Common Respiratory Diseases and Oxygen Delivery The respiratory




- Slides: 32
Common Respiratory Diseases and Oxygen Delivery
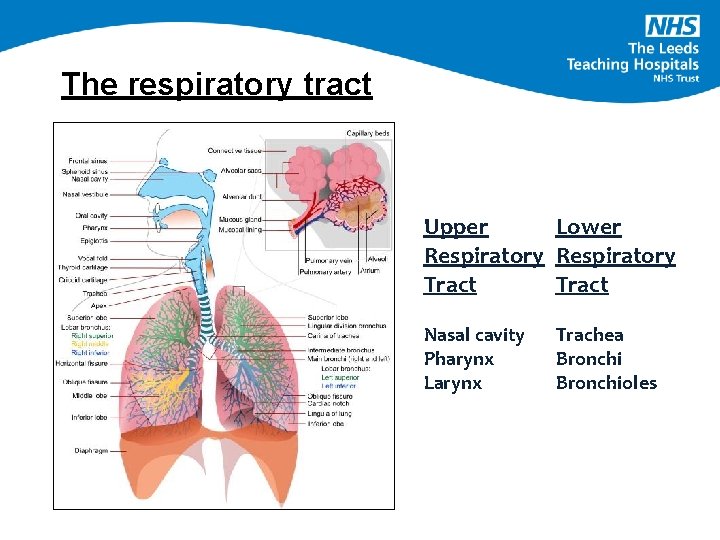
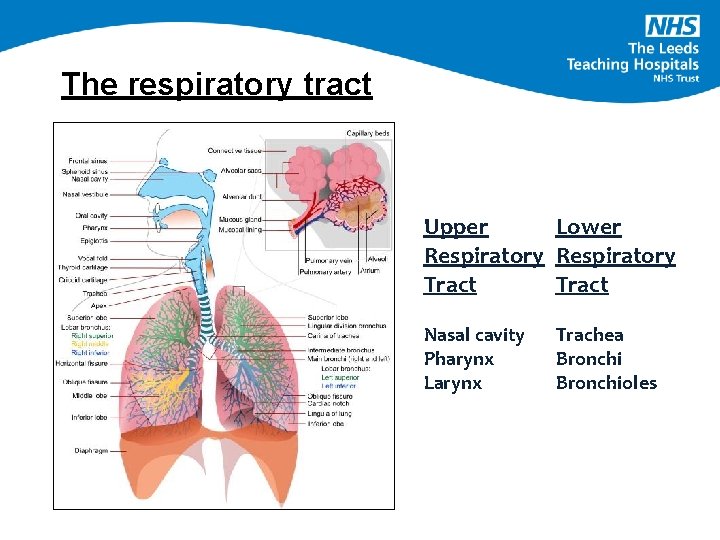
The respiratory tract Upper Lower Respiratory Tract Nasal cavity Pharynx Larynx Trachea Bronchioles
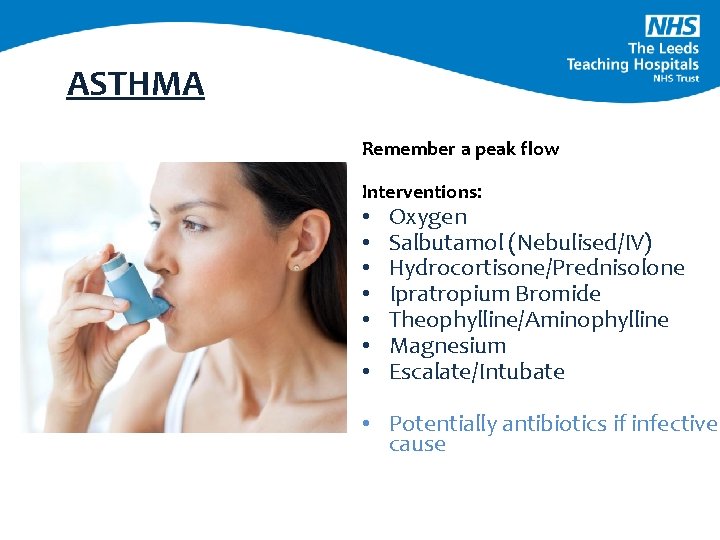
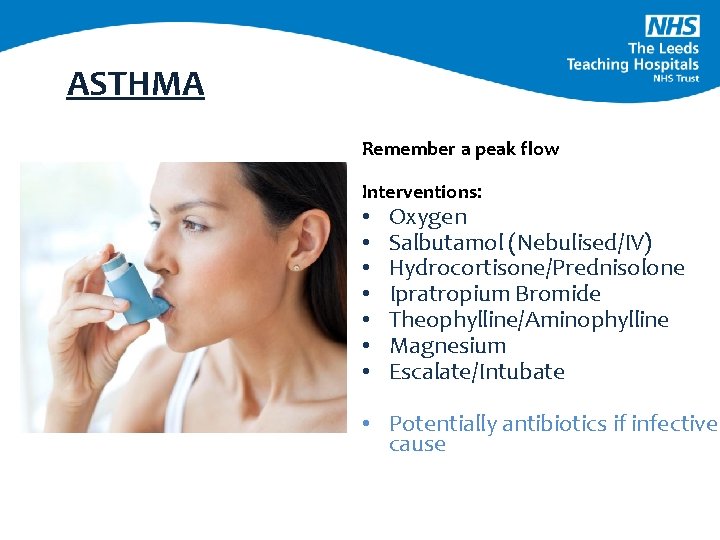
ASTHMA Remember a peak flow Interventions: • • Oxygen Salbutamol (Nebulised/IV) Hydrocortisone/Prednisolone Ipratropium Bromide Theophylline/Aminophylline Magnesium Escalate/Intubate • Potentially antibiotics if infective cause


If you’re worried or want more information re asthma during this time look at Asthma UK website https: //www. asthma. org. uk/advice/triggers/coronavirus-covid-19/
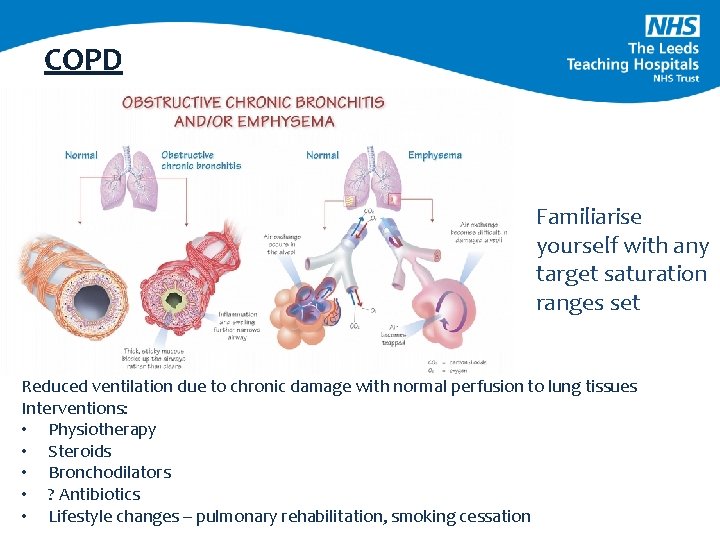
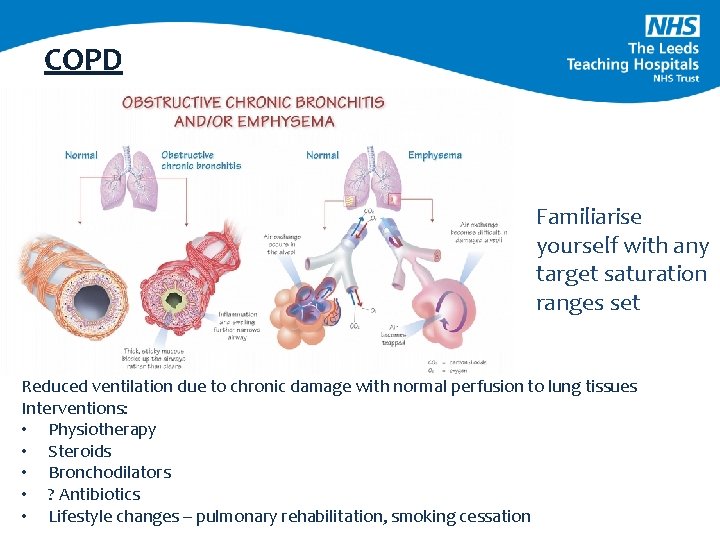
COPD Familiarise yourself with any target saturation ranges set Reduced ventilation due to chronic damage with normal perfusion to lung tissues Interventions: • Physiotherapy • Steroids • Bronchodilators • ? Antibiotics • Lifestyle changes – pulmonary rehabilitation, smoking cessation
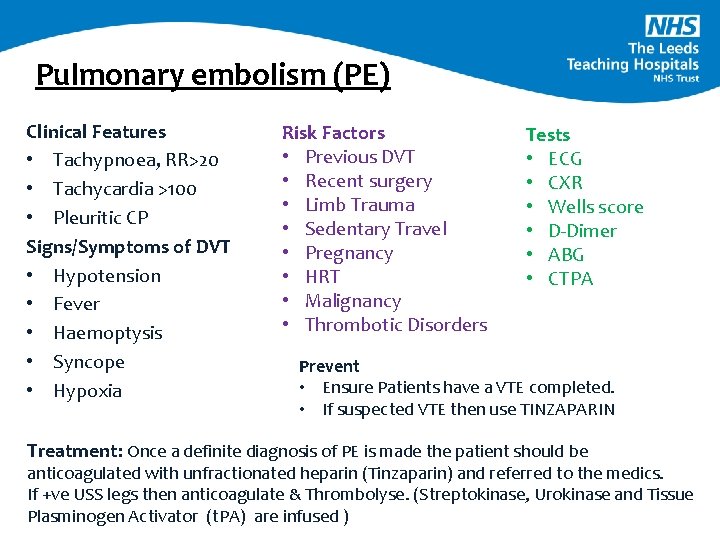
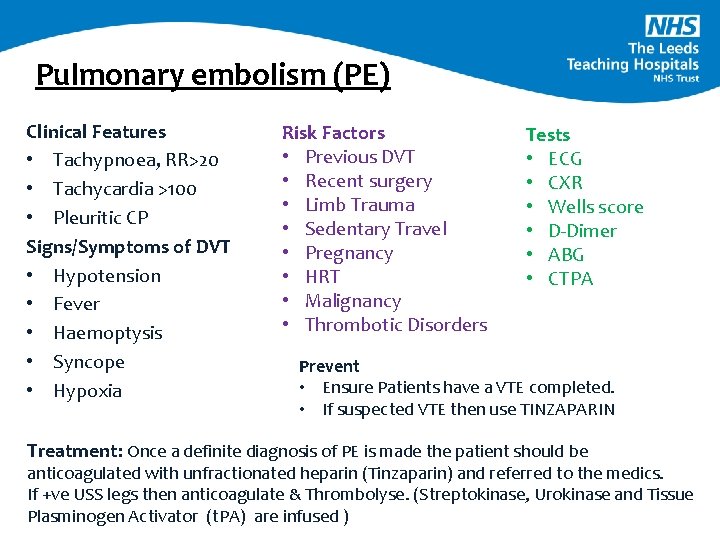
Pulmonary embolism (PE) Clinical Features • Tachypnoea, RR>20 • Tachycardia >100 • Pleuritic CP Signs/Symptoms of DVT • Hypotension • Fever • Haemoptysis • Syncope • Hypoxia Risk Factors • Previous DVT • Recent surgery • Limb Trauma • Sedentary Travel • Pregnancy • HRT • Malignancy • Thrombotic Disorders Tests • ECG • CXR • Wells score • D-Dimer • ABG • CTPA Prevent • Ensure Patients have a VTE completed. • If suspected VTE then use TINZAPARIN Treatment: Once a definite diagnosis of PE is made the patient should be anticoagulated with unfractionated heparin (Tinzaparin) and referred to the medics. If +ve USS legs then anticoagulate & Thrombolyse. (Streptokinase, Urokinase and Tissue Plasminogen Activator (t. PA) are infused )
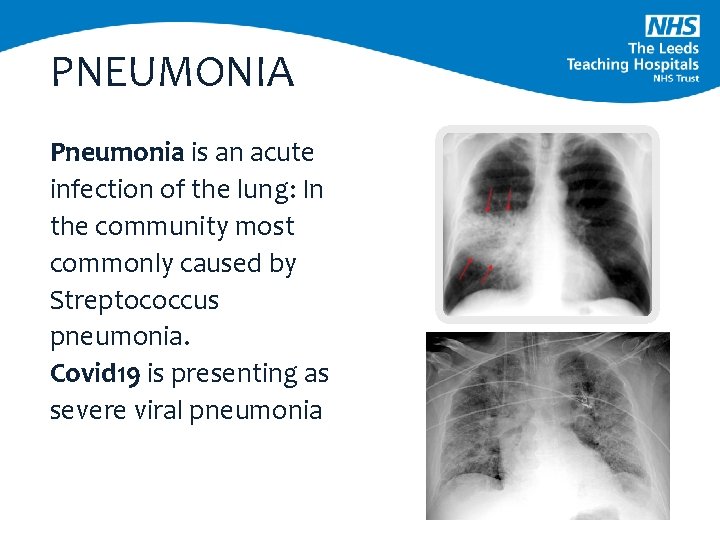
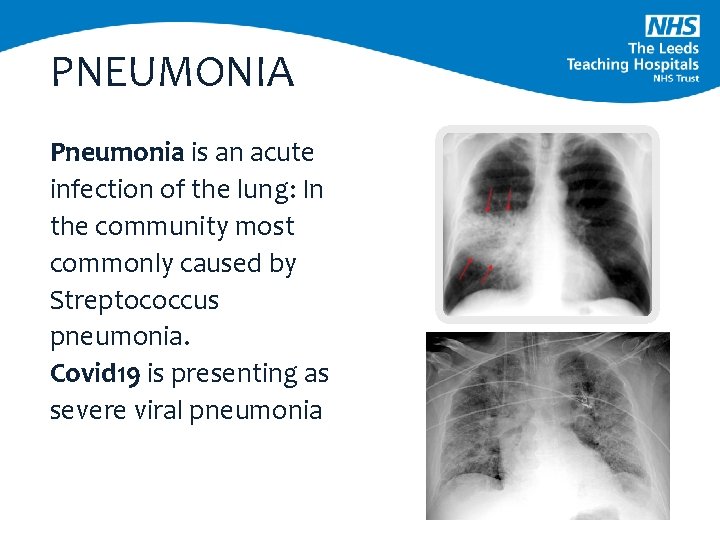
PNEUMONIA Pneumonia is an acute infection of the lung: In the community most commonly caused by Streptococcus pneumonia. Covid 19 is presenting as severe viral pneumonia
Key points 1. Good oxygen delivery appropriate for each individual patient 2. Early recognition of respiratory failure and ventilation instigation as soon as feasible 3. Excellent fluid balance recording – vital for the deteriorating patients developing pulmonary oedema from acute respiratory distress syndrome 4. Nutritional support to be instigated early to prevent muscle mass loss
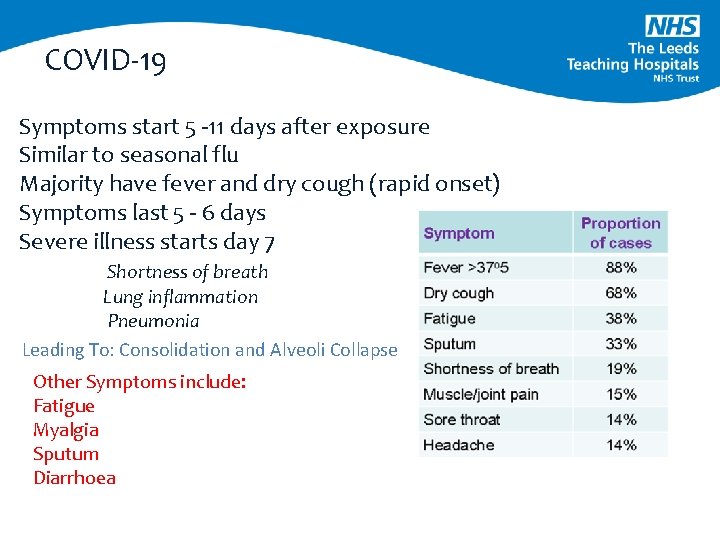
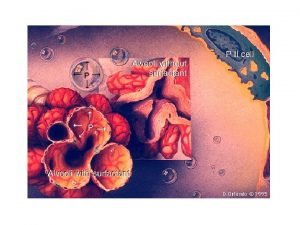
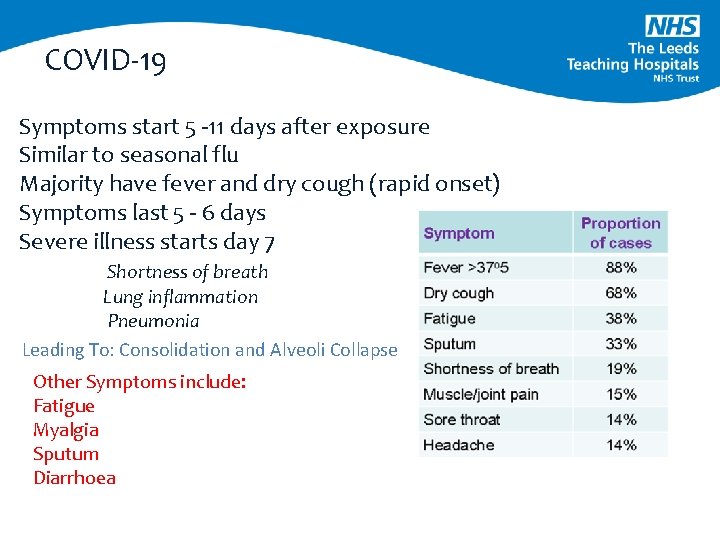
COVID-19 Symptoms start 5 -11 days after exposure Similar to seasonal flu Majority have fever and dry cough (rapid onset) Symptoms last 5 - 6 days Severe illness starts day 7 Shortness of breath Lung inflammation Pneumonia Leading To: Consolidation and Alveoli Collapse Other Symptoms include: Fatigue Myalgia Sputum Diarrhoea
Fever management and cough 98% of the patients have a fever (data is constantly evolving) • Ibuprofen should not be used to manage a fever in isolation • It can supress the body’s normal response to infection and mask disease progression. • 65% - 75% of patients presenting with Covid 19 have a dry cough • 30 -35% with sputum production Some patients may have underlying co-morbidities that complicate presentations
COVID-19 - Treatment • Supportive Care: Symptom Control • Antibiotics in SOME patients may continue when confirmed • Conservative fluid resuscitation except if in shock or AKI • Paracetamol for Antipyretic/Analgesia. Guidelines are not to give routine antipyretic. • CPAP • If progresses to ARDS mechanical ventilation is optimum treatment • Proning has been shown to be beneficial (even in conscious patients) • Research trial therapies
Resources for Covid-19 • • • https: //hhs. hud. ac. uk/covid 19/ BMJ Best Practice Up. To. Date - Need Athens Login WHO/PHE Guidelines https: //www. elfh. org. uk/programmes/coronavirus/
PULSE OXIMETRY – O 2 SATURATIONS
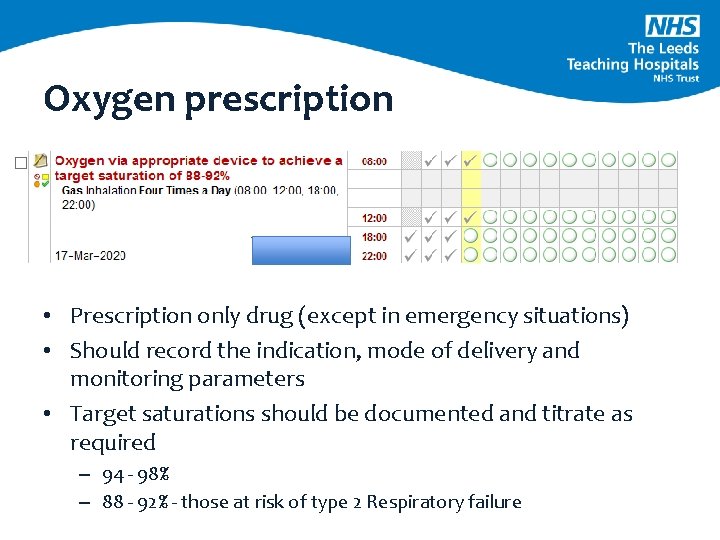
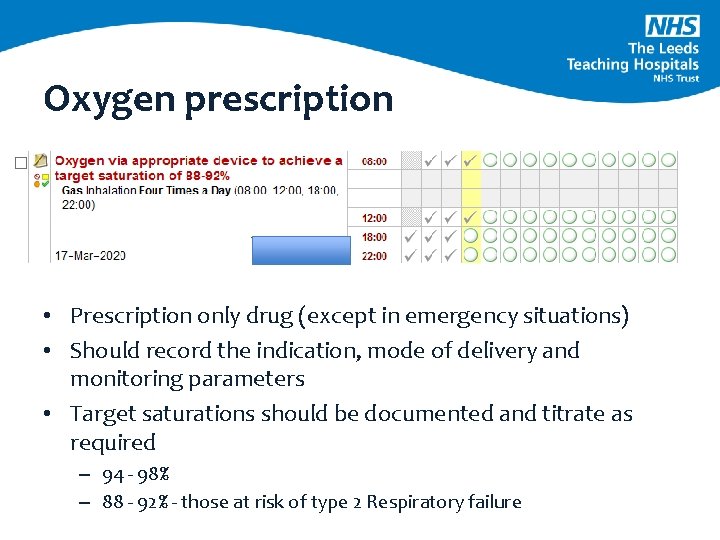
Oxygen prescription • Prescription only drug (except in emergency situations) • Should record the indication, mode of delivery and monitoring parameters • Target saturations should be documented and titrate as required – 94 - 98% – 88 - 92% - those at risk of type 2 Respiratory failure


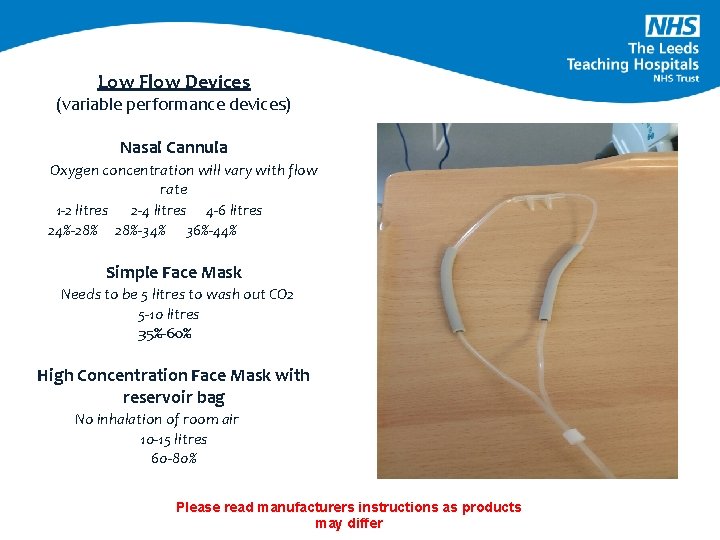
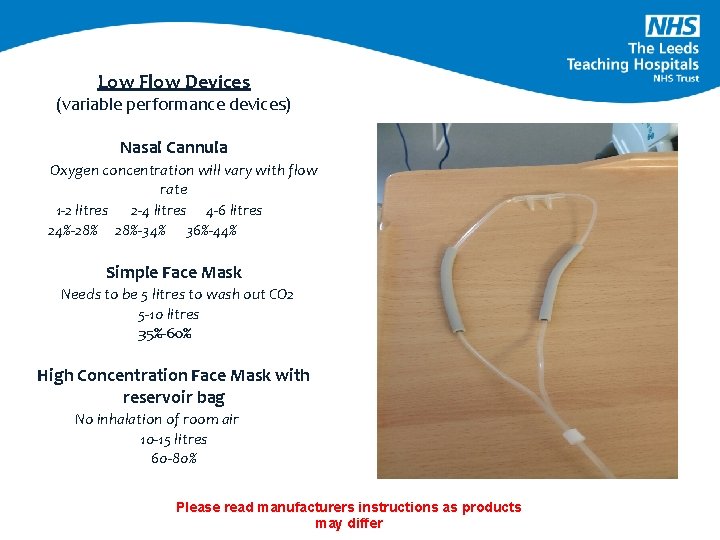
Low Flow Devices (variable performance devices) Nasal Cannula Oxygen concentration will vary with flow rate 1 -2 litres 2 -4 litres 4 -6 litres 24%-28% 28%-34% 36%-44% Simple Face Mask Needs to be 5 litres to wash out CO 2 5 -10 litres 35%-60% High Concentration Face Mask with reservoir bag No inhalation of room air 10 -15 litres 60 -80% Please read manufacturers instructions as products may differ
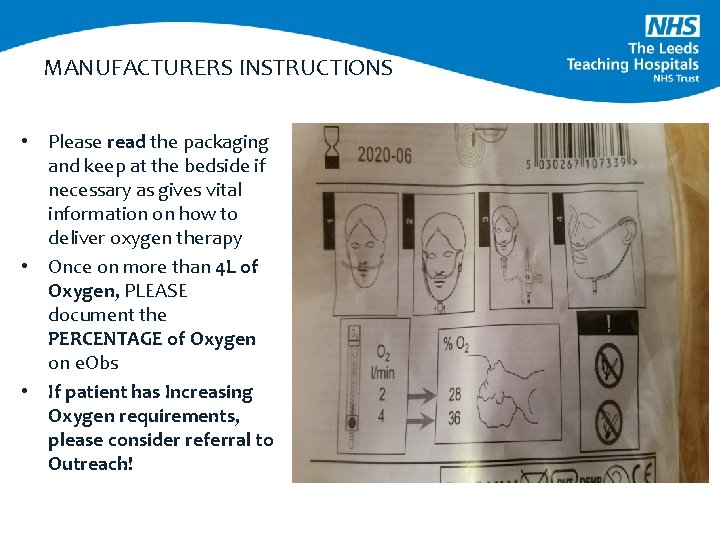
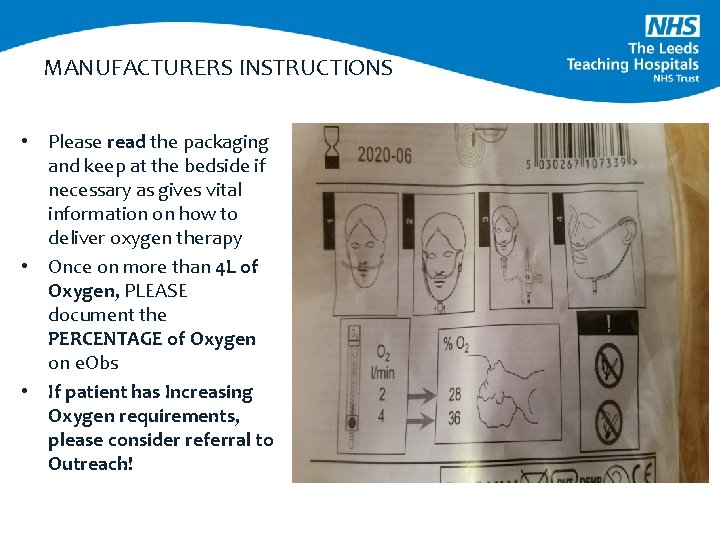
MANUFACTURERS INSTRUCTIONS • Please read the packaging and keep at the bedside if necessary as gives vital information on how to deliver oxygen therapy • Once on more than 4 L of Oxygen, PLEASE document the PERCENTAGE of Oxygen on e. Obs • If patient has Increasing Oxygen requirements, please consider referral to Outreach!
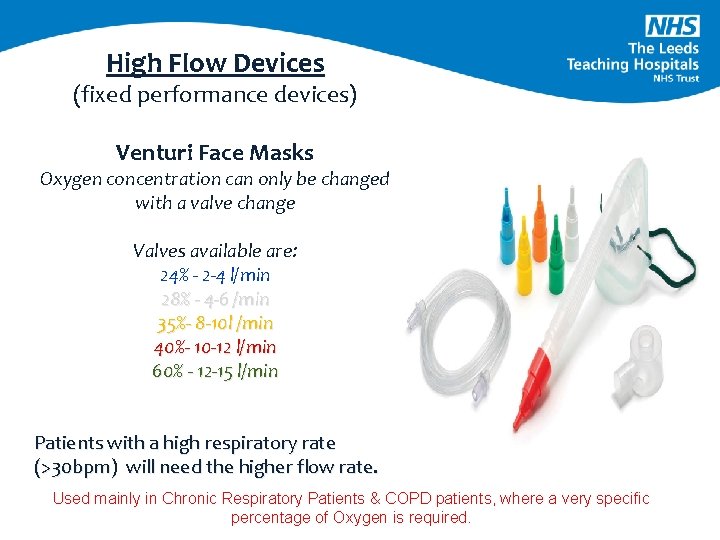
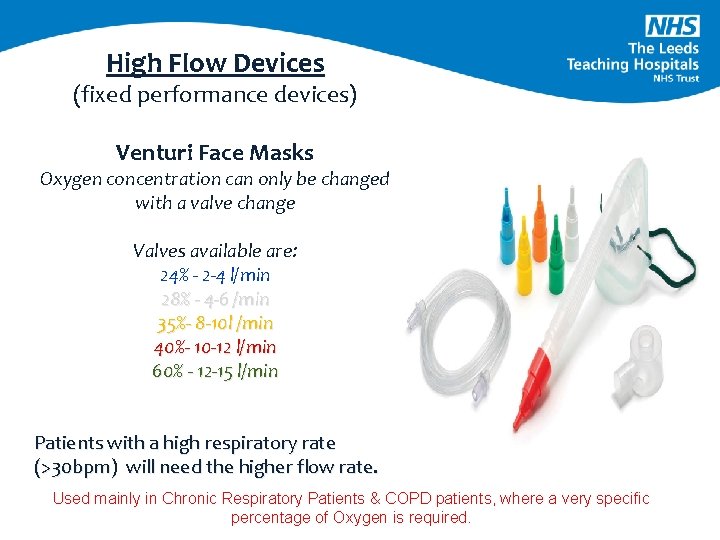
High Flow Devices (fixed performance devices) Venturi Face Masks Oxygen concentration can only be changed with a valve change Valves available are: 24% - 2 -4 l/min 28% - 4 -6 /min 35%- 8 -10 l /min 40%- 10 -12 l/min 60% - 12 -15 l/min Patients with a high respiratory rate (>30 bpm) will need the higher flow rate. Used mainly in Chronic Respiratory Patients & COPD patients, where a very specific percentage of Oxygen is required.
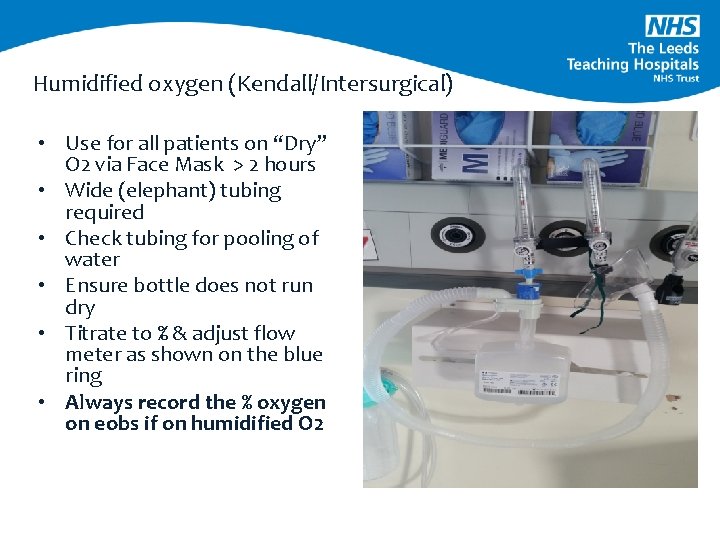
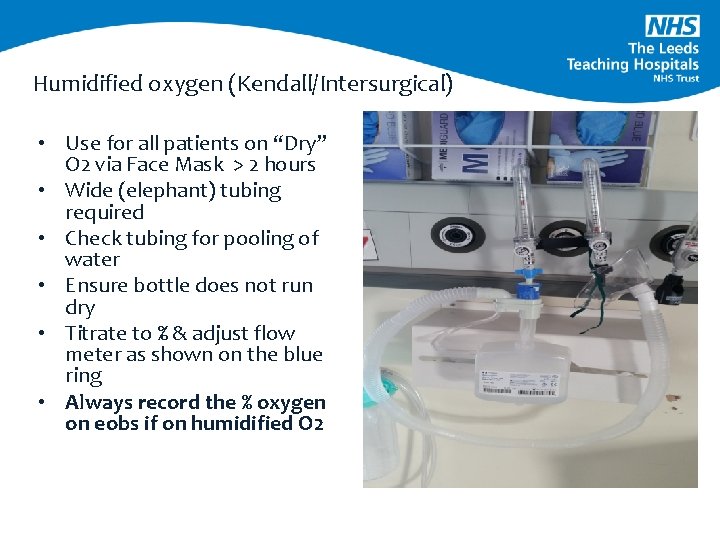
Humidified oxygen (Kendall/Intersurgical) • Use for all patients on “Dry” O 2 via Face Mask > 2 hours • Wide (elephant) tubing required • Check tubing for pooling of water • Ensure bottle does not run dry • Titrate to % & adjust flow meter as shown on the blue ring • Always record the % oxygen on eobs if on humidified O 2
POINTS TO REMEMBER • • • Whichever system your area uses to deliver humidified oxygen, remember that you need to look at the dial to understand the litres per minute that you need to run the system at, to deliver a set percentage of Oxygen If changing the % and/or the litres, please check that the 2 correlate, LOOK at the Valve! Oxygen treats hypoxaemia not breathlessness Target is normal oxygen saturations (94 -98%) for all, except those with Type II respiratory failure (88 -92%) Oxygen must be prescribed with target saturation Appropriate oxygen device must be used Patients receiving oxygen need close monitoring, allow at least 5 minutes between increasing their inspired oxygen delivered (unless emergency situation) Oxygen saturations must be measured with the appropriate probe and be wary in very unwell patients Different manufacturers will have slightly different variations Always, always record the % of inspired O 2 on e. Obs if on humidified oxygen – please ask someone if you are unsure
Nebuliser therapy • Assist patient in upright position • Ensure correct drugs - Salbutamol - Ipratropium - Normal Saline • Administer one drug at a time (Gold Standard) • Use nebuliser pack • Delivery through compressor or air (hazard) • If patient on Oxygen – keep this going
Nursing considerations • Mouth care – foam sticks • Lip care - avoid products with petroleum jelly/oil based • Encourage oral fluids (if possible) • Ensure teeth/dentures are cleaned regularly • Report and record any abnormality • Give prescribed medication • Check for pressure damage from devices
TREATMENT FAILURE • Deterioration in patient’s condition • Failure to improve/deterioration in oxygen saturations or ABG results • Development of new symptoms or complications such as pneumothorax, sputum retention • Intolerance or failure of coordinating with the oxygen delivery system • Failure to alleviate symptoms • Deteriorating conscious levels • Patient and carer wish to withdraw treatment
MANAGEMENT & MONITORING OF THE PATIENT IN RESPIRATORY DISTRESS • Ensure Safe Environment (O 2, suction, emergency buzzer) • Observe your patient (A-E) (Resus Council do a great article on this) • RR, pattern of breathing, pallor, degree of distress • Oxygen therapy appropriate to situation • Pulse Oximetry • Positioning • Reassurance • Pain assessment & analgesia
Nurse in charge Medical team Physiotherapy (oncall if needed) Outreach
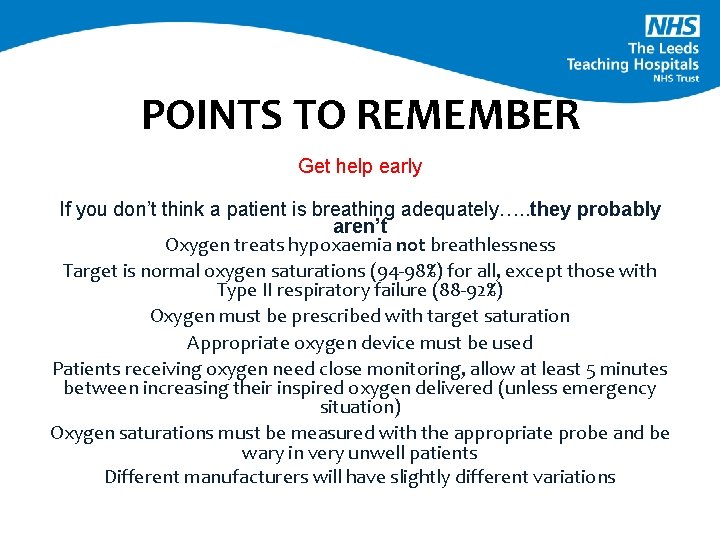
POINTS TO REMEMBER Get help early If you don’t think a patient is breathing adequately…. . they probably aren’t Oxygen treats hypoxaemia not breathlessness Target is normal oxygen saturations (94 -98%) for all, except those with Type II respiratory failure (88 -92%) Oxygen must be prescribed with target saturation Appropriate oxygen device must be used Patients receiving oxygen need close monitoring, allow at least 5 minutes between increasing their inspired oxygen delivered (unless emergency situation) Oxygen saturations must be measured with the appropriate probe and be wary in very unwell patients Different manufacturers will have slightly different variations
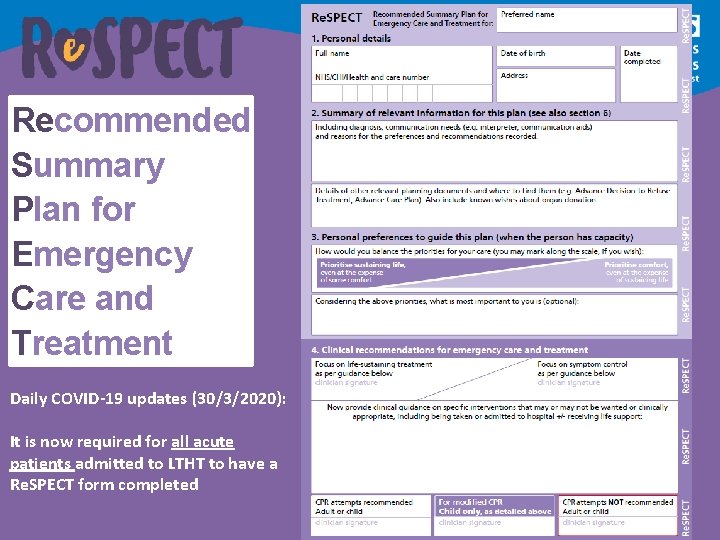
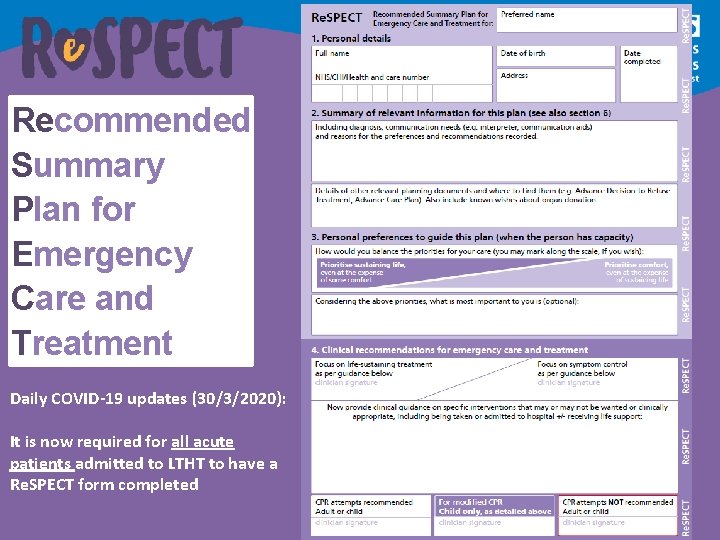
Recommended Summary Plan for Emergency Care and Treatment Daily COVID-19 updates (30/3/2020): It is now required for all acute patients admitted to LTHT to have a Re. SPECT form completed
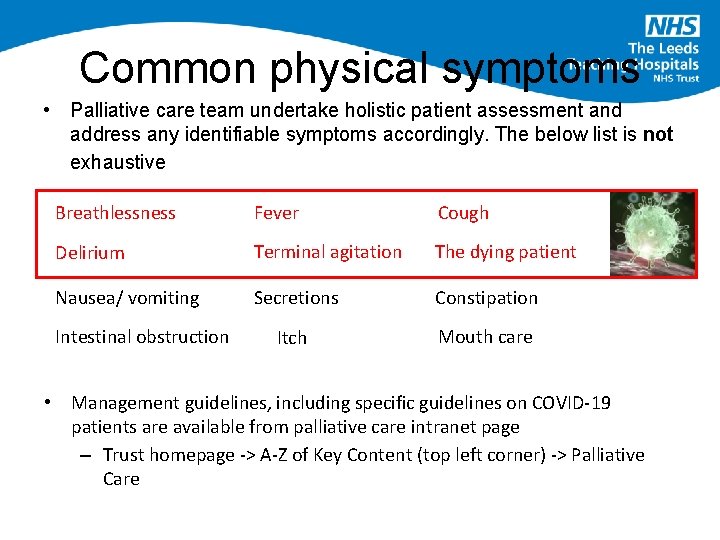
Common physical symptoms • Palliative care team undertake holistic patient assessment and address any identifiable symptoms accordingly. The below list is not exhaustive Breathlessness Fever Cough Delirium Terminal agitation The dying patient Nausea/ vomiting Secretions Constipation Itch Mouth care Intestinal obstruction • Management guidelines, including specific guidelines on COVID-19 patients are available from palliative care intranet page – Trust homepage -> A-Z of Key Content (top left corner) -> Palliative Care
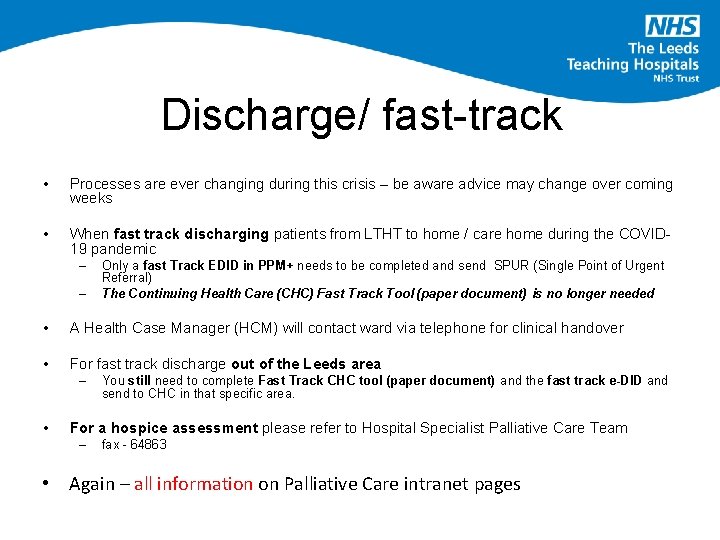
Discharge/ fast-track • Processes are ever changing during this crisis – be aware advice may change over coming weeks • When fast track discharging patients from LTHT to home / care home during the COVID 19 pandemic – – Only a fast Track EDID in PPM+ needs to be completed and send SPUR (Single Point of Urgent Referral) The Continuing Health Care (CHC) Fast Track Tool (paper document) is no longer needed • A Health Case Manager (HCM) will contact ward via telephone for clinical handover • For fast track discharge out of the Leeds area – • You still need to complete Fast Track CHC tool (paper document) and the fast track e-DID and send to CHC in that specific area. For a hospice assessment please refer to Hospital Specialist Palliative Care Team – fax - 64863 • Again – all information on Palliative Care intranet pages
 Respiratory system
Respiratory system Global alliance against chronic respiratory diseases
Global alliance against chronic respiratory diseases Chapter 23 communicable diseases
Chapter 23 communicable diseases Non common communicable diseases
Non common communicable diseases Fraction of inspired oxygen
Fraction of inspired oxygen Venturi mask oxygen flow rate
Venturi mask oxygen flow rate Bag valve mask flow rate
Bag valve mask flow rate Tracheostomy oxygen delivery
Tracheostomy oxygen delivery Respiratory zone
Respiratory zone Accenture delivery methods focus areas
Accenture delivery methods focus areas Common factors of 12 and 24
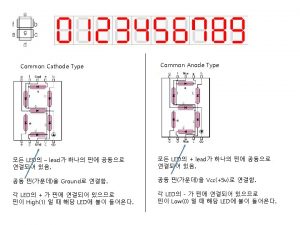
Common factors of 12 and 24 Common anode and common cathode
Common anode and common cathode 56 prime factorization
56 prime factorization How to find lowest common factor
How to find lowest common factor Factors of 60 and 48
Factors of 60 and 48 Multiples of 9 and 21
Multiples of 9 and 21 Lifestyle modern
Lifestyle modern Is hemophilia communicable or noncommunicable
Is hemophilia communicable or noncommunicable Section 19-3 diseases caused by bacteria and viruses
Section 19-3 diseases caused by bacteria and viruses Chapter 8 skin disorders and diseases
Chapter 8 skin disorders and diseases Chapter 6 musculoskeletal system diseases and disorders
Chapter 6 musculoskeletal system diseases and disorders Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Chapter 22 genetics and genetically linked diseases
Chapter 22 genetics and genetically linked diseases Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Plicatured nail
Plicatured nail Chapter 8 skin disorders and diseases
Chapter 8 skin disorders and diseases Nail disease
Nail disease Certain infectious and parasitic diseases
Certain infectious and parasitic diseases Chapter 8 cardiovascular system
Chapter 8 cardiovascular system Kronfeld mountain pass theory
Kronfeld mountain pass theory Milady chapter 8 skin disorders and diseases
Milady chapter 8 skin disorders and diseases