UCSD SKIN ASSESSMENT DOCUMENTATION Cheryl Garnica RN CWOCN



























- Slides: 50
UCSD SKIN ASSESSMENT & DOCUMENTATION Cheryl Garnica RN, CWOCN Spring 2011
SKIN TRENDS AND REGULATION CHANGES 2007: Changes by CMS for payment of HAPUs NUAP new definitions for pressure ulcers Addition of Pressure Ulcer Stages: Unstageable and Deep Tissue Injury 2009: Clarification of MMPs (mucous membrane pressure ulcers: do not fit in staging guidelines Best practice/evidence based guidelines published by NPUAP and EPUAP
REGULATION & REPORTING CHANGES POA defined (Present on Admit) Medicare payment changes: Stage III , Stage IV, Deep Tissue injuries and unstageable HAPUs: Possibly no $$monetary compensation CDPH: MUST be notified within 5 days of finding HAPPU Stage III, IV, Unstageable and DTI present on admit that converts to unstageable eschar
Who Stages Pressure Ulcers? ? ANA position Statement 2010: Nurses!! BUT: you must be able to differentiate between pressure ulcers and other types of wounds Physicians
RESOURCES FOR SKIN CARE AT UCSD Skin Team Champion CNS/Clinical Nurse Educator WOCN MD Wound Manual Skin Standards on Web Ref Cal Noc Tutorial: User ID: tuto 620 Password: tuto 634 www. nursingquality. org PU learning modules
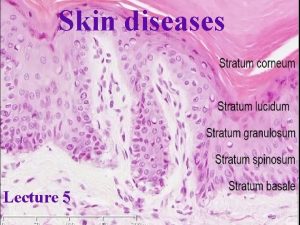
Skin Facts Largest organ Often reflects patient’s general condition First line of defense against moisture, pathogens Thermoregulation Sensory Metabolism (Vit. D) Communication

Changes with aging Less fat, collagen: decreased elasticity Decreased sensation Decreased thermoregulation Decreased ability to fend off pathogens

Factors that alter skin integrity Nutrition Age Disease State Hydration Medications Sensory Impairment Mental Impairment Immobility Incontinence Circulation

SKIN: NURSES RESPONSIBILITY Promote and maintain skin integrity Assess and Identify risk factors: for skin impairment Implement Interventions: to prevent skin breakdown Document: findings & interventions Communicate: to physicians and staff Educate: family re: Breakdown prevention and treatment
Skin Assessment: Frequency On admit, within first hour Every shift Transfer to unit Change in condition or level of care Post procedure Reassessment: every position change

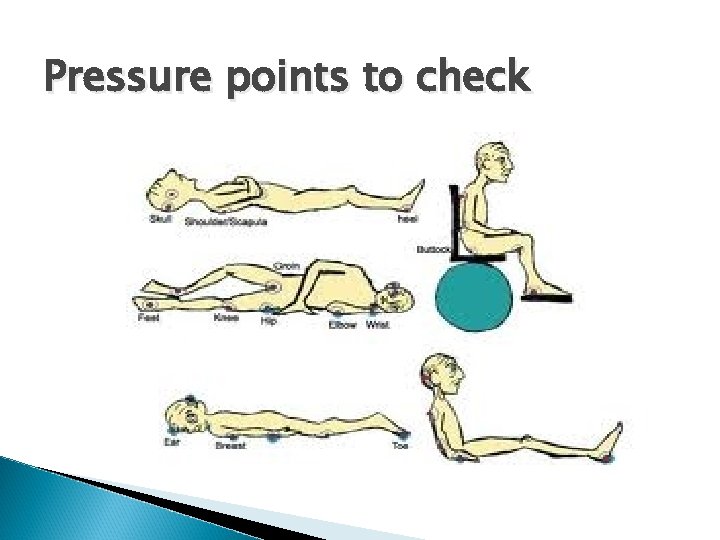
Methods of Skin Inspection Visual and Touch Head to toe inspection Particular attention to boney prominences: occiput, spine, shoulder blades, elbows, sacrum, coccyx, heels, trochanters, Maleolus, ischeum In skin folds (especially with Bariatric patients) Check under medical devices
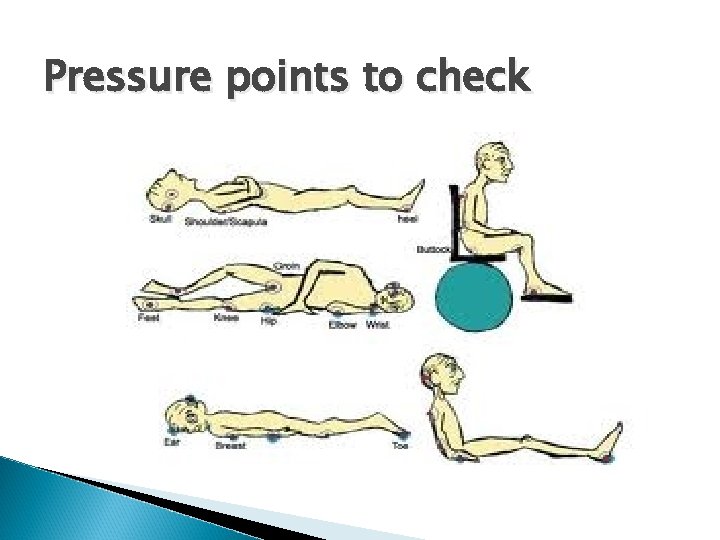
Pressure points to check

What to assess? ? Color: blanchable, pale, redness; dark skin may require flashlight for assessing at risk pressure areas Intact or not? Turgor (resilience, hydration) Temperature: warm, cold Moisture: incontinent, sweating, dry, flakey Texture: hard, soft, boggy, mushy, induration, blistering Existing skin issues: wounds, rashes, bruises, skin tears, ecchymosis
BRADEN SCALE Identifies Risk Factors Contributing to Skin Breakdown Sensory Moisture Activity Mobility Nutrition Friction and Shear 18 or less: MUST HAVE CARE PLAN

BRADEN SCALE: Completed every shift and on change in condition or level of care Low scores on Braden subscale: should drive your care plan and interventions for skin care

FINDINGS ON ASSESSMENT Skin alterations, open wounds: Identify source (pressure, skin tear, shear, abrasion, surgical wound, venous or arterial ulcers, trauma, etc. Get a history from the patient Describe what you see
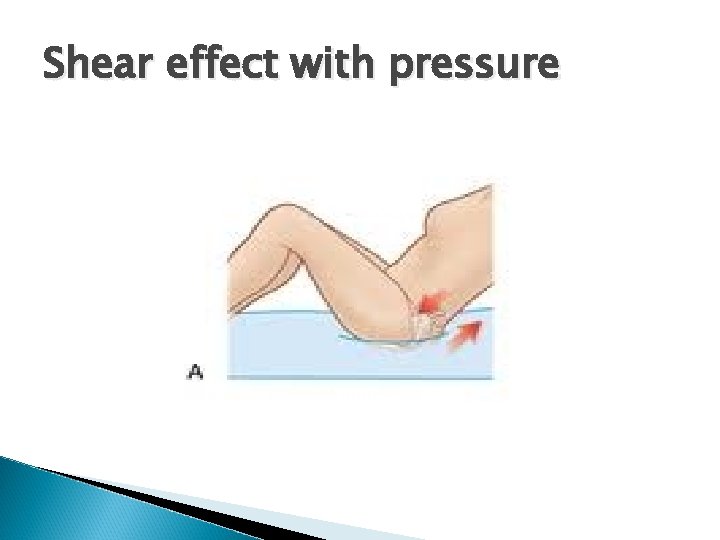
Is it a pressure ulcer? Definition: Damage caused to skin and underlying soft tissue by unrelieved pressure when the tissue is compressed between a bony prominence and external surface over a prolonged period of time 3 main contributing factors in formation: Pressure, Shear and Friction Most pressure ulcers are over a bony prominence, however, they may be present over soft tissues. Keypoint: assess over bony areas AND under medical devices (SCDs, oxygen prongs and tubings, foleys, drains, objects left in bed, etc. )
STAGE I Intact skin with non-blancheable redness of a localized area usually over a boney prominence. Darkly pigmented skin may not have visible blanching; its color may differentiate from the surrounding area. Keypoint: dark skin individuals: inspect skin for warmth, coolness, induration (firm, hard) or boggy areas. May be painful.

Stage I

Stage II Partial thickness loss of dermis which may present as a shallow crater, NO SLOUGH (yellow dead tissue). May also present as a serum filled blister (intact or ruptured). Keypoint: dermal depth, all pink, shallow; do not use Stage II to define skin tears

Stage II
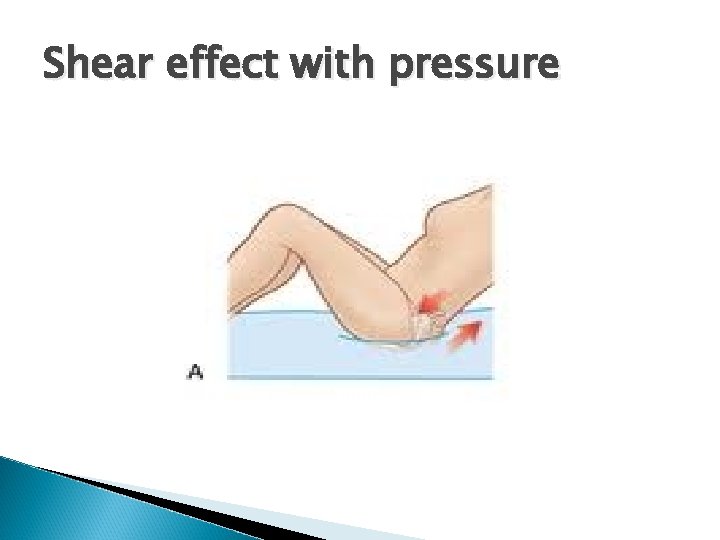
Shear effect with pressure


Stage III Full thickness tissue loss. Subcutaneous fat may be visible. Bone, tendon or muscle NOT exposed. Slough may be present, but does NOT obscure the depth of tissue loss. May include undermining and tunneling. Keypoint: amount of subcutaneous tissue varies per anatomical area and per individual. Thin folks: little subcutaneous tissue whereas morbidly obese may have excess

Stage III

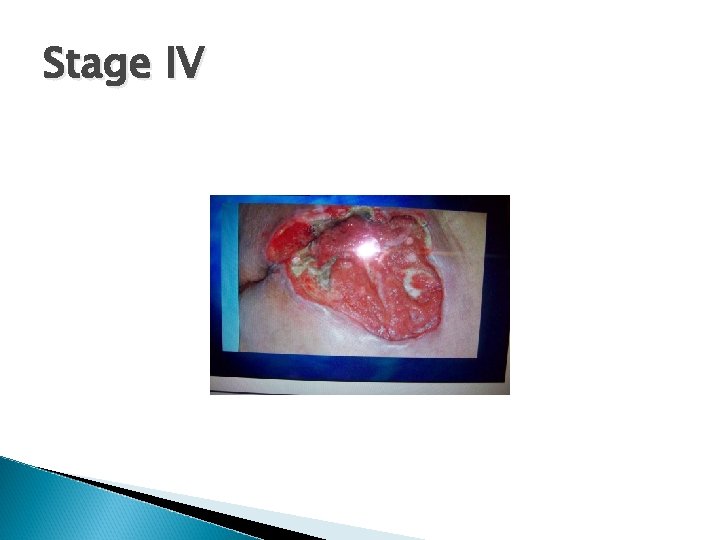
Stage IV Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present on some parts of the wound bed. Often include undermining and tunneling. Keypoint: Depth of tissue loss varies per anatomical location. Bridge of nose, ear, occiput and malleolus have little or no subcutaneous tissue; these Stage IV ulcers CAN BE SHALLOW
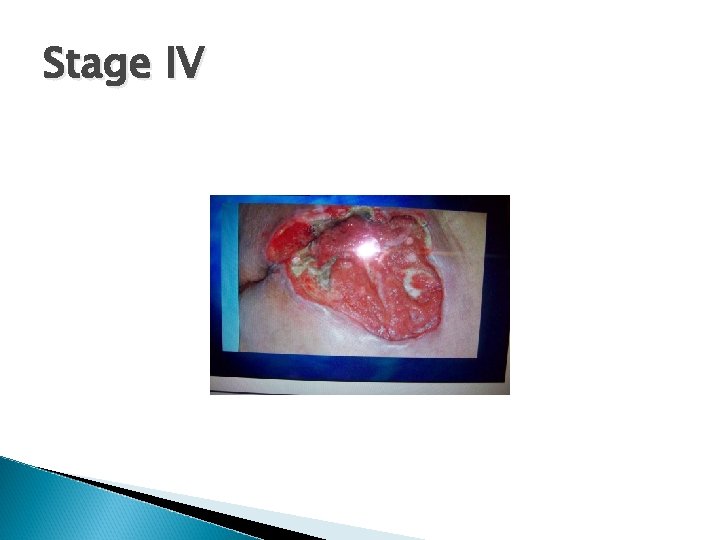
Stage IV
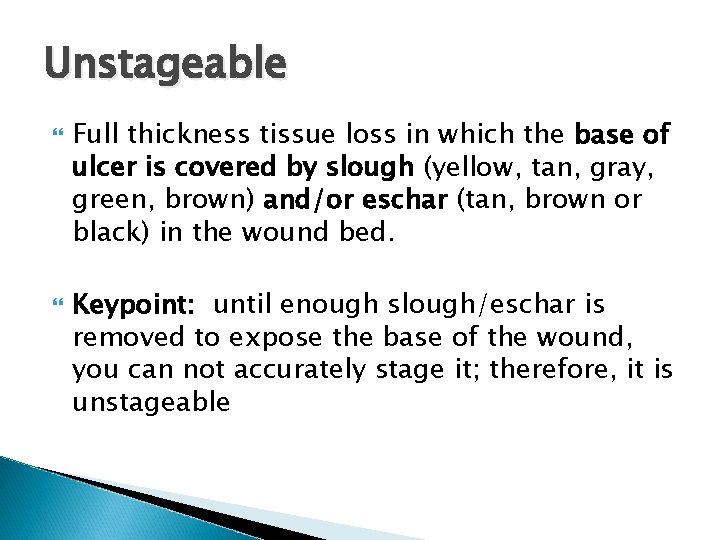
Unstageable Full thickness tissue loss in which the base of ulcer is covered by slough (yellow, tan, gray, green, brown) and/or eschar (tan, brown or black) in the wound bed. Keypoint: until enough slough/eschar is removed to expose the base of the wound, you can not accurately stage it; therefore, it is unstageable

Unstageable
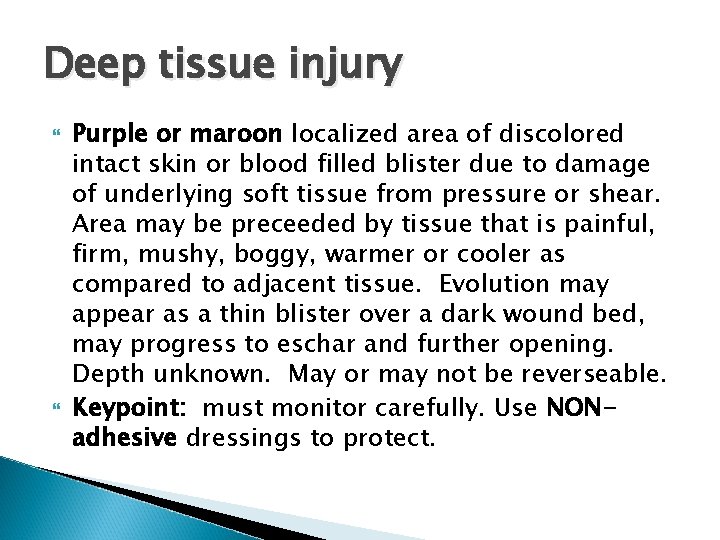
Deep tissue injury Purple or maroon localized area of discolored intact skin or blood filled blister due to damage of underlying soft tissue from pressure or shear. Area may be preceeded by tissue that is painful, firm, mushy, boggy, warmer or cooler as compared to adjacent tissue. Evolution may appear as a thin blister over a dark wound bed, may progress to eschar and further opening. Depth unknown. May or may not be reverseable. Keypoint: must monitor carefully. Use NONadhesive dressings to protect.

Deep Tissue Injury

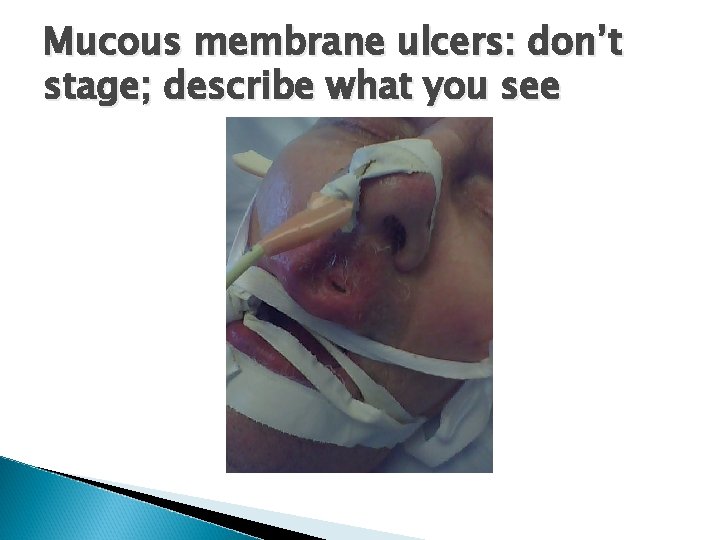
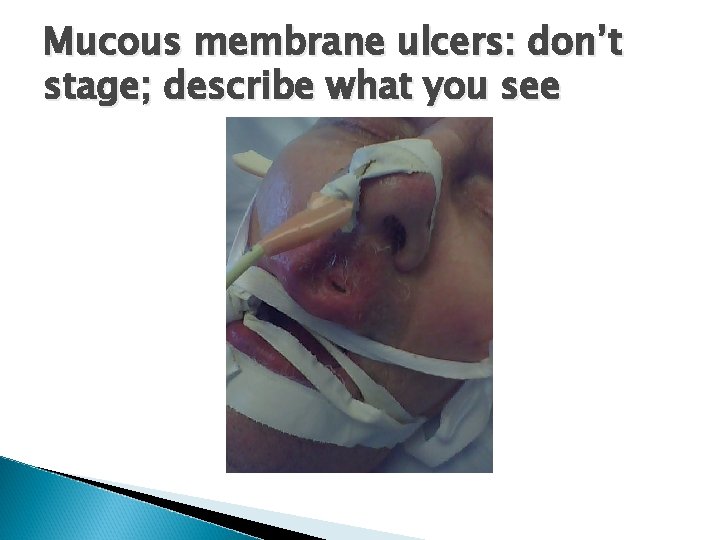
Mucous membrane ulcers: don’t stage; describe what you see

Intertrigo An inflammatory condition of the skin with our without skin loss in skin folds induced or aggravated by mechanical friction, maceration, moisture, heat. May have bacterial or fungal component. Often found in skin folds, axilla, gluteal fold, perineal area, abdominal panus, under heavy breasts. Morbidly obese high risk in skin folds.


Intertrigo with fungal infection

DOCUMENTATION PADB: Chronic skin issues? ? ? YES!! Further elaboration should be in note and on skin assessment Basic skin condition: moist, dry, flakey, skin turgor, ecchymotic, paper thin skin If wounds found on admit, ASK the pt. how, where, when acquired and DOCUMENT
DOCUMENTATION: WOUND CHARACTERISTICS MUST include: location, type of wound, color or general appearance of wound base (pink, red, slough, eschar, etc. ) Describe surrounding skin (intact, macerated, red, hard, moist, etc) Measurements: on finding wound and weekly Drainage (amount, character, color, odor or lack of odor) PAIN!! Presence or absence
DOCUMENT YOUR INTERVENTIONS ◦ Treatment done or condition of dressing if not changed ◦ Who notified ◦ Pain level/analgesia offered or given/response ◦ Pressure Ulcer prevention interventions/consults (WOCN, PT, OT, nutrition, turning, pressure offloading, specialty boots, specialty mattresses, Geomatt) ◦ Document education done with patient and family

CARE PLAN Patient/individual specific (difficult with EPIC) Measureable outcomes/Realistic Interventions: specific for patient vs. canned responses Special attention to Braden Scale using subscales with low scores : address in care plan interventions Document who was notified if unusual findings EVALUATE: is the treatment working? ? If not, what should you change? Address!
Current Treatment Specific Standards you can implement NOW Incontinence: Baby wipes, skin cleanser, skin barriers, moisturize with lotion, fecal pouches Offload pressure: Prevalon boots, pillows for bridging and turning, turning schedule, Geomatt cushion for sitting Resource utilization: WOCN, MD, CNS/Educator, Skin Champion

Nursing Interventions: No orders required: Stage I Options: open to air, dry dressings, Tegaderm, Allevyn, Alleyn Non-adhesive, skin prep Stage II: Allevyn, Allevyn non-adhesive, Tegaderm, use of Solosite Gel if wound bed dry in addition to cover dressing Deep. Tissue Injuries: Open to air (dry, non blistered); Allevyn NON-adhesive if blistered or thin skin coating and at risk with adhesives, Elastogel
Skin Tears: Superficial Xeroform or Vaseline gauze/Kerlix. AVOID adhesives. Change every 1 -2 days depending on drainage. Deeper tears or flap tears: extensive tissue damage and need MD or WOCN consult
Wound Wednesdays Wounds that have dressing orders should be measured, photographed and documented weekly; Wednesdays preferred. Fill out EPIC wound documentation, upload photo. You may document below photo or in care plan notes. Notify MD of findings, can click “cosign” to alert to photo
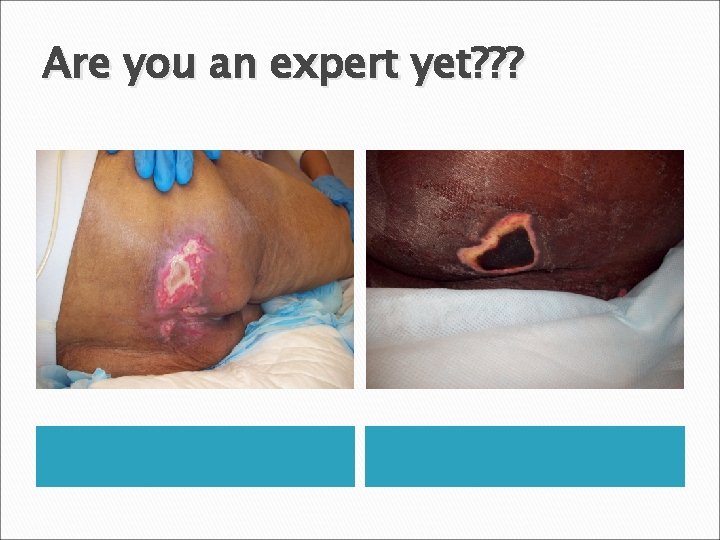
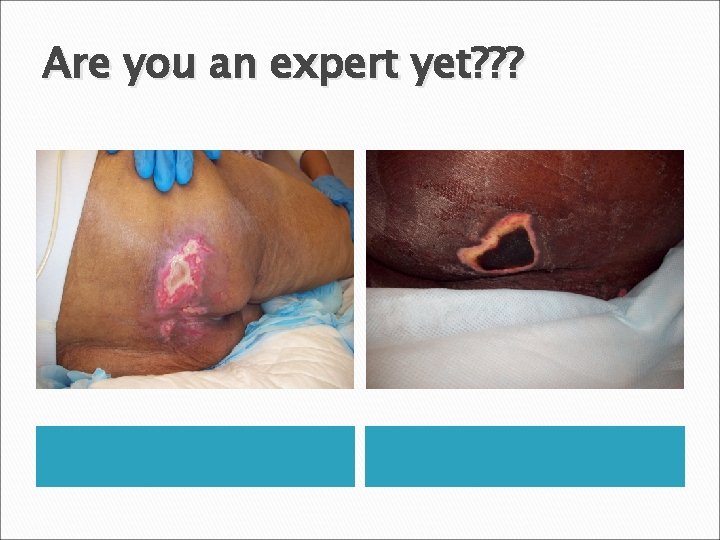
Are you an expert yet? ? ?




THE END!!
 Skin turgor assessment charting
Skin turgor assessment charting Skin is the largest organ
Skin is the largest organ Thin skin vs thick skin
Thin skin vs thick skin Milady chapter 23 pdf
Milady chapter 23 pdf Precordum
Precordum Tactile fremitus pleural effusion
Tactile fremitus pleural effusion Cheryl bendtsen
Cheryl bendtsen Cheryl wold
Cheryl wold Cheryl goddard
Cheryl goddard Wcet san
Wcet san Cheryl schaub
Cheryl schaub Cheryl gta 5
Cheryl gta 5 Cheryl kiser
Cheryl kiser Cheryl heinz
Cheryl heinz Dr cheryl fitzgerald
Dr cheryl fitzgerald Cheryl marcum
Cheryl marcum Cheryl dileo
Cheryl dileo Cheryl roldan
Cheryl roldan Dr cheryl flynn
Dr cheryl flynn Cheryl hinds
Cheryl hinds Dr cheryl holder
Dr cheryl holder Cheryl ann peters
Cheryl ann peters Cheryl schaub
Cheryl schaub Denny learner
Denny learner Production techniques
Production techniques Cheryl waterhouse
Cheryl waterhouse Nysana
Nysana Brown and levinson 1987
Brown and levinson 1987 Unengaged parenting
Unengaged parenting Cheryl carner
Cheryl carner Cheryl cole malaria
Cheryl cole malaria Cheryl goddard
Cheryl goddard Cheryl dunham
Cheryl dunham Cheryl weiss
Cheryl weiss Skin integrity assessment
Skin integrity assessment Skin integrity assessment
Skin integrity assessment Skin assessment nursing
Skin assessment nursing Hair distribution assessment
Hair distribution assessment 4 eyes skin assessment tool
4 eyes skin assessment tool Skin assessment
Skin assessment Purpose of skin assessment
Purpose of skin assessment Porfolio assessment
Porfolio assessment Define dynamic assessment
Define dynamic assessment Portfolio assessment matches assessment to teaching
Portfolio assessment matches assessment to teaching Ucsd library
Ucsd library Phys courses ucsd
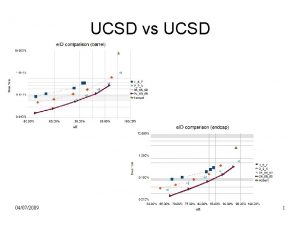
Phys courses ucsd Ucsd vac
Ucsd vac Ece 191 ucsd
Ece 191 ucsd Uc campus link
Uc campus link Avi yagil
Avi yagil Tom murphy ucsd
Tom murphy ucsd