Fertility issues for patients with lymphoma Cheryl Fitzgerald









- Slides: 34
Fertility issues for patients with lymphoma Cheryl Fitzgerald Dept of Reproductive Medicine St Mary’s Hospital Manchester

Issues to consider • Two diagnoses – Malignancy and infertility – Counselling • Delay in conception – Marked decline in female fertility 35 onwards • Effect of disease/treatment – Spermatogenesis – Ovary – oocytes – Uterus – radiotherapy induced damage
Issues affecting fertility • • • Delay in conception – female Disease Surgery Chemotherapy Radiotherapy Long term prognosis – Welfare of Child
• Male • Female • Options - easy • Options complex
Men • • Men and postpubertal boys Need to screen for Hep B, Hep C and HIV Urgent direct referral Phone Andrology SMH – 276 6473 Produce single (? more) sample Frozen in several ampoules Stored for up to 55 years Sperm used for insemination or IVF

Options for treatment with cryopreserved sperm • Sperm quality good – use for insemination • Sperm quality poor – use for IVF • Treatment within NHS dependent upon NHS assisted conception guidelines • Sperm can be transferred to private sector is not eligible

Delay in conception - females Initial treatment Long term therapy (breast) Time until “cure” • • Age related decline in female fecundity Age related decline in ovarian reserve Increase in oocyte aneuploidy Marked reduction 35 onwards
Effects of chemotherapy • Damage to primordial follicles • Damage to primary follicles • Oogenesis – many months • May be temporary disruption • No benefit from Gn. RH agonist treatment • No effect on uterus
Risk factors for iatrogenic POF • Older women – poor ovarian reserve • Dose, type and duration of chemotherapy • Pelvic radiotherapy / TBI

Effects of radiotherapy • Site specific • Pelvic radiotherapy / TBI – profound oocyte damage – profound uterine damage • Oocyte damage – Premature ovarian failure • Uterine damage – Poor implantation rates after XRT – Poor pregnancy outcome after XRT

Fertility preservation options – pre-treatment • Cryoprserve ovarian tissue • Cryopreserve oocytes • Cryopreserve embryos • Consider uterine function
Ovarian cryopreservation • • Laparoscopic oophorectomy Ovarian cortex frozen in strips Later – replace ovarian tissue within pelvis Spontaneous/stimulated ovarian cycle ? ? In vitro maturation in the future 10 (+2) babies worldwide No time limit on storage
Ovarian storage • Risks • Very low success rates • Risk of laparoscopy • Risk of re-introducing disease • Benefits • No need for hyperstimulation • No raised oestradiol level • No need for partner • Minimal delay in treatment

Who is suitable? Lymphoma patients Very young girls ? ? Prepubertal No metastatic disease in ovaries Limited time
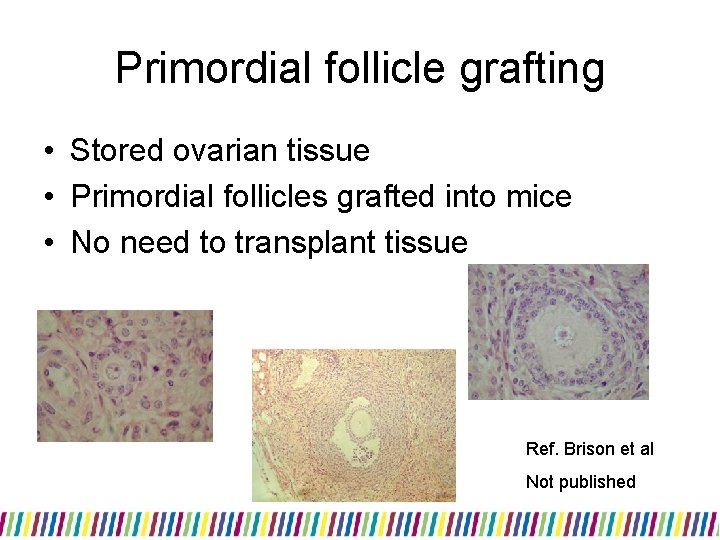
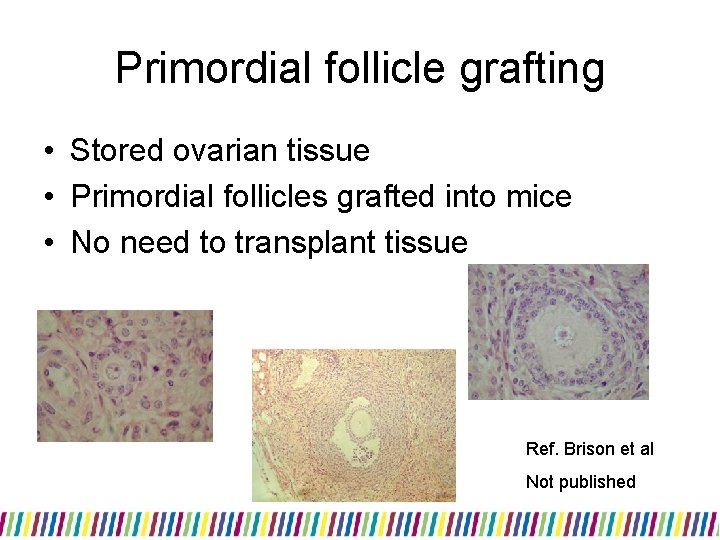
Primordial follicle grafting • Stored ovarian tissue • Primordial follicles grafted into mice • No need to transplant tissue Ref. Brison et al Not published
Egg and embryo freezing • Need to retrieve mature eggs from ovaries • No stimulation – single egg – poor success • Need for ovarian hyperstimulation
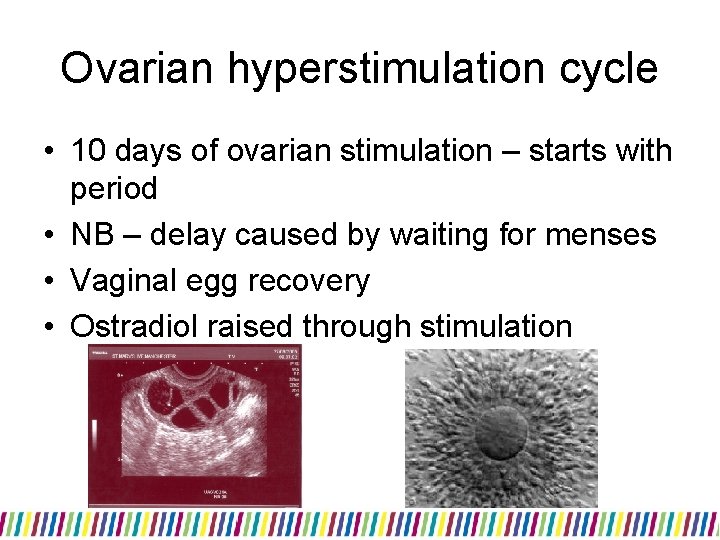
Ovarian hyperstimulation cycle • 10 days of ovarian stimulation – starts with period • NB – delay caused by waiting for menses • Vaginal egg recovery • Ostradiol raised through stimulation
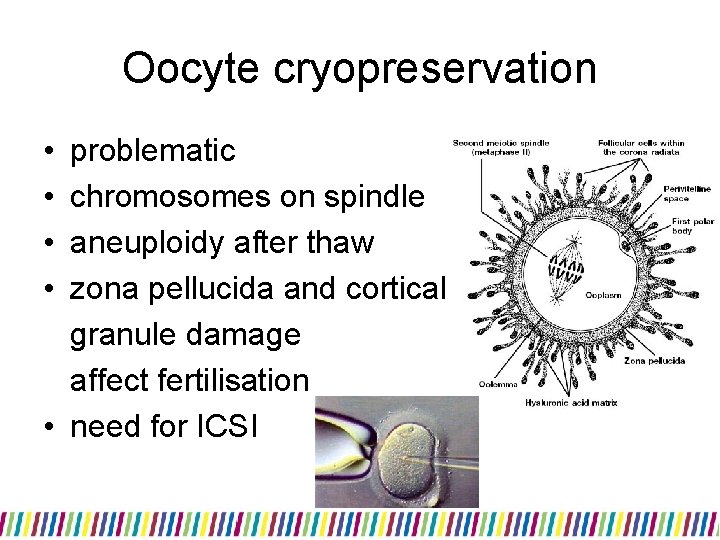
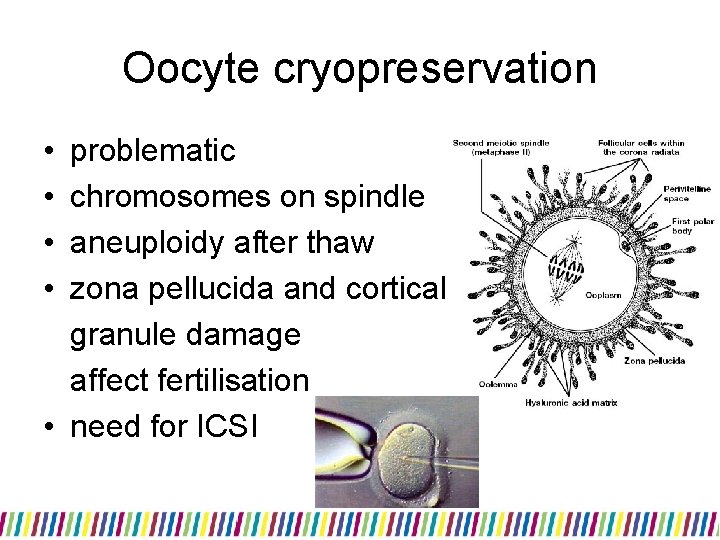
Oocyte cryopreservation • • problematic chromosomes on spindle aneuploidy after thaw zona pellucida and cortical granule damage affect fertilisation • need for ICSI
Oocyte cryopreservation • Freeze all mature eggs recovered • Can be stored for 55 years – HFEA Code of Practice 8 • No reduction in “quality” of eggs with increasing time

Oocyte cryopreservation - progress • Improving ++ vitrification • Rapid cooling without crystal formation • Survival • Fertilisation • Pregnancy Vitrification Slow freeze 80% 75% 9% 60% 65% 4%
Safety of egg freezing • 936 babies • Birth anomalies – 1. 3% • No difference compared to spontaneously conceived children • Noyes et al 2009

Embryo cryopreservation • • need a partner “urgent” IVF minimum time 4 -6 weeks ovarian hyperstimulation oocyte recovery eggs inseminated embryos created frozen
Risks associated with “urgent” IVF for egg or embryo cryopreservation • high circulating oestradiol (20 000 cf 500 pmol/l) – issue with Ca breast • potential seeding of gynae malignancies • delay in cancer treatment
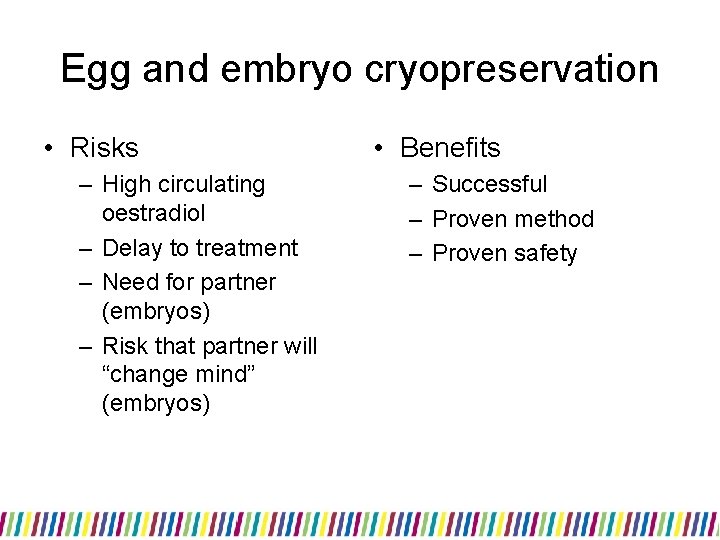
Egg and embryo cryopreservation • Risks – High circulating oestradiol – Delay to treatment – Need for partner (embryos) – Risk that partner will “change mind” (embryos) • Benefits – Successful – Proven method – Proven safety

Chance of baby – embryo freeze • • HFEA data – livebirth per fresh cycle 2008 <35 years 32. 8% 35 -37 years 27. 3% 38 -39 years 19. 0% 40 -42 years 11. 8% 43 -44 years 4. 8% >44 years 3. 8% 30% embryo loss with freezing
Embryo freezing • Freeze all embryos created at pronucleate stage • Can be stored for 55 years • No reduction in “quality” of embryos with increased time in storage
Practicalities • Urgency – referral early • Fax referral and confirm by phone • Cycle control – COCP – limits delay • Details – Timing of chemo – Need for pelvic radiotherapy – Longterm therapies – Prognosis
After treatment • Referred as any infertility patient
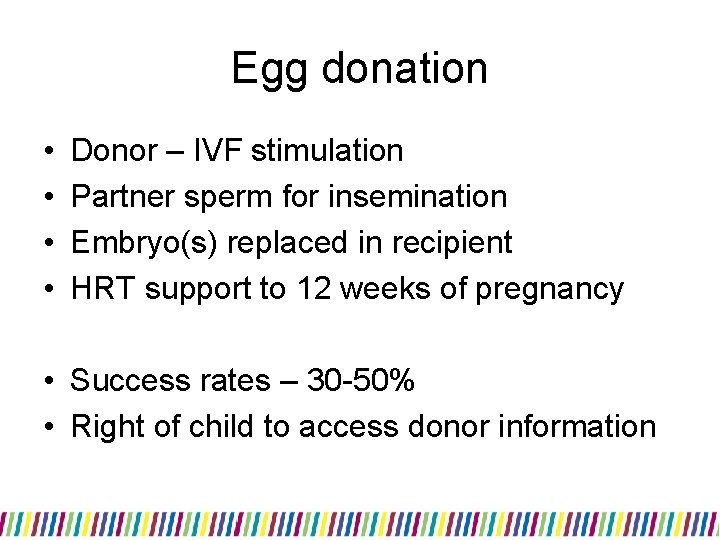
Egg donation • • Donor – IVF stimulation Partner sperm for insemination Embryo(s) replaced in recipient HRT support to 12 weeks of pregnancy • Success rates – 30 -50% • Right of child to access donor information
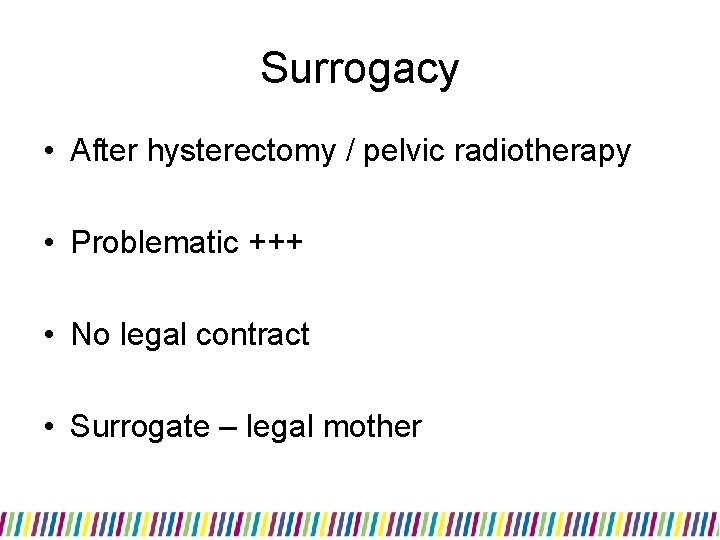
Surrogacy • After hysterectomy / pelvic radiotherapy • Problematic +++ • No legal contract • Surrogate – legal mother
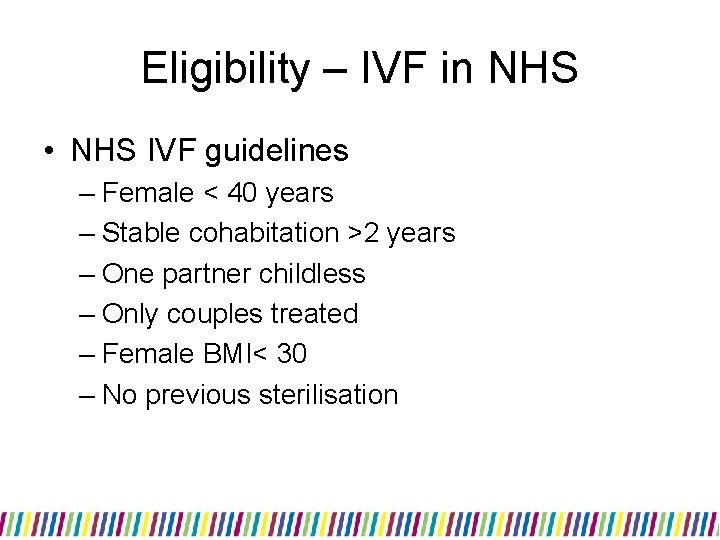
Eligibility – IVF in NHS • NHS IVF guidelines – Female < 40 years – Stable cohabitation >2 years – One partner childless – Only couples treated – Female BMI< 30 – No previous sterilisation
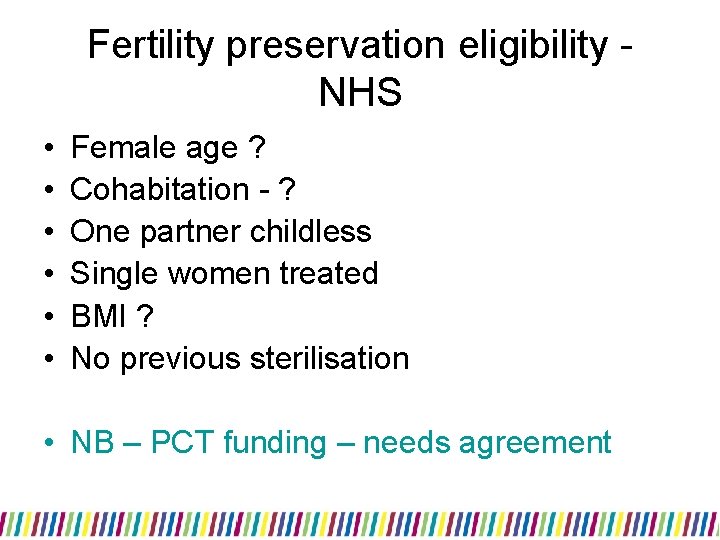
Fertility preservation eligibility NHS • • • Female age ? Cohabitation - ? One partner childless Single women treated BMI ? No previous sterilisation • NB – PCT funding – needs agreement
Welfare of the Child • Legal requirement • HFEA Act • Prognosis for patient important • Partner / family support
Thank-you
 Dr cheryl fitzgerald
Dr cheryl fitzgerald Ethical issues in treating lgbt patients
Ethical issues in treating lgbt patients Burkitt lymphoma
Burkitt lymphoma Difference between hodgkin and non hodgkin lymphoma
Difference between hodgkin and non hodgkin lymphoma Pancreazin
Pancreazin Crab criteria multiple myeloma
Crab criteria multiple myeloma Non-hodgkin lymphoma
Non-hodgkin lymphoma Chylothorax
Chylothorax Hodgkin's lymphoma
Hodgkin's lymphoma Difference hodgkin and non hodgkin lymphoma
Difference hodgkin and non hodgkin lymphoma Hodjkins disease
Hodjkins disease Hodgkin's lymphoma clinical presentation
Hodgkin's lymphoma clinical presentation Cerebriform nuclei
Cerebriform nuclei Bcell lymphoma
Bcell lymphoma Lymphoma case presentation
Lymphoma case presentation Copanlisib package insert
Copanlisib package insert Splenicus
Splenicus What does lymphoma lump look like
What does lymphoma lump look like Burkitt lymphoma
Burkitt lymphoma Burkitt lymphoma cytology
Burkitt lymphoma cytology Lymphoma
Lymphoma Aspiration biopsy
Aspiration biopsy Maintenance rituximab mantle cell lymphoma
Maintenance rituximab mantle cell lymphoma Burkitt lymphoma
Burkitt lymphoma Classification of hodgkin lymphoma
Classification of hodgkin lymphoma Nhl classification
Nhl classification Ann arbour staging system
Ann arbour staging system Szóbajön
Szóbajön Luis fayad
Luis fayad Lymphoma vs leukemia
Lymphoma vs leukemia Hepatosplenic t-cell lymphoma
Hepatosplenic t-cell lymphoma Indolent non-hodgkin lymphoma quizlet
Indolent non-hodgkin lymphoma quizlet Cheryl boyce nih
Cheryl boyce nih Cheryl flynn md
Cheryl flynn md Cheryl ann peters
Cheryl ann peters