RESPIRATORY SYSTEM Function of respiratory system provides oxygen


























- Slides: 65
RESPIRATORY SYSTEM
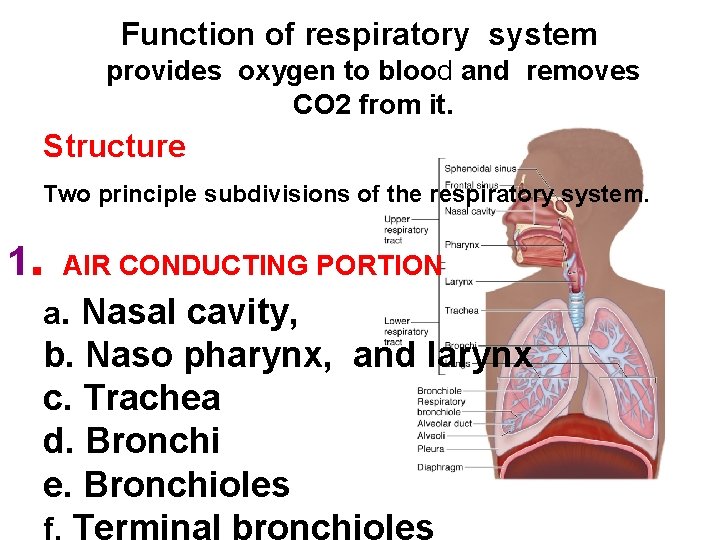
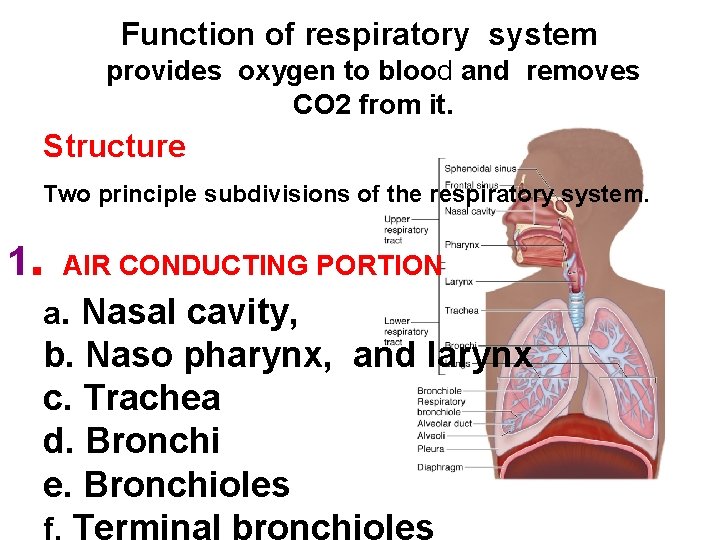
Function of respiratory system provides oxygen to blood and removes CO 2 from it. Structure Two principle subdivisions of the respiratory system. 1. AIR CONDUCTING PORTION a. Nasal cavity, b. Naso pharynx, and larynx c. Trachea d. Bronchi e. Bronchioles f. Terminal bronchioles

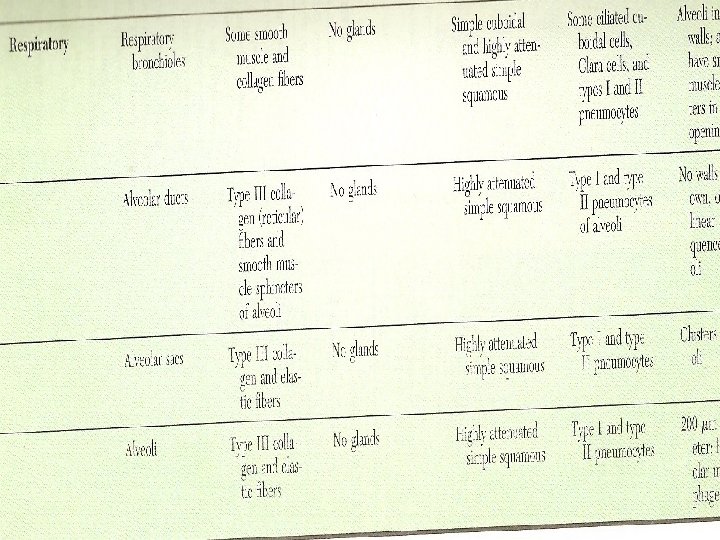
2. RESPIRATORY PORTION a. Respiratory bronchioles b. Alveolar ducts c. Alveolar sacs and alveoli for gas exchange

Conducting portion 1. Provides a passageway to and from lungs 2. Its components "condition" the inspired air (i. e. moistens, removes particles and some noxious gases, and warms air)
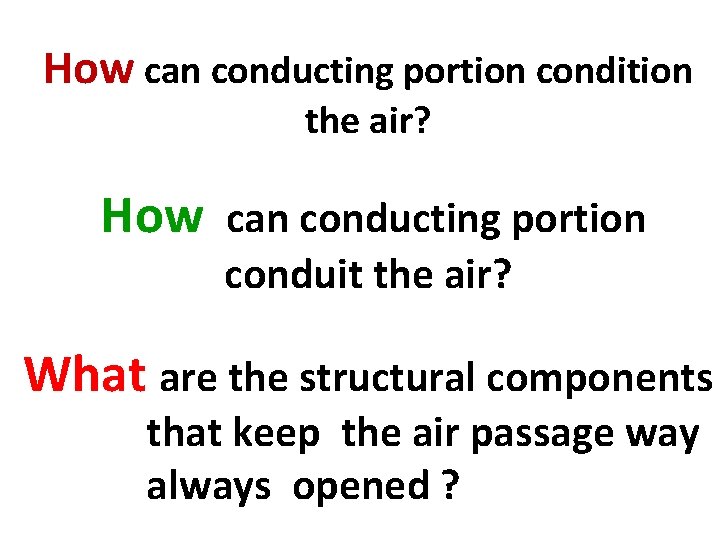
How can conducting portion condition the air? How can conducting portion conduit the air? What are the structural components that keep the air passage way always opened ?

There are three structures in the wall of respiratory tract; they keep the airway patent and opened; they are: 1 -Cartilage. 2 -Elastic fiber. 3 -Smooth muscle. The cartilage: (Hyaline cartilage) . . . Support the wall. Prevent collapse of the lumen. Give rigidity to the wall.
• Elastic fiber - Provide flexibility to wall. -Permit elongation of the conducting portion. • Smooth muscle Reduce the diameter of the tube; regulates the air flow.

The air must be condition before it reaches the respiratory portion, the wall of conducting portion have many structural features to serve these functions: The mucosa is epithelium and lamina propria. Most parts of conducting portion are lined by epithelium called respiratory epithelium
which is pseudo stratified columnarciliated epithelium with goblet cells. • The cilia= Push the dust particles and mucus by its motion toward the pharynx either to be swallowed or thrown out.

• Goblet cells and mucous glands= cover the epithelium with protective mucous secretion that trap the dust particles; and moisten the air.
• The lamina popria contains serous and mucous glands, and numerous blood vessels. The serous gland = keep the epithelium moist, and humidify the air. The blood vessels = warm the air.
Cells of Respiratory epithelium It is composed of five types of cell: 1. Ciliated cells. 2. Goblet cells. 3. Brush cells (intermediate cells) 4. Basal cells. 5. Granular cells (neuro endocrine cells).
• Ciliated cells: Are tall columnar cells have cilia, basal located nucleus. • Goblet cells: • Brush cells: Have microvilli, transform into either ciliated cells or goblet cells. • Basal cells: Are short cells lie on the basement membrane but don’t reach the surface. They are stem cells from which other cell types are developed. • Granular cells: Are rounded cells have dark stained nucleus, and secretary granules.

Nasal cavity Is divided into right& left, by nasal septum and composed of three parts: -Vestibule ; -Respiratory area -Olfactory area.
Vestibule Is widest part continuous with external skin, has stiff thick hairs to remove the dust particles from inspired air, and sweat glands. The lamina propria contains serous mucus glands, and numerous blood vessels.
The respiratory area • Is lined by pseudo stratified ciliated columnar epithelium with goblet cells. • Lamina propria contains serous; mucous glands; and blood vessels
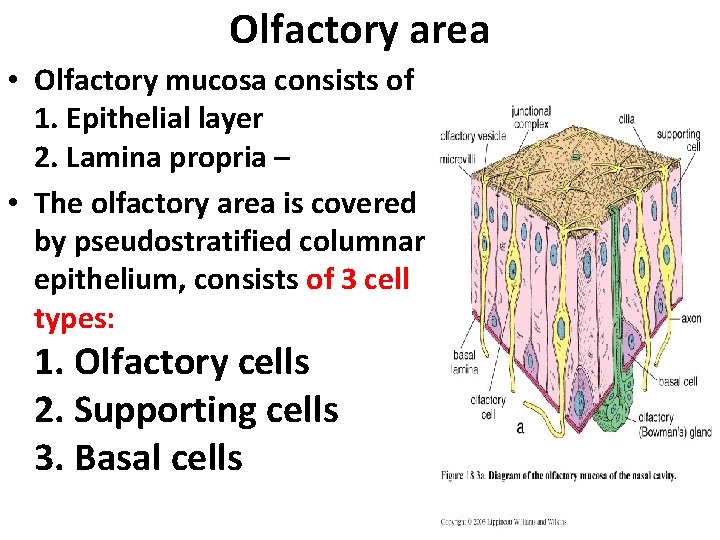
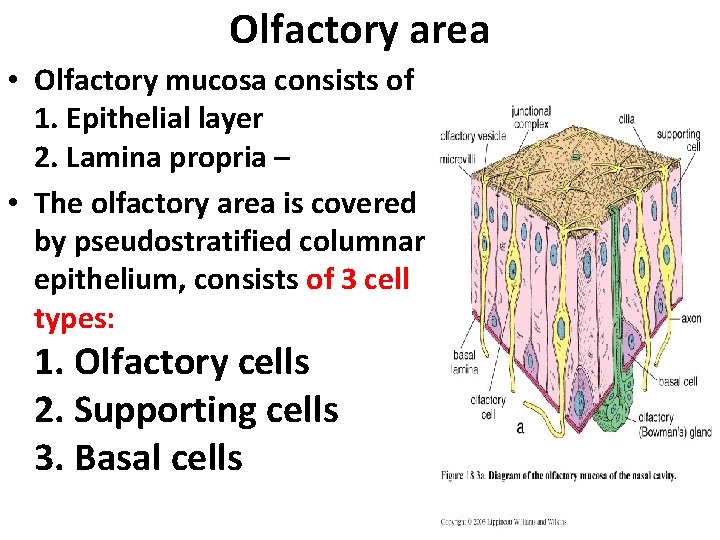
Olfactory area • Olfactory mucosa consists of 1. Epithelial layer 2. Lamina propria – • The olfactory area is covered by pseudostratified columnar epithelium, consists of 3 cell types: 1. Olfactory cells 2. Supporting cells 3. Basal cells

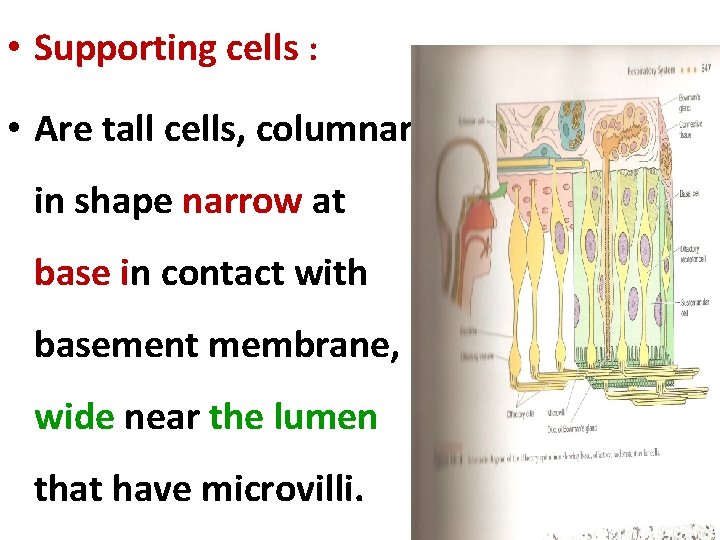
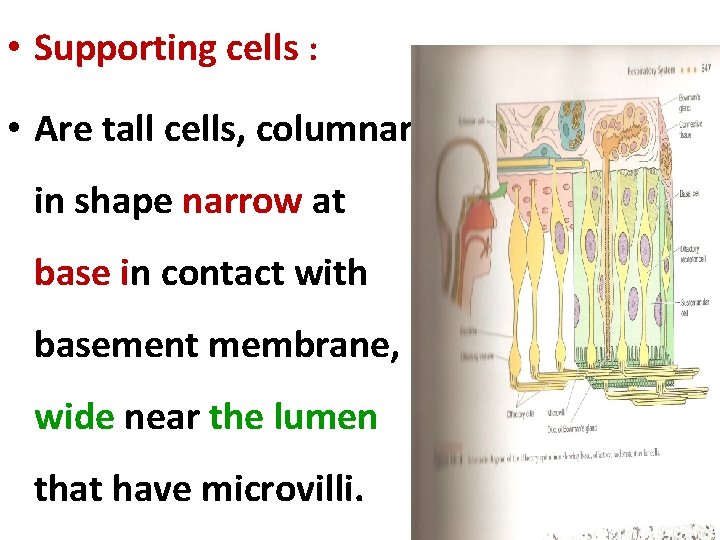
• Supporting cells : • Are tall cells, columnar in shape narrow at base in contact with basement membrane, wide near the lumen that have microvilli.

• Have oval nucleus. Cytoplasm has secretary granules. • These cells help in metabolic and physical support of olfactory cells. • They are may be phagocytic cell.

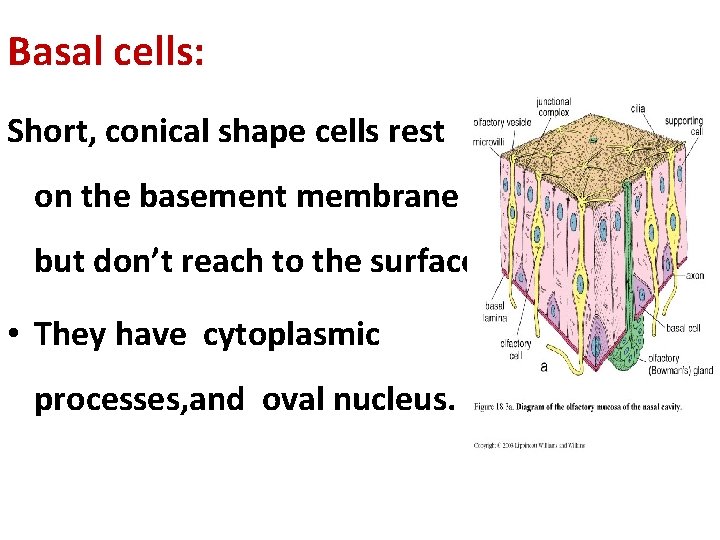
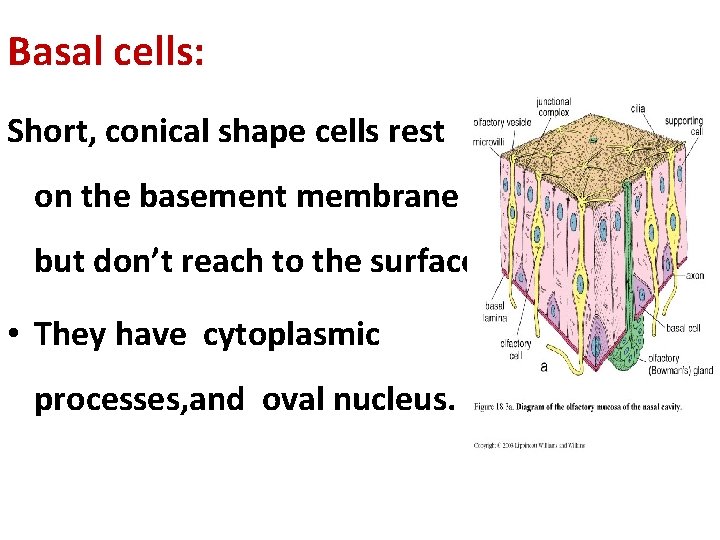
Basal cells: Short, conical shape cells rest on the basement membrane but don’t reach to the surface. • They have cytoplasmic processes, and oval nucleus.
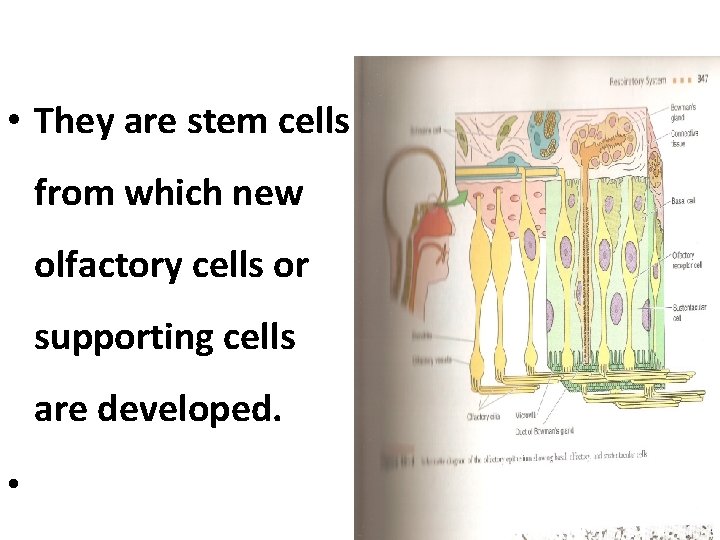
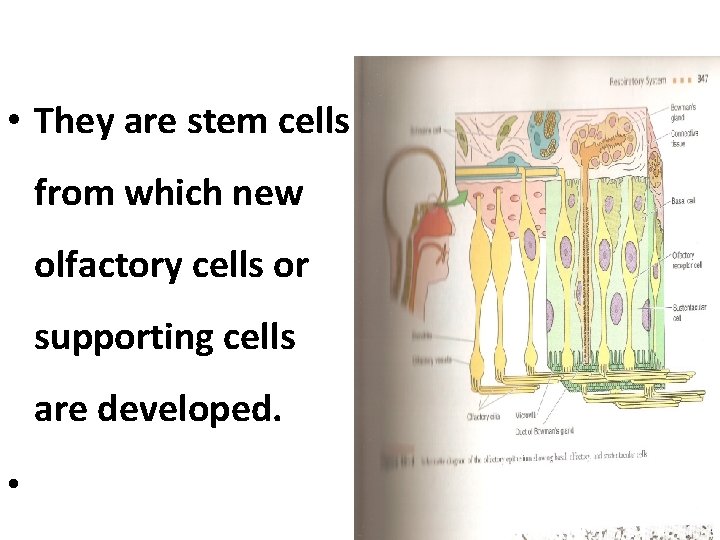
• They are stem cells from which new olfactory cells or supporting cells are developed. •
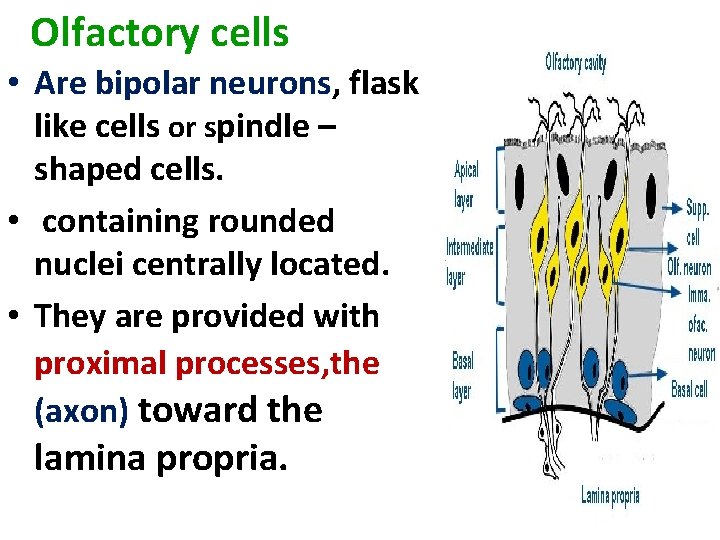
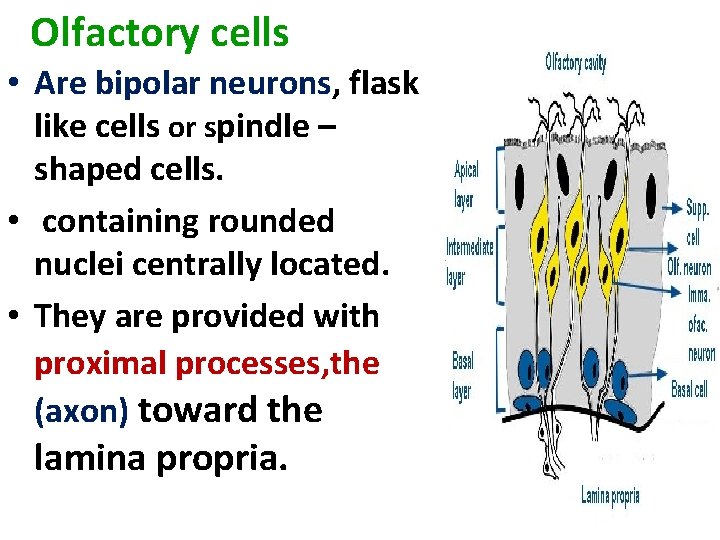
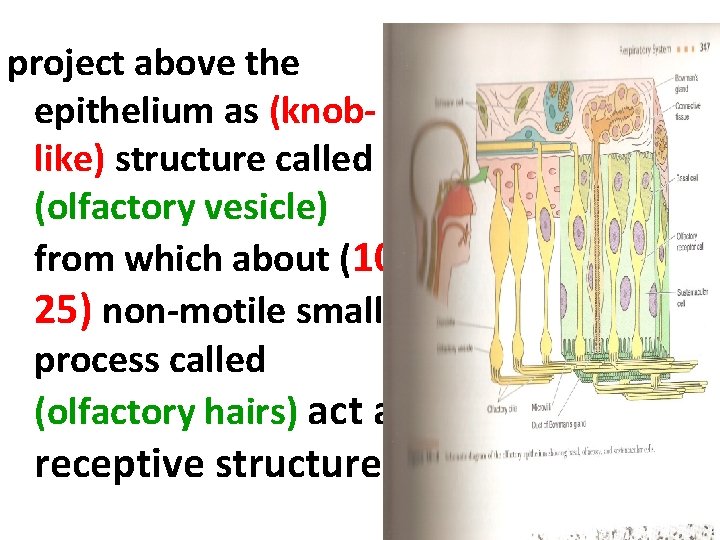
Olfactory cells • Are bipolar neurons, flask like cells or spindle – shaped cells. • containing rounded nuclei centrally located. • They are provided with proximal processes, the (axon) toward the lamina propria.

The distal process also known as dendrites pass towards the surface between the supporting cells,
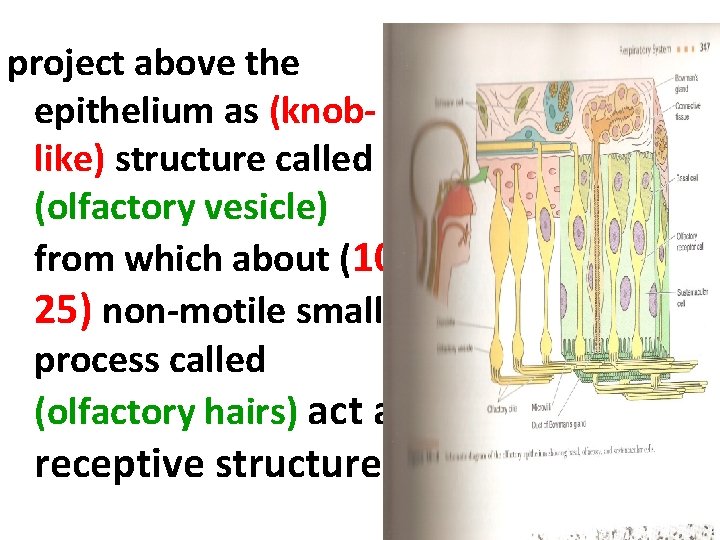
project above the epithelium as (knoblike) structure called (olfactory vesicle) from which about (1025) non-motile small process called (olfactory hairs) act as receptive structure.
Bowman gland • Is tubulo- acinar gland (serous gland). found in the lamina propria that contains collage fiber, blood and lymphatic capillaries The secretion is carried to surface by duct in the olfactory epithelium that act as solvent to substances.

Para nasal sinuses • They are maxillary, ethmoid; sphenoid, frontal sinuses. • Communicated with nasal cavity so they are lined by respiratory epithelium. • They increase the surface area for warming and moistening the air. • Play role in sound.
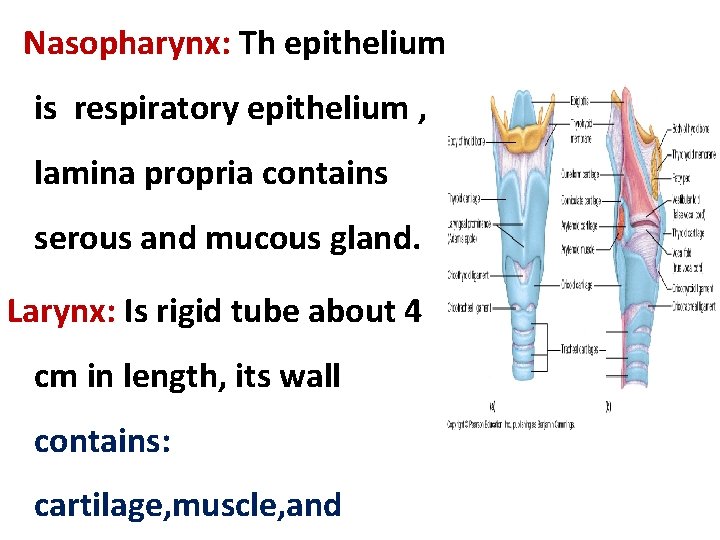
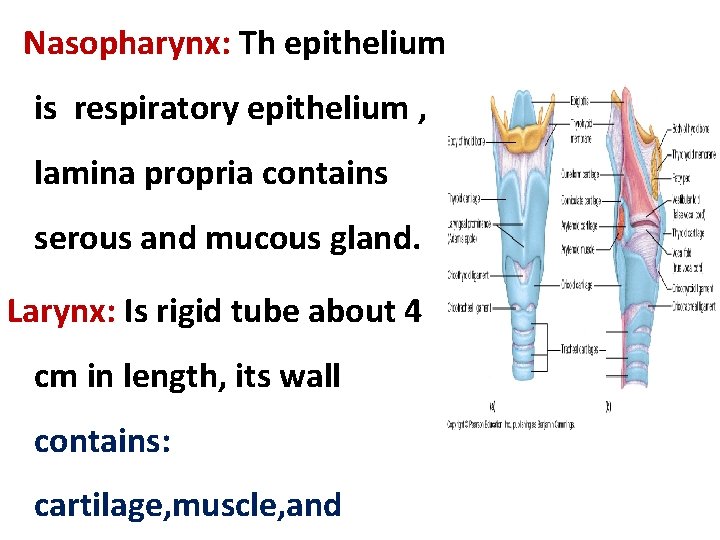
Nasopharynx: Th epithelium is respiratory epithelium , lamina propria contains serous and mucous gland. Larynx: Is rigid tube about 4 cm in length, its wall contains: cartilage, muscle, and

• The cartilage of hyaline type is thyroid, cricoids and, arytenoids cartilage. • The elastic cartilage epiglottis, is valve-like structure covered by mucous membrane on both sides. • Anterior surface stratified squamous epithelium non-keratinized. • Posterior surface pseudo stratified ciliated columnar epithelium with goblet cells.
Vocal cords: Are two pairs of folds extend into the lumen of larynx from the mucosa below the epiglottis. • The upper fold (false vocal cords) lined by respiratory epithelium. • The lower fold (true vocal cord) lined by stratified squamous epithelium. • Vocal ligament and bundle of skeletal muscle (vocals muscle). • •
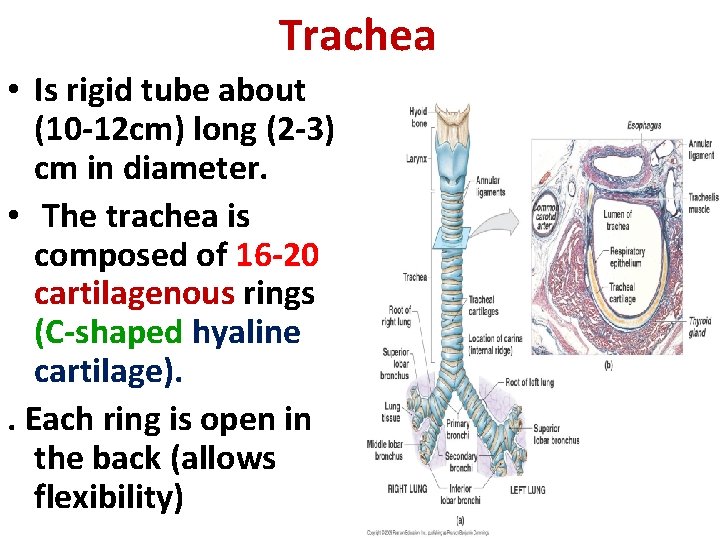
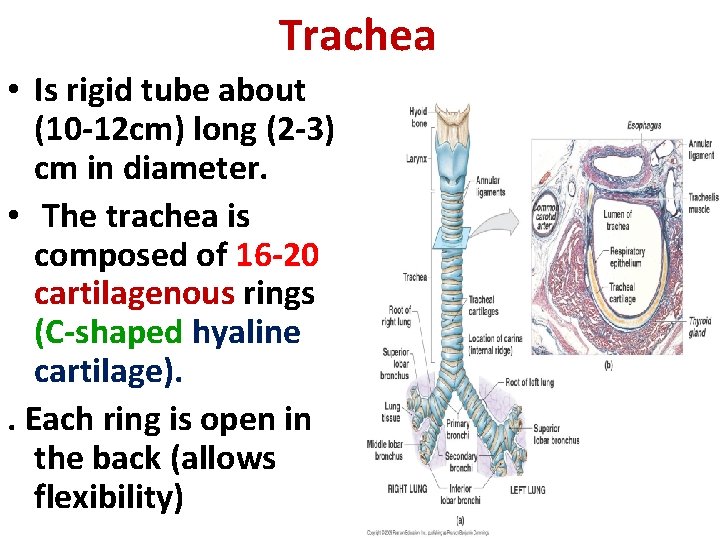
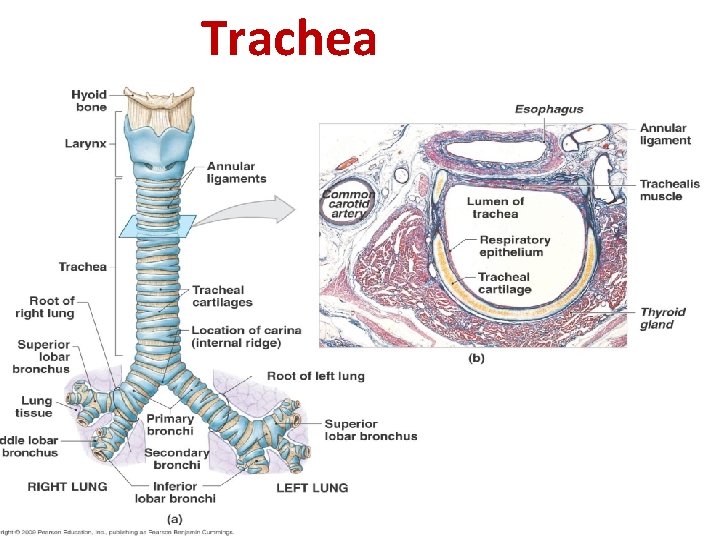
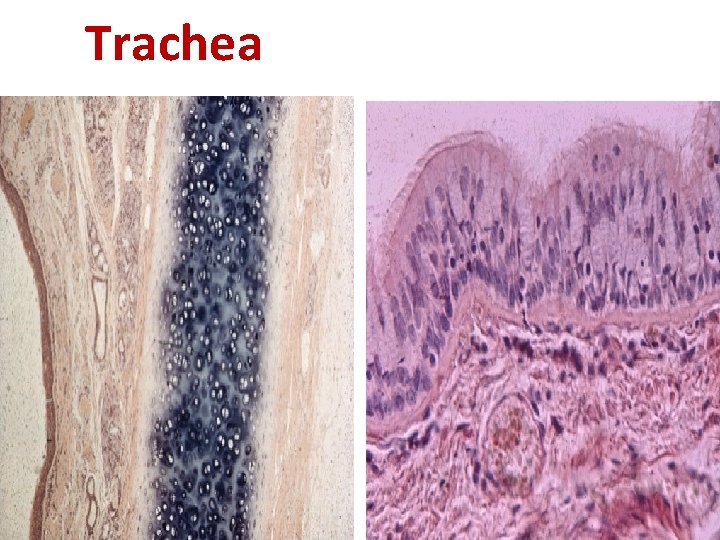
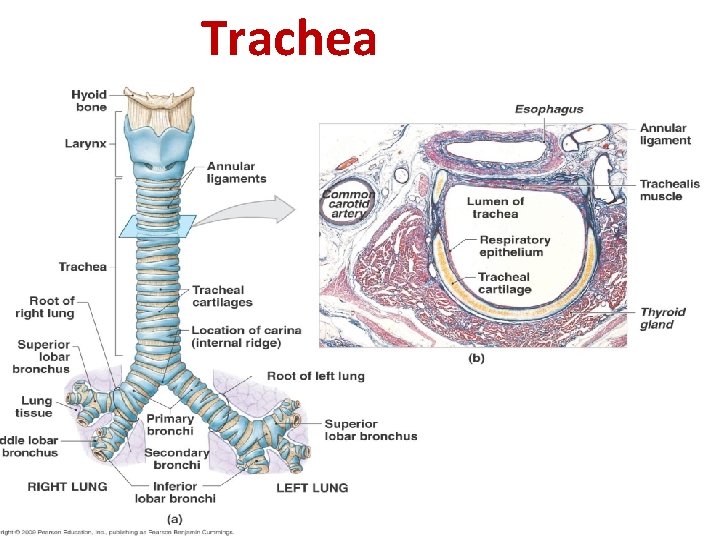
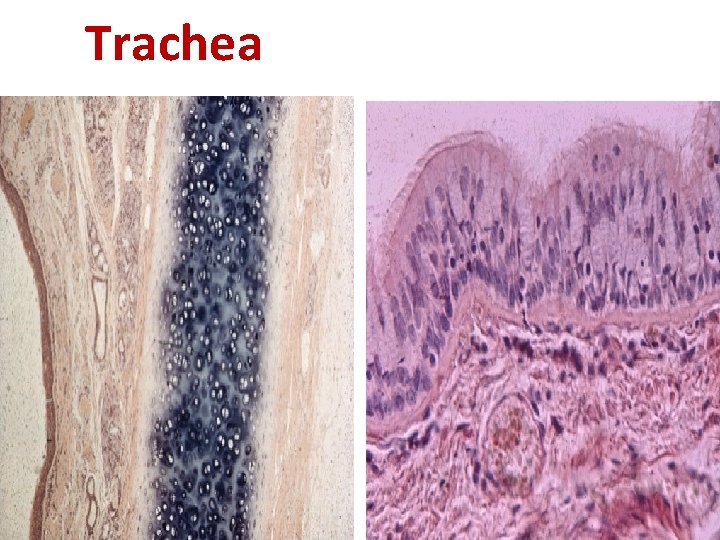
Trachea • Is rigid tube about (10 -12 cm) long (2 -3) cm in diameter. • The trachea is composed of 16 -20 cartilagenous rings (C-shaped hyaline cartilage). . Each ring is open in the back (allows flexibility)
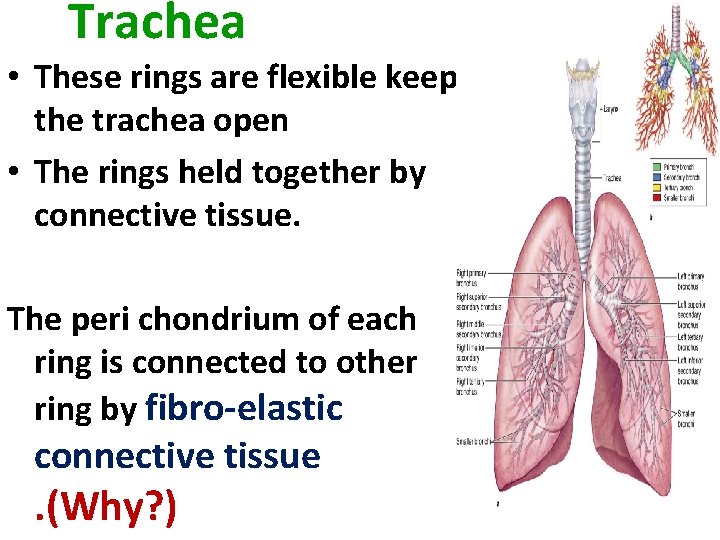
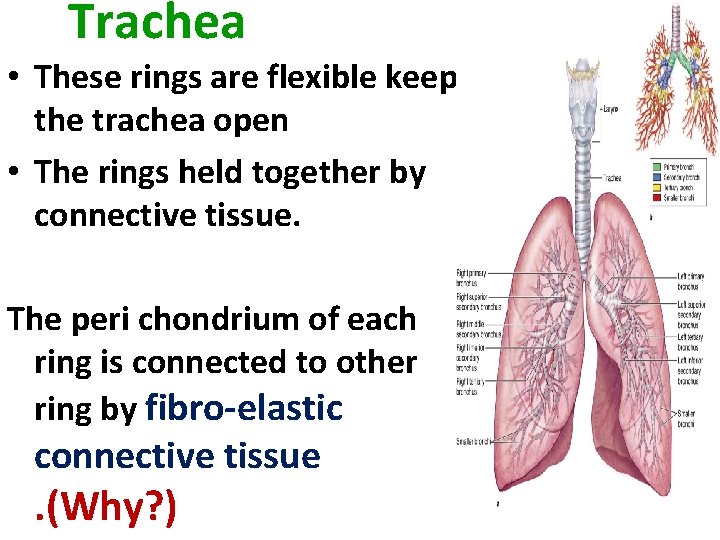
Trachea • These rings are flexible keep the trachea open • The rings held together by connective tissue. The peri chondrium of each ring is connected to other ring by fibro-elastic connective tissue . (Why? )
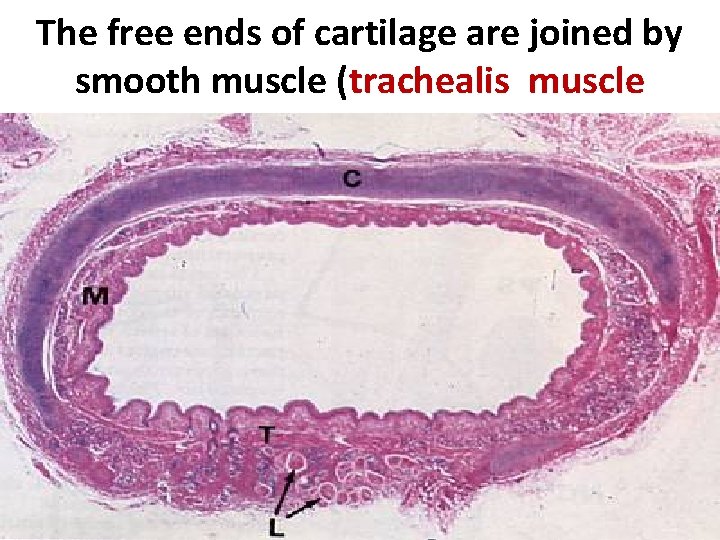
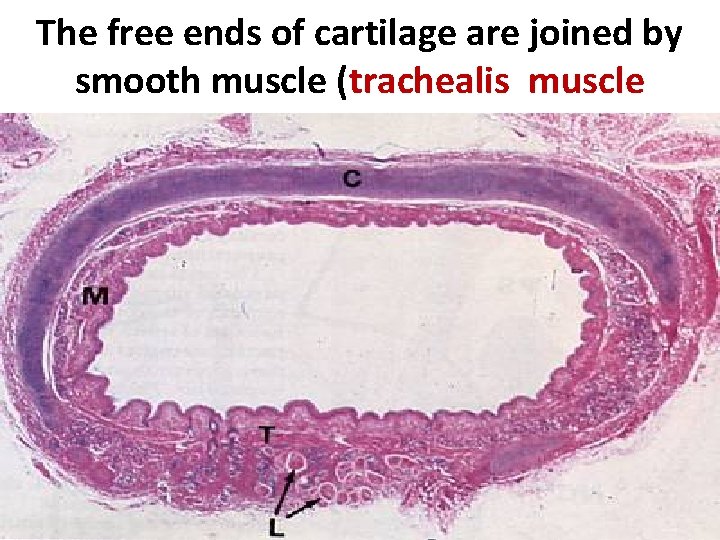
The free ends of cartilage are joined by smooth muscle (trachealis muscle • .
Trachea
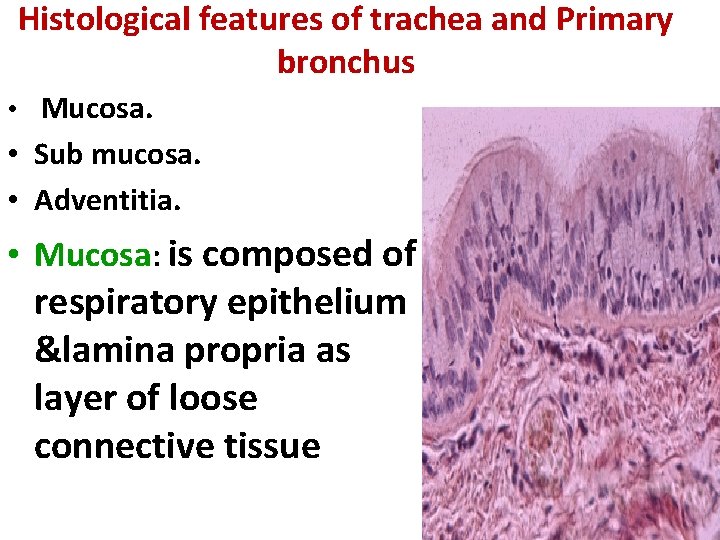
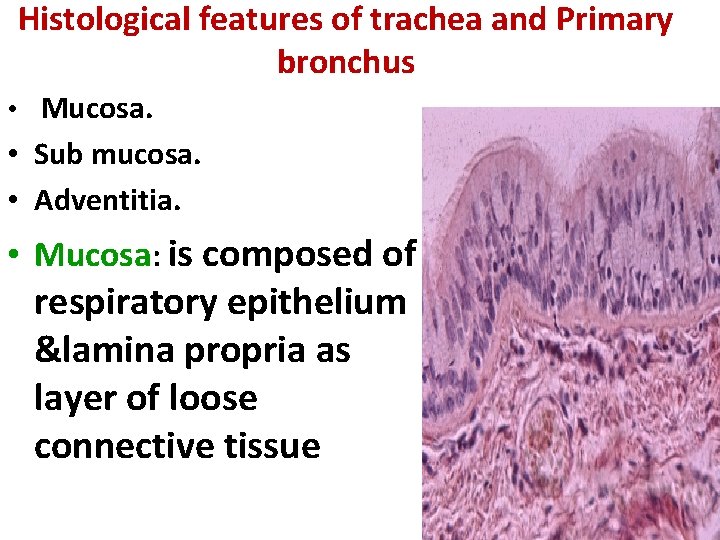
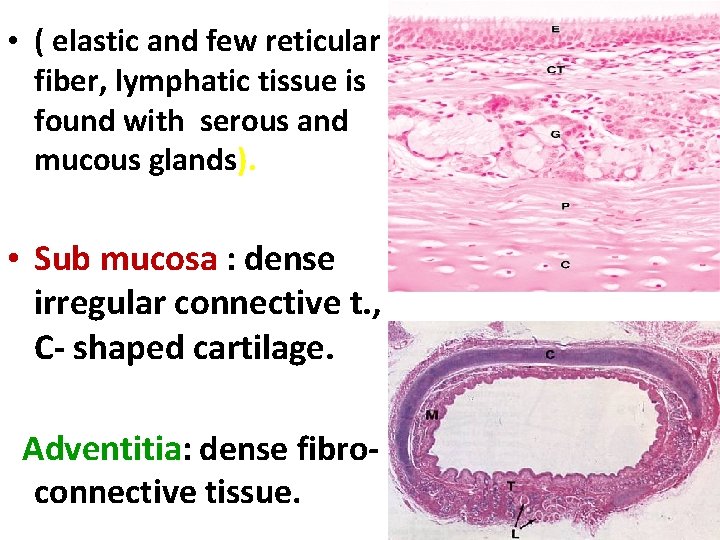
Histological features of trachea and Primary bronchus • Mucosa. • Sub mucosa. • Adventitia. • Mucosa: is composed of respiratory epithelium &lamina propria as layer of loose connective tissue
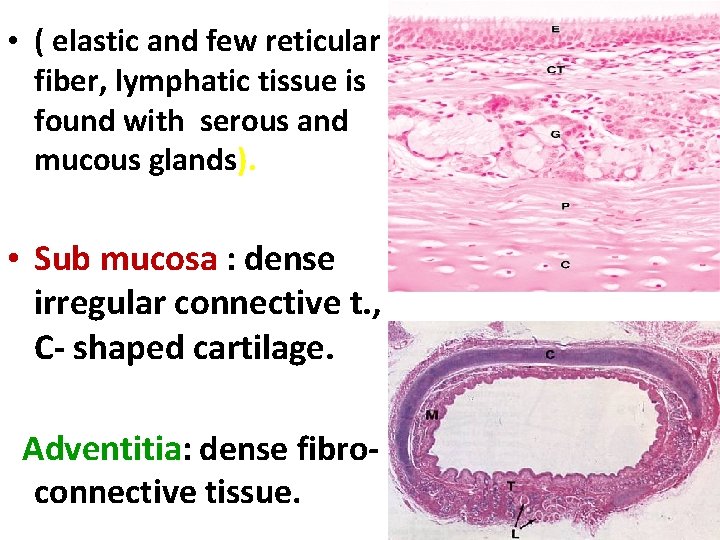
• ( elastic and few reticular fiber, lymphatic tissue is found with serous and mucous glands). • Sub mucosa : dense irregular connective t. , C- shaped cartilage. Adventitia: dense fibroconnective tissue.
Trachea
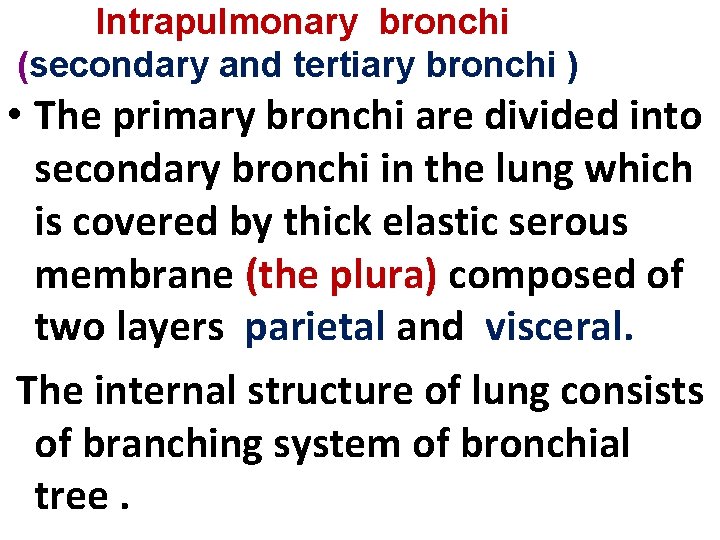
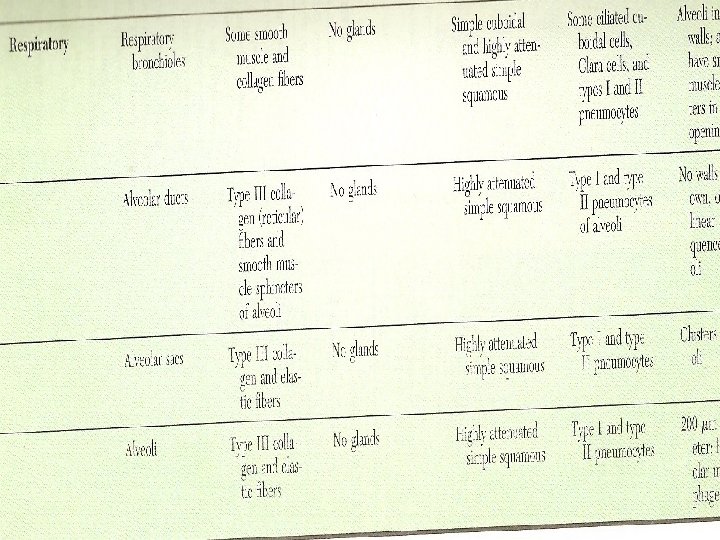
Intrapulmonary bronchi (secondary and tertiary bronchi ) • The primary bronchi are divided into secondary bronchi in the lung which is covered by thick elastic serous membrane (the plura) composed of two layers parietal and visceral. The internal structure of lung consists of branching system of bronchial tree.


Secondary bronchus The mucosa, is composed of respiratory epithelium and lamina propria contains connective tissue , serous and mucous glands. • Irregular plates of cartilage instead of Cshaped cartilage.
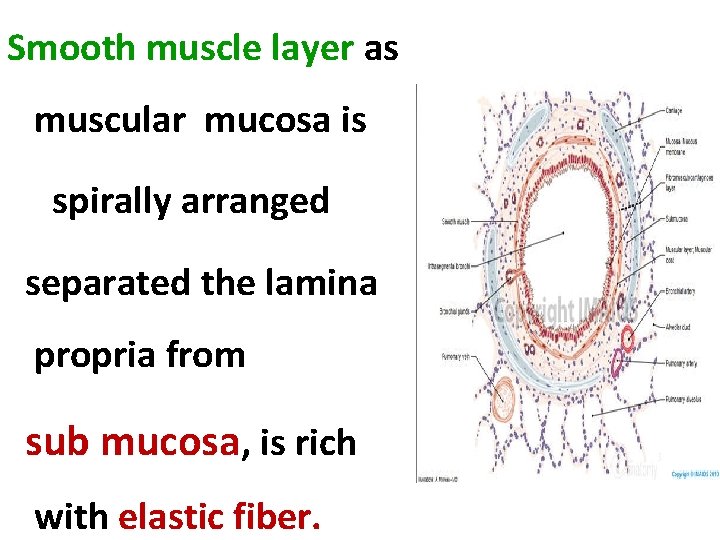
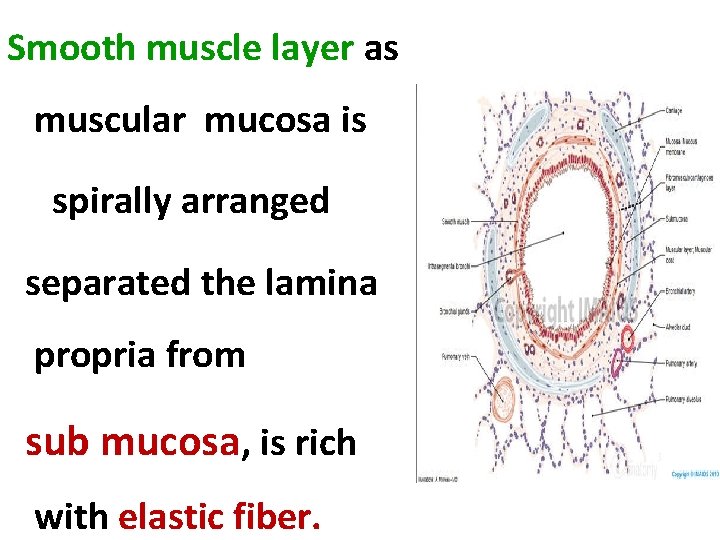
Smooth muscle layer as muscular mucosa is spirally arranged separated the lamina propria from sub mucosa, is rich with elastic fiber.

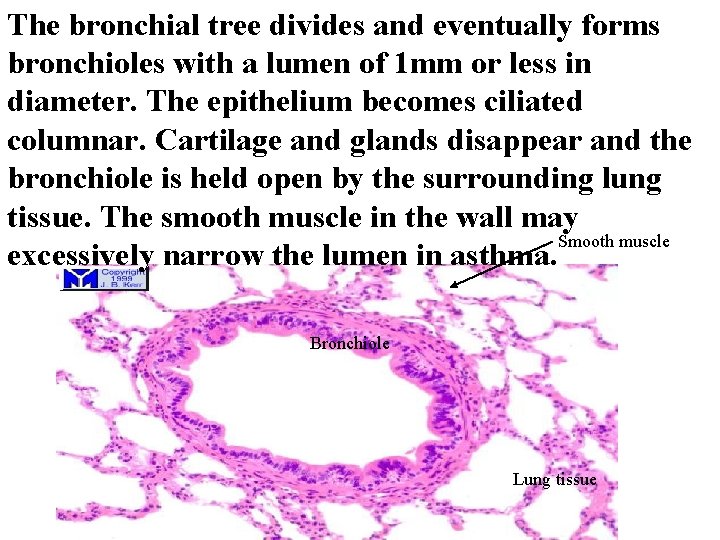
Bronchioles • large bronchioles about 5 mm or less in diameter: • Their wall is lined by respiratory epithelium , no glands , no cartilage. Diameter about 1 mm or less: • The epithelium becomes ciliated columnar with some goblet cells. • Bundle of smooth muscle is increased run in spiral manner.
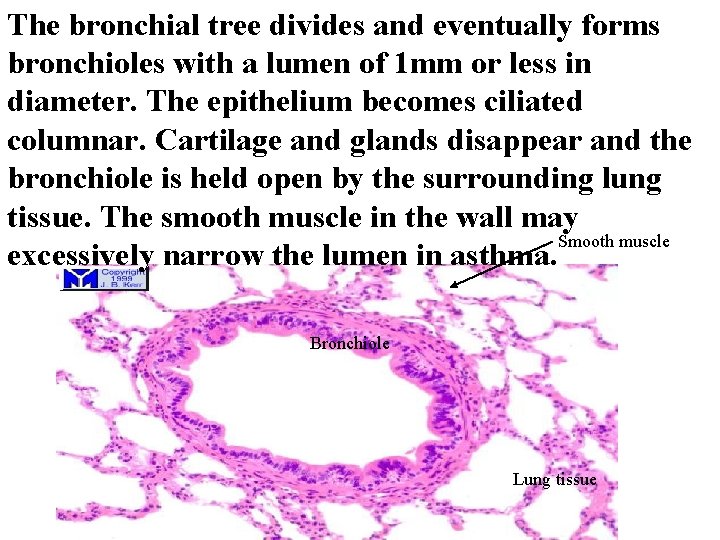
The bronchial tree divides and eventually forms bronchioles with a lumen of 1 mm or less in diameter. The epithelium becomes ciliated columnar. Cartilage and glands disappear and the bronchiole is held open by the surrounding lung tissue. The smooth muscle in the wall may Smooth muscle excessively narrow the lumen in asthma. Bronchiole Lung tissue
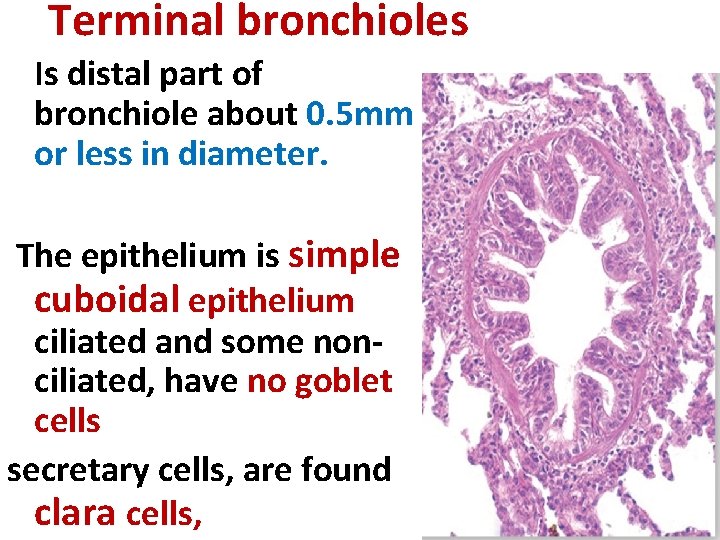
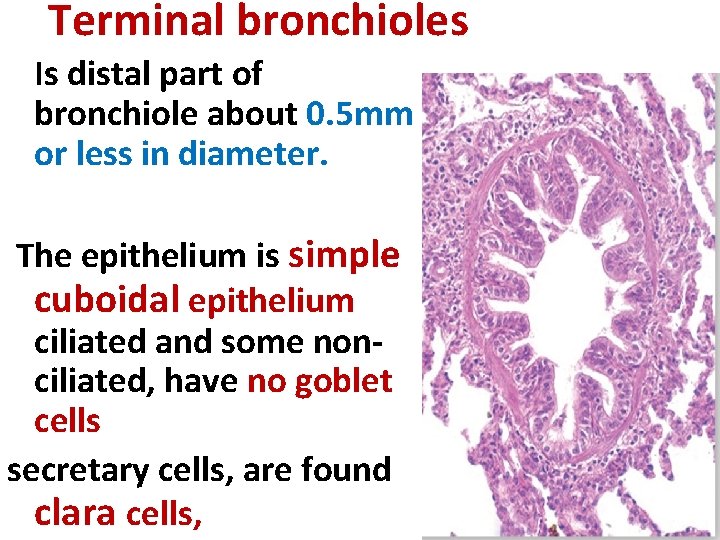
Terminal bronchioles Is distal part of bronchiole about 0. 5 mm or less in diameter. The epithelium is simple cuboidal epithelium ciliated and some nonciliated, have no goblet cells secretary cells, are found clara cells,

Clara cells a-Secretary cell, domeshaped. b-Secrete surfactants that decrease surface tension of fluid that moistens and protect the surface of the bronchiolar lining.

Lamina propria composed of elastic fiber (high amount). The smooth muscles, thick bundles one or two layers spirally arranged, so the mucosa show longitudinal folding.

Bronchioles continue to divide and decrease in size, becoming terminal, and then respiratory, which give the alveolar ducts, alveolar sacs and alveoli.
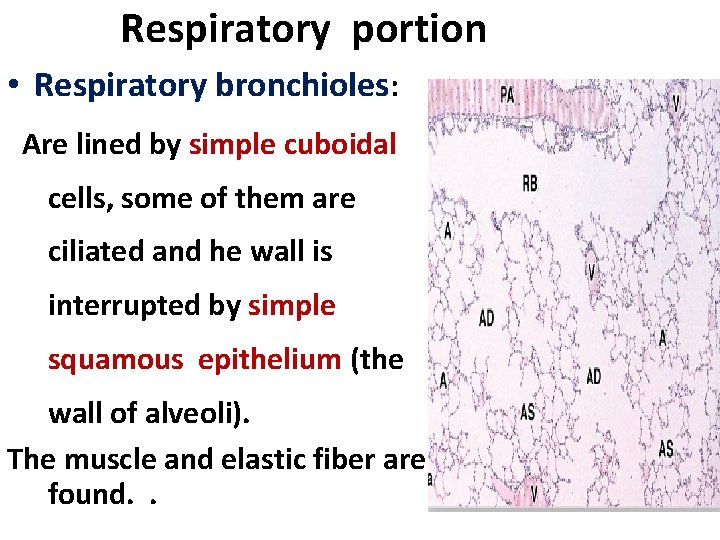
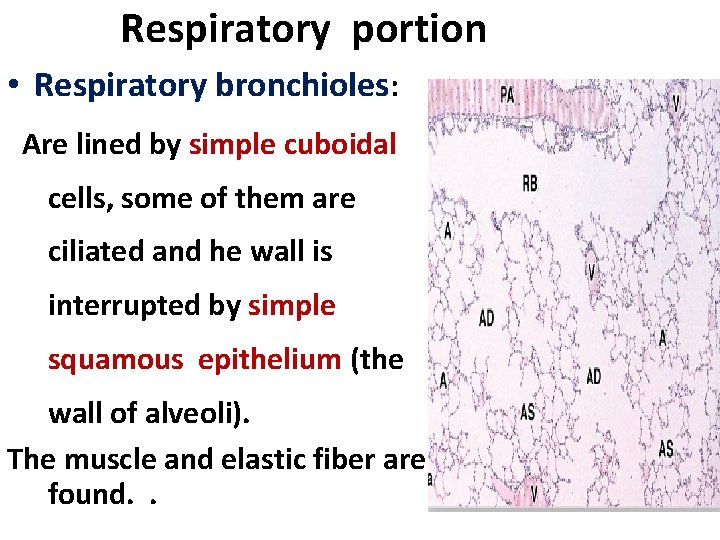
Respiratory portion • Respiratory bronchioles: Are lined by simple cuboidal cells, some of them are ciliated and he wall is interrupted by simple squamous epithelium (the wall of alveoli). The muscle and elastic fiber are found. .
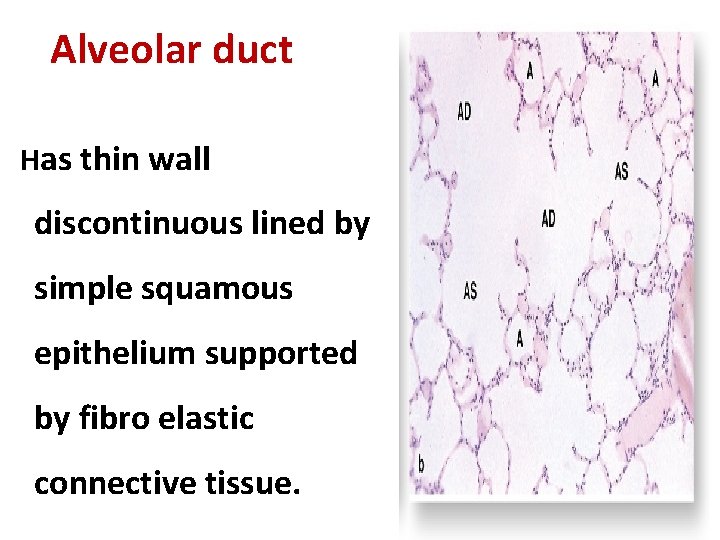
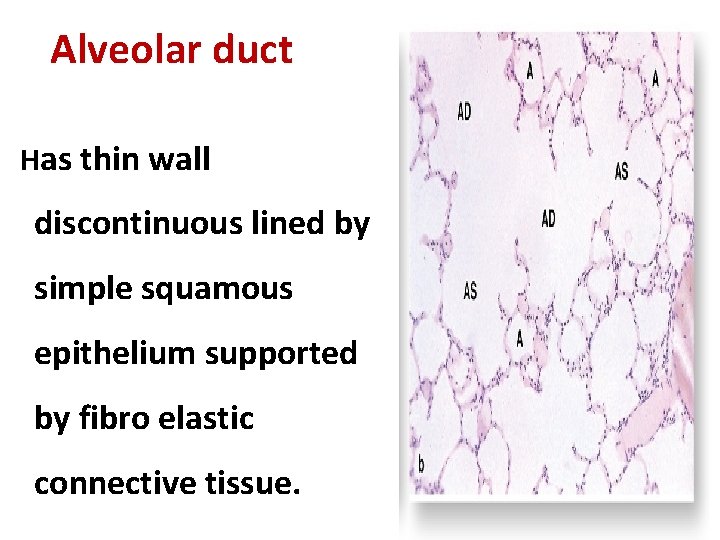
Alveolar duct Has thin wall discontinuous lined by simple squamous epithelium supported by fibro elastic connective tissue.

Respiratory bronchiole Alveolar duct Terminal bronchiole Lung alveoli
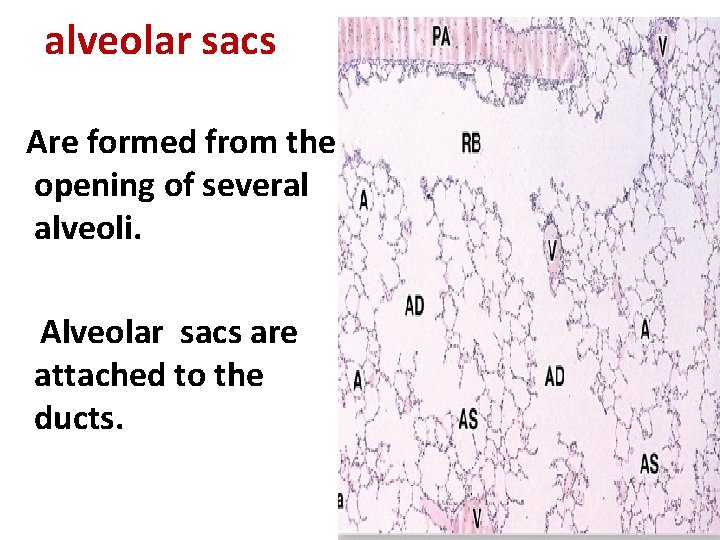
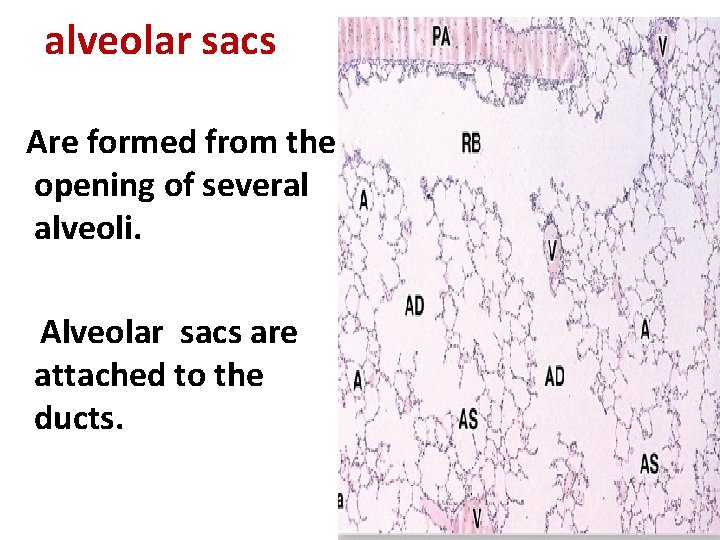
alveolar sacs Are formed from the opening of several alveoli. Alveolar sacs are attached to the ducts.
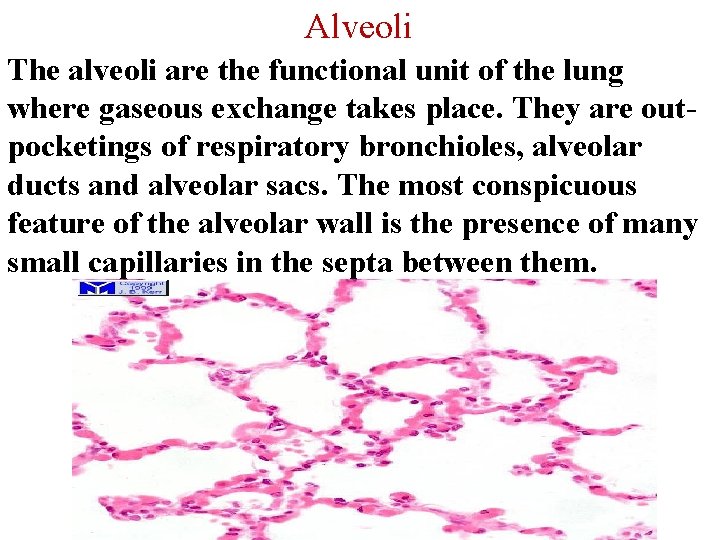
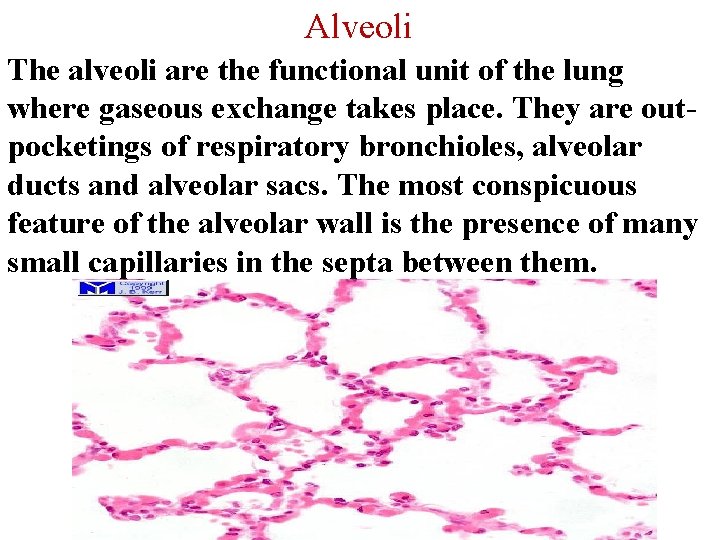
Alveoli The alveoli are the functional unit of the lung where gaseous exchange takes place. They are outpocketings of respiratory bronchioles, alveolar ducts and alveolar sacs. The most conspicuous feature of the alveolar wall is the presence of many small capillaries in the septa between them.

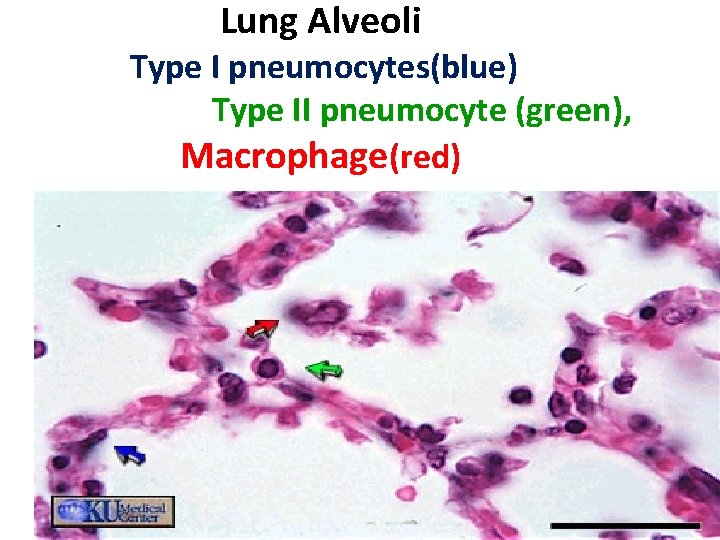
Lung Alveoli (pneumocytes) Alveolar cells - Type 1 They form about 45% of alveolar cells population. Are lined by an thin, simple squamous epithelium, their ends are connected by tight Junction to prevent leakage of tissue fluid into the alveolar lumen.

Alveolar Type II cells • They are roughly cuboidal with many microvilli on their free surface 1 - Synthesize and secrete a surfactant, it reduces surface tension across the squamous epithelium of the alveoli in the lungs.
• Prevent collapse of alveoli during expiration. • 2 -Regenerate themselves and replace the damaged type І pneumocytes. • The elastic fiber, few collagen gives support to alveoli.

Alveoli surrounded by fine elastic fibers Alveolar macrophages – “dust cells - usually free in the alveolar lumen, and in tissues between alveoli.
• Dust cells (macrophages) • Their role is to clear the lungs of invading bacteria and inspired particulate material (eg dust and carbon particles).
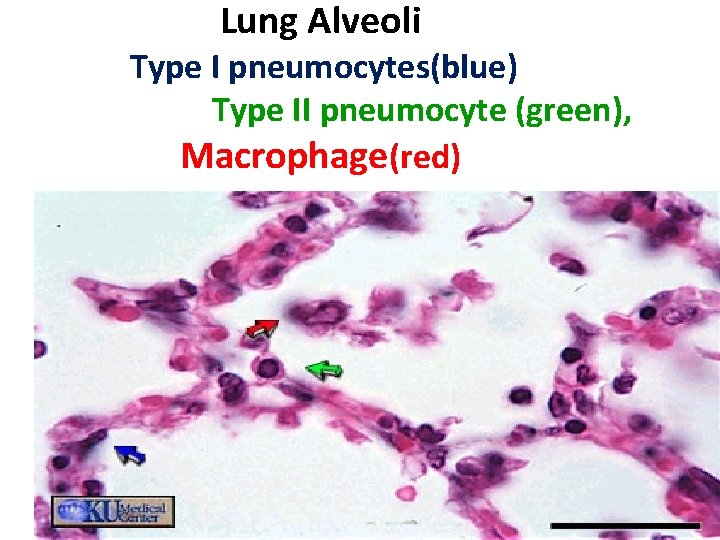
Lung Alveoli Type I pneumocytes(blue) Type II pneumocyte (green), Macrophage(red)

The blood-air barrier(respiratory membrane) The blood-air barrier prevents air in gaseous form from mixing with the blood. -Type I alveolar cells lining the alveolus. -Non-fenestrated (continuous) endothelium of capillary

The blood-air barrier *-Basal lamina of both alveolar cells and capillary endothelial cells (fused in some areas) significance?