregulation Febris inversa
Febris inversa Thermogénèse
Thermogénèse Thermoregulation
Thermoregulation Specific heat simulation
Specific heat simulation Thermoregulation mechanism
Thermoregulation mechanism Thick skin and thin skin
Thick skin and thin skin Thin skin vs thick skin
Thin skin vs thick skin Milady chapter 23 pdf
Milady chapter 23 pdf Chapter 7 skin structure growth and nutrition
Chapter 7 skin structure growth and nutrition Skin assessment documentation
Skin assessment documentation Skin integrity assessment
Skin integrity assessment Skin integrity assessment
Skin integrity assessment Skin assessment nursing
Skin assessment nursing Nails assessment
Nails assessment Four eyes skin assessment
Four eyes skin assessment Skin assessment
Skin assessment Purpose of skin assessment
Purpose of skin assessment Community nutrition assessment
Community nutrition assessment Abcd in nutrition assessment
Abcd in nutrition assessment Capillary refill
Capillary refill Focused gi assessment
Focused gi assessment Levothyroxine side effects
Levothyroxine side effects